Abstract
With rising burdens of obesity and chronic disease, the role of diet as a modifiable risk factor is of increasing public health interest. There is a growing body of evidence that low consumption of dairy products is associated with elevated risk of chronic metabolic and cardiovascular disorders. Surveys also suggest that dairy product consumption falls well below recommended targets for much of the population in many countries, including the USA, UK, and Australia. We reviewed the scientific literature on the health effects of dairy product consumption (both positive and negative) and used the best available evidence to estimate the direct healthcare expenditure and burden of disease [disability-adjusted life years (DALY)] attributable to low consumption of dairy products in Australia. We implemented a novel technique for estimating population attributable risk developed for application in nutrition and other areas in which exposure to risk is a continuous variable. We found that in the 2010–2011 financial year, AUD$2.0 billion (USD$2.1 billion, €1.6 billion, or ∼1.7% of direct healthcare expenditure) and the loss of 75,012 DALY were attributable to low dairy product consumption. In sensitivity analyses, varying core assumptions yielded corresponding estimates of AUD$1.1–3.8 billion (0.9–3.3%) and 38,299–151,061 DALY lost. The estimated healthcare cost attributable to low dairy product consumption is comparable with total spending on public health in Australia (AUD$2.0 billion in 2009–2010). These findings justify the development and evaluation of cost-effective interventions that use dairy products as a vector for reducing the costs of diet-related disease.
Introduction
Diet is increasingly recognized as a matter of public health concern, with most developed nations publishing food-based dietary guidelines (FBDG)4 for healthy eating that reflect the role of diet for health (1–5). Recommendations may relate to essential micronutrients, the balance of macronutrients, or total energy intake. The Australian guidelines are broadly phrased (e.g., “eat plenty of vegetables, legumes and fruit”) but supplemented by a food selection guide (FSG) that recommends a minimum number of standard serving units5 to aim for in each food group (3). These minimum targets together provide ∼70% of the micronutrient requirements and one-half of the average energy needs for defined age/sex demographics (6). By following the FSG, it is presumed that the remaining 30% of nutrient requirements would be met by whichever foods are selected to fulfill the individual’s energy needs.
The typical diet of the Australian population is not consistent with the FSG, especially with respect to underconsumption of vegetables (7) and dairy foods (8). A consequence of this is that many Australians fail to achieve the recommended daily intakes of some essential micronutrients, as is documented for calcium, vitamin A, folate, magnesium, iron, and zinc (9). Diets that lack essential nutrients or contain an unbalanced mix of macronutrients have adverse implications for individual health and are responsible for excess morbidity, reduced quality of life, and premature death (10, 11). These in turn increase the demand for health services, thus creating a problem at the population level (11).
Very little has been invested by Australian governments to address poor diet at the population level. In 2008–2009 the total expenditure on public health activities accounted for only 2.1% of total recurrent health expenditure, of which “encouraging healthy weight through nutrition and exercise” was 1 of 7 programs that collectively accounted for 17% of this budget (12). Less than 0.1% of the recurrent health budget was allocated by governments at a population level to promoting a healthy diet and almost exclusively in the context of body weight management.
In considering what resources should be allocated to encourage the adoption of a healthier diet, it is useful to understand the costs to society of current deviations from the recommended diet. Estimates of attributable costs can highlight where effective interventions might yield good returns. Health economists classify attributable costs into impacts on health (i.e., morbidity, mortality, and quality of life), impacts on the healthcare budgets, and other impacts of poor health on society. These are often referred to as burden of disease, direct costs, and indirect costs, respectively (13). In this article, we report findings from a cost-of-illness analysis, which focuses on one dietary component for which most Australians fail to meet the recommended target for consumption: dairy foods (4, 8).
The Australian FBDG recommend including “milks, yogurts, cheeses and/or alternatives” (referred to in this article as dairy foods) as part of a varied diet (3), while the FSG recommends that people aged ≥4 y should aim for a minimum of between 2 and 3 servings of dairy foods per day, depending on age and gender (2). Similar recommendations have been published by government bodies in the US (4) and Canada (1), but the U.K. government has yet to develop quantitative FBDG (5). Evidence suggests that only 35% of Australians meet their recommended number of daily servings of dairy foods (8).
Dairy foods are the primary source of calcium in the Australian diet (2) and contain a wide range of micro- and macronutrients such as vitamin A, folate, magnesium, and zinc, for which a considerable proportion of the population fail to meet the recommended daily intake (9). Dairy foods are also a valuable source of protein and contain a wide variety of fatty acids, including several with cardioprotective effects (14). The nutritional value of dairy foods may be affected by processes such as fat-skimming and heat treatment (14), but the implications for health are not well understood.
There is a growing body of evidence to support a protective effect of dairy product consumption on the risk of chronic disease (15–19) and there is some evidence of greater health benefits being associated with whole-fat milk than skim milk (20). In the current review of Australian dietary guidelines, systematic reviews of the literature found “satisfactory” or “good” evidence of associations between dairy product consumption and 8 beneficial health outcomes [improved bone mineral density and reduced risk of ischemic heart disease (IHD), stroke, hypertension, type II diabetes, metabolic syndrome, colorectal cancer (CRCa), and rectal cancer) and “poor” evidence of an association with one negative health outcome [increased risk of prostate cancer (PrCa)]6 (22). Our study aims to quantify the potential effects of increasing Australians’ dairy product consumption to recommended levels in terms of both the impact on population health and on the direct costs of healthcare (indirect costs were excluded from the analysis).
The potential benefits of increasing Australians’ consumption of dairy products to recommended levels can be considered equivalent to the current costs of low consumption of dairy products. Calculation of these costs relies upon an estimation of population attributable risk (PAR), which measures the portion of disease incidence that can be attributed to low consumption of dairy products. Attributable risk analyses compare the current health status of a population with a “counterfactual” state in which the risk factor has been removed, i.e., a state in which everyone consumes at least the recommended amount of dairy products. This is distinct from analyzing a change from one state to the other, which would have associated costs that are not represented in an analysis of PAR (but would be within a cost-effectiveness or cost-benefit analysis). However, when PAR is high, then modifying the risk factor will also have a large impact on the incidence of disease. Therefore, interventions are more likely to prove cost effective or cost saving and the rationale for cost-of-illness and PAR analyses is to identify areas for further research and development of effective interventions.
Methods for calculating PAR rely on being able to categorize exposure and determine the relative increase in risk for each category of exposure when compared with the category of least risk (23). However, in the case of consumption of a broad dietary food group, exposure is not a categorical variable; any distinctions made between one level of dairy product consumption and another are largely arbitrary and do not represent thresholds in either the distribution of consumption or its relationship to risk of disease. In this article, we present a modified technique for applying standard PAR formulae in a manner that more closely approximates the treatment of exposure and risk as continuous variables and is thus well adapted to nutrition research.
Approach and Methods
Overview.
