SUMMARY
Aim of the work
Aim of this work is to evaluate the efficacy of the Partsch I surgical technique which is considered to be first choice in the treatment of cystic lesions according to the international literature and also to evaluate the regeneration capacity of the bone tissue without any grafting procedure.
Materials and methods
The patient reported pain in the second quadrant. The objective intraoral examination showed a swelling which was of a hard-elastic consistency and, the x-ray, opt and ct scan exams showed an osteolitic lesion which expanded from the element 2.3 to the elment 2.6 involving the maxillary sinus, too. The lesion was removed by the Partsch I method after disinfecting and shaping the radicular canals of the 2.3 element. It was assessed that the maxillary sinus requested no treatment for the presence of a thin cortical layer residue. The removed neoformation was then sent to the Anatomy and Histology Pathology Service.
Results
The histologic test confirmed the radicular origin of the odontogenic neoformation containing a necrotic-hemorrhage. Clinically the post-operative course showed no complications, with a good healing of the bone tissue and there was no oral-antral communications.
Conclusions
The clinical results obtained confirmed the validity of the enucleation technique in the treatment of cystic neoformations. Such approach has always to be preferred because it presents no intraoperative risks, especially for what it concerns the post-operative course. It has also been confirmed the great capacity for the bone tissue to regenerate following the organization of the hematic coagulum.
Keywords: cyst, enucleation
RIASSUNTO
Scopo del lavoro
Lo scopo del lavoro è di valutare l’efficacia della tecnica chirurgica Partsch I, considerata dalla letteratura internazionale la prima scelta nel trattamento delle lesioni cistiche; è altresì importante valutare la capacità di rigenerazione del tessuto osseo, in assenza di procedure di grafting.
Materiali e metodi
Il paziente giunto alla nostra osservazione lamentava sintomatologia algica in corrispondenza del II quadrante. L’esame obiettivo intraorale evidenziava una tumefazione di consistenza duro-elastica e gli esami Rx OPT e TC mostravano una lesione osteolitica che si estendeva dall’elemento 2.3 all’elemento 2.6 con interessamento del seno mascellare. Si procedeva dunque alla rimozione della lesione mediante tecnica Partsch I, previa disinfezione e sagomatura dei canali radicolari dell’elemento 2.3. Non si riteneva necessario alcun trattamento del seno mascellare per la presenza di un sottile strato di corticale residua. La neoformazione asportata veniva inviata al Servizio di Anatomia ed Istologia Patologica.
Risultati
L’esame istologico confermava l’origine radicolare della neoformazione odontogena, a contenuto necrotico-emorragico. Clinicamente, il decorso post-operatorio si mostrava privo di complicanze, con una buona guarigione del tessuto osseo, in assenza di comunicazioni oro-antrali.
Conclusioni
I risultati clinici ottenuti confermavano la validità della tecnica di enucleazione nel trattamento delle neoformazioni cistiche; in assenza di rischi intraoperatori, infatti, tale approccio è sempre da preferire, soprattutto in riferimento al decorso post-operatorio. Era altresì confermata l’ottima capacità di rigenerazione del tessuto osseo in seguito all’organizzazione del coagulo ematico.
Introduction
Maxillary cysts are pathologic cavities with a liquid or semiliquid content delimited wholly or partially by epithelium; the origin of the latter one allows to distinguish cysts in odontogenic or nonodontogenic. The former, which are more frequent, are characterized by a layer of the epithelium deriving from the residues in which the tooth forms itself; being more specific, the Serres glands which persist even after the dissolution of the dental lamina, the enamel epithelium and the Malassez residues formed by the fragmentation of the Hertwig epithelial sheath. The activation of these residues by a degenerative mechanism is not completely clear but can be led to processes of an inflammatory kind or to phenomena of congenital nature (3, 13). Cystic lesions, though benigne and often asymptomatic, can be characterized by a tendency to grow at the expense of the other surrounding structures so that a treatment of surgical type is required. The techniques described in literature (1, 3) are mainly the enucleation (Partsch I) and the marsupialization of the lesion (Partsch II) or a combination of the two. Enucleation is the first choice treatment; should it involve serious intra-operative risks a different technique has to be opted for. Particular large neoformations at the expense of the bone components, with a risk of fracturing them or very close to important anatomical structures represent the principal conditions for a surgical approach with the Partsch II technique.
