Abstract
Course and outcome of Borderline Personality Disorder (BPD) are favorable for the vast majority of patients; however, up to 10% die by suicide. This discrepancy begs the question of whether there is a high lethality subtype in BPD, defined by recurrent suicidal behavior and increasing attempt lethality over time. In a prospective, longitudinal study, we sought predictors of high lethality among repeat attempters, and defined clinical subtypes by applying trajectory analysis to consecutive lethality scores. Criteria-defined subjects with BPD were assessed using standardized instruments and followed longitudinally. Suicidal behavior was assessed on the Columbia Suicide History, Lethality Rating Scale, and Suicide Intent Scale. Variables discriminating single and repeat attempters were entered into logistic regression models to define predictors of high and low lethality attempts. Trajectory analysis using 3 attempt and 5 attempt models identified discrete patterns of Lethality Rating Scale scores. A high lethality trajectory was associated with inpatient recruitment, and poor psychosocial function, a low lethality trajectory with greater Negativism, Substance Use Disorders, Histrionic and/or Narcissistic PD co-morbidity. Illness severity, older age, and poor psychosocial function are characteristics of a poor prognosis subtype related to suicidal behavior.
Recurrent suicidal behavior is a defining characteristic of Borderline Personality Disorder (BPD), associated with suicide attempts in 46%–92% of patients, and suicide completion in 3% to 10% (Zanarini, Frankenburg, Reich, Fitzmaurice, Weinberg & Gunderson, 2008). Despite a fatal outcome in a minority of borderline patients, the vast majority experience favorable outcomes. Two recent prospective, longitudinal studies demonstrated progressive symptomatic and diagnostic remissions in the months to years following initial assessment. The Collaborative Longitudinal Personality Disorders Study (CLPS), a multi-site, prospective study of treatment-seeking patients with personality disorders (PD), found that diagnostic criteria among patients with BPD decreased significantly in the first 6 – 12 months following assessment, with improvement continuing through the following 6 years (Shea, Stout, Gunderson, Morey, Grilo, McGlashan et al., 2002; Shea, Edelen, Pinto, Yen, Gunderson, Skodol, et al., 2009). Similarly, the McLean Study of Adult Development reported progressive remission of diagnostic criteria through 10 years of follow-up (Zanarini, Frankenburg, Reich & Fitzmaurice, 2010). Acute symptoms, including suicide attempts, remitted most rapidly. With favorable outcomes in a majority of cases, who dies by suicide? Is there a poor prognosis subtype in BPD related to increasing medical lethality of recurrent suicide attempts? In search of a high lethality subtype, we asked if there are clinical predictors of attempt lethality in patients with BPD, if attempt lethality increased with repeated attempts, and if subtypes could be defined by analysis of the trajectories of medical lethality scores over time.
Method
This study was approved by the Institutional Review Board of the University of Pittsburgh and is part of a prospective longitudinal study of suicidal behavior in BPD. Subjects were drawn from the inpatient and outpatient services of Western Psychiatric Institute and Clinic, and, by advertisement, from the surrounding community. After a complete description of the study was given to the subjects, written informed consent was obtained. At intake, subjects participated in multidimensional assessments of demographic, diagnostic, clinical, and psychosocial factors related to suicidal risk, with follow-up assessments at 3 months, one year, and annually. All subjects were assessed by Master's prepared research interviewers for Axis I disorders using the Structured Diagnostic Interview for DSM III-R (SCID) (Spitzer, Williams, Gibbon & First, 1988) and for Axis II disorders using the International Personality Disorders Examination (IPDE) (Loranger, Janca & Sartorius,1997). The diagnosis of BPD was established by first meeting probable or definite criteria for BPD on the IPDE (with a lifetime time frame), followed by a definite diagnosis on the Diagnostic Interview for Borderline Patients (DIB), (with a 3 month to 2 year timeframe for component parts) (Gunderson, Kolb & Austin,1981). The DSM III-R and DIB were used to maintain diagnostic continuity with the longitudinal study. Subjects were also required to meet DSM IV and definite DIB-R criteria for BPD when these measures were introduced (Zanarini, Gunderson, Frankenburg, & Chauncey, 1989). The DIB/R interviews were conducted by the senior author (PHS), who also obtained an Abuse History of childhood sexual and physical abuse (Soloff, Lynch & Kelly, 2002). All diagnoses were confirmed in a consensus conference of raters, using a best estimate process and all available data from medical records, SCID, IPDE, and DIB/R interviews (Leckman, Sholomskas, Thompson, Belanger & Weissman, 1982). Exclusion criteria for this study included: a lifetime (past or current) Axis I diagnosis of schizophrenia, delusional (paranoid) disorder, schizoaffective disorder, any bipolar disorder (I, II, mixed, manic, or depressed) or psychotic depression. Subjects with current non-psychotic MDD were included. Subjects were also excluded for: clinical evidence of CNS pathology, recent ECT, seizure disorder, physical disorders with known psychiatric consequences (e.g. thyroid disease), and borderline mental retardation (IQ<70 by WAIS).
