Abstract
Objective
To examine the association between residential segregation and geographic access to primary care physicians (PCPs) in metropolitan statistical areas (MSAs).
Data Sources
We combined zip code level data on primary care physicians from the 2006 American Medical Association master file with demographic, socioeconomic, and segregation measures from the 2000 U.S. Census. Our sample consisted of 15,465 zip codes located completely or partially in an MSA.
Methods
We defined PCP shortage areas as those zip codes with no PCP or a population to PCP ratio of >3,500. Using logistic regressions, we estimated the association between a zip code's odds of being a PCP shortage area and its minority composition and degree of segregation in its MSA.
Principal Findings
We found that odds of being a PCP shortage area were 67 percent higher for majority African American zip codes but 27 percent lower for majority Hispanic zip codes. The association varied with the degree of segregation. As the degree of segregation increased, the odds of being a PCP shortage area increased for majority African American zip codes; however, the converse was true for majority Hispanic and Asian zip codes.
Conclusions
Efforts to address PCP shortages should target African American communities especially in segregated MSAs.
Keywords: Primary care, racial, ethnic, health care disparities, segregation, physician shortage
Numerous studies have explored the relationship between residential segregation and racial disparities in health. Some scholars have concluded that segregation is a fundamental cause of health disparities (Acevedo-Garcia 2000, 2001; Williams and Collins 2001; Morello-Frosch and Jesdale 2006). Prior research has found associations between residential segregation and infant mortality, adult mortality, poor health status, smoking during pregnancy, poor birth outcomes, TB and other infectious diseases, and exposure to cancer-causing air toxins (Yankauer 1950; LaVeist 1989, 1993, 2003; Polednak 1991, 1996a,b; Morello-Frosch and Jesdale 2006; Bell, Zimmerman, and Mayer 2007; Osypuk and Acevedo-Garcia 2008). The impacts of segregation are not limited to the United States, researchers have found that racial and economic segregation negatively affect health in South Africa, Rio De Janeiro, London, and Helsinki (Wyndham 1981; Christopher 1993; Szwarcwald et al. 2002; Myer, Ehrlich, and Susser 2004; Stafford et al. 2004).
The association between residential segregation and health care resources is not well studied. We hypothesize that the impact of segregation on minority access to health care is similar to its negative impact on minority access to quality jobs, education, safety, and social networks (Smith 1999; Charles 2003). Morrison and colleagues found an association between segregation and the availability of pharmacy services to minority communities (Morrison et al. 2000). Nursing homes and hospitals serving minority communities were at greater risk of closure and reductions in services compared to those serving white communities (Gaskin 1997; Feng et al. 2011) and segregation resulted in the concentration of blacks in poor-performing nursing homes (Smith et al. 2007). Similarly, residential segregation is correlated with racial segregation of elderly minority black patients in relatively fewer hospitals resulting in black patients receiving lower quality care for some hospital services (Smith 1998; Jha, Orav, and Epstein 2007; Gaskin et al. 2011).
Racial and ethnic disparities in primary care are well documented (U.S. Department of Health, Human Services, Agency for Healthcare Research and Quality 2008). In addition to socioeconomic factors, disparities in primary care may be due in part to geographic barriers to care (Shi 1999; Smedley, Stith, and Nelson 2003; Mayberry, Mili, and Ofili 2005; Gaskin et al. 2009). However, not much is known about the extent to which minorities face geographic barriers to care in comparison to whites. Disparities in health care may be caused by higher proportions of minorities living in “medical deserts,” that is, communities with limited health care resources. However, minorities may have better geographic access to care because they tend to live in the center cities near major teaching hospitals and federally qualified community health centers. Prior research has found that minorities relied more on community health centers, hospital outpatient departments and emergency rooms for their usual source of care in comparison to whites (Lillie-Blanton, Martinez, and Salganicoff 2001; Gaskin et al. 2007). These providers are more accessible to low-income minorities because they receive federal and state government subsidies to finance indigent care, whereas private physicians must absorb most of the cost of free or discounted services.
Nationally, there is a shortage of primary care physicians (Bodenheimer 2006; Dill and Salsberg 2008). The proportion of physicians practicing primary care has steadily declined and interest among U.S. medical school graduates in entering primary care has dropped (Freed and Stockman 2009; Lakhan and Laird 2009). Lower reimbursement for primary care relative to specialty care is listed as a primary cause for this trend (Freed and Stockman 2009; Steinbrook 2009). To supply our current demand for primary care services, the United States is reliant on internationally trained physicians, especially minority communities (Dill and Salsberg 2008). Foreign-born and internationally trained physicians disproportionately serve minority and underserved communities. This study explores whether minorities differentially face geographic barriers to primary care physicians.
Conceptual Framework
Fundamental cause theory is a useful framework for understanding why minority communities may have limited access to primary care physicians (Link and Phelan 1995). Although the theory has been employed to explain how social mechanisms operate to increase socioeconomic disparities in disease outcomes, it can be extended to understand how other mechanisms of structural inequality, such as residential segregation, operate to influence access and use of health care services. Fundamental cause theory contends that social causes have persistent associations with disease despite changes in intervening mechanisms (i.e., sanitation) because they affect access to resources that can be used to avoid risk or to minimize the consequences of disease once it occurs. “Fundamental causes” such as socioeconomic status, race, ethnicity, gender, and structural constraints such as residential segregation are tied to resources like money, power, prestige, and social connectedness where those with the most access and control over resources are in a better position to avoid risks, diseases, and the consequences of disease. This is consistent with theories of social determinants of health and social exclusion that explain the deleterious effects of the marginalization of minorities and other vulnerable populations (White 1998; Nazroo and Williams 2006; Shaw, Dorling, and Smith 2006). African American communities bear higher health risks because segregation results in lower quality of public safety, transportation services, garbage collection, public schools, restaurants, and other community amenities (Massey, Condran, and Denton 1987; Massey and Fong 1990; Massey and Denton 1993; Alba, Logan, and Bellair 1994). These health risks are further increased if minorities residing in segregated neighborhoods have limited access to primary care physicians and other health care services.
Economic theory can help explain why segregation affects the availability of physician care because of its impact on health care markets. The racial composition of neighborhood influences the demand for health care because it is correlated with the ability to pay for health care services. Higher proportions of African Americans and Hispanics are covered by Medicaid or are uninsured. Also, African Americans and Hispanics have lower incomes and are therefore less able to pay for services out-of-pocket. In addition to lower reimbursement under Medicaid (Mitchell 1991; Perloff et al. 1997; Bronstein, Adams, and Florence 2004), physicians also may be concerned about delays in receiving payment (Cunningham and O'Malley 2009). Physicians operating in minority communities would tend to have higher proportions of Medicaid and uninsured patients in their payer mix. This constrains their ability to provide high-quality care to their patients and refer their patients for specialty care (Reschovsky and O'Malley 2007). The supply of physicians and other health care providers in minority neighborhoods may be affected by lower quality of community amenities. The lack of commercial development in minority communities may reduce area physicians' access to commercial enterprises, medical laboratories, medical supply companies, financing and credit for small businesses, internet/broadband, and other communication services. This may discourage physicians from locating in minority communities because the limited availability of resources may increase the costs of operating a practice.
