SUMMARY
Objectives
Fibro-osseous neoplasm remains somewhat controversial, and differing concept have been advanced regarding their nature and the proper terminology for them. Cemento-ossyfying fibroma juvenile (JOF) is a rare type of fibro-osseous tumor as also been included under the “umbrella” of cemento-ossyfying fibroma. The JOF is most often seen in patients who are between 5 and 15 years of age. With this work we emphasize the importance of a correct diagnostic approach.
Material and methods.
The case describes a form of cemento-ossyfying fibroma hight active and aggressive like JOF. The patient thirteen older showed from 2004 to 2008 three times the palatal lesion, it was performed with a incisional biopsy and excisional biopsy. The tumor were fixed in 10% buffered formalin embedded in paraffin cut into thick sections and stained with ematoxylineosin.
Results
The incisional biopsy was inadequate to formulate a correct diagnosis. The histological exams have showed for three times different aspects.
Conclusion
Some authors in the past have suggested different classification. The COFs show different clinical, histological and radiographical patterns.
Keywords: escissional biopsy, cemento-ossyfing fibroma, fibro-osseous neoplasm
RIASSUNTO
Obiettivi.
Le neoplasie fibro-ossee rappresentano un capitolo controverso della letteratura scientifica internazionale, per la difficoltà nell’inquadramento della loro natura e della terminologia utilizzata per classificarli. Il fibroma cementoossificante giovanile (JOF) è un raro tipo di tumore fibroosseo incluso nella famiglia dei tumori ossificanti. È a comportamento attivo o aggressivo ed è piu frequentemente presente nella popolazione fra i 5 e 15 anni. Con questo lavoro vogliamo sottolineare l’importanza di un corretto approccio diagnostico.
Materiali e metodi.
Il caso clinico descrive una forma di fibroma cemento-ossificante altamente aggressiva e recidivante riconducibile al quadro clinico ed istologico di JOF. Il paziente di anni 13 ha manifestato dal 2004 al 2008 tre recidive trattate con biopsie prima incisionale e poi escissionale. Il pezzo operatorio è stato prima fissato con formaldeide 10% e poi incluso in paraffina. Gli esami istologici sono stati eseguiti mediante colorazione con ematossilina ed eosina.
Risultati.
La biopsia incisionale si è dimostrata una tecnica inadeguata per il corretto inquadramento della patologia. Gli esami istologici eseguiti hanno mostrato per tre volte quadri differenti.
Conclusioni.
Diversi Autori hanno nel corso del tempo suggerito diverse classificazioni. Il fibroma cemento-ossificante mostra differenti aspetti clinici, istologici e radiografici.
Introduction
The cemento-ossifying fibroma (COF) is the most common benign fibro-osseous lesion of the jaw, with a slow-growing process (1).
The COF is a mesodermal type of non-odontogenic aggressive tumour which is highly destructive and shows a marked tendency to recur.
It arises from ectopic multipotential blast cells of the periodontal membrane of the jaws (2).
Although it has principally been found in the jaws, it also been reported in the frontal, ethmoid, sphenoid (3), temporal bones and in the orbit, in the anterior cranial fossa (4).
The COF exhibits a variable behaviour ranging from slow growth to aggressive local destruction; some cases recur after surgery.
This variable behaviour cannot be predicted on the basis of the histopathology which is itself variable.
Material and methods
A 13-years-old boy was referred to the dental hospital “S. Giovanni Calibita” Fatebenefratelli of Rome in April 2004 for examination of a swelling of the right maxillary region between 1.5–1.6 dental elements. The surgeon decided to make an incisional biopsy. It was incomplete because there was partial removal.
In 2006, 2 years later, the patient was referred in the same hospital, but there was another surgeon group, he complained of swelling in the right maxillary with no signs of inflammation. There was nothing significant in his medical and dental history. Laboratory tests were all within normal limits. There was no history of trauma. The vitality test of the teeth was negative. Clinical examination showed a marked swelling of the right maxillary, the overlying mucosa was normal in colour and intact (Fig. 1).
Figure 1.
Frontal vision of the lesion. Note right palatal swelling between 1.5–1.6 dental elements.