Demographic, clinical and psychosocial characteristics were obtained using standardized interviews or self rated measures. The Hamilton Rating Scale for Depression-24 item (HamD-24) (Guy, 1976), the Beck Depression Inventory (BDI) (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961), and the Beck Hopelessness Scale (Beck, Weissman, Lester, & Trexler,1974) were used to assess affective symptoms. Global and psychosocial function were assessed using the Global Assessment Scale (GAS) (Endicott, Spitzer, Fleiss & Cohen, 1996) and Social Adjustment Scale-self report (SAS-sr) (Weissman & Bothwell, 1976), respectively. The Brown-Goodwin Lifetime History of Aggression (LHA) (Brown, Goodwin, Ballenger, Goyer & Major,1979), Buss-Durkee Hostility Inventory (BDHI) (Buss & Durkee, 1957), Barratt Impulsiveness Scale (BIS) (Barratt, 1965), and MMPI Psychopathic Deviance subscale (MMPI_Pd) (Hathaway & McKinley, 1943) were used to assess impulsivity and aggression. Suicidal behavior and attempt characteristics were assessed using the Columbia Suicide History and a Lethality Rating Scale, quantifying medical consequences on an 8 point scale for 8 separate suicide methods (Oquendo, Halberstam & Mann et al., 2003; Beck, Beck & Kovacs, 1975). The 6 most recent baseline attempts, and all follow-up attempts were rated for attempt lethality. The Suicide Intent Scale (SIS) provided a self-rated baseline measure of subjective intent to die for the most recent and most serious attempts to date (Beck, 1975). At follow-up, changes in demographic, diagnostic, clinical, psychosocial and suicide variables were updated.
Statistical procedures
The focus of our study is on lethality of repeat attempts. Subjects with attempt histories were divided into groups with single and repeat attempts and compared on all study variables to define discriminating characteristics using Chi Square or t-tests (2 tailed), as appropriate. A median split of lifetime maximum Lethality Rating Scale scores was used to define subjects with Low Lethality (score < 3) and High Lethality attempts (score > 4). The distinction between Low and High Lethality using these scores is clinically meaningful. (e.g. For a suicide attempt by overdose with sedative drugs, a Lethality Rating Scale score of 3 is defined, in part, as “asleep but easily aroused”, while a score of 4 is defined as “comatose, injury sufficient for hospitalization”). Logistic regression was used to define relationships between the discriminating characteristics and Low or High Lethality attempter status.
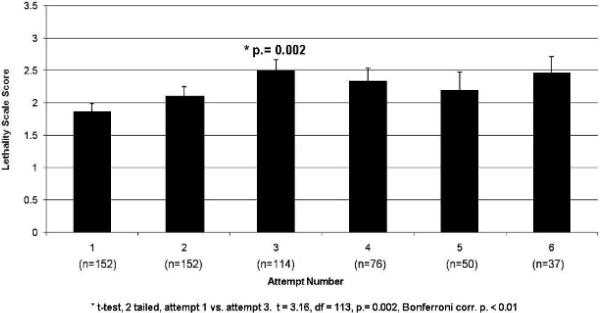
To assess if medical lethality increased with recurrent attempts, Lethality Rating Scale scores were compared within repeating subjects across attempts using paired t tests (with Bonferroni correction) for up to 6 attempts, including both baseline and follow-up data.
The medical lethality of repeat suicide attempters over time was analyzed using trajectory analysis. Trajectory analysis is a data-driven approach to identify clusters (or groups) of observations which follow a similar path (trajectory) over time. Complementary to latent growth curve and hierarchical modeling, trajectory analysis uses a semiparametric modeling approach which allows for model parameters to differ across groups, but also accounts for the longitudinal change in the path of the trajectory for each group. Trajectory analysis methodology is an intersection of longitudinal data analysis techniques (e.g., generalized linear modeling and generalized estimation equation modeling) in which we take repeated measurements over time and analyze observed patterns and latent variable models (e.g., latent class analysis, cluster analysis and multivariate mixture estimation) where we use the data to find latent (unmeasured) patterns in the data and then describe them clinically. It provides a technique that identifies groups or subtypes in the data but extends it from one measurement to repeated, longitudinal patterns that unmeasured subgroups may take over time. Thus, as applied to the current problem, this model allows the analysis of the heterogeneity with respect to lethality of repeat attempters at the level of one attempt, but also in the development over each subsequent attempt. In this modeling approach, groups are established using trajectory analysis and the likelihood of a participant to belong to one of the groups is estimated. With group membership established based on the latent grouping of the data over time, the groups can then be compared to identify characteristics that may be similar between the two groups that could potentially be used for early identification of following a certain path. The statistical theory detailing the method has can be found in detail elsewhere (Nagin and Land 1993; Land, McCall, and Nagin 1996; Roeder, Lynch, & Nagin 1999; Nagin & Tremblay 1999; Nagin 1999). PROC TRAJ (Jones, Nagin, Roder 2001, Jones & Nagin 2007), a procedure developed for the SAS (ref) system, was used for analysis. This procedure uses the Bayesian Information Criterion (BIC, D'Unger, Land, McCall, and Nagin, 1998) to identify the ideal group solution to the trajectory model and estimates group membership and the probability thereof for each observed case. To define clinical characteristics, the identified groups were then compared on all baseline study variables using Chi Square or t-tests (2 tailed), as appropriate.
