Abstract
Purpose
The hypothesis of this study was that single-legged horizontal hop test ratios would correlate with IKDC, KOOS, and Marx activity level scores in patients 2 years after primary ACL reconstruction.
Methods
Individual patient-reported outcome tools and hop test ratios on 69 ACL reconstructed patients were compared using correlations and multivariable modeling. Correlations between specific questions on the IKDC and KOOS concerning the ability to jump and hop ratios were also performed.
Results
The triple-hop ratio was moderately but significantly correlated with the IKDC, KOOS Sports and Recreation subscale, and the KOOS Knee Related Quality of Life subscale, as well as with the specific questions related to jumping. Similar but weaker relationship patterns were found for the single-hop ratio and timed hop. No significant correlations were found for the Marx activity level or crossover-hop ratio. Multivariable modeling showed almost no significant additional contribution to predictability of the IKDC or KOOS subscores by gender, BMI, or the number of faults on either leg.
Conclusions
The triple-hop test is most significantly correlated with patient-reported outcome scores. Multivariable modeling indicates that less than a quarter of the variability in outcome scores can be explained by hop test results. This indicates that neither test can serve as a direct proxy for the other; however, assessment of patient physical function by either direct report using validated outcome tools or by the hop test will provide relatively comparable data.
Level of evidence
II.
Keywords: ACL, Hop test, KOOS, IKDC, Marx activity, Function
Introduction
Multiple manuscripts have been written addressing the problem of an array of different outcome measures utilized in outcomes-based research in orthopedics, particularly as it relates to the issues of clinician-based “observed” measures and patient-based “reported” measures [4, 6, 11, 15, 25, 27, 30]. “Function” is an outcome important to patient satisfaction after ACL reconstruction [12]. However, there are numerous tools that can be used to measure function, and measurements used to determine return-to-play may be different than those ultimately used to determine surgical outcome [11]. Several studies have investigated various measures of function to determine whether a single test could be sufficient for describing patient function and found that observed measurements and patient-reported measurements of function have poor correlation [1, 4, 14, 15, 21, 24], leading to the recommendation that both types of measurements should be utilized [4].
The overall goal of this study was to examine the specific relationship between observed measurements and patient-reported measurements at a minimum of 2 years after ACL reconstruction. This study compared functional outcomes in primary ACL reconstruction patients using four clinician-administered functional hop tests [16] and three patient-reported outcome tools: the Knee injury and Osteoarthritis Outcomes Survey (KOOS) [22], the current version of the International Knee Documentation Committee (IKDC) subjective form [10], and the Marx activity level score [13]. These patient-reported outcome surveys have been shown to have good reliability, validity (IKDC [10], KOOS [22], Marx [13]), and significance to patients [26]. The single-legged hop test is the only functional test incorporated as part of the IKDC overall outcome measurements and has also been shown to have good reliability and validity [15, 20, 23].
While some studies have been performed on similar topics [1, 4, 14, 15, 21, 24], this is the first to compare all four hop tests with the current versions of the IKDC, KOOS, and Marx activity scale with enough patients for multivariable analysis, which allows for controlling for variable patient contributions, such as gender and BMI and including a “faults” variable as a potential indicator of hop quality. Additionally, the relationship between the specific question on the KOOS and the IKDC related to jumping and the hop scores were evaluated.
The purpose of this study was to determine which of the observed hop scores most closely correlates with patient report of function and to examine how much of the variability in the patient report can be explained by direct observation of hopping. We also tested the hypothesis that the hop scores would be more highly correlated with individual questions related to jumping than with the entire outcomes scores.
Materials and methods
All subjects participated between 24 and 39 months after ACL reconstruction. Subjects were required to be between 12 and 35 years of age, injured while playing a sport (self-reported at the time of surgery), have no previous surgery on the contralateral knee, and at the time of surgery found to have no greater than a grade 2 sprain of the medial collateral ligament (MCL), lateral collateral ligament (LCL), or posterior cruciate ligament (PCL). All subjects were originally enrolled by three surgeons in the Multicenter Orthopaedic Outcomes Network (MOON) study and had undergone a primary ACL reconstruction which had not been revised at the time of testing. Patients could not participate while pregnant or if they had a known rupture of either ACL. Patients who could not be scheduled for testing prior to the end of 39 months were determined to be no longer eligible for study. One hundred eighty-one potential candidates were identified (see Fig. 1). Twenty-five individuals were not offered participation because they were unable to be reached in the appropriate time frame. Study numbers from one site were ordered by random sampling using R software, and the last 16 individuals were removed from the eligible pool prior to study initiation due to throughput concerns. Nine patients were determined to be ineligible at the time of contact or became ineligible due to retear or surgery on the contralateral knee. Thus, 131 individuals were informed of the study and offered participation. Eighty-one of these 131 individuals chose to participate in the study. Twelve individuals were not included in the analysis of the hop test. Of those 12, two individuals did not attempt the hop test due to unrelated health issues; one did not complete study testing due to scheduling constraints. One began the testing protocol, but discontinued testing after reporting instability in the knee. Eight people prior to attempting the hop test reported that they had some problem related to lower limb or trunk, which in the patient’s judgment might prevent one or both legs from performing the test properly. The remaining group of 69 included 28 men, of whom 15 had ACL reconstructions on the left leg and 13 on the right; and 41 women, of whom 16 had ACL reconstructions on the left and 25 on the right.
Fig. 1.
