Abstract
Objectives. We examined relationships between neighborhood poverty and allostatic load in a low- to moderate-income multiracial urban community. We tested the hypothesis that neighborhood poverty is associated with allostatic load, controlling for household poverty. We also examined the hypotheses that this association was mediated by psychosocial stress and health-related behaviors.
Methods. We conducted multilevel analyses using cross-sectional data from a probability sample survey in Detroit, Michigan (n = 919) and the 2000 US Census. The outcome measure was allostatic load. Independent variables included neighborhood and household poverty, psychosocial stress, and health-related behaviors. Covariates included neighborhood and individual demographic characteristics.
Results. Neighborhood poverty was positively associated with allostatic load (P < .05), independent of household poverty and controlling for potential confounders. Relationships between neighborhood poverty were mediated by self-reported neighborhood environment stress but not by health-related behaviors.
Conclusions. Neighborhood poverty is associated with wear and tear on physiological systems, and this relationship is mediated through psychosocial stress. These relationships are evident after accounting for household poverty levels. Efforts to promote health equity should focus on neighborhood poverty, associated stressful environmental conditions, and household poverty.
A burgeoning literature has demonstrated relationships between socioeconomic status (SES) and a variety of health outcomes.1–7 The persistence of relationships between SES, assessed at individual or neighborhood levels, and health outcomes over time has led scholars to suggest that SES influences health through a broad range of behavioral and physiological mechanisms.8–10 Attention has increasingly turned to disentangling the pathways through which SES may influence health, including both individual and neighborhood socioeconomic characteristics. We have contributed to this literature by examining relationships between socioeconomic characteristics of residential neighborhoods and allostatic load, an indicator of cumulative physiological response to stress. We examined potential pathways linking neighborhood SES to allostatic load by testing the extent to which these relationships are mediated by perceived or self-reported indicators of psychosocial stress and by health-related behaviors.
The conceptual model that guides this analysis builds on both conceptual and empirical research arguing that SES is a fundamental factor that influences health through multiple pathways,8,9,11,12 with cumulative health effects over the life course. Neighborhood poverty levels influence local social and physical environmental conditions (e.g., access to food, safe places for physical activity),12 which influence health-related behaviors (e.g., dietary practices, physical activity). Conditions in the social and physical environment may also influence health if they are conducive to stress and are referred to as stressors if they are likely to be perceived as harmful, threatening, or bothersome13 or as placing a demand on individuals that results in a physiological adaptational responses.14 Physiological responses are initiated as the body attempts to achieve stability (allostasis) when exposed to chronically stressful physical and social environments, for example, chronic challenges experienced as a result of poverty.15–23
Physiological responses to stress can accumulate and result in overexposure to neural, endocrine, and immune stress mediators (allostatic load), leading to enduring negative health outcomes through effects on the hypothalamic–pituitary–adrenal cortex, sympathetic nervous system, and immune system, with subsequent implications for peripheral biology.16,20,24–31 Negative health outcomes include effects on systolic and diastolic blood pressure, which are associated with higher mortality rates, cardiovascular disease, stroke, and the loss of physical and cognitive functioning.32–35 Chronic exposures to stress also affect metabolic systems, with established implications for health, including higher total cholesterol, lower high-density lipoproteins, higher weight,30,36–39 and elevated glucose levels.30,40–43 These metabolic indicators have been associated with heightened risk of mortality, increased cardiovascular risk, and poorer cognitive functioning.30,32,44–46
McEwen et al.29,30 conceptualized allostatic load as an indicator of the “cumulative physiological toll on multiple major biological systems over the life course”30(p223) that results from exposure to stressful life circumstances. Substantial evidence suggests that cardiovascular and metabolic risk varies by individual- or household-level SES, and recent studies have specifically demonstrated an inverse socioeconomic gradient in allostatic load.30,47–49 A growing body of research1–7 also demonstrates relationships between neighborhood SES and a variety of health outcomes, independent of the effects of individual or household income. Merkin et al.50 tested whether associations between percentage of households below the poverty line at the census tract level and allostatic load differed by race/ethnicity, using a nationally representative sample of non-Hispanic White, non-Hispanic Black, and Mexican Americans (National Health and Nutrition Examination Survey [NHANES] 1988–1994). They reported a significant inverse relationship between neighborhood SES and allostatic load among non-Hispanic Blacks, with similar but not significant trends among non-Hispanic Whites and Mexican Americans. Stimpson et al.,51 using data from NHANES III, found a positive association between a composite measure of neighborhood deprivation and serum triglyceride levels, 1 component of allostatic load.
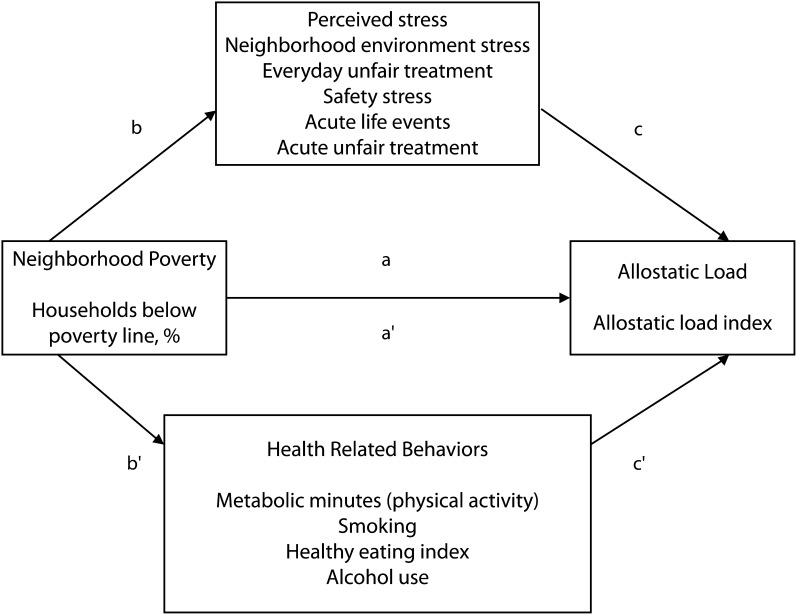
Building on this conceptual model and empirical literature, we examined 3 major research questions (Figure 1). First, we asked whether neighborhood poverty is associated with allostatic load among non-Hispanic Black, non-Hispanic White, and Hispanic residents of a major Midwestern urban community, independent of the effects of household income. Second, we tested specific pathways through which neighborhood poverty may contribute to allostatic load. Specifically, we tested the hypothesis that relationships between neighborhood poverty and allostatic load are mediated by self-reported psychosocial stress associated with neighborhood conditions. To examine the specificity of mediating effects, we tested the extent to which relationships between neighborhood poverty and allostatic load are mediated by indicators of psychosocial stress that reflect domains other than neighborhood environments, for example, experiences of unfair treatment.52,53 Third, because numerous health-related behaviors have been found to be associated with neighborhood poverty, including dietary patterns,54–56 smoking,57–59 physical activity,51,59–61 and alcohol use,51,62 and these behaviors may also be associated with components of allostatic load (e.g., blood pressure, lipid levels), we examined the extent to which relationships between neighborhood poverty and allostatic load are mediated by health-related behaviors.