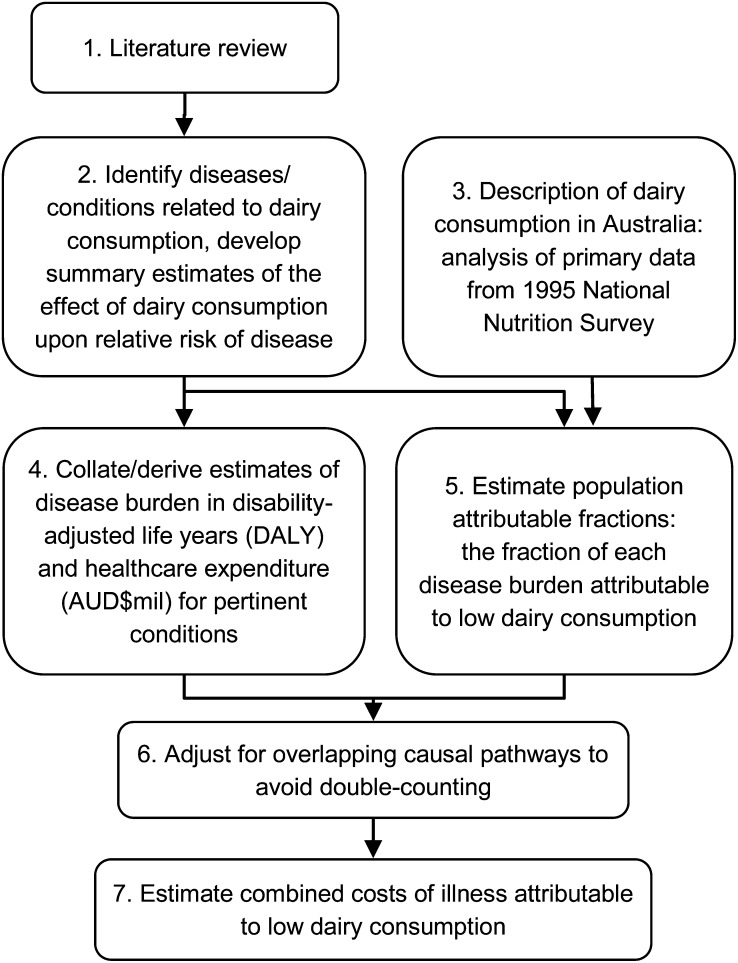
The approach taken in this analysis is illustrated in Figure 1. A literature review was undertaken to identify health outcomes that may be affected, either positively or negatively, by consumption of dairy products. For each outcome identified, estimates for the RR associated with low compared with recommended levels of dairy product consumption were sought from empirical studies. The RR were then combined with data on population dietary patterns from an analysis of the 1995 Australian National Nutrition Survey (NNS) (8) to calculate PAR, and the PAR were then applied to estimates of disease burden and healthcare expenditure. Burden of disease was defined in units of disability-adjusted life years (DALY), a measure that combines the effects of disease upon morbidity and mortality. Estimates of direct healthcare expenditure included all healthcare costs (hospital, pharmaceutical, clinical, etc.) that were directly attributable to the outcome, irrespective of who incurred the cost (e.g., government, patient, insurance provider). Indirect costs, such as those arising from reduced economic production, were not included in the analysis.
FIGURE 1.
Overview of analytic process. One serving of dairy is equivalent to 250 mL milk, 200 g yogurt, or 40 g cheese.
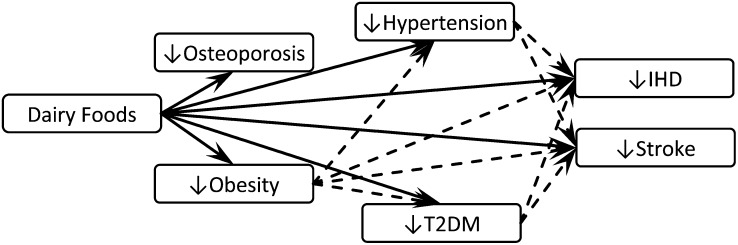
To avoid double-counting, the costs attributable to low consumption of dairy products were summed across health outcomes only once adjustments had been made for overlapping causal pathways (Fig. 2). This is a critical step, because without such an adjustment, overestimation is certain and can be substantial (10).
FIGURE 2.
Associations between dairy product consumption and eight diseases or risk factors. Within the text boxes, a downwards pointing arrow indicates that increasing dairy product consumption to recommended levels would decrease incidence of the disease or risk factor, and inversely. Between the text boxes, solid lines represent associations with consistent evidence bases and plausible mechanisms while dashed lines represent overlapping causal pathways. Where causal pathways overlapped, estimates for disease burden and expenditure on the proximal disease or risk factor (illustrated left to right) were adjusted to exclude the attributable portion of the distal disease to avoid double-counting. IHD, ischemic heart disease; T2DM, type 2 diabetes mellitus.
Values reported in tables are point estimates and do not have associated variance or significance parameters.
Identifying diseases related to dairy product consumption.
The aim of the literature review was to identify relevant studies reporting outcomes suitable for economic analysis rather than formally assess the evidence for each effect. A total of 223 refereed articles were reviewed to establish if they met inclusion criteria with respect to reporting of: 1) the level of total dairy product consumption for designated subgroups and 2) either the incidence of disease or the development of an established risk factor for disease (e.g., obesity) across levels of dairy product consumption. Studies reporting only intermediate outcomes such as changes in biochemistry or biometrics were excluded. No prior selection was made to limit the scope of diseases included in the search or the analysis.
Obtaining RR.