Results
A. Patient Characteristics
A total of 252 BPD subjects are currently enrolled in the longitudinal study. Of these, 195 (77.4%) are lifetime suicide attempters and 180 (71.4%) were attempters at time of intake. Attempters had a mean (s.d.) of 4.0 (3.5) lifetime attempts per subject at time of intake, with a range of 1 to 21 attempts. They were predominately Caucasian (77.8%), female (74.4%), never married (63.9%), and had low SES (Hollingshead Classes IV+V, 81.3%). Of baseline attempters, 35.6% were recruited as inpatients, 24.2% as outpatients, and 40.0% as non-patient volunteers; 43 (23.9%) had single attempts, 137 (76.1%) repeat attempts. In the course of the longitudinal study, 15 subjects with single attempts at baseline became repeat attempters, for a total of 152 lifetime repeat attempters.
B. Predictors of Attempt Lethality
Significant differences between single and repeat attempter groups are shown in Table 1. Compared to subjects with single attempts, repeat attempters were older, with more MDD, state depression, and poorer psychosocial functioning. They were more likely to have made High Lethality attempts, had higher lifetime maximum Lethality Rating Scale scores, and histories of prior hospitalizations.
Table 1.
Discriminating characteristics of single and repeat attempters.
| Single Attempter (n=43) | Repeat Attempter (n=137) | Stat, p | |
|---|---|---|---|
|
| |||
| Age (mean ± SD) | 27.0 ± 7.6 | 29.9 ± 8.1 | t=2.06, df=178, p=0.04 |
|
| |||
| Race (% Caucasian) | 88.4 | 74.5 | χ2=3.67, df=1, p=0.06 |
|
| |||
| SES (% Low) | 76.2 | 89.1 | χ2=4.43, df=1,p=0.04 |
|
| |||
| BDI | 20.6 ± 13.7 | 30.9 ± 11.0 | t=4.89, df=168, p<0.001 |
|
| |||
| HRSD | 17.8 ± 8.3 | 21.2 ± 8.6 | t=2.23, df=166, p=0.03 |
|
| |||
| Hopelessness | 8.5 ± 6.0 | 13.8 ± 5.2 | t=5.40, df=167, p<0.001 |
|
| |||
| GAS | 53.6 ± 10.8 | 49.7 ± 11.4 | t=1.98,df=178, p=0.05 |
|
| |||
| SAS Social/Leisure | 2.5 ± 0.6 | 3.0 ± 1.2 | t=2.35, df=163, p=0.02 |
|
| |||
| SAS Ex Family | 2.2 ± 0.5 | 2.6 ± 0.7 | t=3.16, df=163, p=0.002 |
|
| |||
| SAS Family Unit | 2.5 ± 0.8 | 2.9 ± 1.0 | t=2.11, df=108, p=0.04 |
|
| |||
| SAS Overall | 2.3 ± 0.5 | 2.6 ± 0.7 | t=3.03, df=163, p=0.003 |
|
| |||
| Major Depression (%yes) | 46.5 | 63.5 | χ2=3.92, df=1, p=0.05 |
|
| |||
| Maximum Lethality Scale Score | 2.0 ± 1.5 | 3.3 ± 1.7 | t=4.39, df=178, p<0.001 |
|
| |||
| Prior Hospitalization (%yes) | 53.5 | 83.7 | χ2=16.52, df=1, p.<0.001 |
|
| |||
| High Leth. Atts at baseline (%high) | 14.0 | 37.2 | χ2=8.19, df=1, p=0.004 |
|
| |||
| Suicide Intent Scale | |||
|
| |||
| SIS #9, Alleged Purpose (% yes): | χ2=8.42, df=3, p=0.02 | ||
| To manipulate/get attention | 28.6 | 10.2 | |
| Escape, solve problems | 19.0 | 23.6 | |
| Components of above | 52.4 | 66.1 | |
|
| |||
| SIS#10, Expectation of Lethality (%yes): | χ2=7.32, df=3, p=0.0.03 | ||
| Death Unlikely | 19.5 | 17.6 | |
| Death Possible but not Probable | 36.6 | 17.6 | |
| Death Probably Certain | 43.9 | 64.8 | |
|
| |||
| SIS #11, Conception of Lethality(%yes): | χ2=8.25, df=3, p=0.02 | ||
| Did less than would be lethal | 19.0 | 17.6 | |
| Not sure if action would be lethal | 42.9 | 21.6 | |
| Did what thought lethal | 38.1 | 60.8 | |
|
| |||
| SIS#12, Seriousness of Attempt(%yes): | FET, p=0.02 | ||
| Not attempt to end life | 14.3 | 7.9 | |
| Uncertain of seriousness | 35.7 | 18.9 | |
| Attempted to end life | 50.0 | 73.2 | |
|
| |||
| SIS#16, Reaction to attempt (%yes): | χ2=10.80, df=3,p=0.005 | ||
| Sorry, Foolish, Ashamed | 38.1 | 24.4 | |
| Accepts attempt and failure | 40.5 | 25.2 | |
| Regrets failure of attempt | 21.4 | 50.4 | |
Note: SES = Socio-Economic Class, BDI = Beck Depression Inventory, HRDS = Hamilton Depression Rating Scale, GAS = Global Assessment Scale, SAS = Social Adjustment Scale, SIS = Suicide Intent Scale FET = Fisher's Exact Test,
Characteristics of the most serious lifetime attempt at baseline were derived from an item analysis of the Suicide Intent Scale (Table 1). Compared to repeat attempters, more subjects with single attempts indicated their purpose was to manipulate, get attention, or revenge (item 9), felt death was “possible but not probable” (item 10), were not sure if (their) action would be lethal (item 11), were uncertain about seriousness to end life (item 12), felt “sorry, foolish, ashamed” or accepted the failure of their attempt (item 16). In contrast, more subjects with repeat attempts felt “death was probable or certain” (item 10), “equaled or exceeded what (they) thought was lethal” (item 11), seriously attempted to end life (item 12), and regretted the failure of the attempt (item 16).
