Abstract
Introduction
Patient care in the emergency department (ED) is often complicated by the inability to obtain an accurate prior history even when the patient is able to communicate with the ED staff. Personal health records (PHR) can mitigate the impact of such information gaps. This study assesses ED patients' willingness to adopt a PHR and the treating physicians' willingness to use that information.
Methods
This cross-sectional study was answered by 184 patients from 219 (84%) surveys distributed in an academic ED. The patient surveys collected data about demographics, willingness and barriers to adopt a PHR, and the patient's perceived severity of disease on a 5-point scale. Each patient survey was linked to a treating physician survey of which 210 of 219 (96%) responded.
Results
Of 184 surveys completed, 78% of respondents wanted to have their PHR uploaded onto the Internet, and 83% of providers felt they would access it. Less than 10% wanted a software company, an insurance company, or the government to control their health information, while over 50% wanted a hospital to control that information. The patients for whom these providers would not have used a PHR had a statistically significant lower severity score of illness as determined by the treating physician from those that they would have used a PHR (1.5 vs 2.4, P < 0.01). Fifty-seven percent of physicians would only use a PHR if it took less than 5 minutes to access.
Conclusion
The majority of patients and physicians in the ED are willing to adopt PHRs, especially if the hospital participates. ED physicians are more likely to check the PHRs of more severely ill patients. Speed of access is important to ED physicians.
INTRODUCTION
A personal health record (PHR) is a patient-controlled tool used to manage health information.1–3 By centralizing the patient's medical history, different physician encounters, evaluations and treatments, a PHR offers more complete medical information. The individual can access and has ownership of this information, making PHRs a consumer-centered model that bridges different providers.4 Increased adoption of PHRs might lead to better care by providing the physician with a more complete picture of the patient, thereby reducing errors and improving follow-up regardless of provider location or network interoperability.1,5,6
Some of the barriers to PHR adoption previously identified include the economic costs of developing and paying for the system, transferring information from paper charts, an inadequate level of computer competency on the part of physicians and patients, and an absence of a universal or standard platform for interoperability.1,7,8 Emergency departments (ED) might provide an alternative method for increasing patient use of PHRs since they serve as an entry point into the medical system. Patients might be uniquely willing to initiate a PHR while waiting for ED care and the importance of their medical care is in focus. This study aims to identify which ED patients are willing to initiate a PHR and whether the treating ED physicians would use this PHR. Our primary hypothesis was that most ED patients are willing to have their data entered into a PHR and that their willingness is a function of their severity of illness. Also, we hypothesized that ED physicians are more likely to review PHRs of patients that they perceive to be more seriously ill.
METHODS
Study Design
This was an observational cross-sectional survey study (Appendix, online only). Stanford's Institutional Review Board approved this study and waived the signature requirement for patient consent; verbal consent was obtained.
Study Setting and Population
Surveys were distributed between April 2008 and November 2008 at the Stanford University Medical Center Emergency Department. Stanford University Medical Center is an academic level 1 trauma center with an annual patient volume in the ED of 50,000. Physicians and nurses at Stanford use EPIC (EPIC Spring 2007 IU1; Verona, Wisconsin) for electronic health records. Images and medications are also ordered and stored in EPIC. Currently, no PHR is offered by Stanford.
Study Protocol
The study population was comprised of a convenience sample of patients over 18 presenting to the ED who were medically stable. A research assistant did a rotating shift, 7:00 am to 3:00 pm, 3:00 pm to 11:00 pm, and 11:00 pm to 7:00 am, approaching patients, distributing and collecting surveys at regular intervals. Patients well enough to respond were asked if they would be willing to answer questions and either handed the survey to read or read the survey by the assistant. A standard introduction was read to all patients. Patients unable or unwilling to answer the survey were excluded; however, their treating physician was still surveyed to gather data on the physician's willingness to use the PHR. Consequently, there are more physician responses than patient responses. Similarly, patients whose corresponding physician could not be surveyed were not excluded.
The patient survey described a PHR and then asked 24 questions answered via checking a box on 1 double-sided page. Demographic data on age, race, sex, insurance coverage, income, and education level was collected. We asked the patient about their perceived state of health, computer familiarity, and degree of concern about their current visit as measured on a 5-point scale. In addition, the survey assessed patient attitudes towards PHR availability, utilization, and security.
