Abstract
A complex sequence of steps is required for insulin to cause glucose uptake. Impairment of any one of these steps can contribute to insulin resistance. We observed the effect of insulin resistance induced by hyperlipidemia on the dynamics of insulin injected into skeletal muscle. Basal insulin euglycemic clamps (0.2mU/min/kg) with or without lipid infusions (20% at 1.5ml/min) were done on anesthetized dogs. Sequential insulin doses were administered by intramuscular injection directly into the vastus medialis of one hindleg, using the contralateral leg for comparison. Intramuscular insulin injection in normal animals caused a clear dose-dependent increment in interstitial insulin levels, as well as dose-dependent increase in leg glucose uptake. In a second group of animals, lipid was infused before and during intramuscular insulin injection to cause systemic increase in free fatty acids. In sharp contrast, systemic lipid infusion caused insulin resistance, indicated by reduced glucose infusion required to maintain euglycemia, and prevented injection-induced increase in lymphatic insulin and leg glucose uptake observed without lipid. The injected insulin was instead detected in the venous outflow from the leg. Lipid infusion caused intramuscular insulin to be diverted from interstitium into the capillary circulation, preventing a rise in intersitial insulin and any increase in local leg glucose uptake. The diversion of insulin from the interstitium under hyperlipidemic conditions may play a role in the insulin resistance observed coincident with elevated nocturnal free fatty acids as is observed in obesity.
INTRODUCTION
Insulin resistance is a risk factor for various diseases, including type 2 diabetes, cardiovascular disease, hypertension and cancer (1). The mechanisms causing insulin resistance continue to be debated (2). Most research currently focuses on cellular defects and signaling abnormalities (3). But, there are other factors that enhance insulin mediated glucose disposal. For skeletal muscle and adipose tissue, insulin must first cross the capillary endothelial barrier, and enter the interstitial space. Once in interstitium, insulin can bind to insulin receptors to initiate signaling cascades, causing GLUT4 translocation and glucose uptake (4;5). In insulin resistant states including Type 2 diabetes, there is a reduction in skeletal muscle insulin signaling (5-7). Intracellular lipids in muscle and liver can interfere with oxidative phosphorylation in the mitochondria, activating kinases that reduce insulin signaling and glucose transport (8). While reduction in insulin signaling may be a cause of insulin resistance, it could also result from reduced access of insulin to the interstitial space and insulin receptors (9).
In fact, we have presented evidence that experimental obesity due to high-fat diet reduces access of insulin to skeletal muscle (10) possibly due to changes in capillary recruitment (11) or sluggish transport of insulin across the capillary endothelium (12). Definitive studies showing that insulin resistance is associated with a decrease in the hormone's ability to access insulin-sensitive tissues are lacking.
Many studies examining the effects of free fatty acids on insulin action involve insulin resistance secondary to acute hyperlipidemia caused by infusion of lipid. The latter raises plasma free fatty acids, which inhibit insulin signaling (13) and impair insulin-mediated glucose transport in skeletal muscle (14;15), possibly secondary to impaired insulin signaling (16;17). Also, increased intramyocellular lipid content has been associated with the development of insulin resistance (3;18). We suggest that lipid-mediated cellular defects in insulin action may be secondary to insulin's failure to access skeletal muscle during lipid infusion.
Even in normal individuals, glucose uptake is delayed after insulin infusion, becoming significantly elevated only 30 minutes after the beginning of the hyperinsulinemic euglycemic clamp, and does not reach steady state for several hours. Changes in capillary recruitment occur much earlier than increased glucose disposal; from 7 minutes, reaching a peak at approximately 20 minutes (19). The insulin action delay may be due to sluggish appearance of insulin in the interstitial space, delaying the binding of insulin to myocytes (20). Data in healthy canines indicates delivery of insulin to the interstitial space is temporally limiting (21); whether this is due to trans-endothelial transport delay or changes in distribution of blood flow that supplies muscle is not clear.
Here, we used the intramuscular injection of insulin to investigate the correlation between interstitial insulin concentrations and local glucose uptake in skeletal muscle. Insulin was injected into a hindlimb muscle under hyperlipidemia induced by lipid infusion. If lipid causes insulin resistance at the receptor or signaling level, there would be a delay in local glucose uptake even with immediate appearance of interstitial insulin, such that for the same amount of interstitial insulin, less glucose uptake occurs. In effect, the myocytes would become resistant at a cellular level. However, if interstitial insulin causes local glucose uptake to a comparable extent with or without lipid infusion, resistance caused by lipid is upstream of the interstitial space, and the issue is delivery to the interstitial space. The present data argues that hyperlipidemia induced by lipid infusion causes insulin resistance by limiting the access of insulin to the interstitial space.
METHODS AND PROCEDURES
Animals
One acute glucose clamp experiment was performed on each of 8 anesthetized one year-old male mongrel dogs (29.6±1.6kg lipid, 31.3±1.3kg control). Large animals were necessary to allow dynamic collection of skeletal muscle lymph exudate, which mirrors interstitial fluid. For ethical reasons, it is mandatory to utilize a minimal number of animals in acute experiments such as these. Therefore we utilized control experiments, previously published using the identical experimental design but in which lipid was not infused (n=13) (21). Control studies used a similar protocol and overlapped the time frame of lipid studies, so we did not consider it prudent to repeat identical previously published control experiments for this manuscript, and previous data is shown here.
