Abstract
Objectives
To estimate the age- and gender-specific consultation rates of patients who availed primary health care service in Greenland and to analyse contact patterns among patients in Nuuk.
Design
Observational and cross-sectional register study using data captured from the medical records.
Materials and methods
The number of patients specified by age and gender who had contacted the primary health care centres within the last year was identified using a statistic module applied to the electronic medical records system. The population as it was on the 1st of January 2011 was used as the background population. The age- and gender-specific consultation rates were calculated. Review of most recent contact was performed in a subsample of patients from Nuuk, and information of the type of contact and diagnoses was obtained.
Results
Eighty-three percent of the population in Greenland had been in contact with the primary health care centre within the last year. Females were more frequent users than males. A subsample of 400 patients in Nuuk was identified. Personal contact was the most frequent type of consultation (75.8%), followed by telephone (14.8%) and e-mail (9.8%) consultations. Musculoskeletal symptoms accounted for the most frequent bases for diagnoses.
Conclusion
More than 80% of the whole population has been in contact with the primary health care system within the last year. This indicates that opportunistic case-finding of chronic diseases such as diabetes, hypertension, etc. providing a possible strategy for decreasing the number of undiagnosed cases.
Keywords: Greenland, Inuit, chronic disease, primary health care
With 2.2 million square metres of area, Greenland is the largest island in the world, with 85% of it covered by ice. This means that only the coastline is inhabited, with a population of 57,000 inhabitants (1). The population is widely spread in 18 towns and a number of small settlements. The largest town is the capital Nuuk, with almost 16,000 inhabitants. Approximately 15% of the total inhabitants live in the settlements. Around 90% of the population is of Greenlandic origin, whereas around 10% – mostly Danes (1) – are immigrants.
Greenland has undergone a rapid transition during the last half century from a traditional Inuit society dominated by small communities, villages and settlements to a modern society with more than 60% of the inhabitants living in towns with at least 2,500 inhabitants (2,3).
Within a few decades since the 1950s Greenland was transformed from a traditional hunting society to a modern society (2). The profound social and cultural changes have been followed by a health transition with an increasing prevalence of lifestyle-related diseases such as obesity, diabetes and ischaemic heart disease, a transition similar to that observed among the Inuit in Alaska and Canada (3–15).
Population surveys performed in Greenland within the last 15 years indicate a high prevalence of diabetes mellitus, around 10% of adults (11,16). However, 70–80% of those cases were undiagnosed (11,16). Also, the prevalence of undiagnosed hypertension is high. In a recent population survey only a fourth of those with elevated blood pressure were treated for hypertension (8). Awareness of these chronic conditions either in the population or in the health care system seems to be suboptimal. The national consumption of cardiovascular drugs in Greenland is much lower (around 50% lower) than in the other Nordic countries (17). This may indicate that either these conditions are undiagnosed or untreated in Greenland compared to the other Nordic countries or the actual prevalence is lower in Greenland.
Low diagnostic activity has been stated as a possible explanation for the high proportion of undiagnosed cases of diabetes (11). Explanations could include that patients are reluctant to seek treatment or that the health care personnel are inattentive to case-finding. However, the use of the primary health care service among the population in Greenland is unknown. The aim of this study was to estimate age- and gender-specific consultation rates in Greenland and to examine the types of consultations taking place in a subsample in Nuuk.
Methods
Setting
Health care services are primarily the responsibility of the government of Greenland. The health care system is obligated to deliver equal health care to all citizens regardless of their place of residence; all health care services are free – including the prescribed medicine.
In January 2010, the primary health care system in Greenland was reorganized into 5 regions comprised of 2–4 towns (19). Thus, 16 towns have a primary health care clinic each (which also functions as a local hospital) which serves the population in the towns and a variable number of surrounding settlements. The largest towns are staffed with doctors, nurses, health visitors, midwifes, medical laboratory technicians, etc. In the settlements the staff consist of nurses and health care workers. Queen Ingrid's Hospital in Nuuk functions as a national hospital for more specialized treatment and also serves as a local hospital for the population in Nuuk.
All persons registered with a permanent address in Greenland are automatically affiliated with one of the 16 primary health care clinics. All the primary health care clinics use the same electronic medical records system (EMR, implemented autumn 2007) which allows the identification of persons affiliated with the clinics (19). By law, all contacts to the health care system have to be recorded in the EMR.