Residential segregation may lower the demand for primary care services (Gaskin et al. 2012). Neighbors and social networks in general may influence individuals' decision to use health care services. Segregation limits the social networks available to minorities particularly those with low incomes (Wilson 1987). Cornwell and Cornwell (2008) found that minorities compared to whites had less informal access to medical experts because of the size and composition of their social networks. Studies report that higher rates of perceived discrimination and lower rates of trust in medical providers among African Americans and Hispanics compared to whites contributed to disparities in health care use (LaVeist, Nickerson, and Bowie 2000; LaVeist, Rolley, and Diala 2003; Johnson et al. 2004; Casagrande et al. 2007; Burgess et al. 2008; Hausmann et al. 2010). Because of segregation, minorities may have relatively fewer peers who would encourage health care use and relatively more peers who may have negative experiences with the health care system. This could result in lower overall demand for health care services in minority communities regardless of their ability to pay.
Data and Methodology
This study combined data from the 2006 American Medical Association Master File and the 2000 U.S. Census Summary File 1 and Summary File 3. Specifically, we obtained counts of primary care physicians for each zip code located fully or partially in metropolitan statistical area (PMSA/MSA). Primary care physicians (PCPs) were defined as those whose primary specialties were family practice, general practice, internal medicine, pediatrics, adolescent medicine, obstetrics, and gynecology. We linked these data to demographic and socioeconomic information from 2,000 U.S. Census. The demographic variables were total population, percent female, racial, and age distributions. The socioeconomic variables were percent poverty status, educational attainment, and home ownership. For each zip code we computed the population to primary care physician ratio and defined PCP shortage areas as those zip codes where the population to PCP ratio was >3,500 or those zip codes that did not have a PCP. This threshold is consistent with the Health Resources and Services Administration's designation of Primary Medical Care Health Professional Shortage Areas (HPSA). (See http://bhpr.hrsa.gov/shortage/primarycare.htm). Because it may be convenient for some residents to obtain care outside their zip code if their zip code is small or they live near the boundary, we conducted a sensitivity analysis using a more conservative measure. We computed the ratio of the population to the number of PCPs within three miles of the zip code. Zip codes were designated as shortage areas if it met the definition for its population to PCP ratio and its 3-mile population to PCP ratio. This second measure tends to exclude zip codes in densely populated areas with relatively few PCPs that are adjacent to zip codes with a relative abundance of PCPs.
The Sample
The unit of observation was the zip code tabulation areas (ZCTAs). For the 2,000 Census, U.S. Census Bureau developed ZCTAs to correspond to U.S. Postal Service (USPS) ZIP code areas. (For ease of composition we will refer to ZCTAs as zip codes.) We started with 33,178 zip codes. We dropped 1,140 zip codes that ended in “HH” and “XX”, that is, those designating water or rural areas with little settlement. We dropped 15,914 rural zip codes, excluded 523 urban zip codes with fewer than or equal to 200 residents, and 99 zip codes in Puerto Rico for a total of 15,502. Finally, we only used those zip codes with valid segregation data for each minority group for final sample of 15,465. These zip codes cover 82.7 percent of the U.S. population and over 99 percent of the urban population.
Measuring Segregation
We designated zip codes as majority African American, Asian, or Hispanic where more than 50 percent of the residents were African American non-Hispanic, Asian, or Hispanic, respectively. We used dichotomous variables to define the racial/ethnic composition of a zip code because preliminary analysis suggests that the percentage of minority residents in the zip code has a threshold effect on the availability of physician services. We linked these zip code level data to the MSA/PMSA level measures of segregation published by the Census Bureau for each minority group. (For detailed information about these measures, see http://www.census.gov/hhes/www/housing/housing_patterns/housing_patterns.html.) Specifically, we used five measures of segregation for each race/ethnic minority group: dissimilarity, isolation, spatial clustering, absolute centralization, and relative concentration indices (Massey and Denton 1988; Massey and Denton 1989). The dissimilarity index measures evenness, that is, the proportion of minority residents who would have to change census tracts in order for the population to be evenly distributed. The isolation index measures exposure, that is, the propensity that minorities and whites would come in contact with each other. The clustering index measures the degree to which minorities and whites reside in proximity to one another. The centralization index measures the degree to which minorities live in the urban center. Lastly, the concentration index measures the degree to which minority residents are concentrated within a small geographic area within the MSA. These five dimensions can be collapsed into two concepts: separation and location (Johnston, Poulson, and Forrest 2007). The dissimilarity, isolation, and clustering indices measure separation and may identify the impact of segregation on access to social institutions and community resources. Centralization and concentration indices measure location within the metropolitan area and may identify the impact of neighborhood quality associated with concentrated disadvantage (Morenoff, Sampson, and Raudenbush 2001). The isolation and dissimilarity indices are frequently used in the public health and health service research literature (Shihadeh and Flynn 1996; Collins and Williams 1999; Acevedo-Garcia et al. 2003). However, we explored the association between physician availability and all five dimensions of segregation to identify possible unique effects of each dimension.
Estimation Strategy
We conducted bivariate and multivariate analyses. First, we compared the demographic and economic characteristics of zip codes designated as PCP shortage areas versus PCP adequate areas. We tested whether the mean values of each of the demographic and economic characteristics were statistically different across the two types of zip codes using t-tests. Second, we estimated the association between zip code demographic and economic characteristics using logistic regression. In the base model, the dependent variable was whether the zip code was a PCP shortage area. Our independent variables of interest were the majority African American, Asian, or Hispanic indicators. We controlled for gender and age distribution, education level, poverty status, and degree of home ownership in the zip code. We used MSA/PMSA level fixed effects to control for unobserved state and MSA level factors, for example, medical licensing policies, and presence of medical school and academic medical centers. We estimated random effects models by including MSA/PMSA level factors that influence physician location decisions, that is, the ratios of population to total hospital beds, the presence of a major teaching hospital in the MSA/PMSA, and the average incomes for family and general practitioners, general internists, OBGYNs, and pediatricians.
