Abstract
The coronal cast restoration continues to be used commonly to restore mutilated, endodontically treated teeth. The tensile bond strength of luting cements is of critical importance as many of failures are at the core and the crown interface. An invitro study with aim to evaluate and compare bond strengths of luting cements between different core materials and cast crowns. A total of 45 extracted identical mandibular second premolars were endodontically treated and divided into 3 groups of 15 each. Specimens in first group were restored with cast post and core (Group C), and specimens in second group were restored with stainless steel parapost and composite core material (Group B) and specimens in third group were restored with stainless steel parapost and glass ionomer core build (Group G). Standardized crown preparation was done for all the specimens to receive cast crowns. Each group was further divided into 3 subgroups and were cemented using 3 different luting cements namely, resin cement, polycarboxylate cement, glass ionomer cement (Type I). The samples of each subgroup (n = 5) were subjected to tensile testing using Universal Testing Machine at a crosshead speed of 2 mm/min till the dislodgement of crown from the core surface was observed. The bond strengths were significantly different according one way ANOVA (F-150.76 and p < 0.0000). The results of the study showed that the specimens cemented with resin cement in cast core, composite core and glass ionomer core exhibited significantly higher bond strengths as compared to specimens cemented with glass ionomer and polycarboxylate cement. Composite resin core and resin cement combinations were superior to all other cement and core combinations tested.
Keywords: Endodontically treated tooth, Post and core, Luting agent, Cast crown, Tensile bond strength
Introduction
Practitioners of dentistry have been confronted with problems of restoring lost portions of tooth structure as a result of pulpal or periapical disease. Since preservation of what remains and its restoration is more acceptable to the patient than extraction, the means of restoring missing tooth structure by artificial materials continue to account for a large part of dental research. Recent advances in material science and techniques have led to a significant impact on the restoration of endodontically treated teeth. The use of prefabricated post in conjunction with various core materials viz., reinforced glass ionomer, composite etc., and their ability to bond with multiple restorative materials and to tooth structure will continue to revolutionize this relationship [1]. A post and core is used to provide retention and support for the coronal cast restoration. The important factors which influence the success of such a cast restoration are (1) the luting medium and its biophysical properties, (2) the degree of bond strength between the luting cement and core material, (3) the type of core material to which the casting is cemented (4) the design and quality of tooth/core and (5) the accuracy of the casting [2, 3]. The tensile bond strengths of various luting agents to dentin and cast crown have been extensively researched and have been widely reported in the literature. Several studies have compared the tensile bond strengths of various luting media with different core materials [4–8].
The specimens for several studies were models simulating teeth which were prepared using dies or molds. The models thus fabricated had essentially a uniaxial rounded configuration. The samples used in this study are freshly extracted mandibular second premolars, which have a multiaxial configuration with a flat occlusal surface. The objective of the present study is to evaluate and compare the tensile bond strengths of luting agents between different cores and cast crowns cemented with different luting agents.
Materials and Methods
Forty-five freshly extracted, single rooted mandibular 2nd premolars with adequate root length and uniformity in size and shape were collected. The criteria for selecting these teeth were absence of cracks or fractures in the cervical area of the root, no evidence of caries, no restorations and no history of previous endodontic treatment. All the teeth were cleaned with hydrogen peroxide for remaining debris and tissue tags and stored in normal saline.
Preparation of the Samples
All the teeth were endontically treated and root canals were obturated with gutta-percha using standard lateral condensation method. The anatomic crown of each tooth was removed with a diamond bur using high-speed handpiece under copious water spray. In each case the angle of the cut was perpendicular to the long axis of the tooth 2 mm coronal to the cemento-enamel junction. The root portion of each tooth, with reinforced wire, was embedded in a block measuring 3.5 × 1.5 × 1.5 cm of self-cure acrylic resin with coronal tooth surface 2 mm above the cementoenamel junction (Fig. 1). The prepared samples were then divided into three groups by randomly selecting fifteen samples for each group. The three groups were designated as Group C (cast post and core), Group B (composite core) and Group G (glass ionomer core) and the specimens in each group were subdivided into three groups of five samples each and were designated as CR, CP CG, BR, BP, BG and GR, GP, GG. In each sub group, the first alphabet denotes the type of core material and the second alphabet denotes the type of luting cement.CR (cast core/resin cement), CP (cast core/polycoboxylate cement) CG (cast core/glass ionomer cement), BR (composite core/resin cement), BP (composite core/polycorboxylate cement), BG (composite core/glass ionomer cement) and GR (glass ionomer core/resin cement), GP (glass ionomer core/polycorboxylate cement), GG (glass ionomer core/glass ionomer cement).