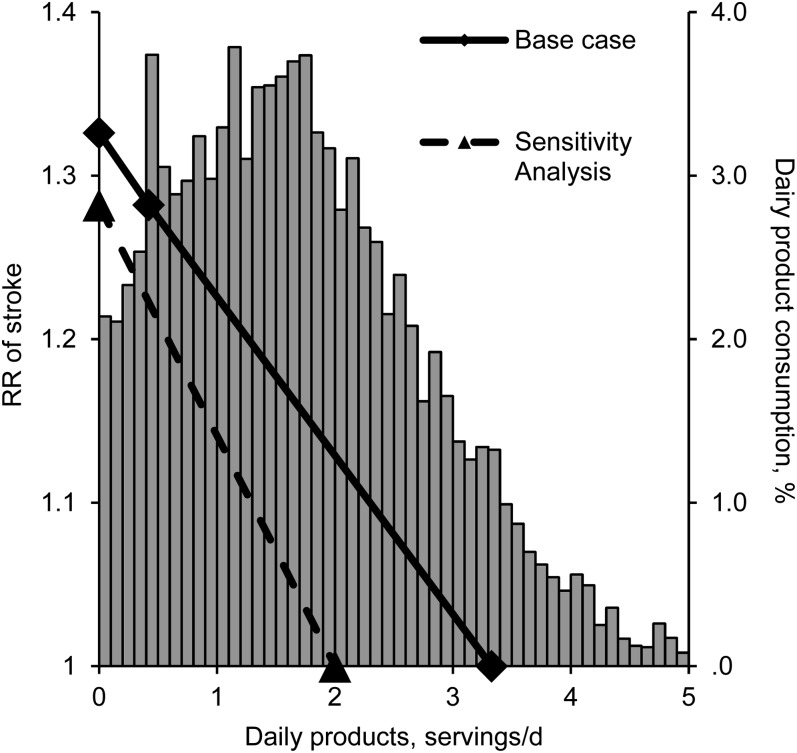
For each disease for which there was published evidence of an association with dairy product consumption, RR were extracted from the study that represented the highest “level of evidence for studies of etiology or harm” (24). If the highest level of evidence included more than one study, preference was given to studies based on larger samples. Because there was considerable variation in the way in which dairy product consumption was measured in the original studies, all of the quantitative systematic reviews that were identified adopted the strategy of categorically meta-analyzing study data as “high” compared with “low” consumption of dairy products rather than treating consumption as a continuous variable. This is similar to the way in which most of the individual studies analyzed disease risk by quintiles or other ordinal categories of consumption. Thus, when RR were extracted from meta-analyses, they were assumed to relate to consumption levels at the medians of the first and fifth quintiles (i.e., the 10th and 90th percentiles) of the Australian population. These correspond to 0.4 and 3.3 servings/d, respectively (8). We assumed a linear relationship between risk of outcome and consumption across this range (as illustrated in Fig. 3 for stroke). Variation of these assumptions in the sensitivity analyses is discussed below.
FIGURE 3.
Consumption of dairy products in Australia and the relative risk of stroke. In ‘high versus low’ meta-analysis of the effects of dairy product consumption upon stroke, Elwood et al. (17) report the relative risk of stroke to be 0.78 (equivalent to 1.28 comparing low consumption level with high). Based on this result and on median daily consumptions of 0.5 and 3.4 servings of dairy foods in the first and fifth quintiles of the Australian population (8), the solid line shows how risk of stroke was assumed to vary with dairy product consumption in the base case analysis (including an extrapolation from 0.5 to 0.0 servings). In sensitivity analysis S1, the same RR was assumed to relate to nil consumption and two servings per day (the lower limit of the recommended daily consumption according to Australian guidelines (2). In both analyses, it was assumed that no further reductions in risk would occur beyond the point at which RR = 1.00.
To calculate risk across the entire population (not just for the lowest quintile), we divided the population into finely differentiated categories of daily dairy product consumption (increments of 0.1 standard servings). The population within each category was considered to be at a RR of disease that was equal to the intersection of the category midpoint with a linear regression of RR (Fig. 3). In this way, we were able to model risk in a more realistic manner, avoiding the assumption of constant risk across broad ranges of consumption. An even more realistic approach would allow for nonlinear associations between consumption and risk, but this was beyond the limits of the 2 data points provided by each meta-analysis.
Disease burdens and expenditure.
Wherever possible, estimates of disease burden and expenditure were sought from the Australian Institute of Health and Welfare. When those estimates were unavailable, they were obtained from the peer-reviewed literature, from other government reports, or from primary analysis of publicly available databases and government reports. Estimates were updated to Australian fiscal year 2010–2011 values and measured in Australian fiscal year 2010–2011 dollars using projections by Voss et al. (25) or Access Economics (26–28) and adjusted for inflation using the Australian Total Health Price Index (29). A full description of these data sources and the methods used to update them is available in Supplemental Appendix A.
Consumption of dairy products in Australia.
Due to the paucity of published information on consumption of dairy products in Australia, it was necessary to conduct a descriptive analysis of primary data from the NNS (30). The NNS provides data for Australians aged ≥2 y based on a sample of 13,858 individuals weighted according to demographic characteristics of the population. Although some more recent datasets do exist (31–34), they are either limited to only a subgroup of the population or do not provide sufficient detail of dairy product consumption patterns for economic evaluation. A full description of the methods and findings of the NNS study, along with a discussion of the other datasets and what they indicate about more recent changes to Australians’ consumption of dairy foods, has been reported elsewhere (8). In brief, we described the distribution of dairy product consumption in standard servings by combining data from a 24-h recall with data from a FFQ administered to a subsample of 9906 participants aged ≥12 y.
Estimating PAR.
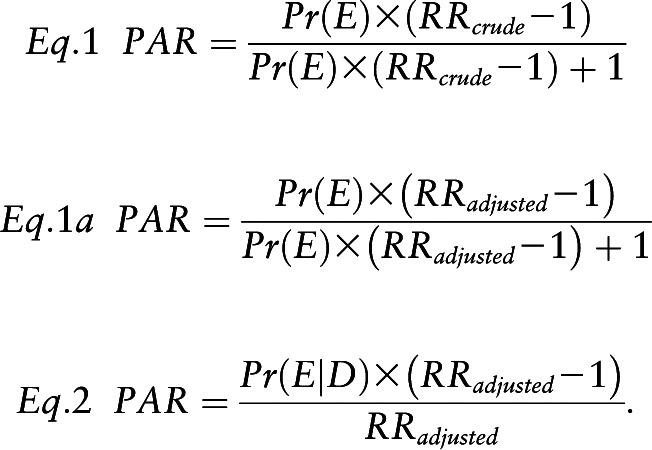
Our base case analysis broadly followed the approach used by the WHO Comparative Risk Assessment project [CRA; part of the Global Burden of Disease study (35)] but incorporates some changes to achieve greater methodological rigor. The CRA estimated the fraction of disease that could be attributed to a selection of common risk factors, including dietary factors, but not low consumption of dairy foods. The approach adopted by the CRA was to adapt a formula (Eq. 1) by incorporating adjusted RR instead of crude RR (Eq. 1a). Both Eq. 1 and 1a are biased in the presence of confounding variables (i.e., if adjusted RR does not equal crude RR) (23), although Eq. 1a is defended on the basis that the bias is often, but not always, conservative (36). The theoretically valid approach (Eq. 2) uses the prevalence of exposure among cases of the disease,  rather than the prevalence of exposure in the population,
rather than the prevalence of exposure in the population,  (37). Although this statistic is available in most observational studies, it is rarely reported outside of case-control studies in which it is used to calculate an OR. We used this more rigorous approach where possible, using Eq. 1a only when
(37). Although this statistic is available in most observational studies, it is rarely reported outside of case-control studies in which it is used to calculate an OR. We used this more rigorous approach where possible, using Eq. 1a only when  was not available.
was not available.
 |
Core assumptions and sensitivity analyses.
