Abstract
The manuscript examines the influence of contextual factors on whether and for whom a colon polyp diagnosis might be a teachable moment, as indicated by engagement with a proactively delivered intervention. Baseline and 8-month follow-up data were analyzed from a two-site behavioral intervention trial with patients in Massachusetts and North Carolina, USA who had recently undergone polypectomy for pre-cancerous colon polyps and were randomized to a behavior change intervention condition (N = 591). Intervention “buy-in” was used as an indicator of response consistent with the polyp identification serving as a teachable moment. Cancer worry, personal risk, health-related self-identity and other sociodemographic factors were tested to predict intervention buy-in. As predicted, those who were most worried about colon cancer were most likely to engage in the intervention. One indicator of personal risk, number of risk behaviors, was significantly and negatively associated with buy-in. Predictors of intervention buy-in and cancer worry were not consistent. We recommend that expanded measures of affect and health-related self-identity should be considered in future research to understand the motivational potential of health events for increasing engagement in effective behavior change interventions.
Keywords: Worry, Teachable moment, Behavior change, USA, Colon cancer
Introduction
The term “teachable moment” has been used colloquially with great frequency to suggest that health events can be powerful motivators of health behavior changes (Carlos, Underwood, Fendrick, & Bernstein, 2005; Esler & Bock, 2004; Gorin, Phelan, Hill, & Wing, 2004; McBride, Emmons, & Lipkus, 2003). Indeed, numerous observational studies have documented, for example, that cancer diagnosis, cardiovascular event, and pregnancy determination are associated with abrupt and proximal smoking cessation (McBride et al., 2003). However, it also is notable that a sizeable proportion of individuals who experience these often life-threatening health events do not make behavioral changes. This raises questions about the factors that influence whether and for whom such events become “teachable moments”. Very little research has explored what inter- and intrapersonal factors underlie the teachable moment, that is, what factors shape how individuals respond to health events and how these responses might influence motivation for and subsequent behavior change.
Research aimed at better understanding what influences the potency of a teachable moment holds several advantages. Some individuals might be relatively more inclined than others to participate and make behavior changes if formal interventions are timed to coincide with these events. Accordingly, capitalizing on this heightened receptivity might mean that low-intensity interventions that also are low in cost and amenable to dissemination could achieve better outcomes. Improved understanding of individuals’ cognitive and affective responses to health events and their effects on behavior change also could lend insight into the underpinnings of motivation more generally.
However, research that aims to characterize teachable moments is especially challenging because health events often cannot be predicted or randomly assigned and thus are not amenable to proximal pre- and post-test assessments or experimental control. At best, cognitive and affective reactions to these health events are assessed coincident with, or well after the event has occurred. Moreover, determining appropriate comparison groups, that is, individuals who are otherwise comparable but are not experiencing the relevant health event also raises significant challenges.
A more feasible initial approach that could advance our understanding would be to identify a group that has experienced a common health event and retrospectively characterize the cognitive and affective responses of those who were most likely to engage with an offered intervention timed to coincide with the health event. This retrospective characterization, however, should be guided by a conceptual framework to suggest which factors to consider and their possible inter-relationships.
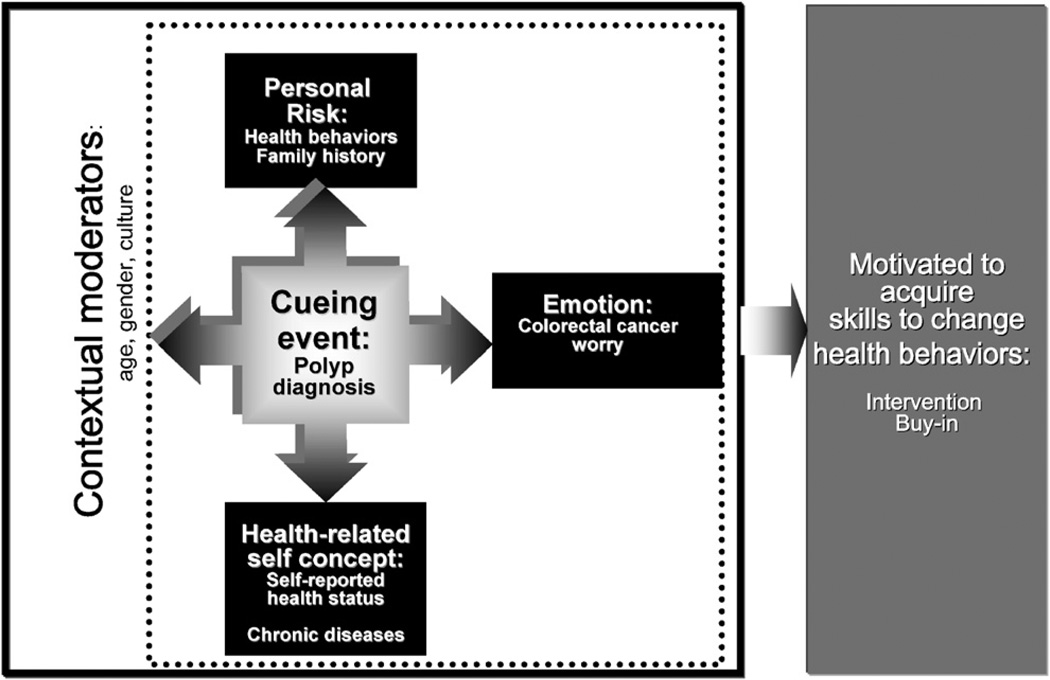
Teachable moment heuristic
