Abstract
This study investigates that role of area economic characteristics in predicting employment, a key aspect of social participation for adults with physical disabilities, using data from a national registry of persons with spinal cord injury (SCI). SCI results in chronic impairment and most commonly occurs during young adulthood when working is a key aspect of the adult social role. Geocoded data was collected from two of the 14 SCI Model Systems (SCIMS) centers involved in the National SCIMS database and used to link individual-level data with area-level measures extracted from the 2000 US Census. The analysis included participants of working age (18–64 years) and living in the community (N=1,013). Hierarchical generalized linear modeling was used to estimate area-level variation in participation and the relative contribution of area-level economic indicators, adjusted for individual-level health, functioning, and background characteristics. The likelihood of employment for adults with SCI varied by area and was associated with area SES and ubanicity, but not area unemployment. These findings suggest that variation in area economic conditions may affect the feasibility of employment for persons who experience chronic physical disability during adulthood, thus limiting full participation in society.
Keywords: Spinal cord injury, Physical Disability, Participation, Employment, Area effects, USA
Introduction
Employment is a key aspect of social participation and a well-documented social determinant of health for persons with disabilities (Kirsh et al., 2009). Despite decades of public policy and research focused on understanding and eliminating the barriers to employment, persons with disabilities remain underrepresented in the American workforce (Anderson et al., 2007; Moon & Shin, 2006). In 2009, approximately 19% of disabled versus 65% of non-disabled adults were employed (US Department of Labor, 2010) and recent reports suggested that the widespread unemployment of the recent economic downturn disproportionally affected persons with disabilities (Kaye, 2010). Research concerning the environmental predictors of employment for adults with disabilities has largely focused on structural (i.e., workplace accessibility and accommodations) and attitudinal (i.e., employer discrimination) factors. To our knowledge, few studies have investigated whether the feasibility of working for persons with disabilities depends on, in part, upon where they live.
This investigation explored the role of economic differences across geographic areas on employment for adults with chronic spinal cord injury (SCI). SCI results in the sudden and permanent loss of mobility and other physical functions that can limit independence and social participation. Employment is a particularly salient aspect of participation for this population. The average age at injury has reported to be 37 years (DeVivo & Chen, 2011), with the majority of these injuries occurring in the 16 to 30 year age group (Jackson et al., 2004). In other words, SCI most commonly occurs among young and working age adults, thus coinciding with the formative period of the lifecourse for career development. Employment post-injury has been estimated between 11– 35% (Krause, 2001; National Spinal Cord Injury Statistical Center, 2011). Although the incidence rate of SCI in the United States has been relatively low—approximately 12,000 new injuries are reported to occur annually—the number of people surviving SCI has continued to increase (DeVivo, 2011). Therefore, improving social integration for this population remains a key goal for healthcare professionals, policymakers, and disability advocates alike.
Research has documented that apart from mobility, economic self-sufficiency and occupational functioning are the most disrupted dimensions of independence for adults with SCI (Kirsh et al., 2009), which consequently has negative socioeconomic implications for individuals, their families, and society (Lidal et al., 2007). The downward social mobility elicited by discontinued or interrupted employment following a chronic condition can place individuals at increased risk for further health problems. Unemployment after SCI increases the risk for health complications (Yasuda et al., 2002) and complicates the recovery of identity and autonomy (Ville, 2005). Conversely, paid employment and other types of participation have been linked to higher life expectancy (Krause et al., 2004), functional outcomes (Kirsh et al., 2009), and quality of life (Chapin & Holbert, 2010; Yasuda et al., 2002). In short, empirical research has suggested that returning to work significantly benefits the health and well-being of this population.
The relationship between community socioeconomic (SES) factors in health outcomes has well established (Robert, 1999) and there substantial evidence has demonstrated that geographic variation in SES disadvantage has contributed to a range of negative physical, emotional, and social outcomes for persons with disabilities. Neighborhood indicators of economic hardship and SES disadvantage have been linked to poor self-rated health for persons with intellectual disabilities (Emerson & Hatton, 2007), functioning and activity limitations among physically and cognitively impaired adults (Corrigan & Bognar, 2008), and physical impairment among older adults (Freedman et al., 2008). Similarly, area-level economic inactivity (Fone et al., 2007) and high unemployment (Zunzunegui et al., 2006) have been linked to poor physical and mental health outcomes among persons with disabilities and other vulnerable groups.
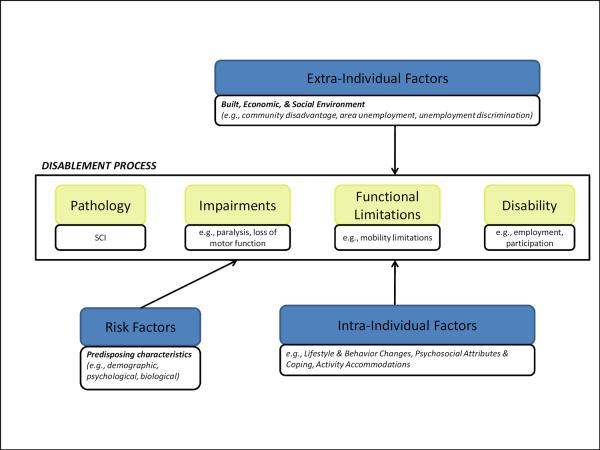
Although there has been an extensive body of research examining the predictors and correlates of employment following SCI, work in this area is largely confined to the role of individual background characteristics (e.g., race, age, and education level), resources (e.g., autonomous transportation and assistive devices), injury severity (e.g., level of impairment), and injury-related complications (e.g., pain, number of re-hospitalizations) (Krause, 2001; Meade et al., 2004). Studies of the environmental predictors have included investigations of the role of physical barriers, transportation, housing, accessibility, perceived community support, and workplace accommodations assessed at the individual level (Anderson et al., 2007; Murphy et al., 2009). Conceptually, the role of environmental characteristics is depicted in current models of disability (Verbrugge & Jette, 1994; World Health Organziation, 2001). Using the framework provided by the Disablement Process for this analysis (Figure 1), the process through which a person with SCI (e.g., pathology) experiences impairment (e.g., paralysis), loss of functioning (e.g., mobility limitations), and subsequently disability (e.g., inability to work), is influenced by risk factors that are external to the individual as well as differences intra-individual behaviors, attributes, lifestyle, and other background characteristics. For the purpose of this investigation, the extra-individual factors, which can also include access to care, support networks, and built environment characteristics, are differences in the economic conditions across environments.