The groups did not differ in gender, recruitment source, SES, marital status, educational level (HS or greater), co-morbid ASPD, SUD, impulsivity, aggression or history of childhood abuse. A higher proportion of minority subjects tended to have repeat attempts compared to Caucasian subjects (Table 1).
Using the sample of repeat baseline attempters, a logistic regression analysis was conducted seeking associations between the discriminating variables and Lethality status. Baseline predictors of lifetime High Lethality status included a history of prior hospitalization [OR =4.28, 95%C.I.: 1.40–13.10, p. = 0.01], and older age [OR = 1.05, 95% C.I.: 1.00 – 1.10, p. = 0.025]. Good psychosocial functioning (high baseline GAS) was protective [OR = 0.96, 95%C.I.: 0.92 – 0.99, p. = 0.007]. Co-morbidity with MDD was not a significant predictor and had little effect on these results when entered as a co-variate. B. Increasing lethality over time.
Among the 252 BPD subjects in the longitudinal study, 152 (60.3%) had a lifetime history of repeat attempts, including both baseline and follow-up attempts. Among lifetime repeat attempters, 38 subjects (25%) had no change in Lethality Rating Scale scores across repeat attempts; 23 (15.1%) had their maximum medical lethality score on their first attempt, and 91 subjects (59.9%) had at least one increasing Lethality Rating Scale score across attempts. Among repeat attempters, the mean (s.d.) maximum Lethality Rating Scale score across the first 6 lifetime attempts was 3.5 (1.6); however, for the 91 repeat attempters with increasing scores, the mean (s.d.) maximum medical lethality score was 4.0 (1.5), across 5.3 (4.0) attempts. Maximum Lethality Rating Scale scores increased significantly between the first and third lifetime attempts. (t 3.24, 114df, p.002, (p.01 required for Bonferroni correction.) (Fig. 1) The same pattern was found when analysis was limited to the 36 subjects with 6 or more lifetime attempts (t = 2.81, 35 df, p. = 0.008).
Figure 1.
Increase in Attempt Lethality with Repeat Attempts
Among the 91 repeat attempters who had an increase in attempt lethality with repeat attempts, the time from first attempt to the attempt with maximum medical lethality was long and extremely variable, with a mean (s.d.) of 465 (414) weeks (i.e. 8.94 years), median of 354 weeks (6.81 years) and a range of 8 weeks to 1930 weeks (37.1 years).
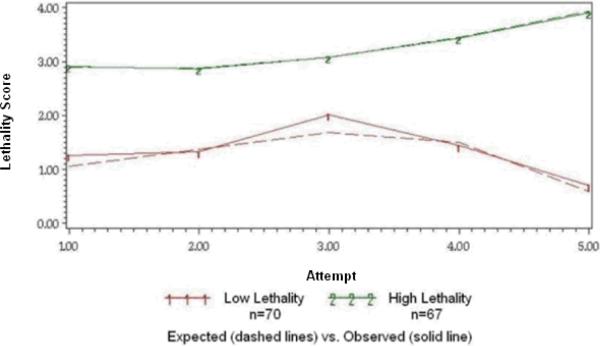
C. Trajectory Analysis
A Trajectory analysis of lifetime maximum Lethality Rating Scale scores by attempt number was conducted on 137 repeat attempters with up to 5 lifetime attempts. The best fitting model was a 2-group solution, which identified one group (n= 70, 51.1%) with an index attempt of lower lethality and little change with subsequent re-attempts (“Low Lethality” group), and a second group (n = 67, 48.9%) with an index attempt of higher lethality and increasing lethality with re-attempts (“High Lethality” group) (Fig.2). Compared to the Low Lethality group, the High Lethality group was predominately recruited from inpatient units (X2 = 3.88, 1df, p. =0.05), and had poorer psychosocial functioning at baseline (i.e. lower GAS (t. = 2.39, 135 df, p. = 0.02), higher SAS-sr-overall score (t. = 2.22, 121 df, p. = 0.03). Two subscales of the SAS-sr contributed most to this difference: poor relationships in the immediate family unit (t = 1.99, 81df, p. = 0.049), and a poor work history (t = 2.01, 118 df, p. = 0.047.) The groups did not differ significantly on measures of diagnostic co-morbidity, mood, impulsivity or aggression, The Low Lethality group endorsed more BDHI Negativism (t 3.26, 118df, p.= 0.001).