We acknowledged that the analysis would be sensitive to variation in the assumptions used to relate levels of dairy product consumption in the source studies to levels in the Australian population and to RR. A multivariate sensitivity analysis (S1) was performed in which conservative but plausible assumptions were adopted across key parameters connecting exposure to risk. In S1, meta-analyzed RR were assumed to compare nil dairy product consumption with 2 servings/d, the lower limit of the current Australian recommendations (Fig. 3). This was considered to be the most conservative interpretation of the results of low compared with high consumption of dairy products from meta-analyses. Because the effect of varying this one parameter was similar to adopting smaller estimates of effect size for each outcome, the individual RR parameters were not separately varied.
When we could not use Eq. 2 in the base case analysis, we used secondary data from individual risk studies to calculate the PAR for low consumption of dairy products in their study samples according to Eq. 2. Because there were few assumptions involved in such analyses, they provided relatively unbiased estimates of PAR for those study samples and a benchmark for comparison with estimates of Australian PAR that have had to rely upon the use of Eq. 1a. If both dairy product consumption and the background risk of disease in the study sample are similar to the Australian population, then the PAR should also be similar; any substantial difference between the estimates is likely to represent the bias inherent in the misapplication of Eq. 1a. A second sensitivity analysis (S2) was conducted, applying these study-specific PAR to the Australian population. The core assumption in S2 was that there were no differences between the patterns of dairy product consumption and other disease risk factors between the study populations and the current Australian population.
Results
Effects of dairy product consumption on risk of disease.
From a review of the literature, 6 health outcomes—type 2 diabetes mellitus (T2DM), IHD, stoke, osteoporosis, obesity, and hypertension—were identified, for which there was strong evidence of independent associations with total consumption of dairy products. The key studies contributing to these conclusions and the economic analysis are listed in Table 1.
TABLE 1.
Effects of dairy product consumption on risk of disease: core findings from a review of the literature1
| Disease or risk factor | RR2 | Core studies |
| Obesity | 0.70 (35+ times/wk vs.0–10 times/wk) | Based on data reported by Pereira et al. (2002) (39) (prospective cohort study, level 2b evidence), supported by Dougkas et al. (2011)3 (16) (systematic review of observational and interventional studies, level 2a evidence) |
| T2DM | 0.85 (high vs. low consumption) | Elwood et al. (2010)4 (17) (homogenous meta-analysis of 5 prospective cohort studies, level 2a evidence) |
| IHD | 0.92 (high vs. low consumption) | Elwood et al. (2010) (17) (homogenous meta-analysis of 11 prospective cohort studies, level 2a evidence) |
| Stroke | 0.78 (high vs. low consumption) | Elwood et al. (2010) (17) (homogenous meta-analysis of 11 prospective cohort studies, level 2a evidence) |
| Hypertension | 0.87 (high vs. low consumption) | Ralston et al. (2011) (19) (homogenous meta-analysis of 5 prospective cohort studies, level 2a evidence) |
| Osteoporosis | 0.96 (per increase of 300 mg dietary calcium) | Cumming et al. (1997) (38) (homogenous meta-analysis of 5 cohort studies, level 2a evidence) |
IHD, ischemic heart disease; T2DM, type 2 diabetes mellitus.
RR of disease or risk factor in low consumption of dairy products compared with high consumption of dairy products.
This systematic review did not include a meta-analysis and so does not provide any quantitative outcomes suitable for economic modeling.
The authors of this meta-analysis reported statistical heterogeneity (17), but closer examination revealed that the only outlier was a study of high-fat dairy foods in which a positive association was reported, excluding this (because of the inappropriate exposure), would have substantially reduced heterogeneity.
Homogenous meta-analyses of cohort studies [meta-analyses that demonstrate consistency in the results of their studies and therefore represent a high level of evidence (24)] found significant negative associations between increasing consumption of dairy products and risk of T2DM (17), IHD (17), osteoporosis (38), and hypertension (19). Increasing levels of dairy product consumption were found to be protective for each of these conditions. A meta-analysis of studies investigating the effect of dairy product consumption upon risk of stroke reported statistical heterogeneity (17), although close examination revealed that the only outlier was a single study that had investigated the effect of high-fat dairy foods upon risk and reported a positive association; excluding this study would have substantially reduced heterogeneity and revealed a greater benefit of total dairy product consumption. Thus, stroke was included as an outcome in the economic analysis. A recent systematic review found that dairy product consumption is associated with improved maintenance of healthy body weight (16), but only one study was identified that reported on the incidence of obesity across levels of total dairy product consumption (39) (the outcome most relevant to a cost of illness study), and this study warrants more detailed discussion.
Pereira et al. (39) analyzed data from the Coronary Artery Risk Development in Young Adults (CARDIA) cohort to investigate the role of dairy foods in prevention of insulin resistance syndrome, as characterized by the presence of (2 of) obesity, hypertension, abnormal glucose homeostasis, and dyslipidemia. The authors report an analysis that was stratified by baseline overweight status that found significantly better metabolic profiles with high compared with low consumption of dairy products among individuals who were overweight at baseline. In the subgroup who were not overweight at baseline, the trend to improvement was not significant. An analysis of the entire cohort was not reported, but close examination of the findings reveals that analysis in the normal-weight stratum was underpowered, because this group naturally had a much lower incidence of obesity. Furthermore, because anyone who becomes obese must first be overweight, separate measures of RR have no meaningful interpretation. Thus, in our base case analysis, we adopted the RR reported by Pereira et al. (39) for their overweight subgroup. In S2, we pooled the results of the subgroup analyses to produce a RR of obesity of 1.89 in the first compared with the fifth quintiles for the whole cohort.
Two further outcomes, CRCa and PrCa, were identified as potentially associated with dairy product consumption, but after a careful analysis of both trials and published reviews, the results were considered inconclusive in terms of the presence or direction of impact. One homogenous meta-analyses found a significant negative association with CRCa (18), although a subsequently published cohort study reported a positive association with childhood dairy product consumption (40). Two meta-analyses that did not report any formal tests of heterogeneity found a small but significant positive association between dairy product consumption and risk of PrCa, whereas a subsequent homogenous meta-analysis did not find any significant associations (41) and a 65-y cohort study found that childhood dairy product consumption decreased the risk of PrCa (40). Because of uncertainty regarding the effects of dairy foods upon risk of these 2 cancers, they were excluded from the analysis.
Attributable burden of disease and expenditure.
Updated estimates of the total Australian direct healthcare expenditure and burden of disease for the selected health conditions are reported in Table 2. The combined amounts in parentheses represent the burden or cost of each outcome that is exclusive of overlapping causal pathways.
TABLE 2.
Total costs of illness for selected health conditions in Australia, 2010–20111
| Disease or risk factor | Total estimated costs of illness in 2010–2011 |
|||
|
Direct healthcare expenditure
(AUD$million) |
Burden of disease (DALY) |
|||
| Sep2 | ∑3 | Sep2 | ∑3 | |
| Obesity | 79834,5 | (5848)7 | 238,0145,6 | (45,482)7 |
| T2DM | 49548 | (2328)9 | 454,7236,10 | (180,498)9 |
| IHD | 242611,12 | (2426)13 | 271,7976,12 | (271,797)13 |
| Stroke | 147011,13 | (1470)12 | 135,0036,13 | (135,003)12 |
| Hypertension | 207713,14 | (1347)9 | 205,5936,15 | (129,413)16 |
| Osteoporosis | 359617 | (3596)18 | 32,27517 | (32,275)18 |
| Total | 17,016 | 794,468 | ||
Values are point estimates. DALY, disability-adjusted life year; IHD, ischemic heart disease; Sep, separately; T2DM, type 2 diabetes mellitus.