Fig. 1.
Endodontically treated and decoronated specimens mounted on acrylic blocks
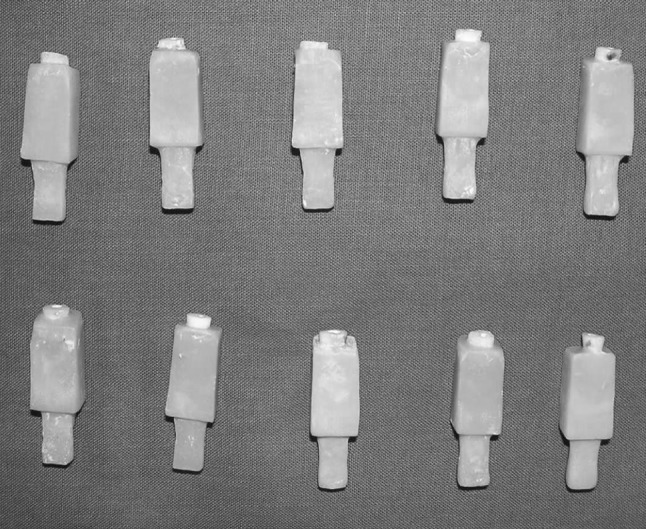
The root canal spaces for all the three groups were prepared with Parapost twist drill no. 5 (Coltene Whaldent) using contrangle micromotor hand piece. The root canals were prepared to a final diameter of 1.25 mm and a depth of 12 mm from the prepared flat occlusal surface. In Group C (cast post and core), a plastic burn out post pattern of 1.25 × 15 mm was inserted into 12 mm of the prepared root canal space and a custom post and core pattern was fabricated using auto polymerizing resin using Tofflemire matrix retainer and matrix band. Cervico occlusal height of all the samples was maintained 5 mm above remaining occlusal tooth surface. The prepared resin patterns were designated and numbered with their respective dies, sprued and invested in phosphate bonded investment (Bellasun, Bego, Inc) according to the manufacturer’s recommendations, and casted using Wirolloy (Ni–Cr) (Bego, Inc). The castings were inspected and adjusted to a passive fit, and then air abraded with 50 μm aluminium oxide. For the specimens in Group B and Group G stainless steel Parapost XP no. 5 (Coltene Whaledent) were adjusted in the prepared root canals, leaving 4 mm of post head extended above the preparation. For all the three groups post cementation was done using Relyx ARC (3M Dental Products Div) along with single bond dental adhesive (3M Dental Products Div). In Group B and Group G, Tofflemire matrix retainer and clear plastic matrix were applied around the coronal surface of the tooth. The coronal core portion was made with a dual cure core build-up composite Bis core (Bisco Inc) and light cured Glass Ionomer (Vitremer™ core Build up—3M Dental Products Div) respectively (Fig. 2).
Fig. 2.

Prepared cast core, composite core and glass ionomer core specimens
Standardized and identical crown preparations with respect to size, shape and surface area were done on all the specimens to receive full metal crowns with a chamfer finish line on the remaining tooth structure using k-9 crown finishing installation. This instrument aided to orient the diamond point in contact with the core and tooth surface at a similar angle for all the specimens, thereby producing the same angle of convergence (Fig. 3). Flat occlusal reduction was done to height of 5 mm from the remaining occlusal tooth surface to the prepared margins and was maintained for all the specimens.
Fig. 3.

Specimen with high turbine hand piece mounted in K-9 crown finishing installation
Determining the Fitting Surface Area
Copper band impressions were made in medium body impression material. To measure the surface area of the axial surface, the band was removed and the impressions were cut exactly at the margins using a new sharp bard parker knife and then an imprint of the fitting surface was made on the graph paper. Number of squares of each imprint on the graph paper were added and then counted, which gave the approximate surface area (Fig. 4).
Fig. 4.