Peculiar features of the radicular cysts
Radicular cysts are considered to be lesions of an odontogenic nature which originate from the epithelial residues present in the parodontium space, and its proliferation is activated by an inflammatory-type mechanism. As a consequence of the necrosis of a dental element, the batterial and necrotic residues of the pulp reach the root apices and the parodontium space, where are frequently present the residual cells of the Hertwig sheath (residues of Malassez); these are incited to proliferate and form a column like epithelial cells in the periapical area (3–5, 10). According to the literature (7, 2, 6, 12, 13), the mechanism which sustains the growth of the cystic lesion could it be double; the most reliable theory is called the hydrostatic theory: within the proliferating epithelial cells there is a build-up of other residues (protein, cholesterol) and the relative increase of the osmotic pressure results in fluid accumulation; the increase in the hydrostatic pressure determines an osteoclastic activation and thus a progressive expansion of the lesion at the expense of the surrounding bone structure. The prostaglandinic theory, instead, supports the osteoclastic activation by the proglandine and prostacicline present in the cystic wall. It is probable that both mechanisms contribute to the formation and development of such a lesion.
Clinical and radiographical characteristics
The radicular cyst is the most common cystic lesion, with a frequency of about 50% amongst all cystic lesions of odontogenic nature (3). In most cases it is diagnosed accidentally while taking normal radiographic tests. As such lesions are typically asymptomatic, the clinical diagnoses is rather rare unless the cyst reaches such dimensions as to erode the cortical bones or flogistic processes spring up. A rather useful indication to address the diagnoses is the vitality test, as a radicular cyst is always associated with a necrotic dental element (3, 4, 10, 11). From a radiographic point of view, this neoformation appears as a unilucular radio-transparency with very clear margins with a roundish shape still in relation with the radicular apex (9). From a histologic point of view is covered by a stratified squamous epithelium unkeratinized (5, 8, 13).
Materials and methods
Clinical case
A 65-year-old male patient presenting an algic symptomatology corresponding to the upper left arch came to our attention. To an objective intra-oral examination a tumefaction of a hard elastic consistency was detected, with the entire mucosa above and of a normal color (Fig. 1). An OPT (Fig. 5) and denta scan examination (Figs. 2–4) was requested in which an osteolitic lesion appeared extended to the maxillary sinus, too. The patient underwent a thorough anamnesis and informed about the possible therapeutic solutions. It has been opted for a surgical approach through the enucleation of the lesion (Partsch I technique).
Figure 1.
Vestibular swelling.
Figure 5.
Radiographic orthopanoramic.
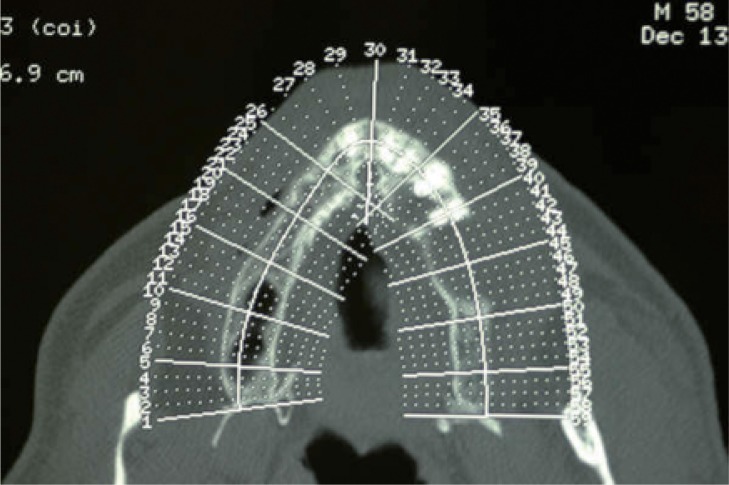
Figure 2.
Axial scan.
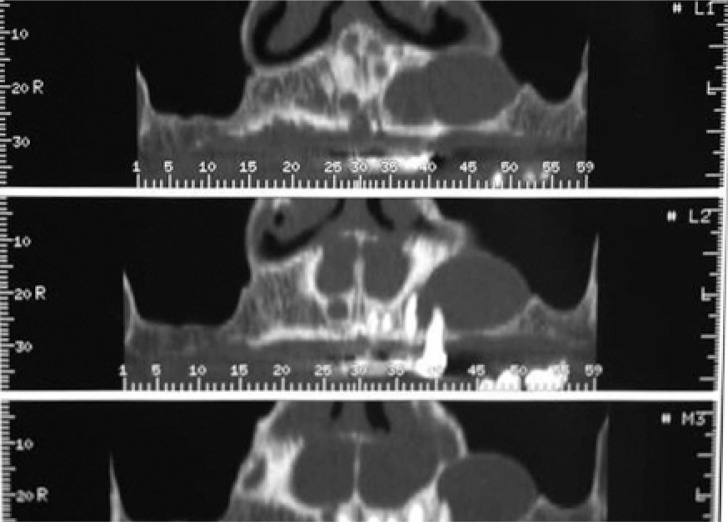
Figure 3.
