Abstract
Perimesencephalic subarachnoid haemorrhage is usually asymptomatic other than meningeal irritation sign. The authors report a case of subarachnoid haemorrhage at the quadrigeminal cistern showing ipsilateral trochlear nerve palsy and discuss the pathogenesis. A 71-year-old man with a history of diabetes mellitus and acute myocardial infarction presented with diplopia. He underwent CT, which revealed subarachnoid haemorrhage at the left quadrigeminal cistern. Neurological examination revealed left isolated trochlear nerve palsy, with results otherwise normal. The diagnosis of perimesencephalic subarachnoid haemorrhage was established on neuroimaging. The amount of haemorrhage is related to symptoms. A dense clot in the quadrigeminal cistern might have been the cause of trochlear nerve palsy.
Background
We examined a patient suffering from left trochlear nerve palsy after perimesencephalic subarachnoid haemorrhage (SAH). CT revealed a high-density lesion consistent with SAH in the left quadrigeminal cistern. This is the first report of isolated trochlear nerve palsy with perimesencephalic SAH. The aetiology of nerve palsy is discussed.
Case presentation
A 71-year-old man was referred to our hospital with double vision when he focused downwards. He had been suffering from diabetes mellitus for 5 years, and had a history of myocardial infarction and subsequent arrhythmia 2 years ago. He had been treated with calcium channel blocker and warfarin. He had no history of head injury. Blood pressure was 184/104 mm Hg and heart rate was 80 beats/min. No neurological deficits were identified other than abnormal ocular movement. No tinnitus or sensory disturbances were present. Double vision was in the form of vertical diplopia which increased with downward and rightward gaze. Hypertropia also aggravated on left head tilt, which would require intorsion of the left eye. These findings were most consistent with left trochlear nerve palsy.
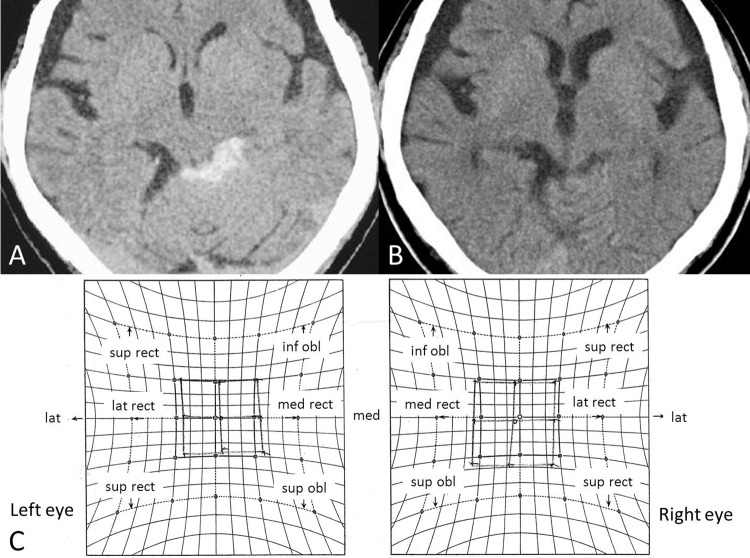
CT performed 15 h after the initial presentation showed a localised high-density lesion in the left quadrigeminal cistern (figure 1A). MRI also indicated SAH in the form of a low-intensity area on T2-weighted imaging and a high-intensity area on T1-weighted imaging in the same region. No evidence of any contusion or vascular anomaly was apparent within the midbrain. Angiography on day 1 showed no aneurysm or other vascular abnormality. Perimesencephalic SAH was diagnosed. Hess red-green test showed solitary palsy of the left superior oblique muscle (figure 1C). The medical treatment to prevent vasospasm was performed, and no ischaemia was observed on neuroimaging. Perimesencephalic haematoma appeared more obscure day by day and disappeared on CT 16 days after onset (figure 1B). Double vision gradually improved and resolved by day 16.
Figure 1.
A) Initial CT. A thick clot is present in the left quadrigeminal subarachnoid space, consistent with perimesencephalic SAH. No oedema or hydrocephalus is observed. B) CT on day 16, showing no SAH in the perimesencephalic region. C) Hess red-green test on day 5. Diplopia is most prominent with right-downward gaze, indicating weakness of the left superior oblique muscle. The Hess chart results are also consistent with left trochlear nerve palsy.