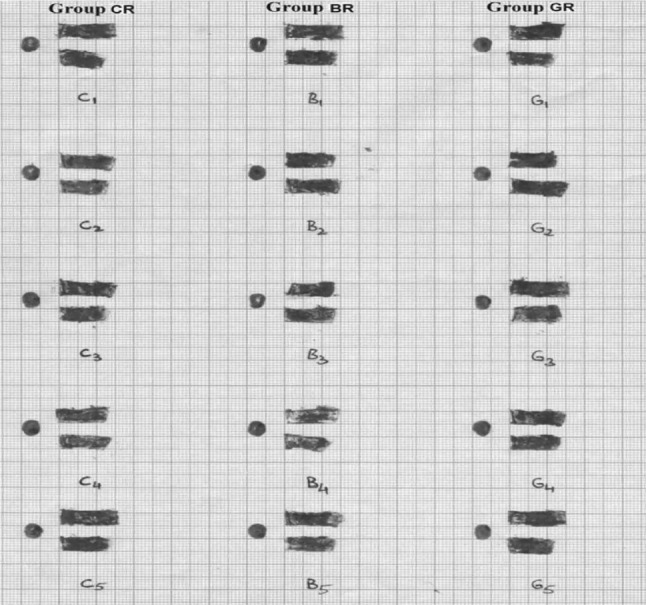
Imprint showing measurement of surface area for cast core, composite core and glass ionomer core
Crown Fabrication
Total of 45 wax patterns were fabricated for each sample by direct wax pattern technique. An inverted ‘U’ shaped wax loop was attached on the occlusal surface of the patterns, which later would serve as an attachment for the tensile loading. The wax patterns were cast in base metal alloy Ni–Cr (Wirolloy, Bego. Inc) using Induction casting machine. The castings were divested, air abraded with 50 μm aluminium oxide, and ultrasonically cleansed. All the casting were examined and seated on its respective die to evaluate the marginal fit and complete seating.
Cementation Procedure
For each sample the cast crowns were cemented using three different luting cements which were resin cement (Relyx ARC, 3M Dental Products Div), polycarboxylate cement (Poly-F, Densply Inc) and glass ionomer cement (GC Type I, GC Corporation). Each acrylic block along with the prepared specimens were marked as groups and subgroups. Each cast crown was cemented one at a time and the cements were manipulated according to manufacturer’s specifications.
Determination of the Tensile Bond Strength
After storing the cemented specimens in distilled water for 24 h, they were tested on a Universal testing machine. Determination of the tensile bond strength of the specimens comprising of post, core and cemented crown (Fig. 5) (the restoration assembly dislodged from the root canal) was done by directly engaging the specimen in lower crosshead of the Universal testing machine. The retentive loop of the test crown was engaged with 18:8 stainless steel wire (19 gauge) and was mounted in the upper cross heads of the Universal testing machine (Instron 1011, code QC1008A). Tensile force was applied with a 1,000 N load cell at a crosshead speed of 2 mm/min, till the dislodgement of the crowns from the core surface. The load at which the cast crown was dislodged from the core indicated the tensile bond strength of that particular specimen (Fig. 6). The values obtained were noted and recorded in Newton’s, which forms the basic data of the study. The values were converted to (Kgf) using the following formulae and conversions and the data was subjected to statistical analysis.
Fig. 5.

Debonded specimens with post, core and cast crown
Fig. 6.
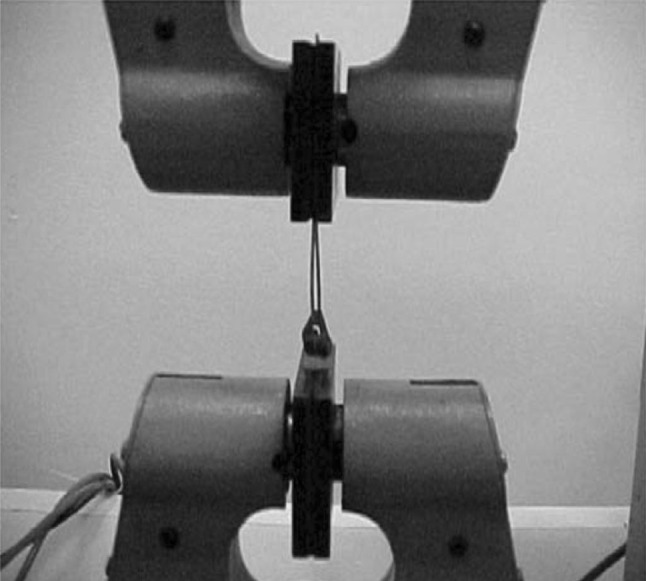
Post, core and cast crown assembly mounted on universal testing machine showing debonding at core and crown interface
Formulae/Conversions Used [7]
1Kgf = 9.81 N
1 mm2 = 1/10 × 10 cm2
Results
The measurements of tensile bond strength of Group C (cast core), Group B (composite core) and Group G (glass ionomer core) cemented with resin cement, polycarboxylate cement and glass ionomer cement were subjected to statistical analysis to draw conclusions from the experimental data. Descriptive statistical measures, such as mean, range between maximum and minimum values of tensile bond strengths, standard deviation (SD), coefficient of variation (CV), standard error of mean (SEm) were computed for all the study groups. In order to collectively compare the means of study groups, One way ANOVA (analysis of variance) test was used (p < 0.05) and pair wise comparison of the groups tested was done using student’s t test (p < 0.05).
