Abstract
Background
Highly pathogenic H5N1 avian influenza viruses continue to spread via waterfowl, causing lethal infections in humans. Vaccines can prevent the morbidity and mortality associated with pandemic influenza isolates. Predicting the specific isolate that may emerge from the 10 different H5N1 clades is a tremendous challenge for vaccine design.
Methods
In this study, we generated a synthetic hemagglutinin (HA) on the basis of a new method, computationally optimized broadly reactive antigen (COBRA), which uses worldwide sequencing and surveillance efforts that are specifically focused on sequences from H5N1 clade 2 human isolates.
Results
Cynomolgus macaques vaccinated with COBRA clade 2 HA H5N1 virus-like particles (VLPs) had hemagglutination-inhibition antibody titers that recognized a broader number of representative isolates from divergent clades as compared to nonhuman primates vaccinated with clade 2.2 HA VLPs. Furthermore, all vaccinated animals were protected from A/Whooper Swan/Mongolia/244/2005 (WS/05) clade 2.2 challenge, with no virus detected in the nasal or tracheal washes. However, COBRA VLP–vaccinated nonhuman primates had reduced lung inflammation and pathologic effects as compared to those that received WS/05 VLP vaccines.
Conclusions
The COBRA clade 2 HA H5N1 VLP elicits broad humoral immunity against multiple H5N1 isolates from different clades. In addition, the COBRA VLP vaccine is more effective than a homologous vaccine against a highly pathogenic avian influenza virus challenge.
Since the first identified cases of H5N1 influenza in Hong Kong [1], the World Health Organization (WHO) influenza surveillance network increased its intensive monitoring of both human and avian populations for influenza virus infections [2]. Following the resurgence and subsequent spread of H5N1 influenza in 2004, there has been an intense need for vaccine strategies that elicit broadly reactive immunity against H5N1 isolates, in light of its pandemic potential. Vaccination is a potent and cost-effective countermeasure to the threat of seasonal or pandemic outbreaks of influenza [3]. However, there are several challenges for designing an effective vaccine against H5N1 influenza, including the phylogenetic characterization and sequence homology in hemagglutinin (HA) that groups H5N1 viruses into 10 clades as defined by the WHO/OIE/FAO H5N1 Evolution Working Group [4], with many clades having additional subclades and sub-subclades [5]. Human infections have been limited to clades 0, 1, 2, and 7.
To address the sequence diversity inherent in H5N1 isolates circulating in avian populations, consensus strategies have been designed for vaccine development [6, 7]. Our research group has expanded on the consensus strategy and developed computationally optimized broadly reactive antigen (COBRA) strategies to overcome pathogen sequence diversity. Traditional consensus sequences are generated by aligning a population of sequences and selecting the most common residue at each position [7–10]. The COBRA method of antigen design uses multiple rounds of consensus generation to address antigenic diversity, specifically within clade 2 H5N1 HA sequences (Figure 1).
Figure 1.
Phylogenetic diversity of H5N1 influenza virus. The unrooted phylogenetic tree was inferred from hemagglutinin (HA) amino acid sequences derived from 8–10 representative isolates in all clades and subclades and also the computationally optimized broadly reactive antigen (COBRA) HA, using the maximum likelihood method. Clade/subclade clusters were identified and are indicated in the shaded ovals. The star identifies where the COBRA antigen is located relative to the various representative isolates. Sequences were aligned with MUSCLE 3.7 software, and the alignment was refined by Gblocks 0.91b software. Phylogeny was determined using the maximum likelihood method with PhyML software. Trees were rendered using TreeDyn 198.3 software [44]. The National Center for Biotechnology Information accession numbers for the HA sequences used in phylogeny inference were obtained through the Influenza Virus Resource [45].
While these mouse and ferret models are effective for seasonal influenza vaccine studies [11–16], they are not as informative for determining protective efficacy by H5N1 vaccines. There is often a lack of correlation between hemagglutination inhibition (HAI) and protection against H5N1 challenge [11, 13, 17–19]. Therefore, we chose to use a nonhuman primate model to determine the breadth of HAI and the ability to protect against H5N1 infection and pathologic effects. Nonhuman primate models have been effectively used for H5N1 (clades 0 and 1) [20], as well as the reconstructed 1918 H1N1 influenza virus [21], since the pathologic effects of infection with these highly pathogenic influenza viruses are similar to those in humans. However, there is currently no published nonhuman primate model that is based on an avian clade 2 H5N1 isolate and demonstrates the pathologic or immune responses induced following infection of vaccinated or unvaccinated macaques.
In this report, COBRA HA proteins were displayed on the surface of a virus-like particle (VLP) and used to vaccinate cynomolgus macaques. The elicited immune responses were directly compared to a VLP with the HA from a clade 2.2 isolate, A/Whooper swan/Mongolia/244/2005, to analyze the protective responses to H5N1 challenge because the clade 2.2 viruses are the most geographically widespread of the H5N1 isolates [22–25]. The COBRA HA VLP not only elicited broader antibody responses against H5N1 but also protected nonhuman primates from clade 2.2 H5N1 challenge more efficiently than the homologous vaccine.
MATERIAL AND METHODS
Expression and Purification of VLPs
The COBRA HA sequence has been described [26]. Briefly, the sequence was generated by aligning amino acid sequences of all available HA proteins isolated from clade 2 H5N1 human infections (2004–2007) and deposited in the Influenza Virus Resource database available through the National Center for Biotechnology Information. 293T cells were transiently transfected with plasmids expressing HA, M1, and neuraminidase (NA) in low-serum media, incubated for 72 hours at 37°C, and purified by ultracentrifugation through a 20% glycerol cushion as previously described [26]. HA content was quantified as previously described [26] with WS/05 VLPs at 0.38 μg/μL HA and COBRA VLPs at 0.27 μg/μL. Vaccines were normalized for HA content (15 μg), and HA titer was measured to confirm quality. HA titers of both vaccines were between 1:256 and 1:512 at all time points.
