Abstract
Background
For more than 50 years, Community Health Aides and Community Health Practitioners (CHA/Ps) have resided in and provided care for the residents of their villages.
Objectives
This study is a systematic description of the clinical practice of primary care health workers in rural Alaska communities. This is the first evaluation of the scope of health problems seen by these lay health workers in their remote communities.
Study design
Retrospective observational review of administrative records for outpatient visits seen by CHA/Ps in 150 rural Alaska villages (approximate population 47,370).
Methods
Analysis of electronic records for outpatient visits to CHA/Ps in village clinics from October 2004 through September 2006. Data included all outpatient visits from the Indian Health Service National Patient Information Reporting System. Descriptive analysis included comparisons by region, age, sex, clinical assessment and treatment.
Results
In total 272,242 visits were reviewed. CHA/Ps provided care for acute, chronic, preventive, and emergency problems at 176,957 (65%) visits. The remaining 95,285 (35%) of records did not include a diagnostic code, most of which were for administrative or medication-related encounters. The most common diagnostic codes were: pharyngitis (11%), respiratory infections (10%), otitis media (8%), hypertension (6%), skin infections (4%), and chronic lung disease (4%). Respiratory distress and chest pain accounted for 75% (n=10,552) of all emergency visits.
Conclusions
CHA/Ps provide a broad range of primary care in remote Alaskan communities whose residents would otherwise be without consistent medical care. Alaska's CHA/P program could serve as a health-care delivery model for other remote communities with health care access challenges.
Keywords: rural health care, community health workers, health aides, primary care, CHA/P, Alaska Native Health Care
The 1978 World Health Organization Alma Ata Declaration envisioned universally accessible health care for all individuals and communities, with Community Health Workers (CHWs) a cornerstone in achieving that goal (1). The northern circumpolar region is home to a diverse group of peoples with unique traditions, health care organizations, and political systems who share many challenges of health care access. The communities of the circumpolar region face many hurdles including geographic and climatic constraints, the need for health care delivery that is respectful of indigenous cultures, and difficulties in recruiting and retaining qualified health care professionals to provide care in remote locations.
Circumpolar nations have addressed these health care delivery challenges in a variety of ways. In northern Canada (Yukon, Northwest Territories, Nunavut), nurses are the main providers of primary medical care, although some community health representatives and midwives may be included among the staff (2,3). Family physicians are located in regional centres, and more specialized care is primarily located in the south of the country (3).
Nurses have an important role in both Sweden and Finland, frequently serving as a patient's first contact with the health system. Nurses may provide injections, remove sutures, provide maternal and child health care, and in some settings provide acute care prior to, or instead of, a patient's consultation with a physician (4–6). In Sweden, Finland and Norway, regional municipalities or county councils are responsible for providing primary care. General practitioners are based in regional health centres and serve specific geographic areas. For specialized care, a health centre physician can refer to a hospital within the municipality, while more complicated treatment is referred to a centralized hospital (4–6).
Small villages in Greenland are served by a health assistant or village health worker. Larger communities of approximately 300 residents have a village clinic staffed with a nurse and frequently several emergency beds. These communities are part of Greenland's 16 autonomous health districts ranging in population from 600 to 15,000, each with a district health care centre staffed by at least 1 physician. Rural communities may also be visited by dentists, medical specialists, midwives, and other healthcare professionals. Patients requiring more specialized care are referred to the National Hospital in Nuuk, or to treatment at clinics in Denmark (7,8).
The first contact for rural health care in Northern Russian villages is the health post or feldsher (medical assistant)/midwife station. Nurses and feldshers may receive an additional 2 years of training beyond nursing school and provide immunizations, health checks and routine prenatal and newborn care. If there is a need for prescriptions, patients are referred to a health centre staffed by a physician. More complex cases are referred to a district or regional level polyclinic or hospital (9).
Like other circumpolar regions, Alaska also has substantial challenges to providing access to health care in its remote communities. Sixty percent of Alaska's indigenous people live in small villages of 20–1700 people scattered across 1,481,473 km2 (10). Most of these villages are not accessible by road, and can be reached only by airplane or boat in the summer and by airplane or snow machine in the winter. Prior to the inception of the Community Health Aide Program in the 1950s, residents of Alaska village communities waited for infrequent visits from itinerant physicians and nurses, made costly trips to larger towns, or relied on self-care.
