Abstract
Objectives
The objective was to assess trends in Inuit, First Nations and non-Aboriginal birth outcomes in the rural and northern regions of Quebec.
Study design and methods
In a birth cohort-based study of all births to residents of rural and northern Quebec from 1991 through 2000 (n = 177,193), we analyzed birth outcomes and infant mortality for births classified by maternal mother tongue (Inuit, First Nations or non-Aboriginal) and by community type (predominantly First Nations, Inuit or non-Aboriginal).
Results
From 1991–1995 to 1996–2000, there was a trend of increasing rates of preterm birth for all 6 study groups. In all rural and northern areas, low birth weight rates increased significantly only for the Inuit mother tongue group [RR1.45 (95% CI 1.05–2.01)]. Stillbirth rates showed a non-significant increase for the Inuit mother tongue group [RR1.76 (0.64–4.83)]. Neonatal mortality rates decreased significantly in the predominantly non-Aboriginal communities and in the non-Aboriginal mother tongue group [RR0.78 (0.66–0.92)], and increased non-significantly for the First Nations mother tongue group [RR2.17 (0.71–6.62)]. Perinatal death rates increased for the First Nations mother tongue grouping in northern areas [RR2.19 (0.99–4.85)].
Conclusion
There was a disconcerting rise of some mortality outcomes for births to First Nations and Inuit mother tongue women and to women in predominantly First Nations and Inuit communities, in contrast to some improvements for births to non-Aboriginal mother tongue women and to women in predominantly non-Aboriginal communities in rural or northern Quebec, indicating a need for improving perinatal and neonatal health for Aboriginal populations in rural and northern regions.
Keywords: Aboriginal health, trends, preterm birth, perinatal mortality, infant mortality
Despite significant improvements over recent decades, Indigenous peoples worldwide experience worse birth outcomes than non-Indigenous populations (1–11). The Canadian Constitution Act recognises 3 groups of Aboriginal peoples: First Nations (North American Indians), Inuit and Métis (12). The health status of Aboriginal women and their babies has consistently been shown to be poorer than their non-Aboriginal counterparts in Canada (4,9,13–17). Such health inequalities remain a major public health concern. First Nations infants are at 1.5–2 times (4,13,18–22), and Inuit infants at 2–5 times higher risk (9,21) of infant mortality than are non-Aboriginal infants.
Although urban areas in the southern parts of Canada are increasingly home to a large number of Aboriginal people, the majority still live in rural and northern areas, in contrast to the non-Aboriginal population which is overwhelmingly urban and southern. Aboriginal peoples often account for a high proportion of the population residing in rural and northern areas. In Quebec, according to the 2006 census, approximately 70% of First Nations people and over 90% of Inuit lived in rural and northern areas.
Due to a lack of ethnicity identifiers on birth registrations, little is known about the trends in birth outcomes and infant mortality for Aboriginal and non-Aboriginal populations living in rural and northern areas. Our objective was to assess trends in Inuit, First Nations and non-Aboriginal birth outcomes in the rural and northern regions of Quebec, using 2 different proxy measures to classify births by ethnicity: maternal mother tongue, and predominant self-identification of the residents of each community.
Material and methods
This was a population-based retrospective cohort study of all births to residents of rural and northern Quebec (n=177,193), based on Statistics Canada's linked stillbirth, live birth and infant death data for 1991–2000. We used birth data up to the year 2000 because it was the most recent year for which data were available at the initiation of the study. Also, in more recent years, mothers with both an Aboriginal and a French or English mother tongue would have been coded as French or English plus “other” mother tongue and thus could not have been identified as Aboriginal in the birth data. The validity of the Canadian linked vital data has been well documented (23). The study was approved by the Research Ethics Board of Sainte-Justine Hospital, the University of Montreal, the First Nations of Quebec and Labrador Health and Social Services Commission, and the Nunavik Nutrition and Health Committee.
According to Statistics Canada's recommended definition, rural refers to all areas outside the limits of any census metropolitan area or census agglomeration – which has a population of 10,000 people or more (24). By this definition, all of northern Quebec is rural. For clarity, we will refer to our study rural areas as “rural and northern Quebec”, to emphasise that Northern Quebec is a part of rural and northern Quebec. However, since northern Quebec is characterized by unique geographical characteristics, we conducted further subgroup analyses for births to residents of northern Quebec.
At the individual level, births were grouped into 3 maternal mother tongue groups: First Nations, Inuit and non-Aboriginal, according to the maternal mother tongue recorded on each birth registration (9). If maternal mother tongue was missing but paternal mother tongue was available, maternal mother tongue was imputed from paternal mother tongue (such cases were rare, <5%). At the community level, all births in communities classified as predominantly First Nations, Inuit or non-Aboriginal were identified and grouped as explained below, after geocoding using software developed by Statistics Canada (25). The geocoding was primarily based on maternal residential postal codes as recorded on birth registrations. When postal codes were missing, municipality codes were used instead (such cases were <5%). A community was identified as a predominantly First Nations community if it was served by a postal code linked primarily to an Indian Reserve (according to First Nations sources consulted by the researchers), and identified as a predominantly Inuit community if the postal code or census subdivision code referred to any of the recognised Quebec Inuit communities. A total of 7,192 births (4.6%) had insufficient information on maternal place of residence to determine whether the mother resided in a predominantly First Nations, Inuit or non-Aboriginal community; such cases were dropped from the community-level analyses.