Nonhuman Primate Immunizations and H5N1 Challenges
Cynomolgus macaques (Macaca fascicularis, male, 3–5 years old) were vaccinated with 15 μg (on the basis of HA content) of purified COBRA HA VLPs (n = 7) or WS/05 VLPs (n = 7) via intramuscular injection at weeks 0, 3, and 6. Vaccines at each dose were formulated with alum adjuvant (Imject Alum, Pierce Biotechnology, Rockford, IL) immediately prior to use. Imject Alum adjuvant and vaccine schedule were chosen on the basis of findings from a previous study involving ferrets (unpublished observations). Ferrets vaccinated with VLP without an adjuvant had a poor seroconversion rate, and even with the adjuvant mixture, the ferret HAI titers were still low. Although the exact formulation of this adjuvant is different from that approved for use in humans, it is reasonable to expect similar performance. Twenty-one days after each vaccination, blood was collected from anesthetized macaques. All procedures were in accordance with the NRC Guide for the Care and Use of Laboratory Animals and with the approval of University of Pittsburgh IACUC and biosafety officials.
Three weeks after final vaccination, macaques were placed into BSL3+ isolator units (Bioqual, Rockville, MD) and challenged by multiple routes of infection (ocular, nasal, and tracheal) as previously described [21, 27, 28], using 1 × 106 plaque-forming units (PFU) of the highly pathogenic H5N1 virus A/Whooper Swan/Mongolia/244/2005 (clade 2.2) at each location. Nonhuman primates were monitored daily for weight loss, signs of disease, and mortality until 7 days after infection. Individual body weights, sickness scores (determined on the basis of lethargy, temperature change, nasal discharge, lack of appetite, dehydration, and lack of responsiveness), and death were recorded for each group.
Nasal and tracheal washes were performed at days 0, 1, 3, 5, and 7 after infection. In addition, subsets of nonhuman primates were sacrificed following administration of anesthesia, and necropsies were performed according to standard procedures for assessment of gross pathologic and histopathologic changes, as well as the extent of virus replication.
Serological Assays
A quantitative enzyme-linked immunosorbant assay (ELISA) was performed to assess anti-HA specific immunoglobulin G (IgG) in immune serum as previously described [17, 26]. The hemagglutination inhibition (HAI) assay was used on sera treated with receptor-destroying enzyme (RDE; Denka Seiken, Japan) prior to being tested [11, 14, 17] to assess functional antibodies to the HA that were able to inhibit agglutination of horse red blood cells [29], as adapted from the Centers for Disease Control and Prevention's laboratory-based influenza surveillance manual [3, 17]. Serum neutralizing antibody titers were determined by microneutralization (MN) assays performed on Madin Darby Canine Kidney (MDCK) cells after the procedure, until cytopathic effect was observed [30]. The neutralizing antibody titers are expressed as the reciprocal of the highest dilution of serum that gave 50% neutralization of 100 median tissue culture infective doses of virus in MDCK cells. Geometric mean neutralizing antibody titers were calculated for each group.
Histopathologic Evaluation and Immunohistochemical Analysis
Formalin-inflated lungs and trachea were fixed in 10% neutral buffered formalin. Cross-sections of upper and lower left and right lung lobes and trachea were made, concentrating on gross lesions. Tissue was paraffin embedded, and 6-μm sections were stained with hematoxylin and eosin for histologic evaluation. Sequential sections were processed for immunohistochemistry or in situ hybridization. Immunohistochemistry was performed as described previously [31], using an immunoperoxidase method with a polyclonal antibody (Maine Biotechnology Services, Portland, ME) directed against influenza A virus. A biotinylated donkey anti–goat IgG (Rockland Immunochemicals, Gilbertsville, PA) was used as the secondary antibody. In situ hybridization was performed as described previously [32], using a 35S-labeled riboprobe synthesized using templates derived from 760 base pairs of influenza A/California/04/2009 matrix protein.
RESULTS
Vaccine-Induced Antibody Responses
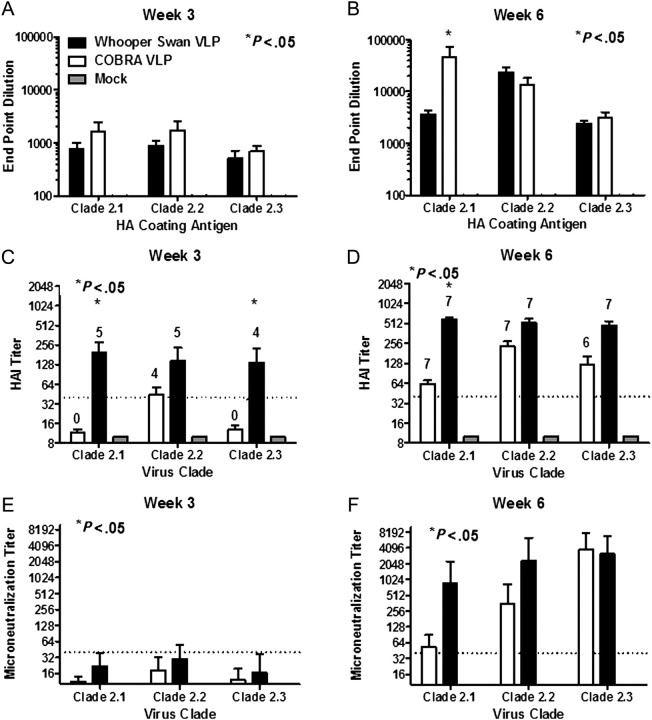
Cynomolgus macaques were vaccinated with COBRA VLPs or WS/05 VLPs formulated with Imject alum at 0, 3, and 6 weeks. At week 3 after vaccination, all COBRA VLP–vaccinated animals had anti-HA antibodies that recognized recombinant HA derived from 3 subclades of clade 2, which were boosted at week 6 (Figure 2A and 2B). There was no statistical difference (P > .05) in the anti-HA titers elicited against any of the HA proteins, except nonhuman primates vaccinated with COBRA VLPs had a statistically higher titer against the Indo/05 HA (clade 2.1), compared with nonhuman primates vaccinated with the WS/05 VLP (derived from clade 2.2) on week 6.