To determine how residential segregation affected the PCP availability in majority minority zip codes, we estimated five additional models, including the level of segregation in the MSA, one model for each segregation measure. The segregation measures were centered about their respective means; thus, the coefficients can be interpreted relative to zip codes in MSAs with the average levels of segregation. In these models, we estimated the effect of the segregation measure and the interaction between segregation and the majority minority indicator variable on likelihood of PCP shortage. Each minority group was interacted with its own segregation measure. The main effect of segregation (i.e., the coefficients on the segregation measure) captures the impact of segregation on the majority white zip codes. The coefficients on the interaction terms capture the effect that segregation has on majority minority zip codes. We hypothesized that zip codes designated as majority African American, Hispanic, or Asian would have greater odds of being a PCP shortage area compared to majority white zip codes and majority minority zip codes located in segregated MSAs would have greater odds of being a PCP shortage area compared to majority minority zip codes in nonsegregated MSAs.
We conducted three sensitivity analyses. First we estimated our models defining the PCP shortage using the zip code only and then using a 3-mile radius around the zip code. We reported all four models in Table 2. Second, because of potential heteroskedascity, we divided the sample into low- and high-population zip codes. We re-estimated the fixed effect and random effect models. We reported the results for the random effects models in Table 2. Third, we divided PCP shortage zip codes into two categories: those with no PCP, and those with a population to PCP ratio of >3,500. We used multinomial logistic regression to re-estimate the model.
Table 2.
Odds Ratios for Likelihood of a Zip Code Being a Primary Care Physician (PCP) Shortage Area for Demographic and Socioeconomic Characteristics
| PCP Shortage Area within Zip Code | PCP Shortage Area within Zip Code and 3 miles around | PCP Shortage Area within Zip Code and 3 miles around | ||||
|---|---|---|---|---|---|---|
| Fixed Effects Model | Random Effects Model | Fixed Effects Model | Random Effect Model | Fixed Effects for Low-Population Zip Codes | Fixed Effects for High-Population Zip Codes | |
| Majority African American | 1.671*** [1.332 2.095] | 1.590*** [1.276 1.980] | 1.121 [0.840 1.496] | 1.041 [0.790 1.372] | 0.824 [0.535 1.269] | 1.530 [0.943 2.484] |
| Majority Hispanic | 0.734* [0.541 0.996] | 0.784 [0.588 1.045] | 0.470*** [0.325 0.680] | 0.483*** [0.342 0.682] | 0.455** [0.254 0.817] | 0.874 [0.490 1.560] |
| Majority Asian | 0.445 [0.096 2.052] | 0.694 [0.174 2.759] | 0.380 [0.053 2.732] | 0.863 [0.154 4.841] | 0.893 [0.064 12.43] | 0.00002 [0.000 NA] |
| Percent under 17 | 1.183** [1.066 1.300] | 1.237*** [1.122 1.353] | 1.463*** [1.278 1.648] | 1.544*** [1.362 1.726] | 1.286*** [1.118 1.454] | 0.647*** [0.465 0.830] |
| Percent from 45 to 64 | 1.119* [1.019 1.219] | 1.185*** [1.083 1.286] | 1.426*** [1.276 1.576] | 1.526*** [1.372 1.681] | 1.193** [1.058 1.328] | 0.642*** [0.446 0.839] |
| Percent over 65 | 0.690*** [0.631 0.749] | 0.720*** [0.662 0.778] | 0.752*** [0.677 0.827] | 0.772*** [0.699 0.844] | 0.770*** [0.688 0.853] | 0.405*** [0.296 0.513] |
| Poverty rate | 0.986 [0.936 1.035] | 0.985 [0.939 1.032] | 0.985 [0.928 1.042] | 1.000 [0.946 1.055] | 0.967 [0.909 1.025] | 1.259* [1.041 1.476] |
| Near poor rate | 1.191*** [1.128 1.253] | 1.194*** [1.136 1.252] | 1.203*** [1.135 1.271] | 1.244*** [1.177 1.310] | 1.156*** [1.089 1.223] | 1.502** [1.189 1.814] |
| Percent less than HS | 1.798*** [1.668 1.928] | 1.836*** [1.709 1.963] | 1.928*** [1.771 2.086] | 2.023*** [1.863 2.182] | 1.737*** [1.580 1.895] | 2.003*** [1.508 2.498] |
| Percent some HS | 1.626*** [1.518 1.734] | 1.608*** [1.507 1.709] | 1.474*** [1.365 1.583] | 1.485*** [1.380 1.589] | 1.445*** [1.332 1.558] | 1.507*** [1.131 1.884] |
| Percent HS | 2.041*** [1.947 2.136] | 1.994*** [1.906 2.082] | 2.167*** [2.051 2.284] | 2.118*** [2.009 2.227] | 1.828*** [1.722 1.933] | 2.863*** [2.335 3.391] |
| Percent some college | 1.583*** [1.475 1.691] | 1.672*** [1.566 1.778] | 1.559*** [1.437 1.680] | 1.719*** [1.592 1.846] | 1.394*** [1.281 1.508] | 2.367*** [1.722 3.013] |
| Percent female | 0.744*** [0.668 0.820] | 0.708*** [0.640 0.775] | 0.532*** [0.468 0.595] | 0.507*** [0.450 0.563] | 0.700*** [0.610 0.790] | 0.953 [0.688 1.219] |
| Vacancy rate | 1.194*** [1.157 1.230] | 1.181*** [1.147 1.216] | 1.186*** [1.147 1.226] | 1.183*** [1.145 1.221] | 1.140*** [1.10 1.179] | 1.115 [0.955 1.275] |
| Home occupancy rate | 1.189*** [1.158 1.221] | 1.172*** [1.143 1.200] | 1.339*** [1.294 1.384] | 1.336*** [1.295 1.378] | 1.221*** [1.176 1.266] | 1.552*** [1.424 1.681] |
| Population to beds | – | 1.000* [1.000 1.001] | – | 1.000 [1.000 1.001] | – | – |
| Presence of a teaching hospital | – | 0.962 [0.824 1.124] | – | 0.730** [0.607 0.877] | – | – |
| Family/general pract income | – | 1.023 [0.984 1.063] | – | 1.024 [0.979 1.071] | – | – |
| Internist income | – | 0.955 [0.908 1.005] | – | 0.954 [0.898 1.014] | – | – |
| Pediatric income | – | 0.987 [0.948 1.028] | – | 1.004 [0.957 1.053] | – | – |
| OB-GYN income | – | 0.980 [0.935 1.027] | – | 0.949 [0.898 1.004] | – | – |
| Pseudo R2 | – | – | – | – | – | – |
| N | 15450 | 15295 | 15142 | 15295 | 7564 | 5834 |
Odds ratios for continuous variables are based on a five percentage point increase in the factors relative to the reference/omitted group, for example, for the education variables the reference group is percent college graduates.
The sample size varies across the models because the number of groups with all positive and outcomes vary across specifications.
NA - We could not report the upper bound of the confidence interval for majority Asian in the Fixed Effects Model for High Population Zip Codes because the point estimate has a large standard error. This makes the upper bound enormous.
denotes p<0.05
denotes p<0.01
denotes p<0.001.
