Abstract
Background
The study objectives were to compare and examine mammography use trends among ethnic/racial women in the context of United States Healthy People 2010 goals.
Methods
We analyzed pooled, multistage probability sample data from the 1996–2007 Medical Expenditure Panel Survey. Included in the sample were female respondents ages 40–75 years (n=64,811) from six ethnic/racial groups (Black, White, Mexican, Other Latinas, Puerto Rican and Cuban). The primary outcome was self-reported, past two-year mammography use consistent with screening practice guidelines.
Results
We found that for most U.S. women, the Healthy People 2010 mammography goal (70%) was achieved between 1996 and 2007. Puerto Rican and White women, respectively, had the highest mammography rates, and Black and Cuban women had rates that approached the 2010 goal.
Conclusion
Mexican Latinas reported the lowest rates of past two-year mammography; however, factors enabling healthcare access markedly moderated this lower likelihood. From 2000, Mexican Latinas’ mammography use was markedly below (10%) the Healthy People 2010 goal and remained there for the duration.
Impact
Our findings indicate that healthcare equity goals are attainable if efforts are made to reach a sizeable portion of vulnerable populations.
INTRODUCTION
Breast cancer is the most common cancer among women in the United States.(1) For breast cancer screening (BCS), mammography and clinical breast examination are the principal tools available to healthcare providers.(2) Early detection, accomplished through timely mammography screening, is one of the most effective methods for decreasing breast cancer mortality.(3) The National Healthcare Quality Report and the National Healthcare Disparities Report use mammography screenings as the most common indicator of healthcare quality.(4) Furthermore, many institutions and states in the country (e.g., California and Ohio) have widely adopted mammography screening as an objective healthcare quality and equity indicator on the “report cards.” (5, 6) Nationally, a core Healthy People 2010 objective includes “increasing the proportion of women aged 40-years and older who have received a mammogram within the preceding 2 years” to a national target of 70% for all women, regardless of ethnicity or race.(7)
Ethnic/racial “disparities” in mammography screening between White and Black women have decreased in the past decades;(4, 8) however, it is not clear from extant research if those increases apply to other ethnic/racial minorities. Research does suggest that Black, Latina, Native American, and Asian women are less likely than White women to receive adequate mammography screenings (9). However, this research does not differentiate between subcategories of Latino (i.e. Puerto Rican, Cuban, Mexican, and other Latinas), who may differ largely in health screening practices (10). Furthermore, although mammography “disparities” have been reported,(4) the mammography disparity is rarely well-defined and thereby rigorously tested to examine if ethnic/racial differences in healthcare meet commonly accepted criteria for a disparity.(11) In this study, we used the Institute of Medicine (IOM) Unequal Treatment committee definition which defines “healthcare disparity” as, “racial or ethnic differences in the quality of health care that are not due to access-related factors or clinical needs, preferences, and appropriateness of intervention” (p32) to examine mammography trends in the U.S. between ethnic/racial groups. (12) To do so, we examined eleven-years of mammography utilization among U.S. women ages 40-years and older and compare those trends between US White, Black, and disaggregated Latino, i.e. Cuban, Puerto Rican, Mexican, and other Latinos ethnic/racial minority groups. Secondly, we sought to determine which of the six ethnic/racial groups have achieved the Healthy People 2010 mammography goal and which have not. Third, we sought to determine which, if any, ethnic/racial groups met the IOM criteria for a healthcare disparity in mammography. To operationalize the IOM criteria, we used the Behavioral Model of Health Services Use.(13, 14)
METHODS
Data Collection
We used pooled data from the 1996 through 2007 full-year consolidated files of the U.S. Medical Expenditure Panel Survey (MEPS). Two survey years (1997 and 1999) were excluded due to the unavailability of the outcomes of interest. The MEPS is based on a complex sample design including clustering, stratification and probability weighting and uses a combination of face-to-face and phone interviews in English and Spanish. Detailed descriptions of the MEPS design are provided in several published reports.(15) MEPS staff generated a common variance structure that allows analysis of pooled data. Accounting for the common variance structure allows analysts to generate accurate standard errors and reach appropriate population inferences for estimated parameters. Each considered MEPS year includes a nationally representative survey of the non-institutionalized U.S. population. Post survey probability weights were generated by MEPS staff to adjust for disproportionalities, including nonresponse bias, and render the weighted sample distributions concordant with known population estimates. As a result, and despite the possible dependence between some observations, time trends could be examined by pooling data from the yearly cross sections. The annual survey response rates ranged from a high of 70.7% in 1996 to a low of 56.9% in 2007.
