Abstract
Objectives
This study had three objectives. Firstly, the prevalence of post-traumatic stress disorder (PTSD) and trauma exposure was compared between individuals with and without substance use disorder (SUD). Secondly, we compared self-rating of PTSD and clinical judgement. Thirdly, an analysis of the characteristics of SUD/PTSD patients was performed.
Methods
The sample consisted of 423 patients with SUD and 206 healthy controls. All individuals were screened on PTSD using the self-rating inventory for PTSD.
Results
Significantly higher numbers of PTSD and trauma exposure were found in the SUD group (resp. 36.6 and 97.4%). PTSD went frequently unnoticed when relying on clinical judgement alone. Patients with SUD/PTSD were significantly more often unemployed and had a lower educational level. Axis I comorbidity and especially depressive disorders were more common in the SUD/PTSD group.
Conclusion
It is concluded that patients with SUD/PTSD are a substantial and vulnerable subgroup in addiction treatment facilities and that a systematic screening for PTSD is required.
Keywords: prevalence, trauma exposure, post-traumatic stress disorder, substance use disorder, clinical judgment
Previous research has documented a strong link between substance use disorder (SUD) and post-traumatic stress disorder (PTSD). The prevalence of current PTSD (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DSM-IV) in SUD patients is around three times higher than in the general population, ranging from 25.3 to 49% (Bonin, Norton, Asmundson, Dicurzio, & Pidlubney, 2000; Driessen et al., 2008; Kessler et al., 2005; Ouimette, Coolhart, Funderburk, Wade, & Brown, 2007; Read, Brown, & Kahler, 2004; Reynolds et al., 2005). Besides this high comorbidity, studies suggest a poorer SUD treatment outcome when comorbid PTSD is left untreated (Mills, Teesson, Ross, Darke, & Shanahan, 2005; Read et al., 2004).
Dragan and Lis-Turlejska (2007) used three different diagnostic tools to measure PTSD and found substantial differences in PTSD prevalence depending on which tool was used. Therefore, comparisons between prevalence studies are hard to make, unless they used the same measures in a similar way to assess the prevalence of PTSD. As of yet, no study has directly compared the prevalence of PTSD in a SUD population with the prevalence of PTSD in the general population using the same diagnostic tool within one and the same study.
In the present study three different aims can be distinguished: (1) to measure the prevalence of current PTSD and trauma exposure in a representative SUD sample relative to the prevalence of current PTSD and trauma exposure in the general population; (2) to assess whether a PTSD diagnosis is detected without using a standardised questionnaire; (3) to evaluate whether patients in the SUD/PTSD group are a more vulnerable subgroup in terms of socio-economic factors and psychiatric comorbidity.
In the present study the prevalence of PTSD was compared between a sample of individuals without substance dependence or abuse and a sample of treatment seeking SUD patients. To avoid confounding factors as symptoms of detoxification and craving and thereby the risk of overdiagnosis, we chose to measure PTSD with a validated symptom checklist [self-rating inventory for PTSD (SRIP); Hovens, Van der Ploeg, Bramsen, & Klaarenbeek, 1994] extended with a trauma-exposure checklist. Within these scales, we measured PTSD symptoms that were prevalent in the past 4 weeks, thereby excluding lifetime and sub-threshold PTSD. Furthermore, we chose to explore PTSD prevalence in a representative SUD treatment seeking sample. In most prior prevalence studies only one specific substance group was included (Dragan & Lis-Turlejska, 2007; Driessen et al., 2008; Johnson, 2008; Norman, Tate, Anderson, & Brown, 2007). In clinical practice, however, polydrug use is very common and the same treatment protocol is applied to all patients, independent of their primary substance (Emmelkamp & Vedel, 2007). To further improve the representativeness of our sample, no other exclusion criteria were imposed than being able to read and write (as they were expected to complete the SRIP).
A second objective of this study arose from conclusions of previous research, showing that PTSD often remains undiagnosed in SUD patients (Dansky, Roitzsch, Brady, & Saladin, 1997; Najavits, 2005). This is important given that untreated PTSD may lead to a poorer outcome in SUD treatment (Back, Brady, Sonne, & Verduin, 2006; Read et al., 2004). A diagnosis can be made by means of clinical judgement, by using standardised assessment instruments or by both means. It is interesting to find out whether PTSD is correctly diagnosed by clinicians without using a standardised questionnaire, based solely on their clinical experience. In the present study, we thus compared the prevalence of current PTSD as diagnosed by the clinician in the intake phase (without using a standardised diagnostic tool) with the prevalence of PTSD as diagnosed with the SRIP.