Figure 1.
Conceptual framework
Adapted from Verbrugge and Jette (1994)
Research on the association between communities and economic attainment is more common in the general population. For instance, Brisson and colleagues (2009) reported that residents of areas with a higher proportion of households below poverty had lower odds of employment (Brisson et al., 2009). Casciano and Massey (2008) demonstrated that the probability of receiving welfare for poor women decreased with higher levels of neighborhood affluence, and that the prospect of finding work for disadvantaged women was actually best in neighborhoods composed of residents from diverse economic backgrounds (Casciano & Massey, 2008). The influence of neighborhood poverty and ethnic segregation on employment seeking and job attainment has also been reported to vary by race/ethnicity (Elliot & Sims, 2001), suggesting that the association between place and employment may be moderated by differences in individual background.
The rationale for this analysis stems from work that has emphasized the importance of the characteristics of geographical areas in understanding the constraints posed on social inclusion and access for persons with disabilities (Imrie, 2000). To our knowledge, only a handful of studies have specifically examined the relationship between area economic characteristics and employment for disabled groups. An earlier study found that workforce participation among adults with intellectual disabilities varied by differences in county-level per capita income, employment rates, and geographic region (Cunningham & Altman, 1993). Another study reported that persons with physical and cognitive disabilities who live in urban areas received more vocational services compared to persons living in rural areas (Johnstone et al., 2003). Research has also demonstrated a mismatch between the geographical location of vocational services for persons with disabilities and areas with large concentrations of persons with disabilities, suggesting that communities with the greatest need remain underserved (Metzel & Giordano, 2007).
The process of readjustment following a disabling health condition may be constrained by the opportunity structure of the environment, which includes access to jobs, education, healthcare, and other resources. More empirical work is needed to demonstrate the role of contextual-level factors in the experience of disability; therefore, the goal of this investigation was to assess the role of area-level economic conditions in the likelihood employment following SCI. We hypothesize that living in an area characterized as urban, socioeconomically advantaged, and low unemployment will improve the likelihood of employment among adults with chronic SCI.
Methods
Sample
The study sample was a subset of adults with SCI selected from the national Spinal Cord Injury Model Systems (SCIMS) database. The SCIMS has prospectively tracked the morbidity and mortality of the traumatic SCI population in the United States since 1970 and has involved the participation of over 27,553 persons with SCI. Detailed information on the database history and methodology is available elsewhere in the literature (Chen et al., 2011) and at the National Spinal Cord Injury Statistical Center (NSCISC) website (http://www.nscisc.uab.edu). Currently, 14 rehabilitation centers across the US are funded by the National Institute for Disability Research and Rehabilitation to collect data for the SCIMS program. With the approval of local institutional review boards, two of these centers—New Jersey and Alabama—collaborated to pilot the use of geographic identifiers to link individual outcomes data from the SCIMS database with area-level data from administrative databases (Botticello et al., 2011).
Individuals were selected from each site based on three criteria: 1) 18 years or older at the time of injury; 2) an active participant in the ongoing, long-term follow-up for the SCIMS conducted by the New Jersey and Alabama centers; and 3) completed at least one follow-up interview between 2000 and 2009. Based on these criteria, the initial study sample included 2,303 persons with SCI. Data from 849 participants was excluded because the individual's address could not be geocoded or they had moved out of state. We further excluded 181 cases of persons over age 65, and 260 cases with missing data on key variables. These analytic selections yielded a final sample of 1,013 persons. We assessed whether these selection criteria resulted in disproportionate exclusions in one site compared to another (i.e., New Jersey compared to Alabama) and found no differences. Bivariate tests (not tabled) indicated that persons among the excluded sample were significantly more likely to be married, unemployed prior to injury, and not completed high school. Reflective in part of the age-related exclusions, the omitted cases were also more likely to be injured after age 25 and were older on average than the analytic sample (47.6 versus 41.2 years). Omitted cases were also more likely to be tetraplegic and have lower physical functioning.
Data
The SCIMS combines injury-related information obtained from the medical charts of consented participants with self-reported follow-up information on a range of physical, social, and psychological outcomes obtained one-year post-injury and then at regular 5-year intervals. Follow-up surveys are administered via telephone interview or, on occasion, a mailed survey or in-person interview. To date, the NSCID contains data from approximately 103,169 follow-up interviews obtained up to 35 years post-injury (Chen et al., 2011). The area-level characteristics used for this analysis were based on data from the 2000 US Census Summary File 3 (SF3), which provided detailed information on nativity, education, employment, income, and housing. Area-level Census data was extracted via the National Historical Geographical Information System (NHGIS; http://www.nhgis.org) (Minnesota Population Center, 2004) at the county-level.
Area-Level Measures
The 1,013 individuals in our final sample were nested in 76 counties (61 in Alabama and 15 in New Jersey, respectively), with an average of 13 people per area (range 1 to 203). The use of county-level data results in a broader unit of analysis and was based on the fact that the average employed American commute approximately 25.5 minutes to work (US Census Bureau, 2004), suggesting that typically, people work outside their community or neighborhood of residence. Area data at the county level has been used in prior reports of the relationship between employment and county economic characteristics among adults with disabilities (Cunningham & Altman, 1993) as well as other population-based studies of the relationship between area characteristics and health (Scheffler et al., 2008). Several economic indicators were extracted from Census data: 1) the employment rate, 2) the percent of the population residing within an urban area, and 3) measures of household income (annual and interest income), housing values, education (high school and college completion), and the portion of residents employed in high status occupations combined to create an aggregate area-level socioeconomic index. This index was developed by Diez-Roux and colleagues (2001) and applied in various analyses of the relationship between community stratification and health (Botticello et al., 2011; Echeverria et al., 2008). The final standardized SES score had a mean of 0 and standard deviation of 1 for the 76 areas and a higher score corresponds with a higher level of SES. The variable for percent of residents residing in an urban area—which is defined by the Census Bureau as an area populated by at least 50,000 residents (US Census 2001)—was highly skewed. For analytic purposes, this variable was divided into three categories: urban (>90% of residents lived in an urban area), suburban (90–60% of residents lived in an urban area), and rural (<60% of residents lived in an urban area). The variable for percent unemployed was coded into substantively meaningful categories of low (<5%), moderate (5–10%) and high (>10%) unemployment.