The MEPS is sponsored by the Agency for Health Care Research and the National Center for Health Statistics. The MEPS surveys generate data on health status, disability, quality of care, patient satisfaction, health insurance, person-level medical care use and expenditures, as well as several socioeconomic and demographic indicators. Our secondary data analysis for this study was reviewed and approved by the authors’ Institutional Review Boards.
Analysis of Subpopulation
We examined mammography use over an 11-year period among respondents from six ethnic/racial groups who self-identified as Black, Cuban, Mexican, Puerto Rican, other Latino, and non-Latino White. To examine Healthy People 2010 goals, we focused on past two-year mammography use within women 40-years and older (N=64,811). Establishing clinical need per the IOM criteria was less than straightforward due to historic changes and differences in American Cancer Society (ACS)(3) and U.S. Preventive Services Task Force (USPSTF) guidelines (16–20). Without clear guidance, we chose ages 40–74 years as our subpopulation with clinical needs as guided by randomized clinical trials findings and simulation work.(21–23) Appropriate methods for subpopulation analyses of complex sample survey data were used for estimation of descriptive parameters and analytic models.(24, 25)
Outcomes measures
Self-reported past two-year mammography use was the primary outcome of interest. Reported values ranged from 1 to 6 (1=past year; 2= past 2-years; 3=past 3-years; 4=past 5-years; 5=more than 5-years ago; and 6=never). Mammography screening within the past two-years was defined as concordant with ACS and USPSTF guidelines.(3), (16–20) Scores were collapsed to generate a dichotomous indicator grouping respondents reporting ACS guideline concordant use (within past 2-years) into one category, and those reporting non-concordant use (more than 2 years or never) into a second category.
Primary predictor
Ethnicity/race was the primary behavioral model of healthcare services use predisposing predictor used with the subpopulation of interest. The six ethnic/racial groups examined were Black, Cuban, Mexican, Puerto Rican, Other Latinas, and White (reference group).(13)
Covariates
To examine mammography trends, we included all women ages 40-years and older. To this end, four age categories were considered 40–49; 50–64; 65–74 and 75 years or older. Three age categories were modeled, including 40–49; 50–64 (reference group); and 65 to 74 years. Behavioral model of healthcare services use specific enabling factors were also modeled. Enabling factors included: 1) household income relative to the Department of Health and Human Services Poverty Guidelines using 5 categories, including ≤ 100% (reference group); <125%; <200%; <400%; or ≥400%; 2) education using four categories, including less than high school (reference group); high school; some college; and college or more; and 3) health insurance status measured as a three category indicator accounting for coverage by private insurance, public (government provided) insurance, and no insurance coverage (reference group). Survey year was included to account for time trends with year 1996 set as a reference.
Analytic Approach
Complex survey data procedures in the Stata software package 11.1 were used for all analyses (Stata Statistical Software, College Station, TX). Using Stata’s survey procedures, more specifically a Taylor Series Linearization approach to variance estimation, we adjusted for the common variance structure of the pooled MEPS sample when computing estimated standard errors. All estimates accounted for sampling probability weights to ensure adequate population level representation.
First, sample descriptive characteristics were calculated for the pooled sample (Table 1). Second, pooled ethnic (Table 2) and age specific prevalence estimates of mammography use were calculated. Third, mammography rates by age categories by ethnic/racial groups were generated for each survey year considered (Table 3), and linear trends in prevalence rates by group were plotted (Figure 1). Finally, a modified behavioral model of healthcare services use was applied to test IOM healthcare disparities criteria in mammography use by fitting logistic regression models to our outcome of interest using the subpopulation of women aged 40- to 74-years who reported past two-year screening (Table 4). Ethnicity/race was our principal predisposing factor of interest (Model 1). Consequently, factors enabling access to healthcare (household income, education, health insurance coverage) were added to account for attenuation effects on our principal predictor, ethnicity/race (Model 2). All models were age and survey year adjusted. Interaction effects between survey year and the main predictor were considered to account for differential time effects in BCS use by ethnic/racial groups. These interactions were largely not significant across all models suggesting that, controlling for our covariates, the trajectory of the time trend is shared by all the considered groups. Interaction effects were excluded from the final models to achieve better parsimony.