A separate physician survey asked whether they would have accessed the given patient's PHR at all, whether they would spend less than 5 minutes, 5 to 10 minutes, or over 15 minutes accessing the patient's PHR, and how sick they considered the patient to be as measured on a 5-point scale. Physician and patient surveys were coupled through a nonidentifying marker and stored for analysis. Neither physician nor patient ever saw their counterpart's survey. Prior to use, the survey was distributed to several patients and physicians to assess its readability.
Data Analysis
Statistical analysis was completed with the aid of SAS software (9.0, Cary, North Carolina). Descriptive statistics were computed for demographic and preference characteristics. The primary mode of comparison was achieved with a chi-square test for binary comparisons such as willingness to use a PHR between different comparison groups. A Mann-Whitney test was used for ranked comparisons that involved a response with the 5-point scale, such as willingness to use a PHR and severity of illness. Significance was determined by a P value less than 0.05. A power calculation for proportions suggested a sample size of 190, given a power of 80 and a significance level of 0.05, in order to test our primary hypothesis that patient willingness to use a PHR related to the severity of their illness.
RESULTS
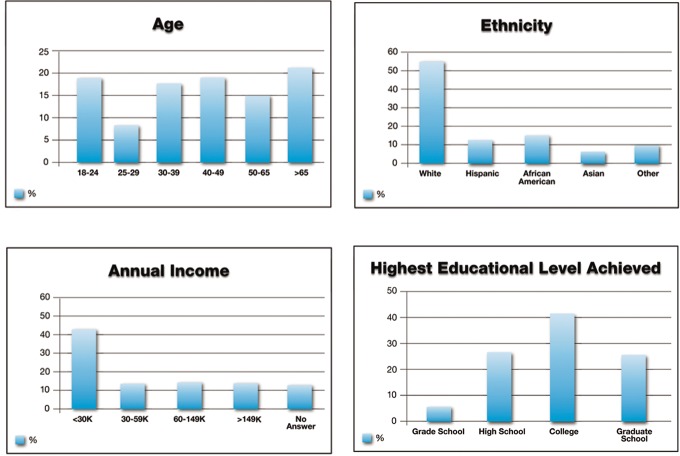
A total of 219 patients were approached, and 184 (84%) surveys were completed. Thirty-five surveys were excluded for incompleteness or patients who refused to be surveyed. Of the 219 physician surveys distributed, 210 (96%) were returned. All physicians agreed to answer the survey. The resultant demographics are summarized in Figure 1. Males comprised 56% of the sample population, while females comprised 44%. In the survey population, 93% were insured (including Medicaid recipients), 78% had a primary care provider, and 54% had changed providers in the past 5 years.
Figure 1.
Patient demographics.
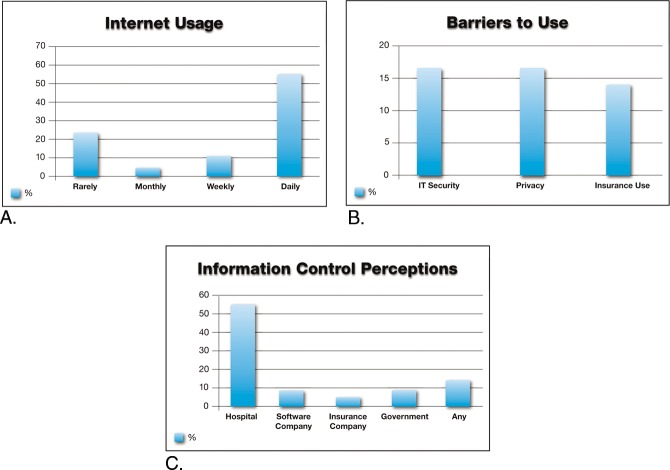
Seventy-eight percent of the respondents were willing to have all of their health information available on the Internet. In a life-threatening emergency, 96% of respondents wanted the physician to access all of their health information. Of those surveyed, 68% would upload their information only if they did not have to perform the task of entering the information. As summarized in Figure 2, over 50% of respondents used the Internet daily, and a similar percentage wanted the hospital to retain their health information. Respondents with multiple medical problems, life threatening allergies, a primary doctor, and private insurance were just as likely to use a PHR as those who did not have these characteristics (P > 0.05, chi-square). There was no significant relationship between the patient's perceived severity of disease and their willingness to use a PHR (P > 0.05, Mann-Whitney).