Before experiments animals were housed in the University of Southern California Medical School Vivarium under controlled conditions (12h light:12h dark) and fed standard chow (49% carbohydrate, 25% protein, 9% fat; Alfred Mills, Chicago, IL) once per day. Dogs in good health as determined by visual observation, body weight, hematocrit, and body temperature were used for experiments. Protocols were approved by the USC Institutional Animal Care and Use Committee, and were in accordance with the Principles of laboratory animal careg suggested by the NIH.
Surgery
Animals were fasted 15 hours before the morning of the experiment at 0600hrs and preanesthetized with acepromazine maleate (Prom-Ace, Aueco, Fort Dodge, IA; 0.22mg/kg) and atropine sulfate (Western Medical, Arcadia, CA; 0.11mL/kg). Anesthesia was induced with sodium pentobarbital (Western Medical, Arcadia, CA; 0.44mL/kg) and maintained with inhalant isofluorane (Western Medical, Arcadia, CA). Dogs were placed on heating pads to maintain body temperature. Indwelling catheters were implanted in the right jugular vein for a continuous saline drip (~1L for the first 60 minutes of surgery and a slow drip thereafter) and the left carotid artery for sampling and blood pressure monitoring (Space Labs, Issaquah, WA; model #90603A). Intracatheters were inserted into the left cephalic vein for variable glucose infusion and the right cephalic vein for insulin, somatostatin and lipid infusion. Indwelling catheters were placed into both right and left femoral arteries and veins for blood sampling. Perivascular ultrasonic flowprobes (2mm diameter; Transonic, Ithaca, NY) were placed around right and left femoral arteries proximal to the femoral catheter for measuring blood flow rates. Left and right hindlimb lymphatic vessels were cannulated by placing polyethylene catheters (PE10) into the afferent lymphatic vessels of the deep inguinal lymph node. Blood pressure, heart rate, O2 saturation and CO2 were monitored continuously. At the conclusion of these experiments, animals were euthanized with an overdose of sodium pentobarbital (Eutha-6, Western Medical; 65mg/kg).
Clamps
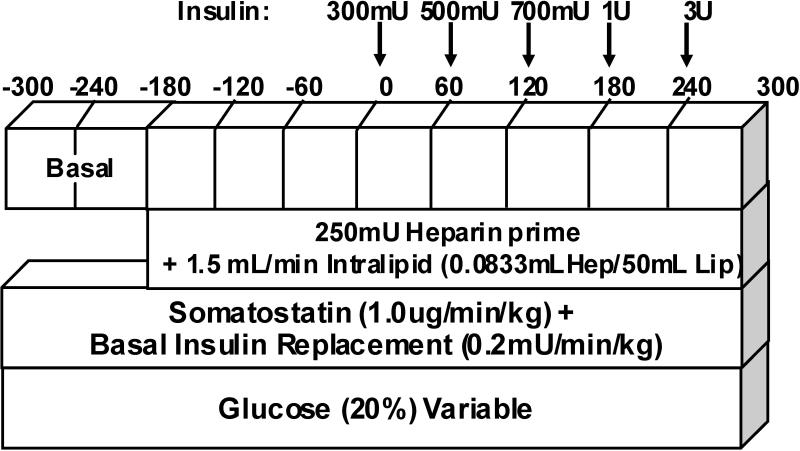
Immediately after starting surgical procedures, a basal insulin eugylcemic clamp was started (t=−240min). Simultaneous systemic infusions of somatostatin (1ug.min−1kg−1; Bachem) and basal insulin replacement (0.2mU.min−1kg−1; Novo Nordisk, Bagsvaerd, Denmark) were continued for the remainder of the study (Fig. 1). Exogenous 20% glucose was infused at variable rates to maintain euglycemia at the basal level based on online glucose measurements from the injected leg's (INJ) femoral artery plasma. (established prior to insulin infusion) throughout the entire experimental period. At least sixty minutes after insulin infusion commenced, a bolus of heparin was given (250mU), immediately followed by a lipid infusion containing heparin (20% Liposyn with 16mU/ml heparin, 1.5ml/min). Samples were taken simultaneously from the right and left femoral arteries and veins. Left and right hindlimb lymph vessels were sampled by gently massaging the hindlimb distal to the site of catheterization from 2 minutes prior to 2 minutes after each blood sample.
Figure 1.
Experimental protocol used throughout the study. Time in minutes is shown across the top. Somatostatin was infused with basal insulin replacement, glucose was infused at a variable rate to maintain euglycemia. In lipid experiments, 180 minutes prior to the first injection, a priming heparin injection was given, and lipid infusion was initiated. Samples were taken periodically to ensure euglycemia was maintained. Every 60 minutes from time 0, an insulin injection was given, with doses of 300mU, 500mU, 700mU, 1U and 3U. Samples were taken every 10 minutes during from time 0-300 from the femoral artery and vein, as well as lymph, of INJ and NINJ legs.