Discussion
Various reports have described isolated trochlear nerve palsy, with aetiologies including head injury,1–4 infarction1 5–7 and intracerebral haematoma.5 6 8–13 Review articles of trochlear nerve palsy before the MRI era reported head trauma, stroke, tumor, congenital anomalies and demyelination as aetiologies.14–16 Isolated trochlear nerve palsy associated with SAH is rare.17 In cases of perimesencephalic SAH, the bleeding mechanisms remain unclear, although small vascular anomalies may exist and cause bleeding. Trochlear nerve palsy after perimesencephalic SAH has not previously been reported.
The present case showed no neurological signs of mesencephalic parenchymal lesions, such as tinnitus or heminumbness. The trochlear nerve may be influenced directly by SAH. When the nucleus of the trochlear nerve and intramedullary fibres before decussation are damaged, contralateral superior oblique muscle palsy will occur. Conversely, in cases with lesions affecting subarachnoid fibres and intramedullary fibres after decussation, ipsilateral palsy will be seen. SAH usually does not influence nerve fibres across the subarachnoid space. Relatively few cases of aneurysmal SAH show damage to the nerve from the haemorrhage itself, rather than by aneurysmal compression, particularly when a dense clot is present.17 18 Nerve palsy may result from the osmotic tonicity of the surrounding blood clot, the deleterious effects of concentrated blood breakdown products or ischaemia from compression of the small nutrient vessels of the nerve.19 Especially, the trochlear nerve may be sensitive to intracranial pressure variation or haemorrhage, because it is the finest cranial nerve and runs a long distance in subarachnoid space. In the present case, the perimesencephalic clot on the left side, as revealed on initial CT, was sufficiently large to warrant consideration as the cause of left trochlear nerve palsy.
Other potential indirect causes of cranial nerve palsy in patients with SAH include elevated intracranial pressure (ICP), oedema or hydrocephalus, with subsequent displacement of the cerebral hemisphere and major arteries against the nerve.20–22 Vasospasm has also been implicated as an indirect cause of cranial nerve palsy.23 24 The trochlear nerve may be affected by the same aetiologies.14 24 However, in the present case, the amount of haemorrhage was not enough to result in an excessively high ICP and no oedema or hydrocephalus was observed. Moreover, the early onset of palsy shortly after the episode and the absence of other neurological signs and symptoms suggest that vasospasm was less likely as a cause of trochlear nerve palsy.
Isolated trochlear nerve palsy usually displays a good prognosis.25 Spontaneous regression is expected within 2–6 months, particularly in cases of presumed microvascular origin or due to minor head trauma.26 In the present case, the appearance of trochlear nerve palsy seemed to be related to haemorrhage density in the subarachnoid space. The palsy persisted about 16 days, as did the SAH.
Trochlear nerve palsy associated with SAH may not be rare, but rest therapy is needed in the acute stage of SAH before clipping or other radical treatments, so patients do not usually undergo full neurological testing that includes ocular movements. Moreover, the diagnosis of isolated trochlear nerve palsy is difficult, particularly when the patient is not fully alert, because the symptoms can be subtle.
Learning points.
We have described a patient with quadrigeminal SAH and ipsilateral isolated trochlear nerve palsy. A large subarachnoid clot is suggested as the most likely aetiology.
