Abstract
Lung cancer is the leading cause of cancer-related mortality in the United States and around the world. There are > 90 million current and ex-smokers in the United States who are at increased risk of lung cancer. The published data from the National Lung Screening Trial (NLST) suggest that yearly screening with low-dose thoracic CT scan in heavy smokers can reduce lung cancer mortality by 20% and all-cause mortality by 7%. However, to implement this program nationwide using the NLST inclusion and exclusion criteria would be extremely expensive, with CT scan costs alone > $2 billion per annum. In this article, we offer a possible low-cost strategy to risk-stratify smokers on the basis of spirometry measurements and emphysema scoring by radiologists on CT scans.
Lung cancer is a global public health problem, causing 1.2 million deaths per year.1 In the early stages, it can be cured with surgery; however, most non-small cell lung cancer (NSCLC) cases are diagnosed in advanced stages when curative therapy is usually not feasible. Thus, the best hope of reducing the burden of lung cancer in the United States and elsewhere is with prevention and early detection. The publication by the National Lung Screening Trial (NLST) offers new hope for reducing lung cancer mortality through screening of heavy smokers.2 The study showed that yearly lung cancer screening with low-dose thoracic CT scan for 3 years reduced lung cancer mortality by 20% and all-cause mortality by 7% compared with screening with chest radiography alone in ex-smokers and current smokers between the ages of 55 and 74 years who had at least 30 pack-years of smoking history.2 However, these promising data are counterbalanced by some sobering realities. In the United States, there are approximately 9 million people who fulfill the entry criteria for the NLST study. To screen these individuals, the CT scan costs alone could be > $2 billion per year.3 These costs do not include subsequent follow-up CT scans and other diagnostic imaging studies such as PET scans or invasive procedures such as bronchoscopy, mediastinoscopy, or needle biopsies, which are often needed in the work-up of suspicious-appearing lung nodules.
Another important conundrum is what to do with individuals who have “normal” or near-normal baseline CT scans. What advice should be given to such individuals? Should they be told that their risk of lung cancer is negligible and that additional screening CT scans are not needed? Or should they be advised to have yearly CT scans until age 75 years? Or screening CT scans every 2 to 5 years? Neither NLST nor the Dutch Belgian randomized lung cancer screening trial (Nederlands Leuvens Longkanker Screenings Onderzoek [NELSON])4 will be able to address this critically important question adequately. However, the early findings from NLST suggest that a “normal” baseline CT scan offers no guarantees to the patients. In that study, many who did not have a suspicious lesion on the baseline CT scan developed new suspicious lesions in subsequent years of screening. Thus, a negative CT scan did not negate the need for future CT scans.
A Possible Solution?
A reasonable solution to this conundrum is accurate risk stratification. If we can find a low-cost but highly accurate clinical or biochemical “filter” (ie, algorithm) that can be applied to risk-stratify current and ex-smokers for screening, then low-dose CT screening may become economically acceptable. In this article, we evaluate the possible role of two low-cost strategies, spirometry and emphysema scoring on thoracic CT scans and for risk assessment of lung cancer in those who have already received a baseline CT scan.
FEV1 as a Marker of Lung Cancer Risk
It has been known for years that reduced lung function is a significant risk factor for lung cancer independent of smoking history.5 However, the value of FEV1 as a screening tool for lung cancer remains controversial. A study examined 3,806 subjects as part of an early lung cancer detection program6 and found that reduced FEV1 was a significant risk factor for lung cancer in a linear dose-dependent fashion. Even a relatively small reduction in lung function (eg, as little as 10%) resulted in a tripling of the risk of lung cancer, imposing an attributable risk for lung cancer of 37%. In this study, the c-statistic for FEV1 (ie, the ability of FEV1 to discriminate patients with lung cancer from those without) was 0.70, indicating good discrimination. The most optimal FEV1 cutoff in predicting lung cancer was 85% of predicted, which had a sensitivity of 53% and specificity of 79%.6 Interestingly, in this analysis, the relationship between reduced FEV1 and this risk of lung cancer was driven by lung cancers other than adenocarcinomas.
