Abstract
Introduction
Recent research suggests that men who have sex with men (MSM) experience intimate partner violence (IPV) at significantly higher rates than heterosexual men. Few studies, however, have investigated implications of heterosexist social pressures – namely, homophobic discrimination, internalized homophobia, and heterosexism – on risk for IPV among MSM, and no previous studies have examined cross-national variations in the relationship between IPV and social pressure. This paper examines reporting of IPV and associations with social pressure among a sample of internet-recruited MSM in the United States (U.S.), Canada, Australia, the United Kingdom, South Africa, and Brazil.
Methods
We recruited internet-using MSM from 6 countries through selective banner advertisements placed on Facebook. Eligibility criteria were men age over 18 reporting sex with a man in the past year. Of the 2,771 eligible respondents, 2,368 had complete data and were included in the analysis. Three outcomes were examined: reporting recent experience of physical violence, sexual violence, and recent perpetration of physical violence. The analysis focused on associations between reporting of IPV and experiences of homophobic discrimination, internalized homophobia, and heteronormativity.
Results
Reporting of experiencing physical IPV ranged from 5.75% in the U.S. to 11.75% in South Africa, while experiencing sexual violence was less commonly reported and ranged from 2.54% in Australia to 4.52% in the U.S. Perpetration of physical violence ranged from 2.47% in the U.S. to 5.76% in South Africa. Experiences of homophobic discrimination, internalized homophobia, and heteronormativity were found to increase odds of reporting IPV in all countries.
Conclusion
There has been little data on IPV among MSM, particularly MSM living in low- and middle-income countries. Despite the lack of consensus in demographic correlates of violence reporting, heterosexist social pressures were found to significantly increase odds of reporting IPV in all countries. These findings show the universality of violence reporting among MSM across countries, and highlight the unique role of heteronormativity as a risk factor for violence reporting among MSM. The results demonstrate that using internet-based surveys to reach MSM is feasible for certain areas, although modified efforts may be required to reach diverse samples of MSM.
INTRODUCTION
Recent studies suggest that men who have sex with men (MSM) experience intimate partner violence (IPV) at rates that are substantially higher than those experienced by men who do not have sex with men, rates that are comparable or higher to those among heterosexual women, and that MSM are uniquely at risk for experiencing IPV over their lifetimes.1–3 Although the majority of data on IPV among MSM are drawn from cross-sectional samples of United States (U.S.) MSM, and existing studies vary widely in their definitions of violence, the existing data do suggest that approximately 25–50% of MSM report experiencing physical IPV over their lifetimes, and 12–30% report experiencing sexual IPV.1,2,4–6 Fewer studies have measured perpetration of IPV among MSM, but existing estimates range from 12–36%.7 There has been a lack of attention regarding rates of IPV among non-U.S. MSM, although recently, high rates of IPV have been documented among MSM in Canada (28% experience of physical IPV) and among South African MSM (8% experience of physical IPV and 4.5% experience of sexual IPV).8,9
Historically, the preponderance of evidence indicates that IPV, experienced and/or perpetrated, is correlated both with acute physical effects (e.g., trauma), sustained physical effects (e.g., substance abuse, sexually transmitted infections), and adverse mental health outcomes (e.g., suicidal ideation, depression, chronic mental illness).10–12 These associations have been found in diverse settings and populations, and although such evidence is primarily drawn from heterosexual populations, similar associations are beginning to be documented among MSM.13–17 Of particular importance to MSM is emergent evidence demonstrating a link between IPV, sexual risk-taking, and risk for Human Immunodeficiency Virus (HIV) infection, as MSM worldwide continue to be disproportionately affected by the HIV epidemic.4,8,14,16,18–23
While several of the aforementioned studies have begun to examine the influence of IPV on MSM's mental and physical health, few published studies have examined the influence of sources of negative social stress, for example, internalized homophobia, experiences of homophobic discrimination, and experience of heteronormativity, as influencing risk for IPV itself, despite emerging evidence that such sources of social stress interact with known syndemics of partner violence, poor mental health, substance abuse, and sexual risk-taking among MSM.7,24–30 The confluence of all of these sources has been described by Meyer31 as the theory of Minority Stress, which postulates that the social stress experienced by persons of minority status is (a) unique to their minority status and (b) additive in nature. For example, the vulnerability experienced by MSM experiencing partner violence would be exacerbated by the stress experienced by MSM from social stigmatization and legal persecution, creating syndemic processes. However, the specific nature of these syndemics may vary across different regions and social contexts, given the wide variation in both the legality and the social acceptance of same-sex sexual behavior worldwide.22,32–34 Thus, while IPV and adverse mental and physical health outcomes exist syndemically in MSM, the characteristics of these syndemics may be specific to different geographic locations or cultural settings.35–37
This study addresses gaps in the literature in several key ways. We report rates of IPV among MSM, including experiencing and perpetrating both physical and sexual violence, using data drawn from online surveys conducted in 6 countries, including one middle-income country (Brazil) and one low-income country (South Africa). For 3 of these countries (UK, Australia, and Brazil), the authors found no previous studies that report the prevalence of IPV among MSM. Critically, the authors also found no studies that compare the varying influences of sources of social stress, including homophobia and heteronormative social pressures, on the experience of IPV among MSM across multiple countries.
METHODS
We drew the data for this study from an online survey. Study participants were recruited through advertisements on social networking site Facebook in the U.S., Canada, Australia, United Kingdom, Republic of South Africa (RSA), Brazil, Nigeria, Kenya, and India over a 5-14 day period in each country. Advertisements were shown to male Facebook users over 18 years of age who indicated an interest in men in their user profiles. Clicking the advertisement led potential participants to information on the survey, after which informed consent was obtained and participants were directed to the survey. Participants were eligible for survey completion if they reported being born male, being over 18 years of age, and having had sex with a man in the past year. The surveys were conducted in English in all countries, with the exception of the Brazilian survey, which was administered in Portuguese. The response to the survey was insufficient for analysis in Nigeria (n=11), Kenya (n=22), and India (n=80). Of the combined 2,771 responses to the survey in the six countries with sufficient response, 2,368 men had complete data for all covariates of interest and were included in the analysis.