Tc panorex.
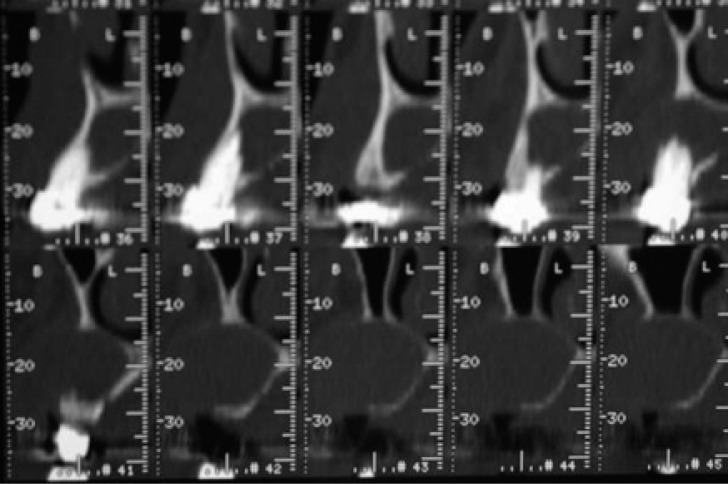
Figure 4.
Oblique cross-sections.
Clinical procedure
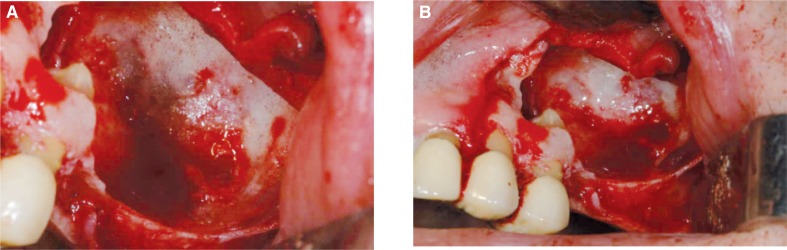
After having verified the necrosis of the 2.3 element, cleaning and shaping of the root canal was performed on the same tooth and with the neoformation being removed. After having anaesthetised the second region and by blocking the infraorbital nerve, a mucoperiosteal flap was prepared through an intrasulcular and crestal incision stretching from the element 2.3 to 2.6 with two releasing incisions, mesially to the canine and distally to the first molar (Fig. 6). After raising the flap, in which it was possible to see the erosion of the vestibular cortical bone by the neoformation, its remotion was performed by using periosteal elevators (Fig. 7). The analysis of the cavity detected the presence of a thin layer of residual cortical bone, which insured the integrity of the maxillary sinus and any other treatment was superfluous (Figs. 8 a, b). After curettage of the cavity washes were done with hydrogen peroxide and hemostasis and sutured 3.0 silk sutures (Fig. 9). It was then performed a local infiltration in the buccinator muscle of Bentelan (4 mg/2 ml) and prescribed an antibiotic therapy of Augmentin for six days, an antiflogistic therapy and analgesics when needed and mouthwashes with clorhexidine 0.2%. The removed neoformation was then sent to the Pathological and Anatomy & Histology Services.
Figure 6.
Mucoperiosteal flap setting and exposure cystic neoplasm.
Figure 7.
Radicular cyst.
Figure 8 a, b.
Residual bone cavity.
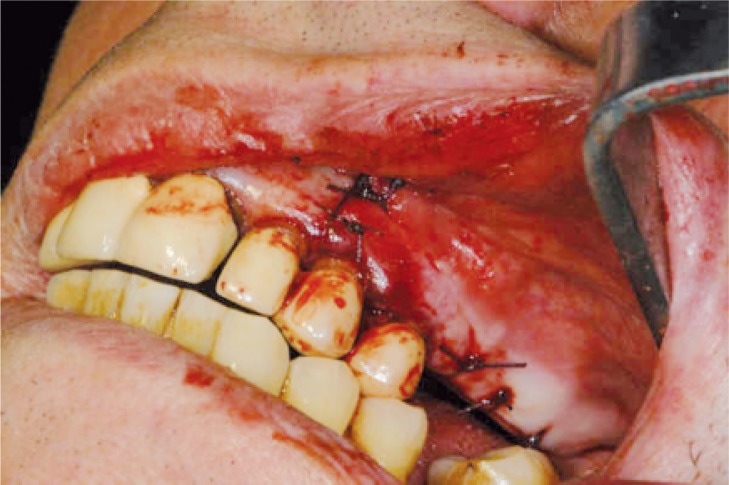
Figure 9.