Birth outcomes under study included preterm birth (<37 completed weeks in gestational age), small-for-gestational-age [SGA, <10th percentile in birth weight for gestational age using the Canadian standards (26)], low birth weight (LBW, <2,500 g), stillbirth (foetal deaths at ≥20 weeks and≥500 g), neonatal death (at 0–27 days of life), perinatal death (stillbirth + neonatal death), post-neonatal death (at 28–364 days of life), and infant death (at 0–364 days of life).
Crude rates and relative risks (RRs) with 95% confidence intervals (CI) were calculated to compare birth outcomes in 1996–2000 to those of 1991–1995 across the 6 groups defined by maternal mother tongue and predominant population of the community. Available maternal and pregnancy characteristics, including maternal age (<20, 20–29, 30–34, ≥35 y), parity (primiparous, multiparous), education (<11 y, 11 y (completed high school in Quebec), ≥12 y [some college or university]), marital status (legally married, in a common-law union, or single [neither married nor in a common-law union]), infant sex (male, female) and plurality (singleton, multiple) were similar within the same study groups over time and thus did not affect the effect size (RRs) estimates, and therefore only crude RRs are presented. Perinatal mortality and stillbirth rates were calculated per 1,000 total births (live births plus stillbirths). For infant and neonatal mortality, rates were calculated per 1,000 live births. Post-neonatal mortality rates were calculated per 1,000 neonatal survivors. All data analyses were carried out using SAS, Version 9.1.