We collected demographic data for age, race, and education level. Survey participants were asked about their sexual orientation, and we included only men who self-identified as homosexual/gay in the analysis. We classified HIV status as negative for men who reported negative HIV status and positive/unknown for men who reported positive HIV status, had never been tested for HIV, had received an indeterminate/inconclusive result, had never received the results of their last test, or preferred not to answer. Participants reported drug use in the last 12 months, and were categorized as having any drug uses versus none. We defined behavioral bisexuality as having ever had sex with a woman.
We assessed internalized homophobia using a 20-item subset of the Gay Identity Scale, a validated scale that measures an individual's acceptance of his homosexual thoughts, feelings, and behaviors.38 From respondents' answers, we created an index scale by assigning positive point values to responses agreeing with internally homophobic sentiments, negative point values to responses affirming gay pride, and no points to any neutral response. Forty points were added to each index score to shift the range from −40 to 40 to zero to 80, with increasing index scores correlated with decreasing pride and lowered acceptance of one's homosexual thoughts, feelings, and behaviors. We quantified experiences of homophobic discrimination by creating an index scale of responses to 11 types of homophobic decimation that have been previously shown to correlate to adverse mental health outcomes.39 Any affirmative response to an experience of discrimination (e.g., “Due to your sexual orientation were you ever made fun of as a child?”), resulted in one index point, creating a hypothetical range of zero to 11, with a higher score signifying increasing experiences of homophobic discrimination. Drawing from previous qualitative work with U.S. and South African MSM, we quantified experiencing heteronormative social pressure by creating an index scale of 4 questions on the degree to which respondents felt pressure to hide their sexuality, get married, have children, and have sex with women. We summed participants' reported responses to create an index scale ranging from 4 to 20, with a higher score representing greater experience of heteronormativity.
Finally, participants were asked about their experience of or perpetration of IPV, both physical and sexual, with any partner in the previous 12 months. Using WHO definitions of IPV, men were asked if they had been physically hurt by a partner (i.e., “In the last 12 months have any of your partners ever tried to hurt you, this includes pushing, holding you down, hitting you with his fist, kicking, attempting to strangle, attacking with a knife, gun or other weapon?”), and if a partner had forced him to have sex against his will (i.e., “In the last 12 months have any of your partners ever used physical force or verbal threats to force you to have sex when you did not want to?”). We used the same definitions of violence to assess if participants had perpetrated these same acts of physical and sexual violence against a partner in the past year.