Figure 2.
Trajectory of Lethality Rating Scale Scores Across 5 Attempts
Since attempt lethality in the overall sample peaked at the third attempt, we re-ran the trajectory analysis on 137 repeat attempters using Lethality Rating Scale scores for the first 3 attempts only. This “conservative” model has the advantage of minimizing missing data and is based more on “actual” than “expected” lethality scores. As in the 5 attempt model, a 2 class solution was found. The High Lethality group (n = 106) was again characterized by poorer psychosocial functioning (e.g. lower GAS score, t = 2.23, df = 57.6, p.= 0.03), while the Low Lethality group (n=31) had more Negativism (t =2.25, df = 118, p.= 0.03), lifetime Substance Use Disorders (X2 = 4.56, df = 1, p. = 0.04) and co-morbidity with Cluster B histrionic and/or narcissistic PDs compared to the High Lethality group (X2 = 4.90, df = 1, p.= 0.03). Prevalence of Antisocial PD did not differ between groups. Negativism was significantly associated with a lifetime history of Substance Use Disorders in the total sample (t = 2.03, df = 227, p. = 0.04).
DISCUSSION
Risk factors associated with high lethality attempts and completed suicide in BPD include older age, lower SES, social, vocational and financial stressors, similar to other high-risk groups. The role of co-morbid depression or substance use disorders is equivocal, with some studies, though not all, finding a relationship (Soloff 2005, for review). Are there unique characteristics of BPD which increase vulnerability to suicidal behavior? Cross-diagnostic studies suggest that the borderline patient's high frequency of attempts, impulsive and antisocial behaviors (or ASPD co-morbidity) increase their risk of suicidal behavior. Within the BPD diagnosis, high lethality attempts are predicted by low SES, comorbidity with ASPD, a high degree of subjective intent to die and long treatment histories. Impulsivity and aggression are ubiquitous within a cohort of BPD subjects and do not discriminate between high and low lethality attempters (Soloff, Fabio, Kelly, Malone & Mann, 2005). However, impulsivity is significantly related to frequency of attempts and may play an indirect role in high lethality attempts and completion (Chesin, Jeglic & Stanley, 2010). The interaction of impulsivity and aggression may contribute to suicide completion in BPD, though this effect is not significant after controlling for Cluster B co-morbidity, (i.e. co-morbid ASPD, found in 92.5% of suicides (McGirr, Paris, Lesange, Renaud & Turecki, 2007). In the present study, we assessed the predictive association of these risk factors with high lethality attempts and increasing trajectories of attempt lethality over time in an effort to define a poor prognosis subtype of BPD.
Among repeat suicide attempters, we found older age and a history of prior hospitalizations predicted High Lethality attempter status, suggesting that chronicity and illness severity play an important role in the vulnerability to high lethality suicidal behavior. These results are consistent with earlier retrospective studies of completed suicide in patients with BPD, which found greater initial illness severity, prior attempts, more admissions and time in hospital among suicide victims (Soloff, 2005). The time to maximum attempt lethality among subjects with increasing Lethality Scale scores in our sample was measured in years (mean 8.94 years), but with extreme variance. Studies of completed suicide in BPD report that the duration of the “suicidal process,“ from first unequivocal suicidal communication (by verbal threat and attempt) to death, may be as brief as 30 months (Runeson, Beskow & Waern, 1996) or as long as 10 years (Paris & Zweig-Frank, 2001). Suicide completion in BPD tends to occur relatively late in the course of the illness. In their 27 year follow-up study, Paris and Zweig-Frank (2001) reported that completed suicide occurred at an average age of 37 years. Younger patients with BPD tended to make frequent low lethality attempts as communicative gestures while older patients completed suicide after years of illness.
A subgroup of borderline patients may experience increasing psychosocial impairment as they age, increasing the vulnerability to suicidal behavior (McGlashen, 1986). Older patients in the CLPS sample (e.g. those recruited at age 35–45 years of age) began to lose previously achieved psychosocial improvement by the third year of follow-up, reversing the direction of change. From the third through sixth year, the older cohort showed a progressive decline in function and an increase in psychopathology, significantly different from 2 younger, more stable cohorts (Shea, 2009).
Good psychosocial functioning was protective in our analysis of attempt lethality, while poor psychosocial functioning was associated with repeated suicide attempts, and a trajectory of increasing attempt lethality over time. Similar findings have been reported in prospective studies of repeat suicide attempters, independent of diagnosis. In a 10 year study of patients admitted following a suicide attempt, Tejedor, Diaz, Castillon & Pericay et.al. (1999) found that higher GAF scores on admission and at last evaluation were associated with lower probability of repeated suicide attempt and completion. Similarly, Cedereke and Ojehagen (2005) reported that a low GAF score (i.e. less than 49) one month after an index attempt, predicted recurrent attempts in the ensuing 1–12 months. In a cross-diagnostic study, Kelly, Soloff, Lynch, Haas & Mann, (2000) found that depressed and non-depressed patients with BPD who were low on social adjustment were 16 times more likely to be suicide attempters than patients with MDD alone. In our longitudinal studies, we noted that poor psychosocial functioning was a prospective predictor of suicide attempts at 1 year, 2 year and 2 to 5 year follow-ups (Soloff and Fabio, 2008a).