Intramuscular insulin
At times 0, 60, 120, 180 and 240 minutes, porcine insulin (0.3, 0.5, 0.7, 1, and 3U) was injected into the vastus medialis of the quadriceps femoris with two 30 gauge needles inserted approximately 1cm apart with a volume of 0.5mL per syringe (Fig. 1A), given at approximately 0.6ml/min. Simultaneous injection enabled a larger area of distribution of insulin throughout the muscle, and subsequent injections were administered to a similar area as the original injection for consistency between administrations. Volume and rate of injection was matched for each dose to ensure similar tissue damage (if any) among doses. For individual experiments, right or left hindlimb was chosen at random for injections (INJ) while the non-injected contra-lateral limb (NINJ) was used for comparison. Plasma and lymph samples were taken every 10 minutes after each injection.
Assays
Plasma and lymph samples were collected in microtubes that were pre-coated with lithium-heparin (Becton Dickinson, Franklin Lakes, NJ) and assayed for insulin and glucose. Plasma tubes also contained 50uL 20g/L EDTA (Sigma Chemicals) providing less than 5% dilution of sample. Blood samples were centrifuged immediately; the supernatant was transferred and stored at −20°C until further assay. INJ femoral artery plasma samples were immediately assayed for glucose with an YSI 2700 auto-analyzer (Yellow Springs Instrument Co., Yellow Springs, OH) before freezing at −20°C. Lymph samples were stored at −20°C after sampling. Samples were assayed for insulin by ELISA, and glucose with an YSI 2700 auto-analyzer.
Calculations
We calculated “net” insulin or local glucose uptake as INJ minus NINJ values. Glucose uptake across each limb was calculated based on Fick's principle: LGU=(GA-GV)*BF, where LGU=local glucose uptake; GA=arterial glucose; GV=venous glucose; BF=femoral blood flow.
Statistical analyses
All experimental data are expressed as the means ± SE, and interpolated where necessary. Two-way repeated measures (RM) ANOVAs were performed on all groups; once a significant difference was detected, comparisons made within each group (control or lipid) used paired t-tests, and control and lipid groups were compared using unpaired t-tests. Significance was assumed at P≤0.05.
RESULTS
Glucose clamp stability
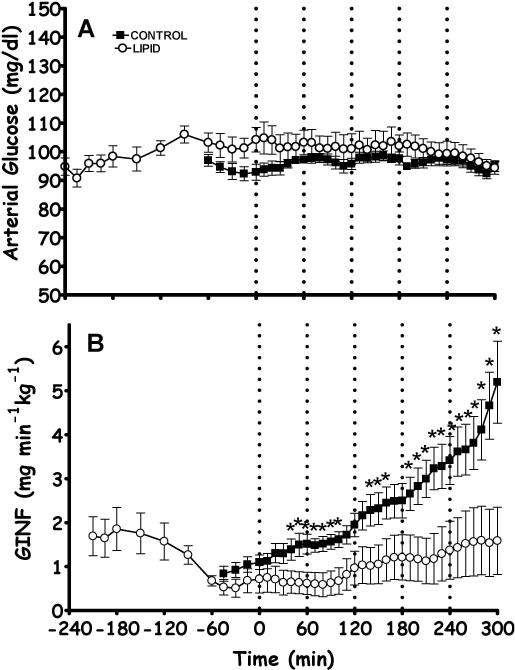
Artery glucose was successfully clamped at each animal's basal glucose concentration (99.1±2.0mg/dl) as shown in Fig. 2A, and was not different from studies without lipid infusion. The infusion rate required to maintain euglycemia was significantly reduced in the presence of lipid (compared to control data (21), two-way RM ANOVA Fig. 2B).
Figure 2.
A. Femoral artery glucose,was maintained throughout the experiment by modifying the glucose infusion rate (GINF)(B). Dotted lines represent an intramuscular insulin injection of increasing concentration, in control (black filled symbols) and lipid (white symbols) experiments as described in the methods. Lipid infusion began at -180minutes, and basal insulin replacement occurred throughout the experiment; unpublished data shows that lipid causes insulin resistance in 2-3hours. 2-way RM ANOVA demonstrated no difference in arterial glucose, but a significant difference in GINF between groups; these were then analyzed by unpaired t-test at each timepoint.
Blood Pressure and Blood Flow
Vital signs were monitored and maintained throughout the experiments, with an average systolic blood pressure of 124.5±1.0mmHg, diastolic pressure of 57.0±0.4mmHg and pulse of 109.7±0.4bpm, all of which are significantly different from control values (108.7±0.4mmHg, 47.6±0.7mmHg, 112.7±0.5bpm, respectively). Blood flow comparing INJ to NINJ legs was not significantly different at basal (INJ 171.6±21.04ml/min; NINJ 172.0±16.17 ml/min, P=0.622) and was unaffected by lipid infusion (Control basal: INJ 165.4±19.1 ml/min; NINJ 160.0±13.9 ml/min, P=0.780) or insulin injections, even at the highest dose (INJ 153.7±17.4ml/min, P=0.155). Thus, blood flow changes are not implicated in effects of lipid or insulin.