We analyzed the data using STATA 12. We categorized age into discrete groups of 18–24, 25–34, and >34 in all countries but Brazil, in which age was dichotomized as 18–24 and >24. Race was defined differently in each country: White or Other (U.S., UK, Canada, Australia); White African, Black African, or Colored/Other (South Africa); and White, Mixed, or Black/Other (Brazil). We categorized level of education as having completed ≤12 years of education or having completed >12 years of education. In each country, we created 3 logistic regression models for 3 outcomes of interest: experiencing physical IPV, experiencing sexual IPV, and perpetrating physical IPV. Due to low reported prevalence of reporting perpetration of sexual IPV in all countries, perpetrating sexual IPV could not be modeled as an outcome. All models in all countries controlled for age, level of education, race/ancestry, HIV status, drug use, behavioral bisexuality, with the key covariates of interest being internalized homophobia, experiences of homophobic discrimination, and experiences of heteronormativity.
RESULTS
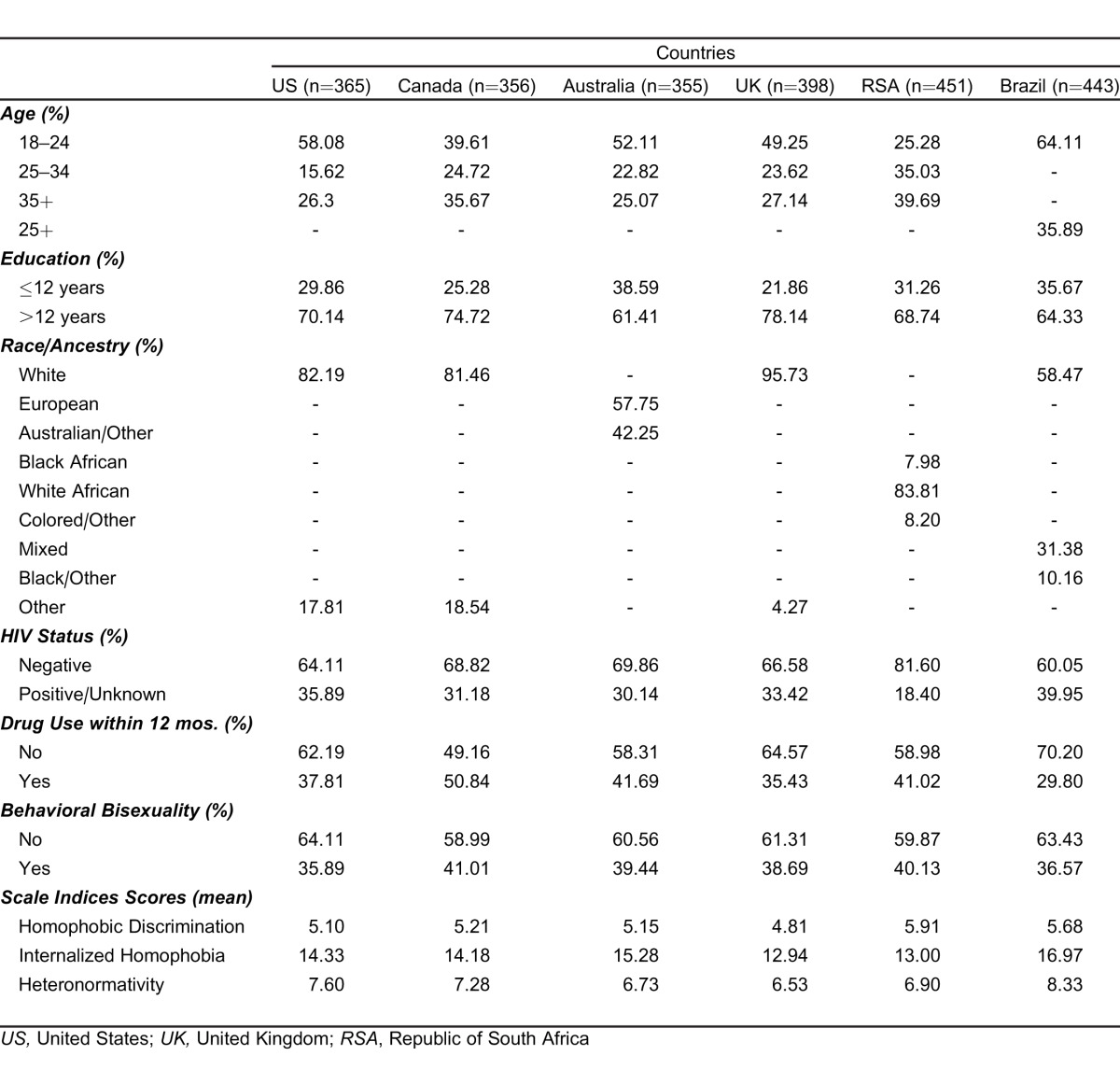
Demographic characteristics of the sample and mean index scores for homophobic discrimination, internalized homophobia, and heteronormativity are summarized by country in Table 1. In all countries, the sample was predominantly young (18–24), educated (>12 years of education), and of White/European race or ancestry. Additionally, the majority of the sample reported negative HIV status, no drug use in the past 12 months (excepting Canada, where 50.84% reported recent drug use), and no history of behavioral bisexuality. We observed some variation in reported experiences of homophobia and heteronormativity. Mean number of homophobic discrimination episodes ranged from 4.81 (SD: 0.11) in the UK to 5.91(SD: 0.11) in RSA. Internalized homophobia mean scores ranged from 12.94 (SD: 0.54) in the UK to16.97 (SD: 0.55) in Brazil, and heteronormativity mean scores ranged from 6.53 (SD: 0.17) in the UK to 8.33 (SD: 0.21) in Brazil.
Table 1.
Background demographic characteristics and mean index scale score by country of 2,368 internet-recruited men who have sex with men in 6 countries.
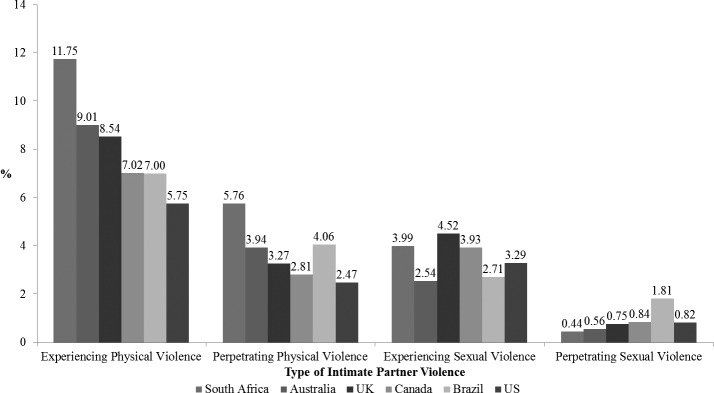
The prevalence of IPV reporting in each country is shown in the Figure, and the variation in reporting of IPV across covariates is reported in Table 2. In all countries, the most commonly reported form of IPV was experiencing physical violence, with a range of 5.75% of respondents in the U.S. to 11.75% of respondents in South Africa. Reported experience of sexual violence was somewhat lower, with prevalence ranging from 2.54% in Australia to 4.52% in the U.S. Fewer men reported perpetrating violence, with 2.47% of U.S. men (lowest) and 5.76% of South African men (highest) reporting perpetrating physical violence against a partner in the past year. Very few respondents (less than 2% in all countries) reported perpetration of sexual violence.