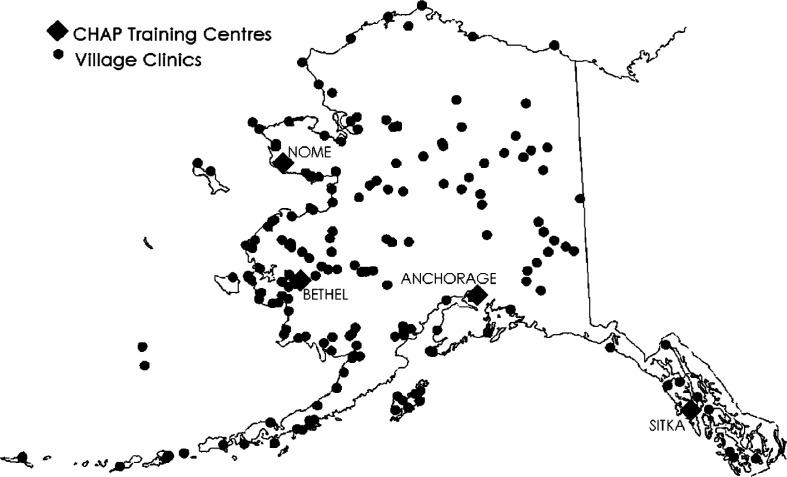
Alaska's Community Health Aide (CHA/P) Program began with the provision of village-based oral antibiotic treatment during the tuberculosis epidemics of the 1940s and 1950s, then became a formal Indian Health Service-funded program in 1968 (11,12). Since then, the Community Health Aide Program has grown throughout the state to include well defined roles, selection criteria, curricula, training standards and certification at 5 different levels: Community Health Aide I–IV (CHA) and Community Health Practitioner (CHP) (13). CHA/Ps now provide emergency, acute, chronic, and preventive health care for all ages. They are the front-line providers in a comprehensive, integrated Alaska Tribal Health System. Over 550 village-based Community Health Aides and Community Health Practitioners (CHA/Ps) currently provide care for 50,000 patients with an estimated 250,000 clinical encounters per year in 178 remote villages scattered throughout Alaska (11) (Figure 1).
Fig. 1.
Community health aide/practitioner village clinics and training centres in Alaska.
Community Health Aides and Community Health Practitioners are hired by their communities and tribal councils. They are supervised by and employees of Tribal Health Organizations who operate a Community Health Aide Program in Alaska under the Indian Self-Determination and Education Assistance Act, Public Law 93-638 (12). Their practice is based on the Alaska Community Health Aide/Practitioner Manual (CHAM), which directs all patient encounters (14). The CHAM provides scripted questions and directed exams for specific patient complaints. It guides the CHA/P towards the best assessment and treatment for the patient's presented problem. While CHA/Ps practice remotely, they work with the supervision and support of physicians and mid-level providers in regional health clinics and hospitals often several hundred air miles away.
The training of CHA/Ps is governed by the Federal Community Health Aide Program Certification Board Standards and Procedures as authorized under amendment 119 to the Indian Health Care Improvement Act (15). Training prerequisites include demonstration of a 6th grade minimum mathematics and English proficiency; however 94% of CHA/Ps have graduated from high school (16). After being hired, training occurs over a period of approximately 2 years while on the job and takes place in 1 of 4 regional centres. CHA/Ps receive 15 weeks of formal didactic and clinical training divided into 4 sessions, with supervised clinical practice completed between sessions. Session training includes an introduction to all body systems, recognition and stabilization of emergency situations, and treatment for common acute outpatient problems. CHA/Ps also receive training on maternal and child health care, behavioural health, common chronic problems, and procedures such as suturing, starting and maintaining intravenous fluid therapy, and some laboratory tests. At the end of 4 sessions of training, CHAs may complete an additional weeklong evaluation course and final exam, which if finished successfully allows them to hold the title of Community Health Practitioner (CHP). Certification of Health Aides at all levels is provided by the Federal Community Health Aide Program Certification Board. In addition to session training, all CHA/Ps are required to maintain emergency medical skills including basic life support and initial trauma stabilization and treatment. After the initial training series is finished, CHA/Ps are required to maintain their skills by attending 48 hours of continuing education every 2 years (15). Throughout training, clinical practice and continuing education, CHA/P training emphasizes hands-on acquisition of skills and knowledge.
Although the CHA/P program has been in existence for 50 years, this study is the first comprehensive assessment of the scope of health problems routinely addressed by CHA/Ps. These data will assist CHA/P program evaluation and training, as well as improve the understanding and recognition of this longstanding and successful program for possible adaptation in other underserved or remote settings.
Material and methods
This report is based on record-level data extracted from records written by village CHA/Ps. These records were coded at the regional health centre and submitted electronically into the Indian Health Services’ National Patient Information Reporting System (IHS NPIRS) (17). Data were made available by request from the Office of Information Technology at IHS NPIRS and included only patient care given by a CHA/P in a village clinic.
This project was a program evaluation, not research, as determined by the Alaska Area Institutional Review Board. Permissions to utilize data for this evaluation were obtained from the Association of Alaska Community Health Aide Program Directors, Association of Tribal Health Directors and individual Tribal Health Directors from each participating organization.
Patient visit data, without individual identifiers, were examined from 11 of the 27 (40.7%) Tribal Health Organizations employing CHA/Ps between October 1, 2004 and September 30, 2006. While only 40.7% of Tribal Health Organizations are included in this analysis, these organizations comprise 92% of the CHA/P work force and serve 90% of all patients served by village Community Health Aides and Practitioners in Alaska (18,19).