An analysis of variance (One way ANOVA) of tensile bond strengths of specimens in cast core, composite core and glass ionomer core specimens cemented with resin cement and glass ionomer cement showed the statistically significant difference (F-173.27, p < 0.000 and F-13.37, p < 0.0009) (Tables 1, 2), and specimens cemented with polycarboxylate cement were not statistically significant (F-3.29, p < 0.0724) (Table 3).
Table 1.
Statistical analysis (One Way ANOVA) of tensile bond strengths of luting agents between cast crown and cast core, composite core and glass ionomer core specimens cemented with resin cement
| Source of variance | Degrees of freedom | Sum of squares | Mean sum of squares | F-ratio | p value | Remarks |
|---|---|---|---|---|---|---|
| Between cements | 2 | 614.1 | 370.0 | 173.27 | 0.0000 | S |
| Within cements | 12 | 21.26 | 1.772 | |||
| Total | 14 | 635.3 |
S Significant
Table 2.
Statistical analysis (One Way ANOVA) of tensile bond strengths of luting agents between cast crown and cast core, composite core and glass ionomer core specimens cemented with glass ionomer cement
| Source of variance | Degrees of freedom | Sum of squares | Mean sum of squares | F-ratio | p value | Remarks |
|---|---|---|---|---|---|---|
| Between cements | 2 | 154.7 | 77.36 | 13.37 | 0.0009 | S |
| Within cements | 12 | 69.45 | 5.788 | |||
| Total | 14 | 224.2 |
S Significant
Table 3.
Statistical analysis (One Way ANOVA) of tensile bond strengths of luting agents between cast crown and cast core, composite core and glass ionomer core specimens cemented with polycarboxylate cement
| Source of variance | Degrees of freedom | Sum of squares | Mean sum of squares | F-ratio | p value | Remarks |
|---|---|---|---|---|---|---|
| Between cements | 2 | 15.35 | 7.673 | 3.29 | 0.0724 | NS |
| Within cements | 12 | 27.96 | 2.330 | |||
| Total | 14 | 43.30 |
NS Non significant
On pair wise comparison using (student’s t test) the tensile bond strengths of specimens in cast core, composite core and glass ionomer core cemented with resin cement and glass ionomer cement showed statistically significant difference (|t|-15.77, p < 0.0000, |t|-16.56, p < 0.0000 and |t|-6.22, p < 0.0003) and (|t|-5.18, p < 0.0008, |t|-3.17, p < 0.0132 and |t|-2.05, p > 0.0742) (Tables 4, 5). On the contrary specimens cemented with polycarboxylate cement showed no statistically significant difference in tensile bond strengths (|t|-2.13, p > 0.0655, |t|-2.70, p < 0.0269 and |t|-1.17, p > 0.2761) (Table 6).
Table 4.
Statistical comparison (student’s t test) for tensile bond strengths of luting agents between cast crown and cast core, composite core and glass ionomer core specimens cemented with resin cement (n = 5)
| Cement | Core material | Mean | Standard deviation | |t| value | p value | Remarks |
|---|---|---|---|---|---|---|
| Resin cement | CR | 27.33 | 1.131 | 15.77 | 0.0000 | S |
| BR | 42.81 | 1.880 | ||||
| CR | 27.33 | 1.131 | 16.56 | 0.0000 | S | |
| GR | 37.22 | 0.7095 | ||||
| BR | 42.81 | 1.880 | 6.22 | 0.0003 | S | |
| GR | 37.22 | 0.7095 |
S Significant
Table 5.