Basal Glucose and Insulin
Confirming previous results (21;22), basal lymph glucose levels tended higher (+10%) than plasma glucose levels (Table 1), though this apparent difference was not significant. Other studies show interstitial glucose is lower than plasma (eg. (23)); it is possible that the sampling mechanism may be responsible for this difference. Lymph insulin was half that of arterial plasma (Table 1) as previously reported (21;22). When compared to results for experiments without lipid infusion, there were no differences between basal glucose or insulin levels.
Table 1.
Average insulin and glucose concentration at basal.
| |
Control |
Lipid |
||
|---|---|---|---|---|
| Insulin (mU/L) |
INJ |
NINJ |
INJ |
NINJ |
| Artery | 11.86±0.12 | 12.15±0.29 | 13.62±1.26 | 13.38±1.09 |
| Vein | 11.32±0.57 | 11.36±0.21 | 13.31±1.13 | 12.32±1.24 |
| Lymph |
6.04±0.6 |
5.53±0.18 |
6.33±0.57 |
7.72±0.72 |
| Glucose (mg/dL) |
|
|
||
| Artery | 93.66±1.87 | 93.3±1.52 | 103.04±3.51 | 100.27±3.83 |
| Vein | 94.18±1.87 | 93.11±1.83 | 101.06±3.34 | 102.25±5.49 |
| Lymph | 108.01±1.87 | 105.18±3.46 | 115.55±4.63 | 108.47±6.34 |
Arterial Insulin
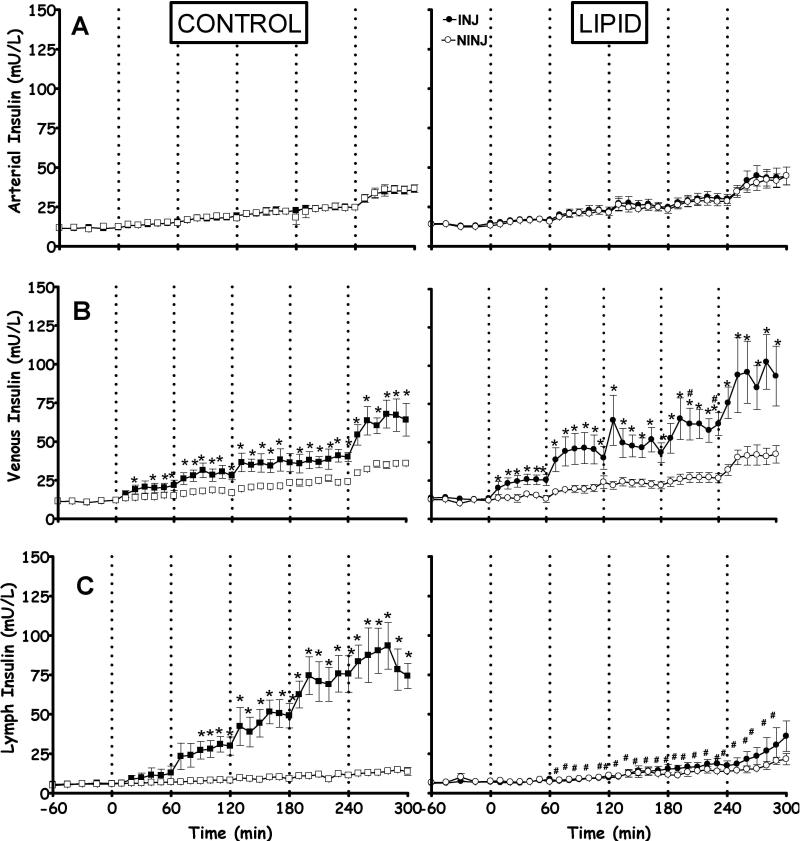
Basal arterial insulin was 14.1±1.4mU/L in both legs. There was a small rise in arterial insulin with the intramuscular injections; this was the same for both limbs (Fig. 3A). This increase was presumably due to a portion of the injected insulin exiting through the venous circulation and being redistributed through the systemic circulation. There was no significant difference in arterial insulin between INJ and NINJ or between lipid experiments and controls at any time point during the experiments.
Figure 3.
Femoral artery (A), femoral vein (B) and lymph (C) insulin concentration throughout experiment for control (left) and lipid (right) in INJ (black symbols) and NINJ (white symbols) legs after insulin injection (dotted lines). There was no significant difference in arterial insulin as determined by 2-way RM ANOVA, though there were significant differences between vein and lymph insulin concentrations. *, significantly different from corresponding NINJ leg at same time point with paired t-test; #, significantly different from control INJ leg, using unpaired t-test.
Venous insulin
Direct, stepwise injection of insulin only into one leg caused an increase in the INJ vein insulin, which was not observed in the contralateral NINJ (Fig. 3B). Subsequent insulin injections induced a further rise in venous insulin in the INJ leg, which was not observed in the NINJ leg. There was a significant difference between INJ vein insulin in control and lipid studies. The washout of insulin in the femoral vein accounted for 24.87±6.82% of the total injected insulin (compared to 17.15±5.19% in controls, no significance).