Whether an event can be a teachable moment that motivates behavior change is thought to depend on the individual’s subjective interpretation of the significance, cause and meaning of the event (Fife, 2005; Weick, 1993). We previously have characterized the teachable moment to represent the immediate sense-making processes that are prompted by the occurrence of a health event (McBride et al., 2003). We distinguished these antecedent processes from more distal self-evaluations of confidence and competencies needed to remediate any health threat posed by the event. We suggested a conceptualization of this immediate subjective response to encompass at least three domains that may be important in determining whether the experience motivates consequent steps towards risk reduction (McBride et al., 2003). These suggested domains derive from widely accepted conceptual models of behavior change (Bandura, 1977; Fishbein & Ajzen, 1975; Lazarus, 1993; Weinstein, 1988) and include: the extent to which the event: (a) affects perceived personal risk, (b) prompts emotions such as worry, and (c) challenges the individual’s self-concept. In this report, we use this conceptual rationale to explore how one’s subjective response to a health event might influence engagement with a proactively offered intervention (see Fig. 1).
Fig. 1.
Heuristic model for teachable moment.
As we have described previously (McBride et al., 2003), there is conceptual and empirical support for each of the three domains in our heuristic and their potential to influence motivation for behavior change. Theories of health behavior consistently suggest the centrality of perceived threat and its association with negative affect and attentive vigilance in motivating preventive action (Witte, 1998). Affective responses, such as worry, have been studied with some frequency, in particular with respect to cancer-related events. Some affective responses have been found to increase adherence to cancer screening recommendations (Consedine, Magai, Krivoshekova, Ryzewicz, & Neugut, 2004; Hay, Buckley, & Ostroff, 2004). Worry, which has been characterized as “persistent awareness of or attention to possible danger” (Gladstone & Parker, 2003), can be prompted by a threatening event (Eysenck, 1992). The event acts as a cue that increases threat-relevant thoughts that can prompt the individual to think about and anticipate potential negative outcomes. In turn, motivation to reduce threat is a common coping response (Aspinwall & Taylor, 1997; Folkman & Moskowitz, 2000; Frijda, 1986; Lazarus, 1993). With respect to the teachable moment, it is posited that health events that elicit emotional responses such as worry will be attended to and appraised as most significant and meaningful. Accordingly, motivation to reduce risk might take the form of increased receptivity to engage with concurrently timed interventions.
Risk perceptions also have been associated with motivation for behavior change (see for example, Lipkus & Klein, 2006). Personal health events may increase perceptions of personal vulnerability to threat, and in so doing, increase motivation for behavior change. Indeed a health event experience occurs against a backdrop of an individual’s understanding of their personal disease risk. For example, individuals who acknowledge having a relevant family history of disease, prior experiences with the health threat, or engaging in poor health habits may have different subjective responses to a health event than their contemporaries without these acknowledged personal risk factors.
The domain of self-identity is less explored, and potentially as important, to creating a teachable moment. Health events also occur against the back drop of an individual’s sense of self-identity. Subjective response to the event then might be influenced to the extent that the event poses a challenge to an individual’s self-identity. For example, theories of the self suggest that individuals are motivated to maintain positive self-illusions or “esteem motivation”. These motives can contribute to how life events are interpreted (Steele, 1988; Taylor, Kemeny, Reed, Bower, & Gruenewald, 2000). Individuals see events that threaten or enhance their self-identity or endanger positive expectations of the future as more personally relevant (Aspinwall & Brunhart, 1996; Jannoff-Bulman & Frieze, 1987; Tennen & Affleck, 1987). Several studies have suggested that motives related to preserving one’s present self image or a projected future hoped- for self may prompt behavior changes such as improved dietary habits (Satia, Kristal, Curry, & Trudeau, 2001), physical activity (Ouellette, Hessling, Gibbons, Reis-Bergan, & Gerrard, 2005), and mammography screening (Black, Stein, & Loveland-Cherry, 2001).
One must consider as well that these health events also occur within a broader social context as indicated by sociodemographic characteristics. While unchangeable, these characteristics may influence how the health event is perceived. For example, age, gender, socioeconomic status and ethno-cultural background all have been suggested to play a role in how an individual makes sense of a health event (Collie & Long, 2005). For example, expectations about the appropriate timing of health events have been suggested to explain why those who experience a cancer-related event at younger ages report stronger emotional responses such as worry than those who experience the same event at older ages (Costello & Boblin, 2004; Wenzel et al., 1999).