FIGURE 1—
Hypothesized pathways mediating relationships between neighborhood poverty and allostatic load: Healthy Environments Partnership Community Survey, Detroit, MI, 2002–2003.
METHODS
We drew the data for this study from the Healthy Environments Partnership Community Survey, 1 component of a community-based participatory research study involving academic-, health care–, and community-based organizations in Detroit, Michigan.12 The Healthy Environments Partnership Community Survey is a stratified 2-stage probability sample of occupied housing units, designed for 1000 completed interviews with adults older than 25 years across 3 areas of Detroit, which allows comparisons of residents of similar demographics across geographic areas of the city.12 The survey sample was designed to achieve adequate variation in SES within each of the 3 predominant racial/ethnic groups in Detroit: non-Hispanic Black, Hispanic, and non-Hispanic White. Interviews were conducted in 2002 and 2003 and were completed with 75% of households in which an eligible respondent was identified. The final sample consisted of 919 face-to-face interviews, nested within 69 block groups.12
The Healthy Environments Partnership Community Survey included the following clinical and anthropometric measures: resting blood pressure, measured 3 times by a team of trained and certified phlebotomists using a portable cuff device (Omron model HEM 711AC) that passed Association for the Advancement of Medical Instrumentation standards63; waist circumferences (in centimeters); height (in centimeters); and weight in pounds using a calibrated scale. Glucose, total cholesterol, and high- and low-density lipid levels were derived from fasting blood samples from survey participants.
Measures
We adapted our measure of allostatic load from Seeman et al.30 as a measure of cumulative physiological toll on biological systems. It includes systolic and diastolic pressure derived by taking the mean of the second and third measured levels; waist circumference; glucose, high-density lipoproteins, total cholesterol, and triglycerides from fasting blood draws; and self-reported use of medication for hypertension, diabetes, and hypercholestemia. We calculated an allostatic load index as the sum of the following: systolic blood pressure 140 millimeters of mercury or greater; diastolic blood pressure 90 millimeters of mercury or greater; waist circumference 102 centimeters or greater (men) or 88 centimeters or greater (women); glucose 110 milligrams per deciliter or greater; triglycerides 150 milligrams per deciliter or greater; total cholesterol greater than 240 milligrams per deciliter or total cholesterol 240 milligrams per deciliter or less and LDL greater than 130 milligrams per deciliter; and high-density lipoproteins less than 40 milligrams per deciliter (men) or less than 50 milligrams per deciliter (women). Following Geronimus et al.,64 the index included points for individuals whose systolic and diastolic blood pressure levels were below the high blood pressure cutpoints and who were taking hypertension medication, those with glucose levels below the high-risk cutpoint who were taking medication, and those whose lipid levels were within the normal range and who were taking medication for dyslipidemia. The mean for this index was 2.63 (SD = 0.07; min = 0, max = 7).
Individual-level independent variables included a dichotomous indicator of household poverty, calculated using the poverty income ratio (1 < poverty, 0 ≥ poverty). We independently calculated the poverty income ratio using 2002 census estimates for US poverty thresholds and 2002 survey data available for total household income and the total number of adults and children in the household. We classified individuals and families as “in poverty” when total household income was below the poverty threshold.65
We used 5 measures of perceived or self-reported stress: perceptions of the neighborhood environment, everyday unfair treatment, safety stress, acute unfair treatment, and acute life events.
Neighborhood environment stress is a mean scale including 13 indicators of social and physical characteristics of the neighborhood environment: 6 items assessed the frequency with which respondents indicate that aspects of the social environment, such as gang activity, shootings, and theft, were a problem in their neighborhood (response categories ranged from 1 = never to 5 = always),66,67 and 7 items assessed agreement with statements about the physical environment, such as, “Houses in my neighborhood are generally well maintained” (reverse coded) and “There is air pollution like diesel from trucks or pollution from factories or incinerators in my neighborhood” (response categories ranged from 1 = strongly disagree to 5 = strongly agree; Cronbach α = 0.83).67,68
Everyday unfair treatment53 is the mean of 5 items assessing the frequency of experiences of unfair treatment, such as poorer service than other people in restaurants or stores and being treated with less courtesy or respect than other people in the previous 12 months (Cronbach α = 0.77). Response categories ranged from 1 = never to 5 = always.53 Safety stress is the mean of 3 items rated on a 5-point scale from 1 = never to 5 = always with items such as, “worry about your safety in your home” and “worry about your safety in the neighborhood” (Cronbach α = 0.85).