The study by Tammemagi et al7 provided supporting data on the role of FEV1 as a screening tool for lung cancer that complemented the findings of Calabrò et al.6 They found that although the risk of lung cancer was associated with reduced lung function, the relationship was modified by sex. In men, the relationship between reduced FEV1 and the risk of lung cancer was exponential, whereas in women the relationship was linear and relatively flat.7 By including an interaction term of FEV1 and sex, the c-statistic of the baseline model increased significantly from 0.70 to 0.75. Importantly, by considering FEV1 in the risk prediction model, smokers could be more accurately risk-stratified such that among those who were deemed low risk only 1.3% developed lung cancer during 8 years of follow-up (compared with 1.5% in a model that did not include FEV1), whereas 8.2% of high-risk smokers developed lung cancer (compared with 7.0% in a model that did not include FEV1) and 1.6% of those deemed intermediate risk developed lung cancer (compared with 2.6% in a model that did not include FEV1). If these findings can be validated in a large prospective study, it may be reasonable and cost-effective to target screening for the high-risk individuals, which in the study by Tammemagi et al7 constituted 60% of the cohort. By doing this, we may be able to reduce the overall cost of the screening program by 40%. As this study did not include emphysema assessment on CT scans, the incremental improvement in the risk classification with the addition of emphysema scores is not known. Nevertheless, the relative low cost of spirometry makes FEV1 an attractive tool for risk stratification.
Radiologic Assessment of Emphysema
The predominant risk factor for lung cancer is cigarette smoking, but although approximately 85% of lung cancer occurs in smokers, the majority of smokers do not develop lung cancer.8 Smoking is also a shared etiologic factor for emphysema, which is one of the major morphologic phenotypes of COPD. Some epidemiologic studies suggest a significant relationship between emphysema and lung cancer. Is there a plausible mechanism to link emphysema to lung cancer? The exact pathogenic mechanisms underlying the relationship between emphysema and lung cancer remain obscure. One theory is that emphysematous lungs demonstrate impaired ciliary clearance of particles and carcinogens and as such may be more susceptible to oncogenesis.5,9 Another theory suggests that the main pathway is through shared risk factors, including cigarette smoking and aging. The proinflammatory cascade triggered by cigarette smoke unleashes a cascade of cytokines, reactive oxygen species, and proteolytic stress that may promote lung destruction causing emphysema on one hand, and DNA mutagenesis causing lung cancer on the other.10 The fact that emphysema is associated with lung cancer, even when adjusted for smoking exposure, suggests that there is substantial interindividual variation in the risk imposed by cigarette smoke and that other factors, such as those related to genetic polymorphisms, may also be involved.11 Indeed, there are certain genetic loci that have been linked to both emphysema and lung cancer.12,13
Emphysema has traditionally been defined pathologically as permanent destruction of distal airspaces beyond the terminal bronchioles. With the advent of noninvasive chest imaging techniques, CT scanning has emerged as the radiographic tool of choice for the diagnosis and quantification of emphysema. In general, there are two methods of emphysema identification and quantification: one based on a visual scoring system performed by radiologists and the other based on a computer analysis of the overall density of the lungs (ie, densitometry).
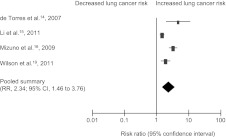
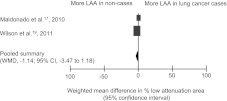
To understand the lung cancer risk imposed by emphysema, we searched the literature for English language articles examining the relationship between CT scan-diagnosed emphysema and lung cancer. Our search identified six studies that were eligible for analysis, two of which used a longitudinal design, whereas the other four were case-control studies (Table 1).14‐19 Of the 910 total lung cancer cases reported in the studies, 113 (12%) were small cell lung cancer, and 797 (88%) were NSCLC. The relative risk (RR) for lung cancer according to “any emphysema” reported by radiologists ranged from 1.9 to 4.7, with a pooled RR of 2.34 (95% CI, 1.46-3.76) (Fig 1). Two studies reported prevalence of “≥ 10% emphysema” of 20% and 37% for a mean prevalence of 24%. The pooled RR for lung cancer according to “ ≥ 10% emphysema” was 1.50 (95% CI, 1.36-1.65). All four of the semiquantitative studies found that emphysema was independently associated with lung cancer in multivariate analyses, with all of these studies adjusting for smoking status. Adjusted OR for lung cancer according to “any emphysema” ranged from 1.73 to 3.14 (Table 2). Two of the studies14,15 made adjustments for the presence of airflow limitation on spirometry and still showed a significant relationship between CT scan-based emphysema diagnosis and the risk of lung cancer. In contrast, quantitative analysis of emphysema using a computerized algorithm was not associated with lung cancer (Fig 2). However, these studies were limited by small sample sizes and there were substantial differences in the cutoffs of low attenuation areas used to categorize emphysema across these studies.
