Abstract
Background: The American Heart Association (AHA), Institute of Medicine (IOM), and US Departments of Health and Human Services and Agriculture (USDA) Dietary Guidelines for Americans all recommend that Americans limit sodium intake and choose foods that contain potassium to decrease the risk of hypertension and other adverse health outcomes.
Objective: We estimated the distributions of usual daily sodium and potassium intakes by sociodemographic and health characteristics relative to current recommendations.
Design: We used 24-h dietary recalls and other data from 12,581 adults aged ≥20 y who participated in NHANES in 2003–2008. Estimates of sodium and potassium intakes were adjusted for within-individual day-to-day variation by using measurement error models. SEs and 95% CIs were assessed by using jackknife replicate weights.
Results: Overall, 99.4% (95% CI: 99.3%, 99.5%) of US adults consumed more sodium daily than recommended by the AHA (<1500 mg), and 90.7% (89.6%, 91.8%) consumed more than the IOM Tolerable Upper Intake Level (2300 mg). In US adults who are recommended by the Dietary Guidelines to further reduce sodium intake to 1500 mg/d (ie, African Americans aged ≥51 y or persons with hypertension, diabetes, or chronic kidney disease), 98.8% (98.4%, 99.2%) overall consumed >1500 mg/d, and 60.4% consumed >3000 mg/d—more than double the recommendation. Overall, <2% of US adults and ∼5% of US men consumed ≥4700 mg K/d (ie, met recommendations for potassium).
Conclusion: Regardless of recommendations or sociodemographic or health characteristics, the vast majority of US adults consume too much sodium and too little potassium.
INTRODUCTION
Hypertension is a well-established and a leading risk factor for cardiovascular disease that has been estimated to account for at least half of stroke and nearly half of ischemic heart disease worldwide (1–3). Evidence from randomized controlled trials indicates a direct dose-response relation between sodium intake and blood pressure, with the greatest response occurring at sodium intakes <2300 mg (4, 5). In addition, potassium intake increases urinary excretion of sodium through action on the renal tubule (4, 6). Evidence indicates that a potassium intake of ≥4700 mg/d in adults optimally decreases the blood pressure response to sodium intake (4, 7). The American Heart Association (AHA)5, the Institute of Medicine (IOM), and the US Department of Health and Human Services/USDA all recommend limiting sodium intake and increasing intake of foods containing potassium to reduce the risk of hypertension and cardiovascular disease (4, 8, 9). The AHA's Strategic Impact Goals include a recommendation for sodium intake of <1500 mg/d (Table 1) (9). According to the US Department of Health and Human Services/USDA Dietary Guidelines, all Americans should reduce usual daily sodium intake to <2300 mg and specific subgroups should further reduce intake to 1500 mg, including persons aged ≥51 y or persons aged ≥2 y who are African American or have hypertension, diabetes, or chronic kidney disease (8). According to the IOM Dietary Reference Intakes, usual intake >2300 mg, the Tolerable Upper Intake Level (UL), may place an individual at risk of hypertension (4).
TABLE 1.
Current recommendations to limit sodium intake among healthy US adults aged 20 y and older1
| Organization | Recommendation | Year | Population | Usual sodium intake |
| American Heart Association | Strategic Impact Goal Through 2020 and Beyond (9) | 2010 | Based on a 2000-kcal diet and “should be scaled accordingly for other levels of intake” | <1500 mg/d |
| US Departments of Health and Human Services and Agriculture | Dietary Guidelines for Americans (8) | 2010 | Age 20–50 y; non–African Americans without hypertension, diabetes, or chronic kidney disease Age 20–50 y; African Americans or persons with hypertension, diabetes, or chronic kidney disease Age ≥51 y | <2300 mg/d1500 mg/d1500 mg/d |
| Institute of Medicine | Dietary Reference Intake: UL (4) | 2005 | Age ≥20 y2 | 2300 mg/d |
Recommendations in this table are truncated at age 20 y to correspond with the population of interest in this study.
Older adults, African Americans, and people with hypertension, diabetes, or chronic kidney disease “should benefit from a level of sodium intake below the UL [Tolerable Upper Intake Level] of 2.3 g (100 mmol)/d,” but this level is not defined (4). The UL is “not a recommended intake … as with other ULs there is no benefit to consuming levels above the AI [adequate intake].” The AI is 1500 mg/d for adults aged 20–50 y, 1300 mg/d for adults aged 51–70 y, and 1200 mg/d for adults aged ≥71 y.
In addition, the IOM and US Department of Health and Human Services/USDA recommend that Americans increase consumption of potassium-containing foods to achieve an intake of ≥4700 mg/d based on the IOM's Adequate Intake, the amount of potassium adequate for almost everyone within the population (4, 8). In 2007–2008, mean daily sodium intake (excluding table salt) among US adults aged ≥20 y was in excess of guidelines, ∼3400 mg (10). In contrast, the mean potassium intake was below guidelines, ∼2600 mg (10).
Accurate estimates of the distribution of sodium and potassium intakes and also the prevalence of meeting or exceeding guidelines are essential for monitoring the effectiveness of current actions to reduce sodium in processed and restaurant foods and efforts to increase consumption of potassium-containing fruit and vegetables, lean meats, and milk. Limited data exist on usual daily sodium and potassium intakes among US adults (4, 8, 11–14). Information from one 24-h dietary recall can be used to estimate mean population intake but does not account for day-to-day variation in food consumed by individuals and can overestimate or underestimate the population prevalence above and below specific thresholds (15–18). In addition, large sample sizes from multiple survey years are required to achieve statistically reliable prevalence estimates among specific population subgroups. Subsequently, our objective is to provide baseline estimates of the distributions of usual sodium and potassium intakes by sociodemographic and health characteristics relative to current recommendations from the AHA, IOM, and US government (4, 8, 9). A secondary objective was to compare our estimates with previous estimates among US adults (4) to determine whether usual sodium or potassium intakes changed since 1988–1994.
SUBJECTS AND METHODS
NHANES is a large, multistage, complex survey of the noninstitutionalized US population conducted by the National Center for Health Statistics (NCHS), CDC. Detailed descriptions of the survey design and data collection procedures are available elsewhere (19–21). Briefly, the population was sampled with a complex, stratified, multistage probability cluster sampling design to provide data that are representative of the overall noninstitutionalized US population. Selected participants consent to a household interview followed by an examination in the NHANES Mobile Examination Center. Data are released in 2-y cycles that include ∼10,000 participants from sampled counties across the country. NHANES was reviewed and approved by the NCHS ethics review board. Participants provided written informed consent before participation.
We combined 6 y (3 cycles) in our analysis, 2003–2004, 2005–2006, and 2007–2008. During these 3 cycles, examination participation rates among adults aged ≥20 y were 68.6%, 71.0%, and 70.6%, respectively (22). Certain population subgroups were oversampled in each phase to allow reliable estimates within the subgroups. For NHANES 2003–2008, subgroups oversampled included, but were not limited to, persons aged ≥60 y, Mexican Americans, and non-Hispanic black Americans. Of the 14,387 participants aged ≥20 y who participated in the examination and provided at least one reliable 24-h dietary recall, we sequentially excluded pregnant women (n = 579) and participants who were missing data on blood pressure or medication use for hypertension (n = 413), chronic kidney disease (n = 667), self-reported diabetes (n = 10), education (n = 8), or BMI (n = 129). The final sample included 12,581 adults. Compared with nonpregnant adult participants excluded from the sample because of missing information (n = 1227), a larger proportion of participants included in the sample were non-Hispanic white (73% compared with 63%; P < 0.001), and a smaller proportion was non-Hispanic black (11% compared with 18%; P < 0.001). In addition, the included participants were slightly older (mean: 47 compared with 46 y; P = 0.04) but did not differ in the distribution of sex.