Individual-Level Measures
Employment status
Employment status post-injury is assessed at each follow-up interview by asking participants to report their occupational status using the categories working, homemaker, job-training program, sheltered workshop, student, retired, unemployed, or other (which includes volunteer work, disability, or medical leave). Nearly half (49.8%) of the participants reported “other” occupational status, whereas 21.3% reported unemployment, 20.3% reported working for pay, 4.0% reported either being a student or participating in training or workshop activities, and 3.2% reported being retired, and 1.4% reported being a homemaker. For all analysis, employment status was dichotomized as paid employment (20.3%) versus not (79.7%).
Several key determinants of employment for persons with SCI that have been documented in prior studies were included as individual-level controls in the current analysis. These include variables germane to health and functioning following SCI, demographic background characteristics, and individual-level SES.
Injury severity
Injury severity was represented in all analyses with a binary variable: tetraplegia (impairment in all four limbs) and paraplegia (impairment in the lower limbs only). Persons with more severe SCI are much less likely to be employed post-injury than persons reporting less SCI-related impairment (Anderson et al., 2007; Krause & Carter, 2009). Injury severity was based on diagnoses of the neurological level of injury and injury grade reported at one-year follow-up. In some instances, diagnostic information was not obtained at one-year follow-up; for these cases the diagnostic information recorded at discharge were substituted.
Timing and duration of injury
Although average age at injury in this sample was 30.6 years (sd = 11.9), the distribution of this variable was considerably right-skewed given that SCI most commonly occurs among young adults. For the analysis, age at injury was divided into quartiles: 25 years and younger, 26–35 years, 36–45 years, and age 46 or older. Time injured was similarly divided into four categories of less than 2 years, 2–10 years, 11–15 years, and greater than 16 years post-injury for the preliminary analyses.
Health and functioning
Prior research has consistently documented that employment is less likely among persons who report more assistance with activities of daily living and more medical complications (Lidal et al., 2007; Meade, 2011). For this analysis, we controlled for the effect of functional independence using individual scores from the 13-item motor Functional Independence Measure (FIM) assessment scale (Uniform Data System for Medical Rehabilitation, 1997). This summated score demonstrated very good internal consistency and reliability for this sample (alpha = 0.96); higher scores indicate greater functional independence. Binary measures indicating whether an individual had been rehospitalized at least once in the past year (1=yes, 0=no) and self-rated health status. The latter measure is based on the 36-item Short Form Health Survey item (McHorney et al., 1993) that asks individuals to rate their own health, dichotomized as either poor health (i.e., poor or fair health) or good health (i.e., good, very good, or excellent).
Demographic Background Characteristics
A number of variables related to individual background characteristics, living situation, and socioeconomic status (SES) were also included in this investigation based on associations with employment document previously in the literature (Krause, 2001; Meade et al., 2004; Pflaum et al., 2006; Yasuda et al., 2002). Demographic variables included gender, race/ethnicity (i.e., Non-Hispanic White, Black, Hispanic, and Asian Pacific Islander or Other) and current age (measured in years). Marital status was categorized as married or unmarried (i.e., single, divorced, separated, or widowed). Participants' highest educational level was used as a proxy for individual socioeconomic status (SES) and divided into three categories: no high school degree, a high school diploma or equivalent, and some college or more. Pre-injury employment status was measured dichotomously as worked prior to injury (1=yes, 0=no).
Analysis
The purpose of this investigation was to assess: 1) area-levels variation in employment among physically disabled working-age adults and 2) the relative contribution of area-level socioeconomic differences to the probability of employment. The analytic dataset consisted of individuals with SCI nested in counties and therefore we estimated a two-level multilevel model with a random intercept. Given the binary nature of the employment, we used a hierarchical generalized linear model (HGLM) approach. Multilevel logistic regression models used the Bernoulli specification and Laplace iterations in HLM version 7 (Raudenbush et al., 2011). Using a sequential modeling strategy, we first estimated the null or unconditional model containing the random intercept. Variation in the likelihood of employment across the areas was determined by the significance both the intercept and of the estimate of the intercept variance component, τ00. Subsequent models tested the main effects of the area-level characteristics. The first set of models estimated the effects of area SES, area unemployment, and urbanicity. Area-level indicators that achieved a significance level of less than 0.05 were retained for further analysis. Next, the multivariate analysis adjusted the model for the of potential individual-level confounders. An individual-level predictor was included as a confounder if a significant difference was observed in a bivariate test between the predictor and post-injury employment status. The second set of models adjusted for the influence of individual-level differences in impairment and disability-related complications (e.g., injury severity, physical functioning, injury timing and duration, poor health, and rehospitalization). The third set of models adjusted for the influence of differences in individual background (e.g., race, age, marital status) and SES (e.g., education level). All of the individual-level predictors that attained significance of less than 0.05 in Models 2 and 3 were combined with the area-level predictors for the final adjusted model. The percent change in τ00 was used across the adjusted models to assess the contribution of each set of area-level and individual-level predictors to the area-level variation observed in the null model and changes to the deviance statistic were used to compare the fit of nested models. Continuous area-level predictors (i.e., the area SES index) were grand mean centered and continuous individual-level predictors (i.e., FIM scores, age) were group-mean centered. All descriptive analyses were performed in Stata (version 12).
As a sensitivity analysis, we repeated our modeling sequence after removing 10% of the analytic sample and found no notable difference in the pattern of results across each model. Additional analyses were also conducted to assess if the inclusion of individuals of pre-retirement age (e.g., 55–64 years) to address a concern that early retirement among adults with SCI (Krause, 2001) may result in an underestimation of the likelihood of employment and the association with area level effects. The exclusion this age group did not substantially change the results. The study findings (described below) reflect the results obtained for the full analytic sample.