Table 1.
Sample demographics for women ages 40-years and older from pooled Medical Expenditure Panel Survey data (available years 1996–2007).
| N=64,811 | |||
|---|---|---|---|
|
| |||
| N | % | SE | |
|
|
|||
| Race/Ethnicity | |||
| Puerto Ricans | 1098 | 1.1 | 0.1 |
| Cubans | 710 | 0.5 | 0.0 |
| Mexicans | 7545 | 5.2 | 0.4 |
| Other Latinas | 2245 | 2.1 | 0.1 |
| Blacks | 10418 | 11.4 | 0.5 |
| Non-Latina Whites | 42793 | 79.7 | 0.6 |
| Age | |||
| 40–49 | 21796 | 33.0 | 0.4 |
| 50–64 | 23623 | 36.3 | 0.3 |
| 65–74 | 9846 | 15.3 | 0.2 |
| 75+ | 9546 | 15.5 | 0.3 |
| Education | |||
| Less than high school | 17352 | 19.8 | 0.4 |
| High school | 21863 | 35.8 | 0.4 |
| Some college | 12922 | 22.1 | 0.4 |
| College or more | 11895 | 22.3 | 0.5 |
| Family Incomea | |||
| <100% | 9779 | 10.2 | 0.2 |
| 100%–124% | 3738 | 4.6 | 0.1 |
| 125%–199% | 9921 | 13.7 | 0.2 |
| 200%–399% | 18670 | 29.5 | 0.3 |
| ≥ 400% | 22703 | 42.0 | 0.5 |
| Insurance Status | |||
| Private | 41704 | 72.8 | 0.4 |
| Public | 15360 | 18.9 | 0.4 |
| Uninsured | 7747 | 8.3 | 0.2 |
Relative to federal poverty level
Table 2.
Prevalence of past-two year mammography by ethnicity/race for women ages 40-years and older in the US. Results are from pooled Medical Expenditure Panel Survey data (available years 1996–2007).
| Mammography | |||
|---|---|---|---|
|
| |||
| % | SE | χ2 Test | |
|
|
|||
| Puerto Ricans | 72.5 | 1.7 | P<0.001 |
| Cubans | 68.3 | 3.1 | |
| Mexicans | 59.4 | 1.2 | |
| Other Latinas | 68.5 | 1.6 | |
| Blacks | 69.5 | 0.7 | |
| Non-Latina Whites | 71.5 | 0.4 | |
Table 3.
Prevalence of past-two year mammography by year and ethnicity/race for women ages 40-years and older in the US. Results are from pooled Medical Expenditure Panel Survey data (available years 1996–2007).