Figure 2.
A, Frequency of Internet use. B, Perceived barriers to uploading information. C, Location where patients would allow their information to be stored. IT, information technology.
Providers assigned an illness severity score for each patient. Eighty-three percent of providers would have accessed the PHR. The patients for whom the providers would not have used a PHR had significantly lower average severity score (1.5) than those for whom they would have used a PHR (2.4) (P < 0.01 by Mann-Whitney test). Among the physicians who would not have used the PHR of a patient under their care, 74% of these patients had 0 to 1 medical problem. Among providers who wanted to use their patient's PHR, 57% would only use the PHR if it took less than 5 minutes to access and review.
DISCUSSION
Seventy-eight percent of patients surveyed in the ED were willing to adopt a PHR. However, while more than half of the patients surveyed would accept the hospital as the source of the PHR, less than 10% would accept control by a private software enterprise or even a governmental agency (Figure 2). Other factors related to PHR adoption included assistance with information upload, as 68% of users would upload their information only if they didn't have to do it themselves.
Emergency physicians were very likely to use a PHR if it was available, though they usually did not want to spend more than 5 minutes interfacing with the system. They were more likely to use the system for patients with more than 1 medical problem and those with a higher illness severity. Though not specific to the ED, time constraints may heighten the need for a rapidly accessible PHR in complicated patients.
LIMITATIONS
The sample's demographics may limit generalizability of the results. Though many income levels were represented, the demographics of our sample do not mirror those of many rural or county EDs or many urban and academic institutions. Additionally, the critical or unresponsive patients who might have benefited from a PHR could not be assessed, so a proportion of ill patients were lost from this assessment. As there is often a discrepancy between stated patient intent and actual patient action, expressing a willingness to adopt a PHR does not necessarily translate into actual completion of the act. Our study only measured their willingness. In addition, the 5-point scale was not previously validated to assess injury severity. Also, physicians were surveyed throughout the day and over 8 months to capture a variety of providers, but it is possible that bias was introduced by multiple responses from a given provider.
CONCLUSION
This survey suggests that many ED patients in this population are willing to start a PHR, and ED physicians would likely access it. Patients would be more comfortable if the PHR was created for them and was controlled by a healthcare facility rather than a nonhealthcare private entity or a governmental agency. Development should focus on speed of access for physicians while focusing on assisting initiation for patients. Though a PHR can be discussed and initiated during a primary care visit, the ED might provide an additional opportunity when wait times permit further consideration and patients are worried about their health. We feel that the ED is a potential focal point for PHR developers and hospitals interested in PHR adoption and utilization.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
REFERENCES
- 1.Tang PC, Ash JS, Bates DW, et al. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13:121–126. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Demiris G, Afrin LB, Speedie S, et al. Patient-centered applications: use of information technology to promote disease management and wellness. A white paper by the AMIA knowledge in motion working group. J Am Med Inform Assoc. 2008;15:8–13. doi: 10.1197/jamia.M2492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Detmer D, Bloomrosen M, Raymond B, et al. Integrated personal health records: transformative tools for consumer-centric care. BMC Med Inform Decis Mak. 2008;8:45. doi: 10.1186/1472-6947-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sittig DF. Personal health records on the internet: a snapshot of the pioneers at the end of the 20th Century. Int J Med Inform. 2002;65:1–6. doi: 10.1016/s1386-5056(01)00215-5. [DOI] [PubMed] [Google Scholar]
- 5.Caglar S, Henneman PL, Blank FS, et al. Emergency department medication lists are not accurate. J Emerg Med. 2008;40:613–616. doi: 10.1016/j.jemermed.2008.02.060. [DOI] [PubMed] [Google Scholar]
- 6.Ralston JD, Carrell D, Reid R, et al. Patient web services integrated with a shared medical record: patient use and satisfaction. J Am Med Inform Assoc. 2007;14:798–806. doi: 10.1197/jamia.M2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson DM, Asher LM, Wilson EA. Physician computer skills: a prerequisite to the future in healthcare services. J Ky Med Assoc. 2007;105:67–71. [PubMed] [Google Scholar]
- 8.Maloney FL, Wright A. USB-based personal health records: An analysis of features and functionality. Int J Med Inform. 2010;79:97–111. doi: 10.1016/j.ijmedinf.2009.11.005. [DOI] [PubMed] [Google Scholar]