Results
Sample Characteristics
The descriptive statistics for the analytic sample are reported in Table 1. The sample was approximately evenly distributed by SCI type (i.e., paraplegia and tetraplegia). The majority of the cases were injured during young adulthood (i.e., before the age of 25) and had been living with a disability for several years. The average score for the physical functioning scale was 5.0 (SD= 1.8), which corresponds with the ability to perform many of the activities of daily living with supervision. Physical functioning scores differed significantly between paraplegics and tetraplegics (F (1, 1011) = 257.89, p = 0.000; results not tabled). The average functioning score among the paraplegia group was 5.8 (SD = 1.0), which corresponded with functioning independence with assistive technology use. Given that persons with tetraplegia are more severely impaired, functioning scores were lower and reflect greater dependence (M = 4.18, SD = 2.06). This sample was relatively healthy with approximately 70% of the cases reporting good health and no recent hospitalizations, respectively. Overall, the demographic characteristics of the analytic sample were consistent with the overall SCI population; the individuals were predominantly male, Non-Hispanic White, and single (National Spinal Cord Injury Statistical Center, 2011). The sample ranged in age from 17 to 64, with an average of 41.2 years. The majority of respondents reported working (full- or part-time) prior to injury and had completed high school or some post-secondary education.
Table 1.
Distribution of Paid Employment for Physically Disabled Adults by Individual-Level Health, Background and Socioeconomic Characteristics [Percent or Mean (SD)]
| Total N = 1,013 | Employed N = 205 | Not employed N = 808 | |
|---|---|---|---|
| Injury & Health characteristics | |||
| Injury type (%) | |||
| Paraplegia | 53.2 | 61.0 | 51.2 |
| Tetraplegia | 46.8 | 39.0 | 48.8* |
| Age at injury (%) | |||
| ≤ 25 years | 42.1 | 57.1 | 38.2 |
| 26 – 35 years | 26.8 | 19.5 | 28.7 |
| 36 – 45 years | 17.4 | 13.2 | 18.4 |
| ≥ 46 years | 13.7 | 10.2 | 14.6*** |
| Injury duration (%) | |||
| < 2 years | 25.0 | 13.7 | 27.8 |
| 2 – 10 years | 37.7 | 43.4 | 36.3 |
| 11 – 15 years | 12.2 | 12.7 | 12.1 |
| ≥ 16 years | 24.1 | 30.2 | 23.8*** |
| Physical Functioning [Mean (SD)] | |||
| FIM score | 5.0 (1.8) | 5.7 (1.4) | 4.9 (1.8)*** |
| Self-rated poor health (%) | |||
| No | 71.6 | 87.3 | 67.6 |
| Yes | 28.4 | 12.7 | 32.4*** |
| Rehospitalized in past year (%) | |||
| No | 70.9 | 82.0 | 68.1 |
| Yes | 29.1 | 18.0 | 31.9*** |
| Background characteristics | |||
| Gender (%) | |||
| Male | 80.9 | 80.5 | 80.9 |
| Female | 19.1 | 19.5 | 19.1 |
| Race/ethnicity (%) | |||
| Non-Hispanic White | 60.8 | 75.6 | 57.1 |
| African American | 35.1 | 22.0 | 38.5 |
| Hispanic | 3.1 | 1.9 | 3.3 |
| Asian/Pacific Islander/Other | 1.0 | 0.5 | 1.1*** |
| Marital Status (%) | |||
| Single | 42.2 | 33.7 | 44.6 |
| Married | 31.0 | 45.4 | 27.3 |
| Divorced/Separated/Widowed | 26.8 | 21.9 | 28.1*** |
| Current age (years) | 41.2 (11.7) | 39.8 (10.2) | 41.6(12.0)* |
| Socioeconomic characteristics | |||
| Paid employment pre-injury (%) | |||
| No | 36.6 | 35.6 | 36.8 |
| Yes | 63.4 | 64.4 | 63.2 |
| Education level (%) | |||
| Less than 12 years | 21.3 | 5.4 | 25.3 |
| High school graduate/GED | 50.7 | 41.4 | 53.0 |
| Some college or more | 28.0 | 53.2 | 21.7*** |
p < 0.05;
p < 0.01;
p < 0.001
Note: Bivariate analyses based on χ2 tests of significance or t-tests.
As expected, the likelihood employment post-SCI differed significantly across most of the sample characteristics. We observed that persons with paraplegia were more likely to report working post-injury, as were persons who were injured during young adulthood, and those injured for a longer duration. The comparatively low proportion of newly injured persons (i.e., less than two years) represented among the employed group is indicative of the lengthy readjustment process following traumatic injury. Employment was also significantly more likely among persons with higher levels of physical functioning, good self-reported health, and no hospitalizations in the past year. Employment was also more likely among persons who were Non-Hispanic White, married, and highly educated. Contrary to results reported in prior studies, employment prior to injury was not associated with employment post-injury and only modestly associated with age at interview.
The distributions for the area-level characteristics are displayed in Table 2. The areas represented in this sample are highly variable in terms of the SES index, whereas the majority of the sample resided in areas that are characterized by a moderate level of unemployment (68.1%) and characterized as urban (68.7%). On average, physically disabled adults who were employed lived in an area with a higher SES (t1011 = −4.22, p = 0.00) and were much less likely to live in an area that had high unemployment (χ2 = 14.53, df = 2, p = 0.001) or was characterized as rural (χ2 = 11.00, df = 23, p = 0.004). Areas with low unemployment had a significant positive association with area SES (r = 0.45, p <0.001), as would be expected. Area SES was also strongly correlated with urbanicity (rurban = 0.67, p < 0.001; rsuburban = −0.38, p <0.001; rrural = −0.49, p < 0.001), suggesting that the urban areas represented in this sample were largely more socioeconomically advantaged in comparison to the suburban and rural areas.
Table 2.
Paid Employment for Persons with Spinal Cord Injury by Area-Level Characteristics (2000 US Census) [% or Mean (SD)]
| Total N = 1,013 | Employed N = 205 | Not employed N = 808 | |
|---|---|---|---|
| Area-level characteristics | |||
| Socioeconomic Index | |||
| Mean (SD) | 3.0 (5.3) | 4.4 (5.9) | 2.6 (2.8)*** |
| Range | [−6.6, 16.5] | [−4.8, 16.5] | [−6.6, 16.5] |
| Percent Unemployed (%) | |||
| Less than 5% | 19.4 | 28.3 | 17.1 |
| 5 – 10 % | 68.1 | 62.9 | 69.4 |
| Greater than 10% | 12.5 | 8.8 | 13.5** |
| Urbanicity (%) | |||
| Urban | 68.7 | 69.3 | 68.6 |
| Suburban | 18.6 | 23.9 | 17.2 |
| Rural | 12.7 | 6.8 | 14.2* |
p < 0.05;
p < 0.01;
p < 0.001
Note: Bivariate analyses based on χ2 tests of significance or t-tests.