| Year | Overall | Puerto Ricans | Cubans | Mexicans | Other Latinas | Blacks | Non-Latina Whites | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | |
|
|
||||||||||||||
| 1996 | 65.1 | 0.9 | 72.1 | 5.8 | 79.3 | 6.8 | 57.7 | 3.7 | 66.6 | 5.2 | 62.8 | 2.4 | 65.6 | 0.9 |
| 1998 | 69.0 | 0.9 | 71.4 | 6.3 | 59.1 | 7.7 | 53.1 | 3.0 | 74.9 | 4.0 | 69.3 | 2.2 | 69.7 | 1.0 |
| 2000 | 71.5 | 1.0 | 75.1 | 4.5 | 78.2 | 5.4 | 61.7 | 2.6 | 65.1 | 4.2 | 69.2 | 1.8 | 72.5 | 1.1 |
| 2001 | 72.7 | 0.7 | 77.0 | 5.1 | 71.1 | 4.3 | 62.5 | 2.2 | 62.2 | 4.6 | 70.8 | 1.9 | 73.7 | 0.8 |
| 2002 | 72.8 | 0.6 | 69.3 | 4.8 | 76.7 | 4.8 | 62.1 | 2.2 | 62.6 | 4.2 | 71.9 | 1.6 | 73.8 | 0.7 |
| 2003 | 71.3 | 0.6 | 77.2 | 4.1 | 73.4 | 4.6 | 59.2 | 2.1 | 63.1 | 4.1 | 72.1 | 1.6 | 72.1 | 0.8 |
| 2004 | 71.2 | 0.7 | 71.1 | 4.3 | 63.2 | 10.7 | 62.0 | 2.9 | 73.5 | 3.0 | 69.4 | 1.6 | 72.1 | 0.8 |
| 2005 | 71.0 | 0.7 | 72.1 | 4.9 | 57.1 | 10.2 | 57.8 | 3.3 | 74.7 | 3.2 | 67.4 | 1.6 | 72.4 | 0.9 |
| 2006 | 70.5 | 0.8 | 74.7 | 4.4 | 67.3 | 7.5 | 57.5 | 2.2 | 75.1 | 3.3 | 69.5 | 1.4 | 71.4 | 0.9 |
| 2007 | 70.3 | 0.7 | 66.7 | 4.9 | 59.3 | 8.2 | 59.3 | 2.2 | 63.7 | 3.6 | 71.3 | 1.6 | 71.3 | 0.8 |
| Total | 70.6 | 0.4 | 72.5 | 1.7 | 68.3 | 3.1 | 59.4 | 1.2 | 68.5 | 1.6 | 69.5 | 0.7 | 71.5 | 0.4 |
| χ2 Test | P<0.001 | P=0.8241 | P=0.2076 | P=0.2785 | P<0.05 | P<0.05 | P<0.001 | |||||||
Figure 1.
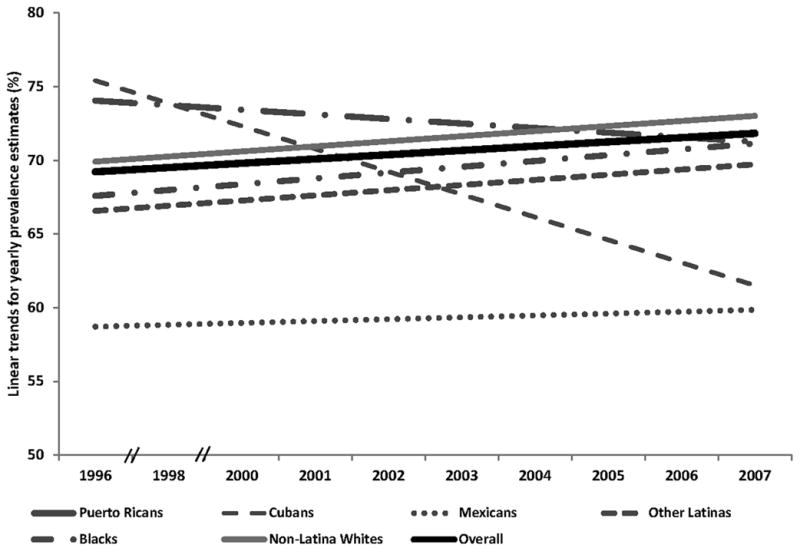
Mammography trends for women ages 40 years and older by Race/Ethnicity in the US. Results are from pooled Medical Expenditure Panel Survey data (available years 1996–2007).
Table 4.
Predictors of past-two year mammography use in the United States among women ages 40- to 74-years. Results are from logistic regression models using pooled Medical Expenditure Panel Survey data (1996–2007).
