Abstract
Objectives
The Sami people constitute the indigenous people in northern Norway. The objective of this study was to clarify whether they have a similar supply of somatic specialist health care (SHC) as others.
Methods
The referrals from general practitioners (GPs) in the primary health care (PHC) in the administration area of the Sami language law (8 municipalities) were matched with a control group of 11 municipalities. Population data was accessed from Statistics Norway and the time period 2007–2010 was analysed. The main outcome was the number of referrals per 1,000 inhabitants according to age group, gender and place of living.
Results
504,292 referrals in northern Norway were indentified and the Sami and control group constituted 23,093 and 22,541 referrals, respectively. The major findings were a similar referral ratio (RR) (1.14 and 1.17) (p =0.624) and women more commonly referred (female/male ratio 1.45 and 1.41) in both groups. GPs in both groups were loyal to their local hospital trust.
Conclusion
Inhabitants in Sami-speaking municipalities in northern Norway have a similar supply of SHC services as controls. Inter-municipal variation was significant in both groups.
Keywords: Sami, specialist health care, referral, ethnic minority
General practitioners (GPs) act as “gatekeepers” in health care service. Referrals from GPs are requests for medical examination and evaluation by a specialist, outpatient clinic or a hospital. When received, they are triaged according to priority guidelines into categories depending on clinical criteria resulting in appointments of various timeframes. The crucial status of GPs in the “health care system pyramid” has caused many health care authorities world-wide to strengthen the primary care, as national healthcare systems with a strong primary care sector tend to have lower healthcare costs (1). In northern Norway, vacancies, short time in positions and steadily replaced GPs in many municipalities has been a constant challenge and concern to health care administrators.
All Norwegians have equal rights concerning supply of primary and secondary health care, independent of ethnical group (2). The Sami constitute an ethnic minority and the Norwegian government has ratified them as the indigenous people in Norway (3). The size of the Sami population has been reckoned to be approximately 75,000–100,000. They are protected by a Sami Act, have a different native language and culture that may cause threshold, counter, queue and cultural challenges when assessing the public health care (2). Prior research has revealed the Sami people less satisfied, than Norwegians in general, with the health care service provided (4,5). Due to this fact, several national reports have put the Sami healthcare into focus (2,6). Furthermore, the concern of Sami's supply of specialist health care (SHC) has been stated in the annual mission document from the Ministry of Health and Care Services to the Northern Norway Regional Health Authority (NNRHA) (7). On this background, we aimed to clarify and explore the referral frequency/index from the Sami-speaking municipalities and a control group to the somatic SHC in our region.
Materials and methods
In February 2011, data on all referrals from the primary health care (PHC) to the SHC in northern Norway in the time period 1 January 2007 until 31 December 2010 was accessed. The data was retrospectively analysed and a comparative study focusing the Sami-speaking municipalities (Sami group) and a control group (non-Sami group) was performed. The number of inhabitants in each group was calculated according to data from Statistics Norway (www.ssb.no). All referrals were recorded with the following information: Patient's place of living (municipality), gender, age-group and address of referral (hospital trust). No sub-classification of the referral for somatic SHC was available.
