Abstract
Giant cell tumour of tendon sheath is a benign soft tissue lesion most commonly found in the flexor aspect of hand and wrist. Being rare in foot and ankle, the unusual presentation of this lesion may sometimes mimic other lesions like lipoma, synovial sarcoma, malignant fibrous histiocytoma, synovial cyst and ganglion. Hence it is important to include this lesion in differential diagnoses especially if the lesion is found to be anchored to any of the surrounding tendons. This article describes the unusual occurrence of giant cell tumour of the tendon sheath of peroneus brevis which is rarely described in literature.
Background
Giant cell tumour of the tendon sheath (GCTTS) is synonymous with fibrous histocytoma of synovium, pigmented nodular synovitis, tenosynovial giant cell tumour, localised nodular tenosynovitis, benign synovioma and fibrous xanthoma of the synovium.1–4 GCTTS is considered as the extra-articular counterpart of pigmented villonodular synovitis, arising from tendon sheaths, bursae or ligaments.5 6 The most frequent site of presentation is in the flexor aspect of the tendon sheath of fingers. Their notoriety in the foot is far less common. This article highlights the atypical occurrence of giant cell tumour along the peroneus brevis tendon sheath.
Case presentation
A 36-year-old lady presented with swelling over the lateral aspect of the foot which was painless in nature and gradually increasing in size over a period of 18 months. There was no history of trauma at onset. The patient had mild discomfort on walking. On examination, there was a 3×3 cm non-tender firm swelling over the lateral aspect of the foot below and in front of the lateral malleolus. The skin over the swelling was pinchable. There was no free mobility of the swelling over the underlying bone. X-ray showed a soft tissue lesion over the lateral aspect of the foot (figure 1). MRI showed a well-defined soft tissue lesion along the anterior aspect of peroneus brevis tendon abutting the calcaneum/cuboid and mild oedema in the area adjoining the peroneus brevis tendon. The lesion was iso-intense to muscles on T1, and mildly hyper intense on T2FS, suggestive of giant cell tumour of tendon sheath of peroneus brevis (figure 2). The patient had a report of fine needle aspiration cytology of the swelling which was done outside. It showed a moderately cellular smear with mononuclear cells, osteoclast like multi-nucleate giant cells in a background of collagenous stromal fragments, chronic inflammatory cells, occasional foamy macrophages and cholesterol clefts – findings suggestive of giant cell tumour of tendon sheath. The patient was posted for excisional biopsy. Intraoperatively, a soft tissue mass was seen arising from the peroneus brevis tendon sheath (figure 3). Following its excision the adjoining areas of cuboid and the anterior process of calcaneum was curetted and treated with hydrogen peroxide followed by thorough wash with normal saline. Postoperative period was uneventful. The excisional biopsy showed a well-encapsulated tumour composed of mononuclear cells and osteoclast type of giant cells along with thick fibrous septae running through the tumour. Foamy cells, hemosiderin laden macrophages and cholesterol clefts were also seen – all findings consistent with the diagnosis of giant cell tumour of tendon sheath (figure 4). There was no clinical or radiological evidence of recurrence in an 18 months follow-up period.
Figure 1.

X-ray of right foot showing a soft tissue density (white arrow) in the lateral part of foot in the region of calcaneum/cuboid.
Figure 2.

T1 weighted MRI image of right foot showing a soft tissue lesion (white arrow) arising from the peroneus brevis tendon sheath abutting the calcaneum/cuboid. Its signal is isointense with that of the muscle.
Figure 3.