Table 1.
—Baseline Characteristics of Studies Evaluating the Relationship of CT Scan-Based Emphysema Diagnosis and the Risk of Lung Cancer
| Baseline Patient Characteristics |
Emphysema Evaluation |
||||||||||
| Study/Year | Population | Design | No. Patients | No. Lung Cancer Cases | % NSCLC Cases | % Men | Age, ya | % Current Smokers | Assessment Method | CT Scan Protocol | STROBE Score |
| de Torres et al14/2007 | Smokers aged ≥ 40 y in lung cancer screening trial; Spain | Cohort | 1,166 | 23 | 83 | 74 | 54 | NR | Semiquantitative; visual scoring of emphysema by two separate readers using five-point scale | Somatom Plus 4, Somatom Volume Zoom, Siemens scanner (single-slice helical), 20/43 mA, 120/140 kVp, 1.25/8 mm collimation | 20 |
| Wilson et al15/2008 | Smokers aged 50-79 y in lung cancer screening trial; Pittsburgh, PA | Cohort | 3,638 | 99 | 87 | 51.4 | NR | 60.2 | Semiquantitative; visual scoring of emphysema by three separate readers using five-point scale | GE Systems scanner (multidetector helical), 40 mA, 140 kVp, 2.5 mm collimation | 20 |
| Mizuno et al16/2009 | Controls from lung cancer screening trial, cases from admissions to academic hospital; Japan | Case-control | 564 | 141 | 89 | 75.9 | Median 63 (cases), 62 (controls) | 31.7 | Semiquantitative; based on % low-attenuation area using defined scoring system; threshold −700 HU; assessed by four separate readers | LightSpeed, GE Healthcare scanner, 110 mA,120 kVp, 1.25 mm collimation (cases); Aquilion, Toshiba scanner (both multidetector helical), 50 mA,120 kVp, 2 mm collimation (controls) | 18 |
| Maldonado et al17/2010 | Smokers aged ≥ 50 y in lung cancer screening trial; Rochester, MN | Case-control | 441 | 64 | 88 | 38.3 | 62.4 | 58 | Quantitative; % low-attenuation voxels/total lung volume on 3D reconstruction; threshold < −900 HU | High Speed Advantage, GE Systems scanner (helical mode), 40 mA, 120 kVp, 5 mm collimation | 20 |
| Li et al18/2011 | Controls from lung cancer screening trial in smokers aged ≥ 50 y, cases from observational lung cancer study; Rochester, MN | Case-control | 1,015 | 565 | 87 | 60 | 66.8 | 42.7 | Semiquantitative; visual estimate of % emphysema assessed by one reader; threshold < −950 HU | Not specified; all scans obtained using standard-dose protocol | 20 |
| Wilson et al19/2011 | Smokers aged 50-79 y in lung cancer screening trial; Pittsburgh, PA | Case-control | 234 | 117 | 87 | 52.1 | NR | 82.1 | Semiquantitative; visual scoring of emphysema by three separate readers using 5-point scale; quantitative; % low-attenuation voxels/total lung volume on 3D reconstruction; threshold < −910 HU | GE LightSpeed scanner (multidetector helical), mean 24.4 mA, 120/140 kVp, 2.5 mm collimation | 18 |
3D = three-dimensional; HU = Hounsfield Units; NR = not reported or impossible to ascertain.
Mean, unless otherwise specified
Figure 1.
The presence of any emphysema on CT scans and the risk of lung cancer. Emphysema was assessed on a semiquantitative visual scale. RR = relative risk.
Table 2.