For a patient encounter to be included in this review, care must have been provided directly by a CHA/P and the record must have the date of visit, age, sex, and a diagnosis or procedure code (International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). The first diagnosis for a visit fitting inclusion criteria was used for this analysis. ICD-9-CM codes were grouped into categories consistent with CHAM assessments by the author and the list is available on request. SAS Statistical Software, 9.1 (SAS Institute, Inc., Cary, NC) was used to summarize CHA/P diagnoses by region, age group, sex, clinical diagnosis, and treatments provided.
In order to evaluate emergency care, all diagnostic codes listed in an NPIRS encounter were reviewed for inclusion as potential emergencies or urgencies. These were categorized into larger groups for analysis. (A list of ICD-9-CM codes included with grouping is available in Appendix 1.) A diagnosis that was an emergency or urgency will appear both in the major categories of diagnoses and in the urgency/emergency category as seen in Tables IV and Table V.
Table IV.
Clinical diagnoses made by Alaska community health aides and community health practitioners in data recorded in FY 2005–FY 2006
| Percentage of all Visits | |||
|---|---|---|---|
| Major Diagnostic Categories | Cummulative (%) | ||
| Rank | n=175,992 | ||
| 1 | Respiratory/Ear, Nose, Throat and Sinus problems | 40.8 | |
| 2 | Circulatory problems | 8.9 | |
| 3 | Skin problems | 6.1 | |
| 4 | Preventive care | 5.4 | |
| 5 | Injuries | 5.3 | |
| 6 | Digestive/Abdominal | 5.2 | |
| 7 | Musculoskeletal problems | 4.4 | |
| 8 | Fever | 2.3 | ≈77 |
| 9 | Eye problems | 3.2 | |
| 10 | Pregnancy | 2.9 | |
| 11 | Nervous system | 2.2 | |
| 12 | Genital problem | 2.1 | ≈90 |
| 13 | Infections not otherwise classified | 2.0 | |
| 14 | Mental health problems | 1.6 | |
| 15 | Endocrine disorders | 1.6 | |
| 16 | Urinary system | 1.5 | |
| 17 | Dental problems | 1.5 | |
| 18 | Paediatric problems | 0.8 | |
| 19 | All other problemsa | 2.8 | |
| Total percent | 100 | ||
All other problems include severe allergic reactions, fatigue, death, end of life care, pain, mass, oedema, hypothermia, sarcoid, anaemia and other hematologic disorders, non cancer breast problems, cancer and nutritional problems and others. Complete list available on request.
Table V.
Respiratory problems found in community health aide and community health practitioner encounters and recorded in Alaska, 2005–2006
| Respiratory Problems | Percentage of All Respiratory Problems |
|---|---|
| Nose/Throat/Sinus | n=71,742 |
| Pharyngitis/Tonsillitisa | 26.0 |
| Otitis Mediab | 18.7 |
| Upper Respiratory Infection (URI)c | 14.0 |
| Bronchitis/Bronchiolitis/Cough | 11.3 |
| Chronic Lung Disease | 8.6 |
| Sinusitisd | 4.0 |
| Otitis Externa, ear drainage, or pain | 3.7 |
| Asthma/Wheezing/Reactive Airway Disease | 3.0 |
| Pneumonia and pneumonia follow up | 3.3 |
| Respiratory Distresse | 2.6 |
| Other respiratory problemsf | 2.8 |
| Other ear problemsg | 0.8 |
| Total percent of all respiratory problems | 100 |
Includes peritonsillar abscess and laryngitis.
Includes mastoiditis, acute, chronic, and serous otitis media; and tympanic membrane perforation.
Includes rhinitis and allergy symptoms.
Includes sinus pain.
Includes shortness of breath, respiratory distress and breathing problem.
Flu, Tuberculosis, other infections, other problems and exam.
Other ear problems include: foreign bodies in the ear; ear injury; hearing loss; vertigo; ear exam without diagnosis; unspecified disorders of the ear; other disorders of ear; tinnitus.
Results
A total of 272,242 CHA/P visits from 150 villages were recorded in IHS NPIRS between October 1, 2004 and September 30, 2006. Of these encounters, 197,190 (72.4%) had at least 1 recorded clinical diagnosis (Table I). While the focus of this report is on clinical practice, 75,052 (28%) of the 272,242 CHA/P records examined did not contain a recorded diagnosis. Most (>98%) of these visits without a diagnostic code were for pharmacy activities, including medication refills and delivering medications. In addition, of the 197,190 encounters with diagnoses, 11,832 were recorded as a diagnosis of “medication refill” (ICD-9 CM code V68.1). Together this means 86,884 (32%) of total workload was for medication and/or pharmacy related activities. Other nonclinical reasons for visits to the clinics included 7,040 (4%) for administrative tasks (ICD-9 CM codes V68.0, 68.2) and 2,326 (1%) for laboratory tests without a specific diagnosis.
Table I.