Lymph insulin
Controls showed a dose-dependent increase in interstitital concentrations following local insulin injection. In stark contrast, there was no significant difference between INJ and NINJ legs with lipid infusion, and control and lipid INJ legs were significantly different (Fig. 3C). There was a trend for increasing lymph insulin with time, likely due to the corresponding increase in arterial insulin supply (Fig. 3A). Hyperlipidemia prevented the appearance of locally injected insulin in the sampled interstitium. The washout of insulin in the lymph accounted for 0.02±0.02% of the total injected insulin (compared to 0.20±0.03% in controls, P<0.001). The total amount of injected insulin remaining in the muscle and unaccounted for in vein or lymph is 74.9±6.8% in lipid, and 81.9±4.9% in control (no significance).
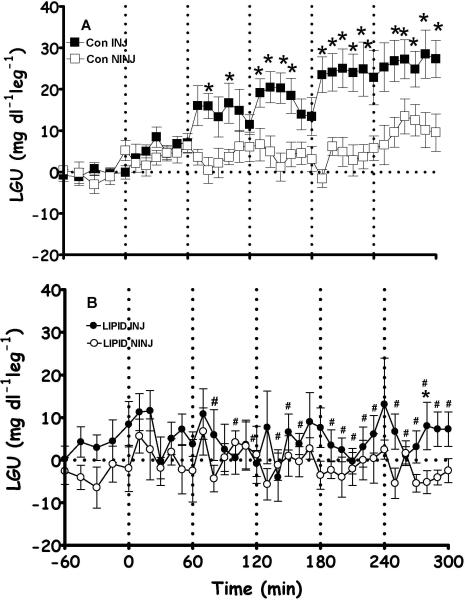
Insulin-mediated glucose uptake
Without lipid, insulin injection increased glucose uptake substantially in INJ, but not NINJ. In contrast, and consistent with failure of interstitial insulin to rise, glucose uptake in INJ, with hyperlipidemia, did not show any significant increment compared to the contralateral leg (NINJ) (Fig. 4). Glucose uptake was significantly higher in INJ controls than with lipid. Lipid prevented insulin-mediated glucose uptake (Fig. 4).
Figure 4.
Local glucose uptake calculated from arterio-venous difference across the INJ (black symbols) and NINJ (white symbols) leg for control (A) and lipid (B) dogs. The insulin injections (indicated by dotted lines) had no effect on local glucose uptake in INJ when compared to NINJ in the lipid experiments, though significantly increased in control experiments. *, significantly different from corresponding NINJ leg at same time point with paired t-test; #, significantly different from control INJ leg, using unpaired t-test.
DISCUSSION
In vivo, secreted insulin must traverse a series of hurdles before it can stimulate glucose uptake into skeletal muscle cells. After release from the pancreas, insulin is distributed through the blood to the capillaries, where it can cross the endothelial barrier to access the interstitial space. Once diffused throughout the interstitial space, it can bind to insulin receptors on skeletal muscle to cause GLUT4 translocation and glucose uptake. This final step of receptor binding and signaling has been well characterized (24), and other studies have observed the effect of delivery of insulin and glucose in the form of local changes in blood flow and distribution (9;11;19), but further characterization of the transport is limited. The novel technique in this study uses a direct intramuscular delivery of insulin, which does not require transport from the blood into the interstitial space, and lymph vessel cannulation allows an indication of the interstitial insulin concentrations.
In healthy animals, intramuscular insulin injections lead to dose-dependent rapid increases in interstitial insulin, which results in proportional dose-dependent rapid increases in local glucose uptake (21). In stark contrast, the present results show that hyperlipidemia due to systematic lipid infusion causes the insulin injected into muscle to divert into the venous circulation, preventing a significant local elevation of interstitial insulin. Also, there is no local glucose uptake during lipid infusion, which would be expected based on the lack of increased insulin in the interstitial space. The venous washout of insulin is on the average greater in the lipid study shown here than in control studies, though the difference is not significant (21). Inclusion of lipid prevents a significant rise in interstitial insulin after an intramuscular injection.
Our results show that lipid significantly lowers insulin sensitivity as measured by glucose infusion rate. While the rate of lipid infusion we use is comparable to that used in previous studies in adults (13;14;18;25;26), it is worth noting that there would be significant weight differences between dogs and adult men, although body weights were not reported in the human studies. However, other studies in rats have used 2.6-5ml.hr−1kg−1 (15-17), which is comparable to the rate of infusion we have used here (approximately 3ml.hr−1kg−1). It would be interesting to know the FFA levels in this study, but the anesthesia and heparin included in the lipid infusion would alter lipolysis, making comparisons to healthy controls difficult.
The mechanism by which fat causes insulin resistance is unclear, as reviewed in Krebs and Roden (6). Much of the effect of fat to cause insulin resistance appears to correlate well with intracellular accumulation of lipid (3;6;26), possibly leading to mitochondrial dysfunction and insulin resistance (27) although there can be exceptions (reviewed in (6)). Fat also alters vascular function and inhibits insulin-mediated capillary recruitment (28). Previous studies observed that palmitate can inhibit insulin-mediated glucose uptake at a cellular level, suggesting that lipid has a direct effect on the cell (29;30). What is most surprising and interesting in the present study is that we have shown that lipid prevents the rise in interstitial insulin, suggesting myocytes are not even exposed to increased insulin. This mechanism may be as important or even more important than lipid-induced downstream signaling impairment (16;17), intramyocellular fat accumulation (3;18) or mitochondrial dysfunction (27).