—Multivariate Analysis of Lung Cancer Risk According to CT Scan-Diagnosed Emphysema
| Study | Extent of Emphysema | OR | 95% CI | Covariates |
| Semiquantitative/visual | ||||
| de Torres et al14/2007 | Any | 2.51 | 1.01-6.23 | Age, sex, smoking history, airflow obstruction |
| Wilson et al15/2008 | Any | 3.14 | 1.91-5.15 | Age, sex, smoking history, airflow obstruction |
| < 10% | 2.48 | 1.37-4.49 | ||
| 10%-25% | 4.43 | 2.53-7.79 | ||
| ≥ 25% | 2.56 | 1.26-5.20 | ||
| Mizuno et al16/2009 | Any | 1.73 | 1.02-2.94 | Age, sex, smoking history, airflow obstruction, lung restriction, fibrosis/ground glass attenuation |
| Li et al18/2011 | Any | 2.79 | 2.05-3.81 | Pack-years, other lung disease, family history of lung cancer |
| ≥ 5% | 3.8 | 2.78-5.19 | ||
| ≥ 10% | 3.33 | 2.30-4.82 | ||
| Quantitative | ||||
| Maldonado et al17/2010 | % Emphysema as continuous variable | 1.04 (NS) | 0.82-1.33 | Age, sex, smoking history |
| < 5% | 1.00 (NS) | NR | ||
| 5%-9% | 1.90 (NS) | 0.90-4.03 | ||
| 10%-14% | 2.17 (NS) | 0.96-4.91 | ||
| ≥ 15% | 1.57 (NS) | 0.73-3.37 | ||
| Lung volume as continuous variable | 1.02 | 1.00-1.03 |
NS = not statistically significant. See Table 1 legend for expansion of other abbreviation.
Figure 2.
The relationship between LAA on CT scans and the risk of lung cancer. LAA = low attenuation area; WMD = weighted mean difference.
The reason for the discordance in the finding between visual scoring of emphysema and quantitative emphysema scores is unclear. However, in general, radiologists look beyond low-attenuation areas for more subtle but complex signs of emphysema, such as “holes” in the parenchyma.20 This approach, although seemingly more crude than quantitative assessment of emphysema, may be more discerning than a Hounsfield Unit (HU)-based threshold, especially in experienced hands. A diagnosis of emphysema on CT scan relies on the identification of very specific CT scan findings. These are clearly defined by the Fleischner Society as focal areas or regions of low attenuation, typically without visible walls.21 This strict definition allows the radiologist to differentiate emphysema from other low-attenuation abnormalities in the chest, such as pulmonary cysts, areas of air trapping, mosaicism with oligemia, and image noise. All of these abnormalities pose a significant issue for a HU threshold-based computerized segmentation algorithm.
Going forward, several issues need to addressed and clarified before CT scan-based emphysema scores (both visual- and quantitative-based scoring systems) can be used to risk-stratify patients for lung cancer. First, it is essential that future studies use similar or preferably the same scoring system to estimate emphysema on CT scans. For the visual approach, one reasonable scoring system is that proposed by Goddard et al.22 It is a four-point quartile scoring system with a score of 1 given if < 25% of the lobe is affected and 4 if > 75% of a lobe is affected. Although this scoring system is rudimentary, it is reproducible and affords a consistent estimation of the burden of disease. For quantitative analysis, the extent of emphysema can be estimated using the threshold method quantifying the percent of voxels with an apparent x-ray attenuation value below certain thresholds (eg, −950 HU), and the size of the emphysematous lesions may be estimated using the low-attenuation cluster method, which takes the slope of the relationship between the cumulative size of the low attenuation areas plotted against the cumulative number of lesions on a log-log scale. If possible, both of these measures should be used in future lung cancer studies, as they provide complementary information.
Summary and Future Directions
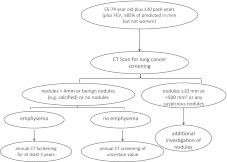
Lung cancer screening with annual CT scans will be prohibitively expensive unless some filters are in place to target high-risk subjects for screening. No such tools currently exist that can guide policy makers and clinicians to develop rational and cost-effective screening strategies. There are some very intriguing data on FEV1 and CT scan-based emphysema scores that suggest that with additional studies these measurements could be incorporated into clinically useful decision aids for clinicians (Fig 3). Until more data are available, a reasonable strategy for lung cancer screening with CT scans is to first identify a group at high risk for lung cancer. As suggested by NLST, such a group may be composed of current or ex-smokers between the ages of 55 and 74 years2 with ≥ 30 pack-years of smoking history.23 The screening tool can be further refined using additional sociodemographic and clinical data24,25 (eg, environmental smoke exposure) as well as FEV1 as suggested by Tammemagi et al.7,23 For those with prior CT scans (and without suspicious nodules), the presence of emphysema can be incorporated into a risk-management strategy for future CT scan-based screening. There are > 94 million adult Americans who are current or ex-smokers and, thus, are at enhanced risk of lung cancer. More than $28 billion per annum would be required to screen these individuals annually with a low-dose CT scan, making this a cost-prohibitive strategy. There is a pressing need to develop some clinical filters for screening. With the available CT scan and spirometry data, NELSON, NLST, and other study groups have an opportunity to determine whether FEV1 and emphysema scores are indeed predictive of lung cancer and most importantly can be used, in addition to traditional markers such as smoking status and age, to develop a simple clinical algorithm for accurate risk-stratification.