Statistical comparison (student’s t test) for tensile bond strengths of luting agents between cast crown and cast core, composite core and glass ionomer core specimens cemented with glass ionomer cement (n = 5)
| Cement | Core material | Mean | Standard deviation | |t| value | p value | Remarks |
|---|---|---|---|---|---|---|
| Glass ionomer cement | CG | 26.86 | 2.04 | 5.18 | 0.0008 | S |
| BG | 34.70 | 2.69 | ||||
| CG | 26.86 | 2.04 | 3.17 | 0.0132 | S | |
| GG | 31.37 | 2.43 | ||||
| BG | 34.70 | 2.696 | 2.05 | 0.0742 | NS | |
| GG | 31.37 | 2.436 |
S Significant, NS Non significant
Table 6.
Statistical comparison (student’s t test) for tensile bond strengths of luting agents between cast crown and cast core, composite core and glass ionomer core specimens cemented with polycarboxylate cement (n = 5)
| Cement | Core material | Mean | Standard deviation | |t| value | p value | Remarks |
|---|---|---|---|---|---|---|
| Polycarboxylate cement | CP | 22.19 | 0.8188 | 2.13 | 0.0655 | NS |
| BP | 19.72 | 2.463 | ||||
| CP | 22.19 | 0.8188 | 2.70 | 0.0269 | S | |
| GP | 21.03 | 0.5025 | ||||
| BP | 19.72 | 2.463 | 1.17 | 0.2761 | NS | |
| GP | 21.03 | 0.5025 |
S Significant, NS Non significant
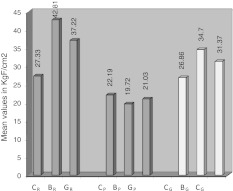
The results of the study indicated significant differences between the tensile bond strengths of specimens in Group C (cast core), Group B (composite core) and Group G (glass ionomer core) cemented with resin cement, polycarboxylate cement and glass ionomer cement (Graph 1).
Graph 1.
Tensile bond strengths values of luting agents between cast crown and cast core, composite core and glass ionomer core specimens cemented with resin cement, polycarboxylate cement and glass ionomer cement
Discussion
The coronal cast metal restoration continues to be used commonly to restore a coronally mutilated, endodontically treated tooth. The bond strength of a luting agent to dentin is an important consideration in the success of cast restoration [3, 5, 9, 10]. It is equally important that the bond strengths of luting agents to various core materials be within the range of clinical acceptability [2, 4–7, 11].
The tensile bond strengths of specimens in cast core, composite core and glass ionomer core cemented with resin cement and glass ionomer cement were statistically significant. On the contrary specimens cemented with polycarboxylate cement showed no statistically significant difference in tensile bond strengths.
Based on the results of the present study, it was inferred that specimens cemented with resin cement in cast core, composite core and glass ionomer core had significantly higher tensile bond strengths than their counterparts cemented with polycarboxylate cement and glass ionomer cement in the respective core groups (Graph 1). These observations of the present study are in accordance with other studies in which the resin adhesive cement yielded highest bond strength with base metal core and composite resin core [4, 12–14].
The specimens in cast core, composite core and glass ionomer core group cemented with resin cement exhibited the highest tensile bond strengths followed by glass ionomer cement and polycarboxylate cement. This may be attributed to the fact that most of the resin cements require dentin bonding agents to promote adhesion to the tooth structure and other restorative materials. The adhesive monomer present in the bonding agent and resin cement contains HEMA, 4-META and organophosphate such as 10-methacryloxydecamethylene phosphoric acid (MDP). The resin cements are used in combination with metal primer which contains an adhesive promoter. Naturally formed oxide on the base metal surface contributes to the bonding when MDP or 4-META resin cements are used. Glass ionomer and polycarboxylate cement yielded lesser bond strength due to their brittle nature, susceptibility to tensile fracture and relatively high film thickness as compared to adhesive resin cements [1, 15].
A comparison of luting agents leads to the conclusion that resin adhesive cement is the most acceptable cementing medium. Its tensile bond strength was significantly greater than all the other core materials tested. Such cements will need further research with clinical study before their wide spread use can be fully supported.
Conclusion
1. The results of the study revealed that the specimens cemented with resin cement in cast core, composite core, and glass ionomer core exhibited significantly higher bond strengths as compared to specimens cemented with glass ionomer and polycarboxylate cement.