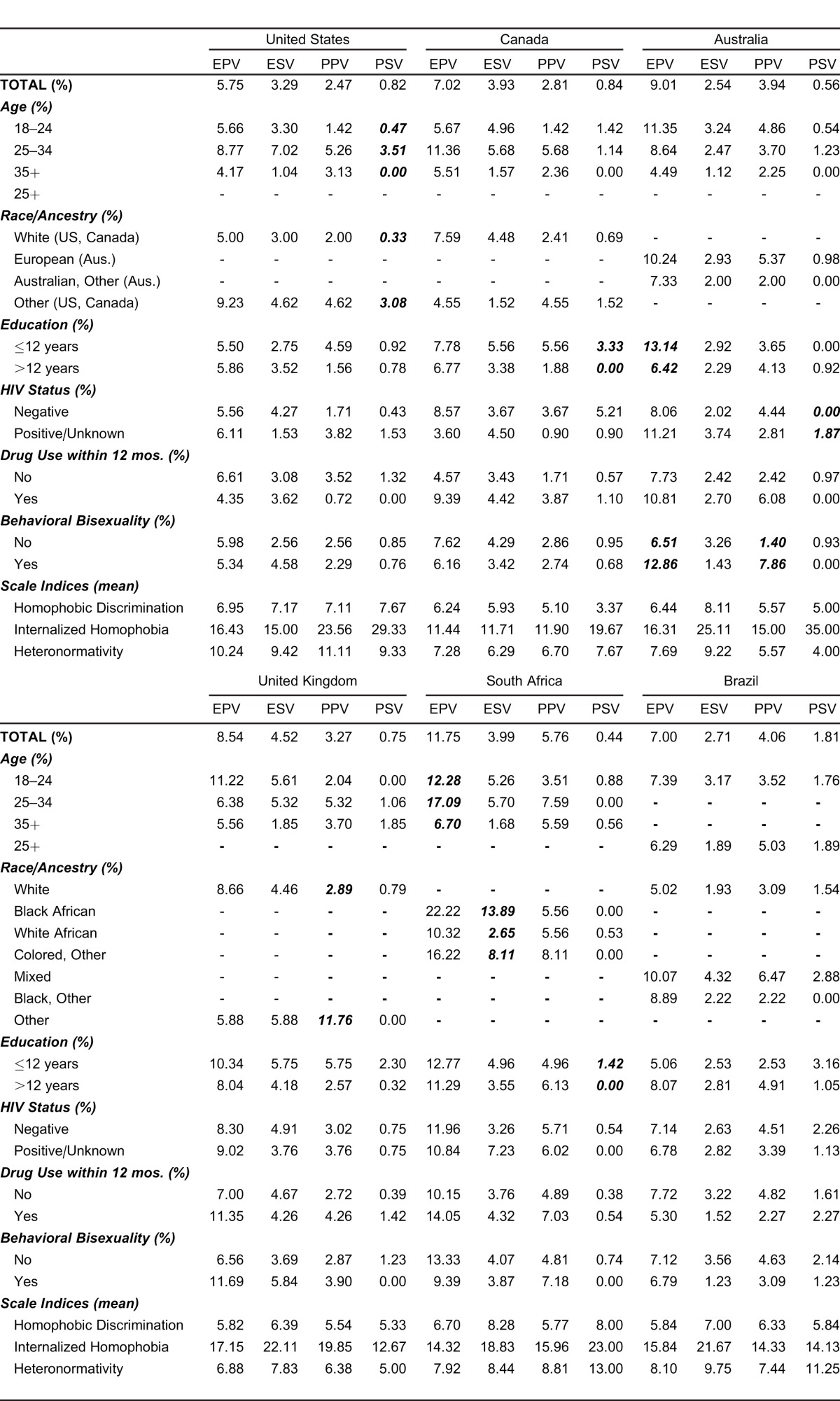
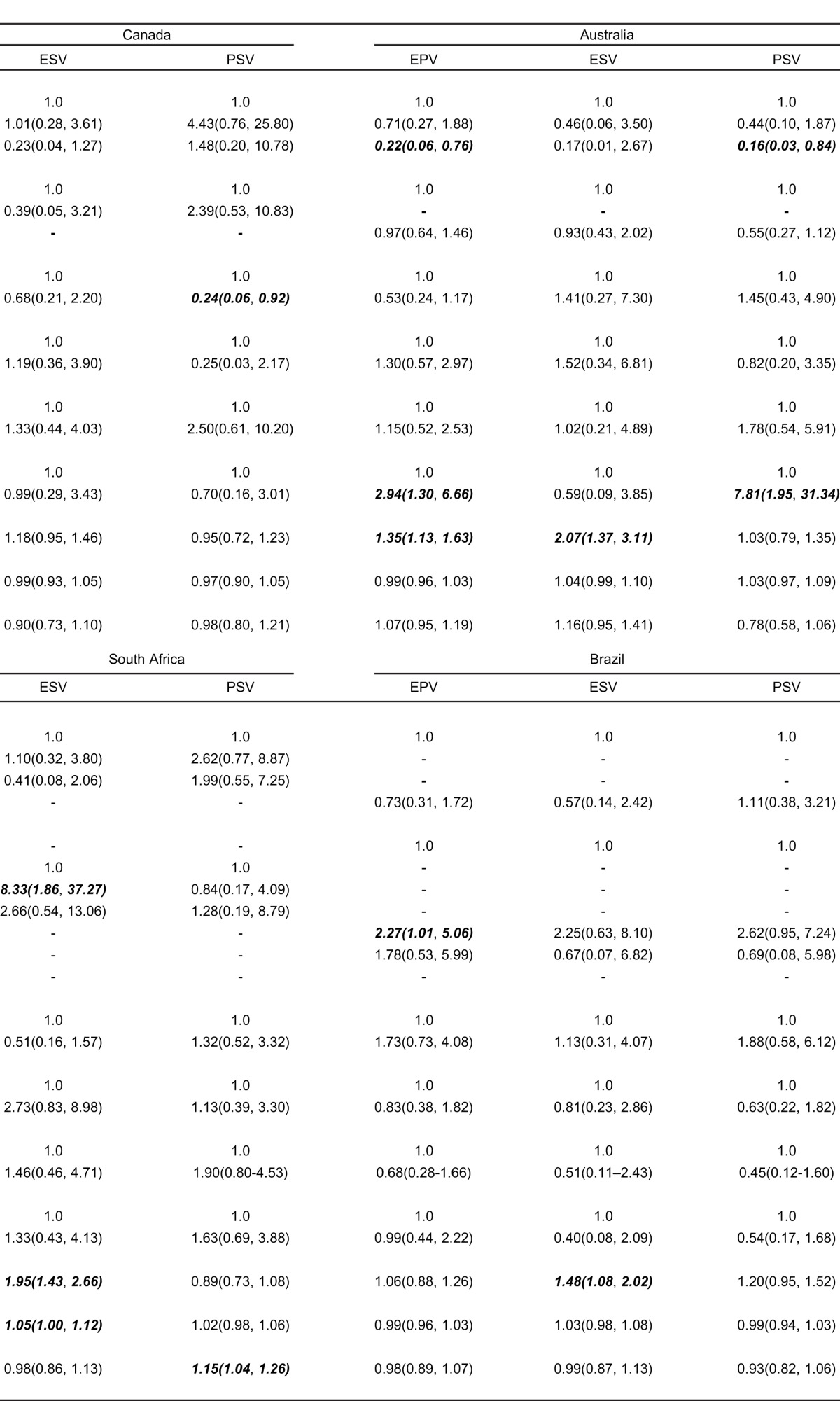
Table 2.
