Abstract
Background
Identification of risk factors for loss of meaning in life among older adults is needed. In the current paper, we test hypotheses derived from the Interpersonal Theory of Suicide concerning the role of perceptions that one is a burden on others as a risk factor for lower meaning in life.
Methods
A prospective design was used to examine the temporal associations between perceptions of burdensomeness on others and perceived meaning in life among older adults (n = 65) seeking mental health treatment (primarily for depression and/or anxiety) at an outpatient geriatric mental health clinic. Participants completed self-report questionnaires within a month following intake. Follow-up questionnaires were completed over the phone two months later.
Results
Perceived burdensomeness predicted lack of meaning in life two months later, while accounting for depression severity. In contrast, baseline levels of meaning in life did not significantly predict levels of burdensomeness at two months.
Conclusion
The findings suggest that burdensomeness may contribute to suicide morbidity and mortality in late-life by eroding meaning in life. Empirically supported treatments for late-life depression could be adapted to focus on perceptions of burdensomeness and its connections with meaning in life.
Keywords: meaning in life, elderly, older adults, interpersonal theory of suicide
Creating, finding, and sustaining meaning in life is considered a key ingredient in psychological well-being across the lifespan (Fegg, Kramer, L'Hoste, & Borasio, 2008; Pinquart, 2002; Steger, Frazier, Oishi, & Kaler, 2006; Steger, Oishi, & Kashdan, 2009). Meaning in life is also targeted in several psychotherapies to help clients reduce distress and manage crises effectively (H. M. Chochinov, 2002; Linehan, 1993; Pot et al., 2010). Given the challenges of aging such as social losses and role changes (Pinquart, 2002), meaning in life is an especially salient component of well-being in older adulthood. Research indicates that older adults, on average, report higher levels of meaning in life (Steger, et al., 2009) and that an absence of meaning is empirically associated with depression (Hedberg, Gustafson, Alex, & Brulin, 2010), suicidal ideation (Heisel & Flett, 2006), and premature mortality (Boyle, Barnes, Buchman, & Bennett, 2009). In the suicide literature, meaning in life has been conceptualized as a protective factor against suicide risk (Heisel & Flett, 2006) because, in cognitive terms, one's life has value or purpose. This belief is relatively stable and generally withstands the ups and downs of daily stressors (Baumeister & Vohs, 2001).
Preventing the loss of meaning in late life could thus have health benefits. Research on risk factors for loss of meaning in late life is needed. In the current paper, we test hypotheses derived from the Interpersonal Theory of Suicide (Van Orden et al., 2010) concerning the role of perceptions that one is a burden on others. The Interpersonal Theory of Suicide posits that perceived burdensomeness is a mental state characterized by the belief that others would “be better off if I were gone.” Among older adults, the association between perceived burdensomeness and greater severity of suicidal ideation holds even after controlling for other risk factors for suicide, including depression and hopelessness (Jahn, Cukrowicz, Linton, & Prabhu, 2011; Yerevanian, Feusner, Koek, & Mintz, 2004). Among older adults with advanced illness, perceived burdensomeness is associated with emotional distress, loss of dignity, and reduced well-being (Akechi et al., 2004a; Chio, Gauthier, Calvo, Ghiglione, & Mutani, 2005; Harvey Max Chochinov et al., 2005; H. M. Chochinov et al., 2007; Ganzini, Johnston, & Hoffman, 1999; Simmons, 2007; Wilson, Curran, & McPherson, 2005), as well as interest in euthanasia or physician-assisted suicide (Akechi et al., 2004b; Berkman, Cavallo, Chesnut, & Holland, 1999; Wilson et al., 2007), suicide ideation (Akechi, et al., 2004b), and suicide (Filiberti et al., 2001).
Grounded in the Interpersonal Theory of Suicide, we hypothesized that perceived burdensomeness would erode meaning in life and that this association would persist above and beyond the contribution of depressive symptoms to meaning in life. Given the cross-sectional associations between depressive symptoms and low meaning (Hedberg, Gustafson, & Brulin, 2010) and the strong contribution of depression to suicide risk in late-life, it is essential to demonstrate that the relationship between perceived burdensomeness and meaning in life is not solely due to depression. Thus, we predicted a significant prospective association between baseline levels of perceived burdensomeness and subsequent levels of meaning in life two months later and also predicted that this association would persist when including associations between baseline depression and both burdensomeness and meaning in life two months later. Further, we did not expect the reverse directional association (i.e., between meaning in life and subsequent perceptions of burdensomeness), because our theoretical model conceptualizes burdensomeness as the causal factor.