| Mammographya
|
||||
|---|---|---|---|---|
| Model 1b | Model 2c | |||
| ORd | 95 % CI | ORd | 95 % CI | |
| Race/Ethnicity | ||||
| Non-Latina Whites | 1.00 | ref | 1.00 | ref |
| Puerto Ricans | 1.03 | 0.83–1.28 | 1.55*** | 1.26–1.92 |
| Cubans | 0.76* | 0.55–1.04 | 1.13 | 0.84–1.53 |
| Mexicans | 0.56*** | 0.50–0.63 | 1.04 | 0.91–1.18 |
| Other Latinas | 0.80** | 0.69–0.94 | 1.25** | 1.05–1.49 |
| Blacks | 0.87*** | 0.80–0.94 | 1.22*** | 1.12–1.32 |
| Age (years) | ||||
| 40–49 | 0.61** | 0.58–0.65 | 0.58*** | 0.55–0.62 |
| 50–64 | 1.00 | ref | 1.00 | ref |
| 65–74 | 0.88*** | 0.82–0.95 | 0.97 | 0.89–1.05 |
| Education | ||||
| Less than high school | 1.00 | ref | ||
| High school | 1.23*** | 1.14–1.32 | ||
| Some college | 1.40*** | 1.28–1.54 | ||
| College or more | 1.67*** | 1.53–1.82 | ||
| Family Incomee | ||||
| <100% | 1.00 | ref | ||
| 100%–124% | 0.96 | 0.85–1.10 | ||
| 125%–199% | 1.07 | 0.98–1.16 | ||
| 200%–399% | 1.27*** | 1.16–1.39 | ||
| ≥ 400% | 1.82*** | 1.67–1.98 | ||
| Insurance | ||||
| Uninsured | 1.00 | ref | ||
| Private | 3.08*** | 2.82–3.37 | ||
| Public | 2.38*** | 2.16–2.62 | ||
Models control for survey year (not included in table)
Logistic regression model of past-two year mammography(0=No; 1=Yes) on main predictor (predisposing factor) race/ethnicity, controlling for age.
Logistic regression model of past-two year mammography(0=No; 1=Yes) on main predictor (predisposing factor) race/ethnicity, controlling for age and enabling factors including education, income and insurance.
Odds ratios
Relative to federal poverty level
P<0.01
P<0.05
P<0.10
RESULTS
Ethnic Differences
Prevalence estimates of past two-year mammography use for the six ethnic/racial groups are provided in Table 2. Overall, results show significant differences in pooled ethnic and racial averages (χ2= 28.1; P<0.001) with Mexican Latinas having the lowest prevalence of past two-year mammography (59.4%; SE=1.2). The prevalence estimates were largely comparable for the other groups. Puerto-Rican Latinas presented the highest average prevalence estimates (72.5%; SE=1.7).
Age Differences
Overall, age was a significant factor in mammography screening (χ2= 208.9; P<0.001). Women aged 50–64 reported the highest past-two year mammography use (77.0%; SE=0.5). Women in the oldest age category (75-years and older) reported the lowest screening use (59.2%; SE=0.9). Mammography use reported by women 40–49 and 65–74 year old were 66.9% (SE=0.5), and 74.9% (SE=0.7), respectively.
Time Differences
Overall, time trends for mammography were largely flat (Table 3). Past two-year mammography use estimates showed a statistically noticeable uptick from 1996 leading to a peak estimated prevalence in 2002 (72.8%; SE=0.6) followed by a slight decline lasting into 2007 (70.3%; SE=0.6). Time trends were not significant for Puerto Ricans, Cubans and Mexicans. The other Latinas group, Blacks, and non-Latino Whites presented a small, albeit significant, increase over time.
Disparity testing
To test if the ethnic/racial differences in mammography use met the IOM healthcare disparity criteria, we ran two logistic regression models. These results (Table 4) indicated that, controlling for survey year and age, Mexican Latinas had the lowest odds of reporting past two-year mammography use of all the ethnic/racial groups examined. Lower odds were also detected among the Other Latinas group and Blacks, compared to White women. The odds of past two-year mammography were lower for Cuban women relative to Whites, but the difference had only marginal statistical significance. Although Puerto Rican woman had the highest odds of past two-year mammography screening, those differences were not statistically distinguishable from those of White women.
Enabling factors (education, income, and insurance) completely moderated the statistical differences in past two-year mammography use between Mexican and White women. Moreover, accounting for enabling factors enhanced the likelihood of screening among Other Latinas, Blacks, and Puerto Ricans relative to Whites. Finally, higher education in general, reporting a family income that is above the set federal poverty level by 200% or more, and insurance coverage (both under private and public plans) increased the odds of reporting past two-year mammography use.