Results
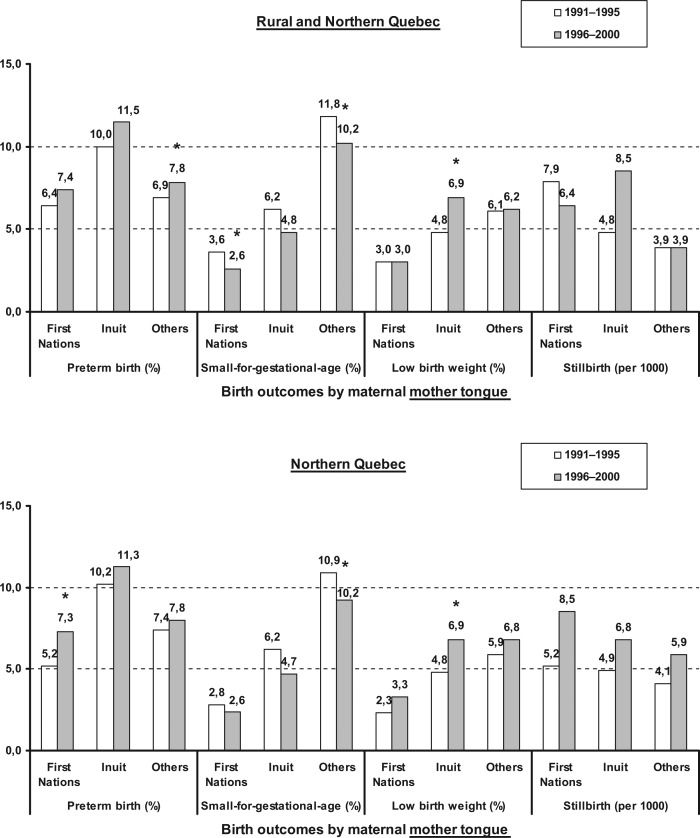
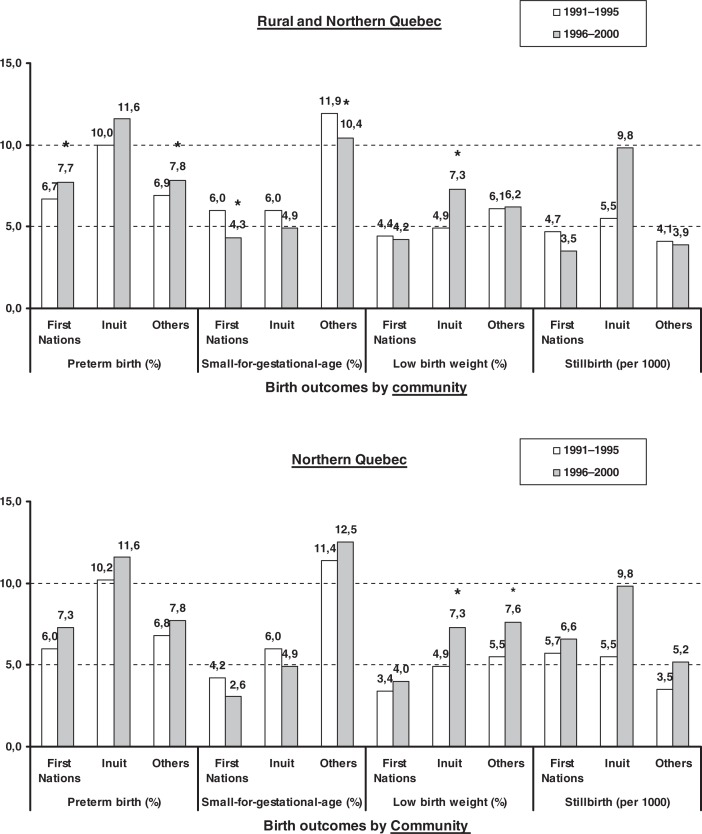
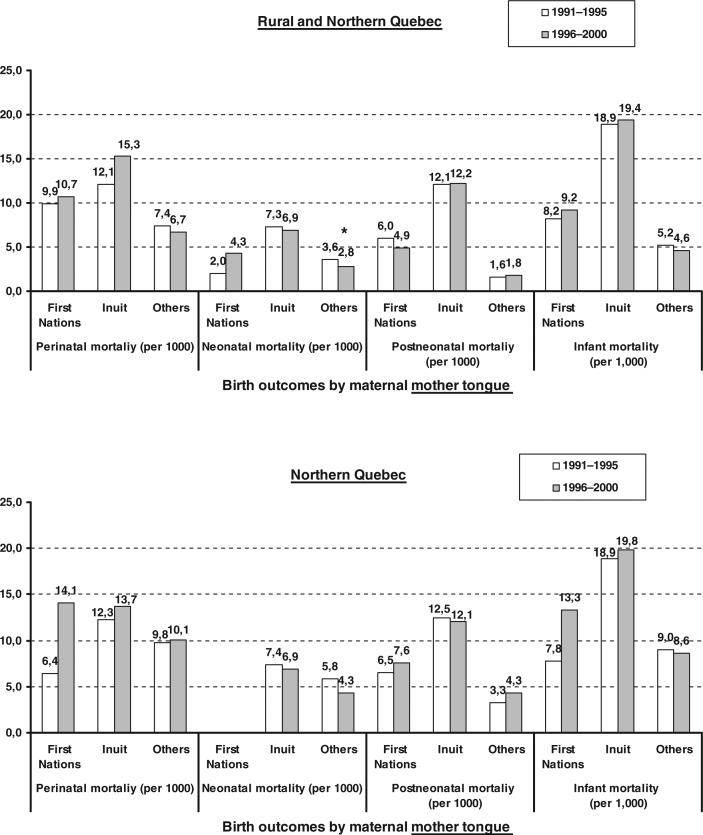
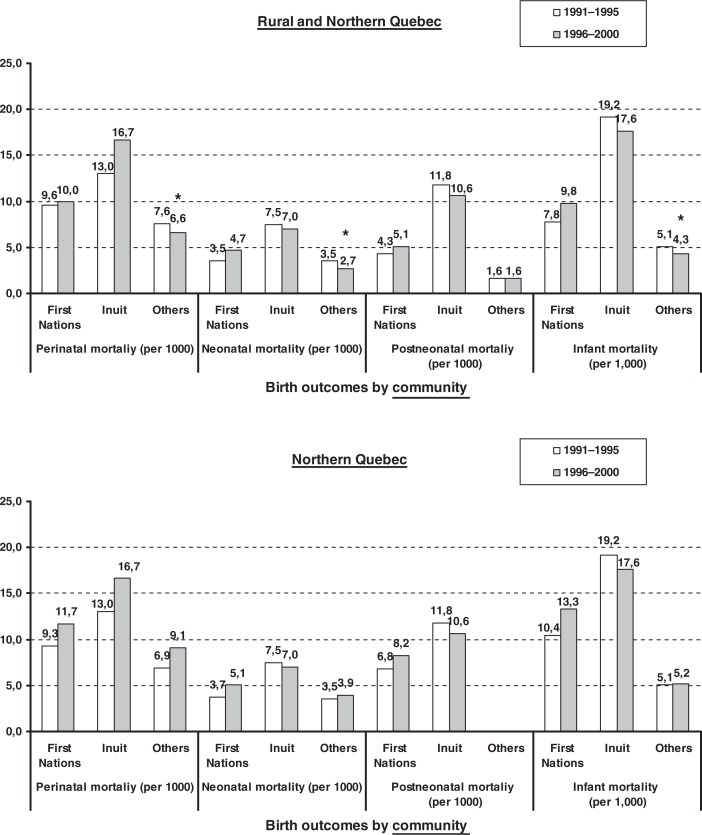
In rural and northern Quebec, at both the individual and community levels, there was a trend of increasing preterm birth rates and decreasing SGA rates for all study groups from 1991–1995 to 1996–2000 (Figs. 1 and 2). LBW rates increased over the 2 time periods for births to Inuit mother tongue women [RR1.45 (95% CI 1.05–2.01)], and to women in Inuit communities [RR1.51 (1.13–2.03)] (Table I and II). Infant mortality rates decreased significantly (by about 15%) for births in the predominantly non-Aboriginal communities of rural and northern Quebec, but not so for births in the predominantly First Nations or Inuit communities. Stillbirth and perinatal death rates increased non-significantly for Inuit mother tongue births [RR1.76 (0.64–4.83) and RR1.27 (0.64–2.50), respectively] and for all births to mothers in the predominantly Inuit communities [RR1.79 (0.75–4.25) and RR1.29 (0.71–2.35), respectively]. Neonatal mortality rates declined significantly for the non-Aboriginal groupings at the individual level [RR0.78 (0.66–0.92)] and the community level [RR0.78 (0.65–0.93)], but rose non-significantly over time for births to First Nations mother tongue women [RR2.17 (0.71–6.62)] as well as for all residents of predominantly First Nations communities [RR1.35 (0.72–2.53)] in rural and northern areas.
Fig. 1a.