To explore the occurrence of teachable moment domains and consider their role in motivating behavior change, we analyzed baseline and 8-month follow-up data from a two-site randomized intervention trial, Project PREVENT, described elsewhere (Emmons et al., 2005). The trial evaluated a proactively delivered intervention offered to patients in the weeks following identification of pre-cancerous colon polyps. A combined screening/baseline survey that occurred within 4 weeks following polyp removal enabled assessment of numerous cognitive and affective variables. The intervention recommended and aided lifestyle changes such as smoking cessation, improved diet, and increased physical activity via the opportunity to participate in multiple telephone counseling sessions. Results of this trial described elsewhere indicated a significant benefit of the intervention over usual care in prompting changes in multiple health behaviors (Emmons et al., 2005).
The current report addresses the question of whether and how the teachable moment- and sociodemographic domains proposed above might have influenced study participants’ response to polyp diagnosis. Because the baseline survey included only an event-specific subjective measure of worry and not perceived risk or self-identity we tested the prospective association of colon cancer worry with a created variable we called “intervention buy-in” to indicate participants’ subjective response to polyp diagnosis. We then explored how indicators of the two other teachable moment domains, that is, personal risk factors, health-related self-identity and sociodemographic domains influenced intervention buy-in. We hypothesized that those for whom the event prompted greater affect in the form of colon cancer worry would buy in most to the intervention, and that personal risk factors, health-related self-identity, and sociodemographic characteristics would be significant determinants of worry and therefore intervention buy-in.
Methods
Project prevent
The study sample included patients who had undergone either flexible sigmoidoscopy or colonoscopy through the gastroenterology department in four health care systems, two in Massachusetts and two in North Carolina. Eligibility criteria included: (a) having an adenomatous colon polyp removed within 4 weeks of recruitment, (b) having no personal history of colorectal cancer, (c) being age 40–75 years, (d) being able to read and speak English, (e) being mentally capable of informed consent, and (f) being reachable by telephone. Institutional review boards at all participating institutions approved the study methods.
From the participating health systems’ databases, 1979 patients were identified as potentially eligible from fall of 1999 through the fall of 2001. Approximately 1 week after notification of their colonoscopy results, these patients received an introductory letter about the study signed by one of the study gastroenterologists. The letter introduced the project and gave potential participants an 800 number to call to refuse participation. Afterwards, a survey research firm telephoned patients who did not refuse contact in order to confirm eligibility, obtain verbal consent and complete the baseline survey. Of those sampled, 115 people were determined to be ineligible, and 192 were unreachable during the study contact window. Of the 1672 eligible people contacted, 425 (25%) refused to participate. The final sample comprised 1247 participants who completed the baseline survey.
Participants who agreed to participate were stratified by site (North Carolina vs. Massachusetts), ages (40–59 and 60+) and gender, and randomly assigned within strata to either the Project PREVENT Intervention (PREVENT, N = 591) or Usual Care (UC, N = 656). The final assessment of behavior change outcomes occurred 8 months after the baseline survey. The Usual Care condition received the standard of care offered by the participating health systems that included notification of colon polyps in the form of a letter signed by the gastroenterologist and sent to the patient within 2 weeks following the polypectomy. The letter informed patients about their polyp and the length of time until their next screening, typically 3–5 years, and included brief information about the risk behaviors that contribute to colon cancer risk.
The PREVENT Intervention was designed to promote change across multiple health behaviors simultaneously. The intervention was grounded in Bandura’s (1986) Social Cognitive Theory which suggests that health habits have common underpinnings, namely a constellation of intrapersonal (e.g., response- and self-efficacy), and interpersonal (e.g., social support) factors. Participants in the PREVENT condition received a proactively delivered intervention that included: (a) a motivational and goal-setting telephone session delivered by a health educator within 2 weeks after screening results were conveyed, (b) four follow-up telephone counseling calls at monthly intervals conducted over the 4 subsequent months, (c) computer-generated tailored print progress reports in tandem with the follow-up calls to reinforce their goals and address areas that needed further consideration, (d) tailored self-help materials containing customized graphs that displayed the participant’s current status and the recommended levels for each of six risk factors (red meat, fruit and vegetables, alcohol, multivitamin, physical activity, and smoking), (e) personalized suggestions for strategies that could help the individual jointly accomplish recommended changes in all of their identified risk behaviors, (f) a logbook (e.g., a personal diary for the participant to record their goals, keep track of their progress, and keep “to do” lists) and (g) behavior-specific tip sheets (e.g., smoking cessation guide, a walking for fun and fitness brochure, and common questions about multivitamin use). Health advisors based in North Carolina and Massachusetts delivered the intervention. After each counseling call, health advisors sent materials summarizing the calls and goals. Health advisors from all sites were trained together, and received 16 h of training and ongoing supervision from an expert in motivational interviewing.
The outcomes of the randomized trial are reported elsewhere (Emmons et al., 2005). Briefly, just one-third of the Usual Care participants dropped any risk factors during the study period compared with almost half of the PREVENT Intervention participants. Almost 20% of the Usual Care group added a risk factor during the study period compared with 10% of the PREVENT participants. PREVENT participants were significantly more likely to change more than one behavior than the Usual Care group.