Updated according to health price index and epidemiological estimates (see table notes below and the online Supplemental Appendix).
Updated and adjusted for overlapping causal pathways as to be mutually exclusive, thereby allowing summation (should not be used or interpreted individually).
Based on estimates by Colagiuri et al. (43).
Based on estimates by Begg et al. (10).
Excluding obesity-attributable fractions of T2DM, IHD, stroke, and hypertension.
Excluding the T2DM-attributable fractions of IHD and stroke.
Updated proportional to the projected expenditure on any diabetes with T2DM-attributable costs of IHD and stroke based on estimates by Begg et al. (10) and Voss et al. (25).
Updated proportional to the projected expenditure on cardiovascular disease treatment (25).
Did not require further adjustment for overlap, because factions of these estimates were excluded from estimates for obesity, T2DM, and hypertension.
Based on analysis of various databases and reports (see Supplemental Appendix).
Updated proportional to the projected prevalence of any cardiovascular disease (25).
Excluding hypertension-attributable fractions of IHD and stroke.
Based on estimates by Access Economics (26) and updated proportional to estimates of expenditure on any musculoskeletal disease (25).
No overlapping causal pathways.
Information on the prevalence of dairy product consumption within cases was available for only one health outcome: obesity. Consequently, the remaining base case estimates of PAR were obtained using Eq. 1a (Table 3). The base case analysis shows that increasing consumption of dairy foods by Australians could prevent 18.4% of incident obesity, 10.2% of incident T2DM, 5.0% of incident IHD, 16.2% of incident stroke, 8.3% of incident hypertension, and 6.2% of incident osteoporosis.
TABLE 3.
Direct healthcare expenditure and burden of disease attributable to low consumption of dairy products in Australia, 2010–20111
| Disease or risk factor | Costs of illness attributable to low consumption of dairy products |
||||||||||
|
Base case analysis |
Sensitivity analysis S1 |
Sensitivity analysis S2 |
|||||||||
|
$million |
DALY |
PAR (%) | $million | DALY | PAR (%) | $million | DALY | ||||
| PAR (%) | Sep2 | ∑3 | Sep2 | ∑3 | ∑3 | ∑3 | ∑3 | ∑3 | |||
| Obesity | 18.4 | 1468 | (1076) | 54,754 | (8365) | 10.1 | (588) | (4574) | 29.84 | (1741) | (13,536) |
| T2DM | 10.2 | 503 | (237) | 46,208 | (18,342) | 5.1 | (119) | (9233) | 13.05 | (304) | (23,465) |
| IHD | 5.0 | 122 | (122) | 13,638 | (13,638) | 2.5 | (61) | (6862) | 14.36 | (347) | (38,867) |
| Stroke | 16.2 | 238 | (238) | 21,873 | (21,873) | 8.2 | (120) | (11,015) | 26.46 | (388) | (35,641) |
| Hypertension | 8.3 | 173 | (112) | 17,148 | (10,794) | 4.3 | (58) | (5608) | 25.67 | (345) | (33,130) |
| Osteoporosis | 6.2 | 223 | (223) | 2000 | (2000) | 3.1 | (112) | (1006) | 19.98 | (716) | (6423) |
| Total | 2007 | 75,012 | 1059 | 38,299 | 3839 | 151,061 | |||||
Values are point estimates. DALY, disability-adjusted life year; IHD, ischemic heart disease; PAR, population attributable risk; Sep, separately; T2DM, type 2 diabetes mellitus.
Application of the PAR to the corresponding estimate of separate direct healthcare expenditure or burden of disease in Table 2.
Application of the PAR to the corresponding estimate of exclusive (summed) direct healthcare expenditure or burden of disease from Table 2 (i.e., adjusted for overlapping causal pathways).
Based on combination of data for Australian population and data reported in (39).
Based on data reported in (46).
Based on data reported in (47).
Based on data reported in (48).
Based on data reported in (49).
In a hypothetical “steady state” in which Australians’ dairy product consumption is at recommended levels and the prevalence of disease is reduced by the amount attributed to low consumption of dairy products, the annual savings would total AUD$2.0 billion (current value, USD$2.1 billion, €1.4 billion) in direct healthcare expenditures and an additional 75,012 DALY (Table 3). Applying a value of a statistical life year of AUD$125,000 [the median value reported by Access Economics (42)] to the DALY would put the value of the total annual costs of illness, excluding indirect costs, at AUD$11.4 billion (USD$11.7 billion, €8.9 billion).
Sensitivity analyses.
The analysis proved sensitive to variation in the assumptions that were used to relate levels of dairy product consumption in the source studies to levels in the Australian population. A multivariate S1 demonstrates that when conservative interpretations are applied to the evidence, the benefits of increasing Australians’ dairy product consumption would be an estimated 38,299 DALY and an estimated healthcare savings of AUD$1.1 billion (USD$1.1 billion, €831 million) annually (Table 3).
The calculation of PAR in study samples using Eq. 2 all returned higher estimates than the calculation of PAR for the Australian population that relied on using Eq. 1a. Applying these PAR to the Australian population would have produced estimates of 151,061 DALY and AUD$3.8 billion (USD$3.9 billion, €3.0 billion) attributable to low consumption of dairy foods in Australia (Table 3).
Discussion
The analysis presented here demonstrates substantial improvements in health and reductions in the cost of healthcare services that could be achieved by increasing Australians’ consumption of dairy foods to the recommended levels. The sensitivity analyses produced a relatively large variation in quantitative estimates of attributable burden of disease and healthcare expenditure; this variation arises from uncertainty associated with a number of assumptions. However, even the most conservative estimates suggest potentially large savings to health and healthcare. The higher PAR in the S2 may reflect differences in dairy product consumption (i.e., a lesser prevalence of low consumption of dairy products in Australia), differences in the prevalence of other risk factors for the respective disease (i.e., a higher background risk in Australians), or a greater effect upon risk in the individual study samples examined than in the meta-analyses used in the base case. However, this finding also supports our expectation that Eq. 1a (used in all base case analyses except obesity) would produce estimates that were conservatively biased.
Our treatment of exposure and risk as quasi-continuous (technically categorical but approximating a continuous relationship through the use of risk regression and fine categories of exposure) is a small but valuable addition to the epidemiological methods available to nutritionists and other researchers, with the potential to be developed further to incorporate nonlinear regressions of risk and Poisson regressions of prevalence.