At palpation the lesion appeared hard, immotile and asymptomatic. Radiographic examination, ortopantomography (OPT), revealed a large calcificed mass, well circumscribed and demarcated, with an oval shaped and without root resorption (Fig. 2). An excisional biopsy was performed on the right maxillary lesion to know the real nature of lesion. The lesion was excised under local anesthesia, with 2% mepivacaine and epinephrine as vasoconstrictive 1/100.000. Subsequently the lesion was incisioned with a blade n° 12 and was performed a total palatal flap (Fig. 3).
Figure 2.
Panoramic radiograph showing one radiopaque lesion in the maxilla between 1.5–1.6 dental elements. The teeth adjiacent to lesion are not displaced or resorbed.
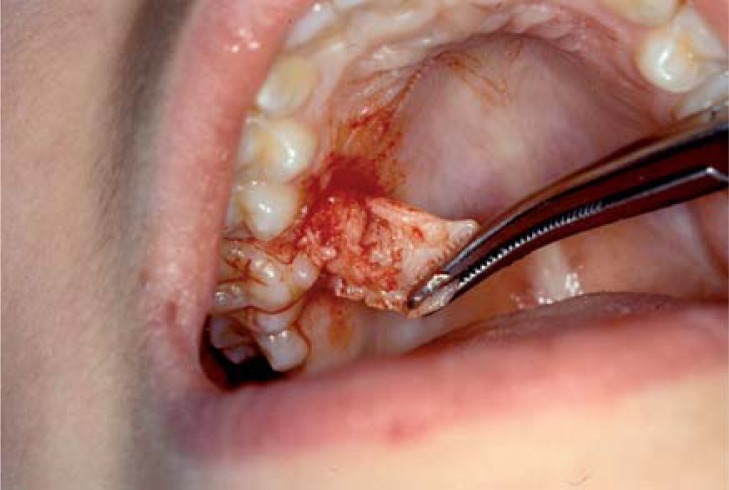
Figure 3.
Excision of the lesion. Introperative vision.
During the dissection, the lesion was easily separable from adjacent palatal mucosa but it was firmly attached to the bone (Picture 4, 5); the cavity was controlled and it was washed with saline solution. The flap was sutured with silk 3-0 (Ethicon Johnson & Johnson) and it was protected by periodontal pack for ten days (Fig. 6, 7, 8). After an uneventful postoperative course the patient was seen every six months.
Figure 4.
This image shows the lesion during the flap arise and removal.
Figure 5.
Using bone clamp bone spicules are removed.
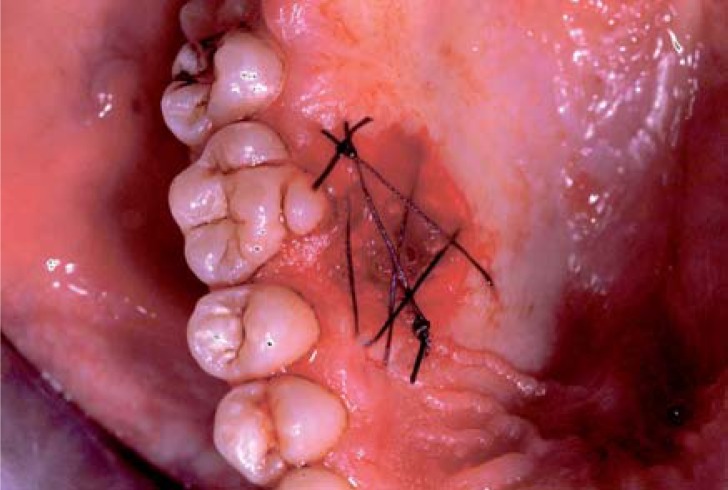
Figure 6.
Nonabsorbable surgical suture.
Figure 7.
Biopsy sample.