Acute unfair treatment53 is a dichotomous variable indicating whether the respondent reported any of 7 experiences with acute unfair treatment (e.g., unfair treatment concerning work, treated unfairly by police or immigration officials) in the past year (0 = none, 1 = 1 or more). Acute life events is a dichotomous variable indicating whether the respondent reported any of 9 major life events in the past year (e.g., death of a loved one, family member, or close friend from a major illness or injury; 0 = none, 1 = 1 or more).69–71
We used 4 measures of health-related behaviors. We included metabolic minutes as a continuous measure of physical activity using methods described in the 2005 International Physical Activity Questionnaire.72 We assessed smoking through a series of items asking about current and former tobacco use, for example, “Have you ever smoked cigarettes regularly?” and “Do you currently smoke cigarettes?”73,74 and including parallel questions about smoking cigars and tobacco pipes. Smoking was coded as a dichotomous indicator (current smoker = 1, former or never smoked = 0). We assessed alcohol use as self-reported frequency and amount of alcohol use,75 and dichotomized as 1 = any, 0 = none. We assessed dietary practices using the Healthy Eating Index, a composite measure of 5 food groups and 4 nutrients related to daily servings that is widely used as an overall indicator of dietary quality.76
Individual-level control variables included age (years); gender (0 = male, 1 = female); self-reported race and ethnicity categorized as non-Hispanic Black, non-Hispanic White, and Hispanic; and education (< 12 years, ≥ 12 years). Length of residence in the neighborhood (years) was used to assess sensitivity of findings.
At the neighborhood level, neighborhood poverty was the percentage of households below the poverty line at the census block group level, derived from 2000 US Census data. Neighborhood-level control variables included percentage non-Hispanic Black and percentage Hispanic at the block group level.
Data Analysis
In preparation for analysis, we used multiple imputation procedures derived from Bayesian models77 to impute missing values using the %IMPUTE routine (Imputation and Variance Estimation software, Ann Arbor, MI) in SAS version 9.1 (SAS Institute, Cary, NC, 2002–2003). Although the proportion of missing data was low, multiple imputation allowed us to incorporate design-based features (weight, strata, primary sampling unit) in our analysis and thus obtain accurate SE estimates.78,79
We estimated 2-level weighted hierarchical regression models for a continuous outcome using HLM 6.08 (Scientific Software International, Lincolnwood, IL). Level 1 was the 919 survey respondents; and level 2 was the 69 census block groups in which respondents resided. We used the multistep procedure Baron and Kenny described80 to test for mediating effects of perceived stress on the relationship between neighborhood poverty and allostatic load. As illustrated in Figure 1, we first tested the hypothesis that percentage poverty at the block group level was positively associated with allostatic load, after accounting for household SES. To test the extent to which this relationship was mediated by each measure of perceived stress, we regressed (1) each measure of perceived stress on neighborhood poverty (path b), (2) allostatic load on each measure of perceived stress (path c), and (3) allostatic load on neighborhood poverty with each measure of perceived stress in the model (path a′). We then examined the difference between a and a′. We used the same steps to test for mediating effects of each of the behavioral indicators (metabolic minutes of physical activity, smoking, Healthy Eating Index, and alcohol use; paths b′ and c′). Finally, we tested a complete model that included all measures of perceived stress and health-related behaviors that were significant predictors of allostatic load to assess the extent to which they attenuated relationships between neighborhood percentage poverty and allostatic load. All models were adjusted for sample weights for unequal probabilities of selection within each stratum and to match the sample to US Census 2000 population distributions for the study areas.
RESULTS
Table 1 shows weighted descriptive statistics for the individual- and neighborhood-level variables. About half of participants were female; 56.8% were non-Hispanic Black, 22.2% were Hispanic, and 18.8% non-Hispanic White; 63.1% had completed high school or more; 37.8% had a per capita annual household income at or above the poverty level; and mean length of residence in the neighborhood was 18.5 years. The mean score on the neighborhood environment stress scale was 2.9 (SD = 0.05), mean for everyday unfair treatment was 1.7 (SD = 0.03), and safety stress was 2.5 (SD = 0.05). Of the study participants, 71% reported 1 or more acute life events in the previous 12 months, and 29.4% reported 1 or more experiences of acute unfair treatment. On average, participants were aged 46.3 years, scored 64.1 (SD = 0.43) on the Healthy Eating Index, and accumulated 3698.7 (SD = 152.1) metabolic minutes per week; 37.1% indicated that they currently smoked cigarettes, and 47.3% indicated that they ever drank alcohol. The mean percentage of households below the poverty line at the block group level was 32.5 (SD = 11.9), mean percentage non-Hispanic Black was 67.5 (SD = 35.5), and mean percentage Hispanic was 15.2 (SD = 26.8).
TABLE 1—
Weighted Descriptive Statistics for Individual- and Neighborhood-Level Variables: Healthy Environments Partnership Community Survey, Detroit, MI, 2002–2003
| Individual Variables | % or Mean (SD) |
| Age, y | 46.3 (0.84) |
| Female | 52.3 |
| Race/ethnicity | |
| Non-Hispanic Black | 56.8 |
| Hispanic | 22.2 |
| Non-Hispanic White | 18.8 |
| Other | 2.3 |
| Education | |
| < high school diploma | 36.9 |
| ≥ high school diploma | 63.1 |
| Household income above poverty | 37.8 |
| Length of residence in neighborhood, y | 18.5 (0.66) |
| Neighborhood environment stress | 2.9 (0.05) |
| Everyday unfair treatment | 1.7 (0.03) |
| Safety stress | 2.5 (0.05) |
| Acute life events | 71.1 |
| Acute unfair treatment | 29.4 |
| Allostatic load | 2.6 (0.07) |
| Current smoking | 37.1 |
| Healthy Eating Index | 64.1 (0.43) |
| Physical activity (metabolic minutes) | 3698.7 (152.10) |
| Alcohol use | 47.3 |
| Neighborhood variables (census block group), % | |
| Below poverty | 32.5 (11.90) |
| Non-Hispanic Black | 67.5 (35.50) |
| Hispanic | 15.2 (26.80) |
Note. The sample size was n = 919.
Table 2 shows the results of the multilevel regression analysis. As shown in model 1, neighborhood poverty was significantly (Β = 0.012; P = .019) and positively associated with allostatic load, controlling for neighborhood racial and ethnic composition and individual demographic characteristics. Household poverty level was independently and positively associated with allostatic load (Β = 0.031; P = .01). Results from models that included interaction terms to assess whether relationships between neighborhood poverty and allostatic load differed by race and ethnicity did not support the hypothesis (results not shown).