Our analysis conforms well to a recently published checklist for critical evaluation of cost-of-illness studies by Larg and Moss (50). The main uncertainties relate to the observational nature of the research informing it and thus the possibility of residual confounding in estimates of RR. However, if dairy foods do improve maintenance of healthy body weight, then it is also likely that many studies are overadjusted by including BMI as a control variable (thus removing any effect that is mediated through improved weight control from the estimates). No randomized controlled trials were identified that had been designed to assess long-term health outcomes of increased total or whole-fat dairy product consumption in a general population sample. Most used calcium supplements or reduced-fat dairy foods in the intervention arm, sampled from obese populations or other subgroups, or lacked sufficient follow-up for investigation of chronic disease outcomes (51–54).
Another implication of reliance upon observational research is that it does not account for substitution effects that would result from increasing consumption of dairy products. Consumption of other foods would inevitably decrease and the overall effects on health could be either reduced or enhanced depending on which foods are substituted. For this reason, public health campaigns should not focus on single food groups but on improving overall diet.
Changes in Australians’ consumption of dairy products since the NNS would have implications for the validity of our findings, but from industry data and previous NNS, this appears unlikely to have been substantial (8). Compared with the patterns of other behaviors that interact with health such as smoking or consumption of alcohol, our understanding of dietary habits is relatively poor (8). Specific micronutrients can be measured in food or blood samples using standard units that allow for studies to be related to each other, or meta-analyzed, but we do not eat micronutrients; we eat food, and the specification and measurement of consumption in food groups remains fraught with subjectivity and inconsistency. This lack of precision in describing diet presents difficulties when researching the role of diet in health and may be responsible for much of the heterogeneity in published findings. Systematic reviews side-step the problems by remaining either narrative or qualitative (16) or by applying simplifying assumptions in high vs. low meta-analyses (17–19, 41).
We note also that the assumed linear relationship between dairy product consumption and health will apply across only part of the range. Just about any nutritious food is beneficial only up to a point, beyond which they begin to have harmful effects because of either overconsumption of a particular nutrient or displacement of others (55). This results in U-shaped associations between consumption and risk. The common practices in nutrition research of estimating changes in risk per unit increase in exposure [e.g., RR of osteoporosis per 300 mg increase in dietary calcium (38)] and of testing the significance of linear trends in risk across quintiles of exposure [e.g., Pereira et al. (39) or Steffen et al. (56)] rely on open-ended, monotonic, and linear associations between exposure and risk, which outside of some range will be unrealistic and thus should be interpreted with caution. At both the individual and population levels, most of the benefit is achieved at the recommended minimums of 2–3 servings, because the highest risks are associated with the lowest intakes.
The finding that the largest healthcare savings were associated with maintenance of a healthy body weight reflects several factors. This was where the greatest effects of dairy product consumption were seen (as measured by RR) and it also reflects the high current incidence of obesity. Although the RR was taken from a single study, it is consistent with a protective effect found in a systematic review of other studies (16), and this particular PAR was calculated using the more valid approach of Eq. 2, enhancing confidence in the estimate. Whereas many other studies have examined the various roles that dairy foods might play in weight management and the mechanisms through which it improves weight control, the CARDIA study was the only study identified that provided outcomes suitable for economic modeling. One study was recently published in which dairy product consumption during adolescence and young adulthood was found not to be related to weight status at age 36 y in a small Dutch cohort with high average consumption of dairy foods (mean ∼3 servings/d) (57). To some extent, this contrasts the findings from the CARDIA cohort, but it is also consistent with risk effects being associated only with low levels of dairy product consumption. Given the potential importance of this relationship and the very considerable societal burden imposed by overweight and obesity, further research into this association is paramount.
The effect seen with osteoporosis was also unexpectedly small, but we note that the only evidence suitable for economic modeling was relatively old and based largely on case-control studies (38). The role of dairy product consumption in risk of fracture is an area in which research is warranted.
Recurrent direct health expenditure in Australia is estimated at $116 billion for the 2009–2010 financial year (29). Our analysis indicates that 0.9–3.3% of this could have been saved if Australians had consumed the recommended quantities of dairy foods in recent decades. Even more powerfully, these savings are comparable with the entire budget for public health interventions [$2.0 billion in 2009–2010 (29)]. Our findings are notably smaller than were reported by McCarron and Heaney (58) for the US. This likely reflects substantial differences in methodology and underlying assumptions.
Public health interventions to target dietary improvement could include taxation policies (e.g., subsidization of desirable foods, taxation of unhealthy foods), regulation around food composition (e.g., to limit the level of sugar or warnings about high sugar content), restrictions on advertising or tax penalty on advertising high-energy, nutrient-poor foods, transport subsidies for nutritious foods, support for healthy food store policies, etc. It is important that interventions are selected based on evidence of effectiveness and cost-effectiveness and are implemented subject to rigorous evaluation. The estimates of potential savings reported in this study can only be realized if interventions do increase dairy product consumption and increasing dairy product consumption does have the effects predicted by observational studies.
One potential limitation to the effectiveness of increasing dairy product consumption is lactose intolerance, which is of particular relevance to Australian Aboriginal and Torres Strait Islander populations and other groups with limited evolutionary exposure to dairy foods. However, there is a broad spectrum of lactose intolerance and most of those affected are able to consume moderate quantities of certain dairy foods, particularly yogurt and cheese, which are naturally low in lactose, and other products that have had their lactose removed (59, 60).
The analysis does not suggest that the entire population could consume the recommended servings of dairy foods, or that this could be achieved without cost; it simply provides an estimate of the health-related cost of current underconsumption of dairy products. Non-health effects of changing the population’s diet have not been considered. These could include both beneficial effects (e.g., increased economic production from a healthier workforce) and detrimental effects (e.g., an increased demand for environmental resources), so the net benefits from a societal perspective are unclear. However, the analysis does demonstrate the potential improvements to health and healthcare savings of investing in effective strategies to improve the quality of the Australian diet through increased consumption of dairy products.
Sixty-five percent of Australians consume less than the recommended servings of dairy (8), which means that public health interventions to increase dairy product consumption could be broadly targeted and even small changes in average consumption may yield relatively large benefits for the community. Our findings provide a case for allocating research funds to identify effective means of promoting a healthy diet, and consideration of dairy foods as a vector for achieving this outcome. Once evidence on the effectiveness of interventions has been established it will then be possible to evaluate their cost-effectiveness and net benefit in order to inform investment decisions.
Supplementary Material
Acknowledgments
J.D., L.S., E.G., Kim Dalziel, and Rachelle Opie (both of Health Economics and Social Policy Group, University of South Australia) designed research; J.D., L.S., K.D., and R.O. conducted research; J.D. analyzed data; J.D., L.S., and E.G. wrote the paper; and J.D. had primary responsibility for final content. All authors read and approved the final manuscript.
Footnotes
Supported by Dairy Australia.