Prevalence of reporting of experience of physical violence (EPV), experience of sexual violence (ESV), perpetration of physical violence (PPV), perpetration of sexual violence (PSV), mean scale index scores, and chi-square test results by covariate strata in six countries. Significant difference across strata at α=0.05 are denoted in bold italics. NB: - denotes a non-applicable stratum.
Violence reporting did not vary significantly by most covariates, and varied differently within each country. Younger men (ages 18–24) in South Africa, less educated men in Australia, and men with a history of behavioral bisexuality in Australia more frequently reported experiencing physical IPV. Reported experience of sexual IPV varied significantly only by race in South Africa, with Black and Colored/Other South Africans reporting significantly more experience of sexual IPV compared to White South Africans (13.89% and 8.11% compared to 2.65%). Non-white British men reported significantly more perpetration of physical violence when compared to white British men (3.0% versus 0.33%), as did Australians with a history of behavioral bisexuality when compared to Australian men without a history of behavioral bisexuality (7.85% versus 1.40%). Lastly, reporting perpetration of sexual violence varied significantly by age and race in the U.S., level of education in Canada and RSA, and HIV status in Australia. Neither drug use, internalized homophobia, experiences of homophobic discrimination, nor heteronormativity varied significantly in any country for any outcome.
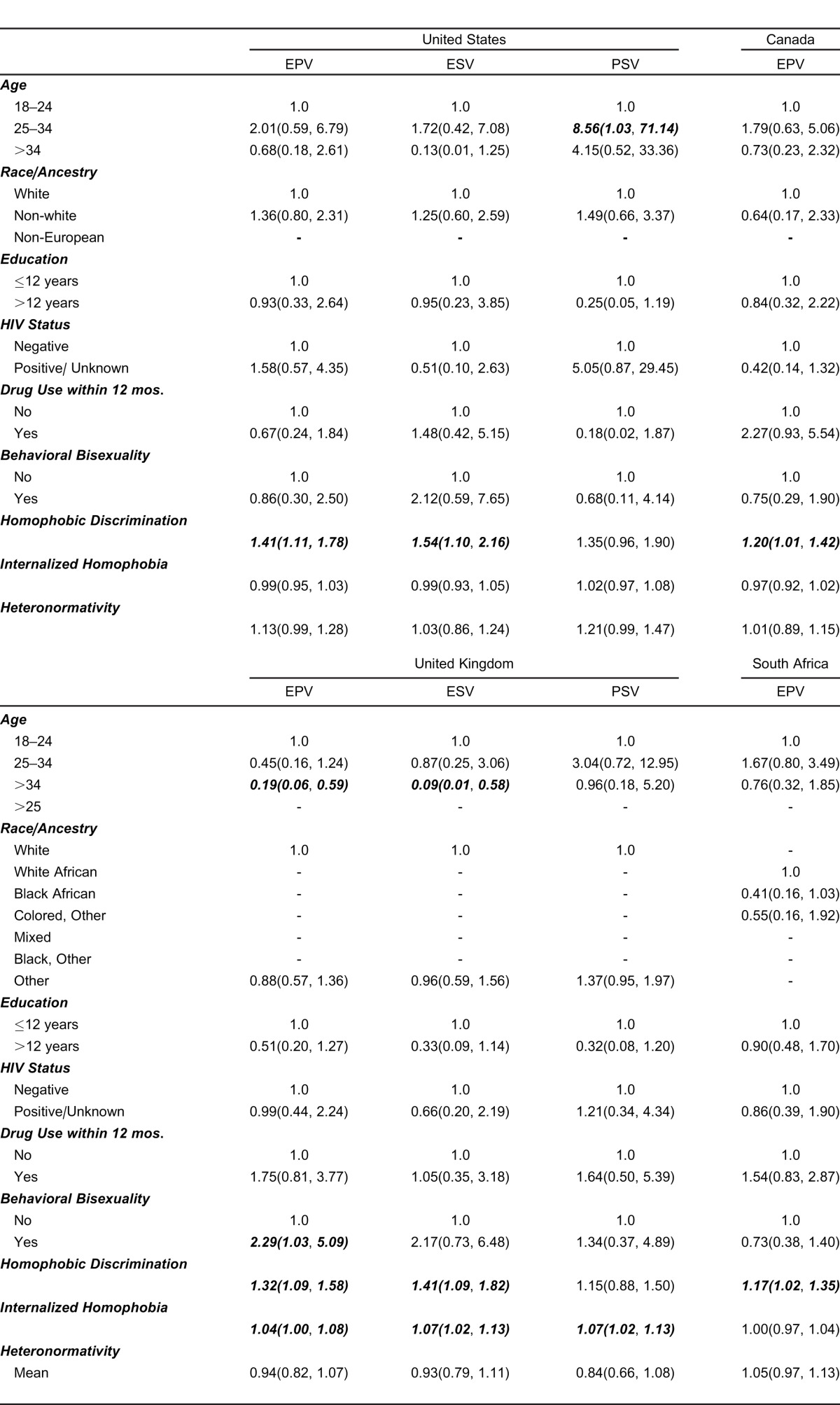
Results from the logistic regression modeling are summarized in Table 3. Across all 6 countries, there was no consistency in significant associations between IPV and demographic variables. For example, race modified odds of reporting violence only in South Africa and Brazil: Black African men were more likely to report experiencing sexual violence when compared to White men (OR: 8.33, 95% CI: 1.86, 37.27) in South Africa, and Mixed men were more likely to report experiencing physical violence in Brazil when compared to White men (OR: 2.27, 95% CI: 1.01, 5.06). A history of behavioral bisexuality was found to significantly increase odds of reporting experiencing physical violence in the UK (OR: 2.29, 95% CI: 1.03, 5.09) and Australia (OR: 2.94, 95% CI: 1.30, 6.66) and odds of reporting perpetrating physical violence in Australia (OR: 7.81, 95% CI: 1.95, 31.34).