Sodium and potassium intakes
Data on sodium and potassium intakes from the diet were assessed by using 24-h dietary recalls. The first recall was administered in person, followed by a telephone recall administered 3–10 d later. Nutrient values, including sodium and potassium, were assigned to foods by using the USDA Food and Nutrient Database for Dietary Studies corresponding to each 2-y phase (23). Dietary sodium and potassium intakes for each day of intake for each individual were estimated by summing the sodium and potassium consumed from each food or beverage reported for that day. Beginning in 2005, consumption of tap and bottled water was collected during the 24-h recall and included in estimates of individual sodium intake. In 2003–2004, tap and plain bottled water intake information was collected after the 24-h dietary recall and not included in estimates of individual sodium intake. The mineral content of water consumed was quantified by using the nutrient profile for those items in the Food and Nutrient Database for Dietary Studies 2.0 (24). We then added the sodium content of water to individual sodium intake from other sources. The sodium content of designated foods likely to be prepared at home and reported to be obtained from the store in What We Eat in America are adjusted downward according to the typical amount of salt added during home preparation for those who reported salt use during cooking as “never,” “rarely,” or “occasionally” (23). Sodium intake does not include salt added at the table (23). We chose to focus on sodium intake from food and beverages, excluding salt added at the table, because foods and beverages are the primary source of sodium intake (25). To examine whether adults exceeded the AHA and IOM UL recommendations to limit sodium intake, we examined the proportion with usual intakes ≥1500 or 2300 mg/d, respectively.
Covariates
Age, sex, race-ethnicity, education, and income were self-reported. Race or ethnicity was categorized as non-Hispanic white, non-Hispanic black, or Mexican American. BMI was calculated as kilograms of measured weight divided by meters of measured height squared. We categorized BMI according to guidelines from the National Heart, Lung and Blood Institute (26). Poverty index ratios are defined as household income relative to national poverty thresholds for a household of similar size, composition, and location. We categorized the poverty index ratio as ≤130% or >130% because this threshold is often used for qualification for federal assistance programs. Mean blood pressure was estimated from up to 3 readings, obtained under standard conditions during a single physical examination at the Mobile Examination Center. Hypertension was defined as mean systolic blood pressure ≥140 mm Hg, mean diastolic blood pressure ≥90 mm Hg, or self-reported use of antihypertensive medication as in previous studies (27, 28). Among individuals without hypertension, prehypertension was defined as a mean systolic blood pressure of 120 to 139 mm Hg or a mean diastolic pressure of 80 to 89 mm Hg (28). Normal blood pressure was defined as a mean systolic blood pressure <120 mm Hg and a mean diastolic blood pressure <80 mm Hg.
Chronic kidney disease was defined as an estimated glomerular filtration rate <60 mL · min−1 · 1.73 m−2 estimated from calibration equations by using the serum creatinine concentration and other factors or the urinary albumin/creatinine ratio >30 mg/g (29, 30). A partial urine specimen (spot) was collected during the examination. Urinary albumin was measured by using a solid-phase fluorescent immunoassay. Urinary and serum creatinine concentrations were analyzed by using a colorimetric assay (Jaffe rate method). The 2005–2006 serum creatinine values were adjusted by using the formula −0.016 + 0.978 × (NHANES 2005–2006 uncalibrated serum creatinine, mg/dL), developed by the NCHS to ensure the comparability with standard creatinine. We defined diagnosed diabetes by an affirmative response to the question, “Other than during pregnancy, have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?”
Statistical analyses
We used the Software for Intake Distribution Estimation for the Windows Operating System (PC-SIDE, version 1.0; Iowa State University) to estimate the usual intake of sodium and potassium, which accounted for between- and within-person variations in intake (31, 32). We estimated the distributions (medians, percentiles, and proportion who consumed ≥1500 or ≥2300 mg Na/d or ≥4700 mg K/d), overall and by subgroup, day of the week of the recall, and age, sex, and race-ethnicity group. All participants in the sample had an initial 24-dietary recall, and 89.6% had a second recall. We also used PC-SIDE to output 1000 representative usual intakes by population subgroups to graph the distribution of intakes. We used R statistical software to plot the estimated probability functions (in mg Na) of usual intakes from the 1000 representative intakes (33). We used combined 6-y first-day dietary sampling weights to account for differential nonresponse and noncoverage and to adjust for oversampling. We estimated SEs and 95% CIs for usual intakes from PC-SIDE by using a set of 92 jackknife repeated-replication weights based on the 6-y combined sampling weights. When 95% CIs did not overlap, differences between independent population subgroups in percentiles of usual nutrient intakes were considered statistically significant. To test differences between participants included and excluded from our sample, we used chi-square tests and t tests in Survey Data Analysis Software (Research Triangle Institute, version 10.0).
Additional analyses
To examine whether usual intake of US adults exceeded the amounts in the 2010 Dietary Guidelines for sodium, we classified adults recommended to reduce sodium consumption to 1500 mg Na/d as adults with one more of the following characteristics: age ≥51 y, non-Hispanic black, hypertension, diabetes (diagnosed or undiagnosed), or chronic kidney disease (8). All other adults were included in the group recommended to consume <2300 mg Na/d. For these subanalyses, we used the same original exclusion criteria but restricted our analyses to the fasting subsample (n = 5564) and defined undiagnosed diabetes as glycated hemoglobin ≥6.5% or fasting plasma glucose ≥126 mg/dL (34). Plasma glucose was analyzed by using a hexokinase enzymatic method and glycated hemoglobin by using HPLC. Along with restricting the previous analytic sample to the fasting subsample, we further sequentially excluded adults with missing information on undiagnosed diabetes (n = 16) or who reported they were receiving dialysis (n = 13) for a sample size of 5535. For this analysis we used PC-SIDE, as described previously, but estimated SEs with a separate set of 92 jackknife repeated-replication weights based on 6-y combined sampling weights for the fasting subsample in 2003–2008.
Finally, to assess whether usual sodium and potassium intakes changed over time, we stratified our original sample into age and sex subgroups and used exclusion criteria and adjustments to duplicate the previous analyses of US adults in 1988–1994 (4). In 1988–1994, ∼5% of adults had a second 24-h dietary recall, which was used to adjust for measurement error variance of usual sodium and potassium intakes (35). As in NHANES 2003–2008, the estimates of sodium from foods and beverages in NHANES 1988–1994 do not include salt added at the table. Similar to NHANES 2003–2008, adjustments were made for salt used in home preparation of foods; however, rather than a single question asked at the end of the survey used to adjust all designated foods, participants were asked about preparation for each of the designated foods (eg, cooking rice in salted or unsalted water), and the salt content was adjusted accordingly (36). To be comparable with 1988–1994 analyses, we limited our data to individuals who provided a complete, reliable, initial dietary recall and excluded women who were pregnant or lactating or missing information on pregnancy and lactating status. After the exclusions, there were 14,208 participants for analyses in 2003–2008. For 2003–2008, data were adjusted for interview method (first or second 24-h dietary recall) and the day of the week but no other characteristics. We estimated SEs and 95% CIs for usual intakes in 2003–2008 by using a set of 92 jackknife repeated-replication weights based on the 6-y combined first-day dietary sampling weights. To compare intakes in 2003–2008 with intakes with those previously published in 1988–1994, we also estimated mean intakes. To test differences in mean usual intakes between usual sodium and potassium intakes over time, we used z tests based on the means and SEs for NHANES 1988–1994 and 2003–2008.