Hemostasis and suture.
Discussion and conclusions
The histological examination confirmed the inflammatory nature of the lesion which was 2.5 × 1 × 0.3 cm big. The radicular type cyst and of odontogenic origin, showed a hemorragic-necrotic content including cholesterol crystals. The clinical and radiographic checks done after surgery showed a postoperative course without complications. The soft tissues showed an excellent healing and the radiographic tests (Fig. 10) showed the absence of oro-antral communication due to the gradual filling of the cavity by the new forming bone tissue; the presence of the haematic clot formed soon after surgery has secured the alternation of those biological phenomena which hesitate in the formation of new bone. Blood clot, contracting, yielded the way to the formation of granulation tissue, characterised by new blood vessels and young collagen fibres; subsequently, the reorganization of this tissue hesitated in forming osteoid trabeculas which, starting from the bone walls, were heading towards mineralization processes.
Figure 10.
Orthopanoramic monitoring.
The good healing of the surgical site, witnessed by both clinical and radiographic follow-ups, indeed confirm that the enucleation technique has to be preferred every time important intraoperative risks are not expected, such as the fracture of the bone components or the lesion of the anatomical structures. As the international literature maintains, the Partsch I surgical technique allows a postoperative course little uncomfortable for the patient and in the vast majority of cases without any complication worth noting. This kind of approach guarantees a healing of the soft tissues as first intention and, thanks to the formation of blood clotting, secures those biological mechanisms as proof of the autonomous regenerative capability of the bone tissue, without using any grafting material.
References
- 1.Bodner L. Title Effect of decalcified freeze-dried bone allograft on the healing of jaw defects after cyst enucleation. Source Journal of Oral & Maxillo-facial Surgery. 1996;54(11):1282–6. doi: 10.1016/s0278-2391(96)90482-6. [DOI] [PubMed] [Google Scholar]
- 2.Benn A, Altini M. Dentigerous cysts of inflammatory origin. A clinicopathological study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Edodontics. 1996;81:203–9. doi: 10.1016/s1079-2104(96)80416-1. [DOI] [PubMed] [Google Scholar]
- 3.Chiapasco M, Motta JJ. Le cisti dei mascellari. In: Chiapasco M, et al., editors. Manuale illustrato di Chirurgia Orale. Masson; 2005. pp. 217–250. [Google Scholar]
- 4.Ciani A, Mangano C, Donzelli R, Bucci Sabattini V. Cisti radicolare della mandibola. Dental Cadmos. 1992;19:74–9. [Google Scholar]
- 5.Ricucci D, Pascon EA, Ford TR, Langeland K. Epithelium and bacteria in periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Feb;101(2):239–49. doi: 10.1016/j.tripleo.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 6.Brown RM. The pathogenesis of odontogenic cysts: a review. Journal of Oral Pathology. 1975;4:31–46. doi: 10.1111/j.1600-0714.1975.tb01738.x. [DOI] [PubMed] [Google Scholar]
- 7.Coli S, Jurisi M, Jurisi V. Pathaphisiological mechanism of the developing radicular cyst of the jaw. Acta Chir Iugosl. 2008;55:87–92. doi: 10.2298/aci0801087c. Review. [DOI] [PubMed] [Google Scholar]
- 8.Pindborg JJ, Kramer IRH, Torloni H. Histological typing of odontogenic tumors, jaw cysts and allied lesions. Geneva: World Health Organization; 1979. pp. 15–23. [Google Scholar]
- 9.Düker J. Radiographic diagnostics Radicular cyst. Quintessence Int. 2005 Apr;36(4):317. [PubMed] [Google Scholar]
- 10.Murmura G, Traini T, Di Iorio D, Varvara G, Orsini G, Caputi S. Residual and inflammatory radicular cysts. Clinical and pathological aspects of 2 cases. Minerva Stomatol. 2004 Nov-Dec;(11–12):53. 693–701. [PubMed] [Google Scholar]
- 11.Summers GW. Jaw Cisis: diagnosis and treatment. Source Head & Neck. 1979;1(3):243–58. doi: 10.1002/hed.2890010308. [DOI] [PubMed] [Google Scholar]
- 12.Shear M. Developmental odontogenic cysts. An update. Journal of Oral Pathology and Medicine. 1994;23:1–11. doi: 10.1111/j.1600-0714.1994.tb00246.x. [DOI] [PubMed] [Google Scholar]
- 13.Soames JV, Southam JC. Cisti dei mascellari e dei tessuti molli del cavo orale. Patologia Orale terza edizione. 2005;6:75–95. [Google Scholar]