Abstract
Introduction:
This study aimed to evaluate the effectiveness of exercise and token-behavior therapy on the negative symptoms of schizophrenic patients.
Objective:
Comparison of the effectiveness of exercise and token-behavior therapy on the negative symptoms of schizophrenic patients.
Methods:
This research was a randomized controlled clinical trial that was done on 45 schizophrenic patients, hospitalized in Rasht, Iran. Through systematic random allocation, the samples were placed in one control and two intervention groups, 15 patients in each. To assess the negative symptoms, the scale for the assessment of negative symptoms (SANS) was used. The effect of the interventions used (exercise and token-behavior therapy) was studied by completing the relevant checklists before and after using the interventions, and then, by comparing it with that of the studied control group. In order to analyze the collected data, one way ANOVA and Bonferroni's test and SPSS software were used.
Results:
Analyses showed that the token reinforcement approach was highly and significantly more effective than exercise for reducing the negative symptoms in schizophrenic patients (–36 ± 7 vs. –21 ± 8, respectively; P<0.001). Exercise was also shown to have a highly significant advantage over no therapy, in controls, to improve the negative symptoms in schizophrenic patients (–25 ± 8 vs. 0.2 ± 1.08, respectively; P<0.001).
Conclusion:
Both exercise and token-behavior therapies, along with drug treatment, are very effective in reducing the negative symptoms of schizophrenia; but the impact of token therapy issignificantly higher.
Keywords: Exercise, negative symptoms, schizophrenia, therapy, token-behavior
INTRODUCTION
Schizophrenia is a mental disorder with an unspecified cause and variable symptoms. The term was first coined by E. Blueler, in 1908.[1] This disease is characterized by the inability to understand or to express the reality. Generally, schizophrenia represents two series of symptoms: Positive and negative symptoms:[2–4] Delusions, disintegrated thinking and speech, heightened perceptions and hallucinations, and irrelevant reactions can be considered as positive symptoms. On the other hand, the negative symptoms are the ‘Pathological Deficits’ of the personality, which the individual has, but can include speechlessness, slow and superficial responses, losing one's free will, and escaping or withdrawing from the society. It is not far from reality to say that there often is no cure for this disease; so our goal from drug therapy is to control the disease, especially when it is diagnosed in its early stages.[2] Generally, the aim of treatment is to help the patient return to the real world. By and large, treatment starts with medications that reduce the symptoms. Then it continues with behavior therapy and rehabilitation, which help the individual to regain skills and behavioral patterns. These therapeutic approaches are used to reduce multiple disorders and to affect various dimensions of the disease. Martin and Pear[5] described the applied fields of behavioral methods. Behaviors for which these methods have been used vary from simple motional behaviors to complicated mental skills of problem solving. They have been increasingly used in education and training, social working, nursing, clinical psychology, psychotherapy, social psychology, medical practice, rehabilitation medicine, the working, industry, and in exercising.[5] Several researches have been conducted on the effectiveness of mental and physical rehabilitation for chronic schizophrenic patients.[6–12] Exercise is proposed as an effective method of managing negative symptoms in schizophrenic patients.[13] A study investigated the beneficial impacts of exercise on both the physical and mental fitness of schizophrenic patients and showed that the patients who underwent exercise, experienced an improvement in both the investigated parameters.[14] Researches on the feasibility of the mentioned methods for the treatment of schizophrenic patients in Iran are very limited. A study by Yasreby et al.[15] reported the positive effect of using social skills and mental-social rehabilitation in reducing negative symptoms. Also, the positive effects of these methods are observed in studies conducted by Ahmadzadeh et al.,[16] Mehrabi,[17] and Foruzandeh et al.[18] However, in none of the above-mentioned studies, have the investigators compared two rehabilitative methods with each other. The current study, however, aims to evaluate the effectiveness of the two rehabilitative methods on controlling the negative symptoms of schizophrenia in our patient population from Guilan Province, Iran.
METHODS
A randomized controlled clinical trial was conducted on 45 schizophrenic patients, hospitalized at Asayesh Chronic Psychiatric Care Center, in Rasht, Guilan Province, Iran. Shamlou [REFF] states that the most suitable number of patients to take part in every treatment group is six to nine and that each group should not have more than 15 people. By taking this point into consideration and after doing a pre-test, 45 individuals, who had the qualifications for being included in the study were randomly selected and placed in one control and two intervention groups (15 patients in each). Criteria for inclusion were having at least a three-year history of the disease since its onset, being a male, being 20 to 50 years old, not suffering from other mental diseases along with schizophrenia, not being mentally retarded or suffering from brain damage and having an active record in the Headquarters for the Welfare of Chronic Schizophrenia Patients. The research tool was the scale for the assessment of negative symptoms (SANS), designed by N. Andreasen (1984), for an extensive assessment of the negative symptoms of schizophrenia. The scale had 24 articles that were organized as five subscales and each article was scored on a 0 – 5 basis (1).