This research was deemed to non-Human subjects research by the Institutional Review Board of The Johns Hopkins Bloomberg School of Public Health and the University of Maryland.
Results
A large percentage of zip codes (32.0 percent) were PCP shortage areas with two-thirds of these areas with no PCP. While almost a third of urban zip codes were PCP shortage areas, only 16.2 percent of the nation's MSA residents live in these zip codes. The proportion of the population residing in PCP shortage zip codes varied across race and ethnic groups. Only 9.6 percent of Asians and 13.2 percent of whites lived in PCP shortage zip codes, compared to 24.8 percent of African Americans and 24.3 percent of Hispanics. Of zip codes in MSAs, 5.0 percent were majority African American, 3.9 percent were majority Hispanic, and only 0.26 percent was majority Asian. In contrast almost 80 percent of zip codes were fewer than 10 percent African American or 10 percent Hispanic and almost 95 percent of zip codes were less than 10 percent Asian. Large percentages of urban African Americans (40.9 percent) and Hispanics (37.7 percent) live in majority African American and Hispanic zip codes, while only 8.3 percent of Asians live in majority Asian zip codes. (This analysis is not presented in the tables.)
We compared PCP shortage zip codes to PCP adequate zip codes in Table 1. PCP shortage zip codes were statistically different from PCP adequate zip codes across most of the demographic and socioeconomic measures. Majority African American and majority Hispanic zip codes were more likely to be PCP shortage zip areas. Majority Asian zip codes were less likely to be PCP shortage areas. PCP shortage zip codes had higher percentages of poor (12.9 percent versus 10.1 percent) and near poor residents (20.5 percent versus 14.9 percent). Adults living in PCP shortage zip codes had lower levels of education. Surprisingly, PCP shortage zip codes not only had higher home ownership rates but also higher vacancy rates too. PCP shortage zip codes were less likely to be in MSAs with a major teaching hospital, but they were more likely to be in MSAs with higher average annual incomes for pediatricians and family and general practitioners. Among PCP shortage zip codes, those with population to PCP ratio of >3,500 had a different racial composition than zip codes with no PCP. Zip codes with population to PCP ratio of greater than 3,500 were 12.1 percent majority African American and 10.1 percent majority Hispanic compared to 3.3 and 3.7 percent for zip codes with no PCP.
Table 1.
Mean and Standard Deviation of Independent Variables for All Urban Zip Codes and by Whether the Zip Code Is a Primary Care Physician (PCP) Shortage Area
| All Urban Zip Codes | PCP Adequate Zip Codes (Population to PCP ratio < 3,500) (n = 10,539) | PCP Shortage Zip Codes (No Physician or Population to PCP ratio >3,500) (n = 4,963) | |||
|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Mean | p-Value | |
| Majority African American | 5.012 | 2.1820 | 4.441 | 6.226 | <.001 |
| Majority Hispanic | 3.929 | 1.9428 | 3.027 | 5.843 | <.001 |
| Majority Asian | 0.264 | 0.5136 | 0.361 | 0.060 | <.001 |
| Percent under 17 | 25.531 | 5.591 | 24.807 | 27.067 | <.001 |
| Percent from 45 to 64 | 23.119 | 4.706 | 23.170 | 23.011 | .049 |
| Percent over 65 | 12.627 | 5.959 | 12.849 | 12.156 | <.001 |
| Poverty rate | 10.972 | 9.013 | 10.078 | 12.871 | <.001 |
| Near poor rate | 16.659 | 8.118 | 14.857 | 20.488 | <.001 |
| Percent less than HS | 6.943 | 6.822 | 5.886 | 9.188 | <.001 |
| Percent some HS | 11.927 | 6.504 | 10.519 | 14.915 | <.001 |
| Percent HS | 31.116 | 10.675 | 28.246 | 37.209 | <.001 |
| Percent some college | 27.145 | 7.180 | 27.764 | 25.831 | <.001 |
| Percent female | 50.478 | 3.408 | 50.765 | 49.871 | <.001 |
| Vacancy rate | 8.917 | 9.284 | 8.001 | 10.864 | <.001 |
| Home owner occupancy rate | 71.805 | 18.365 | 69.683 | 76.313 | <.001 |
| Population to beds | 392.150 | 141.282 | 399.582 | 376.450 | <.001 |
| Presence of a teaching hospital | 67.486 | 46.844 | 71.478 | 59.054 | <.001 |
| Family/GP income | 151,254 | 18,298 | 150,755 | 152,312 | <.001 |
| Internist income | 162,420 | 16,985 | 162,274 | 162,729 | .120 |
| OB-GYN income | 172,328 | 16,992 | 172,412 | 172,150 | .370 |
| Pediatric income | 141,781 | 21,531 | 141,445 | 142,494 | .005 |
p-values are based on the results of t-tests of the mean values comparing the two samples.
When we used the more conservative 3-mile definition of PCP shortage areas, the number of shortage zip codes declined from 4,963 to 3,968. The more conservative definition excluded zip codes that were more likely to be majority African American (16.3 percent versus 3.7 percent) and majority Hispanics (10.2 percent versus 4.7 percent); had higher poverty rates (16 percent versus 12.1 percent); had a greater population density (4,020 versus 299 per square mile); and had a lower percentage of residents owning a car or truck (59.2 percent versus 76.3 percent).
We reported the odds ratios for the base model in Table 2. In the fixed effect models, we estimated that odds of being a PCP shortage area were 67 percent higher for majority African American zip codes and 27 percent lower for majority Hispanic zip codes. There was no association between majority Asian zip codes and the odds of being a PCP shortage area. The random effects models yielded similar findings for majority African American zip codes (OR = 1.59) and majority Hispanic zip codes (OR = 0.78), although the latter was not statistically significant. These findings were sensitive to how we defined PCP shortage areas. When we used the 3-mile definition, the fixed effects and random effects estimates for majority African American zip codes were not statistically significant and the estimated odds ratios were close to one. However, the odds ratios for majority Hispanic zip codes were significant but stronger with a smaller value (OR = 0.47). This result for majority African American zip codes using the 3-mile shortage area definition was sensitive to the size of the zip code population. In low-population zip codes, we found no association. However, in high-population zip codes, majority African American zip codes were more likely to be PCP shortage areas (OR =1.53); but the estimate was only borderline statistically significant (p = .085). The multinomial logistic analysis indicates the association for majority African American zip codes were primarily associated with having a population to PCP ratio of >3,500 (RRR = 1.65), whereas majority Hispanic zip codes were primarily associated with having no PCP (RRR = 0.52). This analysis found no association between majority African American zip codes and having no PCP, and majority Hispanic zip codes and having a population to PCP ratio of >3,500.