Methods
Participants
Participants were sixty-five adults 60 years of age and older newly (< 1 month after intake session) receiving mental health treatment at a university-affiliated outpatient clinic. They had a mean age of 69 years (SD = 8.2 years, range = 60-88 years) and 60% were female. Of those sampled, 83.1% were Caucasian, 13.8% were African American, and 3.1% were mixed race. Prior to the research interview, chart diagnoses were made by an intake clinician (most often a clinical social worker). Patients with dementia, schizoaffective disorder, or schizophrenia were ineligible. Fifty-nine participants were diagnosed with a primary mood disorder (90.8%) and 6 with an anxiety disorder (9.2%). 30 participants were diagnosed with two or more Axis I disorders (46.1%). The majority of participants reported that they either lived alone (43%) or with a spouse (38%). The remaining participants reported living with children or other family, and one participant reported living in a convent with religious sisters.
Measures
Depression symptom severity was measured with the Patient Health Questionnaire (PHQ-9), which is a 9-item measure of depression severity corresponding to the 9 criteria upon which the diagnosis of DSM-IV depressive disorders is based. Items are scored from “0” (not at all) to “3” (nearly every day).”
Perceived Burdensomeness was measured with a 6-item subscale from the Interpersonal Needs Questionnaire-Revised (Gable, Reis, & Elliot, 2000). Perceived burdensomeness reflects the extent to which individuals feel like a burden on others. Items are as follows: “The people in my life would be better off if I were gone; the people in my life would be happier without me; I think I am a burden on society; my death would be a relief to the people in my life; the people in my life wish they could be rid of me; I make things worse for the people in my life.” Respondents indicate the degree to which each item is true for them on a Likert-type scale ranging from “1” (not at all true for me) to “7” (very true for me). Scores are coded such that higher scores represent greater levels of perceived burdensomeness. Data are supportive of the construct validity and reliability of scores derived from the INQ (Gable, et al., 2000). Internal consistencies at time 1 and at follow-up are .90 and .88, respectively (Cronbach's alpha).
Meaning in Life was measured with the 8-item “meaning in life” subscale from the Geriatric Suicide Ideation Scale (Heisel & Flett, 2006) assessing one's perception of meaning or purpose in life. Items are scored on a Likert scale from “1” (strongly disagree) to “5” (strongly agree). High scores reflect a lack of meaning in life. Research has supported the construct validity and reliability of scores derived from the GSIS (Heisel & Flett, 2006). Sample items include, “I feel that my life is meaningful” (reversed), “I am certain that I have something to live for” (reversed), and “I have come to accept life with all its ups and downs.” Internal consistencies at time 1 and at follow-up are .92 and .93, respectively.
Procedures
The current investigation is part of a larger, on-going study that assessed depression and decision-making in late-life. From April 2008 to April 2010, clerical staff members distributed letters of invitation to new patients immediately preceding their initial clinic appointment. . Interested participants who were 60 years of age or older, and English speaking were then contacted by a member of the research team. Of the 396 eligible patients invited to participate, 156 agreed to be contacted by a research assistant and 93 provided informed consent to participate in a research study.
Study entry interviews took place at the clinic or at the participants’ residence, according to their preference. Demographics, as well as study entry levels of depression, perceived burdensomeness, and meaning in life were assessed within one month following initial presentation to the clinic. Depression was assessed in-person with the PHQ-9. Burdensomeness and meaning in life were assessed via paper and pencil and mailed back to the investigators (due to time constraints for the interviews). Follow-up phone interviews were conducted two months later to re-assess depression, perceived burdensomeness, and meaning in life (Time 2). Of the 93 participants who completed Time 1 in-person interviews, 74 returned the self-report questionnaires via mail and 65 completed the follow-up phone interviews. Those who completed the Time 1 mail home packet did not differ from those who did not (i.e., all “small” effect sizes) on age (d=.11), gender (h=.19), or depression severity (d=.07). Those who completed the follow-up interview did not differ from those who did not (i.e., all “small” effect sizes) on baseline perceived burdensomeness (d=.24) or meaning in life (d=.31).