Study group
All persons who had been in contact with the health care system within the period from 1st of June 2010 to 31st of May 2011 were identified for all 16 clinics in Greenland from the EMR system. The population data by age and sex as on the 1st of January 2011 was obtained from the population registry.
A subsample, comprising 25 persons in each 10-year age and sex groups affiliated with the primary health care clinic in Nuuk, was used to describe the type of consultation and the reason for contact. Twenty-five persons were selected by birthdate, and included those born on the first or second day of each month. On the basis of a review of these persons’ medical records, the most recent contact was categorized as a telephone, e-mail or personal consultation. The most recent contact was further classified by a trained nurse according to the 17 chapters of the International Classification of Primary Care [(ICPC-2), (20,21)] (Table I).
Table I.
Distribution of consultations (%) classified according to the International Classification of Primary Care (ICPC-2) for every age group in the subsample from Nuuk
| ICPC-code Age (years) | 0–9 N=50 | 10–19 N=50 | 20–29 N=50 | 30–39 N=50 | 40–49 N=50 | 50–59 N=50 | 60–69 N=50 | 70+ N=50 | Total N=400 | Male N=200 | Female N=200 | P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A – General and unspecified | 20 (10) | 8 (4) | 8 (4) | 6 (3) | 10 (5) | 8 (4) | 8 (4) | 10 (5) | 10 (39) | 10 (19) | 10 (20) | 0.866 |
| B – Blood, blood forming organs, lymphatics, spleen | 0 (0) | 0 (0) | 2 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (1) | 0 (0) | 1 (1) | 0.317 |
| D – Digestive | 6 (3) | 2 (1) | 4 (2) | 14 (7) | 4 (2) | 14 (7) | 2 (1) | 6 (3) | 7 (26) | 8 (16) | 5 (10) | 0.224 |
| F – Eye | 10 (5) | 2 (1) | 4 (2) | 2 (1) | 2 (1) | 4 (2) | 4 (2) | 4 (2) | 4 (16) | 5 (9) | 4 (7) | 0.610 |
| H – Ear | 12 (6) | 12 (6) | 2 (1) | 2 (1) | 6 (3) | 4 (2) | 4 (2) | 8 (4) | 6 (25) | 7 (13) | 6 (12) | 0.840 |
| K – Circulatory | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 4 (2) | 12 (6) | 24 (12) | 20 (10) | 8 (30) | 5 (10) | 10 (20) | 0.058 |
| L – Musculoskeletal | 6 (3) | 20 (10) | 14 (7) | 22 (11) | 12 (6) | 16 (8) | 20 (10) | 12 (6) | 15 (61) | 15 (30) | 16 (31) | 0.889 |
| N – Neurological | 0 (0) | 4 (2) | 4 (2) | 0 (0) | 0 (0) | 4 (2) | 0 (0) | 2 (1) | 2 (7) | 2 (4) | 2 (3) | 0.703 |
| P – Psychological | 4 (2) | 8 (4) | 8 (4) | 4 (2) | 6 (3) | 8 (4) | 2 (1) | 6 (3) | 6 (23) | 7 (14) | 5 (9) | 0.266 |
| R – Respiratory | 24 (12) | 6 (3) | 12 (6) | 18 (9) | 12 (6) | 10 (5) | 14 (7) | 6 (3) | 13 (51) | 13 (26) | 13 (25) | 0.880 |
| S – Skin | 16 (8) | 24 (12) | 10 (5) | 12 (6) | 20 (10) | 8 (4) | 10 (5) | 2 (1) | 13 (51) | 17 (33) | 9 (18) | 0.025 |
| T – Endocrine, metabolic and nutritional | 0 (0) | 2 (1) | 2 (1) | 2 (1) | 8 (4) | 2 (1) | 8 (4) | 12 (6) | 5 (18) | 5 (9) | 5 (9) | 1.000 |
| U – Urology | 2 (1) | 2 (1) | 2 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 12 (6) | 2 (9) | 2 (3) | 3 (6) | 0.312 |
| W – Pregnancy, childbirth, family planning | 0 (0) | 4 (2) | 14 (7) | 12 (6) | 4 (2) | 0 (0) | 0 (0) | 0 (0) | 4 (17) | 0 (0) | 9 (17) | <0.001 |
| X – Female genital system and breast | 0 (0) | 0 (0) | 4 (2) | 2 (1) | 8 (4) | 6 (3) | 4 (2) | 0 (0) | 3 (12) | 0 (0) | 6 (12) | <0.001 |
| Y – Male genital system | 0 (0) | 4 (2) | 8 (4) | 4 (2) | 4 (2) | 4 (2) | 0 (0) | 0 (0) | 3 (12) | 6 (12) | 0 (0) | <0.001 |
| Z – Social problems | 0 (0) | 2 (1) | 2 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (2) | 1 (2) | 0 (0) | 0.156 |
| Total % | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
Analysis
The age- and gender-specific consultation rates were calculated for each decade by age and gender groups. Contact reason and type were described for each age group and gender group in the subsample.