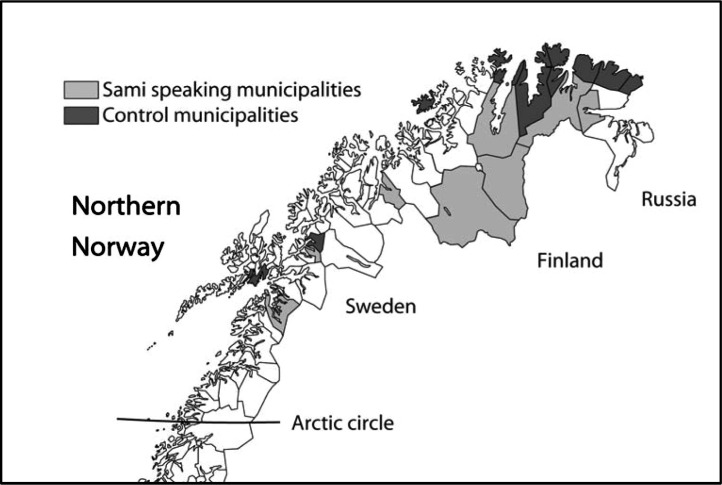
Many Norwegian municipalities have Sami settlers, but only 8 municipalities have been included in the administration area of the Sami language law. The latter were selected as the Sami municipalities (Sami group) in this study. They are all located in the rural inland areas. The coastal municipalities of northern Norway have generally few Sami people and 11 of them were chosen as the control group. They were selected based on rural location, distance to hospital and a similar population in size, ratio between gender and age as the Sami-speaking municipalities. The locations of all municipalities in both groups are shown in Fig. 1. None of the municipalities had any hospital or hospital unit. The names of the municipalities in the administration area of the Sami language law written in Sami language (when employed) and Norwegian were: Deatnu Tana, Unjárga Nesseby, Porsanger Porsángu Porsanki, Kárásjohka Karasjok, Guovdageaidnu Kautokeino, Gáivuotna Kåfjord, Ástávuona Lavangen and Divtasvuona Tysfjord. The municipalities included in the control group (non-Sami group) were: Lødingen, Bjarkøy, Lebesby, Gamvik, Måsøy, Salangen, Båtsfjord, Berlevåg, Nordkapp, Hasvik and Vardø. Despite both Vardø and Honningsvåg (in Nordkapp municipality) are registered as Norwegian towns, we argue that the number of inhabitants (about 2,000 in each town) and their location support the classification as rural areas. The mean number of inhabitants during study period (2007–2010) was 18,840 (51.2%) and 17,987 (48.8%) in the Sami and non-Sami group, respectively. Details are shown in Table I. The female/male ratio was 0.94 and 0.95 in the Sami and the control group, respectively.
Fig. 1.
The map of northern Norway and the Sami and non-Sami-speaking municipalities.
Table I.
The number of inhabitants in Sami and Non-Sami groups during study period
| Inhabitants | ||
|---|---|---|
| Year | Sami group | Non-Sami group |
| 2007 | 18,968 | 18,208 |
| 2008 | 18,891 | 18,043 |
| 2009 | 18,751 | 17,849 |
| 2010 | 18,751* | 17,849* |
| Mean (2007–2010) | 18,840 | 17,987 |
The 2010 figures were not available. The 2009 ones were therefore employed.
Statistical analysis and authorisation
Individual patient referral data was imported from the patient administrative system (PAS) in all hospital trusts in Northern Norway and the Microsoft Excel 2002 version was employed for the final database. The data was depersonalized and made anonymous before exportation to the Centre for Clinical Documentation and Evaluation (SKDE) at the NNRHA trust. Characteristics of the municipalities in terms of population, age groups and gender were derived from Statistics Norway (www.ssb.no). Statistical Package for Social Science (SPSS) version 16.0 was employed for statistical analysis. The comparison between groups (Sami and non-Sami) with regard to frequency of referrals were based on age adjusted rates (number of referrals 2007–2010/Population 2007–2010*1,000). One way analysis of variance (ANOVA) was employed for the comparison between groups with regard to the primary endpoint (referral rate during study period). The study was performed as a retrospective analysis of referral rate for the 2 municipality groups. As a quality of care analysis, no approval from the Regional Committee for Medical and Health Research Ethics (REK) was necessary. Significance was set to 5%. All tests were carried out 2-sided.
The referral ratio (RR) for each municipality was adjusted for age differences (RRa) and calculated employing the following formula:
Results
During the 4 years study period, a total of 504,292 referrals were sent from the PHC to the SHC in northern Norway. Nine per cent (45,634 referrals) of them were related to inhabitants in the Sami and the control group of municipalities. The referrals were similarly distributed between study groups (Sami 23,093 referrals – 50.6%, non-Sami group 22,541 referrals – 49.4%). Details are shown in Table II. Whereas there was a slightly dominance of males in the population, females constituted 57.7% (13.325 referrals) and 57.2% (12.904 referrals) of the referrals in the Sami and non-Sami group, respectively. Correcting for population differences, the female/male referral ratio was 1.45 and 1.41, respectively. The referral rate was lower among Sami and the mean annual total referral rate per 1,000 inhabitants (adjusted for gender and age) was 280 and 305, respectively. Details are shown in Table III. The difference was not statistically significant (p=0.624).
Table II.
