Abstract
Objectives
The aim of the study was to determine the short-term impact of a 7-month whole-school physical activity and healthy eating intervention (Action Schools! BC) over the 2007–2008 school year for children and youth in 3 remote First Nations villages in northwestern British Columbia.
Study design
A pre-experimental pre/post design was conducted with 148 children and youth (77 males, 71 females; age 12.5±2.2 yrs).
Methods
We evaluated changes in obesity (body mass index [wt/ht2] and waist circumference z-scores: zBMI and zWC), aerobic fitness (20-m shuttle run), physical activity (PA; physical activity questionnaire and accelerometry), healthy eating (dietary recall) and cardiovascular risk (CV risk).
Results
zBMI remained unchanged while zWC increased from 0.46±1.07 to 0.57±1.04 (p<0.05). No change was detected in PA or CV risk but aerobic fitness increased by 22% (25.4±15.8 to 30.9±20.0 laps; p<0.01). There was an increase in the variety of vegetables consumed (1.10±1.18 to 1.45±1.24; p<0.05) but otherwise no dietary changes were detected.
Conclusions
While no changes were seen in PA or overall CV risk, zWC increased, zBMI remained stable and aerobic fitness improved during a 7-month intervention.1
Keywords: physical activity, aerobic fitness, cardiovascular risk, children, Aboriginal, nutrition
While 26.3% of Canadian children and youth are overweight or obese, 34.5% of off-reserve Aboriginal young people are considered overweight or obese (1). Preliminary results of the 2008 First Nations Regional Longitudinal Health Survey suggest that 56% of children and 43% of youths living in Canadian First Nations communities are either overweight or obese, but obesity levels vary considerably by region (2). In specific First Nations communities the rate of on-reserve Canadian Aboriginal pediatric obesity and overweight has been reported as varying widely from 38% to as high as 70% (3,4). Obesity not only tracks from childhood into adulthood (5) but adults who were obese during childhood also have an increased risk of developing chronic diseases (6). Aboriginal people in Canada suffer from obesity-related conditions such as diabetes, hypertension and heart disease at 2–3 times the rates of the general population (7). Clearly, something must be done to reverse this trend.
The school environment is an attractive context to promote healthy eating (HE), obesity prevention and physical activity (PA) as children from diverse ethnic and socio-economic strata spend 5 or more hours per day in school (8). Elementary-school-based interventions have successfully increased the amount of PA undertaken during school time (9–11) and have improved dietary habits (12–14).
Action Schools! BC (AS!BC), as described in detail by Naylor et al. (15), is a whole-school framework for action on PA and HE. Efficacy of the model for improving a host of chronic disease risk factors was established in an urban setting in British Columbia (13,15–17). Although the model included Aboriginal children residing and attending school in urban communities, the initiative did not explicitly target issues and contexts specific to Aboriginal children. In response to concerns about type 2 diabetes and obesity among their children (18), 3 remote Tsimshian Nation communities collaborated with the AS!BC team to implement and evaluate the AS!BC intervention and measurement tools to understand its impact within the specific context of rural, remote Aboriginal communities.
Therefore, our aim was to determine the short-term impact of the AS!BC intervention in 3 rural, remote northern Aboriginal communities. Specifically, we addressed the question: Is there a significant change in health outcomes (obesity-related body composition, PA levels, aerobic fitness, CV risk and HE) for First Nations children and youth living in rural and remote northern communities after participation in AS!BC for 7 months?
Materials and Methods
Study design and population
Our study was part of a larger community-based participatory action research project. The initiative was undertaken in response to an invitation from 3 First Nations communities in northwestern British Columbia based on: (i) their longstanding relationship with a clinician-researcher on our team; and (ii) their concern regarding the elevated risk of diabetes in their communities (18). As a result of the unique relationship and context, we implemented a pre-experimental pre/ post design to conduct our study.
Recruitment and participants
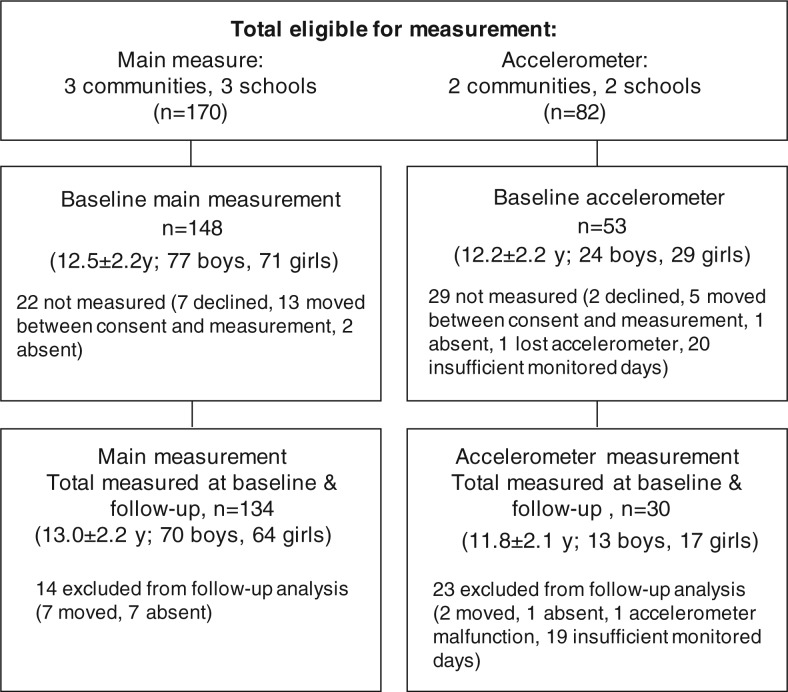
We received approval from the University of Victoria Human Research Ethics Board, the University of British Columbia Clinical Research Ethics Board and the Children's and Women's Research Review Committee to conduct the study. We also received approval and support from elected Band Councils, hereditary band elders, hereditary band chiefs, community health directors, school administrators and our target communities to undertake our study in their communities. We obtained written informed consent from parents or caregivers; the children provided verbal and written assent. The process we adopted to acquire consent/assent, to obtain community approval and to travel to very remote locations to undertake this project is described in more detail elsewhere (19). We invited all children in grades 4–12 at each of the schools (n=3) in the 3 communities to participate. Of the 170 eligible participants, 163 consented to participate (96%), with 148 measured at baseline and 134 at follow- up. Details of the recruitment and reasons for dropping out are displayed in Figure 1.