Figure 2.
Serological findings. Total immunoglobulin G (IgG) levels at week 3 (A) and week 6 (B) were determined via enzyme-linked immunosorbant assay for each vaccine group. Each collected antiserum was assayed for antibody binding to representative hemagglutinin (HA) molecules from clade 2.1 (A/Indonesia/5/2005), clade 2.2 (A/Whooper Swan/Mongolia/244/2005), and clade 2.3 (A/Anhui/1/2005). Hemagglutination inhibition titers for each vaccine group were determined at week 3 (C) and week 6 (D), using representative H5N1 influenza viruses: clade 2.1 (A/Indonesia/5/2005), clade 2.2 (A/Whooper swan/Mongolia/244/2005), and clade 2.3 (A/Anhui/1/2005). The number of nonhuman primates that responded with a titer >1:40 is listed above each bar. None of the mock-vaccinated animals responded, and no value is listed. Neutralizing antibody at week 3 (E) and week 6 (F) was determined via mVN for each vaccine group. All values represent the geometric mean titer (95% confidence interval). Statistical significance of the antibody titer data was determined using 2-way analysis of variance followed by the Bonferroni posttest to analyze differences between each vaccine group for each of the different antigens that were tested (multiparametric). Significance was defined as P < .05. Statistical analyses were performed with GraphPad Prism software. Abbreviations: COBRA, computationally optimized broadly reactive antigen; VLP, virus-like particle.
A Single COBRA VLP Vaccination Induced High-Titer HAI and MN Antibodies to Clade 2 H5N1 Viruses
Nonhuman primates vaccinated with COBRA VLPs (but not with WS/05 VLPs) had HAI activity against viruses representing all 3 clade 2 subclades after a single vaccination (Figure 2C). Four to six nonhuman primates responded to the COBRA VLP vaccine, with an HAI titer ≥1:40 for all of the various test antigens. In contrast, 4 of 7 nonhuman primates vaccinated with the WS/05 VLP responded to the homologous clade 2.2 virus, but none of these vaccinated nonhuman primates responded to the clade 2.1 or 2.3 virus. Following a second vaccination, almost all the nonhuman primates vaccinated with either vaccine responded to all 3 viruses (Figure 2D). These results were confirmed by microneutralization assay (Figure 2E and 2F). However, nonhuman primates vaccinated with COBRA VLPs showed boosted HAI titers to all 3 clade 2 viruses (Figure 3).
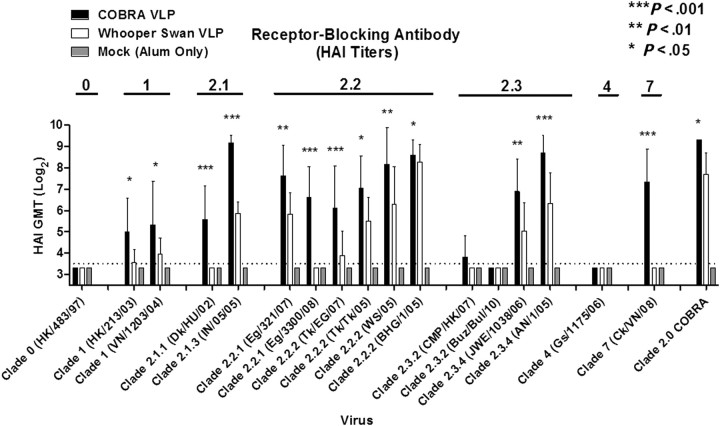
Figure 3.
Hemagglutination inhibition (HAI) serum antibody titers from vaccinated nonhuman primates against a panel of clade 0, 1, 2, 4, and 7 isolates. HAI titer for each vaccine group was determined at week 6 by use of H5N1 influenza viruses. Values represent the geometric mean titer (95% confidence interval) of log2-transformed titers Significant differences were determined by 2-way analysis of variance with the Bonferroni posttest to evaluate differences between the vaccine formulations for each test antigen. A P value of <.05 was considered significant as described in Figure 2. Abbreviations: COBRA, computationally optimized broadly reactive antigen; GMT, geometric mean titer; VLP, virus-like particle.