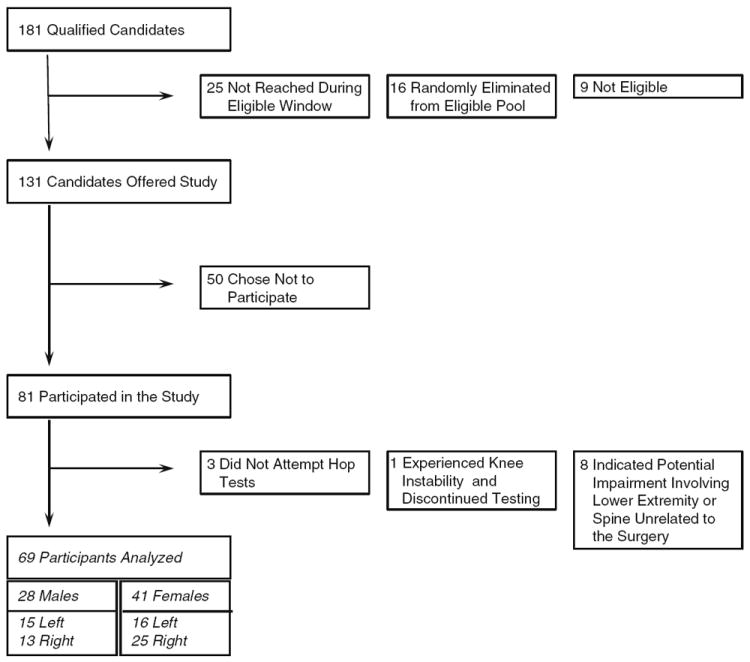
Flow diagram showing qualified candidate enrollment
Patients were introduced to the study by either the operating surgeon or study staff. Patients who indicated interest were mailed Vanderbilt University, The Ohio State University, or Cleveland Clinic Foundation Institutional Review Board (IRB) approved consent documentation. Patients traveled to the testing site where they completed a 13-page questionnaire prior to additional testing ending in a battery of hop tests.
Testing procedures
Subjects completed a 13-page questionnaire on the day of testing, prior to hopping, which included the validated outcome instruments of the KOOS, IKDC, and Marx activity level score. Subjects had completed the same questionnaire at the time of surgery and so had some familiarity with the questions. Scoring was performed according to established methods for each questionnaire [2, 13, 22].
Subjects subsequently completed a battery of four hop tests in the following order: single hop, triple hop, crossover hop for distance, and a six-meter timed hop [16]. All subjects started with their right leg (regardless of their injured side) and had one practice hop followed by the number of trials necessary to document three successful hops measured for distance (or timed) before repeating the process with their left leg. Distance was measured from toe at start to toe at landing. A successful hop required the patient to maintain the one-footed landing so that it could be accurately measured. Two-footed landings, touching the ground or walls with the hands or arms, double hops, or hops that moved too far or not enough in the lateral direction were counted as “faults.” The number of failed hops per side per test was recorded. No instructions about how to hop were given; subjects were simply instructed to hop as far or as fast as they could in a controlled enough way so as to avoid the aforementioned list of “faults.” Testing was done under the supervision of a licensed physical therapist for safety and proper test administration. Subjects paced themselves. The single hop consisted of one forward hop along a line. The triple hop consisted of three consecutive, forward hops along a line, and the cumulative distance was measured. The crossover hop consisted of three consecutive, angled hops during which the subject started on the ipsilateral side of a 6-inch-wide line and hopped as far forward as he/she could while fully crossing the line to the other side, the second hop was the same, but crossed back to the original side, and the third hop mimicked the first. Cumulative distance along the line was measured. For the timed hop test, patients hopped on one leg along a 6-meter line as quickly as possible. Testers began the stopwatch when the tester called “go” and stopped the stopwatch when the tester saw the subject pass the end of the line.
Statistical analysis
All analyses were carried out using R software [19]. (R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0, URL http://www.R-project.org).
Calculation of hop ratio
Initial analysis of hop distances performed on each leg revealed that hop distances increased with the order of the measured hops. Consequently, hops were corrected for learning accrued during the course of each test by applying a linear mixed model. Hop measure was regressed on by gender, order of hop (1–6), and whether the hop was being performed by the involved or uninvolved extremity. This provided an estimate of the order effect, the expected percent increase in hop measure compared with the first hop due to order, when gender and side of injury are controlled. This order effect is assumed to be due to a combination of learning and fatiguing that occurs as the patient repeatedly performs the same test in order to achieve six measured hops (3 right, then 3 left). By dividing each hop measurement by the estimated percent increase due to order, a corrected measure was calculated. The geometric mean for the three adjusted measurements was calculated, and a hop ratio derived for each test by dividing the average corrected hop measurement from the index side by the average corrected hop measurement from the contralateral, normal side. Thus, for hops for distance, a ratio of 1.0 would mean that the surgical limb performed as well as the nonsurgical limb, a ratio less than 1.0 would translate to the surgical limb performing worse than the non-surgical limb, and a ratio greater than 1.0 equates to the surgical side performing better than the normal contralateral limb. Note that for the timed hop, however, lower ratios indicate relatively higher function for the surgical leg.
Correlations
Correlations were assessed using Spearman’s rho (ρ) correlation coefficient. Correlation coefficients between 0.3 and 0.5 are considered to be moderate [5].