DISCUSSION
For many women in the United States, the Healthy People 2010 mammography goal (70%) was achieved between 1996 and 2007. Beginning in year 2000, the overall past-two year mammography target was met and remained relatively stable thereafter. Puerto Rican and White women, respectively, reported the highest mammography use which exceeded the screening criterion, and Black and Cuban women had rates that approached the Healthy People 2010 goal.(7) From 1996 to 2007, Mexican Latinas reported mammography rates that were markedly below (about 10% lower) the Healthy People 2010 goal and the other ethnic/racial groups examined, and remained for the duration. Similar to previous findings, the inequalities for Mexican Latinas we found were largely explained by factors that enable access to healthcare, such as healthcare insurance,(11, 26) and would not meet our use of the IOM criteria for a healthcare disparity. For Mexican Latinas, lack of insurance coverage lessens the likelihood of having a usual source of healthcare that could decrease opportunities for informed counseling and orders for cancer screening, including mammography.(10, 26–28) Lack of healthcare insurance, particularly for foreign-born Mexicans, may further widen the screening divide with other ethnic/racial groups of women. With Mexican Latinas being the largest and most rapidly growing group of Latinos in the U.S., our findings suggest public health efforts clearly specify appropriate targets for reducing ethnic/racial “disparities” in healthcare quality within this vulnerable population. Furthermore, our findings point to potential solutions for decreasing inequalities in cancer screening.
Our findings for Mexican Latinas suggest some reasons for the sustained mammography inequalities. First, the Mexican Latino population has the lowest household income and healthcare insurance rate of all major ethnic/racial groups in the U.S.(29)As our findings indicate, eliminating insurance inequalities has the potential for reducing the striking and unmoving differences in mammography that we observed between 1996 and 2007. Secondly, it may be that the inequalities in mammography use that we found have been simply overlooked. This could be due to the common practice of “lumping” ethnic/racial minorities.(11) Specifically, ethnic/racial minorities are not disaggregated in the National Healthcare Disparities Reports, Healthy People goals and most other state and private healthcare quality surveillance systems.(4, 30) When Latinos are disaggregated as recommended by the IOM report on Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement,(31) the pattern of ethnic/racial inequality we found herein become apparent.(14, 26, 32, 33) Current population estimates indicate that Latinos will comprise about one-third of the U.S. population in year 2050 and Mexican Latinos will remain the vast majority of them in the coming decades. Ignoring the changing ethnic/racial composition of the nation in setting healthcare quality and equity goals may ensure that the inequalities we found will persist. As new healthcare quality and equity goals are established, it becomes essential that the sights are properly trained on targeted populations and identification of needs to improve health services. Furthermore, once breast abnormalities are found some evidence suggests that diagnostic delays persist for non Hispanic Black and Hispanic/Latino populations despite health insurance coverage.(34)
Furthermore, breast cancer remains a leading cause of cancer death among Latinas, which suggests the need for better cancer screening methods and innovative strategies to encourage appropriate cancer screening. Mexican Latinas have the lowest mammography consistent with established screening practice guidelines, and the lowest prevalence of ever having had a lifetime mammogram.(26) Considering previous findings that Mexican Latinas may have above-average rates of pre-menopausal breast cancer,(35) and in the context of the USPSTF recommendations for women of average risk to begin breast cancer screening at age 50, mounting evidence suggests an interventionist role for public health practioners who serve this vulnerable population to discuss the risk of breast cancer. Early mammography screenings may assist in lowering rates among Mexican Latinas.
Readers should consider several caveats in evaluating our study. First, we imposed most of the IOM criteria for a healthcare disparity, but were unable to ascertain the preferences criterion. It is possible that the inequalities in mammography we observed relate to preferences founded in cultural differences. While we were unable to test this alternative explanation for the inequalities we found, our evidence indicates that the differences in mammography by ethnicity/race were related to the availability of health insurance. Nevertheless, examining ethnic/racial subgroup preferences for mammography may provide insights useful in meeting screening goals. Secondly, mammography use was ascertained by self-report, which is subject to recall and social-desirability biases.(36, 37) Previous studies of overestimation of mammography use have found differences based on age and ethnic/racial group, with African American women having the highest rates of over-reporting (24.4%), followed by Whites (19.3%) and then Latinas (17.9%).(2) As such, our estimates of mammography use may be inflated, and the potential bias is likely to have affected all groups. Additionally, it is unclear if overestimates of mammography reporting are similar between Latina ethnic subgroups.