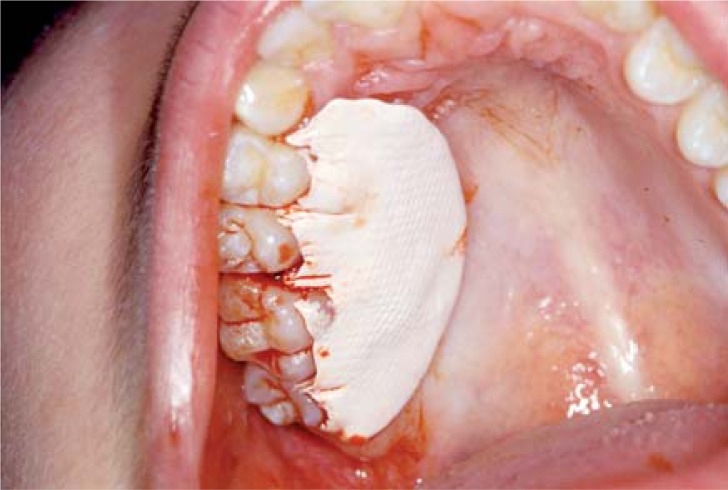
Figure 8.
Periodontal pack.
In April 2009, 5 years later, the patient had a recurrence of the lesion in the right maxillary (Fig. 9). Radiographic examination revelated a large radiopaque mass surrounded by a radiolucent zone. He had another excisional biopsy (Figs. 10, 11, 12, 13).
Figure 9.
Intraoral view of the lesion after 5 years.
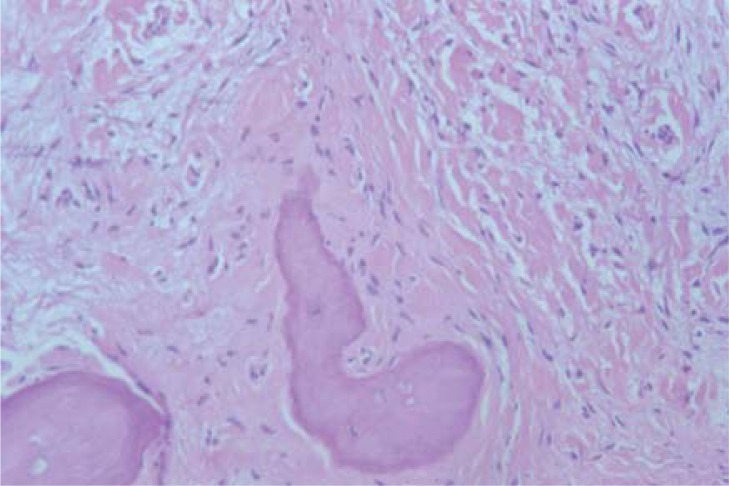
Figure 10.
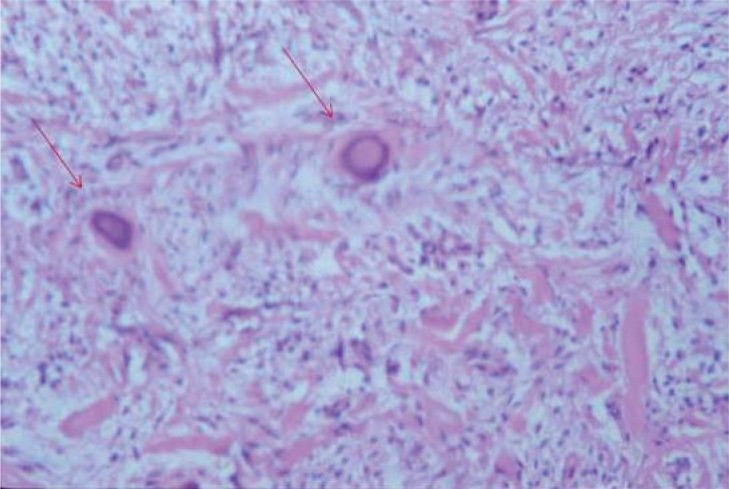
Microphotograph of biopsy material. Fibrous tissue relativity cellular with bone trabecules and acellular cement areas. They have a spherical shape.
Figure 11.
In this image it’s possible to note two psammoma bodies.