We found significant associations for other demographic and economic factors and the odds of being a PCP shortage area. These associations were robust and did not vary across specifications with the exception of the age distribution variables in the low-population zip codes. (We interpret the odds ratios in the fixed effect model.) We computed the odds ratio for a five percentage point increase in each of the factors. Compared to zip codes with higher percentage of young adults, persons ages 18–44, the odds of being a PCP shortage area were 31 percent lower for zip codes with higher percentages of senior residents; however, the odds were 18 percent higher for zip codes with higher percentages of children and 12 percent higher for zip codes with more persons ages 45–64. A five-point increase in the percentage of women in the zip code was associated with 25 percent lower odds of being a PCP shortage area. Compared to zip codes with higher percentages of residents above 200 percent FPL, an increase in the percentage of near poor residents by five points increased the odds by 19 percent. Compared to the zip codes with higher percentages of college graduates, having fewer college graduates increased the odds of being a PCP shortage area. The odds ratios for a five percentage point increase were 1.80 for adults with less than a ninth grade education, 1.62 for adults with some high school education, 2.04 for adults with a high school diploma or GED, and 1.58 for adults with some college education. In the random effect models, with the exception of annual income for family and general practitioners, the other MSA level variables have the correct signs but were not always statistically significant. Being in an MSA with a higher population-to-bed ratio increased the odds of a zip code being a PCP shortage area but the presence of the major teaching hospital lowered the odds.
We estimated the models that include the segregation measures and their respective interaction terms. To interpret these models, we computed the odds ratios across the range of segregation using 0.75 and 1.5 standard deviations above and below the mean and plotted the results. (See Figures 1–3.) The pattern of the coefficients for African Americans' segregation measures supports our hypothesis. The coefficients on majority African American zip codes are positive suggesting that they are more likely to be PCP shortage areas. The main effects of African American segregation measures are negative, indicating segregation lowers the odds of being a PCP shortage area for non-African American zip codes. The interaction effects are positive suggesting that segregation increases the odds of majority African American zip codes of being PCP shortage areas. For majority African American zip codes, the odd ratios for low-segregation MSAs ranged from 0.99 to 1.41 compared to high-segregation MSAs, which ranged from 1.77 to 2.38 (see Figure 1). We do not observe this pattern for Hispanic and Asian segregation measures. We found some evidence that the segregation has the opposite effect for majority Hispanic and Asian zip codes. The heightened odds of being in a physician shortage area for Hispanic zip codes actually declined with greater segregation, as measured by the isolation index. The other segregation measures exhibited no association (see Figure 2). We found that when the dissimilarity, isolation, centralization, and clustering indices for Asians were included in the model, the majority Asian zip codes in low-segregation areas were more likely to be PCP shortage areas compared to high-segregation areas (see Figure 3).
Figure 1.
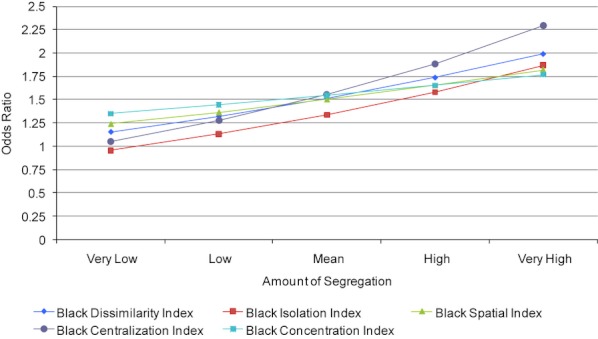
Impact of Segregation on the Odds Being a Primary Care Physicians Shortage Area for Majority Black Zip Codes
Figure 3.
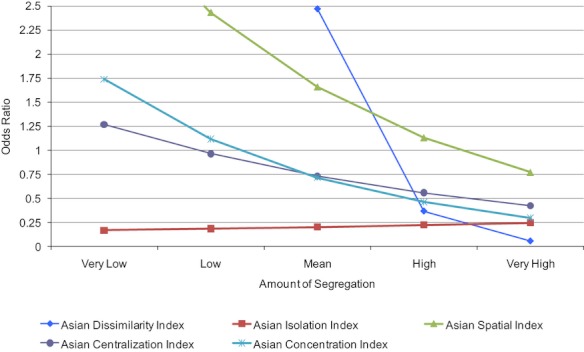
Impact of Segregation on the Odds Being a Primary Care Physicians Shortage Area for Majority Asian Zip Codes
Figure 2.
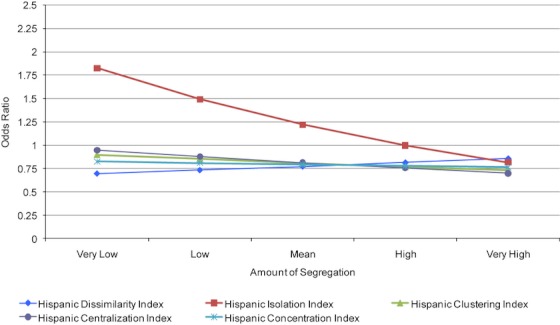
Impact of Segregation on the Odds Being a Primary Care Physicians Shortage Area for Majority Hispanic Zip Codes
Discussion
African American and Hispanic zip codes were more likely to be PCP shortage areas. The disparity for Hispanic zip codes disappeared after controlling for socioeconomic and other factors; however, it persisted for African American zip codes. Our findings indicate that residential segregation matters. In particular, African American segregation was negatively associated with the availability of physician services. African Americans had less geographic access to primary care physicians when they lived in separate areas from whites, resided mostly in the center city, or lived in more densely populated sections of the MSA. This finding supports explanations put forth by fundamental cause, social determinants of health, and social exclusion theories that outline the disadvantages of residential segregation for minorities (Massey, Condran, and Denton 1987; Massey and Fong 1990; Alba, Logan, and Bellair 1994; Link and Phelan 1995; White 1998; Shaw, Dorling, and Smith 2006). The difference in the results between the zip code only and 3-mile definition for PCP shortage areas highlights the plight of poor inner-city neighborhoods. Health care resources may be available in nearby communities but because inner-city neighborhoods are dependent on public transportation these providers may not be geographically accessible (Probst et al. 2007). Also, residents of these poor inner-city neighborhoods may not feel welcomed in more affluent neighboring communities. In the long run, to address persistent access to care problems of poor inner-city communities, urban housing policies must reduce the level of racial and economic segregation.