TABLE 2—
Allostatic Load Regressed on Neighborhood Poverty, Neighborhood Environment Stress, and Acute Life Events, and Alcohol Use: Healthy Environments Partnership Community Survey, Detroit, MI, 2002–2003
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||
| B (SE) | P | B (SE) | P | B (SE) | P | B (SE) | P | |
| Intercept | 2.436 (0.120) | < .001 | 2.442 (0.124) | < .001 | 2.261 (0.154) | < .001 | 2.488 (0.145) | < .001 |
| Level 2 (block group) | ||||||||
| Neighborhood poverty, % | 0.012 (0.005) | .019 | 0.011 (0.006) | .066 | 0.011 (0.005) | .03 | 0.010 (0.006) | .086 |
| Level 1 (individual) | ||||||||
| Household poverty | 0.301 (0.116) | .01 | 0.308 (0.115) | .008 | 0.283 (0.116) | .016 | 0.268 (0.118) | .023 |
| Behavior measures | ||||||||
| Alcohol use (1 = any) | −0.323 (0.117) | .007 | ||||||
| Stress measures | ||||||||
| Neighborhood environment stress | 0.151 (0.070) | .031 | 0.144 (0.070) | .039 | ||||
| Acute life events | 0.233 (0.119) | .051 | 0.216 (0.127) | .088 | ||||
| σ2 | 1.56 (0.036) | 1.55 (0.039) | 1.55 (0.037) | 1.53 (0.039) | ||||
Note. Control variables include neighborhood percentage Non-Hispanic Black, neighborhood percentage Hispanic, and individual age, gender, household income below poverty, education, and race/ethnicity.
Next we tested the hypothesis that the relationship between neighborhood poverty and allostatic load was mediated through self-reported psychosocial stress. To test pathway b (Figure 1), we ran separate models with each of the 5 measures of stress (e.g., neighborhood environment stress, everyday unfair treatment). Neighborhood poverty was significantly and positively associated with perceived neighborhood environment stress (Β = 0.011; P = .038), and acute life events (Β = 1.019; P = .041). Similar trends for perceived safety (Β = 0.000; P = .963), everyday unfair treatment (Β = 0.003; P = .267), and acute unfair treatment (odds ratio [OR] = 1.007; P = .361) were not statistically significant.
To test pathway c (Figure 1), we regressed allostatic load on each measure of psychosocial stress. Allostatic load was positively associated with neighborhood environment stress (Β = 0.190; P = .011) and acute life events (Β = 0.257; P = .029). Relationships between allostatic load and everyday unfair treatment (Β = 0.042; P = .631), safety stress (Β = 0.016; P = .711), and acute unfair treatment (Β = −0.089; P = .465) were not significant.
Results shown in Table 2, model 2 indicated that the relationship between neighborhood poverty and allostatic load was attenuated (Β = 0.011; P = .066) with the inclusion of neighborhood environment stress and that neighborhood environment stress remained a significant predictor of allostatic load (Β = 0.151; P = .031). The relationship between neighborhood poverty and allostatic load was also attenuated (Β = 0.011; P = .03) with the inclusion of acute life events (model 3) but remained significant. Acute life events was marginally significantly associated with allostatic load (Β = 0.233; P = .051).
Next we tested whether relationships between neighborhood poverty and allostatic load were mediated by health-related behaviors (pathway b′-c′). Relationships between neighborhood poverty and alcohol use (Β = 1.000; P = .971), Healthy Eating Index (Β = −0.009; P = .865), metabolic minutes of physical activity (Β = −5.8; P = .792), and smoking (OR = 1.009; P = .209) were not significant. We found no significant relationships between the Healthy Eating Index (Β = −0.007; P = .331), metabolic minutes (Β = 0.000; P = .774), or smoking (Β = −0.135; P = .216) and allostatic load. Alcohol use was significantly negatively associated with allostatic load (Β = −0.322; P = .006). We found no evidence that the behavioral indicators examined attenuated relationships between neighborhood poverty and allostatic load (results not shown).
Finally, we tested a full model that included neighborhood environment stress and acute life events as significant mediators of the relationship between neighborhood poverty and allostatic load. We also included alcohol use, given its significant association with allostatic load. Results shown in Table 2, model 4 indicated that the relationship between neighborhood poverty and allostatic load was attenuated (Β = 0.010; P = .086), with neighborhood environment stress (Β = 0.144; P = .039) but not acute life events (Β = 0.216; P = .088), remaining significant. Alcohol remained independently associated with allostatic load (Β = −0.323; P = .007).
DISCUSSION
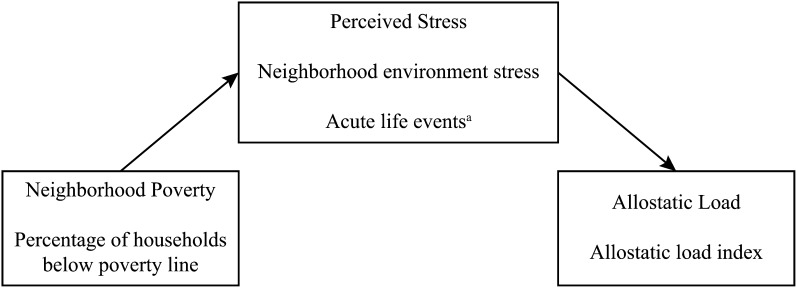
There were 3 main findings from the analyses reported here. Neighborhood poverty was positively associated with allostatic load, independent of household poverty and controlling for potential confounders. Relationships between neighborhood poverty and allostatic load were mediated by self-reported neighborhood environment stress. We found no evidence to support the hypothesis that relationships between neighborhood poverty and allostatic load were mediated by health-related behaviors. Findings are summarized in Figure 2.
FIGURE 2—
Pathways mediating relationships between neighborhood poverty and allostatic load: Healthy Environments Partnership Community Survey, Detroit, MI, 2002–2003.
aPartial Mediator.