Linear regression
Patient-oriented outcome scores were regressed on by the independent variables of gender, body mass index (BMI), and by three test specific factors: the number of faults committed while hopping on the surgical leg, the number of faults committed while hopping on the normal leg, and the hop ratio for that test. Initially, the regressions were performed allowing for a nonlinear contribution of the ratio. The nonlinear contribution had less than 0.05 significance for all models except for one: KOOS Sports and Recreation score regressed on by the single-hop ratio; thus, the nonlinear contribution was dropped from these models and the regression was rerun without them. To check distributional assumptions of the ols models, q–q plots of residuals were used to assess normality.
Results
Participants (Table 1)
Table 1.
Participant summary statistics
| N | Patient summary statistics
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time since ACLR
|
Age
|
Height
|
Weight
|
BMI
|
||||||||||||
| Years
|
Years
|
Meters
|
Kilograms
|
(m/kg2)
|
||||||||||||
| Median
|
Median
|
Median
|
Median
|
Median
|
||||||||||||
| 25% | 75% | 25% | 75% | 25% | 75% | 25% | 75% | 25% | 75% | |||||||
| Female left | 16 | 2.7 | 3.0 | 3.1 | 18 | 20 | 20 | 1.7 | 1.8 | 1.8 | 61 | 64 | 71 | 22 | 23 | 27 |
| Male left | 15 | 3.0 | 3.0 | 3.1 | 21 | 21 | 26 | 1.8 | 1.8 | 1.8 | 71 | 78 | 90 | 23 | 25 | 26 |
| Female right | 25 | 2.6 | 2.9 | 3.1 | 19 | 20 | 25 | 1.6 | 1.7 | 1.7 | 56 | 63 | 70 | 21 | 22 | 24 |
| Male right | 13 | 2.6 | 2.9 | 3.0 | 20 | 21 | 26 | 1.8 | 1.8 | 1.9 | 89 | 96 | 103 | 26 | 28 | 30 |
The chart shows the 25th percentile, median, and 75th percentile stratified by gender and side of injury, for each characteristic
Patients completed the hop test 2.2–3.2 years after ACL reconstruction. Age ranged from 16 to 35 years. Patient variables stratified by gender and surgical knee are presented in Table 1.
Hop ratios (Fig. 2)
Fig. 2.
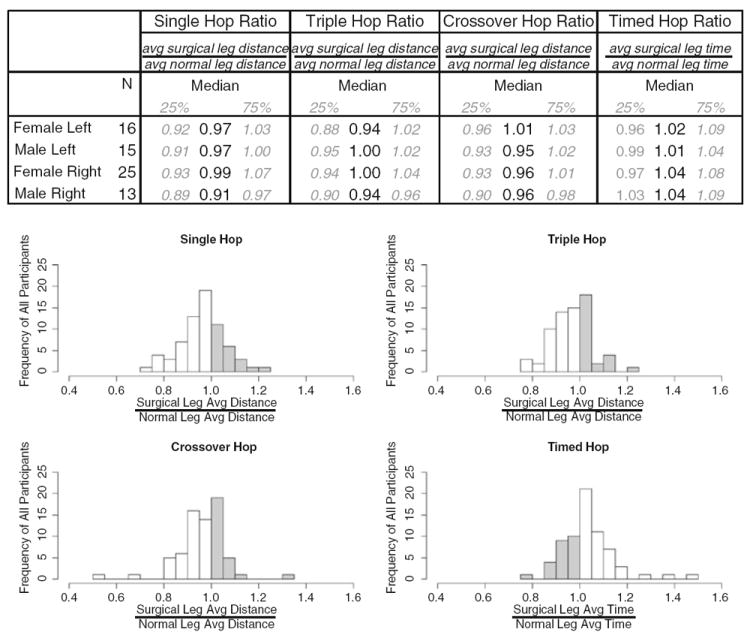
Hop ratio summary statistics. The chart shows the 25th, 50th, and 75th percentiles stratified by gender and side of injury, for each test. The histograms show for each test the frequency of ratios for the entire population. Gray bars represent ratios for which the surgical leg jumped further or faster than the normal leg. Frequencies were summed over ratios at 0.05 intervals
Figure 2 summarizes the frequency distributions of the hop ratios from the 4 tests, stratified by gender and surgical knee.
Patient-reported outcomes (Fig. 3)
Fig. 3.
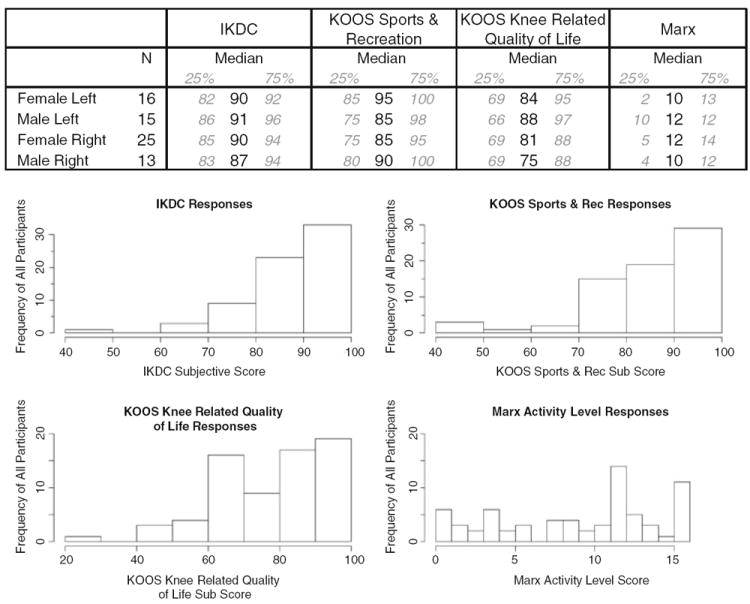
Patient-reported outcomes summary statistics. The chart shows the 25th percentile, median, and 75th percentile of hop ratios stratified by gender and side of injury, for each outcome score. The histograms show for each outcome score the frequency of ratios for the entire population. Frequencies were summed over ratios at 0.05 intervals
IKDC subjective scores, KOOS Sports and Recreation subscores, KOOS Knee Related Quality of Life subscores, and Marx activity scores were calculated for each person and summary statistics are shown in Fig. 3.