The annual number of referrals according to gender and Sami and non-Sami speaking municipalities
| Sami group | Non-Sami group | |||||
|---|---|---|---|---|---|---|
| Year | Females | Males | Total | Females | Males | Total |
| 2007 | 3,355 | 2,583 | 5,938 | 3,171 | 2,332 | 5,503 |
| 2008 | 3,484 | 2,333 | 5,817 | 3,276 | 2,293 | 5,569 |
| 2009 | 3,245 | 2,435 | 5,68 | 3,28 | 2,568 | 5,848 |
| 2010 | 3,241 | 2,417 | 5,658 | 3,177 | 2,444 | 5,621 |
| Mean | 3,331 | 2,442 | 5,773 | 3,226 | 2,409 | 5,635 |
| Total | 13,325 | 9,768 | 23,093 | 12,904 | 9,637 | 22,541 |
Table III.
The gender and age adjusted referral rate per 1,000 inhabitants in the Sami and non-Sami speaking municipalities. The range is within the municipalities in the 2 groups
| Group | 2007 | Range | 2008 | Range | 2009 | Range | 2010 | Range |
|---|---|---|---|---|---|---|---|---|
| Sami group | 291 | 191–389 | 282 | 194–454 | 274 | 174–486 | 273 | 164–422 |
| Non-Sami group | 292 | 193–387 | 300 | 211–386 | 319 | 214–393 | 309 | 222–399 |
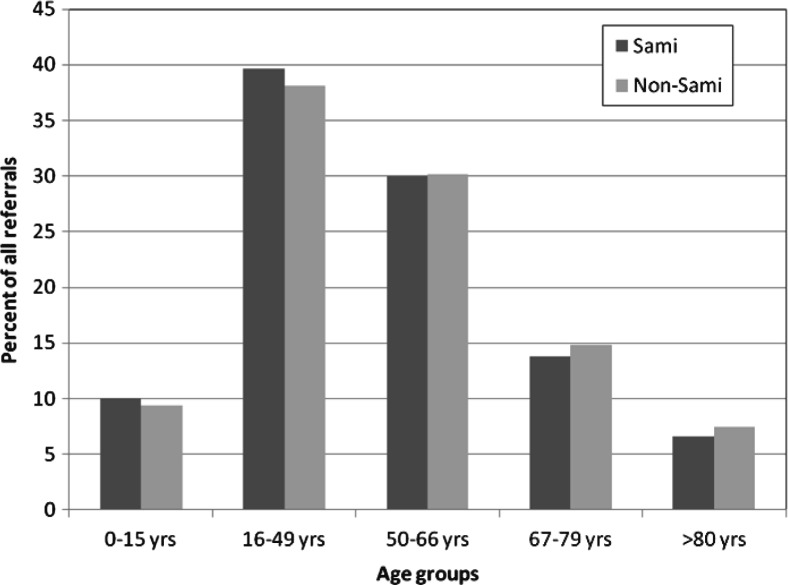
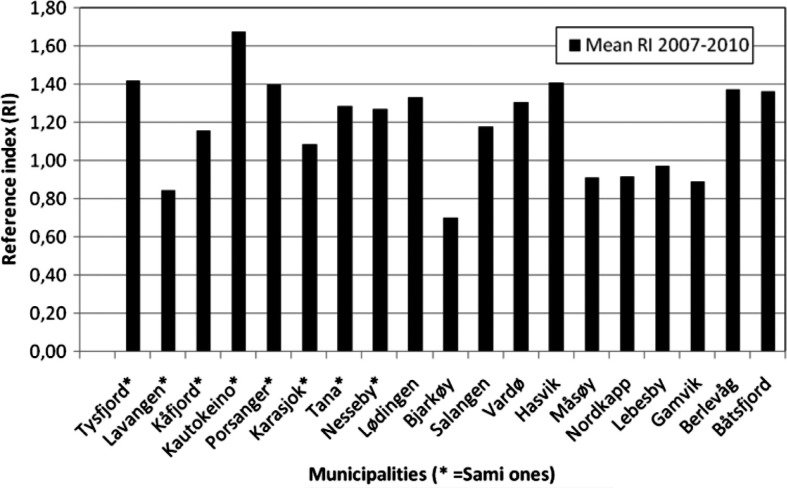
About 70% of all referrals were seen in the age group 16–66 years, and most frequently in the age group 16–49 years. Details are shown in Fig. 2. The age adjusted referral rate of the Sami population and the control group was 1.14 and 1.17 times that of the population of northern Norway. There was no statistically significant difference between the 2 groups (p=0.624). The difference from the north Norway mean figure (1.00) was observed in the population below 67 years of age. Details are shown in Table IV. Whereas the referral rate was slightly lower in the Sami group, the most striking finding was large inter-municipal variations in both groups. The inter-municipal variation did not differ between groups (p=0.230). A factor of 2 was observed between the municipality with the lowest and highest figure (Lavangen vs. Kautokeino and Bjarkøy vs. Båtsfjord) in both groups. No correlation with the share of Sami population and referral rate was observed. The 2 (Karasjok and Kautokeino) most Sami populated municipalities were in both ends of the scale. Details can be seen in Fig. 3.