Fig. 1.
Participation numbers and reasons for exclusion from measurement over the 7-month intervention.
Action Schools! BC intervention
We have described the AS!BC model in detail elsewhere (15) and have also described its implementation in these 3 communities (20). Briefly, AS!BC is a whole-school model that integrates classroom-based HE education and PA opportunities with recess and after-school activities, and environmental change strategies (e.g., playground equipment) with family and community elements (e.g., school spirit and family events) in order to promote healthy living. A primary feature of the AS!BC model is that it is tailored by each school and teacher according to their context. AS!BC advocates that children should accrue 150 minutes of PA per week during school hours. As well as regular physical education classes (typically 75–80 minutes/week), teachers in the program incorporated an additional 15 minutes per day of teacher-selected, classroom-based PA into their school regimen. For the HE component, teachers strove to incorporate at least one HE activity per month into the “classroom action zone” and implemented a fruit and vegetable (FV) and a sugar-sweetened beverage (SSB) campaign into their classroom or school. To facilitate classroom activities, the AS!BC Support Team (who travelled 3 times by seaplane to visit all of the schools) customized the model with teachers and provided an “Action Bin” replete with classroom PA and HE equipment and resources that teachers needed to deliver their customized model. The AS!BC Support Team also provided support to teachers to enhance the likelihood of successful implementation and sustain-ability (20).
Measurement
We assessed children and youth at baseline (September 2007) and again at 7 months following the school-based intervention (April or May 2008). All measurements were conducted at local schools during regular school hours by the same team of university researchers who travelled by seaplane to each of the communities.
Status of overweight and obesity
We assessed height, weight and waist circumference (WC) and calculated body mass index (BMI; kg/m2). We assessed height as stretched stature to the nearest 0.1 cm (Seca 214 Portable Stadi-ometer) and weight to the nearest 0.1 kg (Conair digital electronic scale). Height and weight were measured twice and we used the mean for analysis as per Canadian Society of Exercise Physiology protocol (21). We measured WC to the nearest 0.1 cm at the midpoint between the lowest rib and the iliac crest, at the end of normal expiration. To compare BMI and WC across time periods, we used age- and gender-specific z-scores (zBMI and zWC). zBMI was calculated as per the Centers for Disease Control method (22), with overweight defined as ≥85 percentile and obese as ≥95th percentile (23). zWC was determined from percentile values as per Fernandez et al. (24).
Physical activity (PA)
We estimated PA using a modified version of a valid and reliable tool for assessing moderate-to-vigorous PA (MVPA), the physical activity questionnaire for children (PAQ-c) or adolescents (PAQ-a) (25). We made minor changes to the PAQ by replacing 2 activities that were unavailable in the studied communities (ice hockey and ice skating) with 2 common, culturally oriented PA choices (e.g., seaweed gathering and traditional dance). A physical activity summary score (PA score) was calculated (25) with values ranging from 1 (low active) to 5 (very active). As well, we measured MVPA with GT1M acceler-ometers (Actigraph, Pensacola, FL) in a subset of participants. With a limited number of acceler-ometers and a high recruitment rate, participants from 2 of the 3 communities wore accelerometers for 5–7 days at each measurement period. Accel-erometers were programmed to collect activity counts every 15 seconds, and an age-specific regression equation (26) was used to estimate MVPA. We included all participants with at least 3 monitored days of 10 or more hours/day in our analysis. Our accelerometry protocol is described in detail elsewhere (27).
Aerobic fitness
To assess aerobic fitness, participants performed the Leger-Boucher 20-metre shuttle run as per standard protocol (28) in the school gymnasium; participants ran in groups of no more than 10 students. All participants were verbally encouraged throughout the procedure; the total number of laps completed by each student was recorded by the research assistant.
Cardiovascular risk (CV risk)
We assessed each child's BMI, WC, blood pressure (BP) and aerobic fitness to determine the percentage of participants with elevated CV risk factors. We measured BP 3 times on the left arm and used the mean of the final 2 measurements for analysis. Risk factors were considered elevated if: (i) BMI was greater than the age- and gender-specific 85th percentile (22); (ii) WC was greater than the age- and gender-specific 90th percentile (24); (iii) BP was greater than the age-, gender-and height-specific 90th percentile (29); or (iv) aerobic fitness laps were less than the age-and gender-recommended standards (30).