In contrast to African Americans, segregation of Asians, and to a lesser extent Hispanics, was positively associated with the availability of physician services in their communities. A possible explanation is that Asians are 5.7 percent of physicians compared to 3.9 percent of the population (Castillo-Page 2006). Asian physicians may be more likely to practice in Asian neighborhoods where Asians are highly segregated in MSAs. Some Asian physicians may feel a sense of responsibility to serve Asian communities, and their service may reflect the level of cohesion within Asian communities. Their language skills may also encourage them to settle and practice in locales with language-concordant populations. Thus, segregation may be reflective of barriers that Asian physicians, particularly those who are non-native, face professionally or, conversely, the opportunities available to Asian physicians within Asian neighborhoods. This finding may be related to migration patterns of foreign-born and international medical graduates (IMG) (Lowell and Gerova 2004; Hart et al. 2007). The Asian population is relatively concentrated with 51 percent residing in three states and 75 percent of Asians residing in ten states (Barnes and Bennett 2002). IMGs tend to locate in states with the largest Asian populations: California, New York, Texas, New Jersey, Illinois, and Florida (Barnes and Bennett 2002; Hart et al. 2007). In particular, high percentages of IMGs from Pacific Asian countries practice in California (Hart et al. 2007). A similar explanation may apply to Hispanic communities, which rely heavily on social networks to inform them about the efficacy of doctors, bilingual doctors, and those that adequately serve Spanish-speaking communities (Palloni and Elizabeth 2004). IMGs from Cuba, the Dominican Republic, and Central and South America may also find language-concordant and cultural advantages to locating in Hispanic communities in segregated MSAs (Hart et al. 2007).
This study has a few limitations. Our designation of PCP shortage areas differs from the HRSA's definition. We included OB-GYNs in our definition because some women use them for primary care services. We used zip codes as the basic geographic unit instead of census tracts because we were unable to obtain AMA physician data by census tracts. The HPSA designation controls for age composition, poverty status, and infant mortality rate. We controlled for age composition and poverty explicitly in our models. We controlled for area level health needs by using MSA level fixed and random effects. Finally, our PCP measure is based on physician's primary office location. By not including the secondary offices we likely overstate the shortage problem. This would bias our results if secondary offices were more likely to be located in minority and poor communities. Some have questioned the accuracy of the AMA Masterfile data (Rittenhouse et al. 2004); however, Kletke (2004) concludes that it is “the most complete and authoritative source of information on the nation's supply of allopathic physicians (MDs)” and is routinely used to study physician supply (e.g., Brown, Liu, and Scheffler 2009).
As the United States addresses the shortage of primary care physicians, efforts should target majority minority communities, especially African American communities in segregated MSAs. Other factors, including poverty and educational attainment should be considered, with greater emphasis in areas with high near poor rates. This is a particularly important problem to address as the Patient Protection and Affordable Care Act of 2010 begins to provide health insurance to previously uninsured persons. There are concerns that there will not be enough primary care providers to serve newly insured populations. Expanding community health centers and subsidies programs for physicians to serve in underserved areas may be an effective way to address physician shortages associated with the minority and socioeconomic composition of communities. Other effective strategies may be bolstering community-based efforts to eliminate health care disparities sponsored by the Center of Disease Control and Prevention, the Office of Minority Health, and the National Institute for Minority Health and Health Disparities. These programs typically encourage minorities to use prevention services. Future studies should assess the degree to which limited geographic access to primary care physicians in majority African American communities contribute to disparities.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported by grant number P60MD00214: Hopkins Center for Health Disparities Solutions, awarded by the National Institute on Minority Health and Health Disparities. The content is solely the responsibility of the authors and does not necessarily reflect the views of National Institute on Minority Health and Health Disparities, The Johns Hopkins University or The University of Maryland. Earlier versions of this article were presented at the 2011 American Economic Association annual meeting, the 2010 American Public Health Association annual meeting, and a 2010 Fall Seminar at the National Center for Health Statistics.
Disclosures: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Acevedo-Garcia D. “Residential Segregation and the Epidemiology of Infectious Diseases”. Social Science & Medicine. 2000;51(8):1143–61. doi: 10.1016/s0277-9536(00)00016-2. [DOI] [PubMed] [Google Scholar]
- Acevedo-Garcia D. “Zip Code-Level Risk Factors for Tuberculosis: Neighborhood Environment and Residential Segregation in New Jersey, 1985–1992”. American Journal of Public Health. 2001;91(5):734–41. doi: 10.2105/ajph.91.5.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. “Future Directions in Residential Segregation and Health Research: A Multilevel Approach”. American Journal of Public Health. 2003;93(2):215–21. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alba RD, Logan JR, Bellair PE. “Living in Crime: Implications of Racial/Ethnic Differences in Suburban Location”. Social Forces. 1994;73(2):395–434. [Google Scholar]
- Barnes JS, Bennett CE. The Asian Population: 2000, Census 2000 Brief No. C2KBR/01-16) Washington, DC: U.S. Department of Commerce, Economic and Statistics Administration, U.S. Census Bureau; 2002. [Google Scholar]
- Bell JF, Zimmerman FJ, Mayer JD. “Associations between Residential Segregation and Smoking during Pregnancy among African American Women”. Journal of Urban Health. 2007;84(3):372–88. doi: 10.1007/s11524-006-9152-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenheimer T. “Primary Care—Will It Survive?”. New England Journal of Medicine. 2006;355(9):861–4. doi: 10.1056/NEJMp068155. [DOI] [PubMed] [Google Scholar]