Multilevel models of area-level effects on employment
Results from the null model (i.e., intercept only) in multilevel logistic model indicated that the overall odds of employment for this sample were quite low (OR = 0.23, 95% CI [0.18, 0.30]). That is, the probability of a person with SCI returning to work was 0.19.1 Results for the null model also suggested significant variation in the likelihood of employment by area (τ00 = 0.27, p < 0.05). The odds ratios and 95% confidence intervals for the series of multilevel logistic regression models assessing the effects of area-level economic characteristics on employment are presented in Table 3. Contrary to expectations, the effect of the area-level unemployment rate was non-significant in the multivariate analysis and was excluded from further analysis for parsimony. As hypothesized, we observed a significant positive linear relationship between area-level SES and the average odds of employment for persons with SCI (Model 1 in Table 3). Contrary to our predictions, the average odds of employment were significantly lower in urban compared to suburban areas (OR = 0.33, 95% CI [0.20, 0.54]). The average odds of employment in an area classified as rural compared to suburban were also lower, although not significant. Together, area-level SES and urbanicity reduced the area-level variation in the likelihood of employment by 85% in comparison to the null model.
Table 3.
Multilevel logistic regression models of area-level economic characteristics on employment for persons with SCI
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|
|---|---|---|---|---|
| Odds Ratio [95% CI] | Odds Ratio [95% CI] | Odds Ratio [95% CI] | Odds Ratio [95% CI] | |
| Area-level | ||||
| SES index | 1.11 [1.06, 1.16] | 1.12 [1.06, 1.19] | 1.07 [1.02, 1.11] | 1.09 [1.04, 1.14] |
| Rurala | 0.44 [0.19, 1.03] | 0.45 [0.15, 1.39] | 0.48 [0.16, 1.44] | 0.53 [0.13, 2.20] |
| Urbana | 0.33 [0.20, 0.54] | 0.36 [0.19, 0.66] | 0.47 [0.26, 0.86] | 0.46 [0.23,0.93] |
| Individual-level | ||||
| Injury characteristics | ||||
| Paraplegiab | -- | 1.04 [0.68, 1.60] | -- | -- |
| Physical functioning | -- | 1.40 [1.21, 1.62] | -- | 1.45 [1.26, 1.67] |
| Poor healthc | -- | 0.35 [0.20, 0.63] | -- | 0.41 [0.22, 0.76] |
| Rehospitalized | -- | 0.63 [0.37, 1.07] | -- | -- |
| Age injured ≤ 25 yrsd | -- | 1.90 [1.11, 3.25] | -- | 2.00 [1.04, 3.84] |
| Injured < 2 yrse | -- | 0.42 [0.22, 0.82] | -- | 0.45 [0.22, 0.94] |
| Background characteristics | ||||
| No high school degreef | -- | -- | 0.10 [0.04, 0.28] | 0.12 [0.06, 0.27] |
| High school degreef | -- | -- | 0.34 [0.20, 0.58] | 0.34 [0.17, 0.68] |
| African Americang | -- | -- | 0.66 [0.34, 1.31] | -- |
| Hispanicg | -- | -- | 0.44 [0.12, 1.60] | -- |
| API/Otherg | -- | -- | 0.25 [0.01, 11.2] | -- |
| Marriedh | -- | -- | 2.46 [1.46, 4.15] | 2.62 [1.31, 5.26] |
| Current age | 0.96 [0.94, 0.99] | 0.98 [0.95, 1.01] | ||
| Between-area variance (τ00) | 0.04 | 0.02 | 0.04 | 0.00 |
| % change in τ00 compared to the Null model | − 85% | − 92% | − 85% | − 100% |
| Deviance statistic compared to Model 1 | 2843.47 | 2729.29*** | 2725.28*** | 2647.47*** |
Omitted reference categories:
suburban;
tetraplegia;
good health;
age at injury >26 years;
injured two or more years;
some college education;
Non-Hispanic White;
Not married.
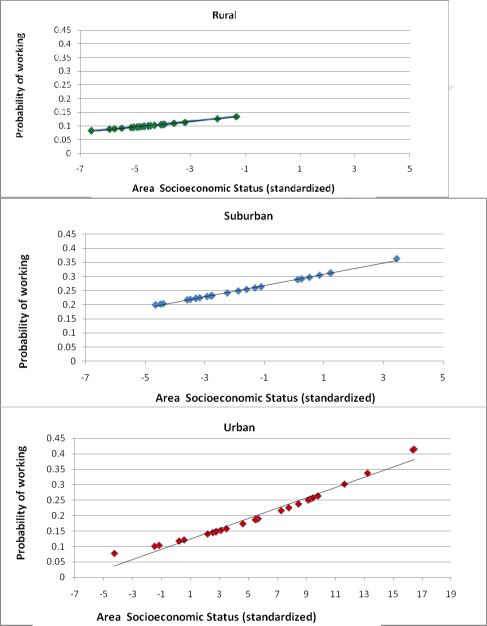
The possibility for an interaction between area-level SES and urbanicity was tested and found to be non-significant; for each area type, we observed a positive linear relationship between SES and the probability of working, depicted in Figure 2. The urban areas in this sample represented a wider spectrum of SES in comparison to the areas that were classified as suburban and rural. The highest predicted probabilities of employment (0.3 and above) were found in urban areas that were also at the highest end of the SES advantage index. A similar probability of employment was found in suburban areas at more moderate levels of SES, suggesting that the likelihood of employment was similar, if not better, in suburban areas that were comparatively less affluent.
Figure 2.
Predicted of probability of working after SCI by Area-Level SES and Urbanicity
Model 2 in Table 3 presents the relationship between area indicators and employment adjusted for disability-related predictors. Together the addition of the disability-related predictors reduced the area-level variation by 92% compared to the null model and significantly improved the model fit. The main effects for area SES and urbanicity remained virtually unchanged. This suggests that geographic variation in the likelihood of employment for physically disabled adults is largely independent of individual-level differences in health and functioning. Although the likelihood of employment did not differ by injury severity, the likelihood of working increased higher levels of physical functioning independence and was lower, on average, among persons who reported poor in comparison good health. The timing and duration of injury also significantly predicted the likelihood of working. Persons who were injured at younger ages (i.e., less than 25 years old) were twice as likely to be working post-SCI in comparison to persons injured later in adulthood. Persons who were recently (i.e., less than two years) injured were also 44% less likely to report working in comparison to persons who had been injured longer.