Measures
Data collection was via telephone surveys at baseline which occurred within 4 weeks of notification of results, and a follow-up survey conducted 8 months after completion of the baseline survey. All independent variables (i.e., colon cancer worry, personal risk factors, health-related self-identity, and sociodemographics) were assessed as part of the baseline survey. Intervention buy-in was averaged over the duration of the 4-month survey as described below.
Intervention “buy-in”
Participants in the PREVENT Intervention were assigned a health advisor who attempted to complete five calls with the same participant. For each participant, the number of completed counseling calls (0–5) was recorded automatically as part of a computerized telephone counseling system. Additionally, at the completion of each of the counseling sessions, the health advisor rated the level of engagement the participant showed during the call on a five-point scale (0 = none to 4 = complete). The reliability of these subjective ratings was not assessed, serving only as a rough indicator of counseling session quality. An “average engagement rating” was calculated by averaging the engagement ratings across the calls completed over a 4-month period. Based on the frequency distributions of average engagement, a categorical buy-in variable was created by assigning those respondents with an average subjective engagement rating less than 0.5 across all completed sessions to a “no buy-in” category. Similarly, those respondents with an average engagement rating greater than 4 were assigned to “total intervention buy-in”. All other participants were categorized as demonstrating “some buy-in”.
Colon cancer worry
Participants were asked to rate on an 11-point scale (0 = not at all concerned to 10 = extremely concerned) their level of concern about developing colon cancer in the future.
Personal risk factors
Participants were asked if they had a family history of colon cancer, that is, any blood relatives who were diagnosed with colorectal cancer, and whether they, themselves, had ever in the past had colon polyps identified. Additionally, a categorical measure was used to summarize six behavioral risk factors (Emmons, Marcus, Linnan, Rossi, & Abrams, 1994). The computed multiple risk factor index included: current smoking status (smoking, not smoking), consumption of fewer than five servings of fruits and vegetables per day, consumption of more than three servings per week of red meat, taking a multi-vitamin less than 7 days per week, drinking more than one (women) or two (men) servings of alcohol per day, and exercising at least moderately less than 150 min per week. Participants received a score of 1 if they had the risk factor and a score of 0 if they did not have the risk factor. The individual risk factor scores were then summed to yield a categorical multiple risk factor index (0 = no risk factors to 6 = all risk factors). These categorizations were based on what is generally accepted in the field as the minimum requirements for risk factor reduction and/or cardio-respiratory benefit. Each of the six risk factors was assessed using well-validated behavioral assessments as described elsewhere (Emmons et al., 2005).
Health-related self-identity
Participants were asked to rate their current health as excellent, good fair or poor. Self-rated health has been argued not only to provide an objective measure of health status but also indicate a subjective consciousness or self-schema related to health, that is, knowledge or appraisals about the self with respect to personal health (Bailis, Segall, & Chipperfield, 2003; Sillen, Nilsson, Mansson, & Nilsson, 2005; Stein, Roeser, & Markus, 1998). Additionally, the 11-item version of the Older American Resources and Services (OARS) questionnaire assessed co-morbid conditions (Fillenbaum, 1988). Using this scale, participants were asked to indicate the presence or absence of major chronic medical conditions (range 0–10) such as stroke, cancer, diabetes, heart disease, or lung disease. These types of health-related self-schemas have been shown to influence information processing about the self (Stein et al., 1998).
Sociodemographics
Automated health system records provided age and gender data. As part of the baseline survey, participants were asked their race-ethnicity, education level, household income, and marital status.
Analysis
The analysis was intended to address two objectives. The first was to evaluate the association of participants’ level of concern for developing colon cancer (worry) as a mediator of their level of buy-in to the intervention while considering the influence of the other teachable moment domains—personal risk factors, and health-related self-identity—and other sociodemographics (age, gender, education, study site and race-ethnicity). The second was to characterize the factors that were associated with participants’ worry. Analyses were restricted to the 591 individuals who were randomly assigned to the PREVENT Intervention condition. Teachable moment domains (colon cancer worry, personal risk factors, and health-related self-identity) and sociodemographics were tested in multivariate analyses to predict intervention buy-in.
Results
Contextual characteristics
Most participants were White (82%), married (76%), and had at least a high school education (74%). About half were female 44% and had incomes greater than $45,000 (57%). The mean age was 60 years (S.D. = 8.5) (see Table 1). Participants reported an average of two behavioral risk factors, with about half of the sample reporting three or more behavioral risk factors. Half of participants reported their health to be good, with another third reporting excellent health. Over 75% reported at least one chronic disease, one-quarter reported a family history of colon cancer, one-third had a personal history of colon polyps, and 12% had both, suggesting moderate to high risk for colon cancer. With respect to intervention engagement, 60% of the participants were characterized as having “total buy-in”, 22% had some- and 17% had no buy-in to the PREVENT Intervention. With respect to worry, 62% reported moderate concern (⩾ 5 on 11-point scale) that they might get colon cancer in the future, and 24% expressed high levels of concern (> 7 on 11-point scale).
Table 1.