Healthy eating (HE)
HE was assessed using a validated 24-hour dietary recall (31) that a member of the research team administered to each participant individually. The EHSA Food Processor Nutrition and Fitness Software (v. 8.7, Salem, OR) was used to generate macro-nutrient servings and total kilocalories consumed. We used hand counting to tally the number of different fruits and vegetables (FV) consumed as well as to assess the number of FV and sugar-sweetened beverage (SSB) servings using the Canadian Nutrient File (32) for serving sizes.
Statistical analysis
We used Predictive Analytics SoftWare (PASW; v18.0, Chicago, IL) for statistical analyses. We used independent t-tests to compare descriptive characteristics between included (n=134) and excluded (n=14) participants, and paired t-tests to assess differences in outcomes at baseline and follow-up. We established the significance level a priori at p<0.05. To determine if maturation (growth and age) was related to the aerobic fitness outcome, we conducted Pearson product moment correlations and simple linear regression analyses where the independent variables were entered simultaneously.
Results
Reasons for participant exclusion are provided in Figure 1 and baseline participant characteristics are displayed in Table I. Participants ranged from 8.7 to 18.5 years. There were no differences at baseline between participants who were measured in both time periods (n=134) and those measured at baseline only (n=14 drop-outs) with the exception that the dropouts had higher aerobic fitness (32.7 versus 25.4 laps; p<0.05) and were older (14.3 versus 12.3 years; p<0.01).
Table I.
Participant characteristics at baseline
| Characteristic | All (n=133) | Males (n=70) | Females (n=63) |
|---|---|---|---|
| Age (years) | 12.4±2.2 | 12.6±2.0 | 12.1±2.3 |
| BMI (kg/m2) | 23.3±5.3 | 23.5±5.8 | 23.2±4.6 |
| % Overweight/Obesea | 51.4% | 48.1% | 54.9% |
| WC (cm) | 74.4±13.7 | 76.4±16.0 | 72.1±10.3 |
| Systolic BP (mm Hg) | 116.5±10.2 | 119.8±10.4 | 112.9±8.7b |
| Diastolic BP (mm Hg) | 61.9±7.7 | 62.6±7.1 | 61.2±8.2 |
BMI=body mass index (wt/ht2); WC=waist circumference; BP=blood pressure.
Obesity determined as per Centers for Disease Control (22).
p<0.05 for difference between males and females.
Status of overweight and obesity
Over one-half (51%) of participants were overweight or obese at baseline; 20% were overweight and 31% were obese (see Table I). Following the intervention, zBMI did not change; however zWC did increase (p<0.05) (see Table II).
Table II.
Baseline and follow-up anthropometric, physical activity, fitness and dietary variables
| Variable | Baseline | n | Follow-up | t | p |
|---|---|---|---|---|---|
| Anthropometrics: | |||||
| zBMI | 1.12±0.86 | 133 | 1.10±0.87 | 1.066 | 0.288 |
| zWC | 0.46±1.07 | 133 | 0.57±1.04 | −2.303 | 0.023 |
| zBP Systolic (mm Hg) | 0.85±0.80 | 131 | 1.00±0.90 | −1.790 | 0.076 |
| zBP Diastolic (mm Hg) | −0.10±0.67 | 131 | −0.18±0.69 | 1.116 | 0.267 |
| Physical activity & fitness: | |||||
| Aerobic fitness laps | 25.4±15.8 | 114 | 30.9±20.0 | −4.065 | 0.000 |
| PA Score | 2.75±0.72 | 134 | 2.83±0.79 | −1.449 | 0.150 |
| MVPA - overall (min/day) | 152.3±36.2 | 30 | 147.7±45.5 | 0.597 | 0.555 |
| - weekdays (min/day) | 166.5±40.4a | 30 | 161.3±51.9b | 0.613 | 0.545 |
| - weekends (min/day) | 120.2±41.9a | 19 | 133.0±48.6b | −1.23 | 0.234 |
| Dietary intake: | |||||
| Kcal/day | 1839.8±761.5 | 115 | 1730.2±744.2 | 1.418 | 0.159 |
| % Calories from carbohydrate | 58.9±11.9 | 115 | 59.5±12.4 | −0.355 | 0.724 |
| % Calories from sugar | 27.3±13.3 | 115 | 28.4±11.8 | −0.74 | 0.461 |
| % Calories from protein | 12.9±5.8 | 115 | 13.4±5.6 | −0.765 | 0.446 |
| % Calories from fat | 28.2±9.0 | 115 | 27.2±9.1 | 0.931 | 0.354 |
| FV servings/day | 2.75±2.45 | 115 | 3.21±3.20 | −1.306 | 0.194 |
| Vegetable servings/day | 1.31±1.7 | 115 | 1.48±1.55 | −0.807 | 0.421 |
| Fruit servings/day | 1.44±1.77 | 115 | 1.72±2.61 | −1.063 | 0.290 |
| # FV type | 2.07±1.55 | 115 | 2.39±1.90 | −1.528 | 0.129 |
| # Fruit type/day | 0.97±1.03 | 115 | 0.94±1.21 | 0.201 | 0.841 |
| # Vegetable type/day | 1.10±1.18 | 115 | 1.45±1.24 | −2.226 | 0.028 |
| SSB (mls/day) | 835.4±725.5 | 115 | 927.2±553.4 | −1.423 | 0.158 |
zBMI=body mass index (wt/ht2) z-score (23); zWC=waist circumference z-score (24); zBP=blood pressure z-score (29); PA Score=physical activity score; MVPA=moderate-to-vigorous physical activity; FV=fruit and vegetable; SSB=sugar-sweetened beverage.
p<0.001 for difference between weekdays and weekends.
p<0.001 for difference between weekdays and weekends.
