Abstract
A stable full-length cDNA clone of the modified live virus (MLV) vaccine strain of equine arteritis virus (EAV) was developed. RNA transcripts generated from this plasmid (pEAVrMLV) were infectious upon transfection into mammalian cells, and the resultant recombinant virus (rMLV) had 100% nucleotide identity to the parental MLV vaccine strain of EAV. A single silent nucleotide substitution was introduced into the nucleocapsid gene (pEAVrMLVB), enabling the cloned vaccine virus (rMLVB) to be distinguished from parental MLV vaccine as well as other field and laboratory strains of EAV by using an allelic discrimination real-time reverse transcription (RT)-PCR assay. In vitro studies revealed that the cloned vaccine virus rMLVB and the parental MLV vaccine virus had identical growth kinetics and plaque morphologies in equine endothelial cells. In vivo studies confirmed that the cloned vaccine virus was very safe and induced high titers of neutralizing antibodies against EAV in experimentally immunized horses. When challenged with the heterologous EAV KY84 strain, the rMLVB vaccine virus protected immunized horses in regard to reducing the magnitude and duration of viremia and virus shedding but did not suppress the development of signs of EVA, although these were reduced in clinical severity. The vaccine clone pEAVrMLVB could be further manipulated to improve the vaccine efficacy as well as to develop a marker vaccine for serological differentiation of EAV naturally infected from vaccinated animals.
INTRODUCTION
Equine arteritis virus (EAV) is a single-stranded, positive-sense RNA virus in the family Arteriviridae (genus Arterivirus, order Nidovirales), which also includes porcine reproductive and respiratory syndrome virus (PRRSV), simian hemorrhagic fever virus (SHFV), and lactate dehydrogenase-elevating virus (LDV) of mice (10, 41). The EAV genome is approximately 12.7 kb and includes 5′ and 3′ untranslated regions and 10 known open reading frames (ORFs) (13, 41, 42). The first two ORFs (1a and 1b) are approximately 9.5 kb and encode two replicase polyproteins (pp1a and pp1ab) that are posttranslationally processed to yield at least 13 nonstructural proteins (Nsp1 to Nsp12, including Nsp7α and Nsp7β) required for virus replication and transcription (41, 51, 58). The remaining seven ORFs (2a, 2b, 3, 4, 5, 6, and 7) are approximately 2.9 kb and encode the envelope proteins E, GP2, GP3, GP4, GP5, M, and the nucleocapsid protein (N), respectively (41, 42). Recently, a novel small arterivirus gene (ORF5a) that overlaps the GP5 coding sequence (ORF5) that is important for virus production has been identified in all arteriviruses (13, 19).
EAV is the causative agent of equine viral arteritis (EVA) and is distributed in many equine populations throughout the world (18, 25, 36). While most EAV infections are asymptomatic or subclinical, some infected horses exhibit clinical manifestations characteristic of EVA (15, 47). The consequences of EAV infection include influenza-like illness in adult horses, abortion in pregnant mares, pneumonia and/or enteritis in young foals, and persistent infection in stallions (29, 47). Economic losses attributable to EAV infection include mainly abortion, illness, and death in young foals, the carrier state in stallions, and restricted export markets for carrier stallions as well as virus-infective semen or embryos. Experience over the past 20 years would indicate that EAV infection is of increasing significance to the $102 billion/annum horse industry in the United States (38).
A modified live virus (MLV) vaccine of EAV (ARVAC; Fort Dodge Animal Health, Fort Dodge, IA [now Pfizer Animal Health Inc., Kalamazoo, MI]) was licensed for use in North America to prevent and control EAV infection following the widespread outbreak of EVA in Kentucky in 1984. While the current MLV vaccine against EVA is safe and efficacious, the vaccine is not recommended by the manufacturer for use in pregnant mares, especially during the last 2 months of gestation, or in foals less than 6 weeks of age, unless they are at high risk of natural exposure (5, 47). Furthermore, horses that are vaccinated with the current MLV vaccine cannot be serologically distinguished from naturally infected animals. Following the 2006-2007 multistate outbreak of EVA in the United States (46, 56), there has been industry demand for a marker vaccine to distinguish naturally infected from vaccinated animals, as well as to increase the safety of the current MLV vaccine for use in pregnant mares. Availability of an infectious cDNA clone of the MLV vaccine would allow development of a marker vaccine and further improvement in the safety and efficacy of the current vaccine. An infectious cDNA clone based on the MLV vaccine strain would also be a useful tool to study EAV pathogenesis and to define genetic determinants of EAV virulence/attenuation. Here, we describe the development of a stable full-length cDNA clone of the current MLV vaccine strain of EAV. The in vitro and in vivo features of the recombinant virus derived from this infectious cDNA clone were further characterized.
MATERIALS AND METHODS
Cells and viruses.
The baby hamster kidney (BHK-21; ATCC CCL-10; Manassas, VA) and high-passage-number rabbit kidney cell line (RK-13 KY; passage levels 399 to 409) were maintained in Eagle's minimum essential medium (EMEM; Mediatech, Manassas, VA) supplemented with 10% ferritin-supplemented bovine calf serum (HyClone Laboratories, Logan, UT), 100 U/ml penicillin-streptomycin (Mediatech, Manassas, VA), and 1 μg/ml amphotericin B (Sigma-Aldrich, St. Louis, MO). Equine pulmonary artery endothelial cells (EECs) (17) were maintained in Dulbecco's modified essential medium (Mediatech, Manassas, VA) with sodium pyruvate, 10% fetal bovine serum (HyClone Laboratories, Logan, UT), 100 U/ml penicillin-streptomycin (Mediatech, Manassas, VA), and 2 mM l-glutamine (Mediatech, Manassas, VA) (3, 8, 23). The current MLV vaccine strain of EAV (ARVAC, lot number 170123A; Fort Dodge Animal Health, Ford Dodge, IA [now Pfizer Animal Health Inc., Kalamazoo, MI]) was used as the source of virus for construction of the infectious cDNA clone. Sixty archived tissue culture fluid (TCF) (20, 54, 56) samples containing various field and laboratory strains of EAV were used for extraction of RNA for developing the allelic discrimination real-time reverse transcription-PCR (rRT-PCR). The virulent KY84 strain of EAV (EAV KY84) was used as the challenge virus (11, 27, 28, 31).
Construction of infectious cDNA clones of the current MLV vaccine (ARVAC) strain of EAV.
A full-length cDNA clone of the MLV vaccine virus was generated by assembling four overlapping PCR fragments that encompass the entire genome of the vaccine virus flanked by Xba-I (5′) and Xho-I (3′) into the pTRSB vector containing the full-length genome of the virulent Bucyrus strain of EAV (pEAVrVBS) (32) (see Fig. S1 in the supplemental material). Step by step, the entire genome of the VB strain of EAV was replaced by the nucleotide sequence of the MLV vaccine strain of EAV. Primers used for reverse transcription and PCR amplification of the MLV vaccine genome are provided in Table S1 in the supplemental material. The resulting plasmid, pEAVrMLV, contained the complete EAV MLV vaccine cDNA downstream of the bacteriophage T7 RNA polymerase promoter. At the 3′ end of the viral insert, a 20-nucleotide poly(A) tail preceded the unique Xho-I restriction site that was used for linearization prior to runoff in vitro transcription.