Correlation between hop tests and patient-reported outcomes (Table 2)
Table 2.
Spearman correlation
| Spearman correlation
|
||
|---|---|---|
| rho | P | |
| IKDC | ||
| Single hop | 0.3 | 0.001* |
| Triple hop | 0.4 | <0.001* |
| Crossover hop | 0.2 | 0.23 |
| Timed hop | −0.3 | 0.03* |
| KOOS sports and recreation | ||
| Single hop | 0.2 | 0.05* |
| Triple hop | 0.2 | 0.05* |
| Crossover hop | 0.2 | 0.07 |
| Timed hop | −0.2 | 0.11 |
| KOOS knee-related quality of life | ||
| Single hop | 0.2 | 0.19 |
| Triple hop | 0.3 | 0.01* |
| Crossover hop | 0.1 | 0.42 |
| Timed hop | −0.2 | 0.08 |
| Marx activity level | ||
| Single hop | 0.2 | 0.23 |
| Triple hop | 0.2 | 0.17 |
| Crossover hop | −0.1 | 0.60 |
| Timed hop | −0.2 | 0.14 |
Table of correlation coefficients (rho) and P values for each Spearman correlation for each outcome score with each hop test.
Indicates P values less than 0.05. These models are also shown in bold
Using Spearman correlations between each outcome measure and each hop test ratio, the strongest relationship was found to be a moderate, positive correlation between the IKDC scores and the hop ratios, particularly for the triple- and single-hop tests (Table 2). The KOOS Sports and Recreation subscore was weakly correlated with the triple- and single-hop test. For the KOOS Knee Related Quality of Life, only the correlation with the triple-hop ratio was significant, and it had a moderate rho value of 0.31. None of the hop ratios were significantly correlated with Marx activity levels.
Logistical model (Table 3)
Table 3.
Multivariable modeling
| Ordinary least squares: Outcome score ~ sex + BMI + faults (surgical leg) + faults (normal leg) + ratio (surgical leg avg distance/normal leg avg distance)
| |||||||
|---|---|---|---|---|---|---|---|
| Model- correlation values
|
Predictors—P values
|
||||||
| R2 values | Adj R2 values | Sex | BMI | Faults | Faults | Hop ratio | |
| Male | Weight
|
No. of faults on surgical leg | No. of faults on normal leg | Surgical leg avg measure
|
|||
| Height2 | Normal leg avg measure | ||||||
| IKDC | |||||||
| Single hop | 0.2 | 0.1 | 0.38 | 0.13 | 0.95 | 0.37 | <0.01* |
| Triple hop | 0.2 | 0.2 | 0.56 | 0.22 | 0.35 | 0.53 | <0.01* |
| Crossover hop | 0.2 | 0.1 | 0.32 | 0.03* | 0.65 | 0.08 | 0.06 |
| Timed hop | 0.2 | 0.1 | 0.52 | 0.13 | 0.65 | 0.99 | 0.01* |
| KOOS sports and recreation | |||||||
| Single hop | 0.2 | 0.1 | 0.53 | 0.95 | 0.02* | 0.26 | <0.01* |
| Triple hop | 0.1 | 0.0 | 0.51 | 0.97 | 0.19 | 0.45 | 0.06 |
| Crossover hop | 0.1 | 0.0 | 0.79 | 0.43 | 0.32 | 0.46 | 0.11 |
| Timed hop | 0.1 | 0.0 | 0.61 | 0.90 | 0.82 | 0.58 | 0.03* |
| KOOS knee-related quality of life | |||||||
| Single hop | 0.1 | 0.0 | 0.96 | 0.66 | 0.66 | 0.10 | 0.19 |
| Triple hop | 0.1 | 0.0 | 0.87 | 0.91 | 0.70 | 0.36 | 0.04* |
| Crossover hop | 0.0 | 0.0 | 0.82 | 0.52 | 0.56 | 0.46 | 0.55 |
| Timed hop | 0.1 | 0.0 | 0.99 | 0.69 | 0.84 | 0.92 | 0.07 |
| Marx | |||||||
| Single hop | 0.1 | 0.0 | 0.53 | 0.32 | 0.70 | 0.04* | 0.61 |
| Triple hop | 0.1 | 0.0 | 0.60 | 0.45 | 0.41 | 0.05* | 0.64 |
| Crossover hop | 0.1 | 0.0 | 0.41 | 0.18 | 0.16 | 0.22 | 0.93 |
| Timed hop | 0.1 | 0.0 | 0.49 | 0.51 | 0.78 | 0.84 | 0.18 |
Results of ordinary least squares modeling. General model is provided above the chart. Models are grouped by outcome score. Each model is identified by the hop test used to create the ratio. Coefficients, coefficients adjusted for the number of degrees of freedom, and the P value for each independent predictor are listed.
