Abstract
Objective:
Transpedicular screws are commonly and successfully used for posterior fixation in spinal instability, but their insertion remains challenging. Even using navigation techniques, there is a misplacement rate of up to 11%. The aim of this study was to assess the accuracy of a novel pedicle screw system.
Methods:
Thoracic and lumbar fusions were performed on 67 consecutive patients for tumor, trauma, degenerative disease or infection. A total of 326 pedicular screws were placed using a novel wire-guided, cannulated, polyaxial screw system (XIA Precision®, Stryker). The accuracy of placement was assessed postoperatively by CT scan, and the patients were followed-up clinically for a mean of 16 months.
Results:
The total medio-caudal pedicle wall perforation rate was 9.2% (30/326). In 19 of these 30 cases a cortical breakthrough of less than 2 mm occurred. The misplacement rate (defined as a perforation of 2 mm or more) was 3.37% (11/326). Three of these 11 screws needed surgical revision due to neurological symptoms or CSF leakage. There have been no screw breakages or dislocations over the follow up-period.
Conclusion:
We conclude that the use of this cannulated screw system for the placement of pedicle screws in the thoracic and lumbar spine is accurate and safe. The advantages of this technique include easy handling without a time-consuming set up. Considering the incidence of long-term screw breakage, further investigation with a longer follow-up period is necessary.
Keywords: spinal instrumentation, pedicle screws, misplacement, pedicle wall perforation
Introduction
Transpedicular screw application is commonly used and has been very successful for posterior fixation in spinal instability due to trauma, tumor, scoliosis, and degenerative disease (Schwarzenbach et al 1997; Merloz et al 1998; Amiot et al 2000; Hart et al 2005). It can be used even when the posterior elements of the spine are absent or injured (Coe et al 1990; Dvorak et al 1993; Liljenqvist et al 1997). The insertion of pedicle screws remains challenging, because of the variability in width, height, and orientation of spinal pedicles and the proximity of nerve roots. This is even more so the case in the thoracic spine, due to the small pedicular diameter and the proximity of the pleura and the spinal cord (Schwarzenbach et al 1997; Merloz et al 1998; Youkilis et al 2001; Hart et al 2005). In the thoracic spine, the diameters of the pedicles are sometimes too small for standard pedicle screws. Therefore, a lateral exit of the pedicle is recommended in some cases and results in safe screw placement in most cases (Hart et al 2005). Neurological lesions and instability may be complications that result from misplacement of pedicular screws. In a study of 4790 screws with 143 malpositioned screws, only 11 screws (7.7%) caused radicular pain or weakness (Girardi et al 1999).
Despite the risks of pedicle screw instrumentation, it does offer several advantages compared to a hook-based instrumentation. The fixation is biomechanically stronger, enables better correction of spinal deformity, has a reduced chance for the loss of fixation, and enables the inclusion of less segments in the fusion so risks of nonunion can be reduced (Roy-Camille et al 1986; Suk et al 1994; Liljenqvist et al 1997; Hart et al 2005). The use of intraoperative fluoroscopy combined with pedicular palpation is the most common of a variety of insertion techniques (Grützner et al 2004). Misplacement of transpedicular screws with this conventional technique is reported to be 21% to 40% (Weinstein et al 1988; Gertzbein and Robbins 1990; Laine et al 2000). Despite the use of navigation techniques when inserting transpedicular screws, there remains a malpositioning rate of up to 11% (Amiot et al 2000; Laine et al 2000; Youkilis et al 2001; Schnake et al 2004). Even placement with intraoperative CT scan showed a malpositioning rate of 6.3% (Ebmeier et al 2003). Moreover, the time taken for screw insertion is significantly longer using computer assisted screw placement (Laine et al 2000), and the use of CT-based navigation has a limited ability to adapt to intraoperative changes of position and anatomy (Gebhard et al 2000).
The aim of this study was to assess the accuracy of pedicular screw placement using a novel wire-guided, cannulated, polyaxial screw system in an otherwise conventional approach.