COBRA VLPs Induced HAI Antibodies That Recognize Broader Numbers of H5N1 Viruses
Antisera collected from both vaccinated and unvaccinated nonhuman primates were then tested against a broad panel of H5N1 viruses representing not only subclades of clade 2, but also nonclade 2 H5N1 virus strains (0, 1, 4, and 7) by HAI. Nonhuman primates vaccinated with the COBRA VLP had high average HAI titers against all clade 2 isolates, regardless of subclade (Figure 2). In general, all 7 nonhuman primates responded to the COBRA VLP vaccine and seroconverted, with an HAI titer ≥1:40 against all the clade 2 viruses. In contrast, nonhuman primates vaccinated with the WS/05 VLP vaccine had lower HAI titers against clade 2 viruses (Figure 2), and fewer number of nonhuman primates responded to the vaccine. Of the 10 clade 2 viruses tested in the HAI assay, WS/05 VLP–vaccinated nonhuman primates responded more poorly (<4 of 7 nonhuman primates) to 4 of the isolates, and none of these nonhuman primates had antibodies that responded to the Dk/HU/02 (clade 2.1.1) or Eg/3300/08 (clade 2.2.1) isolates. The COBRA VLPs elicited significantly higher HAI titers than the WS/05 VLPs against almost all of the clade 2 viruses (Figure 3).
In addition to clade 2 isolates, a minimum of 5 COBRA VLP–vaccinated nonhuman primates had HAI antibodies against both clade 1 and 7 virus isolates (Figure 3). In comparison, almost none of the WS/05 VLP–vaccinated nonhuman primates had HAI antibodies against clade 1 and clade 7 viruses. None of the nonhuman primates, regardless of the vaccine, had antibodies that responded to the clade 0 or 4 isolates. All mock-vaccinated nonhuman primates did not recognize any of the H5N1 isolates.
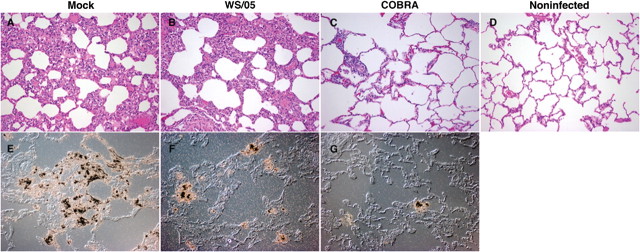
Challenge of Vaccinated and Unvaccinated Non-human Primates with H5N1 Clade 2.2 Virus
Three weeks after final vaccination, both VLP-vaccinated and mock-vaccinated nonhuman primates were transferred to ABSL3+ isolator units and then challenged with highly pathogenic H5N1 virus, A/Whooper Swan/Mongolia/244/2005 (clade 2.2) (1 × 106 PFU), by multiple routes of infection (ocular, nasal, tracheal, and oral) [21, 27, 28]. There was no significant weight loss or mortality in any of the nonhuman primates over the 7-day period of observation. Unvaccinated nonhuman primates had an elevated temperature of approximately 2°C (from 38°C to 39–40°C) that was sustained for 5 days after infection and had higher gross pathology scores by day 3 after infection (Table 1). The lungs of unvaccinated nonhuman primates had mild-to-moderate acute pneumonia with alveolar pulmonary exudate by day 3 after infection, as shown by hematoxylin-eosin staining (Figure 4A). In situ hybridization showed focal collections of H5N1-infected cells present at day 3 after infection in alveolar spaces and, to a lesser extent, in bronchial epithelium (Figure 4E). These results were similar to those for unvaccinated nonhuman primates infected with the clade 1 H5N1 virus A/Vietnam/1203/2004. In contrast, nonhuman primates vaccinated with either the COBRA VLP or the WS/05 VLP vaccine had a reduced gross pathology scores of 2.1–3.3 at day 3 after infection, with a milder increase in body temperature (1.1°C–1.3°C) that spiked between days 2–3 after infection and then returned to the preinfection value (38°C). Vaccinated animals had fewer H5N1-infected cells that were detected primarily on day 1 after infection (Figure 4F and 4G and Table 1). However, nonhuman primates vaccinated with the COBRA VLP had little to no signs of lung inflammation by hematoxylin-eosin staining (Figure 4C), while animals vaccinated with the WS/05 VLP vaccine had signs of inflammation similar to those in nonvaccinated nonhuman primates (Figure 4B and Table 2). In addition, unvaccinated nonhuman primates had high titers of virus in both the nasal and tracheal washes between days 3 and 5 after infection. In contrast, no virus was detected in either vaccinated group.
Table 1.
H5N1 Lung Infection Scores
| Vaccine | Bronchial Infection Score |
Alveolar Infection Score |
Submucosal Infection Score |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Day after infection | 1 | 3 | 5 | 1 | 3 | 5 | 1 | 3 | 5 |
| Mock | 1.00 | 0.5 | 0 | 1.10 | 0.48 | 0.25 | 0 | 0 | 0 |
| WS/05 VLP | 0.5 | 0 | 0 | 0.55 | 0.10 | 0 | 0 | 0 | 0 |
| COBRA VLP | 0 | 0 | 0 | 0.60 | 0.3 | 0.5 | 0 | 0 | 0 |
In situ hybridization for influenza virus was performed on tissue sections from the upper and lower left and right lung. The following semiquantitative scoring system was developed to evaluate the presence of influenza infected cells: 0.2, rare or occasional cells but <5% of fields; 1, >0.5 to 0.25 low-power fields; 2, >0.25 low-power fields; 3, essentially all low-power fields. Scores were then averaged.
Abbreviations: COBRA, computationally optimized broadly reactive antigen; VLP, virus-like particle.
Figure 4.
Histopathologic analysis of H5N1-infected lung. Hematoxylin-eosin–stained sections of lungs from day 3 after infection: unvaccinated (A), WS/05 virus-like particle (VLP; B), computationally optimized broadly reactive antigen (COBRA) VLP (C), and unvaccinated, noninfected (D). Influenza in situ hybridization from day 1 after infection: unvaccinated (E), WS/05 VLP (F), and COBRA VLP (G).