RESULTS
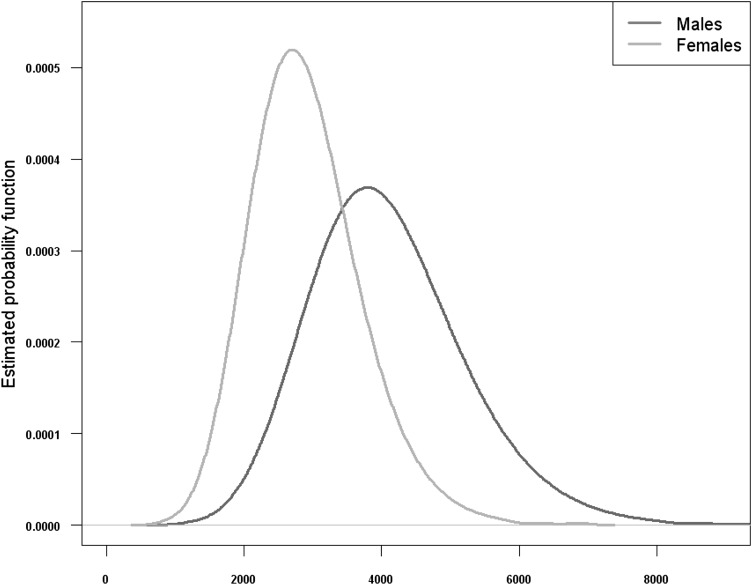
Median usual daily sodium intake excluding table salt was 3371 mg (IQR: 2794, 4029) among US adults aged ≥20 y in 2003–2008 (Table 2). A total of 99.4% and 90.7% of US adults consumed ≥1500 or ≥2300 mg, respectively. Usual sodium intake varied by sociodemographic characteristics. In comparison with adults aged 20–30 y, usual sodium intake did not differ among adults aged 31–50 y but was significantly lower among adults aged ≥51 y (Table 2). Across the sociodemographic and health characteristics examined, adults aged ≥71 y consumed the least amount of sodium: median sodium intake was 2592 mg/d, 97.5% consumed ≥1500 mg/d, and 67.7% consumed ≥2300 mg/d. Compared with men, women consumed significantly less sodium (Table 2, Figure 1). On average, women consumed ∼1000–1400 mg less sodium than did men across the distribution (Table 2). In comparison with non-Hispanic white adults, usual intakes were somewhat lower among non-Hispanic black adults across the distribution. Usual sodium intakes among Mexican-American adults were in between those of non-Hispanic black and white adults. Usual sodium intake was greater with higher income and education.
TABLE 2.
Distribution of usual daily sodium intake among US adults aged ≥20 y: NHANES 2003–20081
| Usual sodium intake |
||||||
| Category | No. of subjects | 25th Percentile | Median | 75th Percentile | Subjects consuming ≥1500 mg/d | Subjects consuming≥2300 mg/d |
| mg/d | mg/d | mg/d | % | % | ||
| All | 12,581 | 2794 (2744, 2844) | 3371 (3318, 3424) | 4029 (3967, 4091) | 99.4 (99.3, 99.5) | 90.7 (89.6, 91.8) |
| Age | ||||||
| 20–30 y | 2161 | 3079 (2959, 3199) | 3697 (3567, 3827) | 4394 (4249, 4539) | 99.8 (99.7, 99.9) | 95.0 (93.4, 96.5) |
| 31–50 y | 4240 | 3002 (2932, 3072) | 3625 (3548, 3702) | 4341 (4245, 4437) | 99.7 (99.5, 99.8) | 93.8 (92.7, 95.0) |
| 51–70 y | 3915 | 2611 (2547, 2675) | 3153 (3079, 3227) | 3775 (3685, 3865) | 99.2 (99.0, 99.4) | 86.6 (84.8, 88.5) |
| ≥71 y | 2265 | 2171 (2115, 2227) | 2592 (2522, 2662) | 3076 (2985, 3167) | 97.5 (96.9, 98.0) | 67.7 (64.1, 71.2) |
| Sex | ||||||
| Male | 6379 | 3326 (3267, 3385) | 4008 (3941, 4075) | 4787 (4703, 4871) | 99.9 (99.8, 99.9) | 96.9 (96.4, 97.4) |
| Female | 6202 | 2357 (2316, 2398) | 2836 (2790, 2882) | 3382 (3324, 3440) | 98.2 (97.9, 98.6) | 77.6 (75.8, 79.5) |
| Race-ethnicity2 | ||||||
| Non-Hispanic white | 6435 | 2864 (2802, 2926) | 3423 (3360, 3487) | 4059 (3987, 4131) | 99.7 (99.6, 99.8) | 92.5 (91.4, 93.7) |
| Non-Hispanic black | 2551 | 2587 (2494, 2680) | 3161 (3053, 3269) | 3820 (3688, 3952) | 98.7 (98.2, 99.3) | 85.2 (82.5, 88.0) |
| Mexican American | 2357 | 2632 (2527, 2737) | 3251 (3131, 3371) | 3954 (3808, 4100) | 98.6 (98.1, 99.1) | 85.9 (83.1, 88.7) |
| Household income3 | ||||||
| ≤130% Federal poverty index | 3317 | 2507 (2420, 2594) | 3115 (3014, 3216) | 3831 (3708, 3954) | 98.0 (97.5, 98.6) | 82.4 (79.7, 85.1) |
| >130% Federal poverty index | 8497 | 2893 (2845, 2941) | 3447 (3391, 3503) | 4076 (4006, 4146) | 99.7 (99.6, 99.8) | 93.2 (92.3, 94.0) |
| Education | ||||||
| <12 y | 3620 | 2452 (2372, 2532) | 3040 (2945, 3135) | 3723 (3602, 3844) | 97.8 (97.2, 98.4) | 80.7 (77.9, 83.4) |
| 12 y or GED | 3108 | 2783 (2716, 2850) | 3351 (3273, 3429) | 3996 (3898, 4094) | 99.5 (99.3, 99.6) | 90.7 (89.2, 92.1) |
| >12 y | 5853 | 2939 (2878, 3000) | 3489 (3424, 3554) | 4116 (4050, 4182) | 99.8 (99.7, 99.8) | 94.1 (93.3, 95.0) |
| BMI | ||||||
| <18.5 kg/m2 | 189 | 2446 (2130, 2762) | 3065 (2759, 3371) | 3763 (3336, 4190) | —4 | 80.1 (69.2, 90.9) |
| 18.5–24.9 kg/m2 | 3547 | 2784 (2708, 2860) | 3361 (3280, 3442) | 4033 (3937, 4129) | 99.4 (99.3, 99.6) | 90.6 (88.8, 92.4) |
| 25.0–29.9 kg/m2 | 4405 | 2788 (2725, 2852) | 3315 (3245, 3385) | 3910 (3830, 3990) | 99.6 (99.4, 99.7) | 91.4 (90.0, 92.8) |
| ≥30.0 kg/m2 | 4440 | 2847 (2769, 2925) | 3453 (3369, 3537) | 4138 (4038, 4238) | 99.4 (99.2, 99.5) | 91.3 (89.7, 92.8) |
| Hypertension status5 | ||||||
| Hypertension | 4867 | 2583 (2504, 2662) | 3121 (3028, 3214) | 3740 (3627, 3853) | 99.1 (98.8, 99.4) | 85.7 (83.3, 88.1) |
| Prehypertension | 3228 | 2991 (2907, 3075) | 3596 (3493, 3699) | 4286 (4169, 4403) | 99.7 (99.5, 99.8) | 93.9 (92.3, 95.4) |
| No hypertension | 4486 | 2857 (2774, 2940) | 3430 (3347, 3513) | 4082 (3987, 4177) | 99.6 (99.5, 99.7) | 92.1 (90.7, 93.6) |
| Diabetes diagnosis6 | ||||||
| Yes | 1471 | 2537 (2455, 2619) | 3071 (2977, 3165) | 3681 (3562, 3800) | 98.9 (98.4, 99.3) | 84.2 (81.4, 87.0) |
| No | 11,110 | 2821 (2771, 2871) | 3399 (3345, 3453) | 4058 (3995, 4121) | 99.5 (99.4, 99.6) | 91.3 (90.2, 92.4) |
| Chronic kidney disease7 | ||||||
| Yes | 2546 | 2397 (2323, 2471) | 2891 (2809, 2973) | 3471 (3375, 3567) | 98.5 (98.0, 98.9) | 79.4 (76.2, 82.5) |
| No | 10,035 | 2870 (2819, 2921) | 3457 (3401, 3513) | 4127 (4062, 4192) | 99.6 (99.4, 99.7) | 92.1 (91.1, 93.1) |
Medians, IQRs, and proportions ≥1500 and ≥2300 mg/d and 95% CIs for all measures (in parentheses) were estimated from Software for Intake Distribution Estimation for the Windows Operating System (Department of Statistics, Iowa State University) with jackknife replicate weights and were adjusted for interview method (in person or by phone), day of the week, age (continuous), sex, and race-ethnicity as possible. Sample sizes are unweighted. Pregnant women and individuals missing data on sodium intakes and covariates were excluded. GED, general equivalency diploma.