Conclusions
Healthy People 2010 goals for ethnic/racial minority parity in mammography have been accomplished for most, but not all ethnic/racial minorities in the U.S., specifically not Mexican Latinas. Our findings indicate that mammography goals should reflect important characteristics of the ethnic/racial composition of the nation to ensure proper targets are set and met. Adequate epidemiologic evidence is essential to ensure ethnic/racial groups are not overlooked in establishing national and local healthcare goals. With the Healthy People 2020 national mammography objectives largely unchanged, it is essential that national healthcare priorities be modified to follow the changing demography and needs of all Americans. Further healthcare providers need to recognize the potential for increased risk of breast cancer in important, but underserved populations.
References
- 1.ACS. Breast Cancer Facts & Figures 2009–2010. Atlanta, GA: American Cancer Association; 2010. [Google Scholar]
- 2.Mandelblatt JS, Cronin KA, Bailey S, Berry DA, de Koning HJ, Draisma G, et al. Effects of Mammography Screening Under Different Screening Schedules: Model Estimates of Potential Benefits and Harms. Annals of Internal Medicine. 2009;151(10):738–747. doi: 10.1059/0003-4819-151-10-200911170-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cancer facts and figures 2010. Atlanta: American Cancer Society, Inc; 2010. [Google Scholar]
- 4.AHRQ. National Healthcare Disparities Report. Rockville: 2009. [Google Scholar]
- 5.Ritley D, Romano PS, Rainwater JA. Quality Performance Measurement in California: Findings and Recommendation. UC Davis Center for Healthcare Policy and Research; 2008. [Google Scholar]
- 6.Healthy Ohioans. [ www.odh.ohio.gov/ASSETS/.../canc2010.pdf]
- 7.Healthy People 2010 Midcourse Review. [ http://www.healthypeople.gov/data/midcourse/html/focusareas/FA03Objectives.htm]
- 8.Sassi F, Luft HS, Guadagnoli E. Reducing Racial/Ethnic Disparities in Female Breast Cancer: Screening Rates and Stage at Diagnosis. Am J Public Health. 2006;96(12) doi: 10.2105/AJPH.2005.071761. %U http://ajph.aphapublications.org/cgi/content/abstract/96/12/2165 %8 December 1, 2006):2165–2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith-Bindman R, Miglioretti DL, Lurie N, Abraham L, Barbash RB, Strzelczyk J, et al. Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Annals of Internal Medicine. 2006;144(8):541–553. doi: 10.7326/0003-4819-144-8-200604180-00004. [DOI] [PubMed] [Google Scholar]
- 10.Miranda PY, Tarraf W, Gonzalez HM. Breast cancer screening and ethnicity in the United States: implications for health disparities research. Breast Cancer Research and Treatment. 2011;128(2):535–542. doi: 10.1007/s10549-011-1367-8. [DOI] [PubMed] [Google Scholar]
- 11.Abraido-Lanza AF, Chao MT, Gammon MD. Breast and Cervical Cancer Screening Among Latinas and Non-Latina Whites. American Journal of Public Health. 2004;94(8):1393–1398. doi: 10.2105/ajph.94.8.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smedley BD, Stith AY, Nelson AR. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Board on Health Sciences Policy. Institute of Medicine; 2002. [Google Scholar]
- 13.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of health and social behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 14.González HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression Care in the United States: Too Little for Too Few. Arch Gen Psychiatry. 2010;67(1):37–46. doi: 10.1001/archgenpsychiatry.2009.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ezzati-Rice T, Rohde F, Greenblatt J. Sample design of the Medical Expenditure Panel Survey Household Component, 1998–2007. 2008. [Google Scholar]
- 16.American Cancer Society. Guidelines for the Early Detection of Cancer. [Google Scholar]
- 17.USPSTF: Screening for breast cancer: recommendations and rationale. Ann Intern Med. 2002;137:344–346. doi: 10.7326/0003-4819-137-5_part_1-200209030-00011. [DOI] [PubMed] [Google Scholar]