A single nucleotide change, C→G, at the nucleotide position 12423 of the EAV MLV genome (silent mutation located on ORF7, encoding the nucleocapsid protein) was further introduced to generate the cDNA clone pEAVrMLVB by using the QuikChange II XL site-directed mutagenesis kit (Agilent, Santa Clara, CA) by following the manufacturer's instructions. The authenticity of the plasmids was confirmed by sequencing (Eurofins MWG Operon, Huntsville, AL). Sequence data were analyzed using CodonCode Aligner version 2.0.6 (CodonCode, Dedham, MA) and Vector NTI Advance 10 (Invitrogen, Carlsbad, CA).
Generation of recombinant viruses.
Capped RNA was in vitro transcribed (IVT) from the Xho-I-linearized full-length cDNA clones and transfected into either BHK-21 or EECs by electroporation as previously described (9). The cells were seeded into 25-cm2 flasks and incubated at 37°C for 72 to 96 h until complete cytopathic effect (CPE) was evident. Cell culture supernatant fluids (passage 0 [P0]) were harvested and centrifuged at 1,600 × g for 10 min at 4°C. The supernatant fluids were aliquoted and stored at −80°C. Virus stocks were titrated by standard plaque infectivity assay in the RK-13 KY cell line, and titers were expressed as PFU/ml (26). For plaque assays, overlay medium used for inoculated cultures was EMEM supplemented with 0.75% carboxymethyl-cellulose (CMC; Sigma-Aldrich, St. Louis, MO). The authenticity of these recombinant viruses (P0) was confirmed by sequencing. Recombinant viruses (P0) harvested from transfected EECs were used for in vitro and in vivo infection studies described in this paper.
Immunofluorescence assay.
The immunofluorescence assay was performed as previously described (55). Briefly, mock- or IVT RNA-transfected BHK-21 cells grown in 8-well chamber slides were fixed at 24 h posttransfection with 4% paraformaldehyde in phosphate-buffered saline (PBS; pH 7.4) and washed with PBS containing 10 mM glycine. Following permeabilization with 0.2% Triton X-100 (Sigma-Aldrich, St. Louis, MO) in PBS, slides were incubated with monoclonal antibody (MAb) 3E2 against the EAV N protein (22) or MAb 12A4 against the EAV Nsp1 protein (52), followed by Texas Red-conjugated goat anti-mouse immunoglobulin (Southern Biotechnology, Birmingham, AL). The cell nucleus was stained with Hoechst 33342 (Invitrogen, Carlsbad, CA).
Allelic discrimination real-time RT-PCR assay.
A duplexed real-time TaqMan RT-PCR assay was developed for the allelic discrimination of the cloned vaccine rMLVB (G12423) from the parental MLV vaccine strain as well as field and laboratory strains of EAV (C12423). The primers were designed to ORF7, flanking the silent nucleotide substitution, and the TaqMan MGB probes were tagged with a 6-carboxyfluorescein (FAM) (probe G) or VIC (probe C) label. Primer and probes were as follows: forward primer EAV7F, 5′GGCGACAGCCTACAAGCTACA3′; reverse primer EAV7R, 5′TGCCTAAGGTCTCCAGGCTC3′; probe G EAV7G12423, 5′FAM-ATGCGGGTCCGGAAA-MGB-NFQ-3′; and probe C EAV7C12423, 5′VIC-TGCGGGTCCGCAAA-MGB-NFQ-3′. The primers and fluorogenic TaqMan MGB probes were designed to amplify and detect a highly conserved region of ORF7 of EAV. This region was identified by comparing 208 EAV ORF7 nucleotide sequences available in GenBank. The tissue culture fluids containing the parental vaccine strain (ARVAC), the cloned vaccine virus (rMLVB), and 60 field and laboratory strains of EAV were used for RNA extraction with the QIAmp viral RNA kit (Qiagen, Valencia, CA). Reactions were performed using the TaqMan one-step RT-PCR master mix (Applied Biosystems [ABI], Foster City, CA) in a 7500 Fast real-time PCR system (ABI). Briefly, 25 μl of RT-PCR mixture for each reaction contained 12.5 μl of 2× master mix without uracil-N-glycosylase (UNG), 0.625 μl of 40× MultiScribe and RNase inhibitor mix, 1.25 μl of 20× primer-probe mix (900 nM forward and reverse primers and 250 nM probes), 5.625 μl of nuclease-free water, and 5 μl of test sample RNA. The following thermocycling conditions were used under standard mode per the manufacturer's recommendation: 30 min at 48°C, 10 min at 95°C, followed by 40 cycles at 95°C for 15 s and 60°C for 1 min.
In vitro growth characteristics and plaque morphology of recombinant viruses.
Monolayers of BHK-21 cells and EECs grown in 6-well plates were inoculated with each of the MLV and rMLVB viruses at a multiplicity of infection (MOI) of 5 and incubated at 37°C for 1 h. The inocula were aspirated off and the cell sheets washed three times with PBS (pH 7.4) to remove unbound virus and then overlaid with 4 ml of complete culture medium. This was designated time zero with respect to infection. At 0, 6, 12, 24, 48, and 72 h postinfection, supernatants were harvested and virus titers determined by plaque assay in RK-13 cells as previously described (26). The plaque morphologies/sizes of the recombinant rMLVB virus and the parental MLV vaccine strain were compared in confluent monolayers of EECs as previously described (34, 35).
Experimental vaccination of horses.
Eight EAV seronegative horses (mares, age 5 to 6 years old) were randomly assigned to two groups. Group one (n = 2 horses; animal ID numbers C7 and C11) and group two (n = 6 horses; animal ID numbers C12, C17, C19, C24, D2, and D8) horses were inoculated intramuscularly (cervical muscle) with PBS (1 ml) and cloned vaccine virus rMLVB (1.0 × 107 PFU of virus in 1 ml of PBS), respectively. Horses were observed for any adverse reactions and the appearance of clinical manifestations of EVA twice daily over the first 2 weeks after immunization and once daily for an additional 2 weeks. Blood samples were collected in buffered sodium citrate (Monojet) tubes at 0, 2, 4, 6, 8, 10, 12, and 14 days postvaccination (DPV) for hematology. Blood samples were also collected for separation of peripheral blood mononuclear cells (PBMCs) for virus isolation at 0, 2, 4, 6, 8, 10, 12, 14, 21, 28, and 35 DPV. Serum samples were collected at 0, 2, 4, 6, 8, 10, 12, 14, 21, 28, and 35 DPV for the detection of neutralizing antibodies to the virus. Nasopharyngeal swabs were collected at 0, 2, 4, 6, 8, 10, 12, 14, 21, 28, and 35 DPV for virus isolation.
Experimental challenge of horses with a heterologous strain of EAV and sample collection.
At 35 DPV, two groups of horses were intranasally challenged with 1.0 × 107 PFU of heterologous EAV KY84 strain that was delivered in 5.0 ml of EMEM using a fenestrated catheter. Horses were monitored twice daily for 4 weeks for clinical manifestations of EVA. Blood for hematology (in buffered sodium citrate [Monojet]) was collected from all horses at 0, 2, 4, 6, 8, 10, 12, and 14 days postinfection (DPI) for complete blood cell counts. Nasopharyngeal swabs and blood samples were collected at 0, 2, 4, 6, 8, 10, 12, 14, 21, 28, and 35 DPI for virus isolation and neutralizing antibody determination.
Clinical laboratory assays.