Categories do not add up to total because “other race-ethnicity” was not included.
Family income was defined as total household income divided by the poverty threshold for the year of the interview multiplied by 100.
Does not meet standard of statistical reliability, relative SE >40%.
Hypertension was defined as a mean systolic blood pressure ≥140 mm Hg, a mean diastolic blood pressure ≥90 mm Hg, or self-reported use of antihypertensive medication (25, 26). Prehypertension was defined as a mean systolic blood pressure 120–139 mm Hg or a mean diastolic blood pressure 80–89 mm Hg (26). Normal blood pressure was defined as a mean systolic blood pressure <120 mm Hg and a mean diastolic blood pressure <80 mm Hg. Mean blood pressure was estimated from up to 3 readings on a single occasion.
Diabetes was defined by self-reported diagnosis by a health care provider.
FIGURE 1.
Estimated usual intake of sodium (in mg/d) among US adults aged ≥20 y by sex, NHANES 2003–2008, n = 12,581. R statistical software was used to plot the estimated probability function (in mg Na) of usual intakes from the 1000 representative intakes. The figure represents the probability of an individual's usual sodium intake falling within a particular region given by the integral of individual usual sodium intake density over the region. The integral over the entire space is equal to one.
Usual sodium intake varied little by BMI, except among the small group of adults with BMI <18.5. Although CIs were wide, among this group median usual sodium intake was 3065 mg/d, and 80.1% consumed ≥2300 mg Na/d (Table 2).
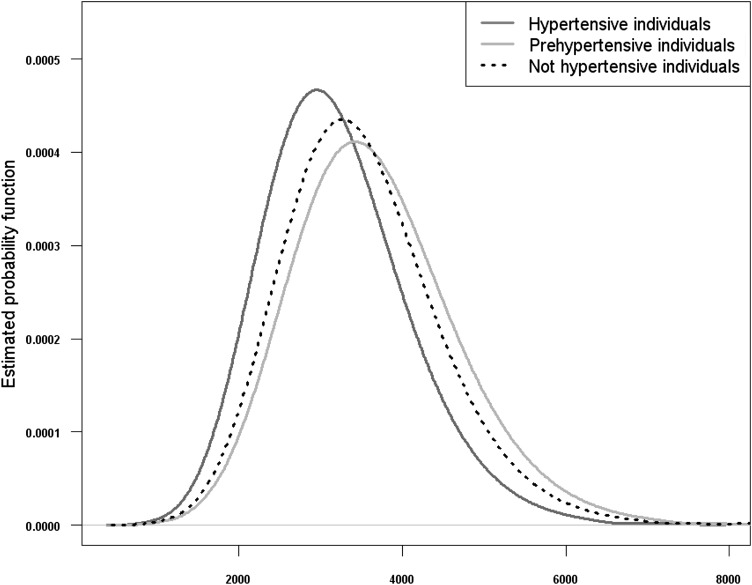
In comparison with their counterparts, usual median daily sodium intake was ∼200–300 mg lower among adults with hypertension, diagnosed diabetes, or chronic kidney disease (Table 1). Despite slightly lower overall intakes, >99% of adults with these specific chronic diseases consumed >1500 mg Na/d (Table 2). In contrast with that in adults with hypertension, usual sodium intake among adults with prehypertension was significantly higher across its distribution. Close to 100% of adults with prehypertension consumed ≥1500 mg/d, and 93.9% consumed ≥2300 mg Na/d (Table 2, Figure 2).
FIGURE 2.
Estimated usual intake of sodium (mg/d) among US adults aged ≥20 y by hypertension status, NHANES 2003–2008, n = 12,581. R statistical software was used to plot the estimated probability function (in mg Na) of usual intakes from the 1000 representative intakes. The figure represents the probability of an individual's usual sodium intake falling within a particular region given by the integral of individual usual sodium intake density over the region. The integral over the entire space is equal to one.
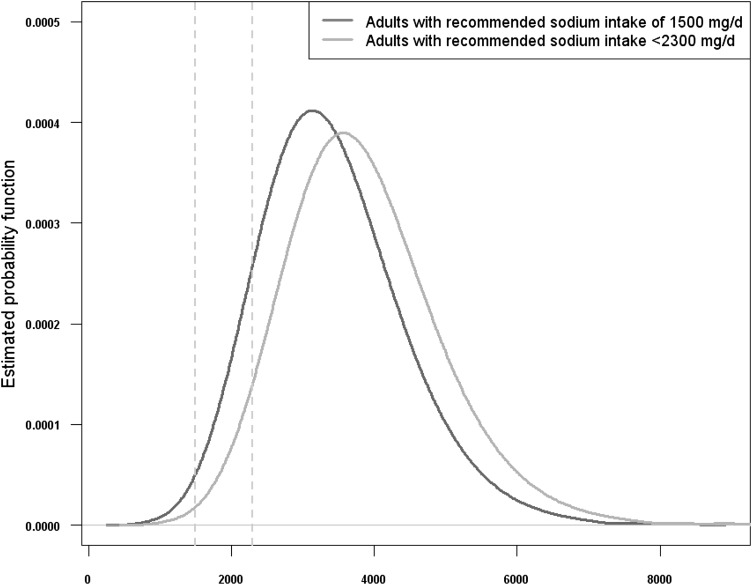
The Dietary Guidelines recommend that persons aged ≥2 y should limit sodium intake to <2300 mg/d, and persons aged ≥51 y, African Americans, or persons with hypertension, diabetes, or chronic kidney disease should further reduce sodium intake to 1500 mg/d. In comparison with adults recommended to further reduce intake to 1500 mg Na/d, usual sodium intake was greater among adults recommended to consume <2300 mg Na/d (Figure 3). Among adults recommended to further reduce sodium intake to 1500 mg/d, median usual daily sodium intake was 3240 mg; 98.8% (95% CI: 98.4%, 99.2%) consumed ≥1500 mg Na/d (Table 3). In addition, most of these adults (60.4%; 95% CI: 56.7%, 64.8%) consumed >3000 mg/d (data not shown). Of the remainder of adults recommended to consume <2300 mg/d, the median intake was 3752 mg, and 95.2% (95% CI: 94.2%, 96.2%) consumed ≥2300 mg/d (Table 3). Even among females recommended to consume <2300 mg/d, the vast majority (72.3%) consumed in excess of recommendations (Table 3).
FIGURE 3.
Estimated usual intake of sodium (mg/d) among US adults aged ≥20 y by recommended sodium intake according to the 2010 Dietary Guidelines for Americans, NHANES 2003–2008, n = 5535. Fasting subsample. According to the Dietary Guidelines for Americans 2010, all Americans should reduce daily sodium intake to <2300 mg (8). Population subgroups who would benefit from further reductions in sodium intake to 1500 mg/d include “persons aged 51 years and older and those of any age who are African-American or have hypertension, diabetes, or chronic kidney disease” (8). Vertical lines are drawn at 1500 and 2300 mg Na/d. R statistical software was used to plot the estimated probability function (in mg Na) of usual intakes from the 1000 representative intakes. The figure represents the probability of an individual's usual sodium intake falling within a particular region given by the integral of individual usual sodium intake density over the region. The integral over the entire space is equal to one.
TABLE 3.