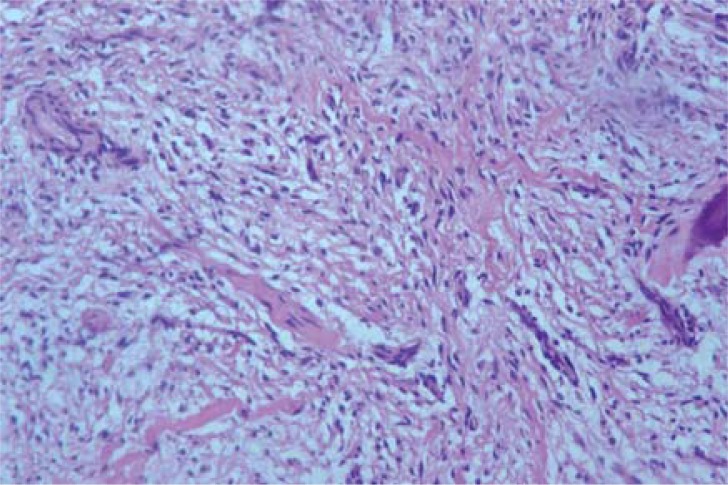
Figure 12.
Histopatologic section showing a fibrous stroma, highly cellular, with an acellular cemental component. On haematoxylin-eosin staining, masses of a cellular basophilic material were demonstrated with concentric lines which were identified as cement.
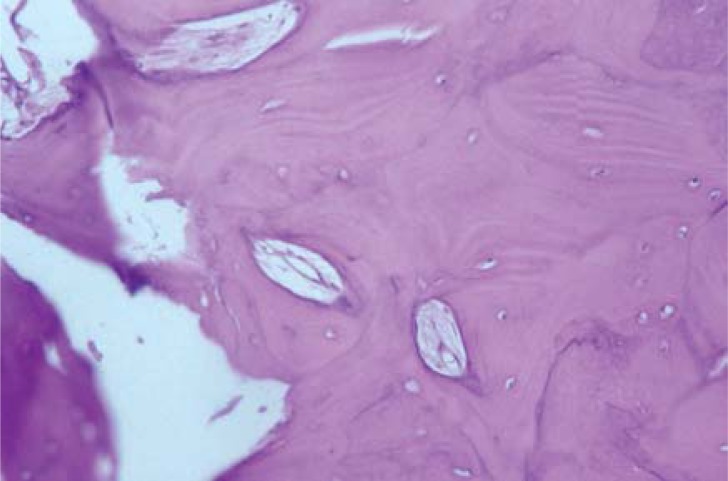
Figure 13.
The image showing bone trabecules with osseus lacunes containing cells.
Results
In our case report the first approach to the lesion was conservative. An incisional biopsy was done. The istological features was “hyperplastic formation with edematous overlining and angiectatic stroma”. Two years later at the onset of the recurrence of the same lesion an excisional biopsy was done. The istological result was not diagnostic: “collection constituted by fibrous tissue and bone spicules with necrosis and regressive aspects; there aren’t atypical cells, there isn’t inflammation”. In this case a watch and wait approach was used. After three years during a follow up visit an initial relapse was found and a new complete removal of the lesion was done biggest than the second.
The istological features were “the material in examination shows fragments of mucosa and Malpighian epithelium in continuity with a neoformation that it’s constituted by fail fibrous tissue with cementicles and bone trabeculae. The histopathological diagnosis was: “Cemento-Ossyfying Fibroma” (Fig. 10, 11, 12, 13).
Discussion
Cemento-ossifying fibroma (COF) is a neoplasm forming part of the spectrum of fibro-osseous lesions of the jaws (5).
The object clinician case of the present work describes varying it youthful, introduced from Jonhnson in 1952 (JOF) (2, 9).
COF is a well demarcated, occasionally encapsulated neoplasm, contains fibrous tissue and varying amounts of calcified tissue resembling bone, cementum, or both. The histological appearance of cementoma of the jaws was first described in 1872 (Menzel). The term “ossifying fibroma” has been used since 1927 (Montgomery) and since 1968 cement-containing tumours were grouped together (2, 6, 7). In 1971 the WHO classified four types of lesions cement containing: fibrous dysplasia, ossifying fibroma, cementing fibroma and cemento ossifying fibroma (8). The WHO revised in 1992 its nomenclature and divided benign fibro-osseous lesions of the oral and maxillo-facial regions into two categories: osteogenic neoplasm (including COF) and non neoplastic bone lesions, including fibrous dysplasia and cemento-osseous dysplasia (9). COF of the jaw shows a predilection for females (10). Many authors have confirmed that COF of the jaw tends to occur in middle-aged patients (6, 10). The peak incidence is in the third and fourth decade with a wide age range (11). JOF is used to describe an actively growing lesion that mainly affects individuals aged < 15 years, whereas COF seems to occur in people aged > 20 years, and mostly occurs in patients in their 20s and 30s (10).