Hematological analysis was performed at the Hagyard Equine Medical Institute (4250 Iron Works Pike, Lexington, KY) using an electronic cell counter (Coulter Electronic Inc.). Differential counts were performed manually.
Virus isolation.
Virus isolation was attempted from peripheral blood mononuclear cells (PBMCs) and nasal swabs using RK-13 cells as previously described (9). The RK-13 KY cells were inoculated with serial 10-fold dilutions (100 to 105 in duplicate) of each sample and overlaid with RK-13 growth medium containing 0.75% carboxymethyl cellulose. The cells were incubated at 37°C for 5 to 7 days, and plaques were visualized by staining of the monolayer with crystal violet. A second passage was performed on negative samples at 4 to 5 days after the initial passage. Virus isolates were confirmed as EAV by real-time RT-PCR (4, 20).
Virus neutralization (VN) test.
The neutralizing antibody titers of the test sera were determined as described by Senne et al. (37, 40). Briefly, serial 2-fold dilutions of each sample from 1:4 to 1:2,048 were made in MEM (Invitrogen, Carlsbad, CA) containing 10% guinea pig complement (Rockland Immunochemicals, Gilbertsville, PA). Each serum sample was tested in duplicate in 96-well plates. Equal volumes of a virus dilution containing an estimated 50% tissue infective dose (TCID50) of 200 of the modified live virus vaccine strain of EAV (ARVAC, Fort Dodge Animal Health [now Pfizer Animal Health Inc. Kalamazoo, MI]) were added to each well, except the serum controls. The plates were shaken to ensure mixing of the well contents and then incubated for 1 h at 37°C. A suspension of RK-13 KY cells was added to each well in a volume double that of the serum-virus mixtures, and the plates were incubated for 72 h at 37°C, until viral cytopathic effect had fully developed in the virus control wells. The titer of a sample was recorded as the reciprocal of the highest serum dilution that provided at least 50% neutralization of the reference virus.
Statistical analysis.
Statistical analysis was performed with the Student t test using Sigma Plot 11 (Systat Inc., Richmond, CA).
GenBank accession numbers.
The nucleotide sequences of the full-length cDNA clones pEAVrMLV and pEAVrMLVB were deposited in GenBank under the accession numbers FJ798195 and FJ798196, respectively.
RESULTS
Construction of full-length cDNA clones of the MLV vaccine strain (ARVAC) of EAV and determination of their infectivity.
A full-length cDNA clone of the MLV vaccine strain was assembled from four overlapping PCR fragments flanked by unique restriction sites. The obtained plasmid contained a bacteriophage T7 RNA polymerase promoter at the 5′ terminus of the viral genome, the 12,704-nucleotide full-length genome of EAV MLV, and a poly(A) tail of 20 residues at the 3′ end of the genome. Compared to the genome sequence of the parental MLV vaccine strain (ARVAC) of EAV (GenBank accession number EU586275) (53), the initially assembled full-length cDNA clone contained two nucleotide differences, 3289C→T (amino acid Ser1022→Leu in Nsp3) and 3933T→G (amino acid Ser1237→Ala in Nsp4), and this initial cDNA clone was named pEAVrMLV-S1022L&S1237A (Table 1). When IVT RNA synthesized from linearized pEAVrMLV-S1022L&S1237A plasmid containing 3289T and 3933G was electroporated into BHK-21 cells and EECs, it was found to be noninfectious. Subsequently, these two sites were reverted back to 3289C and 3933T using site-specific mutagenesis either individually or together. The resulting respective full-length infectious cDNA clones were identified as pEAVrMLV-S1237A, pEAVrMLV-S1022L, and pEAVrMLV (Table 1).
Table 1.
Nucleotide and amino acid differences between the parental MLV vaccine strain (ARVAC) and the full-length vaccine cDNA clones
| Plasmid or virus name | Nt (amino acid) at position: |
Restriction site BspEI | Genome replication | Infectious virus production | ||
|---|---|---|---|---|---|---|
| 3289 | 3933 | 12423 | ||||
| MLV parental virus | C (Nsp3 Ser-1022) | T (Nsp4 Ser-1237) | C (N Arg-37) | No | Yes | Yes |
| pEAVrMLV-S1022L&S1237A | T (Nsp3 Leu-1022) | G (Nsp4 Ala-1237) | C (N Arg-37) | No | No | No |
| pEAVrMLV-S1022L | T (Nsp3 Leu-1022) | T (Nsp4 Ser-1237) | C (N Arg-37) | No | No | No |
| pEAVrMLV-S1237A | C (Nsp3 Ser-1022) | G (Nsp4 Ala-1237) | C (N Arg-37) | No | Yes | Yes |
| pEAVrMLV | C (Nsp3 Ser-1022) | T (Nsp4 Ser-1237) | C (N Arg-37) | No | Yes | Yes |
| pEAVrMLVB | C (Nsp3 Ser-1022) | T (Nsp4 Ser-1237) | G (N Arg-37) | Yes | Yes | Yes |
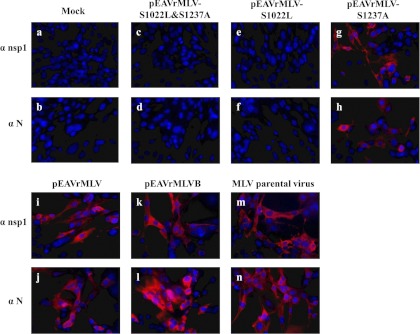
The in vitro-transcribed (IVT) full-length viral RNAs from the XhoI-linearized plasmids pEAVrMLV-S1022L&S1237A, pEAVrMLV-S1022L, pEAVrMLV-S1237A, and pEAVrMLV were then transfected into BHK-21 cells and EECs. At 24 h posttransfection, cells were examined by immunofluorescence assays using MAbs specific to the N protein and Nsp1 of EAV. As shown in Fig. 1, viral protein expressions were observed in cells transfected with pEAVrMLV-S1237A (panels g and h) or pEAVrMLV (i and j) as well as cells infected with the parental MLV vaccine strain (m and n) but were not observed in mock-transfected cells (a and b) and cells transfected with pEAVrMLV-S1022L&S1237A (c and d) or pEAVrMLV-S1022L (e and f). This showed that the reversion of 3933G→T alone did not make the IVT RNA infectious. In contrast, a clone with 3289T→C reversion alone or reversion of both substitutions (3289T→C and 3933G→T) resulted in infectious IVT RNA that led to complete CPE typical of EAV. When supernatants from the transfected cells were passaged into fresh BHK-21 cells and EECs after 96 h posttransfection, viral protein expressions and virus-specific CPE were observed in cells inoculated with supernatants from pEAVrMLV-S1237A- and pEAVrMLV-transfected cells but were not observed in cells inoculated with supernatants from pEAVrMLV-S1022L&S1237A- and pEAVrMLV-S1022L-transfected cells (data not shown). Taken together, these data demonstrated that the clones pEAVrMLV-S1022L&S1237A and pEAVrMLV-S1022L were noninfectious (no genomic replication and infectious progeny virus production), whereas the clones pEAVrMLV-S1237A and pEAVrMLV were infectious (with genomic replication and infectious progeny virus production; Table 1). The mutation on 3289C→T (Nsp3 Ser1022→Leu) is lethal, while the mutation on 3933T→G (Nsp4 Ser1237→Ala) is not critical for genomic replication and infectious virus production.
Fig 1.