During the two month follow-up period, treatment provided to participants in the study consisted of psychotropic medication monitored by nurse practitioners and supportive psychotherapy provided by clinical social workers, both provided every two to three weeks.
Data Analytic Strategy
A regression model with seven observed variables was constructed, with five baseline variables—burdensomeness, depression, meaning in life, age, and gender—each predicting meaning in life two months later (as well as burdensomeness two months later). Mplus version 5.0 was used, with the robust maximum likelihood (MLR) estimator.
Results
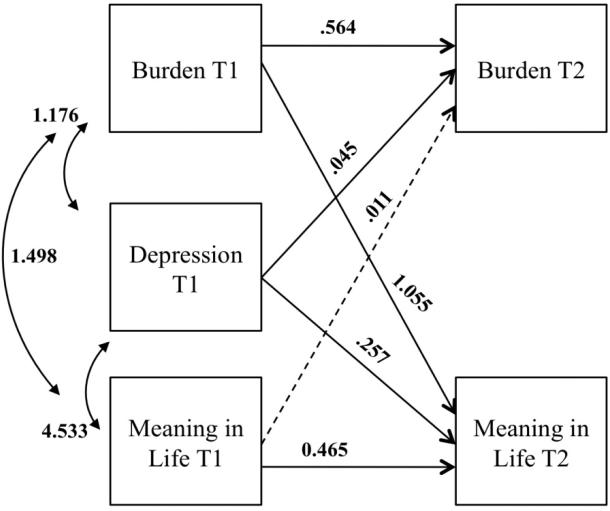
Descriptive statistics, including correlations between all observed variables, are presented in Table 1. The mean perceived burdensomeness score dropped .26 points (on a 7-pt scale), indicating a small, but statistically significant change over the two-month follow-up period (t = 2.38, p < .05). Meaning in life did not evidence statistically significant change (t = 1.36, p = ns). Results from the regression model are presented in Table 2 and graphically in Figure 1. Fit statistics are not presented as the model is fully saturated. All three variables—burdensomeness, depression, and meaning in life—were significantly associated at Time 1. Further, baseline levels of burdensomeness significantly predicted burdensomeness two months later and baseline levels of meaning in life significantly predicted meaning in life two months later. Age and gender were not significant predictors of perceived burdensomeness or meaning in life.
Table 1.
Descriptive Statistics
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| 1 | Age | ----- | ||||||
| 2 | Burden Time 1 | -.19 | ----- | |||||
| 3 | Burden Time 2 | -.06 | 73** | ----- | ||||
| 4 | MIL 1 | -.26* | .55** | 42** | ----- | |||
| 5 | MIL 2 | -.06 | .60** | .62** | 69** | ----- | ||
| 6 | PHQ-9 1 | -.27* | .50** | 48** | .45** | .52** | ----- | |
| 7 | PHQ- 9 2 | -.15 | .45** | .59** | .29* | .55** | .62** | |
| Mean | 69.2 | 2.0 | 1.7 | 17.7 | 17.0 | 8.3 | 7.6 | |
| SD | 8.2 | 1.2 | 1.1 | 6.4 | 5.6 | 5.8 | 5.5 | |
| Range | 60-88 | 1.0-5.0 | 1.0-6.0 | 8.0-34.0 | 8.0-31.0 | 0-21.0 | 0-23.0 |
Note: N = 65; Burden = Interpersonal Need Questionnaire- Perceived Burdensomeness subscale; MIL = Geriatric Suicide Ideation Scale- Meaning in Life Subscale; PHQ-9 = Patient Health Questionnaire 9.
Higher MIL scores suggest lower perceived meaning in life.
Significant change was not observed in either depression (t = 1.09, p = ns) nor meaning in life (t = 1.24, p = ns) scores from Time 1 to Time 2.
p < 0.05.
p < 0.01.
Table 2.