Distribution of reviewed community health aide and community health practitioner encounters with assessments by tribal health organization in Alaska, FY 2005, FY 2006
| Encounters with Diagnosis | |
|---|---|
| Tribal Health Organization | n=197,190 (%) |
| Bristol Bay Area Health Corporation (BBAHC) | 28,289 (14.4) |
| Council of Athabascan Tribal Governments (CATG) | 1,207 (0.6) |
| Chugachmiut | 2,562 (1.3) |
| Eastern Aleutian Tribes (EAT) | 851 (0.4) |
| Maniilaq Association | 3,316 (1.7) |
| North Slope Borough | 4,535 (2.3) |
| Department of Health and Human Services (NSB-DHSS) | |
| Norton Sound Health Corporation (NHSC) | 6,295 (3.2) |
| Southcentral Foundation (SCF) | 1,783 (0.9) |
| SouthEast Alaska Regional Health Consortium (SEARHC) | 2,761 (1.4) |
| Tanana Chiefs Conference (TCC) | 4,336 (2.2) |
| Yukon Kuskokwim Health Corporation (YKHC) | 141,255 (71.6) |
| Total | 197,190 (100) |
Demographics
Females accounted for 57% of CHA/P encounters while 43% were with male patients. The Indian Health Service 2000 estimate of the Alaska Native population shows it evenly divided 50.3% male and 49.7% female (19). This suggests that CHA/P patient encounters are more likely to be female than might be expected, or that females are more likely to seek health care than males.
Table II shows that 45% of CHA/P encounters are persons less than 20 years old while 43% are 20 to 65 years old and that elderly (65+ years old), account for only 12% of encounters. Of the total Alaska Native population, 41.7% is less than 20 years old and 5.5% is older than 65 years (20). Nationally, in the USA, 12.9% of the population is over 65 years old and accounts for 26% of all ambulatory care visits (21).
Table II.
Age distribution for community health aide and community health practitioner encounters in Alaska, FY 2005, FY 2006
| Encounters | |
|---|---|
| Age Group | n=197,190 (%) |
| <1 year | 13,874 (7.0) |
| 1–5 years | 31,271 (15.9) |
| 6–12 years | 22,717 (11.5) |
| 13–19 years | 20,285 (10.3) |
| 20–65 years | 85,325 (43.3) |
| 65 + years | 23,718 (12.0) |
Diagnoses and assessments
The top 20 diagnoses account for 64% of total visits, indicating the CHA/Ps see a broad range of health care problems (Table III).
Table III.
Most frequent diagnoses made by Alaska community health aides and community health practitioners in data recorded in FY 2005, FY 2006
| Encounters | |
|---|---|
| Diagnoses | n=175,992 (%) |
| Pharyngitis | 18,653 (11) |
| Otitis Media | 13,360 (8) |
| Hypertension | 11,000 (6) |
| Upper Respiratory Infection | 10,044 (6) |
| Bronchiolitis/Bronchitis/Cough | 7,891 (4) |
| Skin Infections | 6,179 (4) |
| Chronic Lung Disease | 6,170 (4) |
| Arthritis and Joint pain | 4,649 (3) |
| Lacerations | 4,322 (2) |
| Fever | 4,132 (2) |
| Conjunctivitis | 3,301 (2) |
| Abdominal pain | 3,045 (2) |
| Sinusitis | 2,870 (2) |
| Acute Gastroenteritis, Diarrhoea, and/or Vomiting | 2,769 (2) |
| Immunizations | 2,462 (1) |
| Pneumonia | 2,367 (1) |
| Diabetes | 2,263 (1) |
| Family Planning | 2,216 (1) |
| Asthma | 2.152 (1) |
| Pregnancy Routine Care | 2,133 (1) |
| Total | 111,978 (64) |
Table IV shows diagnoses grouped by body systems. This provides a better view of the scope of health problems for which patients see a CHA/P. Several diagnostic groups are described in subsequent tables. Respiratory and Ear, Nose, and Throat problems comprise 40% of all visits. Pharyngitis and otitis media are seen frequently, accounting for 20% of all visits. Table V shows that while most of the respiratory visits were acute infectious problems, almost 12% were for chronic lung problems including asthma.
The circulatory system comprised the second largest category of health problems (see Table IV). In contrast to respiratory visits, encounters for circulatory issues were mostly for chronic problems and most frequently for hypertensive care. Importantly, about 10% of circulatory visits were for acute ischemic symptoms (see Table VI).
Table VI.
Circulatory problems found in community health aide and community health practitioner encounters and recorded in Alaska, 2005–2006
| Percentage of All Circulatory Problems | |
|---|---|
| Circulatory Problems | n=15,708 |
| Hypertension | 69.9 |
| Acute Ischemic problems | 11.6 |
| Heart Rate problem | 5.0 |
| Lipid disorders | 4.7 |
| Heart Disease chronic care | 3.3 |
| Rheumatic Fever | 2.8 |
| Other circulatory problemsa | 2.7 |
| Total percent of all circulatory problems | 100 |
Other circulatory problems include: valvular disease, problems with arteries and veins, circulatory exam, non-traumatic hypotension, pericarditis, endocarditis, transplants, undiagnosed murmurs, etc.
Skin problems, preventive care, and injuries are other frequent reasons to visit a CHA/P. Table VII shows about half of all skin problems were infections. Most infections were cellulitis or abscesses. About 5% of all visits were for preventive care. This category included immunizations, well child care, patient education and home visits (see Table VIII). Care for minor injuries occupied 5% of clinic visits with lacerations, sprains, and burns being the most frequent minor injury. Common problems of the digestive system cared for by CHA/Ps included gastroenteritis, gastroesophageal reflux and abdominal pain. Details are described in Table IX.