Chi-square tests were performed to compare frequencies. A P-value at 0.05 was used as the level of significance.
Results
A total of 46,802 persons (22,686 males and 24,116 females) were identified as having at least one contact with one of the 16 primary health care clinics within the period from 1st of June 2010 to 31st of May 2011. Thus, 83% (46,802/56,419) of the whole population had been in contact with the health care system within a 1-year period. The proportion was higher among women (90%) than among men (76%) (p<0.001).
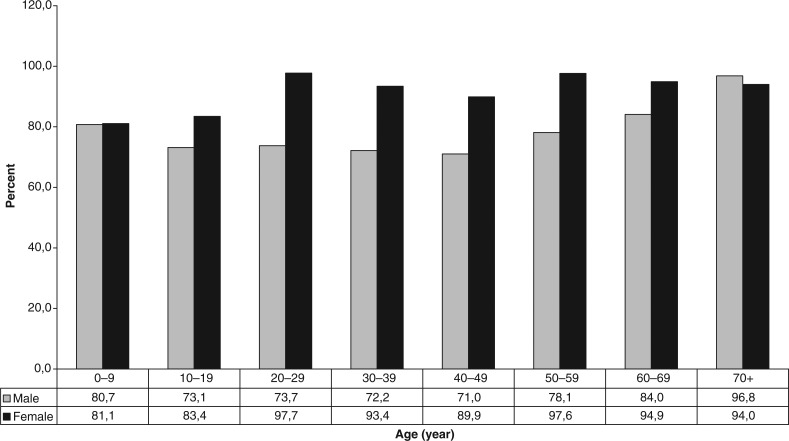
The age- and gender-specific percentages of the population that had been in contact with the primary health care are shown in Fig. 1.
Fig. 1.
Percentage of population with contact to the health care system within the last year.
A subsample of 400 persons in Nuuk including those who had been in contact with the primary health care system within 1 year was identified electronically. The most recent contact was classified as e-mail contact (10%), telephone (15%) and in person (76%). The distribution of ICPC diagnoses for each age group and for gender groups is shown in Table I. The most frequent diagnoses were musculoskeletal, respiratory system, skin conditions and general/unspecified.
Discussion
Eighty-three percent of the whole population has been in contact with the primary health care system in Greenland. Females were more frequent users than males in almost every age group. The greatest difference was observed for in the age group 20–59 years old. Symptoms from the musculoskeletal system, the respiratory system and the skin were the most frequent bases for diagnoses in addition to the general and unspecific chapter looking at all age groups together, whereas children under 10 years old were primarily diagnosed with respiratory and ear symptoms.
The primary advantage for this study was that all primary clinics in Greenland were included, and the data was captured electronically from each clinic.
The results of the sub-analysis concerning types of consultations and diagnoses reflect the conditions found at the primary clinic in Nuuk and cannot be directly generalized to the whole country. Nuuk is the capital and largest town, with around a fourth of the whole population of Greenland. Furthermore, the majority of immigrants (foreign workers) live in Nuuk, and a “healthy worker effect” may influence the demand of primary health care. On the other hand, the capital may also attract people with social problems which may also affect the demand for primary care. Finally, Nuuk is the only town in Greenland with a hospital offering specialized treatment. Some patients are thus seen in the outpatient clinic of Queen Ingrid's Hospital by specialists. This may also affect the demand for primary care.
The high consultation rates demonstrated in this study suggest an adequate access to primary health care service, facilitated by the free service to everyone and the location of a primary health clinic in each town.
The high prevalence of undiagnosed chronic conditions like diabetes and hypertension in Greenland cannot be explained by low consultation rates. Instead, the screening for chronic conditions may fail for other reasons. Less awareness on these lifestyle-related diseases among patients and health care providers may be due to the fact that these conditions are relatively new in Greenland. There is a stronger emphasis on other major health problems such as tuberculosis, sexually transmitted diseases, cancer, tobacco and alcohol abuse, suicide, etc. The health care system in Greenland consists of small geographically isolated units that have to deal with diverse medical, surgical and psychiatric conditions. It is likely that the health care system is preoccupied with managing more acute conditions rather than screening for more chronic conditions.