Results of IFA testing of BHK-21 cells mock transfected or transfected with IVT viral RNA from various EAV cDNA clones as well as cells infected with the parental vaccine strain of EAV. At 24 h posttransfection or postinfection, cells were examined by IFA using MAb 12A4 against EAV Nsp1 protein (α nsp1) and MAb 3E2 against EAV N protein (α N) followed by Texas Red-conjugated goat anti-mouse immunoglobulin (red color). Cell nucleus was stained by Hoechst 33342 (blue color).
Full-length genomic sequencing of the recombinant viruses harvested from the transfected EECs (P0 virus) revealed that the cloned vaccine virus rMLV derived from the cDNA clone pEAVrMLV (GenBank accession number FJ798195) has 100% nucleotide identity to the previously published master sequence of the parental MLV vaccine strain of EAV (GenBank accession number EU586275). In order to distinguish the rMLV strain from the parental MLV vaccine strain, a silent point mutation was introduced into ORF7 (nucleotide 12423C→G encoding N Arg-37) of the pEAVrMLV cDNA clone to create a unique restriction site, BspEI, thus obtaining the full-length cDNA clone pEAVrMLVB (GenBank accession number FJ798196). Upon transfection into BHK-21 cells and EECs, genomic replication was observed (Fig. 1k and l), and infectious progeny virus was obtained from pEAVrMLVB-IVT RNA-transfected cells. Full-length genomic sequencing confirmed that the cloned vaccine virus rMLVB (P0) had a nucleotide sequence identical to the parental MLV vaccine virus except for the single nucleotide substitution at nucleotide 12423; the cloned vaccine virus rMLVB was genetically stable after 10 passages in BHK-21 cells. A 710-bp RT-PCR fragment amplified from nucleotides 11893 to 12603 was cleaved by BspEI in the cloned vaccine virus rMLVB (P0, P5, and P10) but was not cleaved by BspEI in the parental MLV vaccine virus and the recombinant rMLV virus (Fig. 2). These clearly demonstrated that the single nucleotide substitution is stable during serial passage in cell culture.
Fig 2.
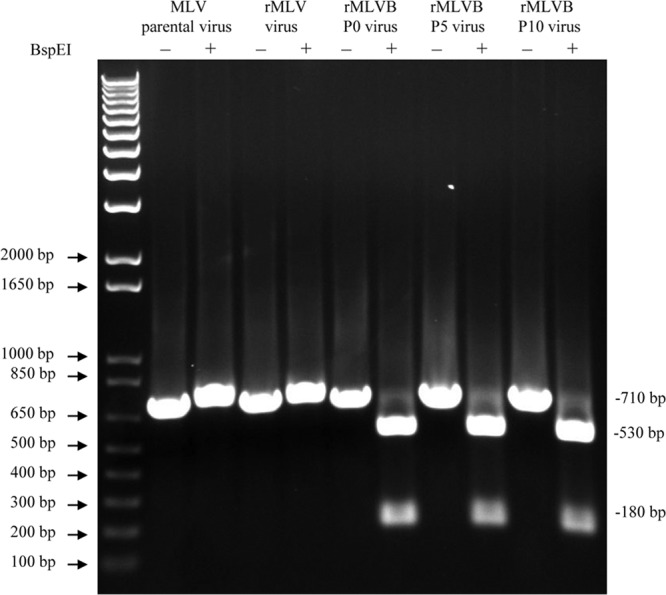
Differentiation between cloned viruses and the parental EAV MLV vaccine strain. A BspEI restriction site was introduced into the full-length cDNA clone for distinguishing the cloned virus rMLVB from the parental MLV virus. A 710-bp RT-PCR fragment containing the BspEI site was amplified and then digested with BspEI. The presence of a BspEI site resulted in fragments of 530 bp and 180 bp after digestion with BspEI.
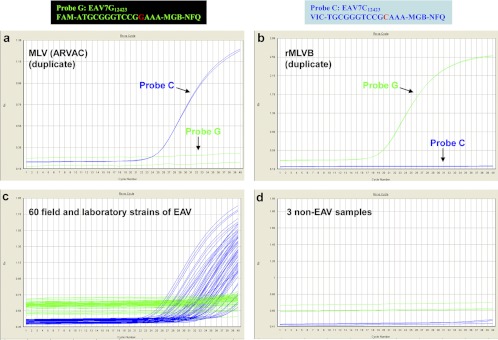
Allelic discrimination real-time RT-PCR assay.
The parental MLV vaccine strain as well as all of the field isolates of EAV had a conserved nucleotide C at position 12423, whereas the cloned vaccine virus rMLVB had a G at this position; therefore, this was used as a unique genetic marker to distinguish the cloned vaccine virus rMLVB from the parental MLV vaccine strain and field isolates of EAV. While the BspEI cleavage assay based on this unique genetic marker at position 12423 is able to distinguish the cloned vaccine virus rMLVB from field isolates of EAV, the assay is laborious and time-consuming. Accordingly, an allelic discrimination real-time RT-PCR assay based on the single nucleotide difference at position 12423 was developed to fulfill this need. The parental MLV vaccine strain (ARVAC) was recognized by probe C but not by probe G (Fig. 3a); in contrast, the cloned vaccine virus rMLVB was recognized by probe G but not by probe C (Fig. 3b). Further analysis of 60 field and laboratory strains of EAV indicated that these strains were also recognized only by probe C but not by probe G (Fig. 3c). Negative control samples were neither recognized by probe C nor by probe G (Fig. 3d).
Fig 3.
An allelic discrimination real-time RT-PCR assay for distinguishing cloned virus rMLVB from parental MLV vaccine virus as well as field and laboratory strains of EAV.
In vitro growth of the cloned vaccine virus.
The cloned rMLVB virus and the parental MLV vaccine virus had identical growth kinetics in either EECs or BHK21 cells (Fig. 4a). Titers peaked at 24 to 48 hpi for both viruses, with maximal titers of ∼4 × 108 PFU/ml. Plaque morphology of these two viruses was also determined, and the plaque size produced by the cloned rMLVB virus was very similar to that of the parental MLV (Fig. 4b). These results indicate that the cloned vaccine virus rMLVB possesses in vitro properties similar to those of the parental MLV vaccine virus.
Fig 4.
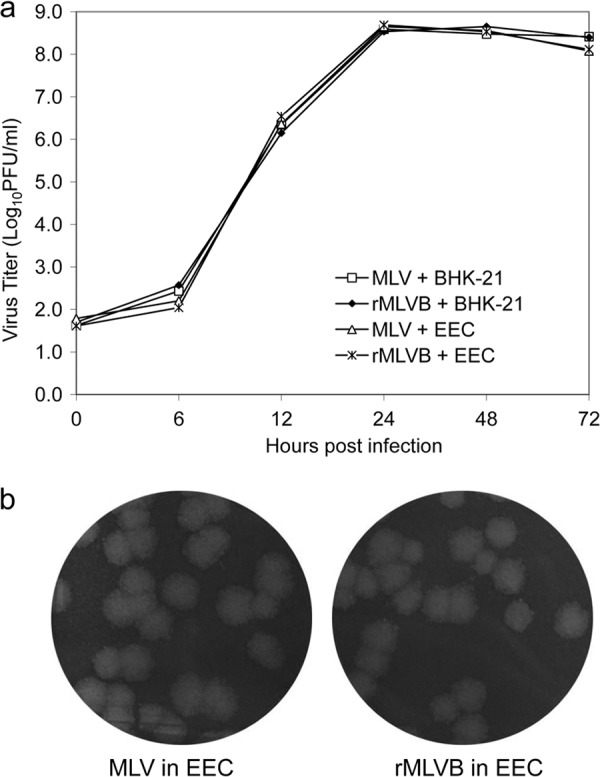
Growth kinetics of cloned virus and parental virus. BHK-21 cells and EECs grown in 6-well plates were infected with the parental MLV vaccine virus and the cloned rMLVB virus at an MOI of 5. (a) At 0, 6, 12, 24, 48, and 72 hpi, supernatants were harvested and virus titers were determined by plaque assay in RK-13 cells. (b) Plaque morphology of the cloned rMLVB virus and parental MLV virus in EECs. Cells were stained with 0.2% crystal violet at 72 hpi.