Indicates P values less than 0.05. These values are also shown in bold
Ordinary least squares multivariable modeling was used to describe the relationship between the patient-reported outcomes and the hop scores, accounting for the contributions of individual patient factors (Table 3). For the models regressed on the IKDC, the single-, triple-, and timed-hop ratios were significant contributors. BMI was a significant contributor in the IKDC regression model using the crossover hop. For the KOOS Sports and Recreation subscores, the single- and timed-hop ratios had P values less than 0.05 in their respective models. The triple-hop ratio had a P value of 0.06. The number of faults on the surgical leg was a significant contributor in the single-hop model. For the KOOS Knee Related Quality of Life subscore, the triple-hop ratio was a significant contributor to the model. For the Marx activity scores, no hop ratio provided any significant contribution to the model; however, the number of faults on the normal contralateral leg was shown to be significant for both the single- and triple-hop models. Predictive discrimination for the models tended to be low although the models for the IKDC had the best predictive value followed by the KOOS Sports and Recreation. The q–q plots of residuals from the ols models appeared normal.
Correlations between individual outcome questions and hop tests (Figs. 4, 5)
Fig. 4.
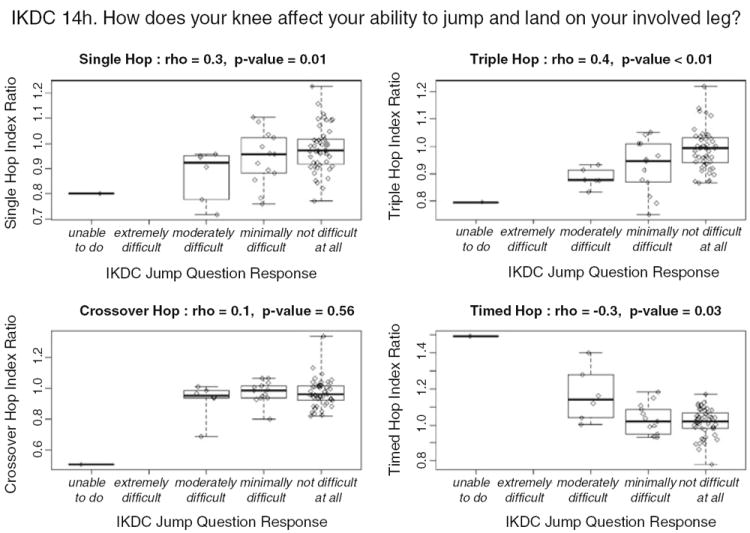
Hop ratios and IKDC jump question correlation. Box and whisker plots showing range 25th, 50th, and 75th quartiles for each hop ratios for each response. Individual ratios are represented by diamonds overlaying the box. Coefficients (rho) and P values for each Spearman correlation are above the plot. Actual jump question is provided above the graphs
Fig. 5.
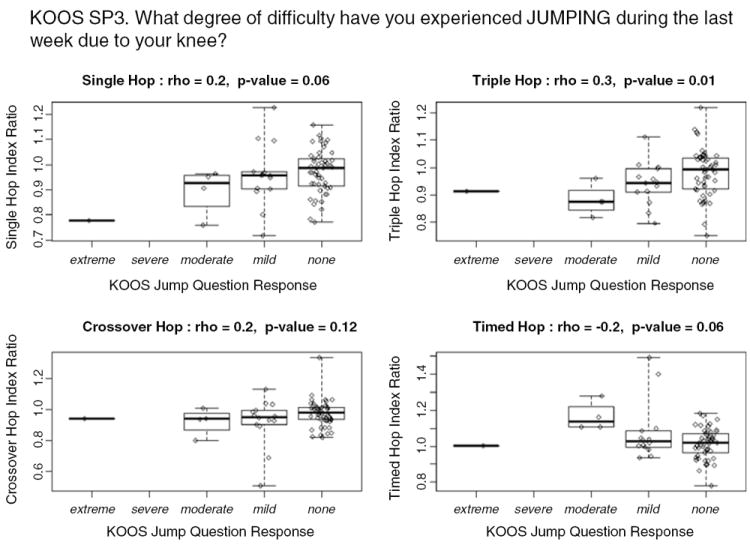
Hop ratios and KOOS jump question correlation. Box and whisker plots showing range 25th, 50th, and 75th quartiles for each hop ratio for each response. Individual ratios are represented by diamonds overlaying the box. Coefficients (rho) and P values for each Spearman correlation are above the plot. Actual jump question is provided above the graphs
For the IKDC jump question, the triple- and single-hop ratios had moderate correlation with significant P values (Fig. 4). The relationship with the timed-hop ratios was weaker but still significant. Again, the crossover hop had poor correlation with the individual jump question. For the KOOS jump question, the triple-hop ratio had moderate correlation and was significant (Fig. 5). The correlations with the single- and timed-hop ratios were a bit weaker and less significant.
Discussion
The most important finding of the present study was the moderate but significant correlation between the triple-hop ratios and the patient-reported outcomes. This study aimed to examine the relationship between measures of function taken from both patient- and clinician-oriented approaches at least 2 years post-ACL reconstruction. The reasons for choosing this time point were threefold: (1) the assumption that all patients had reached full recovery, as opposed to an earlier time point where function is likely to be measured as part of determination of fitness to return-to-play and highly variable among the group due to individualized healing and confidence; (2) due to an interest in evaluating surgical outcomes, and; (3) in accordance with the two-year minimum follow-up time recommended by the International Knee Documentation Committee.
Scores on the patient-reported outcome tools and the hop tests indicate that patients’ responses in this study 2 years after ACL reconstruction were consistent with previous reports. On the IKDC, most of the ACL reconstruction patients fell between the 25th and the 50th percentiles reported for normal populations of similar age [2]. In addition, KOOS Sports and Recreation and Knee Related Quality of Life subscores were comparable to those reported for the normal population and patients 1 year past ACL reconstruction [17, 22]. Hop scores on the single and timed hops are similar to those previously reported at 2 years post-ACL reconstruction [3, 24].