Unstandardized Regression Coefficients
| Unstandardized estimate | Standard error | p | ||
|---|---|---|---|---|
| Endogenous variable | Exogenous variable | |||
| Burden T2 | Burden T1 | 0.564 | 0.908 | 0.000 |
| Meaning T1 | 0.011 | 0.020 | 0.581 | |
| Depression T1 | 0.045 | 0.020 | 0.021 | |
| Age | 0.014 | 0.012 | 0.245 | |
| Gender | -0.208 | 0.192 | 0.279 | |
| Meaning T2 | Burden T1 | 1.055 | 0.481 | 0.028 |
| Meaning T1 | 0.465 | 0.075 | 0.000 | |
| Depression T1 | 0.257 | 0.085 | 0.002 | |
| Age | 0.100 | 0.069 | 0.148 | |
| Gender | -1.017 | 0.962 | 0.290 | |
| Covariances | ||||
| Burden T1 | Meaning T1 | 1.498 | 0.373 | 0.000 |
| Depression T1 | 1.176 | 0.928 | 0.000 | |
| Depression T1 | Meaning T1 | 4.533 | 1.569 | 0.004 |
| Burden T2 | Meaning T2 | 0.655 | 0.295 | 0.027 |
Note. One item in the GSIS meaning in life subscale has some content overlap with the perceived burdensomeness scale (i.e., “Others need me”). Therefore the path analysis was run with this item removed from the meaning in life subscale. The same pattern of results was obtained, including significance values. Thus, results from the model with the full GSIS subscale are presented.
Figure 1. Graphical depiction of regression model.
Note: As age and gender were not significant predictors of Time 2 variables, they are not graphically depicted, but were included in the model.
Consistent with our primary hypothesis, baseline levels of perceived burdensomeness significantly predicted meaning in life two months later, with greater perceptions of burdensomeness predicting subsequent lower levels of meaning in life. This finding is depicted graphically in Figure 1 with the solid line from the “Burden T1” box to “Meaning in Life T2” box (unstandardized coefficient = 1.055, as higher scores on the meaning in life subscale are scored to reflect less meaning in life). In contrast, baseline levels of meaning in life (“Meaning in Life T1” box) did not significantly predict levels of burdensomeness at two months (“Burden T2” box), as reflected by the dotted line (unstandardized coefficient .011). Finally, greater levels of depression at baseline (“Depression T1” box) significantly predicted both lower meaning in life (unstandardized coefficient = .257) and greater perceptions of burdensomeness (unstandardized coefficient = .045) two months later.
Discussion
Consistent with predictions derived from the Interpersonal Theory of Suicide, these results indicate a prospective association between perceived burdensomeness and a lack of meaning in life in older adults seeking outpatient treatment for depression or anxiety. This association persisted even after accounting for participants’ depression severity. Given that the association between perceived burdensomeness and meaning in life was prospective and non-spurious (with regards to depression), our results suggest that perceiving oneself as a burden on others in later life may erode (i.e., cause reductions in) one's sense of meaning in life. Meaning in life is a key construct in health promotion efforts for older adults, as it is associated with better physical and mental health, as well as greater well-being in later life. Our results indicate that perceiving oneself as a burden on others may reduce older adults’ sense of meaning in life, placing them at risk for negative health outcomes such as depression and premature mortality.
Findings also provide support for the applicability of the Interpersonal Theory of Suicide to older adults—an area in need of research given the high rates of suicide among this population. Importantly, these results pertain to outcomes that presumably occur earlier in the trajectory towards suicide: previous studies have investigated suicide ideation, attempts, and deaths by suicide as outcomes of perceived burdensomeness. However, the greater lethality of suicidal behaviors in late life (American Association of Suicidology, 2009) necessitates that interventions be implemented earlier in the trajectory to target and reduce factors that cause the development of suicidal states (Jokinen, Martensson, Nordstrom, & Nordstrom, 2008). Thus, by demonstrating an association between perceived burdensomeness and a known correlate of suicidal ideation in late life—a lack of meaning in life—these results suggest that intervention efforts targeting perceived burdensomeness could potentially mitigate suicide risk.