In vivo studies in healthy individuals have demonstrated insulin signaling and GLUT4 translocation occur within 10 minutes of insulin binding to its receptor (20), a finding supported by our studies (21). Typically, plasma insulin increases before lymph insulin and insulin receptor tyrosine kinase activation at the myocytes, yet there was a close temporal relationship between insulin receptor activation and glucose disposal (20). Therefore, the delay in insulin action in healthy individuals is due to some pre-receptor step: delivery by blood, transendothelial transport, or diffusion within the interstitial space. Our data support this, as glucose uptake is increased within 10 minutes of an interstitial injection (21).
Here, insulin is administered into the intramuscular space, producing a local high concentration compared to the basal levels in the plasma and surrounding interstitium, yet insulin never appears in the lymph. While there is no significant differences between the amounts of injected insulin remaining in the muscle in either study, lymph measures demonstrate that the myocytes in general are not exposed to insulin in lipid studies, whereas a larger proportion of the myocytes are able to react to insulin in controls. The location of the insulin before it appears in the venous blood is not known, but it may involve transport through the endothelial cells; in fact Wang et al (31), showed insulin is sequestered in the endothelial cells.
It is possible that lipid infusion somehow alters the ability of the lymph vessel to sample the interstitial space, whereby the insulin is in the interstitial space, but is not detected in lymph. However, basal lymph insulin is unaffected by lipid and even seems to respond to slight changes in arterial insulin consistent with control experiments (Fig. 3). This suggests that lymph reflects systemic insulin, although there is an apparent failure to reflect the acute local injection. Another method of measuring interstitial insulin concentrations may confirm or clarify these results; however microdialysis, a common method of sampling interstitial fluid, would necessitate that the injections are performed at a constant site in relation to the position of the microdialysis probe. This would be difficult to reproduce between injections and between animals, and would likely provide very inconsistent results. Preliminary studies injecting a higher concentration of insulin have shown that insulin can still appear in the lymph, and therefore can be elevated in the interstitial space even with lipid infusion.
Changes in the permeability of the endothelial wall may be responsible for insulin's movement into the blood, as previous studies have shown that permeability is increased in various insulin resistant states (32;33). However, in the fructose-fed hypertensive rat model, which begins to develop glucose intolerance and elevated plasma insulin, there is a decrease in permeability (34). These studies focus on the movement from plasma to the interstitial space, but an increased permeability may work both ways, causing the insulin to move from an area of high concentration (in this case, the interstitium) to low (plasma). This theory does not account for the location of insulin after injection and prior to appearance in the vein.
An alternative explanation for the present results is that insulin-mediated capillary recruitment is impaired with lipid, preventing the dispersion of insulin through the muscle to cause glucose uptake. It is interesting that in healthy situations, the injection of insulin into the intramuscular space is able to significantly increase the lymph insulin concentration (21), when the injected area is only a small section of the entire muscle sampled by lymph. It is perhaps more likely that the insulin is removed into the surrounding capillaries and redistributed to the local muscle, where the lymph can reflect it more efficiently, and more glucose uptake is induced. This would effectively increase the volume through which the insulin is distributed. As there is no delay in diffusion through the interstitium (21), capillary recruitment would rapidly facilitate the dispersal of the insulin injection to a larger area (19). Lipid reduces capillary recruitment (27), and the insulin injected into the muscle is restricted to the area of injection, without further dissemination through the muscle. This would cause a local high concentration of insulin, which may not be directly sampled by lymph. Whether or not glucose uptake is occurring in this area is difficult to determine, as insulin may cause local glucose uptake, but at too small an amount to detect across the leg. A method to measure capillary recruitment in this dynamic state is currently being developed. Also, vasoactive agents that increase basal capillary recruitment with lipid will determine whether the injected insulin is then able to disperse further into the muscle, and be detected in lymph.
In conclusion, we show that when insulin resistance is induced by lipid infusion, insulin injected into the muscle appears in the vein, but not lymph. This differs from control studies without lipid infusion, where there was a significant elevation of insulin in the lymph (21). Here, insulin resistance occurs because the myocytes are not exposed to insulin; care must be taken to ensure that results suggesting resistance is due to downstream signaling impairment, intramyocellular fat accumulation or mitochondrial dysfunction are not in fact due to insulin's inability to access the tissue(27). This may have implications on the use of intramuscular injections of insulin as obese diabetic patients that have high circulating lipid concentrations will respond differently to lean individuals. The reason for this change is unknown, although future experiments will aim to determine the mechanism of the change induced by lipid and more physiological plasma lipid concentrations may help to understand this result.
ACKNOWLEDGMMENTS
These authors contributed equally to this work. This study was supported by grants from the National Institutes of Health (NIH DK029867 and DK27619). CMK was supported by a Mentor-Based Post-doctoral Fellowship from the American Diabetes Association. Special thanks to Rita Thomas for technical assistance.
Footnotes
DISCLOSURES
The authors have no conflict of interest to declare relevant to these studies.