For clinical practice, it is interesting to examine whether SUD patients with PTSD are different from SUD patients without PTSD. If patients with SUD/PTSD have a lower socio-economic status or a more severe clinical profile, treatment of this vulnerable subgroup should have a more elaborated focus as well. Although most previous researchers agreed upon the more elaborated clinical comorbidity of SUD/PTSD patients (Bonin et al., 2000; Jacobsen, Southwick, & Kosten, 2001; Mills, Lynskey, Teesson, Ross, & Darke, 2005; Peirce, Kindbom, Waesche, Yuscavage, & Brooner, 2008; Read et al., 2004), contradicting results were found with regard to socio-economic factors as employment, educational and relational status. With some researchers finding a more optimistic profile (e.g., being employed, having a higher educational level) than others (Bonin et al., 2000; Driessen et al., 2008; Mills, Lynskey, et al., 2005; Mills, Teesson, Ross, & Peters, 2006; Peirce et al., 2008; Ouimette, Goodwin, & Brown, 2006). Inconsistency was also found with regard to the number of previous treatments, with Bonin et al. (2000) finding no differences between SUD patients and SUD/PTSD patients and Driessen et al. (2008) and Jacobsen et al. (2001) concluding that SUD/PTSD patients had more previous admissions to addiction treatment facilities. Therefore, in this study, we also examined patient characteristics.
In general, we hypothesised (1) a greater prevalence of PTSD and trauma exposure in patients with SUD as compared to the prevalence in the healthy control group, (2) an underdiagnosis of PTSD when not using a standardised tool and (3) a more severe clinical profile and a lower socio-economic status in the SUD/PTSD compared with the SUD/no PTSD group.
Methods
Study design
The present study comprises a cross-sectional design comparing a group of SUD patients and a group of healthy controls.
Setting
For this study, ethical approval was given by the Institutional Review Board of Maastricht University. All control participants signed a consent form prior to their participation.
Patients with SUD were recruited from 11 different addiction treatment branches from a single organisation (Mondriaan) all located within the same region (southern Limburg, with a population of approximately 620,000 inhabitants, located in the most southern tip of the Netherlands). Participants were included in the study from October 2008 to May 2009. Patients gave permission that the information in their patient file could be used for research purpose. Data on the SRIP and trauma-exposure checklist of the patients included in this study were retrieved from their respective patient files. Since October 2008, the patients in treatment for SUD at the Mondriaan treatment centres are structurally screened with the SRIP and trauma-exposure checklist. Note that the data on these questionnaires were obtained after intake and sometimes even after years of treatment. As such, this allowed us to compare the clinician's diagnosis of PTSD at intake (i.e., without input from a standardised tool as the SRIP) against the prevalence of PTSD based on SRIP scores.
Participants
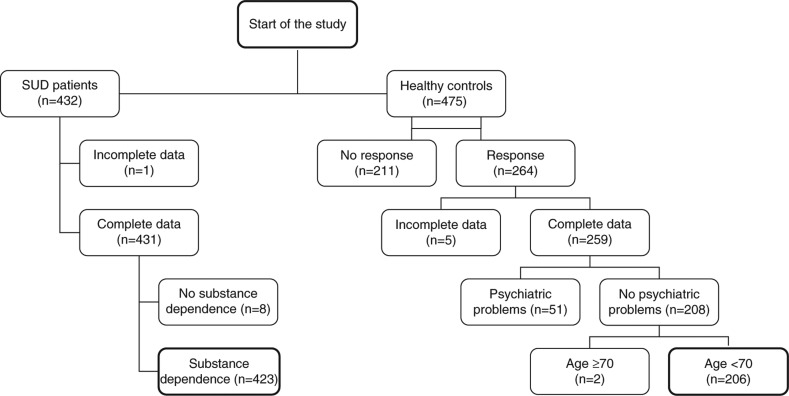
Fig. 1 shows a flowchart for the inclusion and exclusion of participants in the current study. The initial sample consisted of 432 patients with SUD (patient group) and 475 control participants (non-patient control group). We tried to match the control group as closely as possible with the patient group on the basis of age and gender. Participants from the non-patient group were contacted by e-mail. These individuals had previously indicated on the Maastricht University website to be interested in participating in research projects. From the 475 contacted participants, 67 e-mails were automatically returned because of technical problems with email addresses of the recipients, and 144 individuals chose not to participate. The remaining 264 participants in the non-patient group received a website address where they could log in and complete all necessary demographic questions, the SRIP and the trauma-exposure checklist.
Fig. 1.
Flowchart inclusion participants.
Five persons from the non-patient group had incomplete data and were therefore excluded from further analyses. As we wanted to compare the prevalence of PTSD in SUD patients with that in healthy controls, we excluded a further 51 participants from the non-patient group because they admitted abusing drugs or alcohol or because of clear indications of other psychiatric problems. An indication for psychiatric problems was for instance the use of psychiatric medication. In the patient group only one individual was excluded from the analyses due to deficient data and eight patients were excluded because they did not fulfil DSM-IV-TR criteria for substance dependence. As we wanted to match groups on age as closely as possible, two more candidate participants (of 74 and 75 years of age) of the control group were excluded from further analysis. Participants in the patient group were between 18 and 68 years of age (M age = 41 years), as opposed to an age range of 22–68 years in the non-patient group (M age = 54 years). In the patient group 332 (78.5%) participants were male and in the non-patient group 65% was male. In total, data of 423 SUD patients and 206 control participants remained for further analyses. Participant characteristics for the total sample and the SUD patient sample (with and without PTSD) are displayed in Tables 1 and 2, respectively.
Table 1.