The WHO classification of odontogenic tumors in the second edition (10), defines juvenile (aggressive) ossifying fibroma as a lesion showing a particular histological aspects: cell, rich fibrous tissue containing bands of cellular osteoid without osteoblastic rimmig, with trabeculae of more typical bone, giant cells may also be present. Juvenile ossifying fibroma, however, has also been employed as diagnostic label for lesion occurring predominantly in the paranasal sinuses and histologically characterized by the presence of a fibroblastic stroma containing small ossicles resembling psammoma bodies (17). The stroma varied from loose and fibroblastic to intensely cellular without intervening collagen. The mineralized material consisted of spherical ossicles that were acellular or included sparsely distributed cells. Accounts of the biological behaviour of JOF have varied with reports of recurrence ranging from 30–50%, including the form with multiple recurrences (18). JOF of the jaw bone is generally asymptomatic, it’s depend by the size, it may cause pain, swelling and paresthesia. When it involves the paranasal sinus and orbit regions, it may cause nasal obstruction, sinusitis, headache and proptosis (17).
Radiological features depend on the stage of the lesion; early stages present as radiolucensis, late lesions as well-demarcated, dense radiopacities and a minority as mixed. Osteoblastic rimming is present in cementoossifying fibroma but according to the WHO classification of JOF is absent in the latter. This is an important point for differential diagnosis between two lesions. A well-defined border has been reported in 85% of cases of COF (17). COF exhibits a locally aggressive growth pattern, and requires radical surgery for tendency of recurrence and the possibility of malignant transformation (10, 13). Takeda and Fujioka (14) reported a case of multiple cemento-ossifying fibroma in three jaw quadrants, and recently, Yih(15) et al. reported multiple familial ossifying fibroma. The same authors demonstrate microscopically capsule presence. Su et al. reported that 88% of COF tumours consisted of a large enucleated pieces and that 44% of cases had capsules (16).
Conclusion
This case report describes a recurrence of a JOF and illustres the diagnostic difficulties that may be encountered when treating fibro-osseous lesions.
It is almost inevitable that diagnosis of JOF is complicated, because pathologic features are common with other fibro-osseous lesions, such as cementoosseous dysplasia or Juvenile cemento ossifying fibroma.
Radiographical exams, excisional biopsy and histological aspects, are the common instruments for a correct diagnosis. Histology’s aspect of the lesion, psammoma bodies, rich fibrous tissue containing bands of cellular osteoid and the absence of capsule, suggest diagnosis of JOF.
Different diagnosis instruments: radiographical exams, histological exams and pathologic findings is required to ensure an accurate diagnosis.
Treatment depends on the individual clinical features and biological behaviour. Postoperative follow-up is essential, to supervising JOF recurred. It’s important that dentist and pathologist communicate between.
Deep biopsy is very important to know the real nature of lesion and avoid the recurrence. The JOF lesions should be excised with conservative enucleation.