- Bronstein JM, Adams EK, Florence CS. “The Impact of S-CHIP Enrollment on Physician Participation in Medicaid in Alabama and Georgia”. Health Services Research. 2004;39(2):301–17. doi: 10.1111/j.1475-6773.2004.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T, Liu JX, Scheffler RM. “Does the Under- or Overrepresentation of Minority Physicians across Geographical Areas Affect the Location Decisions of Minority Physicians?”. Health Services Research. 2009;44(4):1290–308. doi: 10.1111/j.1475-6773.2009.00978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Ding Y, Hargreaves M, Phelan M, van Ryn S. “The Association between Perceived Discrimination and Underutilization of Needed Medical and Mental Health Care in a Multi-Ethnic Community Sample”. Journal of Health Care for the Poor and Underserved. 2008;19(3):894–911. doi: 10.1353/hpu.0.0063. [DOI] [PubMed] [Google Scholar]
- Casagrande SS, Gary TL, LaVeist TA, Gaskin DJ, Cooper LA. “Perceived Discrimination and Adherence to Medical Care in a Racially Integrated Community”. Journal of General Internal Medicine. 2007;22(3):389–95. doi: 10.1007/s11606-006-0057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo-Page L. Diversity in the Physician Workforce: Fact & Figures 2006. Washington, DC: AAMC, Division of Diversity Policy and Programs; 2006. [Google Scholar]
- Charles C. “The Dynamics of Racial Residential Segregation”. Annual Review of Sociology. 2003;29:167–207. [Google Scholar]
- Christopher AJ. “Segregation Levels in the Late-Apartheid City 1985–1991”. Tijdschrift Voor Econonische en Sociale Geografie. 1993;82:15–24. doi: 10.1111/j.1467-9663.1994.tb00670.x. [DOI] [PubMed] [Google Scholar]
- Collins C, Williams DR. “Segregation and Mortality: The Deadly Effects of Racism”. Sociological Forum. 1999;14:495–523. [Google Scholar]
- Cornwell EY, Cornwell B. “Access to Expertise as a Form of Social Capital: An Examination of Race- and Class-Based Disparities in Network Ties to Experts”. Sociological Perspectives. 2008;51(4):853–76. [Google Scholar]
- Cunningham PJ, O'Malley AS. “Do Reimbursement Delays Discourage Medicaid Participation by Physicians?”. Health Affairs. 2009;28(1):w17–28. doi: 10.1377/hlthaff.28.1.w17. [DOI] [PubMed] [Google Scholar]
- Dill MJ, Salsberg ES. The Complexities of Physician Supply and Demand: Projections Through 2025. Washington, DC: Association of American Medical Colleges; 2008. [Google Scholar]
- Feng Z, Lepore M, Clark MA, Tyler D, Smith DB, Mor V, Fennell ML. “Geographic Concentration and Correlates of Nursing Home Closures: 1999–2008”. Archives of Internal Medicine. 2011;171(9):806–13. doi: 10.1001/archinternmed.2010.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freed GL, Stockman JA. “Oversimplifying Primary Care Supply and Shortages”. Journal of the American Medical Association. 2009;301(18):1920–2. doi: 10.1001/jama.2009.619. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ. “The Impact of HMO Penetration on Hospitals That Serve Minority Communities”. Medical Care. 1997;35:1190–203. doi: 10.1097/00005650-199712000-00003. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Arbelaez JJ, Brown J, Petras H, Wagner F, Cooper LA. “Examining Racial and Ethnic Disparities in Site of Usual Source of Care”. Journal of the National Medical Association. 2007;99(1):22–30. [PMC free article] [PubMed] [Google Scholar]
- Gaskin DJ, Price A, Brandon DT, LaVeist TA. “Segregation and Disparities in Health Services Use”. Medical Care Research and Review. 2009;66(5):578–89. doi: 10.1177/1077558709336445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskin DJ, Spencer CS, Richard P, Anderson G, Powe NR, LaVeist TA. “Do Minority Patients Use Lower Quality Hospitals?”. Inquiry. 2011;48(3):209–20. doi: 10.5034/inquiryjrnl_48.03.06. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Dinwiddie GY, Chan K, McCleary RR. “Residential Segregation and the use of Healthcare Services”. Medical Care Research and Review. 2012;69(2):158–175. doi: 10.1177/1077558711420263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart LG, Skillman SM, Fordyce M, Thompson M, Hagopian A, Konrad TR. “International Medical Graduate Physicians in the United States: Changes Since 1981”. Health Affairs. 2007;26(4):1159–69. doi: 10.1377/hlthaff.26.4.1159. [DOI] [PubMed] [Google Scholar]
- Hausmann LR, Kressin NR, Hanusa BH, Ibrahim SA. “Perceived Racial Discrimination in Health Care and its Association with Patients' Healthcare Experiences: Does the Measure Matter?”. Ethnicity & Disease. 2010;20(1):40–7. [PubMed] [Google Scholar]
- Jha AK, Orav EJ, Epstein AM. “Concentration and Quality of Hospitals That Care for Elderly Black Patients”. Archives of Internal Medicine. 2007;167(11):1177–82. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. “Racial and Ethnic Differences in Patient Perceptions of Bias and Cultural Competence in Health Care”. Journal of General Internal Medicine. 2004;19(2):101–10. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston R, Poulson M, Forrest J. “Ethnic and Racial Segregation in U.S. Metropolitan Areas, 1980–2000: The Dimensions of Segregation Revisited”. Urban Affairs Review. 2007;42(4):479–504. [Google Scholar]
- Kletke P. “Physician Workforce Data: When the Best Is Not Good Enough”. Health Services Research. 2004;39(5):1251–5. doi: 10.1111/j.1475-6773.2004.00288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakhan SE, Laird C. “Addressing the Primary Care Physician Shortage in an Evolving Medical Workforce”. International Archives of Medicine. 2009;2(1):14. doi: 10.1186/1755-7682-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA. “Linking Residential Segregation and Infant Mortality in U.S. Cities”. Sociology and Social Research. 1989;73(2):90–4. [Google Scholar]
- LaVeist TA. “Segregation, Poverty, and Empowerment: Health Consequences for African Americans”. Milbank Quarterly. 1993;71(1):41–64. [PubMed] [Google Scholar]
- LaVeist TA. “Racial Segregation and Longevity Among African Americans: An Individual-Level Analysis”. Health Services Research. 2003;38(6 Pt 2):1719–33. doi: 10.1111/j.1475-6773.2003.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Nickerson KJ, Bowie JV. “Attitudes about Racism, Medical Mistrust, and Satisfaction with Care among African American and White Cardiac Patients”. Medical Care Research and Review. 2000;57(Suppl 1):146–61. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Rolley NC, Diala C. “Prevalence and Patterns of Discrimination among U.S. Health Care Consumers”. International Journal of Health Services. 2003;33(2):331–44. doi: 10.2190/TCAC-P90F-ATM5-B5U0. [DOI] [PubMed] [Google Scholar]
- Lillie-Blanton M, Martinez RM, Salganicoff A. “Site of Medical Care: Do Racial and Ethnic Differences Persist?”. Yale Journal of Health Policy, Law, and Ethics. 2001;1:15–32. [PubMed] [Google Scholar]
- Link B, Phelan J. “Social Conditions as Fundamental Causes of Disease”. Journal of Health and Social Behavior. 1995;35 (SI):80–94. (extra issue) [PubMed] [Google Scholar]
- Lowell BL, Gerova SG. “Immigrants and the Healthcare Workforce: Profiles and Shortages”. Work and Occupations. 2004;31(4):474–98. [Google Scholar]
- Massey DS, Condran GA, Denton NA. “The Effect of Residential Segregation on Black Social and Economic Well-Being”. Social Forces. 1987;66(1):29–56. [Google Scholar]
- Massey DS, Denton NA. “The Dimensions of Segregations”. Social Forces. 1988;67(2):281–315. [Google Scholar]