Physical activity
Participants accumulated significantly less accelerometer MVPA during weekend days compared to weekdays at both baseline (−46.3 minutes; p<0.001) and follow-up (−28.3 minutes: p<0.001). No significant change in daily, weekday or weekend MVPA or in the PA score was detected after the 7-month intervention (see Table II).
Aerobic fitness and CV risk
Participants showed a substantial (22%) increase in aerobic fitness laps (p<0.001) (see Table II). Age and growth were not significant predictors of the change in aerobic fitness laps (F[2]=0.846, p=0.435). While we observed a significant decrease in the proportion of children and youth at risk for low aerobic fitness (from 57% to 45%; p<0.05), no other changes were seen in the CV risk profile (see Table III).
Table III.
Percentage of participants with CV risk factors at baseline and follow-up
| Variable | Baseline | n | Follow-up | t | p |
|---|---|---|---|---|---|
| % with a least 1 risk factor | 73.7% | 133 | 72.9% | 0.179 | 0.858 |
| % Overweight/Obesea | 52.2% | 133 | 53.4% | −0.818 | 0.783 |
| % High WC | 26.5% | 132 | 26.5% | 0.818 | 1.000 |
| % Elevated BP | 30.3% | 131 | 35.9% | −1.044 | 0.298 |
| % Low aerobic fitness | 57.3% | 96 | 44.8% | 2.319 | 0.023 |
WC=waist circumference; BP=blood pressure.
Obesity determined as per Centers for Disease Control (22).
Healthy eating
There was a significant increase in the variety of vegetables consumed at follow-up (1.10±1.18 to 1.45±1.24; p<0.05); otherwise, patterns of FV consumption, caloric intake and SSB consumption remained unchanged (see Table II).
Discussion
We previously reported in a randomized controlled trial that AS!BC implemented over 1 school year significantly enhanced aerobic fitness in mixed-ethnicity children attending urban schools (17). Here, we extend our previous work by evaluating the AS!BC model in 3 remote First Nations communities and show a similar cardiovascular benefit in Aboriginal children and youth. Specifically, participants improved their aerobic fitness laps by 22% after 7 months. To place this in context, the magnitude of change we observed in aerobic fitness after less than one year was similar to that seen in other nutrition and PA interventions; while minimal changes in aerobic fitness laps were seen in control groups, intervention groups saw significant increases in laps, with a 27% increase in laps for Crete school children over a similar time period (33), a 21% increase for Swiss children (34), a 20.4% gain for Canadian children living in an urban centre (17) and a similar gain in raw laps for a group of Australian children (35). Other nutrition and PA interventions—such as the Kahnawake Diabetes Prevention Program directed at a Canadian Mohawk community (36) and the Child and Adolescent Trial for Cardiovascular Health study (37)—have reported either no change or a decrement in aerobic fitness following intervention. We acknowledge the clearly established link between overweight/obesity and chronic disease in adults (38). Moreover, an independent, compelling and distinct relationship between aerobic fitness and all-cause mortality has also been established in adults (39). Indeed, in adults, a 1 metabolic equivalent (MET) increase in aerobic fitness decreased the risk of all-cause mortality by approximately 15%. While the 22% improvement in our lap score cannot be directly converted to METs, it does represent an average increased running time of over 40 seconds in a test where each additional 60 seconds of running represents a 1 MET increase in VO2max (28). Further, research supports the notion that, for young people, the harmful consequences attributed to overweight and obesity can be counteracted by having high levels of aerobic fitness (40). Thus, we consider the improved aerobic fitness in these First Nations children and youth to be an important finding.
Interventions directed at the primary prevention of diabetes or obesity in First Nations young people have been unsuccessful in their attempts to reduce the prevalence of overweight. The Pathways study showed no significant differences in BMI or percent fat between intervention and control American Indian children after 3 years, with BMI and percent fat increasing similarly in both groups (41). The Kahnawake diabetes prevention intervention study reported increased age-and gender-adjusted BMI in both elementary school control and intervention groups (36).
In other diabetes prevention studies with First Nations young people, mean BMI increased (42) or did not change (43), despite intervention. Thus, we view our outcome—where zBMI remained constant over the intervention period—as positive. While an average zBMI greater than 1 (as seen in our participants) is high, impeding the rise in BMI is an important first step in controlling obesity (23).
In spite of zBMI not changing, zWC increased, affirming the findings that WC may change independently of BMI (44). This may reflect the tendency of Aboriginals to accumulate fat centrally (45). Some studies suggested that WC was a better marker of CV risk factors than BMI in children and youth (46). Others (44) demonstrated that young people with a high BMI and high WC were twice as likely to have high triglyc-erides, high insulin levels and metabolic syndrome when compared to peers who had a normal WC but carried excess body weight. While 47% of participants in the current study had a normal BMI and normal WC, 29% had either a normal BMI and high WC or a high BMI and normal WC; 24% had both a high WC and high BMI. We share these findings with the caveat that we were unable to undertake ethnic-specific comparisons for WC as norms for Aboriginal children are unavailable.