References
- 1.MacDonald-Jankowski DS. Cemento-ossifying fibromas in the jaws of Hong Kong Chinese. Dentomaxillofacial Radiology. 1998;27:298–304. doi: 10.1038/sj/dmfr/4600378. [DOI] [PubMed] [Google Scholar]
- 2.Brademann G, Werner JA, Janig U, Mehdorn HM, Rudert H. Cemento-ossifying fibroma of the petromastoid region: case report and review of the literature. Journal of Laryngology and Otology. 1997 Feb;111:152–155. doi: 10.1017/s0022215100136709. [DOI] [PubMed] [Google Scholar]
- 3.Som PM, Lidov M. The benign fibro-osseous lesion: its association with paranasal sinus mucoceles and its M R appearance. J. Comp. Assist. Tomography. 1992;16:871–876. [PubMed] [Google Scholar]
- 4.Nakamura K. Ossifying fibroma of the paranasal sinuses, orbit and anterior cranial fossa. Neurosurg. 1995;36:1192–1195. doi: 10.1227/00006123-199506000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Yih WY, Pederson GT, Bartley MH. Multiple familial ossifying fibromas: relationship to other osseous lesions of the jaws. Oral Surg Oral Med Oral Pathol. 1989;68:754–758. doi: 10.1016/0030-4220(89)90167-9. [DOI] [PubMed] [Google Scholar]
- 6.Hamner J E, Scolfield HH, Cornyn J. Benign fibro-osseous jaw lesions of periodontal membrane originan analysis of 249 cases. Cancer. 1968 a;22:861–878. doi: 10.1002/1097-0142(196810)22:4<861::aid-cncr2820220425>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 7.Hamner JE, Lightbody PM, Ketcham AS, Swertlow H. Cemento-ossifying fibroma of the maxilla. Oral Surgey Oral Medicine and Oral pathology. 1968b;26:576–587. doi: 10.1016/0030-4220(68)90341-1. [DOI] [PubMed] [Google Scholar]
- 8.Pingborg J, Kramer IRH. International Histological Classification of Tumours No 5. World Health Organization; Geneva: 1971. Histological typing of odontogenic tumours, jaw cysts and allied lesions; pp. 31–34. [Google Scholar]
- 9.Kramer IRH, Pingborg J, Shear M. Neoplasms and other lesions related to bone. In: World Health Organization, editor. Histologic typing of odontogenic tumours. Berlin: Springer-Verlag; 1992. pp. 28–31. [Google Scholar]
- 10.Cheng C, Tkahashi H, Yao K, Nakayama M, Makoshi T, Nagai H, Okamoto M. Cemento ossifying fibroma of maxillary and sphenoid sinuses: case report and literature review. Acta Otolaryngol. 2002;(supp 547):118–122. doi: 10.1080/000164802760057734. [DOI] [PubMed] [Google Scholar]
- 11.Hwang EH, Kim HW, Kim KD, Lee SR. Multiple cemento-ossifying fibroma: report of an 18-year follow-up. Dentomaxillofacial Radiology. 2001;30:230–234. doi: 10.1038/sj.dmfr.4600608. [DOI] [PubMed] [Google Scholar]
- 12.Knusten B M, Larheim T A, Johannessen S, Hillesad J, Solheim T. StrØmme Koppang. Recurrent conventional cemento-ossifying fibroma of the mandible. Case report. Dentomaxillofacial Radiology. 2002;31:65–68. doi: 10.1038/sj/dmfr/4600665. [DOI] [PubMed] [Google Scholar]
- 13.Bertrand B, Eloy P, Cornelis JP, Gosseye S, Clotuche J, Gilliard C. Juvenile aggressive cemento-ossifying fibroma: case report and review of the literature. Laryngoscope. 1993;103:1385–90. doi: 10.1288/00005537-199312000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Takeda Y, Fujioka Y. Multiple cemento-ossifying fibromas. Int J Oral Maxillofac Surg. 1987;16:368–371. doi: 10.1016/s0901-5027(87)80161-3. [DOI] [PubMed] [Google Scholar]
- 15.Yih Wy, Pederson GT, Bartley MH. Multiple familial ossifying fibromas: relationship to other osseous lesions of the jaws. Ora Surg Oral Med Oral Pathol. 1989;68:754–758. doi: 10.1016/0030-4220(89)90167-9. [DOI] [PubMed] [Google Scholar]
- 16.Su L, Weathers DR, Waldrom CA. Disinguishing features of focal cemento-osseous dysplasias and cemento-ossifying fibroma. II. A clinical and radiologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol. 1997;4:540–549. doi: 10.1016/s1079-2104(97)90271-7. [DOI] [PubMed] [Google Scholar]
- 17.Slootweg PJ, Panders AK, Koopmans R, Nikkels PGj. Juvenile ossifying fibroma. An analysis of 33 cases with emphasis on histopathological aspects. J Oral Pathol Med. 1994;23:385–388. doi: 10.1111/j.1600-0714.1994.tb00081.x. [DOI] [PubMed] [Google Scholar]