Our findings are consistent with the hypothesis that neighborhood poverty is positively associated with allostatic load, independent of neighborhood racial and ethnic composition, household poverty, and individual demographic control variables. The effect size should be interpreted with caution, given the relatively modest sample size and our use of tests for statistical significance, rather than parameter estimation.81 However, these results suggest that residents of neighborhoods with 20% of households below the poverty line would experience an average allostatic load score 0.20 points higher—roughly 10% greater than the sample mean of 2.6—than the average for residents of neighborhoods with no households below poverty. These findings are consistent with trends reported elsewhere indicating that residents of neighborhoods with lower SES experience greater biologic risk.3,30,50,51
Our finding of no difference between racial and ethnic groups in the relationship between neighborhood poverty and allostatic load differs from results reported by Merkin et al.,50 who found significant associations only among non-Hispanic Blacks. Merkin et al. suggest that their findings reflect higher concentrations of neighborhood poverty experienced by non-Hispanic Blacks compared with non-Hispanic Whites in the lowest SES quintile neighborhoods. By contrast, the average neighborhood poverty level in the Detroit sample did not differ significantly for non-Hispanic Blacks, non-Hispanic Whites, and Hispanic (results not shown). Thus, our findings are consistent with the suggestion that racial and ethnic differences in the association between neighborhood poverty and allostatic load reported elsewhere50 reflect greater neighborhood poverty encountered by non-Hispanic Blacks in that sample. When concentrations of neighborhood poverty were comparable, as in our Detroit-based sample, relationships between neighborhood poverty and allostatic load did not differ by race and ethnicity.
Our findings extend the literature by testing potential mediating pathways. Relationships between neighborhood poverty and allostatic load were mediated by perceptions of neighborhood environmental characteristics. Although relationships between neighborhood poverty and allostatic load were partially mediated by acute life events, this effect was no longer significant once we included neighborhood environment stress in the model.
Everyday and acute unfair treatment and safety stress did not mediate relationships between neighborhood poverty and allostatic load. Conceptually, indicators of everyday and acute unfair treatment were developed as measures of exposure to unfair treatment often associated with socially ascribed identities (e.g., race, ethnicity).53 They have been associated with race and with mental health outcomes, with mixed results for physical health indicators.52 Thus, the absence of a mediating effect is consistent with conceptualizations linking unfair treatment more closely to social identities than to neighborhood poverty. Similarly, the measure of safety stress used here, encompassing dimensions associated with safety in the home as well as the neighborhood, did not mediate relationships between neighborhood poverty and allostatic load. Together, these results suggest that relationships between neighborhood poverty and allostatic load may be mediated through stressors associated with neighborhood conditions but not substantially mediated by other dimensions of psychosocial stress assessed.
Finally, our findings suggest that relationships between neighborhood poverty and allostatic load are not substantially mediated by the health-related behaviors (diet, smoking, physical activity, alcohol use) assessed in this study. Although we did not find a significant associated between neighborhood poverty and alcohol use (and thus no mediating effect), a significant negative association between alcohol use and allostatic load remained robust in the full model that included indicators of self-reported stress. This finding is consistent with results reported by Hawkley et al.62 in a Chicago-based study of older adults.56
Stress process frameworks specifically hypothesize that stressful life conditions can set in motion physiological responses to maintain equilibrium within the body and that, under conditions of chronic stress, these responses may contribute to cumulative indicators of increased physiological risk. Results reported here are consistent with conceptual frameworks suggesting that SES operates through multiple pathways to influence physiological indicators of risk. Specifically, neighborhood SES was associated with allostatic load through pathways distinct from those linking household SES to allostatic load and from health-related behaviors.
Limitations and Implications for Future Research
As with most studies, these analyses have numerous limitations. The use of cross-sectional data limits our ability to test the order of associations between variables and to examine exposures over the life course. We attempted to examine this question by running models that included both a main effect of length of residence in the neighborhood and interaction terms to assess whether relationships between neighborhood poverty and allostatic load were modified by length of residence in the neighborhood. Length of residence was not associated with allostatic load (main effect) and did not modify the relationship between neighborhood poverty and allostatic load (results not shown) in these analyses. The mean length of residence in the neighborhood in this sample was quite long (18.5 years) and may have influenced these findings. Future research using longitudinal data will help establish the order of associations, examine implications of duration of exposure to neighborhood poverty and associated psychosocial stress, and explore lagged effects.
A second limitation is the use of self-reported measures of health-related behaviors and stress. We did not find a significant relationship between neighborhood poverty and health-related behaviors in this sample, perhaps because of the use of self-report measures. Future studies that incorporate less subjective measures of health-related behaviors (e.g., accelerometers) are needed to refine these results. Smoking prevalence in this study (37%) was substantially higher than national prevalence in the same year (22%),82 although comparable to rates reported for similar subgroups (44.4% for those with only a general equivalency diploma; 31% among those with incomes below the poverty line).82 Although our findings are consistent with findings reported elsewhere in the literature with levels of smoking more comparable to national rates,62 the relatively high levels of current smoking in this sample may have influenced results in unanticipated ways. Similarly, whereas the protective effect of alcohol use found in this study corroborates findings reported elsewhere,62 it is possible that results were shaped by relatively moderate alcohol consumption in the Detroit sample (mean = 11.4 drinks/month) or the use of a dichotomous indicator of alcohol use (any or none). Analyses that explore, for example, whether protective effects are apparent at various levels of alcohol consumption (e.g., low, moderate, high) and the potential pathways linking alcohol use to allostatic load are needed to better understand this relationship. Future studies examining the effects of variations in levels or in contextual factors on the potential mediating role of health-related behaviors may further clarify the parameters of these relationships.
Similarly, self-reported indicators of stress may inadequately capture social or physical environmental conditions conducive to stress both cross-sectionally and over the life course. In addition, the use of a dichotomous indicator of acute life events (any or none) may fail to adequately capture relationships between the number of acute life events and allostatic load. Future studies may consider the use of more finely graded measures of acute life events to examine this question. Analyses that examine a broader array of behavioral and psychosocial pathways between neighborhood poverty and allostatic load and that incorporate observed as well as self-reported indicators are needed to establish relationships between observed and perceived stressors.