Rates of birth outcomes (preterm, small-for-gestational-age, low birth weight, stillbirth) by maternal mother tongue in rural and northern Quebec, or northern Quebec only. *p<0.05 compared the rates over the 2 time periods (1996–2000 vs. 1991–1995).
Fig. 2a.
Rates of birth outcomes (preterm, small-for-gestational-age, low birth weight, stillbirth) by community type [predominantly First Nations, Inuit, or others (non-Aboriginal) communities] in rural and northern Quebec, or northern Quebec only. *p<0.05 compared the rates over the 2 time periods (1996–2000 vs. 1991–1995).
Table I.
Relative risks (RRs) of adverse birth outcomes, perinatal and infant mortality comparing 1996–2000 vs. 1991–1995 among First Nations, Inuit and non-Aboriginal maternal mother tongue groups, in rural and northern Quebec, or northern Quebec only
| RR (95% CI), 1996–2000 vs. 1991–1995 | |||
|---|---|---|---|
| Outcome | First Nations mother tongue | Inuit mother tongue | Non-Aboriginal mother tongue |
| Rural and northern Quebec, n (births)a | 4,079/2,926 | 2,460/2,348 | 96,143/79,248 |
| Preterm | 1.16 (0.93, 0.45) | 1.15 (0.91, 1.45) | 1.14 (1.10, 1.17) |
| SGAb | 0.71 (0.50, 0.99) | 0.77 (0.55, 1.07) | 0.87 (0.84, 0.89) |
| LBWc | 1.00 (0.71, 1.40) | 1.45 (1.05, 2.01) | 1.02 (0.98, 1.06) |
| Stillbirth | 0.81 (0.40, 1.66) | 1.76 (0.64, 4.83) | 1.01 (0.86, 1.17) |
| Perinatal death | 1.09 (0.60, 1.95) | 1.27 (0.64, 2.50) | 0.90 (0.80, 1.01) |
| Neonatal death | 2.17 (0.71, 6.62) | 0.94 (0.36, 2.43) | 0.78 (0.66, 0.92) |
| Post-neonatal death | 0.82 (0.36, 1.86) | 0.99 (0.48, 2.04) | 1.10 (0.87, 1.39) |
| Infant death | 1.15 (0.61, 2.19) | 0.97 (0.55, 1.72) | 0.88 (0.77, 1.01) |
| Northern Quebec only, n (births)a | 1,552/1,064 | 1,217/1,171 | 2,443/2,564 |
| Preterm | 1.42 (1.05, 1.92) | 1.12 (0.89, 1.42) | 1.08 (0.89, 1.31) |
| SGAb | 0.88 (0.55, 1.43) | 0.75 (0.54, 1.05) | 0.84 (0.72, 0.99) |
| LBWc | 1.42 (0.90, 2.24) | 1.42 (1.02, 1.97) | 1.15 (0.93, 1.43) |
| Stillbirth | 1.64 (0.64, 4.24) | 1.39 (0.48, 3.98) | 1.43 (0.64, 3.18) |
| Perinatal | 2.19 (0.99, 4.85) | 1.11 (0.55, 2.23) | 1.03 (0.59, 1.79) |
| Neonatal death | – | 0.93 (0.36, 2.39) | 0.75 (0.34, 1.65) |
| Post-neonatal death | 1.18 (0.47, 2.97) | 0.97 (0.47, 2.00) | 1.31 (0.53, 3.25) |
| Infant death | 1.71 (0.79, 3.68) | 0.95 (0.54, 1.69) | 0.95 (0.53, 1.72) |
RRs, p<0.05.
n for total births in 1996–2000/1991–1995.
SGA=small-for-gestational-age (<10th percentile).
LBW=low birth weight (<2,500 g).
not estimable, due to small numbers of events.
Table II.
Relative risks (RRs) of birth outcomes, perinatal and infant mortality comparing 1996–2000 vs. 1991–1995 among predominantly First Nations, Inuit and non-Aboriginal communities, in rural and northern Quebec, or northern Quebec only
| RR (95% CI), 1996–2000 vs. 1991–1995 | |||
|---|---|---|---|
| Outcome | First Nations communities | Inuit communities | Non-Aboriginal communities |
| Rural and northern Quebec, n (births)a | 6,841/6,690 | 1,465/1,433 | 95,706/76,860 |
| Preterm | 1.15 (1.00, 1.33) | 1.16 (0.94, 1.43) | 1.13 (1.09, 1.17) |
| SGAb | 0.72 (0.61, 0.86) | 0.81 (0.60, 1.10) | 0.88 (0.85, 0.90) |
| LBWc | 0.96 (0.79, 1.16) | 1.51 (1.13, 2.03) | 1.02 (0.99, 1.06) |
| Stillbirth | 0.87 (0.51, 1.47) | 1.79 (0.75, 4.25) | 0.96 (0.82, 1.11) |
| Perinatal | 1.04 (0.70, 1.56) | 1.29 (0.71, 2.35) | 0.87 (0.78, 0.98) |
| Neonatal death | 1.35 (0.72, 2.53) | 0.93 (0.40, 2.19) | 0.78 (0.65, 0.93) |
| Post-neonatal death | 1.19 (0.66, 2.13) | 0.91 (0.45, 1.81) | 1.02 (0.80, 1.29) |
| Infant death | 1.26 (0.82, 1.93) | 0.92 (0.54, 1.56) | 0.85 (0.74, 0.98) |
| Northern Quebec only, n (births)a | 1,928/1,967 | 1,465/1,433 | 2,023/1,542 |
| Preterm | 1.23 (0.97, 1.56) | 1.16 (0.94, 1.43) | 1.14 (0.90, 1.44) |
| SGAb | 0.74 (0.53, 1.02) | 0.81 (0.60, 1.10) | 1.10 (0.92, 1.31) |
| LBWc | 1.16 (0.84, 1.60) | 1.51 (1.13, 2.03) | 1.38 (1.08, 1.78) |
| Stillbirth | 1.16 (0.52, 2.58) | 1.79 (0.75, 4.25) | 1.50 (0.54, 4.13) |
| Perinatal | 1.25 (0.68, 2.31) | 1.29 (0.71, 2.35) | 1.31 (0.63, 2.74) |
| Neonatal death | 1.40 (0.53, 3.67) | 0.93 (0.40, 2.19) | 1.13 (0.38, 3.35) |
| Post-neonatal death | 1.21 (0.58, 2.51) | 0.91 (0.45, 1.81) | – |
| Infant death | 1.28 (0.71, 2.28) | 0.92 (0.54, 1.56) | 1.05 (0.42, 2.66) |
RRs, p<0.05.