2. Composite resin core and resin cement combinations were superior to all other cement and core combinations tested. The optimum tensile bond strength for clinical success need to be ascertained for different luting agents and different core materials used for cast crown restorations.
Contributor Information
Ramesh P. Nayakar, Email: ramesh_nayakar2k@rediffmail.com
Narendra P. Patil, Email: drnppatil@yahoo.com
K. Lekha, Email: lekhakp@yahoo.com
References
- 1.Rosensteil SF, Land MF, Crispin BJ. Dental luting agents: a review of the current literature. J Prosthet Dent. 1998;80:280–301. doi: 10.1016/S0022-3913(98)70128-3. [DOI] [PubMed] [Google Scholar]
- 2.Chan KC, Azarbal P, Kerber PE. Bond strength of cements to crown bases. J Prosthet Dent. 1981;46:297–299. doi: 10.1016/0022-3913(81)90217-1. [DOI] [PubMed] [Google Scholar]
- 3.Worley JL, Hamm RC, Fraunhofer JA. Effects of cement on crown retention. J Prosthet Dent. 1982;48:289–291. doi: 10.1016/0022-3913(82)90013-0. [DOI] [PubMed] [Google Scholar]
- 4.Dilts WE, Duncanson MG, Miranda FJ, Brackett SE. Relative shear bond strengths of luting media with various core materials. J Prosthet Dent. 1985;53:505–508. doi: 10.1016/0022-3913(85)90635-3. [DOI] [PubMed] [Google Scholar]
- 5.Hormati AA, Denehy GE. Retention of cast crowns cemented to amalgam and composite resin cores. J Prosthet Dent. 1981;45:525–528. doi: 10.1016/0022-3913(81)90040-8. [DOI] [PubMed] [Google Scholar]
- 6.Moody CR, Dewald JP, Ferracane JL. Comparative study of luting agents with composite resin cores. J Prosthet Dent. 1989;62:527–529. doi: 10.1016/0022-3913(89)90072-3. [DOI] [PubMed] [Google Scholar]
- 7.DeWald JP, Moody CR, Ferracane JL, Cotmore JM. Crown retention: a comparative study of core type and luting agent. Dent Mater J. 1987;3:71–73. doi: 10.1016/S0109-5641(87)80007-6. [DOI] [PubMed] [Google Scholar]
- 8.Paige H, Hirsch SM, Gelb MN. Effect of temporary cements on crown-to-composite resin core bond strengt. J Prosthet Dent. 1986;55:49–52. doi: 10.1016/0022-3913(86)90072-7. [DOI] [PubMed] [Google Scholar]
- 9.Ayad MF, Rosensteil SF, Salama M. Influence of tooth surface roughness and type of cement on retention of complete cast crown. J Prosthet Dent. 1997;77:116–121. doi: 10.1016/S0022-3913(97)70223-3. [DOI] [PubMed] [Google Scholar]
- 10.Millstein PL, Nathanson D. Effects of temporary cementation on permanent cement retention to composite resin cores. J Prosthet Dent. 1992;67:856–859. doi: 10.1016/0022-3913(92)90601-6. [DOI] [PubMed] [Google Scholar]
- 11.Arcoria CJ, DeWald JP, Moody CR, Ferracane JL. A comparative study of the bond strengths of amalgam and alloy-glass ionomer cores. J Oral Rehab. 1989;16:301–307. doi: 10.1111/j.1365-2842.1989.tb01345.x. [DOI] [PubMed] [Google Scholar]
- 12.Bayindir YZ, Bayindir F, Akyil SM. Bond strength of permanent cements in cementing cast to crown different core buildup materials. Dent Mater J. 2004;23:117–120. doi: 10.4012/dmj.23.117. [DOI] [PubMed] [Google Scholar]
- 13.Yoshida K, Greener EH, Lautenschlager EP. Shear bond strengths of two luting cements to laboratory-cured prosthetic resin composite. Am J Dent. 1993;6:13–16. [PubMed] [Google Scholar]
- 14.Al-Quoud OA, Millstein P, Nathanson D. Effects of thermal cycling on retention of different cement/core material combinations. J Dent Res. 1989;68:955–957. [Google Scholar]
- 15.Anusavice KJ (2006) Dental cements in skinners science of dental materials, 11th edn. W.B. Saunders, Philadelphia, pp 755–756