As in previous studies, we observed no change in MVPA measured by accelerometry or questionnaire (9,17,41). Even when evaluating accelerometry within and outside of the school day (data not shown), no differences in MVPA were detected. We outlined a number of factors that may have influenced this finding. First, the weather at baseline was considerably warmer (13.4±1.2°C versus 8.9±3.0°C; p<0.001) and drier (43% versus 58% rain days; ns) (47) compared to follow-up. Since adolescents are more physically active on warmer days and on days with no rain (48), it is not surprising that MVPA remained unchanged at follow-up. Second, enthusiastic teachers began implementing the program before and during baseline measurement in spite of requests to wait until after baseline measurement. Regrettably, this could have elevated baseline MVPA levels, masking potential improvements in PA at follow-up. Third, 3 days of accelerometer monitoring may have been insufficient to capture habitual activity patterns (49). However, given our limited access to these remote communities and with relatively few participants wearing acceler-ometers for 4 or more days, we accepted a 3-day minimum for our analyses. Given the significant improvement we report for aerobic fitness, the PA measures we adopted may have lacked the sensitivity to capture the change in PA that likely mediated the aerobic fitness benefit.
To achieve a 22% improvement on the aerobic fitness test, frequency, duration and/or intensity of activity must have increased, even though our tools were unable to detect it. From the teachers' activity logs, as reported in Naylor et al. (20), it appears that extra classroom PA was delivered to participants. Classes averaged 75 minutes of weekly physical education plus an additional 65 minutes of PA outside of physical education classes. This classroom PA likely contributed to enhancing aerobic fitness; a similar dose of PA resulted in modest increases in steps for male students during our preliminary trial (10).
In terms of overall CV risk, almost three-quarters of participants had at least 1 of 4 CV risk factors both pre-and post-intervention (73.7% versus 72.9%; p>0.05). It is encouraging that the number of children and youth in the risk category for aerobic fitness decreased at follow-up, although we observed no improvements in the other risk categories. Comparing CV risk with other studies is difficult as there are many different risk variables, and cut-points for risk are not standardized. Even so, the results of our study are more alarming than results reported elsewhere. Ribeiro et al. (50), who assessed CV risk in 8–15-year-old Portugese youth, and Reed et al. (17), who assessed 9–11-year-old Canadian children, both found that approximately 50% of participants presented with at least 1 of 4 CV risk factors. Clearly, the Aboriginal young people in our study are at an unacceptably high health risk. Thus, minimizing cardiovascular and diabetes risk should be a major public health objective for this population.
We observed no change in SSB consumption and only a small improvement in FV intake. This may have been the result of too little time devoted to HE activities. Teacher logs indicated that an average of 15 minutes of HE activities was delivered twice per week over the year, including both the SSB and FV campaigns (20). Other successful FV interventions have dedicated 42–60 or more minutes per week to HE activities (12–14). While other successful nutrition/SSB interventions involved replacing sugar-sweetened soft drinks with diet (sugar-free) options at school (43) or at home (51), or by banning junk food sold or brought to school (52), ours involved classroom education and student tracking. We accept that the clinical relevance of increasing fruit and vegetable variety by just under half a fruit or vegetable each day is not clear. However, this small increase may prove a marker for a more substantial change in health behaviours that may ultimately lead to increased FV consumption and a better micronutrient profile over the students' lifespans. Anecdotal reports highlighted that fruits and vegetables were particularly vulnerable to transportation and storage issues in these remote communities.
One strength of our study was that it represented a “natural” experiment that illustrated the potential impact of a focused, comprehensive school health model within the context of remote Aboriginal communities and the challenges faced by teachers and students every day. Another strength was the high consent (96%) and participation (87%) rates that demonstrated the willingness of residents to participate in interventions that aim to promote child health. Furthermore, there was little apparent difference between participants measured at both time periods and those measured only at baseline.
Our findings should be interpreted in light of several limitations related to study design, measurement and the intervention itself. The most significant limitation was our inability to include a comparison group. Our research was based on a long-term partnership with the First Nations communities that we approached and all of these communities wished to be involved in the intervention. These partnerships are key to an ethical approach to working with Aboriginal communities in Canada (53). Thus, we were unable to recruit “comparator” communities with which we had no relationship and there was insufficient time to establish new relationships during the relatively short grant-funding time frame. Furthermore, each small community in our study was geographically and socially unique (20) thus it would not have been possible to find a representative comparison community.
Measurement limitations included the use of self-report to assess PA and HE. While the PAQ is a self-report measure, it has good internal consistency and validity compared with several other PA measures (25). To overcome issues related to self-reported PA, we also included an objective measure of PA in a subset of participants. However, extreme seasonal differences in weather and early uptake of the intervention by teachers may have influenced our ability to accurately assess change in PA. In addition, many participants failed to comply with accelerometry protocol (a daily wear period of >10 hours was required to be considered a valid day). This resulted in many follow-up files with less than 3 valid days; their data were excluded from analysis. By using a single dietary recall we may have misrepresented usual patterns of food consumption (54). Unfortunately, administering multiple dietary recalls was not possible given our travel constraints. In addition, 20% of the 24-hour recalls were carried out on a different day (weekend versus weekday) at baseline compared with follow-up. Finally, our findings related to overweight and obesity may be influenced by our use of zWC measurements that were based on non-Aboriginal population standards; fat distribution differs between non-Aboriginal and Aboriginal children (55).