Reference List
- 1.Bergman RN. Orchestration of glucose homeostasis: from a small acorn to the california oak. Diabetes. 2007;56:1489–1501. doi: 10.2337/db07-9903. [DOI] [PubMed] [Google Scholar]
- 2.Kahn R. Metabolic syndrome: is it a syndrome? Does it matter? Circulation. 2007;115:1806–1810. doi: 10.1161/CIRCULATIONAHA.106.658336. [DOI] [PubMed] [Google Scholar]
- 3.Virkamaki A, Korsheninnikova E, Seppala-Lindroos A, et al. Intramyocellular lipid is associated with resistance to in vivo insulin actions on glucose uptake, antilipolysis, and early insulin signaling pathways in human skeletal muscle. Diabetes. 2001;50:2337–2343. doi: 10.2337/diabetes.50.10.2337. [DOI] [PubMed] [Google Scholar]
- 4.Tanner JW, Leingang KA, Mueckler MM, Glenn KC. Cellular mechanism of the insulin-like effect of growth hormone in adipocytes. Rapid translocation of the HepG2-type and adipocyte/muscle glucose transporters. Biochem J. 1992;282:99–106. doi: 10.1042/bj2820099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bjornholm M, Zierath JR. Insulin signal transduction in human skeletal muscle: identifying the defects in Type II diabetes. Biochem Soc Trans. 2005;33:354–357. doi: 10.1042/BST0330354. [DOI] [PubMed] [Google Scholar]
- 6.Krebs M, Roden M. Molecular mechanisms of lipid-induced insulin resistance in muscle, liver and vasculature. Diabetes Obes Metab. 2005;7:621–632. doi: 10.1111/j.1463-1326.2004.00439.x. [DOI] [PubMed] [Google Scholar]
- 7.Marchand-Brustel Y, Gual P, Gremeaux T, Gonzalez T, Barres R, Tanti JF. Fatty acid-induced insulin resistance: role of insulin receptor substrate 1 serine phosphorylation in the retroregulation of insulin signalling. Biochem Soc Trans. 2003;31:1152–1156. doi: 10.1042/bst0311152. [DOI] [PubMed] [Google Scholar]
- 8.Morino K, Petersen KF, Shulman GI. Molecular mechanisms of insulin resistance in humans and their potential links with mitochondrial dysfunction. Diabetes. 2006;55:S9–S15. doi: 10.2337/db06-S002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baron AD, Clark MG. Role of blood flow in the regulation of muscle glucose uptake. Annu Rev Nutr. 1997;17:487–99. doi: 10.1146/annurev.nutr.17.1.487. 487-499. [DOI] [PubMed] [Google Scholar]
- 10.Ellmerer M, Hamilton-Wessler M, Kim SP, et al. Reduced access to insulin-sensitive tissues in dogs with obesity secondary to increased fat intake. Diabetes. 2006;55:1769–1775. doi: 10.2337/db05-1509. [DOI] [PubMed] [Google Scholar]
- 11.Clark MG, Wallis MG, Barrett EJ, et al. Blood flow and muscle metabolism: a focus on insulin action. Am J Physiol Endocrinol Metab. 2003;284:E241–E258. doi: 10.1152/ajpendo.00408.2002. [DOI] [PubMed] [Google Scholar]
- 12.Gudbjornsdottir S, Sjostrand M, Strindberg L, Lonnroth P. Decreased muscle capillary permeability surface area in type 2 diabetic subjects. J Clin Endocrinol Metab. 2005;90:1078–1082. doi: 10.1210/jc.2004-0947. [DOI] [PubMed] [Google Scholar]
- 13.Belfort R, Mandarino L, Kashyap S, et al. Dose-response effect of elevated plasma free fatty acid on insulin signaling. Diabetes. 2005;54:1640–1648. doi: 10.2337/diabetes.54.6.1640. [DOI] [PubMed] [Google Scholar]
- 14.Roden M, Krssak M, Stingl H, et al. Rapid impairment of skeletal muscle glucose transport/phosphorylation by free fatty acids in humans. Diabetes. 1999;48:358–364. doi: 10.2337/diabetes.48.2.358. [DOI] [PubMed] [Google Scholar]
- 15.Jucker BM, Rennings AJ, Cline GW, Shulman GI. 13C and 31P NMR studies on the effects of increased plasma free fatty acids on intramuscular glucose metabolism in the awake rat. J Biol Chem. 1997;272:10464–10473. doi: 10.1074/jbc.272.16.10464. [DOI] [PubMed] [Google Scholar]
- 16.Yu C, Chen Y, Cline GW, et al. Mechanism by which fatty acids inhibit insulin activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3-kinase activity in muscle. J Biol Chem. 2002;277:50230–50236. doi: 10.1074/jbc.M200958200. [DOI] [PubMed] [Google Scholar]
- 17.Kim YI, Lee FN, Choi WS, Lee S, Youn JH. Insulin regulation of skeletal muscle PDK4 mRNA expression is impaired in acute insulin-resistant states. Diabetes. 2006;55:2311–2317. doi: 10.2337/db05-1606. [DOI] [PubMed] [Google Scholar]