Characteristics of the sample (N = 591)
| Percent or mean (S.D.) |
|
|---|---|
| Age (M, S.D.) | 60 (8.5) |
| Age 40–59 | 46 |
| Age 60+ | 54 |
| Female | 44 |
| Race/ethnicity | |
| White | 82 |
| African American | 12 |
| Other | 5 |
| Married or living as married | 76 |
| > High school education | 74 |
| Income > $45,000a | 57 |
| Family history of colon cancer | 30 |
| History of polyps | 34 |
| Number of behavioral risk factors (M, S.D.) | 2.5 (1.3) |
| Have three or more risk factors | 49 |
| Self-rated health | |
| Excellent | 33 |
| Good | 48 |
| Fair/poor | 19 |
| Have a chronic disease | 78 |
| Intervention buy-inb | |
| Total | 60 |
| Some | 22 |
| None | 17 |
| Concerned might get colon cancerc | 62 |
DK/Ref. included as a response category rather than counted as missing.
Average engagement <0.5 = none; average engagement >4 = total; everyone else = some.
Those who responded 5 or above on a scale of 1–10.
Multivariate model testing the effect of cancer worry on intervention buy-in
We created a multivariate ordinal logistic model that tested colon cancer worry and included other baseline contextual factors to predict intervention buy-in (none, some or total buy-in) among participants in the PREVENT Intervention group. The analysis evaluated the association between buy-in and worry (represented by level of concern about getting colon cancer in one’s lifetime) as well as personal risk (represented by family history of colon cancer, having been previously diagnosed with polyps, and number of baseline risk factors), and health-related self-identity (represented by self-rated health, and the number of chronic illnesses as indicated by the OARS). Initial analysis of contingency tables relating buy-in to the various sociodemographic variables listed above, indicated that only gender, site and race showed any association with buy-in. This subset of sociodemographic variables was included in an ordinal logistic model along with the independent variables colon cancer worry, personal risk factors, and health-related self-identity to predict intervention buy-in. After iteratively eliminating independent variables that were not statistically significant, namely, family history of colon cancer (p = 0.58), self-reported health (p = 0.16), age (p = 0.95), and education (p = 0.39), the final model results are shown in Table 2. The constructed model was based on the proportional odds assumption that implies common coefficient estimates.
Table 2.
Multivariate logistic regression model to predict intervention “buy-in”a
| Variable | Odds ratio |
Confidence interval |
p- Value |
|---|---|---|---|
| Worry | 1.07 | (1.02, 1.14) | 0.011 |
| North Carolina site | 1.89 | (1.32, 2.69) | 0.000 |
| Male gender | 0.69 | (0.48, 0.99) | 0.045 |
| Baseline total risk factors | 0.75 | (0.65, 0.86) | 0.011 |
| Race, White | 1.57 | (1.01, 2.45) | 0.045 |
N = 537 with complete data.
Variable computed based on number of counseling calls completed and interventionists’ subjective rating of engagement in calls to yield a continuous score of 0–6 then categorized in tertiles: 0 = no buy-in, 1 = some buy-in, 2 = total buy-in.
These results suggest as hypothesized that a higher level of worry at baseline was significantly associated with greater intervention buy-in. Additionally, a greater number of behavioral risk factors reported at baseline were significantly and negatively associated with buy-in, such that those who had more risk behaviors to change were least engaged in the intervention. Additionally, those participants in North Carolina, who were female and White, were more likely than those in Massachusetts, who were male or were non-White to buy-in to the intervention for the same levels of worry and number of risk factors.
Factors characterizing those who were most worried by polyp identification
A logistic regression analysis was tested with the binary value of worry (0–4 = not worried, 5–10 = worried) because the cancer worry measure was not normally distributed. Independent variables included health-related self-identity, personal risk factors, gender, age and site. Family history of colon cancer (p = 0.19), site (p = 0.43) and number of behavioral risk factors (p = 0.78) were not significantly related to worry and were removed from the model. The subsequent model was significant (p <0.0001) and showed that age and gender both were associated with levels of cancer worry (see Table 3). Those who were younger and female reported greatest worry about developing colon cancer in the future. Moreover, those who reported being in poor health were more worried than those who perceived themselves to be healthier. Those who had had a previous polyp diagnosis also were significantly more worried than those for whom this was their first diagnosis. We replicated analyses with colon cancer worry as a continuous variable and found similar results except that race was a significant predictor of worry and gender was not.
Table 3.
Multivariate logistic regression model to predict worrya about future colon cancer
| Variable | Odds ratio |
Confidence interval |
p- Value |
|---|---|---|---|
| Health status | |||
| Excellent vs. fair/poor | 0.36 | (0.21, 0.61) | 0.000 |
| Good vs. fair/poor | 0.54 | (0.32, 0.90) | 0.018 |
| Age 40–59 | 1.71 | (1.19, 2.45) | 0.003 |
| Male gender | 0.62 | (0.44, 0.89) | 0.009 |
| Prior polyp diagnosis | 1.84 | (1.25, 2.71) | 0.002 |
N = 591 with complete data.