Higher lap scores after the 7-month period may, in part, reflect normal growth and development of children. That said, changes in height and weight did not significantly affect the lap score (as per the regression analysis we performed). Further, when we used age-adjusted lap score cut-points to determine CV risk (30), the CV risk for low cardiovascular fitness had significantly decreased at follow-up (see Table III), confirming that critically low aerobic fitness had improved. Although improvements in the shuttle run may reflect enhanced motivation or effort, based on the magnitude of the increase it is unlikely that these factors alone explain the changes we observed.
Finally, our study may have been limited by the design of the intervention, which was developed for grades K-9. However, given the structure of schools in these remote northern communities, we administered the intervention to all grades. Naylor et al. (20) reported that some teachers from the higher grades were concerned about the potential for disruptive student behaviour, especially during the PA breaks, as a barrier to implementation of the model in older students.
Conclusion
In conclusion, it is imperative that effective strategies be devised to improve the health of children and youth residing in remote First Nations communities. In our study, the positive effect of AS!BC on aerobic fitness and the ability of this school-based model to stay the current upward trajectory of age-and gender-adjusted BMI in Aboriginal children and youth holds great promise for effectively enhancing the health of this population.
Acknowledgements
This project received funding from the following agencies: The Canadian Council on Learning, British Columbia Medical Services Foundation and the Canadian Diabetes Association. Constadina Panagiotopoulos is the recipient of the Child & Family Research Institute Clinician Scientist Award and the Canadian Diabetes Association Clinician Scientist Award.
Footnotes
1Published ‘ahead-of-print’ 2 December 2011 (at www.ijch.fi) in accordance with previous publisher's routines.
Conflict of interest and funding
The authors declare that there are no conflicts of interest.
References
- 1.Katzmarzyk PT. Obesity and physical activity among aboriginal Canadians. Obesity. 2008;16(1):184–90. doi: 10.1038/oby.2007.51. [DOI] [PubMed] [Google Scholar]
- 2.First Nations Information Governance Centre (FNIGC) Akwesasne: First Nations Information Governance Centre; 2011. RHS Phase 2 (2008/10) preliminary results (revised edition) [cited 2011 Aug 11]. Available from: http://www.rhs-ers.ca/sites/default/iles/FIN-ALRHSPreliminaryReportJune2011.pdf. [Google Scholar]
- 3.Bernard L, Lavalle C, Gray-Donald K, Delisle H. Overweight in Cree schoolchildren and adolescents associated with diet, low physical activity, and high television viewing. J Am Diet Assoc. 1995;95(7):800–2. doi: 10.1016/S0002-8223(95)00221-9. [DOI] [PubMed] [Google Scholar]
- 4.Ng C, Marshall D, Willows N. Obesity, adiposity, physical fitness and activity levels in Cree children. Int J Circumpolar Health. 2006;65(4):322–30. doi: 10.3402/ijch.v65i4.18124. [DOI] [PubMed] [Google Scholar]
- 5.Clarke WR, Lauer RM. Does childhood obesity track into adulthood? Crit Rev Food Sci Nutr. 1993;33(4–5):423–30. doi: 10.1080/10408399309527641. [DOI] [PubMed] [Google Scholar]
- 6.DiPietro L, Mossberg HO, Stunkard AJ. A 40-year history of overweight children in Stockholm: life-time overweight, morbidity, and mortality. Int J Obes Relat Metab Disord. 1994;18(9):585–90. [PubMed] [Google Scholar]
- 7.Health Canada. Ottawa: Medical Services Branch, Health Canada; 1999. A second diagnostic on the health of First Nations and Inuit people in Canada; p. 7. [Google Scholar]
- 8.St Leger L. Schools, health literacy and public health: possibilities and challenges. Health Promot Int. 2001;16(2):I97–205. doi: 10.1093/heapro/16.2.197. [DOI] [PubMed] [Google Scholar]
- 9.Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, et al. Outcomes of a field trial to improve children's dietary patterns and physical activity. JAMA. 1996;275(10):768–76. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- 10.Naylor PJ, Macdonald HM, Warburton DE, Reed KE, McKay HA. An active school model to promote physical activity in elementary schools: Action Schools! BC. Br J Sports Med. 2008;42(5):338–43. doi: 10.1136/bjsm.2007.042036. [DOI] [PubMed] [Google Scholar]
- 11.van Sluijs E, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007;335(7622):703. doi: 10.1136/bmj.39320.843947.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baranowski T, Davis M, Resnicow K, Baranowski J, Doyle C, Lin LS, et al. Gimme 5 fruit, juice, and vegetables for fun and health: outcome evaluation. Health Educ Behav. 2000;27(1):96–111. doi: 10.1177/109019810002700109. [DOI] [PubMed] [Google Scholar]