Given that in cases of applying drug and psychological treatments to hospitalized patients in the aforementioned center, there were written consents from the patients’ parents or other legal guardians, the clinical trial was performed immediately after specifying the groups. For data collection, trained assessors implemented the research tool in the intervention and control groups as a pre-test. Subsequently, therapeutic interventions (exercise and token-behavior therapy) were applied to the intervention groups in the form of two-hour sessions, at three sessions a week, for a period of three months. After applying the interventions, a post-test was performed on the three groups, by the same assessors, using the above-mentioned tool.
Statistical analyses
Data were analyzed using descriptive statistical methods (mean and standard deviation) and one-way ANOVA for continuous variables. Bonferroni's test was used for multiple comparisons. Nonparametric tests did not change the results. SPSS v. 17.0 software (SPSS Corp, Chicago, IL, USA) was used for analyses. A P value of less than 0.05 was used as the significance level.
RESULTS
Forty-five schizophrenic patients who were hospitalized at Asayesh Chronic Psychiatric Care Center in Rasht were studied. Table 1 shows and compares the demographic and study test results regarding the three study groups. The demographic data were not different between the study groups. Furthermore, no significant difference was observed between the groups regarding the rate of negative symptoms defined by the pre-test results.
Table 1.
Mean values of the pre- and post-tests, modified means, and standard deviations of the dependent variable of negative symptoms in the intervention and control groups
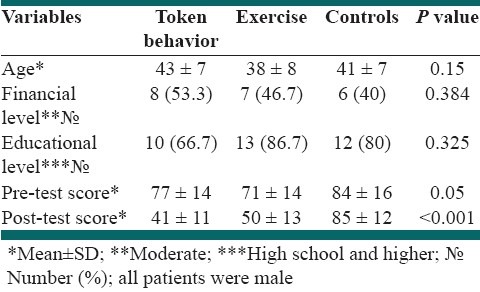
The average negative symptoms of the pre-test for exercise, behavior therapy, and control groups were 71.07, 76.73, and 84.67, respectively. However, after implementing the therapeutic interventions, the average negative symptoms in the exercise, behavior therapy, and control groups changed to 50.47, 41.20, and 84.87, respectively [Figure 1]. The test results showed a significant difference between all the three (P<0.001, for all). The highest improvement was observed in the token-behavior therapy, which was significantly higher than that in both the exercise and control groups (P<0.001, in both). The exercise therapy was also associated with a significantly higher improvement in the negative symptom scores than that in the control group (P<0.001); [Table 1].
Figure 1.
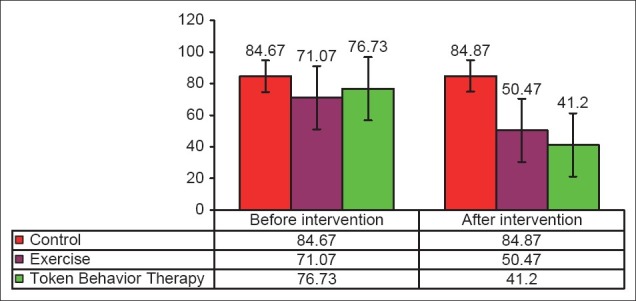
Mean and standard deviations of the negative symptoms of pre- and post-tests in the intervention and control groups
DISCUSSION
Schizophrenia is a multi-dimensional mental disorder that impairs patients on their ability to have a normal life and to communicate with the society. Unfortunately, there is no known treatment for this disorder. However, several medical and complementary therapies have been employed to improve the patients’ well-being and to enhance their ability to communicate and live in the society. What is obvious is that non-medical interventions, in the form of clinical occupational therapy help to improve a patient's condition, through creating a situational relationship triangle (activity-patient-therapist) and develop an environment within which patients experience the possibility to learn and to use their strength. Therefore, a patient-like atmosphere can be changed into a creative and constructive environment. As a result, the patient realizes his or her limitations and expands his or her social interactions. Considering the extent and destructive power of positive and especially negative symptoms of schizophrenia and their resistance to treatment, finding new treatment strategies to control these symptoms are of high importance.