Total sample characteristics (SUD vs. control)
| Total sample (N=629) | SUD (N=423) | Control (N=206) | Statistics | Significance | |
|---|---|---|---|---|---|
| Demographics | |||||
| Mean age (SD) | 45.4 (12.64) | 41 (10.97) | 54.4 (10.96) | U =16117, r= − 0.51 | p<0.001 |
| Gender (%) | |||||
| Male | 74 | 78.5 | 65 | χ2 (1) = 13.03 | p<0.001 |
| Female | 26 | 21.5 | 35 | ||
| Education | |||||
| Low | 28.1 | 38.5 | 6.8 | χ2 (2) = 161.99 | P<0.001 |
| Medium | 32.4 | 24.1 | 49.5 | ||
| High | 16.7 | 4.3 | 42.2 | ||
| Missing | 22.7 | 33.1 | 1.5 | ||
| PTSD as measured by the SRIP (%) | 28.6 | 36.9 | 11.7 | χ2 (1) = 43.17 | p<0.001 |
Table 2.
SUD patient sample characteristics (SUD/PTSD vs. SUD/no PTSD)
| SUD (N=423) | SUD/PTSD (N=156) | SUD/no PTSD (N=267) | Statistics | Significance | |
|---|---|---|---|---|---|
| Demographics | |||||
| Mean age (SD) | 41 (10.97) | 41.6 (10.99) | 40.6 (10.97) | U =19708, r=0.04 | 0.390 |
| Gender (%) | |||||
| Male | 78.5 | 75.6 | 80.1 | χ2 (1) = 1.186 | 0.276 |
| Female | 21.5 | 24.4 | 19.9 | ||
| Primary substance (%) | |||||
| Alcohol | 43.7 | 46.2 | 42.3 | χ2 (4) = 2.686 | 0.612 |
| Heroin | 33.6 | 33.3 | 33.7 | ||
| Cocaine | 7.1 | 7.1 | 7.1 | ||
| Cannabis | 10.9 | 7.7 | 12.7 | ||
| Speed | 3.5 | 3.2 | 3.7 | ||
| Missing | 1.2 | 2.6 | 0.4 | ||
| Treatment branch (%) | |||||
| Detox | 18.4 | 20.6 | 17.2 | χ2 (6) = 8.700 | 0.191 |
| Clinical | 9.9 | 9.0 | 10.4 | ||
| Partial | 4.5 | 3.9 | 4.9 | ||
| Psychiatric | 9.7 | 7.7 | 10.8 | ||
| Ambulatory | 49.4 | 52.3 | 47.8 | ||
| Forensic | 4.3 | 1.3 | 6.0 | ||
| Reintegration | 3.8 | 5.2 | 3.0 | ||
| Previous treatments (%) | |||||
| None | 43.3 | 38.1 | 44.4 | χ2 (3) = 3.783 | 0.286 |
| 1–2 | 34.1 | 33.5 | 32.8 | ||
| 3–5 | 16.1 | 19.4 | 13.4 | ||
| > 5 | 6.6 | 7.7 | 5.6 | ||
Measurement/data sources
Self-rating inventory for PTSD
In all participants PTSD was assessed using the SRIP. The SRIP is a Dutch self-report questionnaire with 22 items covering the 17 symptoms and the 3 symptom clusters (i.e., re-experiencing, persistent avoidance and increased arousal) of PTSD following the DSM-IV (Van Balkom, De Beurs, Hovens, & Van Vliet, 2004). Note that the SRIP does not cover criteria A, E and F as formulated in the DSM-IV. Participants are asked to rate their symptoms over the previous 4 weeks on a 4-point Likert scale (1 = not at all, 4 = extremely). Psychometric properties of the SRIP have proved to be good in different clinical samples, including trauma patients (Hovens, Bramsen, & Van der Ploeg, 2002; Hovens et al., 1994). Cronbach's alpha reliabilities are 0.90–0.94 for the total SRIP score, 0.77–0.87, 0.80–0.88 and 0.76–0.85 for the subscales intrusion, avoidance and hyperarousal, respectively. The questionnaire has an excellent test–retest reliability, with Pearson's r =0.92 for the total score and for the subscales intrusion, avoidance and hyperarousal the correlations are 0.84, 0.91 and 0.85, respectively (Hovens et al., 2002). Sensitivity and specificity of the SRIP were measured with the clinician-administered PTSD Scale (CAPS) (Blake et al., 1995; Weathers, Keane & Davidson, 2001), as an external criterion. Sensitivity (true positives according to the CAPS/true positives + false negatives) was high, ranging between 0.83 and 0.86, and a good specificity (true negatives according to the CAPS/true negatives + false positives) ranging between 0.69 and 0.73 was found (Hovens et al., 2002; Witteveen, Bramsen, Hovens, & Van der Ploeg, 2005). The high sensitivity reflects a low risk for false positives, i.e., a low risk for overdiagnosis. On the basis of the balance between sensitivity and specificity an optimum cut-off score for the diagnosis of PTSD of 52 was established (Hovens et al., 2002; Witteveen et al., 2005). Concurrent validity was also examined. Correlations with two other frequently used PTSD scales (Mississippi Combat-related PTSD Scale, civilian version and the Keane MMPI–PTSD subscale) are 0.80 and 0.82, reflecting an adequate concurrent validity (Hovens et al., 2002).