The high level of contact with the primary health care is comparable to other Nordic countries such as Denmark and Iceland (22,23). The higher utilization rate among women is also similar to that of the other Nordic countries (22–26).
In this study the consultation rate varies by age and gender. The highest consultation rates for males were found among children and over 60 years old. The highest consultation rates for women were found among fertile women and those over 60 years old. This j-shaped curve is also seen in the other Nordic countries (22–26).
The results from Nuuk show that in general for every age, the most frequent type of contacts are concerning musculoskeletal, respiratory or skin diseases, except for children for whom the most frequent type of contact concerns ear or respiratory diseases. Similar patterns have been confirmed in studies from Denmark and Iceland (22,23). The use of primary health care services in Greenland was thus similar to the use reported in the rest of the Nordic countries.
In conclusion the high proportion of the population that has been in contact with the health care system within the last year demonstrated in this study indicates strong public demand and adequate access to primary health care services in Greenland. Given such a high contact rate with the health care system, screening for chronic diseases such as diabetes could be targeted. Special efforts need to be extended to middle aged men who have the lowest contact rate.
Key points
Population surveys indicate high prevalence of undiagnosed chronic diseases in Greenland.
The public health care service in Greenland is free to all inhabitants. However, the use of primary health care is unknown.
This study shows that the majority of the population has contact with the primary health care system in Greenland within the last year indicating an opportunity for case-finding of chronic diseases.
Acknowledgements
We thank Jim Milne who had assisted with linguistic proof reading.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Greenland Statistics. Population in towns and settlements by time, locality, age, gender and place of birth. Greenland Statistics; 2011. [cited 2012 Mar 12]. Available from: http://www.stat.gl/ [Google Scholar]
- 2.Bjerregaard P, Young TK. The circumpolar Inuit – health of a population in transition. Copenhagen: Munksgaard; 1998. pp. 26–30. [Google Scholar]
- 3.Pedersen ML. Diabetes mellitus in Greenland. Prevalence, organisation and quality in the management of type 2 diabetes mellitus. Effect of a Diabetes Health Care Project. Dan Med J. 2012;59:B4386. [PubMed] [Google Scholar]
- 4.Bjerregaard P, Young TK, Dewailly E, Ebbesson SO. Indigenous health in the Arctic: an overview of the circumpolar Inuit population. Scand J Public Health. 2004;32:390–5. doi: 10.1080/14034940410028398. [DOI] [PubMed] [Google Scholar]
- 5.Curtis T, Kvernmo S, Bjerregaard P. Changing living conditions, life style and health. Int J Circumpolar Health. 2005;64:442–50. doi: 10.3402/ijch.v64i5.18025. [DOI] [PubMed] [Google Scholar]
- 6.Bjerregaard P, Curtis T, Borch-Johnsen K, Mulvad G, Becker U, Andersen S, et al. Inuit health in Greenland: a population survey of life style and disease in Greenland and among Inuit living in Denmark. Int J Circumpolar Health. 2003;62(Suppl 1):3–79. doi: 10.3402/ijch.v62i0.18212. [DOI] [PubMed] [Google Scholar]
- 7.Dahl-Petersen IK, Jørgensen ME, Bjerregaard P. Physical activity patterns in Greenland: a country in transition. Scand J Public Health. 2011;39:678–86. doi: 10.1177/1403494811420486. [Epub 2011 Sep 22] [DOI] [PubMed] [Google Scholar]
- 8.Bjerregaard P, Aidt EC. Levevilkår, livsstil og helbred – Befolkningsundersøgelsen I Grønland 2005–2009. Copenhagen: Syddansk Universitet: Statens Institut for Folkesundhed; 2010. pp. 1–30. [Report in Danish and Greenlandic about a population survey performed in Greenland] [Google Scholar]
- 9.Bjerregaard P. befolkningsundersøgelse I Grønland 2005–2007, Levevilkår, livstil og Helbred. Copenhagen: Syddansk Universitet: Statens Institut for Folkesundhed; 2008. pp. 1–174. [Report in Danish and Greenlandic about a population survey performed in Greenland] [Google Scholar]