Model 3 presents the associations between employment and area-level predictors adjusted for individual-level background characteristics. Although the main effects of the area-level variables persisted, the observed effect of area-SES was notably reduced whereas the urban versus suburban difference increased by approximately 31% in Model 3. This suggests that the associations between area SES and employment and the urban-suburban gap were partially mediated by differences in individual background characteristics. Persons with low and moderate levels of education were significantly less likely (91% and 69% less, respectively) to be employed in comparison to highly educated persons. However, no significant differences were observed by race/ethnicity. Married persons were more than twice as likely be employed compared to unmarried physically disabled adults. We also observed a modest negative linear association between age and the odds of working such that increasing age decreased the likelihood of working post-injury. Adjusting for differences in individual background characteristics resulted in no additional explanation of the between-area variation in employment. Model 4 on Table 3 reports the results for the final, restricted model. Notably, the positive linear association between area SES and the likelihood of employment remained significant as did the difference between urban and suburban areas. The area-level variation in the likelihood of employment that was initially observed in the null model is fully accounted for and the final restricted model results in the largest reduction in the deviance statistic.
Discussion
Our findings suggest that employment for adults with SCI is predicted by differences across socioeconomically diverse geographic areas representing urban, suburban, and rural locales. In particular, the significant relationship between area-level SES and the probability of employment confirmed our hypothesis of a linear, positive association between SES advantage and working. Contrary to our expectations, variation in the unemployment rate across geographic areas did not predict differences in the average likelihood of employment for persons with SCI in the multivariate model. The fact that we observed that the SES index was a significant and persistent predictor of employment in the multivariate portion of the analysis suggests that the contribution of area-level SES is multifaceted and more accurately captured by multiple measures indicative of the economic viability of the environment (i.e., aggregate income, housing values, education levels, and employment in high-level occupations) as suggested by Casciano and Massey (2008), rather than a single indicator.
We expected to find that urban areas would offer the best prospects of employment compared to suburban and rural areas. However, our analyses indicated that suburban compared to urban areas were associated with a better probability of employment. We are constrained by the use of secondary data and a geographically limited sample of suburban and urban areas in explaining this observed suburban-urban gap in employment, but this finding leads to several important questions for an expanded future analysis. We posited that the prospects of employment would be better in urban environments due in part to differences in urban and nonurban locales such as resources (i.e., availability of public transportation), built characteristics (i.e., retail and industry density, street connectivity), and social characteristics (i.e., greater population density). Our finding leads us to question what aspects of suburban locales may foster better employment outcomes. For instance, ownership of individual transportation (i.e., a modified car or van) may be more common among persons with disabilities residing in the suburbs and increase the feasibility of working outside the home. Differences in the availability and accessibility of vocational services between areas has also been suggested as a key predictor of region differences in employment (Johnstone et al., 2003; Metzel & Giordano, 2007). Although the difference between rural and suburban areas was not significant, our findings do suggest that on average, persons with SCI living in rural areas are at the greatest disadvantage in terms of the likelihood of employment.
The observed geographical variation in employment in this analysis was small but significant and largely explained by the combination of area-level and individual-level predictors. Education and marital status emerged as key individual-level predictors of employment in this analysis, which is consistent with prior studies (Krause & Carter, 2009). Evidence of race group differences in employment predicted by prior research (Meade et al., 2004) were rendered non-significant in our multivariate multilevel models, however, suggesting that employment disparities in race were largely accounted for by differences in educational background and environmental factors. Studies have suggested that aging also poses a barrier to returning to work after SCI. Although we found that the modest negative relationship between age and working, our results did not suggest that aging posed a significant barrier to working after SCI as is the case in other studies (Krause, 2001). In order to verify that the observations of older individuals were not overly influential in our findings, we ran a subsequent post-hoc multilevel analysis omitting persons in the pre-retirement age range (55–64 years) and found no appreciable difference in the results.
Our results demonstrated that employment was not predicted by the severity of impairment, injury timing, and duration, conflicting with other reports that have cited injury severity (i.e., tetraplegia versus paraplegia; complete versus incomplete) as a key predictor of return to work following SCI (Krause & Carter, 2009). Our analysis was congruent with prior research demonstrating that employment was more likely among persons with higher levels of physical functioning and good reported health (Lidal et al., 2007). These findings suggest the importance of individual background and well-being to long-term social participation following SCI and not the impairment itself. These findings suggest the importance of individual background and well-being to long-term social participation following SCI and not the impairment itself.
This analysis was limited most notably in terms of its generalizability. The study sample was not representative of the wide diversity of adults with disabilities in the US nor was it fully representative of adults with SCI. Although the SCIMS database is the one of the largest longitudinal datasets exclusive to an injury group in the US, it is not population-based. The analytic subsample is further limited to two geographic regions and did not reflect the range of geographic diversity in area-level economic conditions found across the US. A broader sample would also allow the assessment of cross-level interactions between individual- and contextual-level characteristics, thus enabling our ability to test if environmental factors are more salient for certain groups of individual (e.g., racial minorities, the poor) than others. There are other limitations associated with our use of county-level data to approximate measure geographic areas, as there is the potential for more SES heterogeneity across these larger geographic units. However, our use of county-level was also justified by analytic concerns for data sparseness as well national trends indicating that people are likely to work in areas outside the immediate vicinity of their residence, which would be measured by a smaller unit such as a block or Census tract.
The multivariate analysis included an array of individual-predictors of employment that are relevant to this specific disabled population as well as several area-level economic indicators. However, the process obtaining gainful employment following a disabling condition involves a complex array of physiological, socioeconomic, psychological, and contextual influences. In particular, future investigations along this line of inquiry would benefit from the inclusion of additional predictors such as access to transportation (i.e., car ownership) and use of specific assistive devices. These indicators have a demonstrated relationship with employment and are indicative of individual resources. Furthermore, there are other area-level predictors of employment, such as ethnic and age stratification that were not included as controls in this analysis but are important controls to consider in future research.