Table 2.
Lung Involvement and Inflammation Scores
| Vaccine | Percentage of Lung Involvementa |
Bronchial Inflammation Scoreb |
Alveolar Inflammation Scoreb |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Day after infection | 1 | 3 | 5 | 1 | 3 | 5 | 1 | 3 | 5 |
| Mock | 0.38 (0–1) | 1.13 (0–2) | 1.25 (0–2) | 0.63 (0–1) | 0.75 (0–2) | 1.25 (0–2) | 0.63 (0–1) | 1.00 (0–2) | 1.25 (0–2) |
| WS/05 VLP | 0.75 (0–2) | 1.50 (0–3) | 0.88 (0–3) | 1.00 (1) | 1.42 (1–2) | 0.63 (0–2) | 1.00 (0–2) | 1.25 (0–2) | 1.00 (0–2) |
| COBRA VLP | 0.88 (0–2) | 0.50 (0–2) | 0.38 (0–2) | 1.13 (1–2) | 0.75 (0–2) | 0.88 (0–2) | 1.13 (0–2) | 0.67 (0–2) | 0.25 (0–1) |
Abbreviations: COBRA, computationally optimized broadly reactive antigen; VLP, virus-like particle.
a Tissue sections from the upper and lower left and right lung were evaluated for the percentage of the area demonstrating pneumonia. Data are mean percentage (range). 0, <10%; 1, 10%–24%; 2, 25%–50%; 3, >50%.
b Sections from the upper and lower left and right lung were evaluated for presence of bronchial inflammation and denudation and alveolar immune cell infiltration. Data are mean scores (range). 0, absent; 1, present; 2, abundant.
DISCUSSION
Outbreaks of highly pathogenic avian influenza due to the H5N1 subtype of influenza virus are of particular concern because of the high mortality rate (60% case-fatality rate) and novel subtype [33]. Several current H5N1 vaccine candidates elicit immune responses that are able to neutralize viruses within a homologous clade, but they lack cross-clade neutralization ability. Developing vaccines that are able to overcome these challenges of H5N1 antigenic diversity is a crucial step in pandemic preparedness. To our knowledge, we are the first to describe a nonhuman primate model for a clade 2 H5N1 influenza virus and to use this model to test the protective efficacy induced by the clade 2 COBRA VLP vaccine.
The COBRA vaccine strategy represents a novel method of sequence construction that features a layered building approach that is intended to capture the most common antigenic characteristics while avoiding the complication of differential sequence availability that can bias a consensus sequence to the most prevalent antigenic cluster. Avoiding this sampling bias is essential to generating a centralized vaccine that accurately represents the population of input sequences. A COBRA-designed HA phylogenetic analysis in the context of H5N1 human infections demonstrated that use of a layered consensus building approach can indeed overcome the challenges of sequence availability and results in a sequence that retains similarity to the input without localizing into any one antigenic cluster [26].
Why do COBRA-induced antibodies recognize a broader number of H5N1 isolates? First, COBRA HA antigens may have a combination of antibody epitopes that are not all present in any given wild-type sequence and therefore elicit a unique antibody profile. However, only 1 low-titer linear peptide was identified as having differential reactivity (amino acids 136–152) by ELISA (data not shown), and therefore, any putative epitopes are most likely conformational. Second, COBRA HA–elicited antisera did not readily recognize viruses from clade 0 and 4 by HAI assay (Figure 2). Viruses in these clades have conserved HA residues between them, but these residues are divergent from those of the other HA antigens in our panel at several positions reported to be localized in antigenic regions: 100, 140 (region B), 154 (region A), 171 (region B), and 228 (region D). It is possible that these particular residues could play key roles in evading neutralizing antibody responses. The COBRA HA used in this study was based on HA sequences from clade 2 viruses isolated from human infections [26]. The addition of HA sequences from divergent clades may expand the breadth of elicited antibodies to recognize viruses in other clades by HAI or MN assays. However, it is not known whether this expansion will reduce the reactivity to isolates within clade 2. In addition, antibodies elicited by COBRA HA immunogens may elicit higher-affinity antibodies because of the exposure of unique epitopes on the COBRA molecule that result in neutralization of a broad panel of primary virus isolates. How any of these results correlate with human H5N1 vaccination and subsequent protection from challenge is not known, and the COBRA HA immunogen will need to be tested in future clinical trials.
Following vaccination of nonhuman primates, the H5N1 COBRA HA expressed on the surface of a VLP elicited broadly reactive antibody (HAI) titers against not only clade 2 (Figure 2), but also across multiple clades of H5N1 (Figure 3). In general, experimental H5N1 vaccines elicit clade-specific HAI titers [34, 35]. Emergence of the novel H1N1 isolates in 2009 once again demonstrated that influenza viruses can reassort with avian and swine influenza viruses and result in human-transmissible viruses. Since the clade of an emerging, human-transmissible H5N1 isolate cannot be known in advance, a number of approaches have been used to generate vaccines targeting a broad number of H5N1 isolates/clades, including targeting the highly conserved ion channel protein (M2) and the nucleoprotein [36, 37]. However, these influenza proteins are not highly immunogenic. For seasonal influenza viruses, T cells directed against nucleoprotein and antibodies against NA can be effective at preventing viral budding and spread within a host and thereby reduce symptoms of disease, but only antibodies to HA can prevent infection. More recently, a vaccine approach that was based on the stalk region of the influenza virus conferred protection in mice against multiple lethal influenza viral challenges representing different subtypes [38]. This approach may have merit, since antibodies elicited during the recent 2009 H1N1 outbreak had broadly reactive neutralizing activity and cross-reacted against epitopes in the HA stalk and head domain of multiple influenza strains [39]. Furthermore, it is possible that vaccines targeting the HA stalk region could be improved by using a COBRA-based immunogen design. We demonstrated that antibodies elicited by the clade 2 COBRA HA recognized viruses from clades 1 and 7, as well as isolates representing various subclades of clades 2.1, 2.2, and 2.3 with a larger phylogenetic footprint than antibodies elicited by VLPs expressing the clade 2.2-specific HA from A/Whooper swan/Mongolia/244/2005, which had a more restricted footprint (Figure 5). Vaccination with 3 HA molecules representing clades 1, 2.1, and 2.3 elicited broadly reactive antibody responses to divergent H5N1 clades [35]. However, the COBRA HA used in this study elicited similar antibody breadth by use of a single HA immunogen. The addition of HA gene sequences from other clades may expand the breadth of elicited antibodies to more clades of H5N1.