Intraoperative picture showing a soft tissue mass (black arrow) along the peroneus brevis tendon sheath (white arrow).
Figure 4.
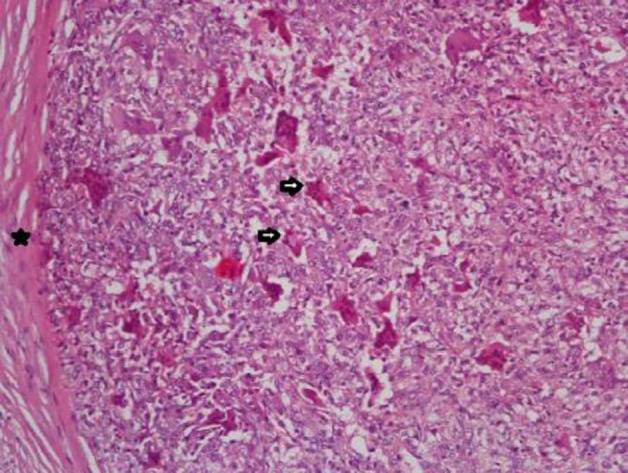
Histopathology showing a well-encapsulated (black star) tumour composed of mononuclear cells and osteoclastic giant cells (black arrows). Foamy cells, hemosiderin laden macrophages and cholesterol clefts are also seen.
Discussion
Giant cell tumour of tendon sheath is a slowly growing benign mesenchymal tumour arising from the synovial membrane. Their nature is unclear whether these lesions represent reactive lesions or true neoplasm.7 These lesions usually present in the third to fifth decades with a slight female predilection. The most common site of occurrence is hand and wrist especially the flexor tendon sheath of fingers. Although ankle and foot constitute the next common site after hand and wrist, it is rare when compared with upper limb lesions.4 To the best of our knowledge, till date there has been only one reported case of giant cell tumour arising from the peroneus tendon sheath.8
The most common presenting clinical feature is a slowly growing painless mass of long duration, as seen in our case. X-rays might show soft tissue densities with or without adjacent bony cortical erosions. Ultrasonography shows solid homogeneous hypoechoic mass. MRI helps in differentiating giant cell tumour of tendon sheath from other soft tissue lesions such as lipoma, synovial sarcoma, malignant fibrous histiocytoma, synovial cyst and ganglion, all of which constitute the differential diagnosis of the former. The MRI features of giant cell tumour of tendon sheath are highly characteristic. T1 weighted image reveals lesions to be isointense or hypointense to that of the muscle and hypointense on T2 weighted images.9 The characteristic low signal on T1W and T2W images is attributed to the paramagnetic effect of hemosiderin and the abundant collagenous stroma.10 Heterogeneous signal intensity may occur depending on the histological composition.
The gross pathological features include a well-circumscribed lobulated or multi-nodular encapsulated mass with varying degrees of hyalinisation. On microscopy, the cellular infiltrate is constituted by macrophage-like mononuclear cells, epithelioid histiocyte-like cells, osteoclast-like giant cells and xanthomatous cells.1 Hemosiderin laden macrophages and cholesterol clefts are also seen. Treatment is by marginal excision. The most bothering fact to the surgeon is the high rate of local recurrence of upto 45%, after excision.11 Complete removal of the affected tissue is of utmost importance in preventing recurrence. Careful meticulous dissection and use of magnification devices aids in achieving this goal. Osseous involvement, radiologically evidenced by the presence of bony erosions, is a risk factor for local recurrence.12 There has been no description in literature regarding usage of any local adjuvants, after tumour excision, for preventing recurrence. In our case, after complete local excision of the tumour, we have thoroughly curetted the adjoining bony surfaces and treated them with hydrogen peroxide followed by a saline lavage. Hydrogen peroxide serves as a mode of chemical cautery and thus helps in eliminating microscopic tumour remnants, if any left over after excision. Postoperative radiotherapy may have a role in cases in which complete excision may not be possible.11 Regular follow-up is a must in all cases after excision to identify recurrences, if any. There has been no clinical or radiological evidence of recurrence in our case in our 18 months follow-up period.
Learning points.
Giant cell tumour of tendon sheath must be considered as a differential diagnosis of a soft tissue lesion around the ankle, even though it is rare. The idea of usage of adjuvants in the context of preventing recurrence sounds promising. Nevertheless it needs to be worked upon in the future to know its true efficacy.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Monaghan H, Salter DM, Al-Nafussi A. Giant cell tumour of tendon sheath (localised nodular tenosynovitis): clinicopathological features of 71 cases. J Clin Pathol 2001;54:404–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martin RC, 2nd, Osborne DL, Edwards MJ, et al. Giant cell tumor of tendon sheath, tenosynovial giant cell tumor, and pigmented villonodular synovitis: defining the presentation, surgical therapy and recurrence. Oncol Rep 2000;7:413–9. [PubMed] [Google Scholar]
- 3.Coster AA. Giant cell tumor of tendon sheath(benign synovioma). J Am Podiatry Assoc 1976;66:538–41. [DOI] [PubMed] [Google Scholar]
- 4.Jones FE, Soule EH, Coventry MB. Fibrous xanthoma of synovium (giant-cell tumor of tendon sheath, pigmented nodular synovitis). A study of one hundred and eighteen cases. J Bone Joint Surg Am 1969;51:76–86. [PubMed] [Google Scholar]
- 5.Waldt S, Rechl H, Rummeny EJ, et al. Imaging of benign and malignant soft tissue masses of the foot. Eur Radiol 2003;13:1125–36. [DOI] [PubMed] [Google Scholar]
- 6.Llauger J, Palmer J, Monill JM, et al. MR imaging of benign soft-tissue masses of the foot and ankle. Radiographics 1998;18:1481–98. [DOI] [PubMed] [Google Scholar]
- 7.Vogrincic GS, O’Connell JX, Gilks CB. Giant cell tumor of tendon sheath is a polyclonal cellular proliferation. Hum Pathol 1997;28:815–9. [DOI] [PubMed] [Google Scholar]
- 8.Ly JQ, Carlson CL, LaGatta LM, et al. Giant cell tumor of the peroneus tendon sheath. AJR Am J Roentgenol 2003;180:1442. [DOI] [PubMed] [Google Scholar]
- 9.De Beuckeleer L, De Schepper A, De Belder F, et al. Magnetic resonance imaging of localized giant cell tumour of the tendon sheath (MRI of localized GCTTS). Eur Radiol 1997;7:198–201. [DOI] [PubMed] [Google Scholar]
- 10.Jelinek JS, Kransdorf MJ, Shmookler BM, et al. Giant cell tumor of the tendon sheath: MR findings in nine cases. AJR Am J Roentgenol 1994;162:919–22. [DOI] [PubMed] [Google Scholar]
- 11.Kotwal PP, Gupta V, Malhotra R. Giant-cell tumor of the tendon sheath: is radiotherapy indicated to prevent recurrence after surgery? J Bone Joint Surg Br 2000;82:571–3. [DOI] [PubMed] [Google Scholar]
- 12.Reilly KE, Stern PJ, Dale JA. Recurrent giant cell tumors of the tendon sheath. J Hand Surg Am 1999;24:1298–302. [DOI] [PubMed] [Google Scholar]