- Massey DS, Denton NA. “Hypersegregation in the US Metropolitan Areas: Black and Hispanic Segregation along Five Dimensions”. Demography. 1989;26(3):373–91. [PubMed] [Google Scholar]
- Massey DS, Denton NA. American Apartheid Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- Massey DS, Fong E. “Segregation and Neighborhood Quality: Blacks, Hispanics, and Asians in San Francisco Metropolitan Areas”. Social Forces. 1990;69(1):15–32. [Google Scholar]
- Mayberry RM, Mili F, Ofili E. “Racial and Ethnic Differences in Access to Medical Care”. Medical Care Research and Review. 2005;57(Suppl 1):108–45. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- Mitchell JB. “Physician Participation in Medicaid Revisited”. Medical Care. 1991;29(7):645–53. doi: 10.1097/00005650-199107000-00004. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Jesdale BM. “Separate and Unequal: Residential Segregation and Estimated Cancer Risks Associated with Ambient Air Toxics in U.S. Metropolitan Areas”. Environmental Health Perspectives. 2006;114(3):386–93. doi: 10.1289/ehp.8500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morenoff JD, Sampson RJ, Raudenbush SW. “Neighborhood Inequality, Collective Efficacy, and the Spatial Dynamics of Urban Violence”. Criminology. 2001;29(3):517–60. [Google Scholar]
- Morrison RS, Wallenstein S, Natale DK, Senzel RS, Huang L. “We Don't Carry That—Failure of Pharmacies in Predominantly Non-White Neighborhoods to Stock Opioid Analgesics”. New England Journal of Medicine. 2000;342(14):1023–6. doi: 10.1056/NEJM200004063421406. [DOI] [PubMed] [Google Scholar]
- Myer L, Ehrlich RI, Susser ES. “Social Epidemiology in South Africa”. Epidemiologic Reviews. 2004;26:112–23. doi: 10.1093/epirev/mxh004. [DOI] [PubMed] [Google Scholar]
- Nazroo JY, Williams DR. “The Social Determination of Ethnic/Racial Inequalities in Health”. In: Marmot M, Wilkinson RG, editors. Social Determinants of Health. New York: Oxford University Press; 2006. pp. 238–66. [Google Scholar]
- Osypuk TL, Acevedo-Garcia D. “Are Racial Disparities in Preterm Birth Larger in Hypersegregated Areas?”. American Journal of Epidemiology. 2008;167(11):1295–304. doi: 10.1093/aje/kwn043. [DOI] [PubMed] [Google Scholar]
- Palloni A, Elizabeth A. “Paradox Lost: Explaining the Hispanic Adult Mortality Advantage”. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Perloff JD, Kletke PR, Fossett JW, Banks S. “Medicaid Participation among Urban Primary Care Physicians”. Medical Care. 1997;35(2):142–57. doi: 10.1097/00005650-199702000-00005. [DOI] [PubMed] [Google Scholar]
- Polednak AP. “Black-White Differences in Infant Mortality in 38 Standard Metropolitan Statistical Areas”. American Journal of Public Health. 1991;81(11):1480–2. doi: 10.2105/ajph.81.11.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polednak AP. “Segregation, Discrimination and Mortality in U.S. Blacks”. Ethnicity & Disease. 1996a;6(1–2):99–108. [PubMed] [Google Scholar]
- Polednak AP. “Trends in U.S. Urban Black Infant Mortality, by Degree of Residential Segregation”. American Journal of Public Health. 1996b;86(5):723–6. doi: 10.2105/ajph.86.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst JC, Laditka SB, Wang J, Johnson AO. “Effects of Residence and Race on Burden of Travel for Care: Cross Sectional Analysis of the 2001 U.S. National Household Travel Survey”. BMC Health Service Research. 2007;7:40. doi: 10.1186/1472-6963-7-40. doi: 10.1186/1472-6963-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reschovsky JD, O'Malley AS. “Do Primary Care Physicians Treating Minority Patients Report Problems Delivering High-Quality Care?”. Health Affairs. 2007;26(3):w222–31. doi: 10.1377/hlthaff.27.3.w222. [DOI] [PubMed] [Google Scholar]
- Rittenhouse DR, Mertz E, Keane D, Grumbach K. “No Exit: An Evaluation of Measures of Physician Attrition”. Health Services Research. 2004;39(5):1571–88. doi: 10.1111/j.1475-6773.2004.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw M, Dorling D, Smith GD. “Poverty, Social Exclusion, and Minorities”. In: Marmot M, Wilkinsom RG, editors. Social Determinants of Health. 2d Edition. New York: Oxford University Press; 2006. pp. 198–223. [Google Scholar]
- Shi L. “Experience of Primary Care by Racial and Ethnic Groups in the United States”. Medical Care. 1999;37(10):1068–77. doi: 10.1097/00005650-199910000-00010. [DOI] [PubMed] [Google Scholar]
- Shihadeh ES, Flynn N. “Segregation and Crime: The Effect of Black Isolation on the Rates of Black Urban Violence”. Social Forces. 1996;74:1325–52. [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- Smith DB. “The Racial Segregation of Hospital Care Revisited: Medicare Discharge Patterns and Their Implication”. American Journal of Public Health. 1998;88(3):461–3. doi: 10.2105/ajph.88.3.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DB. Health Care Divided: Race and Healing a Nation. Ann Arbor: University of Michigan Press; 1999. [Google Scholar]
- Smith DB, Feng Z, Fennel ML, Zinn JS, Mor V. “Separate and Unequal: Racial Segregation and Disparities in Quality across U.S. Nursing Homes”. Health Affairs. 2007;26(5):1448–58. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- Stafford M, Martikainen P, Lahelma E, Marmot M. “Neighbourhoods and Self Rated Health: A Comparison of Public Sector Employees in London and Helsinki”. Journal of Epidemiology and Community Health. 2004;58:772–8. doi: 10.1136/jech.2003.015941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinbrook R. “Easing The Shortage in Adult Primary Care—Is it All about Money?”. New England Journal of Medicine. 2009;360(26):2696–9. doi: 10.1056/NEJMp0903460. [DOI] [PubMed] [Google Scholar]
- Szwarcwald CL, Lourenco CL, Bastos T, de Andrade FI. “Income Inequality, Residential Poverty, Clustering and Infant Mortality: A Study of Rio de Janeiro, Brazil”. Social Science and Medicine. 2002;55:2083–92. doi: 10.1016/s0277-9536(01)00353-7. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health, Human Services, Agency for Healthcare Research and Quality. National Healthcare Disparities Report, 2007 No. 08-0041. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- White P. “Urban Life and Social Stress”. In: Pinder D, editor. The New Europe: Economy, Society and Environment. Chichester, England: Wiley; 1998. pp. 305–22. [Google Scholar]
- Williams DR, Collins C. “Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health”. Public Health Reports. 2001;116(5):404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson WJ. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago: The University of Chicago Press; 1987. [Google Scholar]
- Wyndham C. “The Loss from Premature Deaths of Economically Active Manpower in the Various Populations of the RSA. Part I. Leading Causes of Death: Health Strategies for Reducing Mortality”. South African Medical Journal. 1981;60:411–9. [PubMed] [Google Scholar]
- Yankauer A. “The Relationship of Fetal and Infant Mortality to Residential Segregation”. American Sociological Review. 1950;15(5):644–8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