Table 3.
Regression models for reporting experience of physical violence (EPV), experience of sexual violence (ESV), and perpetration of sexual violence (PSV) among a sample of internet-recruited men who have sex with men in 6 countries. Significant difference across strata at α=0.05 are denoted in bold italics. NB: - denotes a non-applicable stratum.
Although few demographic characteristics significantly modified odds for reporting most forms of violence, both experiences of homophobia and internalized homophobia were found to universally increase odds of reporting IPV. Men reporting increased experiences of homophobic discrimination were significantly more likely to report experiencing physical IPV in 5 of 6 countries, with odd ratios ranging from 1.17 (95% CI: 1.03, 1.35) in South Africa to 1.41 (95% CI: 1.11, 1.78) in the U.S. Similarly, men who reported more experiences of homophobic discrimination were significantly more likely to report experiencing sexual IPV in 5 of 6 countries. For example, UK MSM who reported increasing episodes of homophobic discrimination were 41% (95% CI: 9%, 82%) more likely to report experiencing sexual IPV, and MSM in Australia had odds of experiencing sexual IPV that were 2.07 (95% CI: 1.37, 3.11) times those of Australian men who reported fewer experiences of homophobic discrimination. Men who reported increased amounts of internalized homophobia were found to have increased odds of reporting IPV in South Africa and in the UK, where reporting more internalized homophobia was associated with increased odds of reporting experiencing physical violence (UK, OR: 1.04, 95% CI: 1.00, 1.08), experiencing sexual violence (UK, OR: 1.07, 95% CI: 1.02, 1.13; South Africa, OR: 1.05, 95% CI: 1.00, 1.12), and perpetrating sexual violence (UK, OR: 1.07, 95% CI: 1.02, 1.13).
DISCUSSION
This analysis presents several findings previously not reported in the literature, and provides strong evidence for the influence of heteronormative social pressure on reporting of intimate partner violence among MSM. First, this study presents evidence that using internet-based social networking sites to recruit MSM, a traditionally difficult-to-reach population, is feasible in several settings, but currently less feasible in others. This finding calls attention to added challenges of reaching MSM living in communities where homosexual behavior remains illegal and/or stigmatized, and suggests that internet-based methods in and of themselves may be currently insufficient for these efforts in those places, a finding that has previously been documented for MSM in South Africa.9
Second, this study presents rates of IPV reporting among MSM that have yet to be documented in the literature, namely in the UK, Brazil, and Australia. Perpetration rates of IPV among MSM have also yet to be documented in the majority of these countries. From these data, it is clear that IPV, both physical and sexual, occurs in male-male relationships worldwide. Furthermore, the patterns of violence reporting are similar in each country, and mirror previous studies of partner violence among both heterosexual and MSM populations; that is, in all countries, experience of physical violence was most commonly reported while perpetration of sexual violence was least commonly reported. 9,20,40 Of primary importance in this study is the finding that the demographics correlates that are commonly viewed as “classic” risk factors for partner violence, such as low levels of education and drug use, do not uniformly affect reporting of violence among MSM cross-nationally. Context is critical. For example, while older age was found to significantly decrease odds of reporting violence in the U.S., Australia, and the UK, non-White race was instead the more important demographic risk factor in South Africa and Brazil for increasing odds of reporting IPV. This finding highlights the importance of understanding the unique history and culture of a given community; for example, the influence of race on partner violence in South Africa, with its apartheid past, may be different from the influence of race in a more racially homogenous country, such as Canada. This suggests that interventions targeting IPV among MSM must take said context into account, and that interventions developed in one area or country may need modification before they can be used in other locations. Additional research is needed to clarify these demographic risk factors in each setting such that practitioners may begin to screen for IPV among MSM.
Third, despite the lack of consistency observed between demographic correlates and violence across the 6 countries of interest, heteronormative social pressures were found to significantly increase odds of reporting IPV in all countries. That is, while the influence of different manifestations of heterosexist social pressure did vary across countries, the experience of any form of heterosexism consistently emerged from the data as a risk factor for reporting of IPV in all countries. This finding suggests that MSM who more explicitly report experiencing heteronormative pressures may be at increased risk for IPV, regardless of their geographic location, age, race, or education, and indicates that there may be associations between violence and homophobia that are necessarily unique to MSM. One possible way that homophobia and heterosexism may increase risk for IPV among MSM would be through larger processes of social stigmatization and marginalization, as posited by Minority Stress theory. For example, a lack of formal recognition of gay partnerships through civil unions or marriage may position MSM at a primarily increased risk of experiencing violence from their partners due to the lack of safeguards against IPV normally afforded married or otherwise legally recognized couples. Alternatively, there may be direct effects of heterosexist social pressure on MSM. For example, MSM who feel that they must hide their sexuality may feel less able negotiate un-coerced sex with male partners, or MSM with higher levels of internalized homophobia may report higher levels of sexual violence and sexual coercion owing to their reported lack of acceptance of their homosexual thoughts and behaviors. MSM experiencing violence may also experience a “double closet” of learned social shame of homosexual behaviors and shame of victimhood, making MSM less likely to seek out IPV support. The specific pathways through which homophobic social pressures influence these risks among MSM should be clarified through future research.