Trauma-exposure checklist
To prevent the risk of overdiagnosis of PTSD, the SRIP, which is a symptom-only measure and does not cover criteria A of DSM-IV, was complemented with a trauma-exposure checklist. This checklist was based on different questionnaires and diagnostic interviews (Interview for Traumatic Events in Childhood; Lobbestael, Arntz, Harkema-Schouten & Bernstein, 2009; Traumatic Experiences Questionnaire; Nijenhuis, Van der Hart, & Kruger, 2002 and the Dutch translated version of the Structured Childhood Trauma Interview; Van der Bossche, Kremers, Sieswerda, & Arntz, 1999) to include a broad range of possible traumas, such as a life-threatening situation, being attacked or threatened. In the present study, a positive diagnosis of PTSD was possible only when all of the following conditions were fulfilled: total SRIP is 52 or higher (Hovens et al., 2002), at least one intrusion item is ≥3, three or more avoidance items are ≥3, at least two hyperarousal items are ≥3 (H. Hovens, personal communication, September 2008) and participants indicate on the trauma-exposure checklist to have been exposed to one or more traumatic events.
Mini International Neuropsychiatric Interview (MINI)
To ensure that participants in the control group were not abusing drugs or alcohol, substance-related questions were added derived from the MINI (Sheehan et al., 1997). As participants in the patient group were all patients in addiction treatment SUD was not measured in this group.
Statistical methods
All analyses were conducted using SPSS 18.0 for Windows. The differences in PTSD prevalence and trauma-exposure prevalence between groups were analysed by using chi-square tests. To compare different characteristics of SUD/PTSD patients with SUD/non-PTSD patients we used chi-square tests (for categorical variables) or t-tests for independent samples (for continuous variables). Cramer's V is used to indicate the effect size for the results of the chi-square tests. The Mann–Whitney test was used for continuous data when the assumption of normality was violated. Logistical regression was used to test whether age and sex predicted PTSD.
Results
Prevalence of current PTSD and trauma exposure (SUD vs. Control)
In the sample of SUD patients, 36.6% scored positive on current PTSD. In the control group 10.2% could be diagnosed with PTSD. There was a significant relation between SUD and whether or not a person scored positive on PTSD χ2 (1) = 48.09, p<0.001, with Cramer's V=0.28, representing a small effect size. This reflects the fact that based on odds ratio individuals are 5.27 times more likely to score positive on PTSD if they are patients with SUD than if they are not patients with SUD.
Since patients with alcohol dependence and patients with heroin dependence constituted a large sample of the SUD patients (resp. 43.7 and 33.6%), PTSD prevalence was also calculated for these subgroups. These numbers were comparable with PTSD prevalence in the SUD group (38.4 and 36.6%, respectively).
Since age and sex were not equally distributed between the SUD group and the control group, we conducted another logistic regression analysis controlling for sex and age. The inclusion of sex and age in the model did not have any influence, nor were there any interaction effects. Only the group (SUD vs. healthy control) was a significant predictor for PTSD (B= − 1.63, SE=0.25, p <0.001).
To analyse the continuous SRIP scores (with a higher score representing a more severe PTSD symptomatology), we employed a non-parametric test as the assumption of normal distribution was violated. Patients with SUD (median = 47) had a significantly higher score on PTSD (total SRIP score) than control subjects (median = 33), U=18880.00, p <0.001, r= − 0.44. This again confirms the proposed strong association between SUD and PTSD.
In the control group 86.3% had been exposed to criterion A1 trauma. In the SUD group, 97.4% had encountered such a trauma in their lifetime. There was a significant relation between SUD and whether or not an individual had been exposed to trauma, χ2 (1) = 28.89, p<0.001, with Cramer's V=0.22, representing a small effect size. On the basis of the odds ratio, individuals are 5.91 times more likely to have been exposed to trauma if they are SUD patients than if they are not SUD patients.
Subjects were asked to indicate on a trauma-exposure checklist to which trauma they were exposed to in their lifetime. Table 3 displays the different types of exposed trauma as indicated by the subjects.
Table 3.
Type of trauma (SUD vs. control)
| Total sample (N=629) | SUD (N=423) | Control (N=206) | Statistics | Significance | |
|---|---|---|---|---|---|
| Any kind of trauma | 93.8 | 97.4 | 85.9 | χ2 (1) = 29.005 | p<0.001 |
| Life-threatening situation | 46.7 | 53.3 | 33.2 | χ2 (1) = 22.498 | p<0.001 |
| Being attacked or threatened with a weapon | 42.1 | 55.3 | 15.6 | χ2 (1) = 88.620 | p<0.001 |
| Witnessing death/severe injury | 50.3 | 55.1 | 40.5 | χ2 (1) = 11.807 | p<0.001 |
| Hearing that something terrible has happened to a close relative | 73.1 | 80.2 | 58.5 | χ2 (1) = 32.807 | p<0.001 |
| Being hit, hurt or injured (as a child or as an adult) | 35.7 | 43 | 21 | χ2 (1) = 28.959 | p<0.001 |
| Being forced to endure or to perform sexual acts | 19.1 | 22.7 | 11.7 | χ2 (1) = 10.809 | p<0.001 |
SUD, substance use disorder.