Supplemental Appendix A is available from the “Online Supporting Material” link in the online posting of the article and from the same link in the online table of contents at http://jn.nutrition.org.
Abbreviations used: CARDIA, Coronary Artery Risk Development in Young Adults; CRA, Comparative Risk Assessment project; CRCa, colorectal cancer; DALY, disability-adjusted life year; FBDG, food-based dietary guideline; FSG, food selection guide; IHD, ischemic heart disease; NNS, 1995 Australian National Nutrition Survey; PAR, population attributable risk; PrCa, prostate cancer; T2DM, type 2 diabetes mellitus.
A standard serving was defined as 250 mL milk, 200 g yogurt, or 40 g cheese.
For an explanation of the National Health and Medical Research Council of evidence, see (21).
Literature Cited
- 1. Health Canada. Eating well with Canadaaposs food guide. Ottawa: Health Canada; 2007.
- 2.Kellet E, Smith A, Schmerlaib Y. The Australian guide to health eating. Canberra: Australian Government Department of Health and Ageing; 1998.
- 3.National Health and Medical Research Council. Food for health: dietary guidelines for Australians: a guide to healthy eating. Canberra: Australian Government Department of Health and Ageing; 2005.
- 4. USDA, U.S. Department of Health and Human Services. Dietary guidelines for Americans, 2010. 7th ed. Washington, DC: U.S. Government Printing Office; 2010. [DOI] [PMC free article] [PubMed]
- 5. UK Food Standards Agency. Nutrition publications; 2010 [cited 2011 Apr 27]. Available from: http://food.gov.uk/aboutus/publications/nutritionpublications/
- 6.Smith A, Kellet E, Schmerlaib Y. The Australian guide to health eating: background information for nutrition educators. Canberra: Australian Government Department of Health and Ageing; 1998.
- 7.Australian Bureau of Statistics. National health survey: summary of results, 2004–2005. Canberra: Australian Government; 2006.
- 8.Doidge JC, Segal L. Most Australians do not meet recommendations for dairy consumption: findings of a new technique to analyse nutrition surveys. Aust N Z J Public Health. 2012;36:236–40 [DOI] [PubMed] [Google Scholar]
- 9.McLennan W, Podger A. National Nutrition Survey (1995): nutrient intakes and physical measurements. Canberra: Australian Bureau of Statistics; 1998.
- 10.Begg S, Voss T, Barker B, Stevenson C, Stanley L, Lopez A. The burden of disease and injury in Australia, 2003. Canberra: Australian Institute of Health and Welfare; 2007 [Google Scholar]
- 11.Lester I. Australia's food and nutrition. Canberra: Australian Institute of Health and Welfare; 1994 [Google Scholar]
- 12.Australian Institute of Health and Welfare Public health expenditure in Australia, 2008–09. Canberra: Australian Institute of Health and Welfare; 2011 [Google Scholar]
- 13.Porta MS, Greenland S, Last J, International Epidemiological Association A dictionary of epidemiology. 5th ed. Oxford: Oxford University Press; 2008 [Google Scholar]
- 14.Haug A, Hostmark AT, Harstad OM. Bovine milk in human nutrition: a review. Lipids Health Dis. 2007;6:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes: a systematic review and meta-analysis. J Clin Endocr Metab. 2007;92:2017–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dougkas A, Reynolds CK, Givens ID, Elwood PC, Minihane AM. Associations between dairy consumption and body weight: a review of the evidence and underlying mechanisms. Nutr Res Rev. 2011;15:1–24 [DOI] [PubMed] [Google Scholar]
- 17.Elwood PC, Pickering J, Givens D, Gallacher J. The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: an overview of the evidence. Lipids. 2010;45:925–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huncharek M, Muscat J, Kupelnick B. Colorectal cancer risk and dietary intake of calcium, vitamin D, and dairy products: a meta-analysis of 26,335 cases from 60 observational studies. Nutr Cancer. 2009;61:47–69 [DOI] [PubMed] [Google Scholar]
- 19.Ralston RA, Lee JH, Truby H, Palermo CE, Walker KZ. A systematic review and meta-analysis of elevated blood pressure and consumption of dairy foods. J Hum Hypertens. 2012;26:3–13. [DOI] [PubMed] [Google Scholar]
- 20.Bonthuis M, Hughes MCB, Ibiebele TI, Green AC, van der Pols JC. Dairy consumption and patterns of mortality of Australian adults. Eur J Clin Nutr. 2010;64:569–77 [DOI] [PubMed] [Google Scholar]
- 21.National Health and Medical Research Council NHMRC levels of evidence and grades for recommendations for developers of guidelines. Canberra: National Health and Medical Research Council; 2009 [Google Scholar]
- 22.National Health and Medical Research Council A review of the evidence to address targeted questions to inform the revision of the Australian Dietary Guidelines. Canberra: National Health and Medical Research Council; 2012 [Google Scholar]
- 23.Gefeller O. Comparison of adjusted attributable risk estimators. Stat Med. 1992;11:2083–91 [DOI] [PubMed] [Google Scholar]
- 24.Phillips B, Ball C, Sackett D, Badenoch D, Straus S, Haynes B, Dawes M. Levels of evidence. In: J Howick, editor. Oxford: University of Oxford Oxford Centre for Evidence-based Medicine Levels of Evidence; 2009.
- 25.Voss T, Goss J, Begg S, Mann N. Australian Burden on Disease and Injury Study: projected health care costs report. Brisbane: School of Population Health, University of Queensland and the Australian Institute of Health and Welfare; 2005 [Google Scholar]
- 26.Access Economics Pty Ltd The burden of brittle bones: costing osteoporosis in Australia. Sydney: Osteoporosis Australia; 2001 [Google Scholar]
- 27.Access Economics Pty Ltd The economic costs of obesity. Canberra: Diabetes Australia; 2006 [Google Scholar]
- 28.Access Economics Pty Ltd The growing cost of obesity in 2008: three years on. Canberra: Diabetes Australia; 2008 [Google Scholar]
- 29.Australian Institute of Health and Welfare Health expenditure Australia, 2009–10. Canberra: Australian Institute of Health and Welfare; 2011 [Google Scholar]
- 30.Australian Bureau of Statistics National Nutrition Survey 1995. Basic CURF, CD-ROM ed. Canberra: Australian Bureau of Statistics; 1995 [Google Scholar]
- 31.Dairy Australia. Dairy industry statistics: consumption summary. Melbourne: Dairy Australia; 1985#x20132011.
- 32.Coblac L, Bowen J, Burnett J, Syrette J, Dempsey J, Balle S, Wilson C, Flight I, Good N, Saunders I, et al. 2007 Australian National Children's Nutrition and Physical Activity Survey: main findings. Canberra: Australian Bureau of Statistics; 2008.
- 33. Roy Morgan Research. [Dairy] Usage and Attitude Study 2007. Melbourne: Dairy Australia; 2007.