Fig. 2.
The percentage of referrals in each age group.
Table IV.
The referral ratio according to age intervals in the Sami and non-Sami speaking municipalities in the time period 2007–2010. The figures of northern Norway in total was employed as 1.0
| Year | Group | 0–15 years | 16–49 years | 50–66 years | 67–79 years | ≥80 years | Total |
|---|---|---|---|---|---|---|---|
| 2007 | Sami | 1.23 | 1.12 | 1.25 | 1.01 | 0.89 | 1.15 |
| Non-Sami | 1.13 | 1.09 | 1.12 | 0.96 | 1.00 | 1.11 | |
| 2008 | Sami | 1.16 | 1.18 | 1.20 | 0.97 | 0.90 | 1.15 |
| Non-Sami | 1.11 | 1.15 | 1.18 | 0.99 | 0.95 | 1.15 | |
| 2009 | Sami | 1.21 | 1.17 | 1.18 | 0.94 | 0.91 | 1.14 |
| Non-Sami | 1.32 | 1.25 | 1.25 | 1.04 | 0.92 | 1.24 | |
| 2010 | Sami | 1.20 | 1.09 | 1.21 | 0.99 | 1.10 | 1.13 |
| Non-Sami | 1.30 | 1.22 | 1.16 | 0.94 | 1.07 | 1.19 | |
| 2007–2010 | Sami | 1.20 | 1.14 | 1.21 | 0.98 | 0.95 | 1.14 |
| Non-Sami | 1.22 | 1.18 | 1.18 | 0.98 | 0.98 | 1.17 |
Fig. 3.
The mean age and gender adjusted reference ratio (northern Norway=1.0) in the time period 2007–2010 in all municipalities. The Sami-speaking municipalities are marked with *.
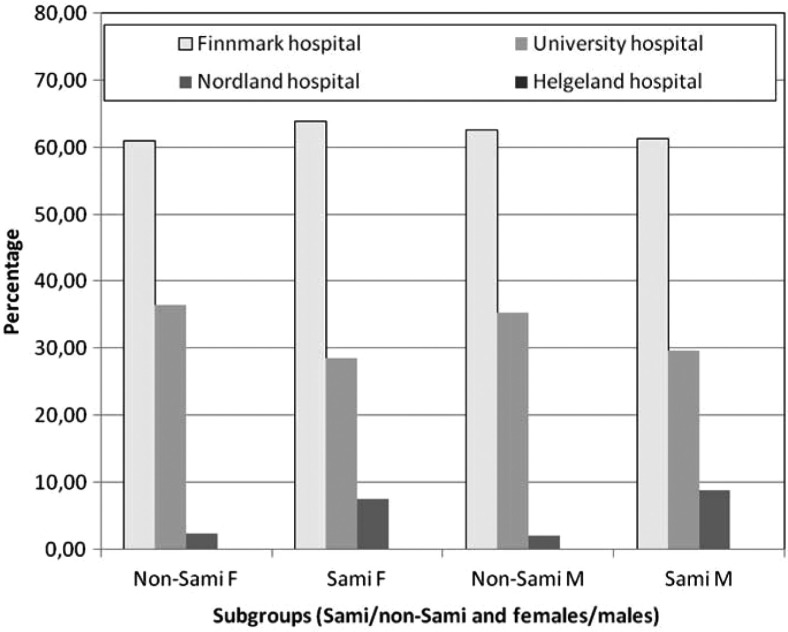
Two-thirds of the referrals were sent to the Finnmark hospital trust and one-third to the University hospital of north Norway trust. The share was similar in both groups and among both gender. Details can be seen in Fig. 4. There were very few referrals to the southern located hospital trust (Helgeland hospital trust). This strongly indicates that GPs in both municipality groups were loyal to their local hospital trust when referring patients.