Relation between PTSD as diagnosed during intake and PTSD diagnosed with the SRIP
A total of 37.9% of patients with SUD mentioned a traumatic experience during the intake interview as reported in the corresponding patient files. A chi-square analysis was performed to check whether this was correlated with a positive PTSD diagnosis as assessed with the SRIP. There was a significant relation between trauma mentioned at intake and whether or not a person scored positive on PTSD as assessed with the SRIP, χ2 (1) = 15.15, p<0.005, with Cramer's V=0.19, representing a small effect size.
In the anamnestic phase, one-fifth (20.2%) of the patients had complained about one or more PTSD symptoms (e.g., recurrent nightmares, avoidance of traumatic stimuli, exaggerated startle response, etc.). There was a significant relation between PTSD symptoms mentioned at intake (mentioning vs. no mentioning) and whether or not a person scored positive on PTSD as assessed with the SRIP χ2 (1) = 15.57, p<0.001, with Cramer's V=0.19, representing a small effect size.
In 4.8% of the intakes, possible PTSD was noted by the interviewer (mere clinical judgement, no use of questionnaires). After intake, a multi-disciplinary staff decides which diagnoses should be written in the patient files (again mere clinical judgement, no use of questionnaires). Only 2.1% (n=9) of the admitted SUD patients were actually diagnosed with PTSD. When comparing this result with the number of PTSD diagnoses as measured with the SRIP (36.6%), it is clear that a large discrepancy in PTSD diagnosis exists, depending on whether or not a questionnaire is used. In four of these nine patients where PTSD was diagnosed type II error seemed to be prevalent given that the clinical judgement diagnosis was not confirmed by the SRIP.
Clinical profile and socio-economic status of SUD patients with vs. without PTSD
We derived information on clinical profile and socio-economic status of the patients from their respective patient files. The SUD/PTSD patients appeared to be quite similar to the SUD/no PTSD patients. No significant differences were found with regard to the criminal past [χ2 (1) = 0.95, p=0.35], financial debts [χ2 (1) = 3.19, p=0.08] and relationship status. Both groups were comparable regarding their time in treatment [χ2 (3) = 1.75, p =0.63], number of previous treatments [χ2 (3) = 3.78, p =0.29] and treatment outcome [χ2 (1) = 0.80, p =0.67]. Two demographic factors were markedly different between the two groups: education level [χ2 (2) = 14.38, p <0.01] and current employment status [χ2 (1) = 4.05, p <0.05]. SUD/PTSD patients were significantly more often unemployed and had a lower educational level.
We further examined whether there might be a more severe pattern of comorbidity (axis I or II) in patients with SUD/PTSD. A significant relation existed between depressive disorders and PTSD. Patients with SUD/PTSD were more likely to have depressive disorders [χ2 (2) = 13.32, p<0.001, with Cramer's V=0.19] than SUD/no PTSD patients. Secondly, SUD/PTSD patients were significantly more likely to be patients with other axis I disorders compared to SUD/no PTSD patients [χ2 (1) = 13.78, p<0.001, with Cramer's V=0.19]. No other significant results were found in examining axes I and II disorders in both groups.
Discussion
A first goal of the study was to gain insight into the prevalence of PTSD and trauma exposure in SUD patients and to compare these numbers with the prevalence of current PTSD and trauma exposure in a healthy control group using the same diagnostic tool. In the present study, we found that 36.6% of SUD patients scored positive on PTSD. Almost every patient had encountered at least one traumatic experience in his/her lifetime. As hypothesised, these numbers were significantly lower in individuals without substance dependence. In this group we found a PTSD prevalence rate of 10.2%, and 86.3% of the persons in this control group had experienced some kind of traumatic event.
We cannot directly compare these results with earlier research, because this study is the first, to our knowledge, that contrasts the prevalence of current PTSD in a heterogeneous SUD population with PTSD in a control group within the same study using the same questionnaire. Nevertheless, the results of some comparable studies (measuring current PTSD in a heterogeneous SUD population) are consistent with our prevalence data. In prior studies in SUD populations, current PTSD was found to be prevalent in 25.3–41% of cases (Bonin et al., 2000; Driessen et al., 2008; Ouimette et al., 2007; Read et al., 2004; Reynolds et al., 2005). Studies in SUD populations that assessed prevalence rates of trauma exposure typically report percentages between 89 and 95% (Dansky, Saladin, Coffey, & Brady, 1997; Farley, Golding, Young, Mulligan, & Minkoff, 2004; Read et al., 2004; Reynolds et al., 2005), which concurs with the present results.
One discrepant finding with previous research is the relatively high number of current PTSD in the control group; in this study, 10.2% of the control subjects had a positive diagnosis. It should be noted that the present sample of healthy controls does not represent the general population. These healthy controls signed up as voluntary participants for psychology research in response to a recruitment advertisement on the university website. Conceivably, individuals who suffer(ed) from psychological problems may be more readily inclined to participate in psychological research such as the present study. Indeed, other researchers have found a typical prevalence rate below 4% in the general population (Bromner, Peek, Bronner, Last, & Grootenhuis, 2009; Creamer, Burgess & McFarlane, 2001; Darves-Bornoz et al., 2008; De Vries & Olff, 2009). Another possible explanation for the high number of PTSD in the control group might be that the SRIP overestimates PTSD. This option does not seem valid because of two reasons. Firstly, researchers documented a good specificity for the SRIP, reflecting a low risk for overdiagnosis (Hovens et al., 2002; Witteveen et al., 2005). Secondly, if the SRIP overestimates PTSD, the same profile should be noted in the SUD group.