Figure 5.
Footprint of hemagglutination inhibition (HAI) reactivity. The unrooted phylogenetic tree was inferred from hemagglutinin amino acid sequences derived from both vaccines and test antigens, using the maximum likelihood method. Phylogenetic analysis is the same as described in the legend for Figure 1. Numbers above each branch identify the clade/subclade of the respective cluster. The stars identify where the 2 vaccine antigens (computationally optimized broadly reactive antigen [COBRA] and WS/05) are located relative to the test antigens. The shading indicates the footprint of HAI reactivity for the COBRA vaccine (light gray) and WS/05 vaccine (dark gray).
Nonhuman primates offer some advantages for studying vaccine-induced immune responses, including the identification of immunological parameters outside of antibodies that may correlate with protection induced by experimental influenza vaccines [40–43]. We developed this clade 2 cynomolgus macaque model to study both H5N1-induced pathologic effects and vaccine efficacy in a nonhuman primate immune model. Grossly, unvaccinated nonhuman primates had lung pathologic findings as soon as day 3 after infection that were present until day 7. Similar results were detected in clade 1–infected nonhuman primates [40]. Hemorrhage and respiratory distress were associated with clade 2.2 (WS/05) H5N1 infection. Nonhuman primates vaccinated with either COBRA VLPs or WS/05 VLPs had few signs of disease and greatly reduced viral titers in the lungs upon challenge, but COBRA VLP–vaccinated nonhuman primates had little lung inflammation and fewer virally infected cells than WS/05 VLP vaccinated animals. Interestingly, the alveolar infection scores, the percentage of lung involvement, bronchial inflammation, and alveolar inflammation were higher at day 1 in the COBRA-vaccinated animals than in the WS/05 VLP–vaccinated nonhuman primates (Tables 1 and 2). We hypothesize that in COBRA VLP–vaccinated animals there is a brisk peak inflammatory response shortly after challenge that results in a quick decrease in virus. In contrast, immune response in WS/05 VLP–vaccinated animals is slower to react, and the duration of the response longer. The viral titers in the tracheal samples appear match these results. These results suggest that appropriately immunized monkeys mount an important early inflammatory response that quickly ablates infection. However, there were few clinical signs associated with infection with this strain of clade 2 H5N1, and therefore, differences in vaccine efficacy could only be determined by lower viral titers and reduced pathologic effects following necropsy and histopathological staining, which may limit the use of this model for vaccine studies.
In conclusion, this is the first report of a COBRA HA eliciting broadly reactive antibody responses across multiple clades of H5N1 that reduces inflammation and pathologic effects in nonhuman primates from a heterologous, highly pathogenic H5N1 virus challenge.
Notes
Acknowledgments. We thank Brianne Stein, for technical assistance; R. Sodnomdarjaa and the Mongolian State Central Veterinary Laboratory, for providing permission to use the A/Whooper Swan/Mongolia/244/2005 influenza virus; Richard Webby, for providing additional H5N1 viruses for assays; and Mark Lewis and Wendeline Wagner at Bioqual, for veterinary assistance for ABSL3+ H5N1 challenges.
Disclaimer. This work was supported, in part, under a grant with the Pennsylvania Department of Health. The department specifically disclaims responsibility for any analyses, interpretations or conclusions.