How is psychosocial function protective? Kelly (2000) suggests that good psychosocial function buffers the stress of recent life events in subjects with BPD. Negative life events were significant predictors of suicide attempts among PD subjects in the CLPS analysis (Yen, Pagano, Shea, Grilo, Gunderson, Skodol et al., 2005). BPD subjects experiencing negative life events, often as a result of their own actions, may lack the psychological, social or financial resources to cope with the ensuing consequences.
Poor psychosocial function remains a risk factor for suicidal behavior in BPD long after acute and temperamental symptoms of the disorder are remitted. The McLean Study found that only half of BPD patients achieved good social and vocational functioning by 10 year follow-up, despite symptomatic improvement in 93% of patients. Among patients who failed to obtain good psychosocial functioning, 93.9% failed because of impaired vocational achievement, not poor social functioning (Zanarini, 2010). The CLPS analysis found that unstable interpersonal relationships were a significant predictor of poor outcome at two year follow-up, but did not assess vocational achievement (Gunderson, Daversa, Grilo, McGlashan Zanarini, Shea, et.al. 2006). Our Trajectory analysis suggests that the High Lethality subgroup is characterized by impairment in both family relationships and work achievement. This is consistent with studies in PD patients which find suicide completion associated with job problems, unemployment, and financial difficulties, but also problems with family relationships, interpersonal loss, separations, and loneliness (Heikkinen, Isometsa, Henriksson,, Marttunen, Aro, Lonnqvist et.al. 1997a,b).
To the best of our knowledge, this is the first reported use of trajectory analysis to characterize patterns of attempt lethality over time. Finding a two class solution suggests that trajectory analysis is a useful statistical tool to identify BPD subtypes relative to suicidal behavior. Subjects with the High Lethality trajectory were characterized by inpatient recruitment (an indirect measure of illness severity), and poor psychosocial functioning compared to those with Low Lethality trajectories. Convergent results in our regression and trajectory analyses suggest that the patient at highest risk for suicide may be older, with greater illness severity, vocational failures, and estrangement from family and friends. Low Lethality subjects had better overall psychosocial functioning but more Negativism, lifetime substance abuse and Cluster B histrionic and /or narcissistic PD co-morbidity. We speculate that the attempts of this group may reflect dramatic “communicative gestures,” which show little change in medical lethality with repeat attempts.
Limitations
Attempters are not completers, but overlapping populations (Maris, Berman & Silverman, 2000). Although a history of prior attempt is a strong predictor of repeat attempts and completion, predictors based on attempt behavior may not apply directly to patients who complete suicide. The same may be true of subtypes defined by attempt behavior. Characteristics of High Lethality attempters with BPD resemble those of suicide completers (Soloff, 2005a).
Several negative findings are noteworthy. We found no significant role for MDD or measures of depressed mood as predictors of attempt lethality or characteristics of BPD subtypes related to lethality. The association of co-morbid MDD with suicidal outcomes in BPD is inconsistent in the literature (Soloff, 2005 b). Large, epidemiologic studies find that mild depressive syndromes (e.g. depression nos), but not MDD, are common in PD patients who complete suicide (Isometsa, Henriksson, Heikkinen, Aro, Marttunen, Lonnqvist et al., 1996). The prevalence of MDD among BPD patients may diminish over time, perhaps reflecting the efficacy of treatment or natural history of the disorder (Paris & Zweig-Frank, 2001). In our longitudinal studies of suicidal behavior in BPD, we used Cox proportional hazards models to identify baseline predictors of medically significant suicide attempts at 1 year, 2 years, and 2–5 year follow ups. MDD was a prospective predictor of suicide attempts in BPD in the first year following assessment, but not at 2 years and beyond. “Outpatient treatment” (prior to any attempt in the interval) was significantly associated with decreased risk of a suicide attempt in the 12 month follow-up, and in the 24 – 60 month follow-up intervals. i.e. Treatment was protective (Soloff & Fabio, 2008).
We found no predictive associations between attempt lethality and measures of impulsivity (BIS), aggression (LHA), or ASPD co-morbidity. Impulsive-aggression is associated with attempt behavior across diagnoses (Mann, Waternaux, Haas & Malone, 1999), and in patients with affective disorders (Oquendo, Galfalvy, Russo, Ellis, Grunebaum, Burke et al., 2004). ASPD is associated with high lethality attempts in subjects with BPD (Soloff, 2005a), and Cluster B co-morbidity (primarily ASPD with impulsive-aggression) with completed suicide (McGirr, Paris, Lesage, Renaud & Turecki, 2007). Impulsive-aggression is a defining characteristic of BPD, ubiquitous within a BPD sample, and did not predict degrees of attempt lethality in our previous retrospective or prospective studies (Soloff, 2005; Soloff, 2008). Increased numbers of subjects and suicide attempts are needed to further refine the trajectory analysis, and will result in a more detailed description of BPD subtypes in relation to suicidal behavior.