If indeed perceived burdensomeness erodes meaning in life, what are the mechanisms underlying the effect? Greater meaning in life is associated with several indices of a satisfied “need to belong” (Baumeister & Leary, 1995) in later life, including greater perceived social support (Krause, 2007) and greater perceived belongingness (Hicks & King, 2009). Perceptions of burdensomeness may reduce the degree to which relationships and interactions satisfy the need to belong, in turn reducing meaning in life. Future research should examine this hypothesis. Other studies could attempt to identify moderators of the association between burdensomeness and meaning. One possible moderator, inflexible goal pursuits (e.g., not adapting to age-related limitations by changing or reframing goals) (Heckhausen, Wrosch, & Schulz, 2010) may magnify the association between perceived burdensomeness and low meaning in life. Thus, in applying the Interpersonal Theory to late-life suicide, future studies could integrate the theory's hypotheses with theories on developmental processes and aging.
Our results should be considered in light of the study's limitations. First, our sample consisted of older adults seeking care at an outpatient mental health clinic and our results may not generalize to older, more frail, and/or non-treatment seeking populations. Second, our sample size was relatively small and only a single follow-up time point was used, indicating the need for a larger-scale replication. Third, we were not able to conduct structured diagnostic interviews or collect systematic information about treatment provision. Finally, we were unable to measure stressful life events, such as increased disability or onset of physical illness that might predict increases in perceptions that one is a burden on others; measurement of such events represents an avenue for future research.
Despite these limitations, our results address an area of public health importance—factors that contribute to a lack of meaning in life among older adults—and can be used to generate hypotheses about potentially effective mechanisms to improve well-being of older adults. For example, it is possible that the benefit of empirically supported treatments for late-life depression, including problem-solving therapy, interpersonal psychotherapy, and cognitive behavioral therapy, could be enhanced by including a specific focus on perceptions of burdensomeness so that meaning in life is preserved or created. Future studies could also examine the benefit of augmenting such treatments with available interventions focused on increasing meaning and purpose in life, such as life review (Pot, et al., 2010; Westerhof, Bohlmeijer, van Beljouw, & Pot, 2010) and dignity therapy (Bartz, Zaki, Bolger, & Ochsner, 2011). Doing so should not only reduce risk factors for loss of meaning in life—perceived burdensomeness and depression—but also directly restore meaning in life, thereby potentially maximizing health and well-being in later life.
Acknowledgments
This work was supported in part by Grant Nos. T32MH20061 and K24MH072712 from the National Institute of Mental Health.
Contributor Information
Kimberly A. Van Orden, University of Rochester Medical Center
Patricia M. Bamonti, West Virginia University
Deborah A. King, University of Rochester Medical Center
Paul R. Duberstein, University of Rochester Medical Center
References
- Akechi T, Okuyama T, Sugawara Y, Nakano T, Shima Y, Uchitomi Y. Major depression, adjustment disorders, and post-traumatic stress disorder in terminally ill cancer patients: associated and predictive factors. Journal of Clinical Oncology. 2004a;22(10):1957–1965. doi: 10.1200/JCO.2004.08.149. doi: 10.1200/JCO.2004.08.149 JCO.2004.08.149 [pii] [DOI] [PubMed] [Google Scholar]
- Akechi T, Okuyama T, Sugawara Y, Nakano T, Shima Y, Uchitomi Y. Suicidality in terminally ill Japanese patients with cancer. Cancer. 2004b;100(1):183–191. doi: 10.1002/cncr.11890. doi: 10.1002/cncr.11890. [DOI] [PubMed] [Google Scholar]
- American Association of Suicidology Elderly Suicide Fact Sheet Retrieved January 22, 2009. 2009 from http://www.suicidology.org/web/guest/stats-and-tools/fact-sheets.