LIMITATIONS
There are several limitations to this study, the majority of which arise from its internet-based sampling. In all countries, the survey tool reached only MSM with access to the internet who were registered users of Facebook and who listed their interest in men in their profiles. Using such methods will necessarily oversample affluent MSM who are more open about the fact that they have sex with men, leading to possible underreporting of internalized homophobia and heteronormativity. Furthermore, this analysis includes only self-identified gay men to the exclusion of non-gay-identifying MSM, as this study seeks to examine the unique role that anti-gay sentiment and heterosexism has in the lives of gay-identified MSM. Reporting of all forms of intimate partner violence was not limited to male partners; although MSM may be reporting violence experienced and/or perpetrated by their female partners, such findings are still of importance. Additionally, the cross-sectional nature of the survey means that all data are correlative and causality cannot be assessed, that is; it remains unknown whether experiencing heterosexist social pressures increases risk for violence or vice versa. Despite these limitations, use of an internet survey is appropriate insofar as it reaches traditionally hard-to-reach populations, and due to the anonymous nature of the internet, social desirability bias, which would lessen reporting of violence, is mitigated.
CONCLUSION
This study demonstrates that, cross-nationally, multiple forms of IPV are prevalent among MSM. Furthermore, these heretofore undocumented findings suggest that regardless of the varied demographic correlates of IPV in different contexts, heteronormative social pressure universally increases odds of reporting of IPV among MSM. An additional finding is that online surveys are able to reach MSM in many different countries and contexts, although modified efforts may be required to reach less affluent, less educated, and non-White MSM via the internet. Given the emerging body of literature that links experience of partner violence among MSM to several comorbidities, particularly risk for HIV infection, these findings elucidate the pressing need for MSM-focused services in all contexts, including non-Western contexts, to address partner violence as it occurs in male-male relationships. Both future research and future public health interventions shoulder consider and address the effect of heterosexist social pressures on the lives of MSM in all contexts, particular as they influence intimate partner violence.
Figure.
Reporting of 4 types of intimate partner violence (experiencing physical violence, perpetrating physical violence, experiencing sexual violence, and perpetrating sexual violence) in the past year among gay men in 6 countries.
Table 3.
Extended.
Footnotes
Supervising Section Editor: Monica H Swahn, PhD, MPH
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.Tjaden P, Thoennes N, Allison CJ. Comparing violence over the life span in samples of same-sex and opposite-sex cohabitants. Violence and Victims. 1999;14(4):413–425. [PubMed] [Google Scholar]
- 2.Blosnich JR, Bossarte RM. Comparisons of intimate partner violence among partners in same-sex and opposite-sex relationships in the United States. AmericanJournal of Public Health. 2009;99(12):2182. doi: 10.2105/AJPH.2008.139535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Messinger AM. Invisible Victims: Same-Sex IPV in the National Violence Against Women Survey. Journal of Interpersonal Violence. 2011;26(11):2228. doi: 10.1177/0886260510383023. [DOI] [PubMed] [Google Scholar]
- 4.Nieves-Rosa LE, Carballo-Dieguez A, Dolezal C. Domestic abuse and HIV-risk behavior in Latin American men who have sex with men in New York City. Journal of Gay & Lesbian Social Services. 2000;11(1):77–90. [Google Scholar]
- 5.Balsam KF, Lehavot K, Beadnell B. Sexual revictimization and mental health: A comparison of lesbians, gay men, and heterosexual women. Journal of Interpersonal Violence. 2011;26(9):1798. doi: 10.1177/0886260510372946. [DOI] [PubMed] [Google Scholar]
- 6.Pantalone DW, Hessler DM, Simoni JM. Mental health pathways from interpersonal violence to health-related outcomes in HIV-positive sexual minority men. Journal of Consulting and Clinical Psychology. 2010;78(3):387. doi: 10.1037/a0019307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong CF, Weiss G, Ayala G, et al. Harassment. Discrimination, violence and illicit drug use among young men who have sex with men. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education. 2010;22(4):286. doi: 10.1521/aeap.2010.22.4.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braitstein P, Asselin JJ, Schilder A, et al. Sexual violence among two populations of men at high risk of HIV infection. AIDS Care. 2006;18(7):681–689. doi: 10.1080/13548500500294385. [DOI] [PubMed] [Google Scholar]
- 9.Stephenson R, de Voux A, Sullivan PS. Intimate partner violence and sexual risk-taking among men who have sex with men in South Africa. Western Journal of Emergency Medicine. 2011;12(3):343. [PMC free article] [PubMed] [Google Scholar]
- 10.Coker AL, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine. 2002;23(4):260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 11.Campbell JC. Health consequences of intimate partner violence. The Lancet. 2002;359(9314):1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 12.Dunkle KL, Jewkes RK, Nduna M, et al. Perpetration of partner violence and HIV risk behaviour among young men in the rural Eastern Cape, South Africa. AIDS. 2006;20(16):2107. doi: 10.1097/01.aids.0000247582.00826.52. [DOI] [PubMed] [Google Scholar]