Financial support. This work was supported by the National Institutes of Health (NIH; training grant T32AI060525 to B. M. G.), the NIH National Institute of Allergy and Infectious Diseases (grant K24MH01717 to C. A. W. and grant U01AI077771 to T. M. R. and C. A. W.), and PATH Vaccine Solutions (collaborative research grant to T. M. R.).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Subbarao K, Klimov A, Katz J, et al. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science. 1998;279:393–6. doi: 10.1126/science.279.5349.393. [DOI] [PubMed] [Google Scholar]
- 2.Adams S, Sandrock C. Avian influenza: update. Med Princ Pract. 2010;19:421–32. doi: 10.1159/000320299. [DOI] [PubMed] [Google Scholar]
- 3.Gillim-Ross L, Subbarao K. Emerging respiratory viruses: challenges and vaccine strategies. Clin Microbiol Rev. 2006;19:614–36. doi: 10.1128/CMR.00005-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. Continuing progress towards a unified nomenclature system for the highly pathogenic H5N1 avian influenza viruses. 2009. cited 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takano R, Nidom CA, Kiso M, et al. Phylogenetic characterization of H5N1 avian influenza viruses isolated in Indonesia from 2003–2007. Virology. 2009;390:13–21. doi: 10.1016/j.virol.2009.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen M-W, Cheng T-JR, Huang Y, et al. A consensus hemagglutinin-based DNA vaccine that protects mice against divergent H5N1 influenza viruses. Proc Natl Acad Sci U S A. 2008;105:13538–43. doi: 10.1073/pnas.0806901105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laddy DJ, Yan J, Corbitt N, Kobasa D, Kobinger GP, Weiner DB. Immunogenicity of novel consensus-based DNA vaccines against avian influenza. Vaccine. 2007;25:2984–9. doi: 10.1016/j.vaccine.2007.01.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McBurney SP, Ross TM. Human immunodeficiency virus-like particles with consensus envelopes elicited broader cell-mediated peripheral and mucosal immune responses than polyvalent and monovalent Env vaccines. Vaccine. 2009;27:4337–49. doi: 10.1016/j.vaccine.2009.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weaver EA, Lu Z, Camacho ZT, et al. Cross-subtype T-cell immune responses induced by a human immunodeficiency virus type 1 group m consensus env immunogen. J Virol. 2006;80:6745–56. doi: 10.1128/JVI.02484-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yan J, Yoon H, Kumar S, et al. Enhanced cellular immune responses elicited by an engineered HIV-1 subtype B consensus-based envelope DNA vaccine. Mol Ther. 2007;15:411–21. doi: 10.1038/sj.mt.6300036. [DOI] [PubMed] [Google Scholar]
- 11.Bright RA, Carter DM, Daniluk S, et al. Influenza virus-like particles elicit broader immune responses than whole virion inactivated influenza virus or recombinant hemagglutinin. Vaccine. 2007;25:3871–8. doi: 10.1016/j.vaccine.2007.01.106. [DOI] [PubMed] [Google Scholar]
- 12.Hamouda T, Sutcliffe JA, Ciotti S, Baker JR., Jr. Intranasal immunization of ferrets with commercial trivalent influenza vaccines formulated in a nanoemulsion-based adjuvant. Clin Vaccine Immunol. 2011;18:1167–75. doi: 10.1128/CVI.00035-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lipatov AS, Hoffmann E, Salomon R, Yen HL, Webster RG. Cross-protectiveness and immunogenicity of influenza A/Duck/Singapore/3/97(H5) vaccines against infection with A/Vietnam/1203/04(H5N1) virus in ferrets. J Infect Dis. 2006;194:1040–3. doi: 10.1086/507709. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell JA, Green TD, Bright RA, Ross TM. Induction of heterosubtypic immunity to influenza A virus using a DNA vaccine expressing hemagglutinin-C3d fusion proteins. Vaccine. 2003;21:902–14. doi: 10.1016/s0264-410x(02)00539-x. [DOI] [PubMed] [Google Scholar]
- 15.Pearce MB, Belser JA, Houser KV, Katz JM, Tumpey TM. Efficacy of seasonal live attenuated influenza vaccine against virus replication and transmission of a pandemic 2009 H1N1 virus in ferrets. Vaccine. 2011;29:2887–94. doi: 10.1016/j.vaccine.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Pushko P, Pearce MB, Ahmad A, et al. Influenza virus-like particle can accommodate multiple subtypes of hemagglutinin and protect from multiple influenza types and subtypes. Vaccine. 2011;29:5911–8. doi: 10.1016/j.vaccine.2011.06.068. [DOI] [PubMed] [Google Scholar]
- 17.Bright RA, Carter DM, Crevar CJ. Cross-clade protective immune responses to influenza viruses with H5N1 HA and NA elicited by an influenza virus-like particle. PLoS One. 2008;3:e1501. doi: 10.1371/journal.pone.0001501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Govorkova EA, Webby RJ, Humberd J, Seiler JP, Webster RG. Immunization with reverse-genetics-produced H5N1 influenza vaccine protects ferrets against homologous and heterologous challenge. J Infect Dis. 2006;194:159–67. doi: 10.1086/505225. [DOI] [PubMed] [Google Scholar]
- 19.Ninomiya A, Imai M, Tashiro M, Odagiri T. Inactivated influenza H5N1 whole-virus vaccine with aluminum adjuvant induces homologous and heterologous protective immunities against lethal challenge with highly pathogenic H5N1 avian influenza viruses in a mouse model. Vaccine. 2007;25:3554–60. doi: 10.1016/j.vaccine.2007.01.083. [DOI] [PubMed] [Google Scholar]
- 20.Rimmelzwaan GF, Kuiken T, van Amerongen G, Bestebroer TM, Fouchier RA, Osterhaus AD. Pathogenesis of influenza A (H5N1) virus infection in a primate model. J Virol. 2001;75:6687–91. doi: 10.1128/JVI.75.14.6687-6691.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kobasa D, Jones SM, Shinya K, et al. Aberrant innate immune response in lethal infection of macaques with the 1918 influenza virus. Nature. 2007;445:319–23. doi: 10.1038/nature05495. [DOI] [PubMed] [Google Scholar]