The use of cross-sectional data limited our ability to assess selection effects, such as people migrating into certain areas based on factors such as job availability and accessibility. Furthermore, the SCIMS follow-up survey only assesses employment status at one particular point in time and does not capture fluctuations that are likely in employment status over a 1-year or 5-year period. Adjustment to disability in adulthood is a lengthy and dynamic process. Therefore, future analysis of the relationship between the environment and aspects of social participation such as employment will benefit from a longitudinal approach.
This investigation adds to the growing literature on the social determinants of health and disability using multilevel modeling (Clarke & George, 2005; Clarke et al., 2011; Freedman et al., 2008) and draws particular attention to an aspect of social participation for persons with disabilities that benefits health and well-being as well as financial and occupational success. The probability of employment for adults with SCI is not uniform but rather affected by differences in the area SES and urbanicity. This study also demonstrates that employment among this vulnerable segment of the population is alarmingly low, which is unsurprising in light of evidence suggesting that disability policies aimed at increasing employment for persons with disabilities and chronic health concerns have been ineffective (Bambra & Eikemo, 2009; Moon & Shin, 2006). The suggestion that people's social and economic attainment is influenced by the places they inhabit as well as by individual circumstances may help direct more targeted interventions to underserved areas, such as rural and impoverished communities. At the individual level, clinicians and disability advocates may consider the congruence between individual goals (e.g., work, family life) and the opportunity structure of a given environment when assisting adults with acquired physical disabilities as they plan their return to the community. Collectively the findings from this investigation underscore that the feasibility of social participation for persons with disabilities may be shaped by community- and area-level factors. In short, a societal approach is required for eliminating barriers and devising interventions to promote full inclusion for persons at all levels of ability.
Highlights
Overall, a key aspect of social participation for adults with disabilities varies geographically and is influenced by area economic conditions.
Employment for persons with SCI is more likely in socioeconomically advantaged areas and in areas that are categorized as suburban versus urban.
Geographic variation in employment was relatively unaffected by individual-level differences in health and functioning and modestly attenuated by educational attainment.
Acknowledgments
Disclosures: Supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (grant number: 5K99HD065957-02) and the National Institute of Disability and Rehabilitation Research (grant number: H133N060022)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Probability of employment = Odds of employment / (1+ Odds of employment)
References
- Anderson D, Dumont S, Azzaria L, Le Bourdais M, Noreau L. Determinants of return to work among spinal cord injury patients: A literature review. Journal of Vocational Rehabilition. 2007;27:57–68. [Google Scholar]
- Bambra C, Eikemo TA. Welfare state regimes, unemployment and health: A comparative study of the relationship between unemployment and self-reported health in 23 European countries. Journal of Epidemiology and Community Health. 2009;63:6. doi: 10.1136/jech.2008.077354. [DOI] [PubMed] [Google Scholar]
- Botticello AL, Chen Y, Cao Y, Tulsky DS. Do communities matter after rehabiliation? The effect of socioeconomic and urban stratification on well-being after spinal cord injury. Archives of Physical Medicine and Rehabilitation. 2011;92(3):8. doi: 10.1016/j.apmr.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brisson D, Roll S, East J. Race and ethnicity as moderators of neighborhood bonding social capital: Effects of employment outcomes for families living in low-income neighborhoods. Families in Society. 2009;90(4):7. [Google Scholar]
- Casciano R, Massey DS. Neighborhoods, employment, and welfare use: Assessing the influences of neighborhood socioeconomic composition. Social Science Research. 2008;37:15. doi: 10.1016/j.ssresearch.2007.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapin MH, Holbert D. Employment at closure is associated with enhanced quality of life and subjective well-being for persons with spinal cord injuries. Rehabilitation Counseling Bulletin. 2010;54(1):9. [Google Scholar]
- Chen Y, Deutsch A, DeVivo MJ, Johnson K, Kalpakjian CZ, Nemunaitis G, Tulsky D. Current research outcomes from the Spinal Cord Injury Model Systems. Archives of Physical Medicine and Rehabilitation. 2011;92(3):3. doi: 10.1016/j.apmr.2010.12.011. [DOI] [PubMed] [Google Scholar]
- Clarke P, George LK. The Role of the Built Environment in the Disablement Process. American Journal of Public Health. 2005;95:1933–1939. doi: 10.2105/AJPH.2004.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke PJ, Ailshire JA, Nieuwenhuijsen ER, de Kleijn-de Vrankrijker MW. Participation among adults with disability: The role of the urban environment. Social Science & Medicine. 2011;72:11. doi: 10.1016/j.socscimed.2011.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan JD, Bognar JA. Neighborhood Characteristics and Outcomes after Traumatic Brain Injury. Archives of Physical Medicine and Rehabilitation. 2008;89(May):912–921. doi: 10.1016/j.apmr.2007.12.027. [DOI] [PubMed] [Google Scholar]
- Cunningham PJ, Altman B. The effects of sociodemographic and contextual factors on employment of persons with mental retardation living in residential facilities. Journal of Developmental and Physical Disabilities. 1993;5(4):281–296. [Google Scholar]
- DeVivo MJ. Epidemiology of spinal cord injury: trends and future implications. The International Spinal Cord Society (ISCoS); Washington, D.C.: 2011. p. 33. [DOI] [PubMed] [Google Scholar]
- DeVivo MJ, Chen Y.-y. Trends in new injuries, prevalent cases, and aging with spinal cord injury. Archives of Physical Medicine and Rehabilitation. 2011;92(3):7. doi: 10.1016/j.apmr.2010.08.031. [DOI] [PubMed] [Google Scholar]
- Echeverria S, Diez-Roux AV, Shea S, Borrell LN, Jackson S. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors:The Multi-Ethnic Study of Atherosclerosis. Health and Place. 2008;14:8. doi: 10.1016/j.healthplace.2008.01.004. [DOI] [PubMed] [Google Scholar]