Acknowledgments
Research supported by a National Institute of Mental Health Grant : MH 48463 (PHS)
Footnotes
Presented, in part, at the annual meeting of the American Psychiatric Association, New Orleans, 24 May, 2010
References
- Barratt ES. Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychol Rep. 1965;16:547–554. doi: 10.2466/pr0.1965.16.2.547. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck R, Kovacs M. Classification of suicidal behavior. I: Quantifying intent and medical lethality. American Journal of Psychiatry. 1975;132:285–287. doi: 10.1176/ajp.132.3.285. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The Measurement of Pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Brown GL, Goodwin FK, Ballenger JC, Goyer PF, Major LF. Aggression in humans correlates with cerebrospinal fluid amine metabolites. Psychiatry Res. 1979;1:131–139. doi: 10.1016/0165-1781(79)90053-2. [DOI] [PubMed] [Google Scholar]
- Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J. Consult. Clin. Psychol. 1957;21:343–349. doi: 10.1037/h0046900. [DOI] [PubMed] [Google Scholar]
- Cederecke M, Ojehagen A. Prediction of repeated parasuicide after 1–12 months. European Psychiatry. 2005;20:101–10. doi: 10.1016/j.eurpsy.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Chesin MS, Jeglic EL, Stanley B. Pathways to high lethality suicide attempts in individuals with borderline personality disorder. Archives of Suicide Research. 2010;14:342–362. doi: 10.1080/13811118.2010.524054. [DOI] [PubMed] [Google Scholar]
- D'Unger AV, Land KC, McCall PL, Nagin DS. “How Many Latent Classes of Delinquent/Criminal Careers? Results From Mixed Poisson Regression Analyses of the London, Philadelphia, and Racine Cohorts Studies.”. American Journal of Sociology. 1998;103:1593–630. [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Daversa MT, Grilo CM, McGlashan TH, Zanarini MC, Shea MT, Skodol AE, Yen S, Sanislow CA, Bender DS, Dyck IR, Morey LC, Stout RL. Predictors of 2-year outcome for patients with borderline personality disorder. Am.J.Psychiatry. 2006;163:822–826. doi: 10.1176/ajp.2006.163.5.822. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Kolb JE, Austin V. The Diagnostic Interview for Borderlines. Am J. Psychiatry. 1981;138:896–903. doi: 10.1176/ajp.138.7.896. [DOI] [PubMed] [Google Scholar]
- Guy W. ECDEU Assessment Manual for Psychopharmacology, Revised. National Institute of Mental Health; Rockville, MD: 1976. [Google Scholar]
- Hathaway SR, McKinley JC. The Minnesota Multiphasic Personality Inventory. Univ. of Minnesota Press; Minneapolis: 1943. [DOI] [PubMed] [Google Scholar]
- Heikkinen ME, Isometsa ET, Henriksson MM, Marttunen MJ, Aro HM, Lonnqvist JK. Psychosocial factors and completed suicide in personality disorders. Acta Psychiatr Scand. 1997;95:49–57. doi: 10.1111/j.1600-0447.1997.tb00373.x. [DOI] [PubMed] [Google Scholar]
- Isometsä ET, Henriksson MM, Heikkinen ME, Aro HM, Marttunen MJ, Lonnqvist KI, Lönnqvist JK. Suicide among subjects with personality disorders. Am J Psychiatry. 1996;153:667–673. doi: 10.1176/ajp.153.5.667. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS Procedure for estimating them. Sociological Methods Research. 2007;35:542–570. [Google Scholar]
- Kelly TM, Soloff PH, Lynch KG, Haas GL, Mann JJ. Recent life changes, social adjustment and suicide attempts in patients with major depression and borderline personality disorder. Journal of Personality Disorders. 2000;14(4):316–326. doi: 10.1521/pedi.2000.14.4.316. [DOI] [PubMed] [Google Scholar]
- Land KC, McCall PL, Nagin DS. A Comparison of Poisson, Negative Binomial, and Semiparametric Mixed Poisson Regression Models With Empirical Applications to Criminal Careers Data. Sociological Methods & Research. 1996;24:387–440. [Google Scholar]
- Laub JH, Nagin DS, Sampson RJ. Good Marriages and Trajectories of Change in Criminal Offending. American Sociological Review. 1998;63:225–38. [Google Scholar]
- Leckman JF, Sholomskas D, Thompson D, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis. Arch Gen Psychiatry. 1982;39:879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- Loranger AW, Janca A, Sartorius N. Assessment and diagnosis of personality disorder: The ICD-10 International Personality Disorder Examination (IPDE) Cambridge University Press; Cambridge: 1997. [Google Scholar]
- Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am.J. Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- Maris RW, Berman AL, Silverman MM. Comprehensive Textbook of Suicidology. The Guilford Press; New York: 2000. p. 19. [Google Scholar]
- McGirr A, Paris J, Lesage A, Renaud J, Turecki G. Risk factors for suicide completion in borderline personality disorder: A case-control study of cluster B comorbidity and impulsive aggression. J. Clin. Psychiatry. 2007;68(5):721–729. doi: 10.4088/jcp.v68n0509. [DOI] [PubMed] [Google Scholar]