n for total births in 1996–2000/1991–1995.
SGA=small-for-gestational-age (<10th percentile).
LBW=low birth weight (<2,500 g).
not estimable, due to small numbers of events.
In northern Quebec, LBW rates increased significantly over time for births to Inuit mother tongue women [RR1.42 (1.02–1.97)], and to mothers living in predominantly Inuit [RR1.51 (1.13–2.03)] and non-Aboriginal [RR1.38 (1.08–1.78)] communities, and increased non-significantly for births to First Nations mother tongue women [RR1.42 (0.90–2.24)] (Figs. 1 and 2 , Tables I and II). For births to First Nations mother tongue women in northern Quebec, preterm birth [RR1.42 (1.05–1.92)], perinatal death [RR2.19 (0.99–4.85)], infant death [RR1.71 (0.79–3.68)] and stillbirth rates [RR1.64 (0.64–4.24)] increased, the latter 2 statistically non-significantly.
Fig. 1b.
Rates of perinatal, neonatal, post-neonatal and infant mortality by maternal mother tongue in rural and northern Quebec, or northern Quebec only. *p<0.05 compared the rates over the 2 time periods (1996–2000 vs. 1991–1995).
Fig. 2b.
Rates of perinatal, neonatal, post-neonatal and infant mortality by community type [predominantly First Nations, Inuit, or others (non-Aboriginal) communities] in rural and northern Quebec, or northern Quebec only. *p<0.05 compared the rates over the 2 time periods (1996–2000 vs. 1991–1995).
Discussion
Using 2 proxy indicators of Aboriginal ethnicity, this study reveals a worse pattern in some mortality-based birth outcomes over time (from 1991–1995 to 1996–2000) for births to First Nations and Inuit mother tongue women and for predominantly First Nations and Inuit communities relative to the rates for births to non-Aboriginal mother tongue women and for births to all women in predominantly non-Aboriginal communities, respectively, in the rural and northern areas of Quebec. This is in contrast to some improvement for births to non-Aboriginal mother tongue women and for women in predominantly non-Aboriginal communities in the same settings. Our results indicate a need to improve socio-economic conditions, perinatal and neonatal care for Aboriginal people in rural and northern regions. The improvements in some birth outcomes for the non-Aboriginal group over the 2 time periods are more consistent in rural and northern areas as a whole, but not so in northern areas only, suggesting that non-Aboriginal women were also affected by poor access to high quality perinatal and neonatal care in northern regions.
The present study showed a general rise in rates of preterm birth for all groups, which is consistent with previous reports of slightly increasing preterm birth rates over recent decades (9,27). Rates of preterm birth are known to be higher in Inuit and some First Nations populations in Canada, but not for Quebec First Nations (4,9,27,28). We found increasing rates of preterm birth for all groups over the study period, but the rates increased more substantially for First Nations mother tongue women (by about 40%, from 5.2 to 7.3%) in northern Quebec. In contrast, a previous study assessing the risks of adverse pregnancy outcomes among Inuit and First Nations vs. other mother tongue women in Quebec between 1985–1987 and 1995–1997 reported a decrease in rates of preterm birth for Inuit mother tongue women (from 14.4% in 1985–1987 to 10.7% in 1995–1997) (9), while almost no change was observed for First Nations mother tongue women. The reasons for the large increase in rates of preterm birth for First Nations mother tongue women and for predominantly First Nations communities in northern areas are unclear. Further research is needed to understand the causes of this unexpected rise.
In Canada, the rate of LBW remained relatively stable between 1979 and 2005, ranging from 5.5 to 6.0% (29). Our study revealed increased rates of LBW over the study period for births to Inuit mother tongue women as well as for all births in predominantly Inuit or non-Aboriginal communities of northern Quebec. This is consistent with previous findings for the Inuit-inhabited areas of northern Canada (28). The reasons for this increase are not entirely understood, but may partly be explained by more preterm births and more mildly poorer foetal growth for births close to term (37 weeks). Higher prevalence of smoking, alcohol and drug use, stress, poverty, poor nutrition during pregnancy, and lack of social support may also contribute to the explanation (30–32). Inuit women might have been differentially more exposed to one or several of these factors compared to non-Aboriginal women, leading to increased rates of LBW, although the extent to which these exposures might have differed among the 3 groups is not known. Increased rates of LBW for Inuit and First Nations mother tongue women have previously been reported in Quebec (27). Here, we confirmed this pattern in rural and northern areas. Consistent with a trend of decreasing rates of SGA in Canada (33,34), we also observed a decrease in rates of SGA among all births in both predominantly Aboriginal and in predominantly non-Aboriginal communities of northern Quebec.