The current study found slightly higher correlations between hop scores and validated outcomes than found by similar studies. Previous work by Sernert et al. [24] looking at outcomes of ACL reconstruction approximately 2–5 years post-surgery showed a 0.28 correlation coefficient between the single hop and the global IKDC scores, slightly lower than the 0.32 coefficient found in this study. This lower score may be due to using the global score from an earlier version of the IKDC in the Sernert study, which included laxity and range of motion evaluated by an independent examiner in addition to the patient subjective score. The correlation of 0.24 for the single and triple hop with the KOOS Sports and Recreation subscore is in agreement with the single-hop results found at a similar time point for a group of reconstructed and conservatively treated patients with ACL tears, although in that study, P values were slightly higher (P = 0.07), possibly due to fewer subjects in their study [1]. In a series of older meniscectomized and normal patients, the correlation coefficient between the single hop and KOOS Sports and Recreation score was lower (r = 0.14) [21], possibly due to the difference in population. Other groups have used different patient-reported outcome tools at approximately 6 months post-ACL reconstruction and found moderate correlations with the hop tests [20, 29]. One study of 345 patients with ACL tears at 6 weeks post-injury found a significant but moderate correlation between the timed hop and a global prediction of knee function [9].
One might expect people with high activity levels in terms of running, cutting, stopping, and pivoting to be high functioning. However, what patients choose to do in terms of activity and level may not be directly related to their functional ability [13]. Finding that some people with high hop scores have low Marx activity levels was less surprising than finding that three individuals with hop ratios of 0.8 or less on the single hop had Marx activity level scores of 12, indicating that a high hop ratio is not always present in a patient with a high activity level. As the Marx activity score focuses on frequency and specific types of activity, it is possible that these individuals maintain high frequency of activity at less intensity than those with better functional scores. Interestingly, the one significant predictor of the Marx activity level score was the number of faults on the normal, contralateral limb. Based upon this team’s interactions with the patients, it is hypothesized that people with very high Marx scores tend to be more competitive and push themselves to achieve hop distances that are beyond their ability to land, even on their good side.
Additional analyses using multivariable modeling showed almost no significant additional contribution to predictability of the IKDC or KOOS subscores by gender or BMI. This was an unexpected result due to significant contribution of these patient variables to the KOOS and IKDC in other population and multivariable analyses [2, 7, 8, 18]. However, this sample is small and homogeneous compared with the population studies and the current analyses additionally less complex than these previous multivariable analyses, possibly explaining the differences seen.
The number of faults on each limb has not previously been examined, but was included in this analysis to account for both a learning effect and fatigue related to hopping over and above the expected four hops (practice plus three) per side and as a potential indicator of hop quality, control, and consistency. It was observed that two limbs may achieve the same distance, but for one, those successful hops may have been three among eight due to unsteady landings or poorly controlled direction of hop, while the other may have landed three in a row without a wobble. This study includes number of faults as a way of addressing hop quality control component without increasing the complexity of the testing procedure. Although faults on either leg were predominantly not predictive of patient-reported outcomes, they were a significant factor in the KOOS Sports and Recreation model using the single hop, and, as previously discussed, the number of faults on the normal limb was a significant factor in several models regressed on the Marx. Additionally, patients were generally consistent on which tests had the most faults. The crossover-hop test had the highest mean and a maximum of 10 faults per side, the timed hop had a maximum of two, and nearly all individuals had fewer than five faults per side for the single and triple hop (data not shown). While the crossover hop was not correlated with patient outcomes, previous studies of several functional tests indicated that the crossover was the best test to use for evaluating landing [28]. In this study this test incurred the most faults, leading to agreement that the crossover is the most difficult task in regard to landing. These data suggest that additional investigation into faults on hop tests is warranted.
These data show that for multiple models, the hop test ratio is a significant predictor for the patient-reported outcome scores; however, only a small part of the patient-reported outcome scores are explained by the results of the hop tests. To determine whether this may have been due to the number of items related to other functions included in the questionnaires, the single questions from the IKDC and the KOOS Sports and Recreation outcome tools specifically related to jumping were examined and compared with the hop test ratios using Spearman correlations. The correlations between the hop ratios and the questions specifically directed toward jumping were similar to the correlations found between the hop ratios and the overall outcomes scores. This similarity suggests that a model including a physical test score corresponding to each question on the outcome tool may not more strongly predict patient outcomes scores than the hop test does alone. This underscores the idea that while sharing some similarities, the information gleaned from observed measurements is different than what is obtained from patient report.
This study is not without its limitations. First, due to low patient number, reconstruction variables such as graft type, surgeon, as well as meniscal and chondral pathology and treatment were not included in the analysis. While neither graft type nor surgeon seems likely to affect these outcomes, meniscal and chondral status may. Second, patients were examined within a 16-month window. The assumption was made that no significant change in function either due to being in or out of sports seasons or to elapsed time would occur during the interval over which patients participated, but this assumption has not been tested. Third, site effect was not evaluated. Variance due to site was addressed and minimized by including training sessions and site visits to standardize testing protocol across centers, although the possibility of an effect remains. Fourth, no attempt was made to account for patients’ sports activities, and it is possible, for example, that basketball players perform differently on hop tests than soccer players due to higher incidence of jumping in their sport. Complete accounting for sports’ contributions would be potentially difficult since previous and secondary sports may also influence performance.