The fact that many SUD patients score positive on PTSD has important implications for clinical practice. At present, PTSD receives little attention in SUD treatment (Najavits, Sullivan, Schmitz, Weiss, & Lee, 2004) and systematically conducted screening with a validated questionnaire does not take place in more than 80% of SUD patients (Young, Rosen, & Finney, 2005). This study emphasises the need to identify the SUD/PTSD patients as a substantial and important subgroup and to systematically screen for PTSD in all SUD patients at intake.
Our second aim was to assess whether PTSD would be correctly diagnosed by interviewers and clinicians without using a standardised questionnaire. As expected, PTSD remained largely undetected when no standardised tool was used. These findings are important because they draw attention to the fact that, with regard to the diagnosis of PTSD, SUD treatment facilities should not solely rely on the opinions of clinicians and interviewers. Clinical judgement is prone to bias and, when possible, validated assessment tools should be used (Dawes, Faust, & Meehl, 1989; Garb, 2005).
The third and final goal was to evaluate whether patients in the SUD/PTSD group have a more severe clinical profile and a lower socio-economic status. Somewhat surprisingly, the SUD/PTSD patients and the group of SUD/no PTSD patients proved comparable on most patient characteristics. There were, however, four significant differences between the groups: (1) patients in the SUD/PTSD group were more often less educated, (2) the SUD/PTSD comorbid patients were more often unemployed, (3) patients with PTSD were more likely to have depressive disorders and (4) patients with PTSD were more likely to have another axis I disorder.
In sum, the present study provides further evidence for the heightened prevalence rate of PTSD among SUD patients. The treatment facilities participating in this research did not employ structural testing for PTSD among newly admitted patients. Clearly, this is associated with severe underdiagnosis of PTSD. This is a problem as it has been shown that SUD patients with comorbid PTSD may benefit from parallel treatment of their PTSD (Amaro et al., 2007; Cocozza et al., 2005; Coffey, Stasiewicz, Hughes, & Brimo, 2006; Morrissey et al., 2005; Najavits, Gallop, & Weiss, 2006; Van Dam, Vedel, Ehring, & Emmelkamp, 2012), and patients are denied a potentially more favourable treatment outcome when their PTSD remains undiagnosed (Mills, Teesson, et al., 2005; Read et al., 2004).
For the abstract or full text in other languages, please see Supplementary files under Reading Tools online
Conflict of interest and funding
There is no conflict of interest in the present study for any of the authors.
References
- Amaro H, Dai J, Arevalo S, Acevedo A, Matsumoto A, Nieves R, et al. Effects of integrated trauma treatment on outcomes in a racially/ethnically diverse sample of women in urban community-based substance abuse treatment. Journal of Urban Health. 2007;84(4):508–522. doi: 10.1007/s11524-007-9160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back S. E, Brady K. T, Sonne S. C, Verduin M. L. Symptom improvement in co-occurring PTSD and alcohol dependence. The Journal of Nervous and Mental Disease. 2006;194(9):690–696. doi: 10.1097/01.nmd.0000235794.12794.8a. [DOI] [PubMed] [Google Scholar]
- Blake D. D, Weathers F. W, Nagy L. M, Kaloupeck D. G, Gusman F. D, Charney D. S, et al. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Bonin M. F, Norton G. R, Asmundson G. J. G, Dicurzio S, Pidlubney S. Drinking away the hurt: The nature and prevalence of PTSD in substance abuse patients attending a community-based treatment program. Journal of Behavior Therapy and Experimental Psychiatry. 2000;31(1):55–66. doi: 10.1016/s0005-7916(00)00008-2. [DOI] [PubMed] [Google Scholar]
- Bromner M. B, Peek N, Bronner A. E, Last B. F, Grootenhuis M. A. A community-based survey of posttraumatic stress disorder in the Netherlands. Journal of Traumatic Stress. 2009;22(1):74–78. doi: 10.1002/jts.20379. [DOI] [PubMed] [Google Scholar]
- Cocozza J. J, Jackson E. W, Hennigan K, Morrissey J. P, Reed B. G, Fallot R, et al. Outcomes for women with co-occurring disorders and trauma: Program-level effects. Journal of Substance Abuse Treatment. 2005;28(2):109–119. doi: 10.1016/j.jsat.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Coffey S. F, Stasiewicz P. R, Hughes P. M, Brimo M. L. Trauma-focused imaginal exposure for individuals with comorbid posttraumatic stress disorder and alcohol dependence: Revealing mechanisms of alcohol craving in a cue reactivity paradigm. Psychology of Addictive Behaviors. 2006;20(4):425–435. doi: 10.1037/0893-164X.20.4.425. [DOI] [PubMed] [Google Scholar]