Since 1991, stillbirth rates have been around 6.0 per 1000 total births in Canada, but varied greatly across the country, ranging from 4.0 per 1000 in Quebec to 11.3 per 1000 in Nunavut (an area with a very high proportion of Inuit residents) in 2005 (29). There is a lack of data on trends in stillbirth or perinatal mortality rates among Aboriginal populations in other countries. We observed a significant increase in perinatal death rates for births to First Nations mother tongue women, and a non-significant increase in the rates of stillbirth for births to Inuit mother tongue women in northern Quebec. Not unexpectedly, the pattern for Inuit in rural settings is consistent with the reported pattern for all Inuit mother tongue births in Quebec (27) because about 95% of Inuit births are to residents of rural areas. Increased stillbirth rates among First Nations mother tongue women in Quebec (6.8 per 1000 in 1985–87 vs. 9.3 per 1000 in 1995–97) have been reported previously (9). Here, we found that the high risk of perinatal death is of particular concern to First Nations mother tongue women in northern areas. Prenatal smoking and alcohol drinking have been associated with increased rates of stillbirth (35), both more prevalent for Aboriginal and especially Inuit women compared to the general population. There is a need for more perinatal health promotion programs targeted at reducing maternal smoking, alcohol use and exposures to second-hand smoke during pregnancy.
In our rural and northern study area, infant mortality rates decreased for all births to residents of predominantly non-Aboriginal communities (a decrease of 16%, from 5.1 to 4.3 per 1000), but not so for births to residents of predominantly First Nations or Inuit communities. A similarly worse pattern for Aboriginal communities was observed in Western Australia. Infant mortality rates declined in Aboriginal and non-Aboriginal populations between 1980 and 2001, but less substantially for Aboriginal (by 36% from 25.0 to 16.1) than for non-Aboriginal infants (by almost 56% from 8.4 to 3.7) (6). In contrast, infant mortality rates declined to a greater extent for First Nations (by 64% from 20.7 to 7.5 per 1000) than for non-First Nations infants (by 47% from 7.5 to 4.0 per 1000) in rural areas of British Columbia from 1981–1984 to 1997–2000 (4). In other words, the patterns observed in Quebec seem worse than those in British Columbia. Similarly, a greater reduction in infant mortality rates have been observed among American Indian and Alaska Native Infants (a decline of 33% from 11.8 to 8.0 per 1000) than among white infants (a decline of 24% from 6.3 to 4.8 per 1000) in the United States between 1989–1991 and 1998–2000 (11). Post-neonatal mortality rates declined more among American Indian and Alaska Native infants (by 39% from 7.0 to 4.0 per 1000) than among white infants (by 33% from 3.0 to 2.0 per 1000) in the United States between 1989–1991 and 1998–2000 (11). Likewise, post-neonatal mortality rates declined more substantially for First Nations (by 66% from 12.4 to 4.2 per 1000) than for non-First Nations infants (by 55% from 3.1 to 1.4 per 1000) for resident of the rural areas of British Columbia from 1981–1984 to 1997–2000 (4). In contrast, for rural and northern Quebec, we observed no significant reductions in post-neonatal mortality rates for both Aboriginal and non-Aboriginal populations during the study period.
Our findings draw attention to the need for reducing the high perinatal and infant mortality rates for births to First Nations people and Inuit living in rural and especially northern areas. Further studies are needed to clarify the pathways associated with the rise of poor birth outcomes in Aboriginal women. More and better programmes for improving socioeconomic conditions, perinatal and neonatal care are needed for Aboriginal populations in rural and northern regions.
This study is subject to some limitations. First, at the individual level, some Inuit and First Nations women (according to their self-identification) may not have reported a native language as their mother tongue, resulting in their classification into the non-Aboriginal mother tongue group. Such “misclassifications” would likely inflate the rates of adverse birth outcomes for the non-Aboriginal mother tongue group, which we know contains substantial numbers of self-identified Aboriginal women in rural and northern areas. According to the 2001 census, about 86% of self-identified Inuit and 60% of self-identified First Nations people in Quebec reported a native language as their mother tongue. Secondly, at the community level, some First Nations communities shared common postal codes with adjacent non-Aboriginal communities, yet all births to residents of those communities were classified as occurring to residents of predominantly First Nations communities – because we could not make a distinction – and all births occurring to residents of predominantly Inuit communities were included, even though 10% of the residents of the predominantly Inuit communities of northern Quebec are known to be non-Inuit. Overall, these limitations would have partly masked the worse outcomes for births to Aboriginal mother tongue women and for births in predominantly Aboriginal communities, though the effect was probably stronger for the First Nations groupings. However, the extent of such misclassification should have been similar in the earlier vs. later 5-year periods, and therefore would be unlikely to have affected the trends within each study sub-group.