Conclusion
Moderate association between the patient-reported outcomes scores for the IKDC and KOOS subscores with the triple- and single-hop test reinforces the idea that neither method of evaluating patient function at least 2 years after ACL reconstruction can be directly substituted for the other, but that both measurements represent some complementary factors related to function. Even after accounting for patient characteristics, less than a quarter of the variability in the patient-reported outcomes scores can be explained by hop scores, and focusing on specific jumping questions has almost no improvement in correlation between patient response and measured hopping. However, for large studies where having all subjects return to the clinic is not feasible, patient-reported outcome scores related to function 2 years after reconstruction will provide relatively comparable results to those that might be collected by direct observation of hopping at that same time point.
Acknowledgments
The project described was supported in part by NIH Grants No. 5R01 AR053684 (Spindler) and 5 K23 AR052392-04 (Dunn) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, an AOSSM-MTF Career Development Award Supplement, a Pfizer Scholars Grant in Clinical Epidemiology, and a grant from NFL Charities. The project was further supported by unrestricted educational gifts from DonJoy, Smith and Nephew Endoscopy, and the Vanderbilt Sports Medicine Research Fund. The authors thank the research coordinators, research assistants, mentors, and others at the participating institutions for their tireless efforts and continuing support in making this project possible. The authors specifically thank MOON (Multicenter Orthopaedic Outcomes Network) members for their support and contributions: Brian R. Wolf, MD, MS (University of Iowa); Robert H. Brophy, MD (Washington University in St. Louis); Robert G. Marx, MD, MSc (Hospital for Special Surgery); Jack T. Andrish, MD (Cleveland Clinic Foundation); Rick W. Wright, MD (Washington University in St. Louis); James L. Carey, MD, MPH (Vanderbilt); Charles L. Cox, MD, MPH (Vanderbilt); Annunziato Amendola, MD (University of Iowa); Eric C. McCarty, MD (University of Colorado); Matthew J. Matava, MD (Washington University in St. Louis). The authors would also like to thank Erica Scaramuzza, Zhouwen Liu, Thomas Dupont, Gene Hannah, MD, Robert S. Dittus, MD, MPH (Vanderbilt); Breanna Beck, ATC, (Ohio State University) Michelle Hines, RN, Lisa Hegemier, PA, Valerie Lewis, and Scott Euype, DPT (Cleveland Clinic Foundation); and Lynn S. Cain (Vanderbilt) for editorial assistance.
Contributor Information
Emily K. Reinke, Department of Orthopaedics and Rehabilitation, Vanderbilt University Medical School, Nashville, TN, USA
Kurt P. Spindler, Email: kurt.spindler@vanderbilt.edu, Department of Orthopaedics and Rehabilitation, Vanderbilt University Medical School, Nashville, TN, USA.
Dawn Lorring, Department of Orthopaedic Surgery, Cleveland Clinic Foundation, Cleveland, OH, USA.
Morgan H. Jones, Department of Orthopaedic Surgery, Cleveland Clinic Foundation, Cleveland, OH, USA
Leah Schmitz, Department of Orthopaedic Surgery, Cleveland Clinic Foundation, Cleveland, OH, USA.
David C. Flanigan, Department of Orthopaedic Surgery, The Ohio State University School of Medicine, Columbus, OH, USA
Angel Qi An, Department of Biostatistics, Vanderbilt University Medical School, Nashville, TN, USA.
Amanda R. Quiram, Department of Orthopaedics and Rehabilitation, Vanderbilt University Medical School, Nashville, TN, USA
Emily Preston, Department of Orthopaedics and Rehabilitation, Vanderbilt University Medical School, Nashville, TN, USA.
Michael Martin, Department of Orthopaedic Surgery, The Ohio State University School of Medicine, Columbus, OH, USA.
Bettina Schroeder, Department of Orthopaedic Surgery, The Ohio State University School of Medicine, Columbus, OH, USA.
Richard D. Parker, Department of Orthopaedic Surgery, Cleveland Clinic Foundation, Cleveland, OH, USA
Christopher C. Kaeding, Department of Orthopaedic Surgery, The Ohio State University School of Medicine, Columbus, OH, USA
Lynn Borzi, Department of Orthopaedic Surgery, Cleveland Clinic Foundation, Cleveland, OH, USA.
Angela Pedroza, Department of Orthopaedic Surgery, The Ohio State University School of Medicine, Columbus, OH, USA.
Laura J. Huston, Department of Orthopaedics and Rehabilitation, Vanderbilt University Medical School, Nashville, TN, USA
Frank E. Harrell, Jr, Department of Biostatistics, Vanderbilt University Medical School, Nashville, TN, USA.