- 10.Niclasen BVL, Petzold MG, Schnohr C. Overweight and obesity at school entry as a predictor of overweight in adolescence in artic population. Eur J Public Health. 2007;17:17–20. doi: 10.1093/eurpub/ckl246. [DOI] [PubMed] [Google Scholar]
- 11.Jørgensen ME, Bjerregaard P, Borch-Johnsen K, Backer V, Becker U, Jørgensen T, et al. Diabetes and impaired glucose tolerance among the Inuit population of Greenland. Diabetes Care. 2002;25:1766–71. doi: 10.2337/diacare.25.10.1766. [DOI] [PubMed] [Google Scholar]
- 12.Jørgensen ME, Bjerregaard P, Kjaergaard JJ, Borch-Johnsen K. High prevalence of markers of coronary heart disease among Greenland Inuit. Atherosclerosis. 2008;196:772–8. doi: 10.1016/j.atherosclerosis.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Ebbesson SO, Adler AI, Risica PM, Ebbesson LO, Yeh JL, Go OT, et al. Cardiovascular disease and risk factors in three Alaskan Eskimo populations: the Alaska-Siberia project. Int J Circumpolar Health. 2005;64:365–86. doi: 10.3402/ijch.v64i4.18014. [DOI] [PubMed] [Google Scholar]
- 14.Howard BV, Comuzzie A, Devereux RB, Ebbesson SO, Fabsitz RR, Howard WJ, et al. Cardiovascular disease prevalence and its relation to risk factors in Alaska Eskimos. Nutr Metab Cardiovasc Dis. 2010;20:350–8. doi: 10.1016/j.numecd.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chateau-Degat ML, Dewailly E, Noël M, Valera B, Ferland A, Counil E, et al. Hypertension among the Inuit from Nunavik: should we expect an increase because of obesity? Int J Circumpolar Health. 2010;69:361–72. doi: 10.3402/ijch.v69i4.17630. [DOI] [PubMed] [Google Scholar]
- 16.Jørgensen ME, Borch-Johnsen K, Witte DR, Bjerregaard P. Diabetes in Greenland and its relationship with urbanization. Diabet Med. 2011 Dec 1; doi: 10.1111/j.1464-5491.2011.03527.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Nomesco. Medicines consumption in the Nordic countries 2004–2008. Copenhagen: Nordic Medico Statistical Committee (NOMESCO); 2009. pp. 62–76. [Google Scholar]
- 18.Redegørelse om sundhedsreformen, Departement for sundhed. Report in Danish about the health care reform in Greenland. 2010. pp. 1–41. [cited 2012 Mar 12]. Available from: http://www.peqqik.gl/
- 19.Sundhedsvæsenets Årsberetning. Annuall report in Danish about activities in the health care system. 2007. [cited 2012 Mar 16]: [p. 1–37]. Available from: http://www.peqqik.gl/
- 20.Wonca. ICPC-2 International Classification of Primary Care, second edition. Prepared by the International Classification Committee of WONCA; Oxford: Oxford University Press; 1998. pp. 1–204. [Google Scholar]
- 21.Okkes IM, Jamoulle M, Lamberts H, Bentzen N. ICPC-2-E. The electronic version of ICPC-2. Differences with the printed version and the consequences. Fam Pract. 2000;17:101–6. doi: 10.1093/fampra/17.2.101. [DOI] [PubMed] [Google Scholar]
- 22.Vedsted P, Olesen F, Hollnagel H, Bro F, Kamper-Jørgensen F. Almen Lægepraksis i Danmark. Tidsskrift for Praktisk Lægegerning og forskningsenheden for Almen Praksis (Report in Danish about use of primary health care in Denmark); Copenhagen: 2005. [Google Scholar]
- 23.Njálsson T. On content of practice. The advantage of computerized information systems in family practice. Scand J Prim Health Care. 1995;13(Suppl 1):1–102. [PubMed] [Google Scholar]
- 24.Krakau I. Trends in use of Health Care Services in Swedish Primary Care District. A ten year perspective. Scand J Prim Health Care. 1992;10:66–71. doi: 10.3109/02813439209014038. [DOI] [PubMed] [Google Scholar]
- 25.Eggen P, Mæland JG, Skjærven R. Use of primary medical care: does place of residence play a role. Scand J Prim Health Care. 1993;11:31–37. doi: 10.3109/02813439308994899. [DOI] [PubMed] [Google Scholar]
- 26.Vehviläinen AT, Kumpusalo EA, Voutilainen SO, Takala JK. General practice consultations in central and northern Finland. Scand J Prim Health Care. 1995;13:197–204. doi: 10.3109/02813439508996761. [DOI] [PubMed] [Google Scholar]