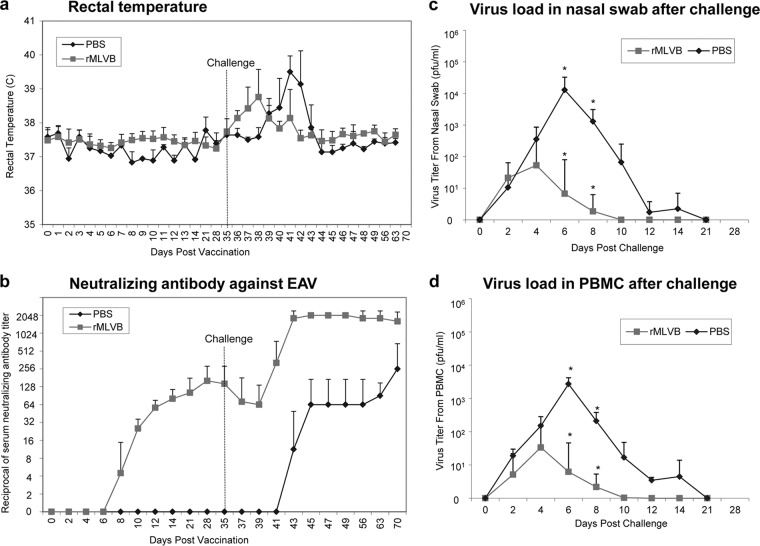
Safety and the immunogenicity of the rMLVB vaccine strain of EAV.
Eight EAV seronegative horses were randomly assigned into two groups and inoculated intramuscularly with PBS or rMLVB virus, respectively (PBS control group one, n = 2 horses; rMLVB virus group two, n = 6 horses). Experimentally vaccinated horses were monitored up to 35 days postvaccination. All horses inoculated with PBS or rMLVB virus remained healthy and did not show any adverse effects after vaccination. The rectal temperature of all horses remained within the normal range of 36.6 to 38.0°C up to 35 days postvaccination (Fig. 5a). Results of virus isolation from PBMCs and nasal swabs after vaccination are summarized in Table 2. No virus was isolated from PBMCs and nasal swabs of the two horses inoculated with PBS. Among the 6 horses vaccinated with the rMLVB virus, very low levels of viremia (2 PFU/ml) were observed in two horses only on day 2 postvaccination; very low levels of transient nasal virus shedding (1 to 2 PFU/ml) were observed in three horses (duration of 1 day in two horses and 2 days in one horse). Sequencing of structural protein genes of these recovered viruses revealed that the single point mutation (12423C→G) introduced to ORF7 was stably maintained in all of the viruses isolated from the immunized horses. Horses inoculated with PBS did not develop neutralizing antibodies to EAV up to 35 days postvaccination, whereas all six horses immunized with rMLVB virus developed substantial titers (maximal titers ranged from 1:128 to 1:256) of neutralizing antibodies to EAV (Fig. 5b). The data clearly indicate that the rMLVB vaccine virus is very safe in horses and is able to induce significant titers of neutralizing antibodies to EAV.
Fig 5.
Experimental vaccination and challenge of horses. Group one (n = 2) and group two (n = 6) horses were intramuscularly inoculated with PBS or vaccinated with the cloned rMLVB virus (1 × 107 PFU), respectively. At 35 days postvaccination, all horses were challenged with a heterologous EAV KY84 strain (1 × 107 PFU). (a) Rectal temperature after vaccination and challenge; (b) neutralizing antibody titers to EAV after vaccination and challenge; (c) virus isolation results from nasal swabs after challenge; (d) virus isolation results from PBMCs after challenge; viral loads with significant difference are indicated by the asterisk.
Table 2.
Results of attempts to isolate virus in RK-13 cells from nasal swab and PBMCs of horses after experimental vaccination with PBS or rMLVB virus
| Horse ID | Vaccination | Specimen | Days postvaccinationa |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| −3 | 0 | 2 | 4 | 6 | 8 | 10 | 12 | 14 | 21 | 28 | 35 | |||
| C7 | PBS | Nasal swab | − | − | − | − | − | − | − | − | − | − | − | − |
| PBS | PBMCs | − | − | − | − | − | − | − | − | − | − | − | − | |
| C11 | PBS | Nasal swab | − | − | − | − | − | − | − | − | − | − | − | − |
| PBS | PBMCs | − | − | − | − | − | − | − | − | − | − | − | − | |
| C12 | rMLVB | Nasal swab | − | − | − | − | − | − | − | − | − | − | − | − |
| rMLVB | PBMCs | − | − | − | − | − | − | − | − | − | − | − | − | |
| C17 | rMLVB | Nasal swab | − | − | − | − | − | − | − | − | − | − | − | − |
| rMLVB | PBMCs | − | − | 2 PFU/ml | − | − | − | − | − | − | − | − | − | |
| C19 | rMLVB | Nasal swab | − | − | − | − | − | − | − | − | − | − | − | − |
| rMLVB | PBMCs | − | − | − | − | − | − | − | − | − | − | − | − | |
| C24 | rMLVB | Nasal swab | − | − | − | 2 PFU/ml | − | − | − | − | − | − | − | − |
| rMLVB | PBMCs | − | − | − | − | − | − | − | − | − | − | − | − | |
| D2 | rMLVB | Nasal swab | − | − | 1 PFU/ml | − | − | − | − | − | − | − | − | − |
| rMLVB | PBMCs | − | − | + | − | − | − | − | − | − | − | − | − | |
| D8 | rMLVB | Nasal swab | − | − | − | 2 PFU/ml | 2 PFU/ml | − | − | − | − | − | − | − |
| rMLVB | PBMCs | − | − | 2 PFU/ml | − | − | − | − | − | − | − | − | − | |
−, virus isolation negative; +, virus isolated only after second passage in cell culture.
Protective efficacy of the rMLVB vaccine in horses.