- Bartz JA, Zaki J, Bolger N, Ochsner KN. Social effects of oxytocin in humans: context and person matter. Trends in cognitive sciences. 2011;15(7):301–309. doi: 10.1016/j.tics.2011.05.002. doi: 10.1016/j.tics.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Leary MR. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin. 1995;117(3):497–529. doi: 10.1037/0033-2909.117.3.497. [PubMed] [Google Scholar]
- Baumeister RF, Vohs KD. The pursuit of meaningfulness in life. In: Snyder CR, Lopez SL, editors. Handbook of positive psychology. Oxford University Press; US; New York, NY: 2001. pp. 608–618. [Google Scholar]
- Berkman CS, Cavallo PF, Chesnut WC, Holland NJ. Attitudes toward physician-assisted suicide among persons with multiple sclerosis. Journal of Palliative Medicine. 1999;2(1):51–63. doi: 10.1089/jpm.1999.2.51. doi: 10.1089/jpm.1999.2.51. [DOI] [PubMed] [Google Scholar]
- Boyle PA, Barnes LL, Buchman AS, Bennett DA. Purpose in life is associated with mortality among community-dwelling older persons. Psychosomatic Medicine. 2009;71(5):574–579. doi: 10.1097/PSY.0b013e3181a5a7c0. doi: 10.1097/PSY.0b013e3181a5a7c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chio A, Gauthier A, Calvo A, Ghiglione P, Mutani R. Caregiver burden and patients’ perception of being a burden in ALS. Neurology. 2005;64(10):1780–1782. doi: 10.1212/01.WNL.0000162034.06268.37. doi: 64/10/1780 [pii] 10.1212/01.WNL.0000162034.06268.37. [DOI] [PubMed] [Google Scholar]
- Chochinov HM. Dignity-conserving care--a new model for palliative care: helping the patient feel valued. JAMA. 2002;287(17):2253–2260. doi: 10.1001/jama.287.17.2253. [DOI] [PubMed] [Google Scholar]
- Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Understanding the Will to Live in Patients Nearing Death. Psychosomatics: Journal of Consultation Liaison Psychiatry. 2005;46(1):7–10. doi: 10.1176/appi.psy.46.1.7. [DOI] [PubMed] [Google Scholar]
- Chochinov HM, Kristjanson LJ, Hack TF, Hassard T, McClement S, Harlos M. Burden to others and the terminally ill. Journal of Pain and Symptom Management. 2007;34(5):463–471. doi: 10.1016/j.jpainsymman.2006.12.012. doi: S0885-3924(07)00343-0 [pii] 10.1016/j.jpainsymman.2006.12.012. [DOI] [PubMed] [Google Scholar]
- Fegg MJ, Kramer M, L'Hoste S, Borasio GD. The Schedule for Meaning in Life Evaluation (SMiLE): validation of a new instrument for meaning-in-life research. Journal of Pain and Symptom Management. 2008;35(4):356–364. doi: 10.1016/j.jpainsymman.2007.05.007. doi: S0885-3924(07)00735-X [pii] 10.1016/j.jpainsymman.2007.05.007. [DOI] [PubMed] [Google Scholar]
- Filiberti A, Ripamonti C, Totis A, Ventafridda V, De Conno F, Contiero P, Tamburini M. Characteristics of terminal cancer patients who committed suicide during a home palliative care program. Journal of Pain and Symptom Management. 2001;22(1):544–553. doi: 10.1016/s0885-3924(01)00295-0. [DOI] [PubMed] [Google Scholar]
- Gable SL, Reis HT, Elliot AJ. Behavioral activation and inhibition in everyday life. Journal of Personality and Social Psychology. 2000;78(6):1135–1149. doi: 10.1037//0022-3514.78.6.1135. [DOI] [PubMed] [Google Scholar]
- Ganzini L, Johnston WS, Hoffman WF. Correlates of suffering in amyotrophic lateral sclerosis. Neurology. 1999;52(7):1434–1440. doi: 10.1212/wnl.52.7.1434. [DOI] [PubMed] [Google Scholar]
- Heckhausen J, Wrosch C, Schulz R. A motivational theory of life-span development. Psychological Review. 2010;117(1):32–60. doi: 10.1037/a0017668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedberg P, Gustafson Y, Alex L, Brulin C. Depression in relation to purpose in life among a very old population: A five-year follow-up study. Aging and Mental Health. 2010;14(6):757–763. doi: 10.1080/13607861003713216. doi: 925182211 [pii] 10.1080/13607861003713216. [DOI] [PubMed] [Google Scholar]