- 13.Greenwood GL, Relf MV, Huang B, et al. Battering victimization among a probability-based sample of men who have sex with men. American Journal of Public Health. 2002;92(12):1964. doi: 10.2105/ajph.92.12.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koblin BA, Torian L, Xu G, et al. Violence and HIV-related risk among young men who have sex with men. AIDS care. 2006;18(8):961–967. doi: 10.1080/09540120500467182. [DOI] [PubMed] [Google Scholar]
- 15.Feldman MB, Ream G, Rafeal D, et al. Intimate partner violence and HIV sexual risk behavior among Latino gay and bisexual men. Journal of LGBT Health Research. 2007;3(2):9. doi: 10.1300/J463v03n02_02. [DOI] [PubMed] [Google Scholar]
- 16.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93(6):939. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stephenson R, Rentsch C, Salazar LF, et al. Dyadic characteristics and intimate partner violence among men who have sex with men. Western Journal of Emergency Medicine. 2011;12(3):324. [PMC free article] [PubMed] [Google Scholar]
- 18.Houston E, McKirnan DJ. Intimate partner abuse among gay and bisexual men: Risk correlates and health outcomes. Journal of Urban Health. 2007;84(5):681–690. doi: 10.1007/s11524-007-9188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Relf MV, Huang B, Campbell J, et al. Gay identity, interpersonal violence, and HIV risk behaviors: An empirical test of theoretical relationships among a probability-based sample of urban men who have sex with men. Journal of the Association of Nurses in AIDS Care. 2004;15(2):14–26. doi: 10.1177/1055329003261965. [DOI] [PubMed] [Google Scholar]
- 20.Welles SL, Corbin TJ, Rich JA, et al. Intimate Partner Violence Among Men Having Sex with Men, Women, or Both: Early-Life Sexual and Physical Abuse as Antecedents. Journal of Community Health. 2010:1–9. doi: 10.1007/s10900-010-9331-9. [DOI] [PubMed] [Google Scholar]
- 21.Van Griensven F, et al. The global epidemic of HIV infection among men who have sex with men. Current Opinion in HIV and AIDS. 2009;4(4):300. doi: 10.1097/COH.0b013e32832c3bb3. [DOI] [PubMed] [Google Scholar]
- 22.Beyrer C, Baral SD, Walker D, et al. The expanding epidemics of HIV type 1 among men who have sex with men in low-and middle-income countries: diversity and consistency. Epidemiologic reviews. 2010;32(1):137–151. doi: 10.1093/epirev/mxq011. [DOI] [PubMed] [Google Scholar]
- 23.Jaffe HW, Valdiserri RO, De Cock KM. The reemerging HIV/AIDS epidemic in men who have sex with men. JAMA: the Journal of the American Medical Association. 2007;298(20):2412. doi: 10.1001/jama.298.20.2412. [DOI] [PubMed] [Google Scholar]
- 24.Herrick AL. School of Public Health. University of Pittsburgh D-Scholarship @ Pitt; 2011. Syndemic Processes Among Young Men Who Have Sex With Men (MSM): Pathways Toward Risk and Resilience; p. 123. p. Available at: http://d-scholarship.pitt.edu/6874/1/Herrick_2011.pdf. [Google Scholar]
- 25.Safren SA, Blashill AJ, O'Cleirigh CM. Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS and Behavior. 2011:1–5. doi: 10.1007/s10461-011-9898-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramachandran S. The intimate partner violence and HIV syndemic among MSM: Gaining a better understanding of disease overlap. University of Pittsburgh; 2008. [Google Scholar]
- 27.Stall R, Friedman M, Catania JA. Interacting epidemics and gay men's health: A theory of syndemic production among urban gay men. Unequal opportunity: Health disparities affecting gay and bisexual men in the United States; 2008. pp. 251–274. [Google Scholar]
- 28.Reynolds R. Social Discrimination Against Men Who Have Sex With Men (MSM) Implications for HIV Policy and Programs. Global Forum on MSM & HIV. 2010 Available at: http://www.msmgf.org/files/msmgf/Advocacy/Policy_Briefs/Stigma_EN_hi.pdf. [Google Scholar]
- 29.Schleifer R. Hated to Death-Homophobia, Violence, and Jamaica's HIV/AIDS Epidemic. 2009 [Google Scholar]
- 30.Peralta RL, Ross J. Understanding the complexity of alcohol-related intimate partner violence in the lives of Hispanic men who have sex with men: Methodological issues and considerations. Gender Issues. 2009;26(1):85–104. [Google Scholar]
- 31.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laurence J. Men who have sex with men: a new focus internationally. AIDS Reader-New York. 2007;17(8):379. [PubMed] [Google Scholar]
- 33.Epprecht M. New African Histories. South Africa: Ohio University Press; 2008. Heterosexual Africa?: The History of an Idea from the Age of Exploration to the Age of AIDS. [Google Scholar]
- 34.Murray SO, Roscoe W. Boy-wives and female husbands: Studies of African homosexualities. Palgrave MacMillan; 2001. [Google Scholar]
- 35.Mayer KH, Mimiaga MJ, Safren SA. Out of the closet and Into public health focus: HIV and STDs in men who have sex with men in middle income and resource-limited countries. Sexually transmitted diseases. 2010;37(4):205. doi: 10.1097/OLQ.0b013e3181d13d3e. p. [DOI] [PubMed] [Google Scholar]
- 36.Bengtsson L, Thorson A. Global HIV surveillance among MSM: is risk behavior seriously underestimated? AIDS. 2010;24(15):2301. doi: 10.1097/QAD.0b013e32833d207d. p. [DOI] [PubMed] [Google Scholar]
- 37.Schneider JA, et al. A protective effect of circumcision among receptive male sex partners of Indian men who have sex with men. AIDS and Behavior. 2011:1–10. doi: 10.1007/s10461-011-9982-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Williamson LM, Dodds JP, Mercey DE, et al. Sexual risk behaviour and knowledge of HIV status among community samples of gay men in the UK. AIDS. 2008;22(9):1063. doi: 10.1097/QAD.0b013e3282f8af9b. [DOI] [PubMed] [Google Scholar]
- 39.Diaz RM, Ayala G, Bein E, et al. The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: Findings from 3 US cities. American Journal of Public Health. 2001;91(6):927. doi: 10.2105/ajph.91.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Relf MV. Battering and HIV in men who have sex with men: A critique and synthesis of the literature. Journal of the Association of Nurses in AIDS Care. 2001;12(3):41–48. doi: 10.1016/S1055-3290(06)60143-X. [DOI] [PubMed] [Google Scholar]