The ability of the recombinant vaccine virus rMLVB to protect immunized horses against EVA was evaluated by experimental challenge using the heterologous KY84 strain of EAV (1 × 107 PFU intranasally) at 35 days postvaccination. Two horses inoculated with PBS developed moderate to severe clinical signs of EVA after intranasal challenge with EAV KY84. These two horses became febrile, typically from 4 to 8 days postchallenge (DPC), with maximum temperatures ranging from 39.2 to 39.8°C (Fig. 5a); both horses developed moderate to severe dependent edema starting from 4 to 6 days postchallenge and persisting for 7 to 9 days and affecting all four limbs. Following intranasal challenge, six horses vaccinated with rMLVB vaccine virus also became febrile, starting from 1 to 3 days postchallenge and lasting for 1 to 3 days, with maximum temperatures ranging from 38.3 to 39.9°C (Fig. 5a); all horses developed moderate edema on both hind limbs that started from 4 to 7 days postchallenge and lasted for 3 to 9 days. However, duration of viremia was shorter, and the virus titers in PBMCs and nasal secretions were lower in rMLVB-immunized horses than in the PBS-inoculated horses (Fig. 5c and d). Virus load differences in nasal secretions were significant at 6 DPC (P = 0.0012) and 8 DPC (P = 0.0069) and in PBMCs at 6 DPC (P = 0.0005) and 8 DPC (P = 0.0046). Whereas the PBS-inoculated horses seroconverted by 8 days postchallenge, the rMLVB-immunized horses developed significantly higher titers (≥2,048) of neutralizing antibodies to EAV by 8 days postchallenge (Fig. 5b).
DISCUSSION
In this study, the development of an infectious cDNA clone of the current MLV vaccine strain (ARVAC) of EAV was described. When electroporated, IVT RNA from a first assembled full-length cDNA clone was noninfectious due to a single nonsynonymous nucleotide substitution in the Nsp3 coding region of ORF1a (resulting in an Ser1022→Leu substitution in Nsp3). It has been previously shown that arterivirus Nsp3 plays a critical role in membrane modification and double membrane vesicle (DMV) formation during the early virus replication cycle (12, 39, 43). Substitutions of each of a cluster of four conserved cysteine residues, residing in a predicted luminal loop of Nsp3, completely blocked DMV formation. Some of these mutant Nsp3 proteins were also found to be highly cytotoxic, in particular, by exerting a dramatic effect on the endoplasmic reticulum. Furthermore, it has been reported that these cysteine mutants also affect the pp1a autoprocessing. Interestingly, the lethal mutation (Ser1022→Leu) in our infectious cDNA clone was located in the cytoplasmic tail of the Nsp3 protein; currently, it is not clear how this mutation adversely affected replication of the virus. Once this lethal mutation was removed and transcripts from the new full-length clone pEAVrMLV were electroporated, CPE typical of EAV infection supervened. Subsequently, a translationally silent marker mutation was introduced into the ORF7 region of pEAVrMLV, thereby creating a unique BspEI restriction site. The clone carrying this genetic marker, pEAVrMLVB, was used for additional in vitro and in vivo studies. The companion allelic discrimination rRT-PCR that was developed allows for differentiation of the recombinant MLV vaccine from field strains of EAV and facilitates molecular epidemiological investigations of reported vaccine-associated outbreaks of EVA. Stability of the recombinant virus was further established by sequential cell culture passage of the virus, confirming presence of the unique BspEI restriction site following 10 serial passages. In summary, the infectious cDNA clone derived from the current MLV vaccine strain is identical to the wild-type virus with the exception of the single nucleotide substitution introduced at position 12423 in ORF7. The recombinant vaccine virus has the same in vitro phenotypic properties as the parental commercial MLV vaccine.
The safety and efficacy of the rMLVB vaccine were evaluated by experimental vaccination and challenge with the heterologous KY84 field strain of EAV. The serologic response of the horses vaccinated with rMLVB was identical to that observed in horses vaccinated with the commercial vaccine virus as previously described (44, 45). There was no adverse effect on the safety and induction of the humoral immune response resulting from incorporation of a single noncoding (synonymous) nucleic acid substitution in ORF7. Similar to the unmodified MLV vaccine studies (44, 50), a very small amount of infectious virus (<2 PFU/ml) was transiently detected in nasal secretions and in the PBMCs of the vaccinated horses within the first week after immunization. Collectively, these data prove that the recombinant virus is very similar, if not identical, to the unmodified commercial MLV vaccine virus in regard to virus shedding pattern and its ability to stimulate a humoral antibody response. Compared to the control animals, the horses vaccinated with rMLVB developed significantly reduced levels of viremia and shorter duration of virus shedding after challenge with the heterologous EAV KY84 strain. However, the level of protection afforded by vaccination did not completely protect horses from developing clinical signs of EVA following challenge with this heterologous strain even though the responses were of lesser clinical severity. While it is believed there is only one known serotype of EAV, field strains differ in their neutralization phenotype (1, 6, 7, 21, 33, 56, 57). With the exception of a few EAV field stains (2, 7, 56), the majority of the field strains are neutralized to a higher titer (1:64 to 1:1,024) by polyclonal antiserum raised against the virulent Bucyrus strain of EAV (EAV VBS). In contrast, it has been shown previously that the serum from horses vaccinated with the MLV vaccine strain neutralizes some EAV field strains to a lower titer (1:8 to 1:64) (1, 7, 16, 56); this includes the EAV KY84 strain used in this study. This may explain why horses were not completely protected from developing clinical signs of EVA following challenge with the heterologous EAV KY84 strain. Furthermore, equine antiserum against the prototype EAV VBS neutralizes the EAV KY84 to a higher titer (1:64 to 1:256) (1, 7, 56), and horses vaccinated with a subunit vaccine containing the GP5 and M heterodimer of the EAV VBS were well protected when challenged with the same KY84 strain of EAV (3). This further confirms the importance of high-titer neutralizing antibodies (≥1:64) in protecting against the clinical signs of EAV infection (14, 50). It is also possible that the very high challenge virus dose (1.0 × 107 PFU) used in this study increased the likelihood of a clinical response in the vaccinated horses. It should be emphasized that the commercial MLV vaccine had been successfully used to control several major EVA outbreaks in the United States in the past 20 to 25 years (24, 30, 46, 48–50). These data also emphasize the importance of conducting additional in-depth cross-neutralization studies using more recent EAV isolates representing all three phylogenetic clades of EAV (North American and two European [EU-1 and EU-2]). It remains to be seen whether more heterologous challenge studies of horses vaccinated with the commercial MLV are indicated. The infectious cDNA clone of the MLV vaccine strain of EAV described in this study could be used to design and to develop more broadly protective recombinant MLV vaccines by systematically incorporating key neutralization epitopes from various EAV isolates of significantly distinct neutralization phenotypes.
In summary, we have generated an infectious cDNA clone of the current MLV vaccine strain with a unique nucleotide mutation in ORF7 to distinguish recombinant vaccine virus from laboratory and field strains of EAV using a companion real-time RT-PCR assay. The vaccine clone pEAVrMLVB could be further genetically manipulated to develop a marker vaccine by either deleting an immunogenic viral epitope(s) to create a negative marker or by inserting a foreign antigenic epitope(s) to create a positive marker. Companion serological assays can be developed to detect antibody responses to the deleted immunogenic viral epitope(s) or to the inserted foreign antigenic epitope(s). Such a marker vaccine would provide a means of serologically differentiating EAV naturally infected from vaccinated animals by using the companion serologic assays. Furthermore, this infectious cDNA clone could be used to design and develop a rational, broadly protective recombinant vaccine(s) by genetically engineering the immunodominant neutralizing epitopes from EAV strains that differ in their neutralization phenotypes. We previously developed an infectious cDNA clone (pEAVrVBS) from the virulent Bucyrus strain of EAV (8). The virulent pEAVrVBS clone and the attenuated vaccine clone pEAVrMLVB provide valuable research tools to study the life cycle of the virus (attachment, entry, replication, transcription, translation, and assembly) and viral pathogenesis, as well as the immune response to the virus.