Distribution of usual daily sodium intake among US adults aged ≥20 y by recommended usual daily sodium intake according to the 2010 Dietary Guidelines for Americans: NHANES 2003–20081
| Usual sodium intake |
||||||
| Population subgroup: recommended usual sodium intake (mg/d)2 | No. of subjects3 | 25th Percentile | Median | 75th Percentile | Subjects consuming >1500 mg/d | Subjects consuming≥2300 mg/d |
| mg/d | mg/d | mg/d | % | % | ||
| All | ||||||
| 1500 mg/d | 3810 | 2649 (2533, 2765) | 3240 (3156, 3324) | 3919 (3813, 4025) | 98.8 (98.4, 99.2) | 86.8 (84.1, 89.5) |
| <2300 mg/d | 1725 | 3119 (3027, 3211) | 3752 (3648, 3856) | 4469 (4349, 4589) | 99.8 (99.7, 99.9) | 95.2 (94.2, 96.2) |
| Age 20–30 y | ||||||
| 1500 mg/d | 288 | 3245 (2988, 3502) | 3905 (3605, 4205) | 4645 (4290, 5000) | —4 | 96.5 (94.3, 98.8) |
| <2300 mg/d | 1006 | 3164 (2988, 3340) | 3818 (3656, 3980) | 4553 (4326, 4780) | —4 | 95.7 (93.9, 97.6) |
| Age 31–50 y | ||||||
| 1500 mg/d | 643 | 2917 (2761, 3073) | 3562 (3381, 3743) | 4296 (4075, 4780) | 99.3 (98.9, 99.7) | 91.8 (89.2, 94.4) |
| <2300 mg/d | 1082 | 3088 (2969, 3207) | 3718 (3578, 3858) | 4430 (4263, 4597) | 99.7 (99.6, 99.9) | 94.8 (93.5, 96.2) |
| Age 51–70 y | ||||||
| 1500 mg/d | 1741 | 2706 (2629, 2783) | 3254 (3160, 3348) | 3860 (3766, 3954) | 99.3 (99.0, 99.6) | 88.9 (86.7, 91.1) |
| <2300 mg/d | NA | NA | NA | NA | NA | NA |
| Age ≥71 y | ||||||
| 1500 mg/d | 988 | 2178 (2085, 2270) | 2623 (2516, 2730) | 3136 (3006, 3266) | 97.0 (95.9, 98.1) | 68.5 (63.1, 73.8) |
| <2300 mg/d | NA | NA | NA | NA | NA | NA |
| Men | ||||||
| 1500 mg/d | 1935 | 3119 (3013, 3225) | 3819 (3703, 3935) | 4624 (4477, 4771) | 99.6 (99.4, 99.8) | 94.4 (93.0, 95.8) |
| <2300 mg/d | 889 | 3666 (3488, 3844) | 4406 (4267, 4545) | 5253 (5055, 5451) | —4 | 98.5 (97.9, 99.1) |
| Women | ||||||
| 1500 mg/d | 1875 | 2242 (2175, 2309) | 2748 (2675, 2821) | 3326 (3222, 3430) | 97.0 (96.2, 97.8) | 72.3 (69.2, 75.4) |
| <2300 mg/d | 836 | 2628 (2526, 2730) | 3165 (3059, 3271) | 3765 (3643, 3887) | 99.0 (98.6, 99.4) | 86.9 (84.0, 89.8) |
| Non-Hispanic white | ||||||
| 1500 mg/d | 1868 | 2684 (2591, 2777) | 3260 (3167, 3353) | 3921 (3797, 4045) | 99.3 (98.9, 99.7) | 88.3 (96.0, 90.6) |
| <2300 mg/d | 1006 | 3215 (3104, 3326) | 3822 (3702, 3942) | 4506 (4370, 4642) | —4 | 96.7 (95.6, 97.8) |
| Non-Hispanic black | ||||||
| 1500 mg/d | 1079 | 2612 (2495, 2729) | 3219 (3087, 3351) | 3920 (3716, 4124) | 98.7 (98.1, 99.2) | 85.6 (81.8, 89.3) |
| <2300 mg/d | NA | NA | NA | NA | NA | NA |
| Mexican American | ||||||
| 1500 mg/d | 543 | 2511 (2324, 2698) | 3136 (2909, 3363) | 3837 (3559, 4115) | 97.7 (96.4, 99.0) | 82.2 (76.7, 87.7) |
| <2300 mg/d | 487 | 2841 (2623, 3059) | 3487 (3246, 3728) | 4210 (3945, 4475) | 99.3 (98.7, 99.8) | 90.5 (86.3, 94.7) |
Medians, IQRs, and proportions >1500 and ≥2300 mg/d and 95% CIs for all measures (in parentheses) were estimated from Software for Intake Distribution Estimation for the Windows Operating System (Department of Statistics, Iowa State University) with jackknife replicate weights and were adjusted for interview method (in person or by phone), day of the week, and sex (for all adults and for all stratified analyses, except by sex). NA, not applicable.
According to the Dietary Guidelines for Americans 2010, all Americans should reduce daily sodium intake to <2300 mg. Population subgroups who would benefit from further reductions in sodium intake to 1500 mg/d include “persons aged 51 years and older and those of any age who are African-American or have hypertension, diabetes, or chronic kidney disease” (4).
Sample sizes are unweighted. Fasting subsample only. Excludes pregnant women and individuals missing data on sodium intakes and covariates and individuals who report being on dialysis.
Does not meet standard of statistical reliability, relative SE >40%.
Usual adult sodium intake by age and sex in 2003–2008 did not differ substantially from previously published estimates for 1988–1994, with few exceptions (see Supplemental Table 1 under “Supplemental data” in the online issue). In 1988–1994, US men aged 19–30 y had the highest median and mean usual sodium intakes of any age group and sex group (median ± SE intake: 4717 ± 132 mg; mean ± SD intake: 4746 ± 88 mg). In 2003–2008, the median daily intake among US men aged 19–30 y was 4359 ± 102 mg, and the mean intake was 4464 ± 83 mg. The mean usual sodium intake in 2003–2008 among men aged 19–30 y did not differ from that among men aged 31–50 y (4432 ± 55 mg; P = 0.37), based on a z test for difference in means (data not shown) The distribution of usual sodium intake among men aged 19–30 y appears to have shifted over time, the 25th percentile was ∼700 mg less and the median ∼300 mg less, whereas the 75th percentile differed little (see Supplemental Table 1 under “Supplemental data” in the online issue). However, as expected, given that ∼5% in 1988–1994 compared with ∼90% in 2003–2008 had a second 24-h dietary recall, at the 25th and 75th percentiles, the SEs around the 1988–1994 estimates were large, ∼400–500 mg, whereas in 2003–2008 the SEs were ∼90–120 mg. In comparison with 1988–1994, the quartiles and means of usual sodium intake in 2003–2008 were lower among men aged ≥71 y (eg, mean intake was 3198 ± 63 mg in 1988–1994 compared with 3021 ± 54 mg in 2003–2008; P = 0.02) but were higher among women aged 51–70 y (eg, mean intake was 2613 ± 33 mg in 1988–1994 compared with 2815 ± 34 mg in 2003–2008; P ≤ 0.01).
Overall, dietary potassium intake was less than sodium intake. The median usual potassium intake was 2631 mg (IQR: 2164 mg, 3161 mg) among US adults aged ≥20 y in 2003–2008 (Table 4). Usual daily intake of <2% of US adults met guidelines (1.4%; 95% CI: 1.2%, 1.7%). Usual potassium intake varied by sociodemographic characteristics (Table 4). In comparison with adults aged 20–30 y, across percentiles usual potassium intake was slightly greater among adults aged 31–50 y (Table 4). Men consumed the most potassium of any sociodemographic or health group examined (median intake: 3037 mg/d), yet only 4.7% consumed ≥4700 mg/d) (Table 4). In comparison with non-Hispanic white adults, usual intakes were significantly lower among non-Hispanic black adults across the distributions of potassium intake. Usual median potassium intake was statistically significantly higher among adults with higher income or >12 y of education. In comparison with their counterparts without these conditions, usual potassium intake was statistically significantly lower among US adults with diabetes or chronic kidney disease but not obesity or hypertension.
TABLE 4.