Acknowledgments
We would like to acknowledge Aboriginal Advisory Board members for their contributions in the project: Nancy Gross-Louis McHugh from the First Nations of Quebec and Labrador Health and Social Services Commission, and Elena Labranche from the Nunavik Regional Board of Health and Social Services. We are grateful to Statistics Canada and to the Institut de la Statistique du Québec for providing access to the data for the research project. F. Simonet was supported by a scholarship from the CIHR Strategic Training Initiative in Research in Reproductive Health Science (2008–2010) and from the Quebec Training Network in Perinatal Research (2010–2011), and ZC Luo by a Clinical Epidemiology Junior Scholar Award from the Fonds de Recherche en Santé du Québec, and a CIHR Gender and Health New Investigator award.
Conflicts of interest and funding
There were no conflicts of interest from the authors. This study was supported by a research grant from the Canadian Institutes of Health Research – Institute of Aboriginal Peoples’ Health (CIHR-IAPH, Grant No. 73551 to ZC Luo).
References
- 1.Grossman DC, Baldwin LM, Casey S, Nixon B, Hollow W, Hart LG. Disparities in infant health among American Indians and Alaska natives in US metropolitan areas. Pediatrics. 2002;109:627–33. doi: 10.1542/peds.109.4.627. [DOI] [PubMed] [Google Scholar]
- 2.Nakamura RM, King R, Kimball EH, Oye RK, Helgerson SD. Excess infant mortality in an American Indian population, 1940 to 1990. JAMA. 1991;266:2244–8. [PubMed] [Google Scholar]
- 3.Grossman DC, Krieger JW, Sugarman JR, Forquera RA. Health status of urban American Indians and Alaska Natives. A population-based study. JAMA. 1994;271:845–50. [PubMed] [Google Scholar]
- 4.Luo ZC, Kierans WJ, Wilkins R, Liston RM, Uh SH, Kramer MS. Infant mortality among First Nations vs. non-First Nations in British Columbia: temporal trends in rural vs. urban areas, 1981–2000. Int J Epidemiol. 2004;33:1252–9. doi: 10.1093/ije/dyh290. [DOI] [PubMed] [Google Scholar]
- 5.Bjerregaard P, Misfeldt J. Infant mortality in Greenland: secular trend and regional variation. Arctic Med Res. 1992;51:126–35. [PubMed] [Google Scholar]
- 6.Freemantle CJ, Read AW, de Klerk NH, McAullay D, Anderson IP, Stanley FJ. Patterns, trends, and increasing disparities in mortality for Aboriginal and non-Aboriginal infants born in Western Australia, 1980–2001: population database study. Lancet. 2006;367:1758–66. doi: 10.1016/S0140-6736(06)68771-0. [DOI] [PubMed] [Google Scholar]
- 7.Baldwin LM, Grossman DC, Casey S, Hollow W, Sugarman JR, Freeman WL, et al. Perinatal and infant health among rural and urban American Indians/Alaska Natives. Am J Public Health. 2002;92:1491–7. doi: 10.2105/ajph.92.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alessandri LM, Chambers HM, Blair EM, Read AW. Perinatal and post-neonatal mortality among Indigenous and non-Indigenous infants born in Western Australia, 1980–1998. Med J Aust. 2001;175:185–9. doi: 10.5694/j.1326-5377.2001.tb143092.x. [DOI] [PubMed] [Google Scholar]
- 9.Luo ZC, Wilkins R, Platt RW, Kramer MS. Risks of adverse pregnancy outcomes among Inuit and North American Indian women in Quebec, 1985–97. Paediatr Perinat Epidemiol. 2004;18:40–50. doi: 10.1111/j.1365-3016.2003.00529.x. [DOI] [PubMed] [Google Scholar]
- 10.Freemantle CJ, Read AW, de Klerk NH, McAullay D, Anderson IP, Stanley FJ. Sudden infant death syndrome and unascertainable deaths: trends and disparities among Aboriginal and non-Aboriginal infants born in Western Australia from 1980 to 2001 inclusive. J Paediatr Child Health. 2006;42:445–51. doi: 10.1111/j.1440-1754.2006.00895.x. [DOI] [PubMed] [Google Scholar]
- 11.Tomashek KM, Qin C, Hsia J, Iyasu S, Barfield WD, Flowers LM. Infant mortality trends and differences between American Indian/Alaska native infants and white infants in the United States, 1989–1991 and 1998–2000. Am J Public Health. 2006;96:2222–7. doi: 10.2105/AJPH.2004.053744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smylie J, Anderson M. Understanding the health of Indigenous peoples in Canada: key methodological and conceptual challenges. CMAJ. 2006;175:602. doi: 10.1503/cmaj.060940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luo ZC, Kierans WJ, Wilkins R, Liston RM, Mohamed J, Kramer MS. Disparities in birth outcomes by neighborhood income: temporal trends in rural and urban areas, British Columbia. Epidemiology. 2004;15:679–86. doi: 10.1097/01.ede.0000142149.34095.88. [DOI] [PubMed] [Google Scholar]
- 14.Munroe M, Shah CP, Badgley R, Bain HW. Birth weight, length, head circumference and bilirubin level in Indian newborns in the Sioux Lookout Zone, northwestern Ontario. CMAJ. 1984;131:453–6. [PMC free article] [PubMed] [Google Scholar]