In their studies, Torres et al.,[10] Buchain et al.,[11] and Blanchard and Cohen[12] showed the effect of complementary medicine, such as, occupational therapy, on the negative symptoms in schizophrenic patients. Also, Ahmadzadeh et al.,[16] Mehrabi,[17] and Foruzandeh et al.,[18] concluded that teaching social skills and occupational therapy helped the patients’ conditions to improve. The current study showed that patients who received interventions - both exercise and token-behavior therapy -showed pronounced improvements in their negative symptom scores, which were statistically significant; while in the control group which had not received any of the mentioned treatments, no changes were observed after the study. Several previous investigators also showed the positive impact of token reinforcement on various aspects of schizophrenia. A study by Wincze et al.,[19] showed that using token reinforcement could reduce the percentage of delusional speech in chronic paranoid schizophrenics. Moreover, a study by McCreadie et al.,[20] also showed that schizophrenic patients took advantage of token-behavioral therapy; but its beneficial effect was most prominent when patients were most initiative and cooperated best with the staff. Data on any possible positive impact of token therapy on the negative symptoms of schizophrenia was very limited in the current literature and a review of the literature found only three randomized controlled studies on this topic.[21] The same review article cumulating data of the mentioned studies proposed that the token-behavioral treatment could probably have some good effects on negative symptoms of schizophrenia; however this effect was not great. This finding was not totally consistent with that of ours, because in our study, token therapy was seen to have quite a substantial impact on the negative symptoms in schizophrenic patients.
The existing literature on the impact of exercise therapy on the symptoms of schizophrenia also suggests that exercise therapy is a beneficial method to implement in schizophrenic patients.[22] A pilot clinical trial by Beebe et al.,[23] studying the impact of exercise on the negative symptoms of schizophrenic patients showed a significant improvement even with only six minutes of walking a day for 16 weeks. Another trial by Marzolinia et al.,[24] showed that an even shorter period of a 12-week exercise therapy, with the same intensity, had a significant beneficial impact on the negative symptoms of schizophrenia.
As mentioned earlier, several studies have shown that both exercise and token-behavior therapies are valuable in the management of negative symptoms of schizophrenia. However, to the best of our knowledge, no study has yet compared the impact of these two therapeutic methods on the negative symptoms of schizophrenia, and our study represents the first evidence. In this study, we have found that the impact of these two therapies is not only highly and significantly associated with the improvements in the negative symptoms, but also, the token therapy is significantly more effective than exercise therapy alone. This finding is of outmost relevance, because, in cases of only minimal impact nothing is achieved from exercise therapy, we can use token therapy to reduce the negative symptoms in our schizophrenic patients.
There is no doubt that applying the designed interventions in the present study (exercise and token-behavior therapy) is an important aspect of rehabilitation, which would entail mental health. However, there are some limitations associated with this study, among which, the limited number of patients included as well as the short period of the study can be mentioned. We suggest that therapeutic interventions of the future studies be focused on a larger patient population, with special emphasizes on various age and gender groups, with a much longer period of study.
ACKNOWLEDGMENTS
We hereby thank the Director and Staff of the Asayesh Chronic Psychiatric Care Center for their kind cooperation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bleuler E. Die Prognose der Dementia Praecox—Schizo- phreniegruppe. Allegmeine Zeitschrift fiir Psychiatrie. 1908;65:436–64. [Google Scholar]
- 2.Sadock BJ, Gholipour A, Abolghasemi SH, Gholinia K, Saeed Taheri. Kaplan and Sadocks Synopsis of psychiatry Behavioral Sciences/Clinical psychiatry Synopsis of psychiatry. 10th ed. Philadelphia PA: Lippincott Williams and Wilkins; 2007. [Google Scholar]