Table VII.
Skin problems found in community health aide and community health practitioner encounters recorded in Alaska, 2005–2006
| Percentage of All Skin Problems | |
|---|---|
| Skin Problems | n=10,654 |
| Infections | 58.2 |
| Dermatitis | 10.7 |
| Acne | 0.7 |
| Other skin problemsa | 30.4 |
| Total percent of all skin problems | 100 |
Other skin problems include skin lesions, nail problems, insect bites, pruritus, hives, cysts, and foreign bodies.
Table VIII.
Preventive care found in community health aide and community health practitioner encounters recorded in Alaska, 2005–2006.
| Percentage of All Preventive Care | |
|---|---|
| Preventive Care | n=8,179 |
| Immunizations | 30.1 |
| Prophylaxisa | 24.4 |
| Recheck | 17.5 |
| Well Child Care | 12.7 |
| Medical Exam/Health Check | 8.7 |
| Patient education | 5.5 |
| Newborn Care | 0.6 |
| Total percent of all preventive care | 100 |
Mostly dental prophylaxis.
Table IX.
Digestive problems found in community health aide and community health practitioner encounters recorded in Alaska, 2005–2006
| Percentage of All Digestive/Abdominal Problems | |
|---|---|
| Digestive Problems | n=9230 |
| Abdominal pain | 33.0 |
| Gastroenteritis-like illnesses | 30.2 |
| Gastroesophageal Reflux Disease/Ulcer/Gastritis | 15.1 |
| Hepatitis and other liver disease | 10.2 |
| Constipation | 5.2 |
| Dehydration | 1.5 |
| Gastrointestinal Bleed | 1.4 |
| All othersa | 3.4 |
| Total percent of all digestive problems | 100 |
Other digestive problems include gallbladder disease, pancreatic problems, hernias, anal problems, and other gastrointestinal problems.
Emergencies and urgencies accounted for approximately 6% of all CHA/P patient encounters (see Table X). Although traumatic injuries occurred, most emergency encounters were respiratory, cardiac, or pregnancy-related. Community Health Aides and Practitioners play a critical role in recognizing a developing emergent situation and arranging treatment and transport in a timely fashion. While larger villages usually have more frequent emergencies, on average, each village clinic has at least 1 emergency every month.
Table X.
Urgencies and emergencies seen by Alaska community health aides and community health practitioners in data recorded in FY 2005–FY 2006
| FY 2005–2006 | Mean Serious Events Per Village Per Yr | |
|---|---|---|
| Serious Event | n=10,552 | n=150 |
| Respiratory distress | 5,007 | 16.7 |
| Acute Ischemic problems | 2,848 | 9.5 |
| Pregnancy-related emergenciesa | 549 | 1.8 |
| Dehydration | 520 | 1.7 |
| Paralysis & Stroke | 369 | 1.2 |
| Suicide/Suicide Attempt | 179 | 0.6 |
| Drug/Alcohol Withdrawal/Overdose | 178 | 0.6 |
| Gastrointestinal Bleed | 177 | 0.6 |
| Nosebleeds | 159 | 0.5 |
| Eye Trauma & serious problemsb | 139 | 0.5 |
| Peritonsillar abscess | 135 | 0.5 |
| Chest Injury | 29 | 0.1 |
| Hypotension | 96 | 0.3 |
| Gunshot injury | 62 | 0.2 |
| Allergic reaction severe | 45 | 0.2 |
| Central Nervous System infection | 24 | 0.1 |
| Death & End of Life care | 18 | 0.1 |
| Altered Level Of Consciousnessc | 18 | 0.1 |
| Total Events Identified | 10,552 | 35.2 |
| Total Number of Villages | 150 | |
| Total Visits | 175,992 |
Include: Deliveries, impending deliveries, active labour both preterm and term, premature rupture of membranes, early or late pregnancy bleeding, postpartum haemorrhage, ectopic pregnancy, severe puerperal infection, retained placenta, and newborn distress.
Include: Open wounds, burns, contusions of eyeball or surrounding tissue, injury to the optic nerve or its pathways, retinal detachments, and keratitis.
Non-alcohol or drug-related altered levels of consciousness.
Treatments and procedures
The 10 most common tests or procedures accounted for 98% of all procedures performed by CHA/Ps and were in rank order: oxygen saturation testing, antibiotic injections, immunizations other than influenza, phlebotomy, injury care, nebulizer therapy, other injections, respiratory testing (including peak expiratory flows), culture collection, and influenza immunizations. Injury care includes wound irrigation, packing, skin closure and splinting injured limbs.
Discussion
Community Health Aides and Community Health Practitioners are the frontline healthcare providers in remote Alaskan communities. Although the CHA/P program has formally existed since 1968, this report is the first state-wide assessment of CHA/Ps’ practice. CHA/Ps see a broad scope of health care problems on a regular basis, as documented above. Their care of patients is directed by their training, reference manual, and system procedures within an integrated referral system that includes physicians, regional hospitals, and a tertiary hospital. They are an important first point of contact for health care in the Alaska Tribal Health System.