Worry about colon cancer original scale 0–10 dichotomized due to non-normal distribution at 0–4 = not worried, 5+ = worried.
Discussion
Overall, a sizable subset of individuals diagnosed with pre-cancerous colon polyps participated more in an offered intervention to lower their risk of colon cancer and reported more worry related to the event than their contemporaries. This is good news considering that the majority had risk profiles suggesting they could benefit from health behavior change, and the intervention was associated with significant reductions in risk factors when compared to usual care (Emmons et al., 2005).
Several contextual factors influenced whether polyp identification influenced levels of intervention participation. Consistent with the teachable moment heuristic, those who reported the most worry engaged most with the intervention. However, increased personal risk factors as indicated by number of baseline risk behaviors was negatively associated with intervention participation. Counter to what we would have predicted, this suggests that having more risk factors to change might have diminished the motivational potential of the health event. Individuals may have felt fatalistic about their risk status, and polyp identification rather than motivating them to participate in the intervention may have prompted them to cope by de-emphasizing the threat potential (Taylor, 1991). Unfortunately, our measures did not enable us to explore this possibility.
It is interesting and a little perplexing that for the most part the variables that predicted intervention buy-in were not associated with colon cancer worry. For example, being younger, female and perceiving one’s self to be in poorer health were associated with greater levels of cancer worry; but of these variables only female gender was associated with greater intervention buy-in. Additionally, those who had prior experience with the health threat, were more worried about getting colon cancer, but were not more likely to participate fully in the intervention. More comprehensive assessments of affective response such as the positive and negative affect scale (see for example, Vastfjall, Friman, Garling, & Kleiner, 2002) or others that enable characterization of a fuller spectrum of event-specific emotions could lend insight into how health events are experienced. This would also enable us to understand better what circumstances prompt motivation to change as a coping response to health events.
As a group, men did not respond to the polyp diagnosis in a manner suggestive of a teachable moment: they were not as likely to engage in the intervention and they were not as likely to report being as worried as women were. Our pilot work related to couples and coping with negative health events (Lewis et al., 2006) also lent some insight into this finding. In interviewing the spouses of our participants, we found that men frequently had not told their wives about the polyp diagnosis whereas the converse was not true. Gender differences in affect experience and its influence on health outcomes have been reported (see for example, Rhudy & Williams, 2005). Broader assessments of affect might help illuminate if men’s reports of experiencing types of affect other than worry in the context of a health event might be capitalized on to encourage engagement in behavior change interventions.
There is no evidence to suggest that polyp diagnosis was perceived as a challenge to health-related self-identity among those who regarded themselves as healthy. Those who described themselves to be in excellent or good health were not more likely to buy into the intervention and were not more worried than their counterparts. This may be due to the fact that the measures we used were not specifically designed to assess this construct and may have been overly simplistic in characterizing the complex nature of self-identity. The finding that the younger were more worried than the older individuals suggests that age may have captured a domain of self-identity that the measure of perceived health did not. The role of self-related identity and how it might be influenced by health events and capitalized upon by interventions merits further study.
Lastly, these data suggest that the oldest individuals, minorities and those with the greatest risk factors may not experience relatively minor health events such as a polypectomy as a teachable moment. In this multi-site study, we also considered site was a proxy for sociodemographic context. Participants from the North Carolina site were more likely to be African American, had lower education and income, and reported poorer health status than those from Massachusetts (Emmons et al., 2005). In a previous report on the baseline data (Clipp et al., 2004), we found that older patients reported more age-related physical, social and economic vulnerabilities, and in turn, were less motivated to reduce their risk and less confident that their behavior change efforts would succeed. This is concerning when one considers the growing evidence to suggest that even small reductions in health risks among those with chronic illness can yield improvements in quality of life and reductions in mortality (e.g., Lorig et al., 2001). Further exploration of factors that may make health events more salient for risk reduction among this sub-sample should be explored. Consideration of the demoralizing effects of the context in which these health events occur also will be critical.
In considering these outcomes, a number of study limitations should be noted. The majority of participants in the sample were White, and thus, the results may not readily generalize to populations that are more racially and ethnically diverse. The measures of the proposed constructs of the teachable moment were predominantly single item measures, although these measures are used widely in this fashion. However, measuring cancer-related affect with a single measure clearly does not capture the complexity of the construct. Moreover, we did not assess the broader set of affective responses that have been noted for cancer-related health events (see for example, Sears, Stanton, & Danoff-Burg, 2003). Similarly, our measures of self-identity using self-reported health status and reported chronic illness does not capture the diversity of self-identity such as constructs of “hoped for” and “future self” that have been shown previously to be associated with health outcomes (Black et al., 2001). Further research employing multi-item and validated measures is needed to get inside the black box of the teachable moment. However, the study has a number of notable strengths including its large sample size, assessment of multiple psychosocial domains, and prospective design.