Supplementary Material
ACKNOWLEDGMENT
We are grateful to Fort Dodge Animal Health Laboratories (now Pfizer Animal Health Inc., Kalamazoo, MI) for providing financial support for this study.
Footnotes
Published ahead of print 27 June 2012
Supplemental material for this article may be found at http://cvi.asm.org/.
REFERENCES
- 1. Balasuriya UB, et al. 2004. Characterization of the neutralization determinants of equine arteritis virus using recombinant chimeric viruses and site-specific mutagenesis of an infectious cDNA clone. Virology 321:235–246 [DOI] [PubMed] [Google Scholar]
- 2. Balasuriya UB, et al. 1998. Serologic and molecular characterization of an abortigenic strain of equine arteritis virus isolated from infective frozen semen and an aborted equine fetus. J. Am. Vet. Med. Assoc. 213:1586–1589 [PubMed] [Google Scholar]
- 3. Balasuriya UB, et al. 2002. Alphavirus replicon particles expressing the two major envelope proteins of equine arteritis virus induce high level protection against challenge with virulent virus in vaccinated horses. Vaccine 20:1609–1617 [DOI] [PubMed] [Google Scholar]
- 4. Balasuriya UB, et al. 2002. Detection of equine arteritis virus by real-time TaqMan reverse transcription-PCR assay. J. Virol. Methods 101:21–28 [DOI] [PubMed] [Google Scholar]
- 5. Balasuriya UB, MacLachlan NJ. 2004. The immune response to equine arteritis virus: potential lessons for other arteriviruses. Vet. Immunol. Immunopathol. 102:107–129 [DOI] [PubMed] [Google Scholar]
- 6. Balasuriya UB, Maclachlan NJ, De Vries AA, Rossitto PV, Rottier PJ. 1995. Identification of a neutralization site in the major envelope glycoprotein (GL) of equine arteritis virus. Virology 207:518–527 [DOI] [PubMed] [Google Scholar]
- 7. Balasuriya UB, et al. 1997. Neutralization determinants of laboratory strains and field isolates of equine arteritis virus: identification of four neutralization sites in the amino-terminal ectodomain of the G(L) envelope glycoprotein. Virology 232:114–128 [DOI] [PubMed] [Google Scholar]
- 8. Balasuriya UB, et al. 2007. Development and characterization of an infectious cDNA clone of the virulent Bucyrus strain of equine arteritis virus. J. Gen. Virol. 88:918–924 [DOI] [PubMed] [Google Scholar]
- 9. Balasuriya UB, et al. 1999. Equine arteritis virus derived from an infectious cDNA clone is attenuated and genetically stable in infected stallions. Virology 260:201–208 [DOI] [PubMed] [Google Scholar]
- 10. Cavanagh D. 1997. Nidovirales: a new order comprising Coronaviridae and Arteriviridae. Arch. Virol. 142:629–633 [PubMed] [Google Scholar]
- 11. Cole JR, et al. 1986. Transmissibility and abortogenic effect of equine viral arteritis in mares. J. Am. Vet. Med. Assoc. 189:769–771 [PubMed] [Google Scholar]
- 12. Fang Y, Snijder EJ. 2010. The PRRSV replicase: exploring the multifunctionality of an intriguing set of nonstructural proteins. Virus Res. 154:61–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Firth AE, et al. 2011. Discovery of a small arterivirus gene that overlaps the GP5 coding sequence and is important for virus production. J. Gen. Virol. 92:1097–1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fukunaga Y, McCollum WH. 1977. Complement-fixation reactions in equine viral arteritis. Am. J. Vet. Res. 38:2043–2046 [PubMed] [Google Scholar]
- 15. Glaser AL, Chirnside ED, Horzinek MC, de Vries AA. 1997. Equine arteritis virus. Theriogenology 47:1275–1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Go YY. 2011. Molecular and genomic approaches to understanding host-virus interactions in shaping the outcome of equine arteritis virus infection. University of Kentucky, Lexington, KY [Google Scholar]
- 17. Hedges JF, et al. 2001. Characterization of equine E-selectin. Immunology 103:498–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huntington PJ, Forman AJ, Ellis PM. 1990. The occurrence of equine arteritis virus in Australia. Aust. Vet. J. 67:432–435 [DOI] [PubMed] [Google Scholar]
- 19. Johnson CR, Griggs TF, Gnanandarajah J, Murtaugh MP. 2011. Novel structural protein in porcine reproductive and respiratory syndrome virus encoded by an alternative ORF5 present in all arteriviruses. J. Gen. Virol. 92:1107–1116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lu Z, et al. 2008. Comparison of two real-time reverse transcription polymerase chain reaction assays for the detection of equine arteritis virus nucleic acid in equine semen and tissue culture fluid. J. Vet. Diagn. Invest. 20:147–155 [DOI] [PubMed] [Google Scholar]
- 21. MacLachlan NJ, Balasuriya UB. 2006. Equine viral arteritis. Adv. Exp. Med. Biol. 581:429–433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. MacLachlan NJ, et al. 1998. Serologic response of horses to the structural proteins of equine arteritis virus. J. Vet. Diagn. Invest. 10:229–236 [DOI] [PubMed] [Google Scholar]
- 23. MacLachlan NJ, et al. 1996. Fatal experimental equine arteritis virus infection of a pregnant mare: immunohistochemical staining of viral antigens. J. Vet. Diagn. Invest. 8:367–374 [DOI] [PubMed] [Google Scholar]
- 24. McCollum WH. 1970. Vaccination for equine viral arteritis, p 143–151 In Bryans JT, Gerber H. (ed), Proceedings of the Second International Conference on Equine Infectious Diseases, Paris 1969 S. Karger, Basel, Switzerland [Google Scholar]
- 25. McCollum WH, Bryans JT. 1973. Serological identification of infection by equine arteritis virus in horses of several countries, p 256–263 In Bryans JT, Gerber H. (ed), Proceedings of the 3rd International Conference on Equine Infectious Diseases, Paris, 1972 S. Karger, Basel, Switzerland [Google Scholar]
- 26. McCollum WH, Doll ER, Wilson JC, Cheatham J. 1962. Isolation and propagation of equine arteritis virus in monolayer cell cultures of rabbit kidney. Cornell Vet. 52:452–458 [PubMed] [Google Scholar]
- 27. McCollum WH, Timoney PJ. 1999. Experimental observation on the virulence of isolates of equine arteritis virus, p 558–559 In Wernery U, Wade JF, Mumford JA, Kaaden OR. (ed), Proceedings of the 8th International Conference on Equine Infectious Diseases Dubai, United Arab Emirates, 1998 R & W Publications, Newmarket, United Kingdom [Google Scholar]
- 28. McCollum WH, Timoney PJ. 1984. The pathogenic qualities of the 1984 strain of equine arteritis virus, p 34–84 In Proceedings of the Grayson Foundation International Conference of Thoroughbred Breeders Organizations, Ireland [Google Scholar]
- 29. McCollum WH, et al. 1999. Features of an outbreak of equine viral arteritis on a breeding farm associated with abortion and fatal interstitial pneumonia in neonatal foals, p 559–560 In Wernery U, Wade JF, Mumford JA, Kaaden OR. (ed), Proceedings of the 8th International Conference on Equine Infectious Diseases, Dubai, United Arab Emirates, 1998 R & W Publications, Newmarket, United Kingdom [Google Scholar]