Distribution of usual daily potassium intakes among US adults aged ≥20 y: NHANES 2003–20081
| Usual potassium intake |
|||||
| Category | No. of subjects | 25th Percentile | Median | 75th Percentile | Subjects consuming ≥4700 mg/d |
| mg/d | mg/d | mg/d | % | ||
| All | 12,581 | 2164 (2116, 2212) | 2631 (2583, 2679) | 3161 (3111, 3211) | 1.4 (1.2, 1.7) |
| Age | |||||
| 20–30 y | 2161 | 2064 (1954, 2174) | 2502 (2412, 2592) | 3007 (2887, 3127) | 0.8 (0.4, 1.2) |
| 31–50 y | 4240 | 2280 (2222, 2338) | 2752 (2688, 2816) | 3285 (3212, 3358) | 1.7 (1.3, 2.1) |
| 51–70 y | 3915 | 2196 (2121, 2271) | 2651 (2569, 2733) | 3166 (3077, 3255) | 1.3 (0.9, 1.6) |
| ≥71 y | 2265 | 1984 (1928, 2040) | 2395 (2331, 2459) | 2863 (2783, 2943) | 0.5 (0.2, 0.8)2 |
| Sex | |||||
| Male | 6379 | 2524 (2472, 2576) | 3037 (2985, 3089) | 3632 (3577, 3687) | 4.7 (4.0, 5.3) |
| Female | 6202 | 1859 (1818, 1902) | 2279 (2231, 2327) | 2754 (2699, 2809) | 0.3 (0.2, 0.5) |
| Race-ethnicity | |||||
| Non-Hispanic white | 6435 | 2221 (2161, 2281) | 2712 (2651, 2773) | 3269 (3207, 3331) | 1.9 (1.5, 2.2) |
| Non-Hispanic black | 2551 | 1781 (1728, 1834) | 2193 (2129, 2257) | 2672 (2582, 2762) | —3 |
| Mexican American | 2357 | 2135 (2050, 2220) | 2586 (2489, 2683) | 3101 (2991, 3211) | 0.9 (0.4, 1.4) |
| Other | 1238 | 2081 (2016, 2146) | 2521 (2445, 2597) | 3036 (2942, 3130) | 1.0 (0.6, 1.4) |
| Household income4 | |||||
| ≤130% Federal poverty index | 3317 | 1922 (1832, 2012) | 2392 (2321, 2463) | 2949 (2853, 3045) | 1.4 (0.8, 2.0) |
| >130% Federal poverty index | 8497 | 2230 (2183, 2277) | 2688 (2638, 2738) | 3205 (3150, 3260) | 1.2 (1.0, 1.5) |
| Education | |||||
| <12 y | 3620 | 1962 (1864, 2060) | 2415 (2347, 2483) | 2941 (2793, 3089) | 1.0 (0.4, 1.6) |
| 12 y or GED | 3108 | 2085 (2032, 2138) | 2537 (2482, 2592) | 3053 (2985, 3121) | 1.1 (0.6, 1.5) |
| >12 y | 5853 | 2288 (2229, 2347) | 2748 (2686, 2810) | 3266 (3202, 3330) | 1.5 (1.1, 1.8) |
| BMI | |||||
| <18.5 kg/m2 | 189 | 2021 (1786, 2256) | 2613 (2337, 2889) | 3298 (2945, 3651) | —3 |
| 18.5–24.9 kg/m2 | 3547 | 2160 (2086, 2234) | 2651 (2574, 2728) | 3214 (3135, 3293) | 1.8 (1.4, 2.3) |
| 25.0–29.9 kg/m2 | 4405 | 2221 (2142, 2300) | 2686 (2613, 2759) | 3218 (3135, 3301) | 1.6 (1.0, 2.3) |
| ≥30.0 kg/m2 | 4440 | 2115 (2033, 2197) | 2554 (2491, 2617) | 3048 (2967, 3129) | 0.7 (0.4, 1.0) |
| Hypertension status5 | |||||
| Hypertension | 4867 | 2098 (2047, 2149) | 2546 (2486, 2606) | 3057 (2987, 3127) | 1.0 (0.8, 1.3) |
| Prehypertension | 3228 | 2290 (2237, 2343) | 2756 (2699, 2813) | 3283 (3217, 3349) | 1.5 (1.0, 1.9) |
| No hypertension | 4486 | 2150 (2072, 2228) | 2613 (2539, 2687) | 3144 (3055, 3233) | 1.4 (0.9, 1.9) |
| Diabetes diagnosis6 | |||||
| Yes | 1471 | 2051 (1979, 2123) | 2486 (2401, 2571) | 2982 (2871, 3094) | 0.9 (0.3, 1.5)2 |
| No | 11,110 | 2174 (2124, 2224) | 2644 (2594, 2694) | 3178 (3127, 3229) | 1.4 (1.2, 1.7) |
| Chronic kidney disease7 | |||||
| Yes | 2546 | 1982 (1915, 2049) | 2408 (2330, 2486) | 2895 (2805, 2985) | 0.7 (0.3, 1.1)2 |
| No | 10,035 | 2197 (2144, 2250) | 2670 (2617, 2723) | 3208 (3151, 3265) | 1.5 (1.2, 1.9) |
Medians, IQRs, and proportions ≥4700 mg/d and 95% CIs for all measures (in parentheses) were estimated from Software for Intake Distribution Estimation for the Windows Operating System (Department of Statistics, Iowa State University) with jackknife replicate weights and were adjusted for interview method (in person or by phone), day of the week, and age (continuous), sex, and race-ethnicity group, as possible. Sample sizes are unweighted. Pregnant women and individuals missing data on potassium intakes or covariates were excluded. GED, general equivalency diploma.
Estimate may be unreliable, relative SE >30% but ≤40%.
Does not meet standard of statistical reliability, relative SE >40%.
Family income was defined as total household income divided by the poverty threshold for the year of the interview multiplied by 100.
Hypertension was defined as a mean systolic blood pressure ≥140 mm Hg, a mean diastolic blood pressure ≥90 mm Hg, or self-reported use of antihypertensive medication (25, 26). Prehypertension was defined as a mean systolic blood pressure 120–139 mm Hg or a mean diastolic blood pressure 80–89 mm Hg (26). Normal blood pressure was defined as a mean systolic blood pressure <120 mm Hg and a mean diastolic blood pressure <80 mm Hg. Mean blood pressure was estimated from up to 3 readings on a single occasion.
Diabetes was defined by self-reported diagnosis by a health care provider.
Patterns of usual potassium intakes by age and sex in 2003–2008 did not differ from patterns in 1988–1994 (see Supplemental Table 2 under “Supplemental data” in the online issue). In 2003–2008, however, the distributions of usual potassium intakes were lower across all age and sex groups. Compared with intakes in 1988–1994, average potassium intakes in 2003–2008 were lower among US men by ∼150–380 mg (P ≤ 0.01 for all comparisons) and among US women by ∼90–150 mg.
DISCUSSION
In 2003–2008, almost all adults exceeded the AHA recommendations for sodium intake, and the vast majority of adults consumed excessive sodium relative to either the IOM UL or the 2010 Dietary Guidelines (4, 8, 9). Given that ∼57% of US adults are recommended to consume 1500 mg/d (13), ∼97% of the US adult population in 2003–2008 consumed more sodium than recommended by the 2010 Dietary Guidelines (8), ie, 97% = (0.57 × 98.8%) + (0.43 × 95.2%). Specific population groups recommended in the Dietary Guidelines to further reduce intake to 1500 mg/d had lower usual median intakes than did their counterparts recommended to consume <2300 mg/d, but >98% consumed in excess of their recommended amount (1500 mg/d), with most consuming >2 times in excess of 1500 mg/d. In addition, <2% of US adults overall and <5% across specific population subgroups consumed ≥4700 mg K/d—the amount recommended to blunt the effects of sodium intake on blood pressure (4, 8).
Our results provide the most recent estimates for usual sodium and potassium intakes among US adults in relation to current dietary recommendations by sociodemographic and health characteristics (11, 14). Our estimates of usual potassium intake ≥4700 mg/d among US men (4.7%) in 2003–2008 are comparable with previously published estimates of usual potassium intake (4.0%) (12).