The Community Health Aide Program's origin was to provide chronic tuberculosis medication to patients living in remote villages. During the 40 years of existence, the scope of care has expanded, but CHA/Ps continue to help with patient's chronic medication needs. The Community Health Aide/Practitioner Manual has specific sections that address follow-up of chronic problems, including evaluating patient health status, providing patient education and assisting with medication refills. From this study, we found nearly one-third of CHA/P practice involves assisting patients with their medications, including helping them obtain refills for management of chronic health problems. This is an important finding and has implications on work load and training. However, it is unclear from the methods we used if these visits were only for facilitating medication refills or if they also included an evaluation of the patient's status. Since these data were collected, some regional pharmacies have begun sending medication refills directly to patients via the US Postal Service. It remains to be seen how this will affect Community Health Aide workload.
Community Health Aides and Community Health Practitioners may be compared to Community Health Workers in the USA and elsewhere in the world. Within the literature we reviewed, we found a wide variety of definitions and duties for Community Health Workers. CHWs in countries such as Peru, Pakistan, and Iran provide direct patient care as do Alaska CHA/Ps (22–26). In the US in 2005, there were an estimated 121,000 Community Health Workers. They play an important role in patient education, advocacy and linking patients to medical providers (27–29). They have been employed to improve outcomes in diabetes, cancer screening, prenatal care, and childhood immunizations through counselling, linguistic and cultural translation, and by arranging transportation for patients and families (27,29,30). Brownstein describes Community Health Workers as “uniquely qualified to be connectors to the community because they generally live in the communities where they work and understand the social context of patients’ lives” (29). CHAPs are similar to Community Health Workers in that they typically live in the communities they serve; many work in the same village where they were raised from childhood. CHA/Ps, however, differ substantially from US Community Health Workers in that they provide direct patient care for acute illness, chronic diseases, preventive services, mental health and medical emergencies.
Limitations
Approximately 56% of CHA/P workload state-wide is entered into the Indian Health Service's Resource and Patient Management System (RPMS), an electronic health record, and exported to NPIRS (31). No provision was made to identify individuals who have repeat visits during the study period. The effects of multiple encounters by individuals may influence the rank and order of reported diagnosis. This might have increased the apparent number of visits for problems requiring follow-up. In addition, because we limited our review to the first diagnosis listed in NPIRS (except for emergency diagnoses), we have no certainty that we captured the most important diagnosis, or indeed, adequately described the full complexity of care provided by CHA/Ps. For example, a child who was seen primarily for otitis media and who also received preventive services such as well-child care or immunizations would register as only an otitis media visit. A more complete assessment of CHA/P practice could be obtained by using “any listed” diagnosis from the NPIRS data. The findings from this review should not be used to infer prevalence or incidence of specific diseases or conditions in the served population.
Conclusion
Uta Lehmann and David Sanders state “CHW programmes are not cheap or easy, but remain a good investment, since the alternative, in reality, is no care at all for the poor living in geographically peripheral areas”. They add, “We need to learn from examples of large-scale successful programmes in this regard, particularly providing longitudinal evidence of what works and what does not work” (32). Recently, Balcazar and others have advocated for integrating Community Health Workers into the full range of health care delivery (33). We believe that the longevity of the Community Health Aide Program and the wide range of their scope of practice points to the program as an example of how CHWs can be successfully integrated into a health care delivery system.
Further study of Alaska's Community Health Aide program should include qualitative research on how well-prepared students are for their clinical practice, what the most effective methods of instruction have been for preparing CHA/Ps, and the benefits and changes to practice and healthcare that have come with increased use of telemedicine. In addition, a systematic evaluation of patient health outcomes is warranted.
Since the inception of the CHA/P program, numerous health status indicators have dramatically improved among the Alaska Native population, including lower infant mortality, longer life expectancy, and dramatically lower rates of tuberculosis (34,35). While the CHA/P program cannot take full credit for these improvements, we believe that easy access to the health care system provided by village-based CHA/Ps has contributed substantially to these health gains. Prior to having local health care provided by CHA/Ps, village residents received only episodic care by itinerant providers, needed to travel to receive care, or did without trained medical care entirely. The expanded role of the Community Health Worker as demonstrated by Alaska's Community Health Aides and Community Health Practitioners can serve as a model for adaptation in other communities with challenging health care access both in the USA and elsewhere.
Acknowledgements
Many thanks to the following people and organizations for their collaboration and energy: Carolyn Craig, PA-C; Linda G. Curda, CNM, MPH, Leslie Fox-Leyva, MPH, FNP (CAPT USPHS-Ret.), Michelle Hall, FNP (CAPT USPHS-Ret.); Victorie Heart, MS, RN; Camille Kuhnley, ANP/CNM, M Ed; Anne Lanier, MD Nina Perino, PA-C; University of Alaska Fairbanks, College of Rural and Community Development; and the State of Alaska Community Health Aide Training and Supervision Grants. We are grateful to the following organizations for sharing their data: Aleutian Pribilof Islands Association, Inc.; Bristol Bay Area Health Corporation; Council of Athabascan Tribal Governments; Chugachmiut; Copper River Native Association; Eastern Aleutian Tribes; Kodiak Area Native Association; Karluk Tribal Council; the Maniilaq Association; the North Slope Borough Department of Health & Social Services; Norton Sound Health Corporation; Southcentral Foundation; SouthEast Alaska Regional Health Consortium; Tanana Chiefs Conference; and the Yukon Kuskokwim Health Corporation.