- 34. Womenaposs Health Australia. The Australian Longitudinal Study on Womenaposs Health; 2011 [cited 2011 May 1]. Available from: http://www.alswh.org.au/surveys.html.
- 35.Murray C, Ezzati M, Lopez A, Rodgers A, Vander Hoorn S. Conceptual framework and methodological issues. In: Ezzati M, Lopez A, Rodges A, Murray C, editors. Comparative quantification of health risks. Geneva: WHO; 2004. [DOI] [PMC free article] [PubMed]
- 36.Williamson DF. The population attributable fraction and confounding: buyer beware. Int J Clin Pract. 2010;64:1019–23 [DOI] [PubMed] [Google Scholar]
- 37.Rockhill B, Newman B, Weinberg C. Use and misuse of the population attributable fraction. Am J Public Health. 1998;88:15–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cumming RG, Nevitt MC. Calcium for prevention of osteoporotic fractures in postmenopausal women. J Bone Miner Res. 1997;12:1321–9 [DOI] [PubMed] [Google Scholar]
- 39.Pereira MA, Jacobs DR, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults. JAMA. 2002;287:2081–9 [DOI] [PubMed] [Google Scholar]
- 40.van der Pols JC, Bain C, Gunnell D, Smith GD, Frobisher C, Martin RM. Childhood dairy intake and adult cancer risk: 65-y follow-up of the Boyd Orr cohort. Am J Clin Nutr. 2007;86:1722–9 [DOI] [PubMed] [Google Scholar]
- 41.Huncharek M, Muscat J, Kupelnick B. Dairy products, dietary calcium and vitamin D intake as risk factors for prostate cancer: a meta-analysis of 26,769 cases from 45 observational studies. Nutr Cancer. 2008;60:421–41 [DOI] [PubMed] [Google Scholar]
- 42.Access Economics Pty Ltd The health of nations: the value of a statistical life. Canberra: Office of the Australian Safety and Compensation Council; 2008 [Google Scholar]
- 43.Colagiuri S, Lee CM, Colagiuri R, Magliano D, Shaw JE, Zimmet PZ, Caterson ID. The cost of overweight and obesity in Australia. Med J Aust. 2010;192:260–4 [DOI] [PubMed] [Google Scholar]
- 44.Australian Institute of Health and Welfare Health system expenditures on disease and injury in Australia, 2000–01. 2nd ed. Canberra: Australian Institute of Health and Welfare; 2005 [Google Scholar]
- 45.Australian Institute of Health and Welfare Health care expenditure on cardiovascular diseases, 2004–05. Canberra: Australian Institute of Health and Welfare; 2008 [Google Scholar]
- 46.Choi HK, Willett WC, Stampfer MJ, Rimm E, Hu FB. Dairy Consumption and risk of type 2 diabetes mellitus in men: a prospective study. Arch Intern Med. 2005;165:997–1003 [DOI] [PubMed] [Google Scholar]
- 47.van der Pols JC, Gunnell D, Williams GM, Holly JMP, Bain C, Martin RM. Childhood dairy and calcium intake and cardiovascular mortality in adulthood: 65-year follow-up of the Boyd Orr cohort. Heart. 2009;95:1600–6 [DOI] [PubMed] [Google Scholar]
- 48.Alonso A, Beunza JJ, Delgado-Rodríguez M, Martínez JA, Martínez-González MA. Low-fat dairy consumption and reduced risk of hypertension: the Seguimiento Universidad de Navarra (SUN) cohort. Am J Clin Nutr. 2005;82:972–9 [DOI] [PubMed] [Google Scholar]
- 49.Jaglal SB, Kreiger N, Darlington G. Past and recent physical activity and risk of hip fracture. Am J Epidemiol. 1993;138:107–18 [DOI] [PubMed] [Google Scholar]
- 50.Larg A, Moss JR. Cost-of-illness studies: a guide to critical evaluation. Pharmacoeconomics. 2011;29:653–71. [DOI] [PubMed] [Google Scholar]
- 51.Caan B, Neuhouser M, Aragaki A, Lewis CB, Jackson R, LeBoff MS, Margolis KL, Powell L, Uwaifo G, Whitlock E, et al. Calcium plus vitamin D supplementation and the risk of postmenopausal weight gain. Arch Intern Med. 2007;167:893–902 [DOI] [PubMed] [Google Scholar]
- 52.Cheng S, Lyytikäinen A, Kröger H, Lamberg-Allardt C, Alén M, Koistinen A, Wang QJ, Suuriniemi M, Suominen H, Mahonen A, et al. Effects of calcium, dairy product, and vitamin D supplementation on bone mass accrual and body composition in 10–12-y-old girls: a 2-y randomized trial. Am J Clin Nutr. 2005;82:1115–26 [DOI] [PubMed] [Google Scholar]
- 53.Summerbell CD, Watts C, Higgins JPT, Garrow JS. Randomised controlled trial of novel, simple, and well supervised weight reducing diets in outpatients. BMJ. 1998;317:1487–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zemel MB, Richards J, Mathis S, Milstead A, Gebhardt L, Silva E. Dairy augmentation of total and central fat loss in obese subjects. Int J Obes (Lond). 2005;29:391–7 [DOI] [PubMed] [Google Scholar]
- 55.Rosenbloom M. Vitamin toxicity. In: Tarabar A, Lavely R, VanDeVoort J, Harchelroad F, Halamka J, editors. Medscape Reference. New York: WebMD; 2011 [cited 2011 May 1]. Available from http://emedicine.medscape.com/article/819426/ [Google Scholar]
- 56.Steffen LM, Kroenke CH, Yu X, Pereira MA, Slattery ML, Van Horn L, Gross MD, Jacobs DR. Associations of plant food, dairy product, and meat intakes with 15-y incidence of elevated blood pressure in young black and white adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Clin Nutr. 2005;82:1169–77 [DOI] [PubMed] [Google Scholar]
- 57.te Velde SJ, Snijder MB, van Dijk AE, Brug J, Koppes LL, van Mechelen W, Twisk JWR. Dairy intake from adolescence into adulthood is not associated with being overweight and metabolic syndrome in adulthood: the Amsterdam Growth and Health Longitudinal Study. J Hum Nutr Diet. 2011;24:233–44 [DOI] [PubMed] [Google Scholar]
- 58.McCarron DA, Heaney RP. Estimated healthcare savings associated with adequate dairy food intake. Am J Hypertens. 2004;17:88–97 [DOI] [PubMed] [Google Scholar]
- 59.Suarez FL, Savaiano D, Arbisi P, Levitt M. Tolerance to the daily ingestion of two cups of milk by individuals claiming lactose intolerance. Am J Clin Nutr. 1997;65:1502–6 [DOI] [PubMed] [Google Scholar]
- 60.Savaiano DA, Boushey CJ, McCabe GP. Lactose intolerance symptoms assessed by meta-analysis: a grain of truth that leads to exaggeration. J Nutr. 2006;136:1107–13 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.