- Creamer M, Burgess P, McFarlane A. C. Post-traumatic stress disorder: Findings from the Australian national survey of mental health and well-being. Psychological Medicine. 2001;31:1237–1247. doi: 10.1017/s0033291701004287. [DOI] [PubMed] [Google Scholar]
- Dansky B. S, Roitzsch J. C, Brady K. T, Saladin M. E. Posttraumatic stress disorder and substance abuse: Use of research in a clinical setting. Journal of Traumatic Stress. 1997;10(1):141–148. doi: 10.1023/a:1024872800683. [DOI] [PubMed] [Google Scholar]
- Dansky B. S, Saladin M. E, Coffey S. F, Brady K. T. Use of self-report measures of crime-related posttraumatic stress disorder with substance use disordered patients. Journal of Substance Abuse Treatment. 1997;14(5):431–437. doi: 10.1016/s0740-5472(97)00120-7. [DOI] [PubMed] [Google Scholar]
- Darves-Bornoz J, Alonso J, De Girolamo G, De Graaf R, Haro J, Kovess-Msfety V, et al. Main traumatic events in Europe: PTSD in the European study of the epidemiology of mental disorders survey. Journal of Traumatic Stress. 2008;21(5):455–462. doi: 10.1002/jts.20357. [DOI] [PubMed] [Google Scholar]
- Dawes R. M, Faust D, Meehl P. E. Clinical versus actuarial judgment,. Science. New Series. 1989;243(4899):1668–1674. doi: 10.1126/science.2648573. [DOI] [PubMed] [Google Scholar]
- De Vries G, Olff M. The lifetime prevalence of traumatic events and posttraumatic stress disorder in the Netherlands. Journal of Traumatic Stress. 2009;22(4):259–267. doi: 10.1002/jts.20429. [DOI] [PubMed] [Google Scholar]
- Dragan M, Lis-Turlejska M. Prevalence of posttraumatic stress disorder in alcohol dependent patients in Poland. Addictive Behaviors. 2007;32(5):902–911. doi: 10.1016/j.addbeh.2006.06.025. [DOI] [PubMed] [Google Scholar]
- Driessen M, Schulte S, Luedecke C, Schaefer I, Sutmann F, Ohlmeier M, et al. Trauma and PTSD in patients with alcohol, drug, or dual dependence: A multi-center study. Alcoholism: Clinical and Experimental Research. 2008;32(3):481–488. doi: 10.1111/j.1530-0277.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- Emmelkamp P, Vedel E. Alcohol- en drugsverslaving. Een gids voor effectief gebleken behandelingen. [Evidence-Based treatment for Alcohol and Drug Abuse. A Practitioner's Guide to Theory, Methods, and Practice]. Amsterdam: Uitgeverij Nieuwezijds; 2007. [Google Scholar]
- Farley M, Golding J. M, Young G, Mulligan M, Minkoff J. R. Trauma history and relapse probability among patients seeking substance abuse treatment. Journal of Substance Abuse Treatment. 2004;27(2):161–167. doi: 10.1016/j.jsat.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Garb H. N. Clinical judgment and decision making. Annual Review of Clinical Psychology. 2005;1:67–89. doi: 10.1146/annurev.clinpsy.1.102803.143810. [DOI] [PubMed] [Google Scholar]
- Hovens J. E, Bramsen I, Van der Ploeg H. M. Self-rating inventory for posttraumatic stress disorder: Review of the psychometric properties of a new brief Dutch screening instrument. Perceptual and Motor Skills. 2002;94(3):996–1008. doi: 10.2466/pms.2002.94.3.996. [DOI] [PubMed] [Google Scholar]
- Hovens J. E, Van der Ploeg H. M, Bramsen I, Klaarenbeek M. T. A. The development of the self-rating inventory for posttraumatic stress disorder. Acta Psychiatrica Scandinavica. 1994;90(3):172–183. doi: 10.1111/j.1600-0447.1994.tb01574.x. [DOI] [PubMed] [Google Scholar]
- Jacobsen L. K, Southwick S. M, Kosten T. R. Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry. 2001;158:1148–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Johnson S. D. Substance use, post-traumatic stress disorder and violence. Current Opinion in Psychiatry. 2008;21(3):242–246. doi: 10.1097/YCO.0b013e3282fc9889. [DOI] [PubMed] [Google Scholar]
- Kessler R. C, Berglund P, Demler O, Jin R, Merikangas K. R, Walters E. E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Lobbestael J, Arntz A, Harkema-Schouten P, Bernstein D. Development and psychometric evaluation of a new assessment method for childhood maltreatment experiences: The Interview for Traumatic Events in Childhood (ITEC) Child Abuse Neglect. 2009;33(8):505–517. doi: 10.1016/j.chiabu.2009.03.002. [DOI] [PubMed] [Google Scholar]
- Mills K. L, Lynskey M, Teesson M, Ross J, Darke S. Post-traumatic stress disorder among people with heroin dependence in the Australian treatment outcome study (ATOS); prevalence and correlates. Drug and Alcohol Dependence. 2005;77:243–249. doi: 10.1016/j.drugalcdep.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Mills K. L, Teesson M, Ross J, Darke S, Shanahan M. The costs and outcomes of treatment for opiod dependence associated with post traumatic stress disorder. Psychiatric Services. 2005;56:940–945. doi: 10.1176/appi.ps.56.8.940. [DOI] [PubMed] [Google Scholar]