Conflict of interest and funding
None of the authors have any conflicts of interest to report. Funding was received from the following organizations: Alaska Native Tribal Health Consortium (ANTHC), Division of Community Health Services: CHAP Training Center; CHAP Statewide Services; Alaska Native Epidemiology Center; ANTHC Department of Data Management and Analytics; The Association of Community Health Aide Program Directors (AACHAPD).
References
- 1.Declaration of Alma-Ata. International Conference on Primary Health Care, Alma-Ata, USSR; 1978. World Health Organization [cited 2010 Apr 19]. Available from: http://www.int/publications/almaata_declaration_en.pdf.
- 2.Young TK, Bjerregard P, editors. Toronto: University of Toronto Press; 2008. Health transition in Arctic populations; pp. 39–52. [Google Scholar]
- 3.Young TK, Chatwood S. Health care in the north: what Canada can learn from its circumpolar neighbors. CMAJ. 2011;183:209–14. doi: 10.1503/cmaj.100948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vuorenkoski L, Mladovsky P, Mossialos E. Finland: health system review. Health Systems in Transition. 2008;10:1–168. [cited 2011 Nov 12]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0007/80692/E91937.pdf. [PubMed] [Google Scholar]
- 5.Glenng[adot]rd AH, Hjalte F, Svensson M, Anella A, Bankauskaite V. Health Systems in Transition: Sweden. Copenhagen: WHO Regional Office for Europe on behalf of the European observatory on Health Systems and Policies;2005 [cited 2011 Nov 10] Available from: http://www.euro.who.int/__data/assets/pdf_file/0010/96409/E88669.pdf.
- 6.Johnsen JR. Health Systems in Transition: Norway. Copenhagen: WHP Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies; 2006 [cited 2011 Nov11] Available from: http://www.euro.who.int/__data/assets/pdf_file/0010/96409/E88669.pdf.
- 7.Niclasen B, Mulvad G. Health care and health care delivery in Greenland. Int J Circumpolar Health. 2010;69:437–47. doi: 10.3402/ijch.v69i5.17691. [DOI] [PubMed] [Google Scholar]
- 8.Aaen-Larsen B. Health care in the circumpolar world: Greenland. Int J Circumpolar Health. 2004;63(Suppl l2):S49–S53. doi: 10.3402/ijch.v63i0.17785. [DOI] [PubMed] [Google Scholar]
- 9.Tragakes E, Lessof S. Health care systems in transition: Russian Federation. In: Tragakes E, editor. Vol. 5. Copenhagen: European Observatory on Health Systems and Policies; 2003. [cited 2011 Nov 15]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0005/95936/e81966.pdf. [Google Scholar]
- 10.US Census Bureau. State and county quick facts. Last revised June 3, 2011 [cited 2011 Aug 21] Available from: http://quickfacts.census.gov/qfd/states/02000.html.
- 11.Gage S, Community Health Aide Program Overview . Anchorage, AK: Association of Alaska Community Health Aide Directors; 2007. 2007 [cited 2010 Jun 23]. Available from: http://www.akchap.org. [Google Scholar]
- 12.Alaska Area Native Health Service. The Alaska Area Health Aide Program. Circular No. 94-138; Anchorage, AK: Alaska Area Native Health Service, Indian Health Service, US Department of Health and Human Services; 1994. [Google Scholar]
- 13.Alaska Community Health Aide Program. General information and history [cited 2010 Jun 23] Available from: http://www.akchap.org/html/about-chap.html.
- 14.Alaska Native Health Board, Alaska Native Tribal Health Consortium. 4th ed. Vol. 4. Seattle, WA: US Government Printing Office; 2006. Alaska Community Health Aide/Practitioner Manual. [Google Scholar]
- 15.Community Health Aide Program Certification Board. Community health aide program certification board standards and procedures. Amended June 19, 2008; Anchorage, AK: Alaska Native Tribal Health Consortium Community Health Aide Program Certification Board; 2008. pp. 1–16. [Google Scholar]
- 16.Cueva M, Lanier A, Dignan M, Kuhnley R, Jenkins C. Cancer education for community health aides/practitioners (CHA/Ps) in Alaska assessing comfort with cancer. J Cancer Educ. 2005;20:85–8. doi: 10.1207/s15430154jce2002_8. [DOI] [PubMed] [Google Scholar]
- 17.Indian Health Service. Rockville, MD: Indian Health Service, US Department of Health and Human Services; 2006. National patient information reporting system [database] [cited 2011 Dec 16]. Available from: http://www.ihs.gov/NDW/ [Google Scholar]
- 18.Community Health Aide Program Certification Board. Summary of community health aides/practitioners certified June 2011; Internal working document of the Community Health Aide Program Certification Board, Authorized by Alaska Area Native Health Service, Administered by Alaska Native Tribal Health Consortium, Anchorage, AK. Report made available by Victorie Heart, Community Health Aide Program Certification Board liaison. [Google Scholar]
- 19.Boedeker B, Foster S. Official IHS Active User Population Report (B). Version 43. Alaska 2010 Native. Report date 12/02/2010 [cited 2011 Nov 21] Available from: http://www.ihs.gov/facilitiesservices/NUserPop.pdf.