- 13.Day ME, Strange KS, McKay HA, Naylor PJ. Action Schools! BC-Healthy Eating: effects of a whole-school model to modifying eating behaviours of elementary school children. C J Public Health. 2009;99(4):328–31. doi: 10.1007/BF03403766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foerster S, Gregson J, Beall D, Hudes M, Magnuson H, Livingston S, et al. The California children's 5 a day –power play! campaign: evaluation of a large-scale social marketing initiative. Fam Community Health. 1998;21(1):46–64. [Google Scholar]
- 15.Naylor PJ, MacDonald HM, Zebedee JA, Reed KE, McKay HA. Lessons learned from Action Schools! BC –An ‘active school’ model to promote physical activity in elementary schools. J Sci Med Sport. 2006;9(5):413–9. doi: 10.1016/j.jsams.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Macdonald H, Kontulainen S, Khan K, McKay H. Is a school-based physical activity intervention effective for increasing tibial bone strength in boys and girls? J Bone Miner Res. 2007;22(3):434–46. doi: 10.1359/jbmr.061205. [DOI] [PubMed] [Google Scholar]
- 17.Reed KE, Warburton DER, Macdonald HM, Naylor PJ, McKay HA. Action Schools! BC: A school-based physical activity intervention designed to decrease cardiovascular disease risk factors in children. Prev Med. 2008;46(6):525–31. doi: 10.1016/j.ypmed.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 18.Zorzi A, Wahi G, Macnab AJ, Panagiotopoulos C. Prevalence of impaired glucose tolerance and the components of metabolic syndrome in Canadian Tsimshian Nation youth. Can J Rural Med. 2009;14(2):61–7. [PubMed] [Google Scholar]
- 19.Panagiotopoulos C, Rozmus J, Gagnon RE, Macnab AJ. Diabetes screening of children in a remote First Nations community on the west coast of Canada: challenges and solutions. Rural Remote Health. 2007;7(3):771. [PubMed] [Google Scholar]
- 20.Naylor PJ, Scott J, Drummond J, Bridgewater L, McKay HA, Panagiotopoulos C. Implementing a whole school physical activity and healthy eating model in rural and remote First Nations schools: a process evaluation of Action Schools! BC. Rural Remote Health. 2010;10(2):1296. [PubMed] [Google Scholar]
- 21.Canadian Society for Exercise Physiology. 3rd ed. Ottawa: CSEP Health and Fitness Program; 2003. Canadian physical activity, itness and lifestyle approach; pp. 8–67. [Google Scholar]
- 22.Ogden CL, Kuczmarski RJ, Flegal KM, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109(1):45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 23.Barlow SE, and the Expert Committee Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 24.Fernández JR, Redden DT, Pietrobebelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004;145(4):439–44. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 25.Crocker PRE, Bailey DA, Faulkner RA, Kowalski KC, McGrath R. Measuring general levels of physical activity: preliminary evidence for the physical activity questionnaire for older children. Med Sci Sports Exerc. 1997;29(10):1344–9. doi: 10.1097/00005768-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Freedson P, Pober D, Janz KF. Calibration of accelerometer output for children. Med Sci Sports Exerc. 2005;37(11 Suppl):S523–30. doi: 10.1249/01.mss.0000185658.28284.ba. [DOI] [PubMed] [Google Scholar]
- 27.Mitchell M, Gaul C, Naylor P, Panagiotopoulos C. Habitual moderate-to-vigorous physical activity is inversely associated with insulin resistance in Canadian First Nations youth. Pediatr Exerc Sci. 2010;22(2):254–65. doi: 10.1123/pes.22.2.254. [DOI] [PubMed] [Google Scholar]
- 28.Leger L, Lambert J, Goulet A, Rowan C, Dinelle Y. Aerobic capacity of 6 to 17-year-old Quebecois – 20 meter shuttle run test with I minute stages. Can J Appl Sport Sci. 1984;9(2):64–9. [PubMed] [Google Scholar]
- 29.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–576. [PubMed] [Google Scholar]
- 30.Cooper Institute. 4th ed. Champaign: Human Kinetics; 2007. Fitnessgram/Activitygram test administration manual: test administration manual; pp. 38–39. [Google Scholar]
- 31.Mullenbach V, Kushi LH, Jacobson C, Gomez-Marin O, Prineas RJ, Roth-Yousey L, et al. Comparison of 3-day food record and 24-hour recall by telephone for dietary evaluation in adolescents. J Am Diet Assoc. 1992;92(6):743–5. [PubMed] [Google Scholar]
- 32.Health Canada. Ottawa: Health Canada; 2005. Food and nutrition, nutrient data, Canadian nutrient file. [cited 2010 Aug 11]. Available from: http://www.hc-sc.gc.ca/fn-an/nutrition/fiche-nutri-data/index_e.html. [Google Scholar]
- 33.Manios Y, Moschandreas M, Hatzis C, Kafatos A. Health and nutrition education in primary schools of Crete: changes in chronic disease risk factors following a 6-year intervention programme. Br J Nutr. 2002;88(3):315–24. doi: 10.1079/BJN2002672. [DOI] [PubMed] [Google Scholar]
- 34.Kriemler S, Zahner L, Schindler C, Meyer U, Hartmann T, Hebestreit H, et al. Effect of school based physical activity programme (KISS) on itness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ. 2010;340:785. doi: 10.1136/bmj.c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vandongen R, Jenner DA, Thompson C, Taggart AC, Spickett EE, Burke V, et al. A controlled evaluation of a fitness and nutrition intervention program on cardiovascular health in 10-to 12-year-old children. Prev Med. 1995;24(1):9–22. doi: 10.1006/pmed.1995.1003. [DOI] [PubMed] [Google Scholar]