Fig. 4.
The percentage of referrals related to the 4 hospital trusts in northern Norway.
Discussions
The age adjusted referral rate in the Sami population and the control group was 1.14 and 1.17 times that of the total population of northern Norway. There was no significant difference between the 2 groups. The difference from north Norwegians in general was observed in the population below 67 years of age. Females were more commonly referred than males. A significant inter-municipality variation was observed in both groups. GPs in both municipality groups were loyal to their local hospital trust as almost all patients were referred to the Finnmark and University hospital trusts.
Despite the Sami municipalities employed the Sami language, the share of Sami people or the percentage having Sami as their mother tongue was not known in the Sami or the control group. However, a Gallup poll back in October 2000 asked people in Finnmark if they could speak Sami and included 5 municipalities from the Sami group and 8 from our control group. The result was 71 and 6%, respectively. This result supports our classification of the 2 groups as Sami and non-Sami.
We had access to all somatic referrals from the primary health care in northern Norway during study period. Consequently, an excellent overview on the macro level concerning referrals and referral index was possible. However, we had no data with regard to psychiatric diseases. Furthermore, any sub-classification of the somatic referrals was not possible due to various clinical and departmental structures within the hospital trusts. Even the subgroups surgery and internal medicine could not be identified properly. Furthermore, the handling of the referrals within hospital is of great interest. However, this information was not available. Furthermore, hospitals were not allowed to register patients on ethnic background. Consequently, we had no data on Sami referrals and/or patients. Sami-speaking municipalities was therefore selected as a surrogate.
Whereas we revealed no difference between groups, several studies (8–13) have documented ethnic minorities having later and/or less access to SHC. Mukadam and colleagues (8) documented that minority ethnic elders presented later to UK dementia services than others. Langford et al. (9) revealed that compared with Whites, Blacks and Hispanics were less likely to have heard of a clinical trial. A British study (10), reported similarly that awareness of breast and cervical cancer screening was high in the White and low in ethnic minority groups. Among US stroke survivors, Levine and colleagues (11) documented Mexican Americans and Blacks reporting worse access to physician care and medications than whites. In a review analysis (12) the authors concluded white children more likely to undergo tympanostomy tube insertion compared to Black or Hispanic children. McGarvey and colleagues (13) analysed residents living in Appalachian countries in Virginia and concluded that they did not receive adequate health care, even those with health insurance.
With regard to emergency and intensive care, race and ethnicity does not seem to have any influence on access to care (14,15). Focusing psychiatric diseases, unequal access for minority groups has been revealed (16,17). Thomas et al. (16) observed in Texas US that depressed white students were more likely than depressed minority youth to report having received treatment for depression. Similarly, Cooper and colleagues (17) observed in 3 English cities an increased risk of self-harm among young Black females, but fewer of them received psychiatric care. Lakso and colleagues (18) documented that persistently worried patients after a GP consultation reported more anxiety than others and expected more often further medical examinations. Knowing that most Sami have a different native language and culture that may cause threshold, counter, queue and cultural challenges when assessing the health care (2), we anticipated more anxiety and a raised number of referrals from this study group, but no difference was revealed.
We observed large inter-municipal variations in referral rate. This may be due to variations in GP practices and health care infrastructure in the municipalities (1,19–21). Dijk and co-workers (1) revealed that GP practices performing more minor surgery interventions had a lower referral rate for patients with a laceration/cut and those with a sebaceous cyst. However, no difference was observed with regard to GP consultations for benign neoplasm skin/nevus. A female majority (58%) with regard to referrals was also observed by Raymont et al. (21) who analysed New Zealand GPs’ non-urgent referrals to surgeons. Stoves and colleagues (19) explored an electronic consultation between SHC and GPs as an alternative to hospital referral for patients with chronic kidney disease in UK. The intervention caused a significant reduction in referrals. Another strategy has been the improvement of collaboration across organisational boarders by a focus on the referral process (20). In this strategy, Heimly (20) argue for the implementation of GPs in part time positions as practice consultants in hospitals. The authors argue that this has been fundamental for the improvement of understanding of each other's needs and the work processes between collaborating actors. Increased competition between GPs and access to low level specialised care can influence on referral index. Tjerbo (22) analysed this topic and the tests revealed that increased competition reduces the use of ambulatory care, while the effects on the use of in-patient services was unaffected. Sørensen and co-workers (23) analysed the expenditures related to GP services and run a multilevel analysis of 2,123 GPs within 15 Danish counties. They concluded that 38% of health care expenditures were associated with GP practices and referrals to specialised care were the main source of variation in GP initiated expenditures. Consequently, they concluded reforms aiming to reduce GP initiated expenditures should focus on general practice access to low level specialised care. Learning groups may reduce referral rate. Kvaerner and Helgaker (24) analysed otitis media referrals and concluded that GPs without speciality, availability to practicing specialist and heavy work load all increased referral. Based on their findings, they suggested that learning groups contribute to update knowledge in primary care and fewer referrals to specialists.