Finally, given our relatively modest sample size, analyses with larger samples that enable specific parameter estimates across various contexts (e.g., varying concentrations of poverty) would further our understanding of relationships between neighborhood poverty and allostatic load. Analyses that examine mediating pathways across contexts (e.g., rural, regional) would also contribute to an understanding of the extent to which mediating pathways described here may vary across contexts.
Concluding Comments
The findings presented here add weight to a body of evidence suggesting associations between neighborhood poverty and allostatic load and extend the literature by examining potential mediating pathways. Results are consistent with arguments that SES is associated with multiple health outcomes through multiple pathways. Such arguments suggest that the health effects of residing in neighborhoods with high concentrations of poverty extend beyond implications for health-related behaviors and occur above and beyond those associated with household income. This body of research is in its infancy, and we have detailed numerous areas in need of further examination.
Despite the early stages of the evidence specifically linking neighborhood poverty to allostatic load, these results join a growing body of literature linking physiological indicators of stress to future morbidity and mortality stemming from cardiovascular and metabolic disorders such as diabetes.30 The finding that the proportion of households in one’s neighborhood with incomes below the poverty line is positively associated with allostatic load is consistent with a body of literature suggesting substantial long-term health implications of living in neighborhoods with high concentrations of poverty, independent of the effects of household income.3 Furthermore, the findings we have reported lend weight to the argument that interventions that seek to promote health-related behaviors or to increase access to resources that enable those behaviors (e.g., grocery stores carrying healthy foods), although important, may be insufficient to eliminate health inequities. Efforts to eliminate pervasive health inequities must attend to underlying economic, political, and social processes that perpetuate the concentration of poverty within urban neighborhoods. Policies that increase economic opportunities within urban neighborhoods with high concentrations of poverty and alleviate stressful social and physical environmental conditions are critical aspects of efforts to promote health equity.
Acknowledgments
This work was supported by the National Institute of Environmental Health Sciences (NIEHS; grants R01ES10936 and R01ES014234).
We thank the members of the Healthy Environments Partnership steering committee for their contributions to this work, including representatives from Brightmoor Community Center, Detroit Department of Health and Wellness Promotion, Detroit Hispanic Development Corporation, Friends of Parkside, Henry Ford Health System, Warren Conner Development Coalition, and University of Michigan School of Public Health. In addition, we thank Sue Andersen for assistance in preparation of this article and the anonymous reviewers who provided thoughtful and constructive comments on an earlier version of this article.
Note. The results presented here are solely the responsibility of the authors and do not necessarily represent the views of NIEHS.
Human Participant Protection
The University of Michigan institutional review board for protection of human subjects approved this study in January 2001, and survey participants provided written informed consent.
References
- 1.Borrell LN, Diez Roux A, Rose K, Catellier D, Clark BL. Neighbourhood characteristics and mortality in the Atherosclerosis Risk in Communities Study. Int J Epidemiol. 2004;33(2):398–407 [DOI] [PubMed] [Google Scholar]
- 2.Cox M, Boyle PJ, Davey PG, Feng Z, Morris AD. Locality deprivation and type 2 diabetes incidence: a local test of relative inequalities. Soc Sci Med. 2007;65(9):1953–1964 [DOI] [PubMed] [Google Scholar]
- 3.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145 [DOI] [PubMed] [Google Scholar]
- 4.Diez Roux AV, Merkin SS, Arnett Det al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106 [DOI] [PubMed] [Google Scholar]
- 5.Mair C, Diez Roux AV, Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health. 2008;62(11):940–946, 8 p following 946 [DOI] [PubMed] [Google Scholar]
- 6.Pickett KE, Pearl M. Multilevel analyses of neighborhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Winkleby M, Sundquist K, Cubbin C. Inequities in CHD incidence and case fatality by neighborhood deprivation. Am J Prev Med. 2007;32(2):97–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.House JS. Understanding social factors and inequalities in health: 20th century progress and 21st century prospects. J Health Soc Behav. 2002;43(2):125–142 [PubMed] [Google Scholar]
- 9.Link BG, Phelan JC, Miech R, Westin EL. The resources that matter: fundamental social causes of health disparities and the challenge of intelligence. J Health Soc Behav. 2008;49(1):72–91 [DOI] [PubMed] [Google Scholar]
- 10.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(suppl):S28–S40 [DOI] [PubMed] [Google Scholar]
- 11.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;35(spec no):80–94 [PubMed] [Google Scholar]
- 12.Schulz AJ, Kannan S, Dvonch JTet al. Social and physical environments and disparities in risk for cardiovascular disease: the Healthy Environments Partnership conceptual model. Environ Health Perspect. 2005;113(12):1817–1825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazarus RS, Folkman S. Stress, Appraisal and Coping. New York: Springer; 1984 [Google Scholar]
- 14.Selye H. History and present status of the stress concept. : Goldberger L, Breznitz S, Handbook of Stress: Theoretical and Clinical Aspects. 2nd ed New York: The Free Press; 1982:7–20 [Google Scholar]