- 30. McCollum WH, Timoney PJ, Roberts AW. 1988. Response of vaccinated and non-vaccinated mares to artificial insemination with semen from stallions persistently infected with equine arteritis virus, p 13–18 In Powell DG. (ed), Proceedings of the Fifth International Conference on Equine Infectious Diseases, Lexington, KY, 1987 University of Kentucky Press, Lexington, KY [Google Scholar]
- 31. McCollum WH, Timoney PJ, Tengelsen LA. 1995. Clinical, virological and serological responses of donkeys to intranasal inoculation with the KY-84 strain of equine arteritis virus. J. Comp. Pathol. 112:207–211 [DOI] [PubMed] [Google Scholar]
- 32. McKnight KL, et al. 1996. Deduced consensus sequence of Sindbis virus strain AR339: mutations contained in laboratory strains which affect cell culture and in vivo phenotypes. J. Virol. 70:1981–1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Miszczak F, et al. 2012. Emergence of novel equine arteritis virus (EAV) variants during persistent infection in the stallion: origin of the 2007 French EAV outbreak was linked to an EAV strain present in the semen of a persistently infected carrier stallion. Virology 423:165–174 [DOI] [PubMed] [Google Scholar]
- 34. Moore BD, Balasuriya UB, Hedges JF, MacLachlan NJ. 2002. Growth characteristics of a highly virulent, a moderately virulent, and an avirulent strain of equine arteritis virus in primary equine endothelial cells are predictive of their virulence to horses. Virology 298:39–44 [DOI] [PubMed] [Google Scholar]
- 35. Moore BD, et al. 2003. Differentiation of strains of equine arteritis virus of differing virulence to horses by growth in equine endothelial cells. Am. J. Vet. Res. 64:779–784 [DOI] [PubMed] [Google Scholar]
- 36. Moraillon A, Moraillon R. 1978. Results of an epidemiological investigation on viral arteritis in France and some other European and African countries. Ann. Rech. Vet. 9:43–54 [PubMed] [Google Scholar]
- 37. OIE 2004. OIE manual of diagnostic tests and vaccines for terrestrial animals, 5th ed, vol 2 Office International des Epizooties, Paris, France [Google Scholar]
- 38. Owens A. 2005. American horsepower: the economic impact of the horse industry on the United States, p 1–19 American Horse Council, Washington, DC [Google Scholar]
- 39. Posthuma CC, et al. 2008. Formation of the arterivirus replication/transcription complex: a key role for nonstructural protein 3 in the remodeling of intracellular membranes. J. Virol. 82:4480–4491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Senne DA, Pearson JE, Carbrey EA. 1985. Equine viral arteritis: a standard procedure for the virus neutralization test and comparison of results of a proficiency test performed at five laboratories, p 29–34 In Proceedings of the 89th Annual Meeting of the United States Animal Health Association, 27 October to 1 November 1985, Milwaukee, WI [Google Scholar]
- 41. Snijder EJ, Meulenberg JJ. 1998. The molecular biology of arteriviruses. J. Gen. Virol. 79(Pt 5):961–979 [DOI] [PubMed] [Google Scholar]
- 42. Snijder EJ, van Tol H, Pedersen KW, Raamsman MJ, de Vries AA. 1999. Identification of a novel structural protein of arteriviruses. J. Virol. 73:6335–6345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Snijder EJ, van Tol H, Roos N, Pedersen KW. 2001. Non-structural proteins 2 and 3 interact to modify host cell membranes during the formation of the arterivirus replication complex. J. Gen. Virol. 82:985–994 [DOI] [PubMed] [Google Scholar]
- 44. Summers-Lawyer KA, et al. 2011. Response of stallions to primary immunization with a modified live equine viral arteritis vaccine. J. Equine Veterinary Sci. 31:129–138 [Google Scholar]
- 45. Timoney P, et al. 2007. The outcome of vaccinating five pregnant mares with a commercial equine viral arteritis vaccine. Equine Vet. Educ. 19:606–611 [Google Scholar]
- 46. Timoney PJ, et al. 2006. Multi-state occurrence of EVA. Report of the Committee on Infectious Diseases of Horses: addressing equine viral arteritis in the United States, p 354–362 Proceedings of the 110th annual meeting of the United States Animal Health Association Pat Campbell & Associates and Spectrum Press, Minneapolis, MN [Google Scholar]
- 47. Timoney PJ, McCollum WH. 1993. Equine viral arteritis. Vet. Clin. North Am. Equine Pract. 9:295–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Timoney PJ, McCollum WH, Roberts AW, McDonald MJ. 1987. Status of equine viral arteritis in Kentucky for 1986. Vet. Rec. 120:282. [DOI] [PubMed] [Google Scholar]
- 49. Timoney PJ, McCollum WH, Roberts AW, McDonald MJ. 1987. Status of equine viral arteritis in Kentucky, 1985. J. Am. Vet. Med. Assoc. 191:36–39 [PubMed] [Google Scholar]
- 50. Timoney PJ, Umphenour NW, McCollum WH. 1988. Safety evaluation of a commercial modified live equine arteritis virus vaccine for use in stallions, p 19–27 In Powell DG. (ed), Proceedings of the Fifth International Conference on Equine Infectious Diseases, Lexington, KY, 1987 University of Kentucky Press, Lexington, KY [Google Scholar]
- 51. van Aken D, Zevenhoven-Dobbe J, Gorbalenya AE, Snijder EJ. 2006. Proteolytic maturation of replicase polyprotein pp1a by the nsp4 main proteinase is essential for equine arteritis virus replication and includes internal cleavage of nsp7. J. Gen. Virol. 87:3473–3482 [DOI] [PubMed] [Google Scholar]
- 52. Wagner HM, Balasuriya UB, MacLachlan NJ. 2003. The serologic response of horses to equine arteritis virus as determined by competitive enzyme-linked immunosorbent assays (c-ELISAs) to structural and non-structural viral proteins. Comp. Immunol. Microbiol. Infect. Dis. 26:251–260 [DOI] [PubMed] [Google Scholar]
- 53. Zhang J, et al. 2008. Amino acid substitutions in the structural or nonstructural proteins of a vaccine strain of equine arteritis virus are associated with its attenuation. Virology 378:355–362 [DOI] [PubMed] [Google Scholar]
- 54. Zhang J, et al. 2007. Genetic variation and phylogenetic analysis of 22 French isolates of equine arteritis virus. Arch. Virol. 152:1977–1994 [DOI] [PubMed] [Google Scholar]
- 55. Zhang J, Timoney PJ, MacLachlan NJ, McCollum WH, Balasuriya UB. 2008. Persistent equine arteritis virus infection in HeLa cells. J. Virol. 82:8456–8464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zhang J, et al. 2010. Molecular epidemiology and genetic characterization of equine arteritis virus isolates associated with the 2006-2007 multistate disease occurrence in the U.S.A. J. Gen. Virol. 91:2286–2301 [DOI] [PubMed] [Google Scholar]
- 57. Zhang J, Timoney PJ, MacLachlan NJ, Balasuriya UBR. 2008. Identification of an additional neutralization determinant of equine arteritis virus. Virus Res. 138(1–2):150–153 [DOI] [PubMed] [Google Scholar]
- 58. Ziebuhr J, Snijder EJ, Gorbalenya AE. 2000. Virus-encoded proteinases and proteolytic processing in the Nidovirales. J. Gen. Virol. 81:853–879 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.