A slightly lower referral index in the Sami group could be explained by a lower risk of cancer among the Sami (25). However, when contracting a cancer, they experienced the same service of radiotherapy as the control group (25).
Conclusion
In the future, hopefully more data on subgroup level will be available and further analysis should be performed. The significant inter-municipality variations with regard to referral index within both study groups call for future studies identifying and clarifying possible explanations. This study documents that people living in Sami-speaking municipalities are not more or less commonly referred to the somatic specialist health care than comparable municipalities within northern Norway. The strategic goal of equal availability to SHC for all inhabitants in the region has been successful.
Acknowledgements
The authors wish to thank Frank Olsen and Lise Balteskard at the Centre for Clinical Documentation and Evaluation (SKDE), NNRHA trust for the assistance in accessing data from the National Patient Registry (NPR) and their useful suggestions.
Conflict of interest and funding
The authors declare no conflict of interest and financial support came from the Northern Norway Regional Health Authority.
References
- 1.van Dijk CE, Verheij RA, Spreeuwenberg P, Groenewegen PP, de Bakker DH. Minor surgery in general practice and effects on referrals to hospital care: observational study. BMC Health Serv Res. 2011;11:2. doi: 10.1186/1472-6963-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haldorsen T, Tynes T. Cancer in the Sámi population of North-Norway 1970–97. Eur J Cancer Prev. 2005;14:63–68. doi: 10.1097/00008469-200502000-00009. [DOI] [PubMed] [Google Scholar]
- 3.International Labour Organization (ILO) Geneva: International Labour Organization (ILO); 1989. C169 Indigenous and tribal peoples convention, 1989. [cited 2011 Jan 19]. Available from: http://www.ilo.org/ilolex/cgi-lex/convde.pl?C169. [Google Scholar]
- 4.Nystad T, Melhus M, Lund E. The monolingual Sámi population is less satisfied with the primary health care. Tidsskr Nor Laegeforen. 2006;126:738–40. In Norwegian. [PubMed] [Google Scholar]
- 5.Broderstad AR, Melhus M, Lund E. Iron status in a multiethnic population (age 36–80 yr) in northern Norway: the SAMINOR study. Eur J Haematol. 2007;79:447–54. doi: 10.1111/j.1600-0609.2007.00929.x. [DOI] [PubMed] [Google Scholar]
- 6.Ministry of Health and Care services. The report no 47 (2008–2009) to the Storting. Oslo: Ministry of Health and Care services; 2009. The coordination reform. Proper treatment at the right place and right time; pp. 1–149. [Google Scholar]
- 7.Department of Health. Oslo: Department of Health, Departments’ service centre; 2009. The Northern Norway Regional Health Authority's mission 2009; pp. 1–34. [Google Scholar]
- 8.Mukadam N, Cooper C, Basit B, Livingston G. Why do ethic elders present later to UK dementia services? A qualitative study. Int Psychogeriatr. 2011;23:1070–7. doi: 10.1017/S1041610211000214. [DOI] [PubMed] [Google Scholar]
- 9.Langord A, Resnicow K, An L. Clinical trial awareness among racial/ethnic minorities in HINTS 2007. Sociodemographic, attitudinal, and knowledge correlates. J Health Commun. 2010;15(Suppl 3):92–101. doi: 10.1080/10810730.2010.525296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robb K, Wardle J, Stubbings S, Ramirez A, Austoker J, Macleod U, et al. Ethnic disparities in knowledge of cancer screening programmes in the UK. J Med Screen. 2010;17:125–31. doi: 10.1258/jms.2010.009112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levine DA, Neidecker MV, Kiefe CI, Karve S, Williams LS, Allison JJ. Racial/ethnic disparities in access to physician care and medications among US stroke survivors. Neurology. 2011;76:53–61. doi: 10.1212/WNL.0b013e318203e952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith DF, Boss EF. Racial/ethnic and socioeconomic disparities in the prevalence and treatment of otitis media in children in the United States. Laryngoscope. 2010;120:2306–12. doi: 10.1002/lary.21090. [DOI] [PubMed] [Google Scholar]