- 3.Tkachev D, Mimmack ML, Ryan MM, Wayland M, Freeman T, Jones PB, et al. Oligodendrocyte dysfunction in schizophrenia and bipolar disorder. Lancet. 2003;362:798–805. doi: 10.1016/S0140-6736(03)14289-4. [DOI] [PubMed] [Google Scholar]
- 4.Ronald J. Abnormal Psychology. 6th ed. New York: Worth Publishers; 2007. [Google Scholar]
- 5.Martin G, Pear J. Behavior modification: What it is and how to do it. 4th ed. Upper Saddle River, New Jersey: Prentice-Hall International; 1992. [Google Scholar]
- 6.Cara E, McRae A. Psychosocial occupational therapy. New York: Delmer Publisher; 1998. [Google Scholar]
- 7.Brekke J, Ansel M. Intensity and continuity of services and functional outcomes in the rehabilitation of person with schizophrenia. Psychiatr Serv. 1999;50:248–56. doi: 10.1176/ps.50.2.248. [DOI] [PubMed] [Google Scholar]
- 8.Lieberman RP, Wallace CJ, Blackwell G. Skills training versus psychosocial occupational therapy for person with persistent schizophrenia. Am J Psychiatry. 1998;155:1087–91. doi: 10.1176/ajp.155.8.1087. [DOI] [PubMed] [Google Scholar]
- 9.Baker F, Thompson J. Two-year Outcome Of black Patients with chronic mental illness. Psychiat Serv. 1999;50:535–9. doi: 10.1176/ps.50.4.535. [DOI] [PubMed] [Google Scholar]
- 10.Torres A, Mendez LP, Merino H, Moran EA. Improving social functioning in schizophrenia by playing the train game. Psychiatr Serv. 2002;53:799–801. doi: 10.1176/appi.ps.53.7.799. [DOI] [PubMed] [Google Scholar]
- 11.Buchain PC, Vizzotto AD, Henna NJ, Elkis H. Randomized controlled trial of occupational therapy in patients with treatment-resistant schizophrenia. Rev Bras Psiquiatr. 2003;25:26–30. doi: 10.1590/s1516-44462003000100006. [DOI] [PubMed] [Google Scholar]
- 12.Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: Implications for assessment. Schizophr Bull. 2006;32:238–45. doi: 10.1093/schbul/sbj013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faulkner G, Biddle SZ. Exercise as an adjunct treatment for schizophrenia: A review of the literature. J Mental Health. 1999;8:441–57. [Google Scholar]
- 14.Beebe LH, Tian L, Morris N, Goodwin A, Allen SS, Kuldau J. Effects of exercise on mental and physical health parameters of persons with schizophrenia. Issues Ment Health Nurs. 2005;26:661–76. doi: 10.1080/01612840590959551. [DOI] [PubMed] [Google Scholar]
- 15.Yasraby K, Jazayeri AR, Poor Shahbaz A, Dowlatshahi B. Psychological efficacy - Social reduce negative symptoms and improving social skills of patients with chronic schizophrenia. Iran J Psychiat Clin Psychol. 2008;14:363–70. [Google Scholar]
- 16.Ahmadzadeh GH, Karim zadeh T. The relative frequency of positive and negative symptoms in chronic schizophrenia Isfahan. Res Med Sci. 2002;1:9–12. [Google Scholar]
- 17.Mehrabi T. Social skills training effect on the positive and negative symptoms of schizophrenic patients referred to community psychiatric centers in Isfahan.Congress on health promotion. Nursing and Midwifery Zanjan. Int J Prev Med. 2004;2:17–30. [Google Scholar]
- 18.Foruzandeh N, Akbari N, Kazemian A, Hassanpour DA, Safdari F, Foruzandeh M, et al. Occupational therapy effects on signs and symptoms of schizophrenia. J Med Sci Res Shahrkord. 2006;2:27–31. [Google Scholar]
- 19.Wincze JP, Leitenberg H, Agras WS. The effects of token reinforcement and feedback on the delusional verbal behavior of chronic paranoid schizophrenics. J Appl Behav Anal. 1972;5:247–62. doi: 10.1901/jaba.1972.5-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCreadie RG, Main CJ, Dunlop RA. Token economy, pimozide and chronic schizophrenia. Br J Psychiatry. 1978;133:179–81. doi: 10.1192/bjp.133.2.179. [DOI] [PubMed] [Google Scholar]
- 21.McMonagle T, Sultana A. Token economy for schizophrenia. Cochrane Database Syst Rev. 2000;3:CD001473. doi: 10.1002/14651858.CD001473. [DOI] [PubMed] [Google Scholar]
- 22.Gorczynski P, Faulkner G. Exercise therapy for schizophrenia. Cochrane Database Syst Rev. 2010;5:CD004412. doi: 10.1002/14651858.CD004412.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beebe LH, Tian L, Morris N, Goodwin A, Allen SS, Kuldau J. Effects of exercise on mental and physical health parameters of persons with schizophrenia. Issues Ment Health Nurs. 2005;26:661–76. doi: 10.1080/01612840590959551. [DOI] [PubMed] [Google Scholar]
- 24.Marzolinia S, Jensenc B, Melvillec P. Feasibility and effects of a group-based resistance and aerobic exercise program for individuals with severe schizophrenia: A multidisciplinary approach. Ment Health Phy Act. 2009;2:29–36. [Google Scholar]