- 20.Census 2000 Demographic Profile Highlights. Selected Population Group: Alaska Native alone or in any combination. US Census Bureau [cited 2011 Aug 22] Available from: http://factfinder.census.gov/
- 21.Cherry DK, Woodwell DA, Rechsteiner EA. National Ambulatory Medical Care Survey 2005 Summary. CDC Advance data from vital and health statistics, No. 387, 2007; [cited 2011 Aug 31] Available from: http://www.cdc.gov/nchs/data/ad/ad387.pdf. [PubMed]
- 22.Haines A, Sanders D, Lehmann U, Rowe AK, Lawn JE, Jan S, et al. Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369:2121–31. doi: 10.1016/S0140-6736(07)60325-0. [cited 2010 Apr 19]. Available from: http://www.thelancet.com. [DOI] [PubMed] [Google Scholar]
- 23.Gilroy K, Winch P. Management of Sick Children by Community Health Workers; Intervention Models and Programme Examples. The United Nations Children's Fund (UNICEF)/World Health Organization (WHO); 2006 [cited: 2011 May15] Available from: http://www.unicef.org/publications/files/Management_of_Sick_Children_by_Community_Health_Workers.pdf.
- 24.Mukherjee JS, Eustache FE. Community health workers as a cornerstone for integrating HIV and primary healthcare. AIDS Care. 2007;19(Suppl 1):S73–S82. doi: 10.1080/09540120601114485. [DOI] [PubMed] [Google Scholar]
- 25.Barzgar MA, Sheikh MR, Bile MK. Female health workers boost primary care. World Health Forum. 1997;18:202–10. [PubMed] [Google Scholar]
- 26.Javanparast S, Baum F, Labonte R, Sanders D. Community health workers’ perspectives on their contribution to rural health and well-being in Iran. Am J Public Health. 2011;101:2287–92. doi: 10.2105/AJPH.2011.300355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Viswanathan M, Kraschnewski J, Nishikawa B, Morgan L, Thieda P, Honeycutt A, et al. Rockville, MD: Agency for Healthcare Research and Quality; 2009. Outcomes of community health worker interventions. Evidence Report/Technology Assessment No. 181, AHRQ Publication No. 09-E014 [cited 2011 May 30]. Available from: http://www.ahrq.gov/downloads/pub/evidence/pdf/comhealthwork/comhwork.pdf. [PMC free article] [PubMed] [Google Scholar]
- 28.US Department of Health and Human Services. Health Resources and Service Administration, Bureau of Health Professions. Community Health Worker National Workforce Study; March 2007 [cited 2011 Aug 31] Available from http://bhpr.hrsa.gov/healthworkforce/reports/chwstudy2007.pdf.
- 29.Brownstein JN, Hirsch GR, Rosenthal EL, Rush CH. Community health workers “101” for primary care providers and other stakeholders in health care systems. J Ambul Care Manage. 2011;34:210–20. doi: 10.1097/JAC.0b013e31821c645d. [DOI] [PubMed] [Google Scholar]
- 30.Spencer MS, Rosland AM, Kieffer EC, Sinco BR, Valerio M, Palmisano G, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health. 2011;101:2253–60. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alaska Native Tribal Health Consortium Division of Data Management & Analytics, Health Information Technology. Anchorage, AK: ANTHC; 2006. Health Statistics for 2005. Report, presented to Community Health Aide Program. [Google Scholar]
- 32.Lehmann U, Sanders D. Geneva: World Health Organization; 2007. Community health workers: What do we know about them? The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers. [cited 2010 Jun 15]. Available from: http://www.who.int/entity/hrh/documents/community_health_workers.pdf. [Google Scholar]
- 33.Balcazar H, Rosenthal L, Brownstein JN, Rush CH, Matos S, Hernandez L. Community health workers can be a public health force for changes in the United States: three actions for a new paradigm. Am J Public Health. 2011;101:2199–203. doi: 10.2105/AJPH.2011.300386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alaska Native Epidemiology Center. Anchorage, AK: Alaska Native Tribal Health Consortium Alaska Native Epidemiology Center; 2009. Alaska Native Health Status Report; p. 21. [Google Scholar]
- 35.State of Alaska Epidemiology. Alaska Health Facts. Anchorage, AK: Section of Epidemiology, State of Alaska Department of Health and Human Services; 1991. Bulletin No. 13; 1991 [cited 2010 Oct 15] Available from: http://www.epi.alaska.gov/bulletins/docs/b1991_13.html.