- Elliot JR, Sims M. Ghettos and barrios: The impact of neighborhood poverty and race on job matching among Blacks and Latinos. Social Problems. 2001;48(3):21. [Google Scholar]
- Emerson E, Hatton C. Socioeconomic disadvantage, social participation, and networks and the self-rated health of English men and women with mild and moderate intellectual disabilities: cross sectional survey. European Journal of Public Health. 2007;18(1):7. doi: 10.1093/eurpub/ckm041. [DOI] [PubMed] [Google Scholar]
- Fone D, Dunstan F, Williams G, Lloyd K, Palmer S. Places, people and mental health: A multilevel analysis of economic inactivity. Social Science & Medicine. 2007;64:9. doi: 10.1016/j.socscimed.2006.09.020. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Grafova IB, Schoeni RF, Rogowski J. Neighborhoods and disability in later life. Social Science and Medicine. 2008;66:2253–2267. doi: 10.1016/j.socscimed.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imrie R. Disabling environments and the geography of access policies and practices. Disability and Society. 2000;15(1):20. [Google Scholar]
- Jackson AB, Dijkers M, DeVivo MJ, Poczatek RB. A Demographic Profile of New Traumatic Spinal Cord Injuries: Change and Stabiltiy over 30 Years. Archives of Physical Medicine and Rehabilitation. 2004;85:1740–1748. doi: 10.1016/j.apmr.2004.04.035. [DOI] [PubMed] [Google Scholar]
- Johnstone B, Price T, Bounds T, Schopp LH, Schootman M, Schumate D. Rural/urban differences in vocational outcomes for state vocational rehabilitation clients with TBI. NeuroRehabilaition. 2003;18:197–203. [PubMed] [Google Scholar]
- Kaye HS. The impact of the 2007-2009 recession on workers with disabilities. Monthly Labor Review. 2010;(October):12. [Google Scholar]
- Kirsh B, Stergiou-Kita M, Gewurtz R, Dawson D, Krupa T, Lysaght R, Shaw L. From margins to mainstream: What do we know about work integration for persons with brain injury, mental illness and intellectual disability. Work. 2009:391–405. doi: 10.3233/WOR-2009-0851. [DOI] [PubMed] [Google Scholar]
- Krause JS. Aging and self-reported barriers to employment after spinal cord injury. Topics in Spinal Cord Injury Rehabilitation. 2001;6 [Google Scholar]
- Krause JS, Carter RE. Risk of mortality after spinal cord injury: relationship with social support, education, and income. Spinal Cord. 2009;47:7. doi: 10.1038/sc.2009.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause JS, DeVivo MJ, Jackson AB. Health status, community integration, and economic risk factors for mortality after spinal cord injury. Archives of Physical Medicine and Rehabilitation. 2004;85:10. doi: 10.1016/j.apmr.2004.06.062. [DOI] [PubMed] [Google Scholar]
- Lidal IB, Huynh TK, Biering-Sorensen F. Return to work following spinal cord injury:A review. Disability and Rehabiliation. 2007;29(17):1341–1375. doi: 10.1080/09638280701320839. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clincial tests of validity in measuring physical and mental health constructs. Medical Care. 1993;31:6. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- Meade MA. The influence of secondary conditions on job acquisition and retention in adults with spinal cord injury. Archives of Physical Medicine and Rehabilitation. 2011;92(3):8. doi: 10.1016/j.apmr.2010.10.041. [DOI] [PubMed] [Google Scholar]
- Meade MA, Lewis A, Jackson N, Hess D. Race, Employment, and Spinal Cord Injury. Archives of Physical Medicine and Rehabilitation. 2004;85:1782–1792. doi: 10.1016/j.apmr.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Metzel DS, Giordano A. Locations of employment services and people with disabilities. Journal of Disability Policy Studies. 2007;18(2):10. [Google Scholar]
- Minnesota Population Center. Minnesota U. o. National Historical Geographic Information System. Prerelease v.01 Minneapolis: 2004. [Google Scholar]
- Moon S, Shin J. The effect of the Americans with Disabilities Act on economic well-being of men with disabilities. Health Policy. 2006;76:10. doi: 10.1016/j.healthpol.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Murphy GC, Middleton J, Quirk R, De Wolf A, Cameron ID. Prediction of employment status one year post-discharge from rehabilitation following traumatic spinal cord injury: An exploratory analysis of particpation and environmental variables. Journal of Rehabilitation Medicine. 2009;41:6. doi: 10.2340/16501977-0465. [DOI] [PubMed] [Google Scholar]
- National Spinal Cord Injury Statistical Center . Spinal Cord Injury Facts and Figures at a Glance. National Spinal Cord Injury Statistical Center; Birmingham, AL: 2011. [Google Scholar]
- Pflaum C, McCollister G, Strauss DJ, Shavelle RM, Devivo MJ. Worklife after traumatic spinal cord injury. Journal of Spinal Cord Medicine. 2006;(29):10. doi: 10.1080/10790268.2006.11753886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk A, Congdon R, I. Scientific Software International . Hierarchical Linear and Nonlinear Modeling. version 7.0 Lincolnwood, IL: 2011. [Google Scholar]
- Robert SA. Socioeconomic position and health: The independent contribution of community socioeconomic context. Annual Review of Sociology. 1999;25:28. [Google Scholar]
- Scheffler RM, Brown TT, Syme L, Kawachi I, Tolystykh I, Iribarren C. Community-level social capital and recurrence of acute coronary syndrome. Social Science and Medicine. 2008:1603–1613. doi: 10.1016/j.socscimed.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Uniform Data System for Medical Rehabilitation . Guide for the Uniform Data Set for Medical Rehabilitation (including the FIM™ instrument) version 5.1 Buffalo, NY: 1997. [Google Scholar]
- US Census Bureau . Journey to Work: 2000. Government Printing Office; Washington: 2004. [Google Scholar]
- US Department of Labor . Persons with a disability: Labor force characteristics -- 2009. Government Printing Office; Washington: 2010. [Google Scholar]
- Verbrugge LM, Jette AM. The Disablement Process. Social Science and Medicine. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Ville I. Biographical work and returning to employment following a spinal cord injury. Sociology of Health and Illness. 2005;27(3):27. doi: 10.1111/j.1467-9566.2005.00445.x. [DOI] [PubMed] [Google Scholar]
- World Health Organziation . International classification of functioning, disability, and health. Geneva, Switzerland: 2001. [Google Scholar]
- Yasuda S, Wehman P, Targett P, Cifu DX, West M. Return to work after spinal cord injury: A review of the recent research. NeuroRehabilitation. 2002;17:177–186. [PubMed] [Google Scholar]
- Zunzunegui M-V, Forster M, Gauvin L, Raynault M-F, Willms JD. Community unemployment and immigrants' health in Montreal. Social Science & Medicine. 2006;63:16. doi: 10.1016/j.socscimed.2006.01.004. [DOI] [PubMed] [Google Scholar]