- McGlashan TH. The Chestnut Lodge follow-up study, III: longterm outcome of borderline personalities. Arch Gen Psychiatry. 1986;43:20–30. doi: 10.1001/archpsyc.1986.01800010022003. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Analyzing Developmental Trajectories: A Semi-Parametric, Group-Based Approach. Psychological Methods. 1999;4:139–77. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nagin DS, Land KC. Age, Criminal Careers, and Population Heterogeneity: Specific Estimation of a Nonparametric, Mixed Poisson Model. Criminology. 1993;31:327–62. [Google Scholar]
- Nagin DS, Tremblay RE. Trajectories of Boys' Physical Aggression, Opposition, and Hyperactivity on the Path to Physically Violent and Non Violent Juvenile Delinquency.”. Child Development. 1999;70:1181–96. doi: 10.1111/1467-8624.00086. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Galfalvy H, Russo S, Ellis SP, Grunebaum MF, Burke A, Mann JJ. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry. 2004;161:1433–1441. doi: 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Halberstam B, Mann JJ. In: Risk factors for suicidal behavior: the utility and limitations of research instruments, in Standardized Evaluation in Clinical Practice. First MB, editor. American Psychiatric Publishing; Washington, DC: 2003. pp. 103–131. [Google Scholar]
- Paris J, Zweig-Frank H. A 27-year follow-up of patients with borderline personality disorder. Comprehensive Psychiatry. 2001;42:782–487. doi: 10.1053/comp.2001.26271. [DOI] [PubMed] [Google Scholar]
- Raftery AE. Bayesian Model Selection in Social Research. In: Marsden PV, editor. Sociological Methodology. American Sociological Association; Washington, DC: 1995. pp. 111–163. [Google Scholar]
- Roeder R, Lynch KG, Nagin DS. Modeling Uncertainty in Latent Class Membership: A Case Study in Criminology. Journal of the American Statistical Association. 1999;94:766–76. [Google Scholar]
- Runeson BS, Beskow J, Waern M. The suicidal process in suicides among young people. Acta Psychiatrica Scand. 1996;93:35–42. doi: 10.1111/j.1600-0447.1996.tb10616.x. [DOI] [PubMed] [Google Scholar]
- Shea MT, Edelen MO, Pinto A, Yen S, Gunderson JG, Skodol AE, Markowitz J, Sanislow CA, Grilo CM, Ansell E, Daversa MT, Zanarini MC, McGlashan TH, Morey LC. Improvement in borderline personality disorder in relation to age. Acta Psychiatr Scand. 2009;119:143–148. doi: 10.1111/j.1600-0447.2008.01274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea MT, Stout R, Gunderson J, Morey LC, Grilo CM, McGlashan T, Skodol AE, Dolan-Sewell R, Dyck I, Zanarini MC, Keller MB. Short-term diagnostic stability of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. Am. J. Psychiatry. 2002;159:2036–2041. doi: 10.1176/appi.ajp.159.12.2036. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Fabio A, Kelly T, Malone KM, Mann JJ. High Lethality Status in patients with borderline personality disorder. J. Personality Disorder. 2005;19(4):386–399. doi: 10.1521/pedi.2005.19.4.386. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Fabio A. Prospective predictors of suicide attempts in borderline personality disorder at one, two and two-to-five year follow-up. Journal of Personality Disorders. 2008;22(2):123–134. doi: 10.1521/pedi.2008.22.2.123. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Lynch KG, Kelly TM. Childhood abuse as a risk factor for suicidal behavior in borderline personality disorder. J. Personality Disorders. 2002;16(3):201–214. doi: 10.1521/pedi.16.3.201.22542. [DOI] [PubMed] [Google Scholar]
- Soloff PH. Risk factors for suicidal behavior in borderline personality disorder: A review and update. In: Zanarini MC, editor. Borderline Personality Disorder. Taylor & Francis; Boca Raton, FL: 2005. pp. 333–365. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Instruction Manual for the Structured Clinical Interview for DSM-III-R, Biometrics Research Department. New York State Psychiatric Inst.; New York, NY: 1988. [Google Scholar]
- Tejedor MC, Diaz A, Castillon JJ, Pericay JM. Attempted suicide: repetition and survival – findings of a follow-up study. Acta Psychiatrica Scandinavica. 1999;100(3):205–211. doi: 10.1111/j.1600-0447.1999.tb10847.x. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Yen S, Pagano ME, Shea MT, Grilo CM, Gunderson JG, Skodol AE, McGlashan TH, Sanislow CA, Bender DS, Zanarini MC. Recent life events preceding suicide attempts in a personality disorder sample: Findings from the Collaborative Longitudinal Personality Disorders Study. Journal of Abnormal Psychology. 2005;112(3):375–381. doi: 10.1037/0022-006X.73.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G, Weinberg I, Gunderson JG. The 10-year course of physically self-destructive acts reported by borderline patients and Axis II comparison subjects. Acta Psychiatr Scand. 2008;117:177–184. doi: 10.1111/j.1600-0447.2008.01155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: A 10 year prospective follow-up study. Am.J.Psychiatry. 2010 doi: 10.1176/appi.ajp.2009.09081130. in advance April 15, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini M, Gunderson JG, Frankenburg FR, Chauncey DL. The revised diagnostic interview for borderlines: Discriminating BPD from other axis II disorders. Journal of Personality Disorders. 1989;3(1):10–18. [Google Scholar]