Future research is needed to understand how contextual factors may strengthen or undermine the motivational potential of health events and their likelihood to become teachable moments. In particular, research might move beyond negative affect towards understanding the broad range of possible affective responses to health events. Moreover, consideration of factors related to self-identity might be informative in attracting individuals to self-help interventions. Fuller consideration of these factors may lend insight into how to engage more men in behavior change interventions. Future research also might consider other contextual factors such as the role that coping plays in how individuals respond to a threatening health event. For example, if individuals typically rely on active coping they may be more likely to participate in a proactively offered intervention than if they typically engage in avoidance coping. Additionally, consideration of individual’s baseline knowledge about how to remediate the health threat also could influence receptivity to interventions. If individuals feel like they know what they need to do to reduce risk, they may be disinclined to participate in an intervention. Advancement in this area of research could be used to increase the efficacy and efficiency of behavior change interventions and in so doing, increase their potential for public health benefit.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aspinwall LG, Brunhart SM. Distinguishing optimism from denial: Optimistic beliefs predict attention to health treats. Personality and Social Psychology Bulletin. 1996;22:993–1003. [Google Scholar]
- Aspinwall LG, Taylor SE. A stitch in time: Self-regulation and proactive coping. Psychology Bulletin. 1997;121:417–436. doi: 10.1037/0033-2909.121.3.417. [DOI] [PubMed] [Google Scholar]
- Bailis DS, Segall A, Chipperfield JG. Two views of self-rated general health status. Social Science & Medicine. 2003;56:203–217. doi: 10.1016/s0277-9536(02)00020-5. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall Inc.; 1986. [Google Scholar]
- Black ME, Stein KF, Loveland-Cherry CJ. Older women and mammography screening behavior: Do possible selves contribute? Health Education and Behavior. 2001;28:200–216. doi: 10.1177/109019810102800206. [DOI] [PubMed] [Google Scholar]
- Carlos RC, Underwood W, III, Fendrick AM, Bernstein SJ. Behavioral associations between prostate and colon cancer screening. Journal of the American College of Surgeons. 2005;200(2):216–223. doi: 10.1016/j.jamcollsurg.2004.10.015. [DOI] [PubMed] [Google Scholar]
- Clipp EC, Carver EH, Pollak KI, Puleo E, Emmons KM, Onken J, et al. Age-related vulnerability of older adults with colon adenomas. Cancer. 2004;100(5):1085–1094. doi: 10.1002/cncr.20082. [DOI] [PubMed] [Google Scholar]
- Collie K, Long BC. Considering ‘meaning’ in the context of breast cancer. Journal of Health Psychology. 2005;10:843–853. doi: 10.1177/1359105305057318. [DOI] [PubMed] [Google Scholar]
- Consedine NS, Magai C, Krivoshekova YS, Ryzewicz L, Neugut AI. Fear, anxiety, worry and breast cancer screening behavior: A critical review. Cancer Epidemiology, Biomarkers & Prevention. 2004;13:501–510. [PubMed] [Google Scholar]
- Costello JA, Boblin S. What is the experience of men and omen with congestive heart failure? Canadian Journal of Cardiovascular Nursing. 2004;14(3):9–20. [PubMed] [Google Scholar]
- Emmons KM, Marcus BH, Linnan L, Rossi JS, Abrams DB. Mechanisms in multiple risk factor interventions: Smoking, physical activity, and dietary fat intake among manufacturing workers. Working Well Research Group. Preventive Medicine. 1994;23(4):481–489. doi: 10.1006/pmed.1994.1066. [DOI] [PubMed] [Google Scholar]
- Emmons KM, McBride CM, Puleo E, Pollak KI, Clipp E, Kuntz K, et al. Project PREVENT: A randomized trial to reduce multiple behavioral risk factors for colon cancer. Cancer Epidemiology Biomarkers & Prevention. 2005;14:1453–1459. doi: 10.1158/1055-9965.EPI-04-0620. [DOI] [PubMed] [Google Scholar]
- Esler JL, Bock BC. Psychological treatments for noncardiac chest pain: Recommendations for a new approach. Journal of Psychosomatic Research. 2004;56(3):263–269. doi: 10.1016/S0022-3999(03)00515-4. [DOI] [PubMed] [Google Scholar]
- Eysenck MW. Anxiety: The cognitive perspective. Hove, UK: Erlbaum; 1992. [Google Scholar]
- Fife BL. The role of constructed meaning in adaptation to the onset of life-threatening illness. Social Science & Medicine. 2005;61(10):2132–2143. doi: 10.1016/j.socscimed.2005.04.026. [DOI] [PubMed] [Google Scholar]
- Fillenbaum GG. Multidimensional functional assessment of older adults. Hillside, NJ: Erlbaum Associates; 1988. [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Folkman S, Moskowitz JT. Positive affect and the other side of coping. American Psychologist. 2000;55:647–654. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- Frijda NH. The emotions. Cambridge: Cambridge University Press; 1986. [Google Scholar]