Figure 3.
Proposed schema for lung cancer screening using CT scan. Based on the National Lung Screening Trial data, we propose that screening programs target smokers 55 to 74 years of age with at least 30 pack-years of smoking history. In addition, we suggest incorporating spirometry data to a risk stratification algorithm for the initial screening CT scan, especially in men. All suspicious nodules should be investigated. For those without significant nodules, we suggest evaluating the CT scan for emphysema by a trained radiologist. Even trace findings of emphysema should prompt additional screening studies. The absence of emphysema, on the other hand, may lead to fewer screening CT scans. Those with nodules between 4 and 10 mm may require more frequent CT scan follow-up.
Acknowledgments
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Coxson is a recipient of GlaxoSmithKline Clinical Scientist Award. Dr Sin is supported by a Canada Research Chair in COPD. Drs Zurawska, Jen, Lam, and Leipsic have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The sponsors had no role in the design of the study, the collection and analysis of the data, or in the preparation of the manuscript.
Abbreviations
- HU
Hounsfield Unit
- NLST
National Lung Screening Trial
- NSCLC
non-small cell lung cancer
- RR
relative risk
Footnotes
Funding/Support: Dr Coxson is supported in part by the University of Pittsburgh COPD Specialized Centers of Clinically Oriented Research and the National Heart, Lung, and Blood Institute, National Institutes of Health [Grants 1P50 HL084948 and R01 HL085096] to the University of Pittsburgh. Dr Sin is supported by a Canada Research Chair Award in COPD, University of British Columbia.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (http://www.chestpubs.org/site/misc/reprints.xhtml).
References
- 1.Youlden DR, Cramb SM, Baade PD. The International Epidemiology of Lung Cancer: geographical distribution and secular trends. J Thorac Oncol. 2008;3(8):819–831. doi: 10.1097/JTO.0b013e31818020eb. [DOI] [PubMed] [Google Scholar]
- 2.National Lung Screening Trial Research Team Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black WC. Cost effectiveness of screening in the National Lung Screening Trial, 2011. National Cancer Institute Web site. http://deainfo.nci.nih.gov/advisory/ncab/158_0611/presentations/1230dBlack.pdf. Accessed September 26, 2011.
- 4.Dutch Belgian randomised lung cancer screening trial (NELSON) NELSON Web site. http://www.nelsonproject.nl/. Accessed September 26, 2011.
- 5.Wasswa-Kintu S, Gan WQ, Man SF, Pare PD, Sin DD. Relationship between reduced forced expiratory volume in one second and the risk of lung cancer: a systematic review and meta-analysis. Thorax. 2005;60(7):570–575. doi: 10.1136/thx.2004.037135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calabrò E, Randi G, La Vecchia C, et al. Lung function predicts lung cancer risk in smokers: a tool for targeting screening programmes. Eur Respir J. 2010;35(1):146–151. doi: 10.1183/09031936.00049909. [DOI] [PubMed] [Google Scholar]
- 7.Tammemagi MC, Lam SC, McWilliams AM, Sin DD. Incremental value of pulmonary function and sputum DNA image cytometry in lung cancer risk prediction. Cancer Prev Res (Phila) 2011;4(4):552–561. doi: 10.1158/1940-6207.CAPR-10-0183. [DOI] [PubMed] [Google Scholar]
- 8.Alberg AJ, Ford JG, Samet JM. American College of Chest Physicians Epidemiology of lung cancer: ACCP evidence-based clinical practice guidelines (2nd ed) Chest. 2007;132(suppl 3):29S–55S. doi: 10.1378/chest.07-1347. [DOI] [PubMed] [Google Scholar]
- 9.Lee G, Walser TC, Dubinett SM. Chronic inflammation, chronic obstructive pulmonary disease, and lung cancer. Curr Opin Pulm Med. 2009;15(4):303–307. doi: 10.1097/MCP.0b013e32832c975a. [DOI] [PubMed] [Google Scholar]