In comparison with published data in 1988–1994 (4), average sodium intake in 2003–2008 did not change significantly over time across most population subgroups. In contrast with sodium intake, our data suggest that potassium intake declined. The reason for this decline is unclear: Usual intake estimates in 2003–2008 are more robust given that most participants had two 24-h dietary recalls, allowing for better adjustment for measurement error. Differences in the data collection protocols (eg, food-specific probes for salt used in preparation in 1988–1994) and processing (use of default food codes in either survey) may contribute to differences in estimates over time (36). However, little to no difference across time was observed in sodium intakes. This suggests a lack of universal bias related to differences in methods of data collection or coding across foods. Although overall dairy consumption, a good source of potassium, has not changed since 1994, the percentage of adults consuming fluid milk declined from 1977–1978 to 2005–2006 (37, 38). Fruit and vegetable consumption among US adults changed little since 1994 (39). Trends in consumption of unprocessed meats and potassium-containing fruit and vegetables are less well known. Decreased intake of these foods is one possible explanation and highlights the need for monitoring total potassium intake by using biomarkers and its major food sources.
Our study had major strengths and potential limitations. The strengths include the large representative national sample and use of two 24-h dietary recalls on a high proportion of adults with measurement error models to account for within individual variation in intake. The prevalence of sodium intake ≥2300 mg based the initial 24-h recall in US adults aged ≥20 y is 73.1% compared with 90.7% based on two 24-h dietary recalls accounting for within-individual variation. Compared with total energy intake from doubly labeled water, energy intake is underestimated by 11% by using the 24-h dietary recall and may underestimate sodium intake because of the correlation between energy and sodium intakes (40, 41). Actual sodium and potassium in foods may be higher or lower than that estimated in the nutrient database. Our estimates exclude sodium from table salt, supplements, and antacids, which account for an estimated 6% of total dietary sodium intake (11, 25), thus underestimating the proportion of US adults with excessive intakes. In 2003–2004 and 2005–2008, the methods for estimating sodium intake from drinking water differed. However, it is doubtful that this affected our results, because the estimated mean sodium intake from drinking water among US adults in 2003–2004 was 37 mg, ∼1% of total intake. Nonresponse bias may result in an over- or underestimate of the usual daily intake of sodium and potassium; estimates of dietary intake are weighted to account for nonresponse, which reduces the possibility of bias; however, in the overall analysis, approximately an additional 10% of the sample was excluded because of missing information on covariates. Usual sodium and potassium intakes did not differ meaningfully with and without these individuals in the analyses.
Our results emphasize how the vast majority of US adults consume sodium in far excess of recommendations, even without added table salt, and confirm that previous advice to avoid salt remains an inefficient way of controlling sodium intake at the population levels. Indeed, despite decades of US consumer-based education initiatives, most US adults do not meet national guidelines for limiting sodium intake or for adequate potassium intake regardless of sociodemographic and health characteristics. Greater than 75% of sodium intake is from packaged and restaurant foods (11, 25), which makes it difficult for individuals to reduce their own sodium intake (4, 8). In 2010, the IOM outlined primary and interim strategies for reducing sodium intake (11). The primary recommended strategy is for the FDA to set mandatory national standards for the sodium content of foods. Public comments on this and other strategies were recently solicited by the FDA and the USDA's Food Safety Inspection Service (42). The interim strategy is for the food industry to act voluntarily to reduce sodium in packaged and restaurant foods. Food procurement and labeling policies at the national, state, and local levels are additional strategies to reduce sodium intake in the US population (43–47). Recent data suggest that most US adult consumers want to reduce their sodium intake and agree with policies to reduce sodium in manufactured and restaurant foods (43). In addition, the minority of US adults with adequate potassium intakes suggests the value of ongoing efforts to change the food environment and improve the accessibility of unprocessed low-fat meats, low-fat dairy products, and fresh fruit and vegetables that are usually good sources of potassium (48).
Furthermore, a common eating pattern recommended to prevent or treat hypertension, the Dietary Approaches to Stop Hypertension (DASH) eating pattern, emphasizes the consumption of fruit, vegetables, and fat-free or low-fat milk and milk products and has targets of 2300 and 4700 mg for sodium and potassium, respectively (48). Although a DASH diet with 2300 mg Na/d was effective at lowering blood pressure, a DASH diet with 1500 mg Na/d and 4700 mg K/d resulted in a further decrease in blood pressure and is recommended for specific population subgroups, including individuals with, or at risk of, hypertension (5, 8, 49). In our study, adults at risk of hypertension, ie, with prehypertension, consumed more sodium than did adults with hypertension, comparable to or slightly greater than the amount consumed by adults without hypertension, which suggests the need for enhanced counseling for this group. Reductions in sodium across the food supply coupled with increased access and availability of fruit and vegetables should make it more feasible for people with, or at risk of, hypertension to adopt the DASH and other low-sodium, high-potassium diets.
Reducing the average dietary sodium intake by 400 mg/d is estimated to save up to $7 billion in US health care costs annually (50). Regardless of recommended limits for sodium intake and sociodemographic and health characteristics, the vast majority of US adults consume too much sodium and too little potassium. Even small shifts in the distributions of intake could increase the proportion of US adults who meet the current dietary recommendations, decrease hypertension, and reduce the associated health care costs.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—MEC: had full access to all of the data in the study and had primary responsibility for the integrity of the data, the accuracy of the data analysis, and the final content; MEC, ZZ, JPG, EVK, SHS, ALC, and AJM: conceived and designed the study; MEC, ZZ, QY, and ALC: performed the statistical analysis; MEC and ZZ: drafted the manuscript; and MEC, ZZ, ALC, JPG, SHS, EVK, QY, and AJM: critically revised the manuscript for important intellectual content. No conflicts of interest were reported.
Footnotes
Abbreviations used: AHA, American Heart Association; DASH, Dietary Approaches to Stop Hypertension; IOM, Institute of Medicine; NCHS, National Center for Health Statistics; PC-SIDE, Software for Intake Distribution Estimation for the Windows Operating System; UL, Tolerable Upper Intake Level.
REFERENCES
- 1.Lawes CM, Vander Hoorn S. Rodgers A for the International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513–8 [DOI] [PubMed] [Google Scholar]
- 2.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiologic studies. BMJ 2009:338;b1665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, Peto R. Collins R for the Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903–13 [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, DC: The National Academies Press, 2005 [Google Scholar]
- 5.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, III, Simons-Morton DG, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med 2001;344:3–10 [DOI] [PubMed] [Google Scholar]
- 6.Morris RC, Jr, Schmidlin O, Freassetto LA, Sebastian A. Relationship and interaction between sodium and potassium. J Am Coll Nutr 2006;25:262S–70S [DOI] [PubMed] [Google Scholar]
- 7.Morris RC, Jr, Sebastian A, Forman A, Tanaka M, Schmidlin O. Normotensive salt sensitivity: effects of race and dietary potassium. Hypertension 1999;33:18–23 [DOI] [PubMed] [Google Scholar]
- 8.US Department of Health and Human Services, USDA. Dietary guidelines for Americans, 2010. 7th ed. Washington, DC: USDA, 2011.