- Gladstone G, Parker G. What’s the use of worrying? Its function and dysfunction. Australian and New Zealand Journal of Psychiatry. 2003;37:347–354. doi: 10.1046/j.1440-1614.2003.01187.x. [DOI] [PubMed] [Google Scholar]
- Gorin AA, Phelan S, Hill JO, Wing RR. Medical triggers are associated with better short-and long-term weight loss outcomes. Preventive Medicine. 2004;39(3):612–616. doi: 10.1016/j.ypmed.2004.02.026. [DOI] [PubMed] [Google Scholar]
- Hay JL, Buckley TR, Ostroff JS. The role of cancer worry in cancer screening: A theoretical and empirical review of the literature. Psycho-Oncology. 2004;14(7):517–534. doi: 10.1002/pon.864. [DOI] [PubMed] [Google Scholar]
- Jannoff-Bulman R, Frieze I. The role of gender in reactions to criminal victimization. New York: Free Press; 1987. [Google Scholar]
- Lazarus RS. Coping theory and research: Past, present and future. Psychosomatic Medicine. 1993;55:234–247. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, Emmons KM. Understanding health behavior change among couples: An interdependence and communal coping approach. Social Science & Medicine. 2006;62(6):1369–1380. doi: 10.1016/j.socscimed.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Lipkus IM, Klein WMP. Effects of communicating social comparison information on risk perceptions for colorectal cancer. Journal of Health Communication. 2006;11:391–407. doi: 10.1080/10810730600671870. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Jr, Bandura A, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001;39(11):1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: The case of smoking cessation. Health Education Research. 2003;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- Ouellette JA, Hessling R, Gibbons FX, Reis-Bergan M, Gerrard M. Using images to increase exercise behavior: Prototypes versus possible selves. Personality and Social Psychology Bulletin. 2005;31(5):610–620. doi: 10.1177/0146167204271589. [DOI] [PubMed] [Google Scholar]
- Rhudy JL, Williams AE. Gender differences in pain: Do emotions play a role? Gender in Medicine. 2005;2(4):208–226. doi: 10.1016/s1550-8579(05)80051-8. [DOI] [PubMed] [Google Scholar]
- Satia JA, Kristal AR, Curry S, Trudeau E. Motivations for healthful dietary change. Public Health Nutrition. 2001;4(5):953–959. doi: 10.1079/phn2001157. [DOI] [PubMed] [Google Scholar]
- Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping and posttraumatic growth in women with early stage breast cancer. Health Psychology. 2003;22(5):487–497. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- Sillen U, Nilsson JA, Mansson NO, Nilsson PM. Self-rated health in relation to age and gender: Influence on mortality risk in the Malmo Preventive Project. Scandinavian Journal of Public Health. 2005;33(3):183–189. doi: 10.1080/14034940410019235. [DOI] [PubMed] [Google Scholar]
- Steele CM. The psychology of self-affirmation: Sustaining the integrity of the self. In: Berkowitz L, editor. Advances in experimental social psychology: Social psychological studies of the self: Perspectives and programs. Vol. 21. San Diego, CA: Academic Press Inc.; 1988. pp. 261–302. [Google Scholar]
- Stein KF, Roeser R, Markus HR. Self-schemas and possible selves as predictors and outcomes of risky behaviors in adolescents. Nursing Research. 1998;47(2):96–106. doi: 10.1097/00006199-199803000-00008. [DOI] [PubMed] [Google Scholar]
- Taylor SE. Asymmetrical effects of positive and negative events: The mobilization-minimization hypothesis. Psychological Bulletin. 1991;110:67–85. doi: 10.1037/0033-2909.110.1.67. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Kemeny ME, Reed GM, Bower JE, Gruenewald TL. Psychological resources, positive illusions, and health. American Psychologist. 2000;55:99–109. doi: 10.1037//0003-066x.55.1.99. [DOI] [PubMed] [Google Scholar]
- Tennen H, Affleck G. The costs and benefits of optimistic explanations and dispositional optimism. Journal of Personality. 1987;55(2):376–393. doi: 10.1111/j.1467-6494.1987.tb00443.x. [DOI] [PubMed] [Google Scholar]
- Vastfjall D, Friman M, Garling T, Kleiner M. The measurement of core affect: A Swedish self-report measurederived from the affect circumplex. Scandinavian Journal of Psychology. 2002;43(1):19–31. doi: 10.1111/1467-9450.00265. [DOI] [PubMed] [Google Scholar]
- Weick K. The collapse of sensemaking in organizations: The Mann Gulch disaster. Administrative Science Quarterly. 1993;38:628–652. [Google Scholar]
- Weinstein ND. The precaution adoption process. Health Psychology. 1988;7:355–386. doi: 10.1037//0278-6133.7.4.355. [DOI] [PubMed] [Google Scholar]
- Wenzel LB, Fairclough DL, Brady MJ, Cella D, Garrett KM, Kluhsman BC, et al. Age-related differences in the quality of life of breast carcinoma patients after treatment. Cancer. 1999;86(9):1768–1774. [PubMed] [Google Scholar]
- Witte K. Fear as motivator, fear as inhibitor: Using the extended parallel process model to explain fear appeal successes and failures. In: Anderson PA, Guerrero LK, editors. Handbook of communication and emotion: Research, theory, applications and contexts. New York, NY: Academic Press; 1998. [Google Scholar]