- Heisel MJ, Flett GL. The Development and Initial Validation of the Geriatric Suicide Ideation Scale. The American Journal of Geriatric Psychiatry. 2006;14(9):742–751. doi: 10.1097/01.JGP.0000218699.27899.f9. [DOI] [PubMed] [Google Scholar]
- Hicks JA, King LA. Positive mood and social relatedness as information about meaning in life. The Journal of Positive Psychology. 2009;4(6):471–482. doi: 10.1080/17439760903271108. [Google Scholar]
- Jahn DR, Cukrowicz KC, Linton K, Prabhu F. The mediating effect of perceived burdensomeness on the relation between depressive symptoms and suicide ideation in a community sample of older adults. Aging and Mental Health. 2011;15(2):214–220. doi: 10.1080/13607863.2010.501064. doi: 928354734 [pii] 10.1080/13607863.2010.501064. [DOI] [PubMed] [Google Scholar]
- Jokinen J, Martensson B, Nordstrom AL, Nordstrom P. CSF 5-HIAA and DST non-suppression -independent biomarkers in suicide attempters? Journal of Affective Disorders. 2008;105(1-3):241–245. doi: 10.1016/j.jad.2007.04.008. doi: 10.1016/j.jad.2007.04.008. [DOI] [PubMed] [Google Scholar]
- Krause N. Longitudinal study of social support and meaning in life. Psychology and Aging. 2007;22(3):456–469. doi: 10.1037/0882-7974.22.3.456. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. Guilford; New York: 1993. [Google Scholar]
- Pinquart M. Creating and maintaining purpose in life in old age: a meta-analysis. Ageing International. 2002;27(2):90–110. [Google Scholar]
- Pot AM, Bohlmeijer ET, Onrust S, Melenhorst AS, Veerbeek M, De Vries W. The impact of life review on depression in older adults: a randomized controlled trial. International Psychogeriatrics. 2010;22(4):572–581. doi: 10.1017/S104161020999175X. doi: S104161020999175X [pii] 10.1017/S104161020999175X. [DOI] [PubMed] [Google Scholar]
- Simmons LA. Self-perceived burden in cancer patients: validation of the Self-perceived Burden Scale. Cancer Nursing. 2007;30(5):405–411. doi: 10.1097/01.NCC.0000290816.37442.af. doi: 10.1097/01.NCC.0000290816.37442.af 00002820-200709000-00012 [pii] [DOI] [PubMed] [Google Scholar]
- Steger MF, Frazier P, Oishi S, Kaler M. The meaning in life questionnaire: Assessing the presence of and search for meaning in life. Journal of Counseling Psychology. 2006;53(1):80–93. doi: 10.1037/0022-0167.53.1.80. [Google Scholar]
- Steger MF, Oishi S, Kashdan TB. Meaning in life across the life span: Levels and correlates of meaning in life from emerging adulthood to older adulthood. The Journal of Positive Psychology. 2009;4(1):43–52. doi: 10.1080/17439760802303127. [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr. The Interpersonal Theory of Suicide. Psychological Review. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerhof GJ, Bohlmeijer ET, van Beljouw IM, Pot AM. Improvement in personal meaning mediates the effects of a life review intervention on depressive symptoms in a randomized controlled trial. Gerontologist. 2010;50(4):541–549. doi: 10.1093/geront/gnp168. doi: gnp168 [pii] 10.1093/geront/gnp168. [DOI] [PubMed] [Google Scholar]
- Wilson KG, Chochinov HM, McPherson CJ, Skirko MG, Allard P, Chary S, Clinch JJ. Desire for euthanasia or physician-assisted suicide in palliative cancer care. Health Psychology. 2007;26(3):314–323. doi: 10.1037/0278-6133.26.3.314. doi: 2007-06671-009 [pii] 10.1037/0278-6133.26.3.314. [DOI] [PubMed] [Google Scholar]
- Wilson KG, Curran D, McPherson CJ. A burden to others: a common source of distress for the terminally ill. Cognitive Behaviour Therapy. 2005;34(2):115–123. doi: 10.1080/16506070510008461. [DOI] [PubMed] [Google Scholar]
- Yerevanian BI, Feusner JD, Koek RJ, Mintz J. The dexamethasone suppression test as a predictor of suicidal behavior in unipolar depression. Journal of Affective Disorders. 2004;83(2-3):103–108. doi: 10.1016/j.jad.2004.08.009. doi: 10.1016/j.jad.2004.08.009. [DOI] [PubMed] [Google Scholar]