- 22.Ducatez MF, Olinger CM, Owoade AA, et al. Molecular and antigenic evolution and geographical spread of H5N1 highly pathogenic avian influenza viruses in western Africa. J Gen Virol. 2007;88:2297–306. doi: 10.1099/vir.0.82939-0. [DOI] [PubMed] [Google Scholar]
- 23.Kiss I, Gyarmati P, Zohari S, et al. Molecular characterization of highly pathogenic H5N1 avian influenza viruses isolated in Sweden in 2006. Virol J. 2008;5:113. doi: 10.1186/1743-422X-5-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salzberg SL, Kingsford C, Cattoli G, et al. Genome analysis linking recent European and African influenza (H5N1) viruses. Emerg Infect Dis. 2007;13:713–8. doi: 10.3201/eid1305.070013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Starick E, Beer M, Hoffmann B, et al. Phylogenetic analyses of highly pathogenic avian influenza virus isolates from Germany in 2006 and 2007 suggest at least three separate introductions of H5N1 virus. Vet Microbiol. 2008;128:243–52. doi: 10.1016/j.vetmic.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 26.Giles BM, Ross TM. Development of a computationally optimized broadly reactive (COBRA) hemagglutinin for elicitation of protective antibodies against multiple clades of H5N1. Vaccine. 2011;29:3043–54. doi: 10.1016/j.vaccine.2011.01.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuiken T, Rimmelzwaan GF, Van Amerongen G, Osterhaus AD, et al. Pathology of human influenza A (H5N1) virus infection in cynomolgus macaques (Macaca fascicularis) Vet Pathol. 2003;40:304–10. doi: 10.1354/vp.40-3-304. [DOI] [PubMed] [Google Scholar]
- 28.Rimmelzwaan GF, Kuiken T, van Amerongen G, Bestebroer TM, Fouchier RA, Osterhaus AD. A primate model to study the pathogenesis of influenza A (H5N1) virus infection. Avian Dis. 2003;47:931–3. doi: 10.1637/0005-2086-47.s3.931. [DOI] [PubMed] [Google Scholar]
- 29.Askonas B, McMichael A, Webster R. The immune response to influenza viruses and the problem of protection against infection. In: Beare AS, editor. Basic and applied influenza research. CRC Press; 1982. pp. 159–88. [Google Scholar]
- 30.Rowe T, Abernathy RA, Hu-Primmer J, et al. Detection of antibody to avian influenza A (H5N1) virus in human serum by using a combination of serologic assays. J Clin Microbiol. 1999;37:937–43. doi: 10.1128/jcm.37.4.937-943.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bissel SJ, Wang G, Ghosh M, et al. Macrophages relate presynaptic and postsynaptic damage in simian immunodeficiency virus encephalitis. Am J Pathol. 2002;160:927–41. doi: 10.1016/S0002-9440(10)64915-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fallert B, Reinhart T. Improved detection of simian immunodeficiency virus RNA by in situ hybridization in fixed tissue sections: combined effects of temperatures for tissue fixation and probe hybridization. J Virol Methods. 2002;99:23–32. doi: 10.1016/s0166-0934(01)00378-0. [DOI] [PubMed] [Google Scholar]
- 33.Gruber PC, Gomersall CD, Joynt GM. Avian influenza (H5N1): implications for intensive care. Intensive Care Med. 2006;32:823–9. doi: 10.1007/s00134-006-0148-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ducatez MF, Bahl J, Griffin Y, et al. Feasibility of reconstructed ancestral H5N1 influenza viruses for cross-clade protective vaccine development. Proc Natl Acad Sci U S A. 2011;108:349–54. doi: 10.1073/pnas.1012457108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prabakaran M, He F, Meng T, et al. Neutralizing epitopes of influenza virus hemagglutinin: target for the development of a universal vaccine against H5N1 lineages. J Virol. 2010;84:11822–30. doi: 10.1128/JVI.00891-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen G, Subbarao K. Attacking the flu: neutralizing antibodies may lead to universal vaccine. Nat Med. 2009;15:1251–2. doi: 10.1038/nm1109-1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu F, Huang JH, Yuan XY, Huang WS, Chen YH. Characterization of immunity induced by M2e of influenza virus. Vaccine. 2007;25:8868–73. doi: 10.1016/j.vaccine.2007.09.056. [DOI] [PubMed] [Google Scholar]
- 38.Steel J, Lowen AC, Wang TT, et al. Influenza virus vaccine based on the conserved hemagglutinin stalk domain. MBio. 2010;1:e00018–10. doi: 10.1128/mBio.00018-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wrammert J, Koutsonanos D, Li GM, et al. Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J Exp Med. 2011;208:181–93. doi: 10.1084/jem.20101352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baskin CR, Bielefeldt-Ohmann H, Tumpey TM, et al. Early and sustained innate immune response defines pathology and death in nonhuman primates infected by highly pathogenic influenza virus. Proc Natl Acad Sci U S A. 2009;106:3455–60. doi: 10.1073/pnas.0813234106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cilloniz C, Shinya K, Peng X, et al. Lethal influenza virus infection in macaques is associated with early dysregulation of inflammatory related genes. PLoS Pathog. 2009;5:e1000604. doi: 10.1371/journal.ppat.1000604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fan S, Gao Y, Shinya K, et al. Immunogenicity and protective efficacy of a live attenuated H5N1 vaccine in nonhuman primates. PLoS Pathog. 2009;5:e1000409. doi: 10.1371/journal.ppat.1000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Laddy DJ, Yan J, Khan AS, et al. Electroporation of synthetic DNA antigens offers protection in nonhuman primates challenged with highly pathogenic avian influenza virus. J Virol. 2009;83:4624–30. doi: 10.1128/JVI.02335-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dereeper A, Guignon V, Blanc G, et al. Phylogeny.fr: robust phylogenetic analysis for the non-specialist. Nucleic Acids Res. 2008;36:W465–9. doi: 10.1093/nar/gkn180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bao Y, Bolotov P, Dernovoy D, et al. The influenza virus resource at the National Center for Biotechnology Information. J Virol. 2008;82:596–601. doi: 10.1128/JVI.02005-07. [DOI] [PMC free article] [PubMed] [Google Scholar]