- 10.Herbst RS, Heymach JV, Lippman SM. Lung cancer. N Engl J Med. 2008;359(13):1367–1380. doi: 10.1056/NEJMra0802714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwartz AG, Ruckdeschel JC. Familial lung cancer: genetic susceptibility and relationship to chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173(1):16–22. doi: 10.1164/rccm.200502-235PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lambrechts D, Buysschaert I, Zanen P, et al. The 15q24/25 susceptibility variant for lung cancer and chronic obstructive pulmonary disease is associated with emphysema. Am J Respir Crit Care Med. 2010;181(5):486–493. doi: 10.1164/rccm.200909-1364OC. [DOI] [PubMed] [Google Scholar]
- 13.Wauters E, Smeets D, Coolen J, et al. The TERT-CLPTM1L locus for lung cancer predisposes to bronchial obstruction and emphysema. Eur Respir J. 2011;38(4):924–931. doi: 10.1183/09031936.00187110. [DOI] [PubMed] [Google Scholar]
- 14.de Torres JP, Bastarrika G, Wisnivesky JP, et al. Assessing the relationship between lung cancer risk and emphysema detected on low-dose CT of the chest. Chest. 2007;132(6):1932–1938. doi: 10.1378/chest.07-1490. [DOI] [PubMed] [Google Scholar]
- 15.Wilson DO, Weissfeld JL, Balkan A, et al. Association of radiographic emphysema and airflow obstruction with lung cancer. Am J Respir Crit Care Med. 2008;178(7):738–744. doi: 10.1164/rccm.200803-435OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mizuno S, Takiguchi Y, Fujikawa A, et al. Chronic obstructive pulmonary disease and interstitial lung disease in patients with lung cancer. Respirology. 2009;14(3):377–383. doi: 10.1111/j.1440-1843.2008.01477.x. [DOI] [PubMed] [Google Scholar]
- 17.Maldonado F, Bartholmai BJ, Swensen SJ, Midthun DE, Decker PA, Jett JR. Are airflow obstruction and radiographic evidence of emphysema risk factors for lung cancer? A nested case-control study using quantitative emphysema analysis. Chest. 2010;138(6):1295–1302. doi: 10.1378/chest.09-2567. [DOI] [PubMed] [Google Scholar]
- 18.Li Y, Swensen SJ, Karabekmez LG, et al. Effect of emphysema on lung cancer risk in smokers: a computed tomography-based assessment. Cancer Prev Res (Phila) 2011;4(1):43–50. doi: 10.1158/1940-6207.CAPR-10-0151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson DO, Leader JK, Fuhrman CR, Reilly JJ, Sciurba FC, Weissfeld JL. Quantitative computed tomography analysis, airflow obstruction, and lung cancer in the Pittsburgh lung screening study. J Thorac Oncol. 2011;6(7):1200–1205. doi: 10.1097/JTO.0b013e318219aa93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gietema HA, Müller NL, Fauerbach PV, et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) investigators Quantifying the extent of emphysema: factors associated with radiologists’ estimations and quantitative indices of emphysema severity using the ECLIPSE cohort. Acad Radiol. 2011;18(6):661–671. doi: 10.1016/j.acra.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246(3):697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 22.Goddard PR, Nicholson EM, Laszlo G, Watt I. Computed tomography in pulmonary emphysema. Clin Radiol. 1982;33(4):379–387. doi: 10.1016/s0009-9260(82)80301-2. [DOI] [PubMed] [Google Scholar]
- 23.Tammemagi CM, Pinsky PF, Caporaso NE, et al. Lung cancer risk prediction: Prostate, Lung, Colorectal And Ovarian Cancer Screening Trial models and validation. J Natl Cancer Inst. 2011;103(13):1058–1068. doi: 10.1093/jnci/djr173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bach PB, Kattan MW, Thornquist MD, et al. Variations in lung cancer risk among smokers. J Natl Cancer Inst. 2003;95(6):470–478. doi: 10.1093/jnci/95.6.470. [DOI] [PubMed] [Google Scholar]
- 25.Spitz MR, Hong WK, Amos CI, et al. A risk model for prediction of lung cancer. J Natl Cancer Inst. 2007;99(9):715–726. doi: 10.1093/jnci/djk153. [DOI] [PubMed] [Google Scholar]