- 13.McGarvey EL, Leon-Verdin M, Killos LF, Guterbock T, Cohn WF. Health disparities between Appalachian and non-Appalachian counties in Virginia USA. J Community Health. 2011;36:348–56. doi: 10.1007/s10900-010-9315-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erickson SE, Vasilevskis EE, Kuzniewicz MW, Cason BA, Lane RK, Dean ML, et al. The effect of race and ethnicity on outcomes among patients in the intensive care unit. A comprehensive study involving socioeconomic status and resuscitation preferences. Crit Care Med. 2011;39:429–35. doi: 10.1097/CCM.0b013e318206b3af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SL, Shekherdimian S, Chiu VY. Effect of race and socioeconomic status in the treatment of appendicitis in patients with equal health care access. Arch Surg. 2011;146:156–61. doi: 10.1001/archsurg.2010.328. [DOI] [PubMed] [Google Scholar]
- 16.Thomas JF, Temple JR, Perez N, Rupp R. Ethnic and gender disparities in needed adolescent mental health care. J Health Care Poor Underserved. 2011;22:101–10. doi: 10.1353/hpu.2011.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper J, Murphy E, Webb R, Hawton K, Bergen H, Waters K, et al. Ethnic differences in self-harm, rates, characteristics and service provision: three-city cohort study. Br J Psychiatry. 2010;197:212–8. doi: 10.1192/bjp.bp.109.072637. [DOI] [PubMed] [Google Scholar]
- 18.Laakso V, Niemi PM, Gronroos M, Karlsson H. Relieved after GP's consultation? Change in the complaint-related worry of young adult patients. Psychol Health Med. 2008;13:291–302. doi: 10.1080/13548500701487705. [DOI] [PubMed] [Google Scholar]
- 19.Stoves J, Connolly J, Cheung CK, Grange A, Rhodes P, O'Donoghue D, et al. Electronic consultation as an alternative to hospital referral for patients with chronic kidney disease: a novel application for networked electronic health records to improve the accessibility and efficiency of healthcare. Qual Saf Health Care. 2010;19:e54. doi: 10.1136/qshc.2009.038984. [DOI] [PubMed] [Google Scholar]
- 20.Heimly V. Collaboration across organizational boarders, the referral case. Stud Health Technol Inform. 2010;157:106–11. [PubMed] [Google Scholar]
- 21.Raymont A, Morgan S, McLeod D, Dowell A, van Rij A, Cumming J, et al. New Zealand general practitioners’ non-urgent referrals to surgeons: who and why? N Z Med J. 2008;121:57–64. [PubMed] [Google Scholar]
- 22.Tjerbo T. Does competition among general practitioners increase or decrease the consumption of specialist health care? Health Econ Policy Law. 2010;5(Pt 1):53–70. doi: 10.1017/S1744133109990156. [DOI] [PubMed] [Google Scholar]
- 23.Sørensen TH, Olsen KR, Gyrd-Hansen D. Differences in general practice initiated expenditures across Danish local health authorities – a multilevel analysis. Health Policy. 2009;92:35–42. [Google Scholar]
- 24.Kvaerner KJ, Helgaker AB. Otitis media referrals – the general practitioner perspective. Int J Pediatr Otorhinolaryngol. 2007;71:1219–24. doi: 10.1016/j.ijporl.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 25.Norum J, Olsen A, Småstuen M, Nieder C, Broderstad AR. Health consumption in Sami-speaking municipalities with regard to cancer and radiotherapy. Int J Cicumpolar Health. 2011;70:319–28. doi: 10.3402/ijch.v70i3.17832. [DOI] [PubMed] [Google Scholar]