- 18.USPSTF: Screening for Breast Cancer: US Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- 19.Calonge N, Petitti DB, DeWitt TG, Dietrich AJ, Gregory KD, Grossman D, et al. Screening for breast cancer: U.S. preventive services task force recommendation statement. Annals of Internal Medicine. 2009;151(10):716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- 20.Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: An update for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2009;151(10):727–737. doi: 10.1059/0003-4819-151-10-200911170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nelson HD, Tyne K, Naik A, Bougatsos C, Chan B, Nygren P, Humphrey L. Evidence Syntheses. Agency for Healthcare Research and Quality; 2009. Screening for Breast Cancer: Systematic Evidence Review Update for the US Preventive Services Task Force. [PubMed] [Google Scholar]
- 22.Jørgensen KJ. Mammography reduces breast cancer mortality in women aged 39 Äì69 years; but harms may outweigh benefits in women under 50. Evidence Based Medicine. 2010;15(2):62–63. doi: 10.1136/ebm1045. [DOI] [PubMed] [Google Scholar]
- 23.Mandelblatt J, Schechter C, Yabroff K, Lawrence W, Dignam J, Extermann M, et al. Toward optimal screening strategies for older women. Journal of General Internal Medicine. 2005;20(6):487–496. doi: 10.1111/j.1525-1497.2005.0116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee ES, Forthofer RN. Analyzing Complex Survey Data. Sage Publications; 2005. [Google Scholar]
- 25.Cochran WG. Sampling Techniques. 3. New York: Wiley; 1977. [Google Scholar]
- 26.Miranda PY, Tarraf W, Gonzalez HM. Breast cancer screening and ethnicity in the United States: Implications for health disparities research. Breast Cancer Research and Treatment. 2011 doi: 10.1007/s10549-011-1367-8. [DOI] [PubMed] [Google Scholar]
- 27.AMA: Hispanic health in the United States Council on Scientific Affairs. Journal of the American Medical Association. 1991;265(2):248–252. [PubMed] [Google Scholar]
- 28.Beal A, Hernandez S, Doty M. Latino Access to the Patient-Centered Medical Home. Journal of General Internal Medicine. 2009;24(0):514–520. doi: 10.1007/s11606-009-1119-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Census: American Community Survey. 2008. [Google Scholar]
- 30.USDHHS. Healthy People 2010: Understanding and Improving Health. 2. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- 31.IOM. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: Institute of Medicine; 2009. [PubMed] [Google Scholar]
- 32.Bustamante AV, Chen J, Rodriguez HP, Rizzo JA, Ortega AN. Use of Preventive Care Services Among Latino Subgroups. American Journal of Preventive Medicine. 2010;38(6):610–619. doi: 10.1016/j.amepre.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 33.Zambrana RE, Breen N, Fox SA, Gutierrez-Mohamed ML. Use of Cancer Screening Practices by Hispanic Women: Analyses by Subgroup. Preventive Medicine. 1999;29(6):466–477. doi: 10.1006/pmed.1999.0566. [DOI] [PubMed] [Google Scholar]
- 34.Hoffman H, LaVerda N, Levine P, Young H, Alexander L, Patierno S. Having health insurance does not eliminate race/ethnicity-associated delays in breast cancer diagnosis in the District of Columbia. Cancer. 2011;117(16):3824–3832. doi: 10.1002/cncr.25970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miranda PY, Wilkinson AV, Etzel C, Zhou R, Jones LA, Thompson P, et al. Policy implications of early onset breast cancer among Mexican-origin women. Cancer. 2011;117:390–397. doi: 10.1002/cncr.25397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rodriguez MA, Ward LM, Perez-Stable EJ. Breast and Cervical Cancer Screening: Impact of Health Insurance Status, Ethnicity, and Nativity of Latinas. Annals of Family Medicine. 2005;3(3):235–241. doi: 10.1370/afm.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fiscella K, Franks P, Meldrum S. Estimating racial/ethnic disparity in mammography rates: it all depends on how you ask the question. Preventive Medicine. 2004;39(2):399–403. doi: 10.1016/j.ypmed.2004.02.002. [DOI] [PubMed] [Google Scholar]