- 36.Paradis G, Levesque L, Macaulay AC, Cargo M, Mc-Comber A, Kirby R, et al. Impact of a diabetes prevention program on body size, physical activity, and diet among Kanien'keha: Ka (Mohawk) children 6 to 11 years old: 8-year results from the Kahnawake Schools Diabetes Prevention Project. Pediatrics. 2005;115(2):333–9. doi: 10.1542/peds.2004-0745. [DOI] [PubMed] [Google Scholar]
- 37.McKenzie TL, Nader PR, Strikmiller PK, Yang M, Stone EJ, Perry CL, et al. School physical education: effect of the child and adolescent trial for cardiovascular health. Prev Med. 1996;25(4):423–31. doi: 10.1006/pmed.1996.0074. [DOI] [PubMed] [Google Scholar]
- 38.Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001;161(13):1581–6. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 39.Blair SN, Kohl HW, Barlow CE, Paffenbarger RS, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273(14):1093–8. [PubMed] [Google Scholar]
- 40.Ortega FB, Ruiz JR, Castillo MJ, Sjöström M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes (Lond) 2008;32(1):1–11. doi: 10.1038/sj.ijo.0803774. [DOI] [PubMed] [Google Scholar]
- 41.Caballero B, Clay T, Davis SM, Ethelbah B, Rock BH, Lohman T, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78(5):1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Saksvig BI, Gittelsohn J, Harris SB, Hanley AJ, Valente TW, Zinman B. A pilot school-based healthy eating and physical activity intervention improves diet, food knowledge, and self-efficacy for Native Canadian children. J Nutr. 2005;135(10):2392–8. doi: 10.1093/jn/135.10.2392. [DOI] [PubMed] [Google Scholar]
- 43.Ritenbaugh C, Teufel-Shone NI, Aickin MG, Joe JR, Po-irier S, Dillingham DC, et al. A lifestyle intervention improves plasma insulin levels among Native American high school youth. Prev Med. 2003;36(3):309–19. doi: 10.1016/s0091-7435(02)00015-4. [DOI] [PubMed] [Google Scholar]
- 44.Janssen I, Katzmarzyk PT, Srinivasan SR, Chen W, Mali-na RM, Bouchard C, et al. Combined influence of body mass index and waist circumference on coronary artery disease risk factors among children and adolescents. Pediatrics. 2005;115(6):1623–30. doi: 10.1542/peds.2004-2588. [DOI] [PubMed] [Google Scholar]
- 45.Downs SM, Marshall D, Ng C, Willows ND. Central adiposity and associated lifestyle factors in Cree children. Appl Physiol Nutr Metab. 2008;33(3):476–82. doi: 10.1139/H08-027. [DOI] [PubMed] [Google Scholar]
- 46.Savva SC, Tornaritis M, Savva ME, Kourides Y, Panagi A, Silikiotou N, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obesity. 2000;24(11):1453–8. doi: 10.1038/sj.ijo.0801401. [DOI] [PubMed] [Google Scholar]
- 47.Environment Canada. Gatineau: Environment Canada; 2008. National Climate Data and Information Archive. [cited 2010 Aug 11]. Available from: www.cli-mate.weatheroffice.gc.ca/climateData/menu_e.html?timeframe=1&Prov=BC&StationID=9999&Year=2010&Month=8&Day=11. [Google Scholar]
- 48.Bélanger M, Gray-Donald K, O'Loughlin J, Paradis G, Hanley J. Influence of weather conditions and season on physical activity in adolescents. Ann Epidemiol. 2009;19(3):180–6. doi: 10.1016/j.annepidem.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 49.Esliger DW, Copeland JW, Barnes JD, Tremblay MS. Standardizing and optimizing the use of accelerometer data for free-living physical activity monitoring. J Teach Phys Educ. 2005;2(3):366–83. [Google Scholar]
- 50.Ribeiro JC, Guerra S, Oliveira J, Teixeira-Pinto A, Twisk JW, Duarte JA, et al. Physical activity and biological risk factors clustering in pediatric population. Prev Med. 2004;39(3):596–601. doi: 10.1016/j.ypmed.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 51.Ebbeling C, Feldman H, Osganian S, Chomitz V, Ellenbogen S, Ludwig D. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: a randomized, controlled pilot study. Pediatrics. 2006;117(3):673–80. doi: 10.1542/peds.2005-0983. [DOI] [PubMed] [Google Scholar]
- 52.Jimenez MM, Receveur O, Trifonopoulos M, Kuhnlein H, Paradis G, Macaulay A. Comparison of the dietary intakes of two different groups of children (grades 4 to 6) before and after the Kahnawake Schools Diabetes Prevention Project. J Am Diet Assoc. 2003;103(9):1191–4. doi: 10.1016/s0002-8223(03)00980-5. [DOI] [PubMed] [Google Scholar]
- 53.Macauley AC, Delormier T, McComber A, Cross EJ, Potvin LP, Paradis G, et al. Participatory research with native community of Kahnawake creates innovative code of research ethics. Can J Public Health. 1998;89(2):105–8. doi: 10.1007/BF03404399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nelson M, Black AE, Morris JA, Cole TJ. Between- and within-subject variation in nutrient intake from infancy to old age: estimating the number of days required to rank dietary intakes with desired precision. Am J Clin Nutr. 1989;50(1):155–67. doi: 10.1093/ajcn/50.1.155. [DOI] [PubMed] [Google Scholar]
- 55.Lohman TG, Caballero B, Himes JH, Davis CE, Stewart D, Houtkooper L, et al. Estimation of body fat from anthropometry and bioelectrical impedance in Native American children. Int J Obes. 2000;24(8):982–8. doi: 10.1038/sj.ijo.0801318. [DOI] [PubMed] [Google Scholar]