- 18.Brechtel K, Dahl DB, Machann J, et al. Fast elevation of the intramyocellular lipid content in the presence of circulating free fatty acids and hyperinsulinemia: a dynamic 1H-MRS study. Magn Reson Med. 2001;45:179–183. doi: 10.1002/1522-2594(200102)45:2<179::aid-mrm1023>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 19.Vincent MA, Clerk LH, Lindner JR, et al. Microvascular recruitment is an early insulin effect that regulates skeletal muscle glucose uptake in vivo. Diabetes. 2004;53:1418–1423. doi: 10.2337/diabetes.53.6.1418. [DOI] [PubMed] [Google Scholar]
- 20.Miles PD, Levisetti M, Reichart D, Khoursheed M, Moossa AR, Olefsky JM. Kinetics of insulin action in vivo. Identification of rate-limiting steps. Diabetes. 1995;44:947–953. doi: 10.2337/diab.44.8.947. [DOI] [PubMed] [Google Scholar]
- 21.Chiu JD, Richey JM, Harrison LN, et al. Direct administration of insulin into skeletal muscle reveals that the transport of insulin across the capillary endothelium limits the time course of insulin to activate glucose disposal. Diabetes. 2008;57:828–835. doi: 10.2337/db07-1444. [DOI] [PubMed] [Google Scholar]
- 22.Yang YJ, Hope I, Ader M, Poulin RA, Bergman RN. Dose-response relationship between lymph insulin and glucose uptake reveals enhanced insulin sensitivity of peripheral tissues. Diabetes. 1992;41:241–253. doi: 10.2337/diabetes.41.2.241. [DOI] [PubMed] [Google Scholar]
- 23.Sjostrand M, Holmang A, Strindberg L, Lonnroth P. Estimations of muscle interstitial insulin, glucose, and lactate in type 2 diabetic subjects. Am J Physiol Endocrinol Metab. 2000;279:E1097–E1103. doi: 10.1152/ajpendo.2000.279.5.E1097. [DOI] [PubMed] [Google Scholar]
- 24.Nystrom FH, Quon MJ. Insulin signalling: metabolic pathways and mechanisms for specificity. Cell Signal. 1999;11:563–574. doi: 10.1016/s0898-6568(99)00025-x. [DOI] [PubMed] [Google Scholar]
- 25.Roden M, Stingl H, Chandramouli V, et al. Effects of free fatty acid elevation on postabsorptive endogenous glucose production and gluconeogenesis in humans. Diabetes. 2000;49:701–707. doi: 10.2337/diabetes.49.5.701. [DOI] [PubMed] [Google Scholar]
- 26.Bachmann OP, Dahl DB, Brechtel K, et al. Effects of intravenous and dietary lipid challenge on intramyocellular lipid content and the relation with insulin sensitivity in humans. Diabetes. 2001;50:2579–2584. doi: 10.2337/diabetes.50.11.2579. [DOI] [PubMed] [Google Scholar]
- 27.Petersen KF, Befroy D, Dufour S, et al. Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science. 2003;300:1140–1142. doi: 10.1126/science.1082889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clerk LH, Rattigan S, Clark MG. Lipid infusion impairs physiologic insulin-mediated capillary recruitment and muscle glucose uptake in vivo. Diabetes. 2002;51:1138–1145. doi: 10.2337/diabetes.51.4.1138. [DOI] [PubMed] [Google Scholar]
- 29.Storz P, Doppler H, Wernig A, Pfizenmaier K, Muller G. Cross-talk mechanisms in the development of insulin resistance of skeletal muscle cells palmitate rather than tumour necrosis factor inhibits insulin-dependent protein kinase B (PKB)/Akt stimulation and glucose uptake. Eur J Biochem. 1999;266:17–25. doi: 10.1046/j.1432-1327.1999.00809.x. [DOI] [PubMed] [Google Scholar]
- 30.Schmitz-Peiffer C, Craig DL, Biden TJ. Ceramide generation is sufficient to account for the inhibition of the insulin-stimulated PKB pathway in C2C12 skeletal muscle cells pretreated with palmitate. J Biol Chem. 1999;274:20, 24202–24210. doi: 10.1074/jbc.274.34.24202. [DOI] [PubMed] [Google Scholar]
- 31.Wang H, Liu Z, Li G, Barrett EJ. The vascular endothelial cell mediates insulin transport into skeletal muscle. Am J Physiol Endocrinol Metab. 2006;291:E323–E332. doi: 10.1152/ajpendo.00047.2006. [DOI] [PubMed] [Google Scholar]
- 32.St Pierre P, Bouffard L, Papirakis ME, Maheux P. Increased extravasation of macromolecules in skeletal muscles of the Zucker rat model. Obesity (Silver Spring) 2006;14:787–793. doi: 10.1038/oby.2006.91. [DOI] [PubMed] [Google Scholar]
- 33.Dell'Omo G, Penno G, Pucci L, Mariani M, Del Prato S, Pedrinelli R. Abnormal capillary permeability and endothelial dysfunction in hypertension with comorbid Metabolic Syndrome. Atherosclerosis. 2004;172:383–389. doi: 10.1016/j.atherosclerosis.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 34.Chakir M, Plante GE, Maheux P. Reduction of capillary permeability in the fructose-induced hypertensive rat. Am J Hypertens. 1998;11:563–569. doi: 10.1016/s0895-7061(97)00411-1. [DOI] [PubMed] [Google Scholar]