- 9.Lloyd-Jones DM, Hong Y, Labarthe D, Mozzaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction, the American Heart Association's Strategic Impact Goal through 2020 and beyond. Circulation 2010;121:586–613 [DOI] [PubMed] [Google Scholar]
- 10.USDA, Agricultural Research Service. 2010. Nutrient intakes from food. Mean amounts consumed per individual, by gender and age. What we eat in America, NHANES 2007–2008. Updated 14 April 2011. Available from: www.ars.usda.gov/ba/bhnrc/fsrg (cited 10 August 2011)
- 11.Institute of Medicine Strategies to reduce sodium intake in the United States. Washington, DC: The National Academies Press, 2010 [Google Scholar]
- 12.US Department of Health and Human Services, CDC. Healthy people 2010. Progress review focus area 19–nutrition and overweight. Calcium, sodium and potassium tables. Updated 14 October 2009. Available from: http://www.cdc.gov/nchs/healthy_people/hp2010/focus_areas/fa19_nutrition2.htm (cited 10 August 2011)
- 13.CDC Dietary sodium intake compared with recommended intake, United States, 2005-2008. MMWR Morb Mortal Wkly Rep 2011;60:1413–7 [PubMed] [Google Scholar]
- 14.USDA, Agricultural Research Service. What we eat in America. Food Surveys Research Group. Data Tables. 2005–2006. Usual nutrient intakes, sodium. Available from: http://www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/0506/usual_nutrient_intake_sodium_2003-06.pdf (cited 20 September 2011)
- 15.Thompson FE, Subar AF. Dietary assessment methodology : Coulston AM, Boushey CJ, eds. Nutrition in prevention and treatment of disease 2nd ed. San Diego, CA: Academic Press, 2008 [Google Scholar]
- 16.Carriquiry AL, Camano-Garcia G. Evaluation of dietary intake data using the tolerable upper intake levels. J Nutr 2006;136:507S–13S [DOI] [PubMed] [Google Scholar]
- 17.Dodd KW, Guenther PM, Freedman LS, Subar AF, Kipnis V, Midthune D, Tooze JA, Krebs-Smith SM. Statistical methods for estimating usual intake of nutrients and foods: a review of the theory. J Am Diet Assoc 2006;106:1640–50 [DOI] [PubMed] [Google Scholar]
- 18.Carriquiry AL. Estimation of usual intake distributions of nutrients and foods. J Nutr 2003;133:601S–8S [DOI] [PubMed] [Google Scholar]
- 19.CDC, National Center for Health Statistics. National Health and Nutrition Examination Survey data. Hyattsville, MD: US Department of Health and Human Services, CDC, 2003–2004. Updated 14 May 2010. Available from: http://www.cdc.gov/nchs/nhanes/nhanes2003-2004/nhanes_03_04.htm (cited 13 August 2011)
- 20.CDC, National Center for Health Statistics. National Health and Nutrition Examination Survey data. Hyattsville, MD: US Department of Health and Human Services, CDC, 2005–2006. Updated 29 April 2011. Available from: http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/nhanes05_06.htm (cited 13 August 2011)
- 21.CDC, National Center for Health Statistics. National Health and Nutrition Examination Survey data. Hyattsville, MD: US Department of Health and Human Services, CDC, 2007–2008. Updated 10 May 2011. Available from: http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/nhanes07_08.htm (cited 13 August 2011)
- 22.National Center for Health Statistics. National Health and Nutrition Examination Survey. Response rates and CPS totals. Available from: http://www.cdc.gov/nchs/nhanes/response_rates_CPS.htm (cited 13 August 2011)
- 23.USDA, Agricultural Research Service. Product & Services. FNDDS (Food and Nutrient Database for Dietary Studies). Updated 12 August 2010. Available from: http://www.ars.usda.gov/services/docs.htm?docid=12089 (cited 13 August 2011)
- 24.USDA USDA food and nutrient database for dietary studies, 2.0. Beltsville, MD: Agricultural Research Service, Food Surveys Research Group, 2006 [Google Scholar]
- 25.Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr 1991;10:383–93 [DOI] [PubMed] [Google Scholar]
- 26.NIH, National Heart, Lung, and Blood Institute Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity: the evidence report. Rockville, MD: US Department of Health and Human Services, 1998 [Google Scholar]
- 27.CDC Vital signs: prevalence, treatment, and control of hypertension—United States, 1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep 2011;60:103–8 [PubMed] [Google Scholar]
- 28.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JI, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, et al. The seventh report or the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. The JNC 7 report. JAMA 2003;289:2560–72 [DOI] [PubMed] [Google Scholar]
- 29.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 2003;139:137–47 [DOI] [PubMed] [Google Scholar]
- 30.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dodd KW. A useraposs guide to C-SIDE: software for intake distribution estimation version 1.0. Ames, IA: Center for Agriculture and Rural Development, Iowa State University, 1996 (CARD Technical Report 96-TR31)
- 32.Guenther PM, Kott PS, Carriquiry AL. Development of an approach for estimating usual nutrient intake distributions at the population level. J Nutr 1997;127:1106–12 [DOI] [PubMed] [Google Scholar]
- 33.R Development Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2009. Available from: http://www.R-project.org (cited 11 September 2011)
- 34.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2011;34:S62–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.CDC, National Center for Health Statistics. Third National Health and Nutrition Examination Survey (NHANES III), 1988ndash94, NHANES III second exam file documentation. Series 11, No. 3A. Atlanta, GA: CDC 2009.
- 36.CDC, National Center for Health Statistics. Third National Health and Nutrition Examination Survey (NHANES III), 1988ndash94, NHANES III individual foods data file from the dietary recall documentation. Series 11, No. 2A. Atlanta, GA: 1998.
- 37.Wang Y, Li S. Worldwide trends in dairy production and consumption and calcium intake: Is promoting consumption of dairy products a sustainable solution for inadequate calcium intake. Food Nutr Bull 2008;29:172–85 [DOI] [PubMed] [Google Scholar]
- 38.USDA, Agriculture Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group. 2010. Fluid milk consumption in the United States: what we eat in America, NHANES 2005–2006. Food Surveys Research Group Dietary Data Brief. Available from: http://www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/DBrief/fluid_milk_0506.pdf (accessed 20 September 2011)
- 39.Blanck HM, Gillespie C, Kimmons JE, Seymour JD, Serdula MK. Trends in fruit and vegetable consumption among U.S. men and women. 1994-2005. Available from: http://www.cdc.gov/pcd/issues/2008/apr/07_0049.htm (cited 18 August 2011) [PMC free article] [PubMed] [Google Scholar]
- 40.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynsk KJ, Ingwersen LA, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88:324–32 [DOI] [PubMed] [Google Scholar]
- 41.Espeland MA, Kumanyika S, Wilson AC, Reboussin DM, Easter L, Self M, Robertson J, Brown WM. McFarlane M for the TONE Cooperative Research Group. Statistical issues in analyzing 24-hour dietary recall and 24-hour urine collection data for sodium and potassium intakes. Am J Epidemiol 2001;153:996–1006 [DOI] [PubMed] [Google Scholar]
- 42.US Department of Health and Human Services, Food and Drug Administration. Approaches to reducing sodium consumption; establishment of dockets: request for comments, data, and information. Fed Reg 2011;76(179): 57050–4. Available from: http://www.regulations.gov/#!documentDetail;D=FDA-2011-N-0400-0001.
- 43.CDC. Public health grand rounds: sodium reduction, time for choice. Atlanta, GA: US Department of Health and Human Services, CDC, 2011. Available at: http://www.cdc.gov/about/grand-rounds/resources/PHGRSodRed5FINAL.pdf.
- 44.US Department of Health and Human Services, CDC. Sodium reduction in communities. Updated 2 August 2011. Available from: http://www.cdc.gov/dhdsp/programs/sodium_reduction.htm (cited 12 August 2011)
- 45.US Department of Health and Human Services, CDC Improving the food environment through nutrition standards: a guide for government procurement. Atlanta, GA: CDC, 2010 [Google Scholar]
- 46.US Department of Health and Human Services, General Services Administration. Health and sustainability guidelines for federal concessions and vending operations. Last reviewed 8 July 2011. Available from: http://www.gsa.gov/portal/content/104429 (cited 14 September 2011)
- 47.US Department of Agriculture. School programs USDA food update. Updated October 2011. Available from: http://www.fns.usda.gov/fdd/news/schupdates1010.pdf (cited 13 August 2011)
- 48.US Department of Health and Human Services, National Heart, Lung, and Blood Institute, NIH. Your guide to lowering your blood pressure with DASH, DASH eating plan. 1998. Revised April 2006. Reprinted February 2010. Available from: http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf (cited 14 September 2011)
- 49.Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG, Conlin PR, Svetkey LP, Erlinger TP, Moore TJ, et al. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-Sodium Trial. Ann Intern Med 2001;135:1019–28 [DOI] [PubMed] [Google Scholar]
- 50.Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010;362:590–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.