Acknowledgments
The authors appreciate Dr Ichiro Takumi and Dr Akira Yamada for their precious opinion about the pathogenesis of this case.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Cackett P, Fleck B, Mulhivill A. Bilateral fourth-nerve palsy occurring after shaking injury in infancy. J AAPOS 2004;8:280–1. [DOI] [PubMed] [Google Scholar]
- 2.Hara N, Kan S, Simizu K. Localization of post-traumatic trochlear nerve palsy associated with hemorrhage at the subarachnoid space by magnetic resonance imaging. Am J Ophthalmol 2001;132:443–5. [DOI] [PubMed] [Google Scholar]
- 3.Ishizaki E, Kurokawa Y. [A case of solitary and unilateral trochlear nerve palsy due to a blunt head impact]. Rinsho Shinkeigaku 2003;43:571–3. [PubMed] [Google Scholar]
- 4.Jin H, Wang S, Hou L, et al. Clinical treatment of traumatic brain injury complicated by cranial nerve injury. Injury 2010;41:918–23. [DOI] [PubMed] [Google Scholar]
- 5.Thömke F, Ringel K. Isolated superior oblique palsies with brainstem lesions. Neurology 1999;53:1126–7. [DOI] [PubMed] [Google Scholar]
- 6.Thömke F, Hopf HC. Isolated superior oblique palsies with electrophysiologically documented brainstem lesions. Muscle Nerve 2000;23:267–70. [DOI] [PubMed] [Google Scholar]
- 7.Walsh RA, Murphy RP, Moore DP, et al. Isolated trochlear infarction: an uncommon cause of acquired diplopia. Arch Neurol 2010;67:892–3. [DOI] [PubMed] [Google Scholar]
- 8.Chen CH, Hwang WJ, Tsai TT, et al. Midbrain hemorrhage presenting with trochlear nerve palsy. Zhonghua Yi Xue Za Zhi (Taipei) 2000;63:138–43. [PubMed] [Google Scholar]
- 9.Galetta SL, Balcer LJ. Isolated fourth nerve palsy from midbrain hemorrhage: case report. J Neuroophthalmol 1998;18:204–5. [PubMed] [Google Scholar]
- 10.Hatori K, Urabe T, Kanazawa A, et al. [A case of brainstem vascular malformation with isolated trochlear nerve palsy as the initial symptom]. No To Shinkei 1991;43:965–8. [PubMed] [Google Scholar]
- 11.Lee SH, Park SW, Kim BC, et al. Isolated trochlear palsy due to midbrain stroke. Clin Neurol Neurosurg 2010;112:68–71. [DOI] [PubMed] [Google Scholar]
- 12.Mon Y. [Midbrain hemorrhage presenting with trochlear nerve palsy–a case report]. Rinsho Shinkeigaku 1996;36:71–3. [PubMed] [Google Scholar]
- 13.Raghavendra S, Vasudha K, Shankar SR. Isolated trochlear nerve palsy with midbrain hemorrhage. Indian J Ophthalmol 2010;58:66–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mansour AM, Reinecke RD. Central trochlear palsy. Surv Ophthalmol 1986;30:279–97. [DOI] [PubMed] [Google Scholar]
- 15.von Noorden GK, Murray E, Wong SY. Superior oblique paralysis. A review of 270 cases. Arch Ophthalmol 1986;104:1771–6. [DOI] [PubMed] [Google Scholar]
- 16.Younge BR, Sutula F. Analysis of trochlear nerve palsies. Diagnosis, etiology, and treatment. Mayo Clin Proc 1977;52:11–8. [PubMed] [Google Scholar]
- 17.Son S, Park CW, Yoo CJ, et al. Isolated, contralateral trochlear nerve palsy associated with a ruptured right posterior communicating artery aneurysm. J Korean Neurosurg Soc 2010;47:392–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rush JA, Younge BR. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1,000 cases. Arch Ophthalmol 1981;99:76–9. [DOI] [PubMed] [Google Scholar]
- 19.Hoya K, Kirino T. Traumatic trochlear nerve palsy following minor occipital impact–four case reports. Neurol Med Chir (Tokyo) 2000;40:358–60. [DOI] [PubMed] [Google Scholar]
- 20.Coyne TJ, Wallace MC. Bilateral third cranial nerve palsies in association with a ruptured anterior communicating artery aneurysm. Surg Neurol 1994;42:52–6. [DOI] [PubMed] [Google Scholar]
- 21.Kang SD. Ruptured anterior communicating artery aneurysm causing bilateral oculomotor nerve palsy: a case report. J Korean Med Sci 2007;22:173–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suzuki J, Iwabuchi T. Ocular motor disturbances occurring as false localizing signs in ruptured intracranial aneurysms. Acta Neurochir (Wien) 1974;30:119–28. [DOI] [PubMed] [Google Scholar]
- 23.Kudo T. Postoperative oculomotor palsy due to vasospasm in a patient with a ruptured internal carotid artery aneurysm: a case report. Neurosurgery 1986;19:274–7. [DOI] [PubMed] [Google Scholar]
- 24.Laun A, Tonn JC. Cranial nerve lesions following subarachnoid hemorrhage and aneurysm of the circle of Willis. Neurosurg Rev 1988;11:137–41. [DOI] [PubMed] [Google Scholar]
- 25.Richards BW, Jones FR, Jr, Younge BR. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol 1992;113:489–96. [DOI] [PubMed] [Google Scholar]
- 26.Mollan SP, Edwards JH, Price A, et al. Aetiology and outcomes of adult superior oblique palsies: a modern series. Eye (Lond) 2009;23:640–4. [DOI] [PubMed] [Google Scholar]