- Mills K. L, Teesson M, Ross J, Peters L. Trauma, PTSD and substance use disorders: Findings from the Australian national survey of mental health and well-being. American Journal of Psychiatry. 2006;163:651–658. doi: 10.1176/ajp.2006.163.4.652. [DOI] [PubMed] [Google Scholar]
- Morrissey J. P, Jackson E. W, Ellis A. R, Amaro H, Brown V. B, Najavits L. M. Twelve-month outcomes of trauma-informed interventions for women with co-occurring disorders. Psychiatric Services. 2005;56(10):1213–1222. doi: 10.1176/appi.ps.56.10.1213. [DOI] [PubMed] [Google Scholar]
- Najavits L. M. Theoretical perspective on posttraumatic stress disorder and substance use disorder. Australian Psychologist. 2005;40(2):118–126. [Google Scholar]
- Najavits L. M, Gallop R. J, Weiss R. D. Seeking safety therapy for adolescent girls with PTSD and substance use disorder: A randomized controlled trial. Journal of Behavioral Health Services & Research. 2006;33(4):453–463. doi: 10.1007/s11414-006-9034-2. [DOI] [PubMed] [Google Scholar]
- Najavits L. M, Sullivan T. P, Schmitz M, Weiss R. D, Lee C. S. N. Treatment utilization by women with PTSD and substance dependence. The American Journal on Addiction. 2004;13:215–224. doi: 10.1080/10550490490459889. [DOI] [PubMed] [Google Scholar]
- Nijenhuis E. R. S, Van der Hart O, Kruger K. The psychometric characteristics of the Traumatic Experiences Questionnaire (TEC): First findings among psychiatric outpatients. Clinical Psychology and Psychotherapy. 2002;9(3):200–210. [Google Scholar]
- Norman S. B, Tate S. R, Anderson K. G, Brown S. A. Do trauma history and PTSD symptoms influence addiction relapse context? Drug and Alcohol Dependence. 2007;90(1):89–96. doi: 10.1016/j.drugalcdep.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Ouimette P, Coolhart D, Funderburk J. S, Wade M, Brown P. J. Precipitants of first substance use in recently abstinent substance use disorder patients with PTSD. Addictive Behaviors. 2007;32(8):1719–1727. doi: 10.1016/j.addbeh.2006.11.020. [DOI] [PubMed] [Google Scholar]
- Ouimette P, Goodwin E, Brown P. J. Health and well being of substance use disorder patients with and without posttraumatic stress disorder. (2006) Addictive Behaviors. 2006;31:1415–1423. doi: 10.1016/j.addbeh.2005.11.010. [DOI] [PubMed] [Google Scholar]
- Peirce J. M, Kindbom K. A, Waesche M. C, Yuscavage A. S. E, Brooner R. K. Posttraumatic stress disorder, gender, and problem profiles in substance dependent patients. Substance Use and Misuse. 2008;43:596–611. doi: 10.1080/10826080701204623. [DOI] [PubMed] [Google Scholar]
- Read J. P, Brown P. J, Kahler C. W. Substance use and posttraumatic stress disorders: Symptom interplay and effects on outcome. Addictive Behaviors. 2004;29(8):1665–1672. doi: 10.1016/j.addbeh.2004.02.061. [DOI] [PubMed] [Google Scholar]
- Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug and Alcohol Dependence. 2005;77(3):251–258. doi: 10.1016/j.drugalcdep.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Sheehan D. V, Lecrubier Y, Harnett Sheehan K, Janavs J, Weiller E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry. 1997;12:232–241. [Google Scholar]
- Van Balkom A. J. L. M, De Beurs E, Hovens J. E. J. M, Van Vliet I. M. Meetinstrumenten bij angststoornissen. [Assessment of Anxiety Disorders] Tijdschrift voor Psychiatrie. 2004;46(10):687–692. [Google Scholar]
- Van Dam D, Vedel E, Ehring T, Emmelkamp P. M. G. Psychological treatments for concurrent posttraumatic stress disorder and substance use disorder: A systematic review. Clinical Psychology Review. 2012;32:202–214. doi: 10.1016/j.cpr.2012.01.004. [DOI] [PubMed] [Google Scholar]
- Van der Bossche C. M. R, Kremers I, Sieswerda S. H, Arntz A. Vragenlijst naar Belastende Gebeurtenissen (VBG) [Structured Childhood Trauma Interview] Maastricht: Maastricht University; 1999. [Google Scholar]
- Weathers F. W, Keane T. M, Davidson J. R. T. Clinical-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Witteveen A. B, Bramsen I, Hovens J. E, Van der Ploeg H. M. Utility of the impact of event scale in screening for posttraumatic stress disorder. Psychological Reports. 2005;97:297–308. doi: 10.2466/pr0.97.1.297-308. [DOI] [PubMed] [Google Scholar]
- Young H. E, Rosen C. S, Finney J. W. A survey of PTSD screening and referral practices in VA addiction treatment programs. Journal of Substance Abuse Treatment. 2005;28:313–319. doi: 10.1016/j.jsat.2005.02.006. [DOI] [PubMed] [Google Scholar]