- 15.Rodrigues S, Robinson EJ, Kramer MS, Gray-Donald K. High rates of infant macrosomia: a comparison of a Canadian native and a non-native population. J Nutr. 2000;130:806–12. doi: 10.1093/jn/130.4.806. [DOI] [PubMed] [Google Scholar]
- 16.Thomson M. Heavy birthweight in Native Indians of British Columbia. Can J Public Health. 1990;81:443–6. [PubMed] [Google Scholar]
- 17.Heaman MI, Blanchard JF, Gupton AL, Moffatt MEK, Currie RF. Risk factors for spontaneous preterm birth among Aboriginal and non-Aboriginal women in Manitoba. Paediatr Perinat Epidemiol. 2005;19:181–93. doi: 10.1111/j.1365-3016.2005.00644.x. [DOI] [PubMed] [Google Scholar]
- 18.British Columbia Vital Statistics Agency, First Nations and Inuit Health Branch of Health Canada. Vancouver: British Columbia Vital Statistics Agency; 2001. Analysis of health statistics for Status Indians in British Columbia, 1991–1999. [Google Scholar]
- 19.First Nations and Inuit Health Branch, Health Canada. 1998 Vital statistics of the Saskatchewan registered Indian population. Ottawa: Health Canada; 2000. [Google Scholar]
- 20.Fisk R, Macdonald J, Vander Kuyl W, Peck S. The declining trend of sudden infant death syndrome – comparison with other major causes of infant mortality and infant deaths due to unknown causes, BC, 1985 to 1996. British Vital Statistics Agency Quarterly Digest. 1998;7 [Google Scholar]
- 21.MacMillan HL, MacMillan AB, Offord DR, Dingle JL. Aboriginal health. CMAJ. 1996;155:1569–78. [PMC free article] [PubMed] [Google Scholar]
- 22.Waldram JB, Herring DA, Young TK. Aboriginal health in Canada: historical, cultural, and epidemiological perspectives. Toronto: University of Toronto Press; 1995. [Google Scholar]
- 23.Fair M, Cyr M, Allen AC, Wen SW, Guyon G, MacDonald RC. An assessment of the validity of a computer system for probabilistic record linkage of birth and infant death records in Canada. The Fetal and Infant Health Study Group. Chronic Dis Can. 2000;21:8–13. [PubMed] [Google Scholar]
- 24.Plessis V, Beshiri R, Bollman RD, Clemenson H. Definitions of rural. Rural and Small Town Canada Analysis Bulletin 2001;3. Ottawa: Statistics Canada; 2001; Catalogue No. 21-006-XIE. [Google Scholar]
- 25.Wilkins R. PCCF+ Version 4J User's Guide; Automated geographic coding based on the Statistics Canada Postal Code Conversion files, including postal codes to September 2006; Ottawa: Health Analysis and Measurement Group, Statistics Canada; 2007. Catalogue No. 82F0086-XDB. [Google Scholar]
- 26.Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:e35. doi: 10.1542/peds.108.2.e35. [DOI] [PubMed] [Google Scholar]
- 27.Simonet F, Wassimi S, Heaman M, Smylie J, Martens P, McHugh NG, et al. Individual- and community-level disparities in birth outcomes and infant mortality among First Nations, Inuit and other populations in Quebec. Open Women's Health J. 2010;4:18–24. doi: 10.2174/1874291201004020018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luo ZC, Senécal S, Simonet F, Guimond E, Penney C, Wilkins R. Birth outcomes in the Inuit-inhabited areas of Canada. CMAJ. 2010;182:235–42. doi: 10.1503/cmaj.082042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Statistics Canada. Live birth, by birth weight (less than 2,500 grams) and sex, Canada, provinces and territories (CANSIM Table 102-4509); Ottawa: Statistics Canada; 2008. [Google Scholar]
- 30.Wenman WM, Joffres MR, Tataryn IV. A prospective cohort study of pregnancy risk factors and birth outcomes in Aboriginal women. CMAJ. 2004;171:585–9. doi: 10.1503/cmaj.1031730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heaman MI, Chalmers K. Prevalence and correlates of smoking during pregnancy: a comparison of aboriginal and non-aboriginal women in Manitoba. Birth. 2005;32:299–305. doi: 10.1111/j.0730-7659.2005.00387.x. [DOI] [PubMed] [Google Scholar]
- 32.Johnson D, Jin Y, Truman C. Influence of aboriginal and socioeconomic status on birth outcome and maternal morbidity. J Obstet Gynaecol Can. 2002;24:633–40. doi: 10.1016/s1701-2163(16)30194-3. [DOI] [PubMed] [Google Scholar]
- 33.Ananth CV, Shi Wu Wen. Trends in fetal growth among singleton gestations in the United States and Canada, 1985 through 1998. Semin Perinatol. 2002;26:260–7. doi: 10.1053/sper.2002.34772. [DOI] [PubMed] [Google Scholar]
- 34.Wen SW, Kramer MS, Platt R, Demissie K, Joseph KS, Liu S, et al. Secular trends of fetal growth in Canada, 1981 to 1997. Paediatr Perinat Epidemiol. 2003;17:347–54. doi: 10.1046/j.1365-3016.2003.00513.x. [DOI] [PubMed] [Google Scholar]
- 35.Cnattingius S, Berendes HW, Forman MR. Do delayed child bearers face increased risks of adverse pregnancy outcomes after the first birth? Obstet Gynecol. 1993;81:512–6. [PubMed] [Google Scholar]