- 15.Heslop P, Smith GD, Metcalfe C, MacLeod J, Hart C. Change in job satisfaction and its association with self-reported stress, cardiovascular risk factors, and mortality. Soc Sci Med. 2002;54(10):1589–1599 [DOI] [PubMed] [Google Scholar]
- 16.Israel BA, Schurman SJ. Social support, control and the stress process. : Glanz K, Lewis FM, Rimer BK, Health Behavior and Health Education: Theory, Research and Practice. San Francisco: Jossey-Bass; 1990:187–215 [Google Scholar]
- 17.Kawachi I, Berkman LF, Neighborhoods and Health. New York: Oxford University Press; 2003 [Google Scholar]
- 18.Klinenberg E. Heat Wave: A Social Autopsy of Disaster in Chicago. Chicago: University of Chicago Press; 2002 [DOI] [PubMed] [Google Scholar]
- 19.Maantay J. Zoning, equality, and public health Am J Public Health. 2001;91(7):1033–1041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McEwen BS. Central effects of stress hormones in health and disease: understanding the protective and damaging effects of stress and stress mediators. Eur J Pharmacol. 2008;583(2–3):174–185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morenoff JD, Sampson RJ. Violent crime and the spatial dynamics of neighborhood transition: Chicago 1970–1990. Soc Forces. 1997;76(1):31–64 [Google Scholar]
- 22.Pickering T. Cardiovascular pathways: socioeconomic status and stress effects on hypertension and cardiovascular function. Ann N Y Acad Sci. 1999;896:262–277 [DOI] [PubMed] [Google Scholar]
- 23.Sampson RJ, Raudenbush SW. Seeing disorder: neighborhood stigma and the social construction of “broken windows.” Soc Psychol Q. 2004;67(4):319–342 [Google Scholar]
- 24.Gunnar M, Quevedo K. The neurobiology of stress and development. Annu Rev Psychol. 2007;58:145–173 [DOI] [PubMed] [Google Scholar]
- 25.Gunnar M, Vazquez D. Stress neurobiology and developmental psychopathology. : Cicchetti D, Cohen D, Developmental Psychopathology: Developmental Neuroscience. New York: Wiley; 2006:533–577 [Google Scholar]
- 26.House JS. Work Stress and Social Support. Reading, MA: Addison-Wesley; 1981 [Google Scholar]
- 27.Katz D, Kahn RL. The Social Psychology of Organizations. 2nd ed New York: Wiley; 1978 [Google Scholar]
- 28.McEwen BS. Early life influences on life-long patterns of behavior and health. Ment Retard Dev Disabil Res Rev. 2003;9(3):149–154 [DOI] [PubMed] [Google Scholar]
- 29.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896:30–47 [DOI] [PubMed] [Google Scholar]
- 30.Seeman T, Epel E, Gruenewald T, Karlamangla A, McEwen BS. Socio-economic differentials in peripheral biology: cumulative allostatic load. Ann N Y Acad Sci. 2010;1186:223–239 [DOI] [PubMed] [Google Scholar]
- 31.Sterling P. Principles of allostasis: optimal design, predictive regulation, pathophysiology, and rational therapeutics. : Schulkin J, Allostasis, Homeostasis, and the Costs of Physiological Adaptation. Cambridge, UK: Cambridge University Press; 2004:17–64 [Google Scholar]
- 32.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4 pt 1):1973–1998 [DOI] [PubMed] [Google Scholar]
- 33.Seeman TE, Charpentier PA, Berkman LFet al. Predicting changes in physical performance in a high-functioning elderly cohort: MacArthur studies of successful aging. J Gerontol. 1994;49(3):M97–M108 [DOI] [PubMed] [Google Scholar]
- 34.Tzourio C, Dufouil C, Ducimetiere P, Alperovitch A. Cognitive decline in individuals with high blood pressure: a longitudinal study in the elderly. EVA Study Group. Epidemiology of Vascular Aging. Neurology. 1999;53(9):1948–1952 [DOI] [PubMed] [Google Scholar]
- 35.Zelinski EM, Crimmins E, Reynolds S, Seeman T. Do medical conditions affect cognition in older adults? Health Psychol. 1998;17(6):504–512 [DOI] [PubMed] [Google Scholar]
- 36.Lee BK, Glass TA, McAtee MJet al. Associations of salivary cortisol with cognitive function in the Baltimore memory study. Arch Gen Psychiatry. 2007;64(7):810–818 [DOI] [PubMed] [Google Scholar]
- 37.Li G, Cherrier MM, Tsuang DWet al. Salivary cortisol and memory function in human aging. Neurobiol Aging. 2006;27(11):1705–1714 [DOI] [PubMed] [Google Scholar]
- 38.Lupien S, Lecours AR, Lussier I, Schwartz G, Nair NP, Meaney MJ. Basal cortisol levels and cognitive deficits in human aging. J Neurosci. 1994;14(5 pt 1):2893–2903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation—allostatic load and its health consequences: MacArthur studies of successful aging. Arch Intern Med. 1997;157(19):2259–2268 [PubMed] [Google Scholar]
- 40.Gradman TJ, Laws A, Thompson LW, Reaven GM. Verbal learning and/or memory improves with glycemic control in older subjects with non-insulin-dependent diabetes mellitus. J Am Geriatr Soc. 1993;41(12):1305–1312 [DOI] [PubMed] [Google Scholar]
- 41.Khaw KT, Wareham N, Luben Ret al. Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of European prospective investigation of cancer and nutrition (EPIC-Norfolk). BMJ. 2001;322(7277):15–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manning CA, Hall JL, Gold PE. Glucose effects on memory and other neuropsychologicla tests in elderly humans. Psychol Sci. 1990;1(5):307–311 [Google Scholar]
- 43.Reaven GM, Thompson LW, Nahum D, Haskins E. Relationship between hyperglycemia and cognitive function in older NIDDM patients. Diabetes Care. 1990;13(1):16–21 [DOI] [PubMed] [Google Scholar]
- 44.Benfante R, Reed D, Brody J. Biological and social predictors of health in an aging cohort. J Chronic Dis. 1985;38(5):385–395 [DOI] [PubMed] [Google Scholar]
- 45.Lynch JW, Kaplan GA, Cohen RD, Tuomilehto J, Salonen JT. Do cardiovascular risk factors explain the relation between socioeconomic status, risk of all-cause mortality, cardiovascular mortality, and acute myocardial infarction? Am J Epidemiol. 1996;144(10):934–942 [DOI] [PubMed] [Google Scholar]
- 46.McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Seeman T, Merkin SS, Crimmins E, Koretz B, Charette S, Karlamangla A. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988–1994). Soc Sci Med. 2008;66(1):72–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seeman TE, Crimmins E, Huang MHet al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc Sci Med. 2004;58(10):1985–1997 [DOI] [PubMed] [Google Scholar]