Warren R. Dunn, Department of Orthopaedics and Rehabilitation, Vanderbilt University Medical School, Nashville, TN, USA
References
- 1.Ageberg E, Thomee R, Neeter C, et al. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup. Arthritis Rheum. 2008;59:1773–1779. doi: 10.1002/art.24066. [DOI] [PubMed] [Google Scholar]
- 2.Anderson AF, Irrgang JJ, Kocher MS, et al. The International Knee Documentation Committee subjective knee evaluation form: normative data. Am J Sports Med. 2006;34:128–135. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 3.Bach BR, Jr, Tradonsky S, Bojchuk J, et al. Arthroscopically assisted anterior cruciate ligament reconstruction using patellar tendon autograft. Five- to nine-year follow-up evaluation. Am J Sports Med. 1998;26:20–29. doi: 10.1177/03635465980260012101. [DOI] [PubMed] [Google Scholar]
- 4.Bent NP, Wright CC, Rushton AB, et al. Selecting outcome measures in sports medicine: a guide for practitioners using the example of anterior cruciate ligament rehabilitation. Br J Sports Med. 2009;43:1006–1012. doi: 10.1136/bjsm.2009.057356. [DOI] [PubMed] [Google Scholar]
- 5.Cohen J. Statistical power analysis for the behavioral sciences. 2. Erlbaum Associates, Inc.; Hillsdale: 1988. [Google Scholar]
- 6.Denegar CR, Vela LI, Evans TA. Evidence-based sports medicine: outcomes instruments for active populations. Clin Sports Med. 2008;27:339–351. vii. doi: 10.1016/j.csm.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38:2040–2050. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunn WR, Spindler KP, Amendola A, et al. Which preoperative factors, including bone bruise, are associated with knee pain/symptoms at index anterior cruciate ligament reconstruction (ACLR)? A Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38:1778–1787. doi: 10.1177/0363546510370279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury: part 2, determinants of dynamic knee stability. Am J Sports Med. 2008;36:48–56. doi: 10.1177/0363546507308191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 11.Keskula DR, Duncan JB, Davis VL, et al. Functional outcome measures for knee dysfunction assessment. J Athl Train. 1996;31:105–110. [PMC free article] [PubMed] [Google Scholar]
- 12.Kocher MS, Steadman JR, Briggs K, et al. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84-A:1560–1572. doi: 10.2106/00004623-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Marx RG, Stump TJ, Jones EC, et al. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29:213–218. doi: 10.1177/03635465010290021601. [DOI] [PubMed] [Google Scholar]
- 14.Moller E, Weidenhielm L, Werner S. Outcome and knee-related quality of life after anterior cruciate ligament reconstruction: a long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2009;17:786–794. doi: 10.1007/s00167-009-0788-y. [DOI] [PubMed] [Google Scholar]
- 15.Neeb TB, Aufdemkampe G, Wagener JH, et al. Assessing anterior cruciate ligament injuries: the association and differential value of questionnaires, clinical tests, and functional tests. J Orthop Sports Phys Ther. 1997;26:324–331. doi: 10.2519/jospt.1997.26.6.324. [DOI] [PubMed] [Google Scholar]
- 16.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 17.Paradowski PT, Bergman S, Sunden-Lundius A. Knee complaints vary with age and gender in the adult population. Population-based reference data for the knee injury and osteoarthritis outcome score (KOOS) BMC Musculoskelet Disord. 2006;7:38. doi: 10.1186/1471-2474-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paradowski PT, Englund M, Lohmander LS, et al. The effect of patient characteristics on variability in pain and function over two years in early knee osteoarthritis. Health Qual Life Outcomes. 2005;3:59. doi: 10.1186/1477-7525-3-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.R Development Core Team. R A language and environment for statistical computing. 2.9.2. R Foundation for statistical computing; Vienna, Austria: 2009. [Google Scholar]
- 20.Reid A, Birmingham TB, Stratford PW, et al. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87:337–349. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- 21.Roos EM, Bremander AB, Englund M, et al. Change in self-reported outcomes and objective physical function over 7 years in middle-aged subjects with or at high risk of knee osteoarthritis. Ann Rheum Dis. 2008;67:505–510. doi: 10.1136/ard.2007.074088. [DOI] [PubMed] [Google Scholar]
- 22.Roos EM, Roos HP, Lohmander LS, et al. Knee injury and osteoarthritis outcome score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 23.Ross MD, Langford B, Whelan PJ. Test-retest reliability of 4 single-leg horizontal hop tests. J Strength Cond Res. 2002;16:617–622. [PubMed] [Google Scholar]
- 24.Sernert N, Kartus J, Kohler K, et al. Analysis of subjective, objective and functional examination tests after anterior cruciate ligament reconstruction. A follow-up of 527 patients. Knee Surg Sports Traumatol Arthrosc. 1999;7:160–165. doi: 10.1007/s001670050141. [DOI] [PubMed] [Google Scholar]
- 25.Suk M, Norvell DC, Hanson B, et al. Evidence-based orthopaedic surgery: what is evidence without the outcomes? J Am Acad Orthop Surg. 2008;16:123–129. doi: 10.5435/00124635-200803000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Tanner SM, Dainty KN, Marx RG, et al. Knee-specific quality-of-life instruments: which ones measure symptoms and disabilities most important to patients? Am J Sports Med. 2007;35:1450–1458. doi: 10.1177/0363546507301883. [DOI] [PubMed] [Google Scholar]
- 27.Valovich McLeod TC, Snyder AR, Parsons JT, et al. Using disablement models and clinical outcomes assessment to enable evidence-based athletic training practice, part II: clinical outcomes assessment. J Athl Train. 2008;43:437–445. doi: 10.4085/1062-6050-43.4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Porat A, Holmstrom E, Roos EM. Reliability and validity of videotaped functional performance tests in ACL-injured subjects. Physiother Res Int. 2008;13:119–130. doi: 10.1002/pri.401. [DOI] [PubMed] [Google Scholar]
- 29.Wilk KE, Romaniello WT, Soscia SM, et al. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20:60–73. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]
- 30.Wright RW. Knee injury outcomes measures. J Am Acad Orthop Surg. 2009;17:31–39. doi: 10.5435/00124635-200901000-00005. [DOI] [PubMed] [Google Scholar]