- 49.Singer B, Ryff CD. Hierarchies of life histories and associated health risks. Ann N Y Acad Sci. 1999;896:96–115 [DOI] [PubMed] [Google Scholar]
- 50.Merkin SS, Basurto-Davila R, Karlamangla Aet al. Neighborhoods and cumulative biological risk profiles by race/ethnicity in a national sample of U.S. adults: NHANES III. Ann Epidemiol. 2009;19(3):194–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stimpson JP, Ju H, Raji MA, Eschbach K. Neighborhood deprivation and health risk behaviors in NHANES III. Am J Health Behav. 2007;31(2):215–222 [DOI] [PubMed] [Google Scholar]
- 52.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2008;98(9 suppl):S29–S37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351 [DOI] [PubMed] [Google Scholar]
- 54.Dubowitz T, Heron M, Bird CEet al. Neighborhood socioeconomic status and fruit and vegetable intake among Whites, Blacks, and Mexican Americans in the United States. Am J Clin Nutr. 2008;87(6):1883–1891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23(11–12):887–894 [DOI] [PubMed] [Google Scholar]
- 56.Zenk SN, Schulz AJ, Mentz G, Israel BA, Lockett M. “Do obesogenic neighborhood food environments exacerbate effects of psychosocial stressors on ‘comfort’ food intake?” Paper presented at the Annual Meeting of the International Society of Behavioral Nutrition and Physical Activity; June 9–12, 2010; Minneapolis, MN. [Google Scholar]
- 57.Ahluwalia IB, Mack KA, Mokdad A. Mental and physical distress and high-risk behaviors among reproductive-age women. Obstet Gynecol. 2004;104(3):477–483 [DOI] [PubMed] [Google Scholar]
- 58.Graham H, Hunt S. Women’s smoking and measures of women’s socio-economic status in the United Kingdom. Health Promot Int. 1994;9(2):81–88 [Google Scholar]
- 59.Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychol. 2003;22(6):638–642 [DOI] [PubMed] [Google Scholar]
- 60.Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality. JAMA. 1998;279(21):1703–1708 [DOI] [PubMed] [Google Scholar]
- 61.Schoenborn CA, Adams PF, Barnes PM, Vickerie JL, Schiller JS. Health behaviors of adults: United States, 1999–2001. Vital Health Stat 10. 2004;(219):1–79 [PubMed] [Google Scholar]
- 62.Hawkley LC, Lavelle LA, Berntson GG, Cacioppo JT. Mediators of the relationship between socioeconomic status and allostatic load in the Chicago Health, Aging, and Social Relations Study (CHASRS). Psychophysiology. 2011;48(8):1134–1145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yarows SA, Brook RD. Measurement variation among 12 electronic home blood pressure monitors. Am J Hypertens. 2000;13(3):276–282 [DOI] [PubMed] [Google Scholar]
- 64.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. Am J Public Health. 2006;96(5):826–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.US Census Bureau Poverty Thresholds. Available at: http://www.census.gov/hhes/www/poverty/data/threshld/index.html. Accessed February 1, 2011
- 66.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924 [DOI] [PubMed] [Google Scholar]
- 67.Schulz AJ, Zenk SN, Israel BA, Mentz G, Stokes C, Galea S. Do neighborhood economic characteristics, racial composition, and residential stability predict perceptions of stress associated with the physical and social environment? Findings from a multilevel analysis in Detroit. J Urban Health. 2008;85(5):642–661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Israel BA, Schulz AJ, Estrada-Martinez Let al. Engaging urban residents in assessing neighborhood environments and their implications for health. J Urban Health. 2006;83(3):523–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Blazer D, Hughes D, George LK. Stressful life events and the onset of a generalized anxiety syndrome. Am J Psychiatry. 1987;144(9):1178–1183 [DOI] [PubMed] [Google Scholar]
- 70.George LK, Blazer DG, Hughes DC, Fowler N. Social support and the outcome of major depression. Br J Psychiatry. 1989;154:478–485 [DOI] [PubMed] [Google Scholar]
- 71.Hughes DC, Blazer DG, George LK. Age differences in life events: a multivariate controlled analysis. Int J Aging Hum Dev. 1988;27(3):207–220 [DOI] [PubMed] [Google Scholar]
- 72.IPAQ Research Committee Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ); 2005. Available at: http://www.ipaq.ki.se/scoring.pdf. Accessed January 8, 2012
- 73.Frazier EL, Franks AL, Sanderson LM. Using behavioral risk factor surveillance data. In: National Center for Chronic Disease Prevention and Health Promotion, ed. Using Chronic Disease Data: A Handbook for Public Health Practitioners. Atlanta, GA: Centers for Disease Control and Prevention; 1992: 1–17. [Google Scholar]
- 74.Gentry EM, Kalsbeek WD, Hogelin GCet al. The behavioral risk factor surveys: II. Design, methods, and estimates from combined state data. Am J Prev Med. 1985;1(6):9–14 [PubMed] [Google Scholar]
- 75.Block G, Coyle LM, Hartman AM, Scoppa SM. Revision of dietary analysis software for the Health Habits and History Questionnaire. Am J Epidemiol. 1994;139(12):1190–1196 [DOI] [PubMed] [Google Scholar]
- 76.Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995;95(10):1103–1108 [DOI] [PubMed] [Google Scholar]
- 77.Barnard J, Rubin DB, Schenker N. Multiple imputation. : Smelser NJ, Baltes PB, International Encyclopedia of the Social and Behavioral Science. New York: Pergamon; 2001:10204–10210 [Google Scholar]
- 78.Rubin DB. Multiple imputation after 18+ years (with discussion). J Am Stat Assoc. 1996;91:473–489 [Google Scholar]
- 79.Schafer JL. Analysis of Incomplete Multivariate Data. London: Chapman & Hall; 1997 [Google Scholar]
- 80.Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182 [DOI] [PubMed] [Google Scholar]
- 81.Knofczynski GT, Mundfrom D. Sample sizes when using multiple linear regression for prediction. Educ Psychol Meas. 2008;68(3):431–442 [Google Scholar]
- 82.Trosclair A, Caraballo R, Malarcher A, Husten C, Pechacek T. 2005. Cigarette Smoking Among Adults—United States 2003. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5420a3.htm. Accessed January 8, 2012