Patients and Methods
Sixty-seven consecutive thoracic and lumbar fusions were performed between May 2005 and September 2006. The procedures performed were: simple dorsal fusion, fusion with decompression of the spinal canal, and fusion with either debridement or tumor resection. The patient series included 47 women and 20 men, all with indications for instrumentation. The mean age of the patients was 67 (range 42–89). The types of operations are shown in Table 1. The underlying diseases were tumor, trauma, degenerative disease, and infection (Table 2). Three hundred-twenty-six cannulated pedicle screws (246 lumbar, 80 thoracic) were placed under fluorsoscopic guidance. The pedicle screws were inserted into the spinal segments Th4–S1 (Table 3). Intraoperative neurophysiological monitoring, navigation or other types of guidance tools were not used in this study.
Table 1.
Types of operations performed and duration of surgery (minutes)
| PLIF | Fusion only | Fusion + laminectomy | Fusion + Debridement/tumor resection | Dorsoventral fusion | Total | |
|---|---|---|---|---|---|---|
| No of patients | 24 | 14 | 13 | 9 | 7 | 67 |
| Mean time of surgery (range) | 205 (126–307) | 151 (58–350) | 135 (60–182) | 163 (70–260) | 336 (232–454) | 187 (58–454) |
Abbreviation: PLIF, posterior lumbar interbody fusion.
Table 2.
Underlying types of diseases
| No of patients | |
|---|---|
| Degenerative disease | 27 |
| Trauma | 22 |
| Tumor | 11 |
| Infection | 7 |
| Total | 67 |
Table 3.
Location and extent of medio-caudal pedicle wall (mcpw) perforations
| Total | Grade A (no perforation) | Grade B (perforation <2 mm) | Grade C (perforation 2–4 mm) | Grade D (perforation >4 mm) | |
|---|---|---|---|---|---|
| Th4 | 2 | 2 | |||
| Th5 | 4 | 2 | 2 | ||
| Th6 | 6 | 6 | |||
| Th7 | 6 | 6 | |||
| Th8 | 4 | 4 | |||
| Th9 | 4 | 4 | |||
| Th10 | 8 | 8 | |||
| Th11 | 16 | 14 | 1 | 1 | |
| Th12 | 30 | 28 | 1 | 1 | |
| L1 | 18 | 18 | |||
| L2 | 36 | 32 | 3 | 1 | |
| L3 | 51 | 47 | 3 | 1 | |
| L4 | 73 | 68 | 5 | 3 | |
| L5 | 58 | 51 | 3 | 2 | 2 |
| S1 | 10 | 9 | 1 | ||
| 326 | 296 (90.8%) | 19 (5.83%) | 6 (1.84%) | 5 (1.53%) | |
| mcpw perforation rate | (Grade B+C+D) | 30/326 (9.2%) | |||
| Misplacementa rate | (Grade C+D) | 11/326 (3.37%) |
Misplacement (= medio-caudal pedicle wall [mcpw] perforation >2 mm), as defined by the majority of the current literature.
Preoperatively, CT scans and plain radiograms were obtained from all patients, and an MRI was performed in selected cases.
In the operations, we used a novel wire-guided, cannulated, polyaxial, screw system (XIA Precision®, Stryker, USA), which has titanium alloy pedicular screws with a diameter of 5.5, 6.5 and 7.5 mm and a length of 30 to 55 mm. In all cases a standard midline approach was used. After preparation of the facet joints, a 2- to 3-mm K-wire was inserted under fluorscopic guidance into the pedicle. In the thoracic spine a more lateral approach was used when the surgeon was confronted with a rather narrow pedicle diameter. After palpation of the entry site, the K-wire was replaced with a 1.2-mm diameter guidance wire. In order to avoid the risk of ventral dislocation within the abdominal cavity, the guidance wire was introduced with the blunt tip going downwards into the pedicle. Then the cannulated awl and slap-guide were guided along the same trajectory of the wire, in order to widen the bony entrance of the pedicle. If the bone was of hard consistency, the cannulated tap was used to prepare the pedicle-screw-canal. After preparation of the pedicle and depth measurement, the cannulated screw was then placed over the guidance wire through the pedicle into the vertebral body (Figures 1 and 2).
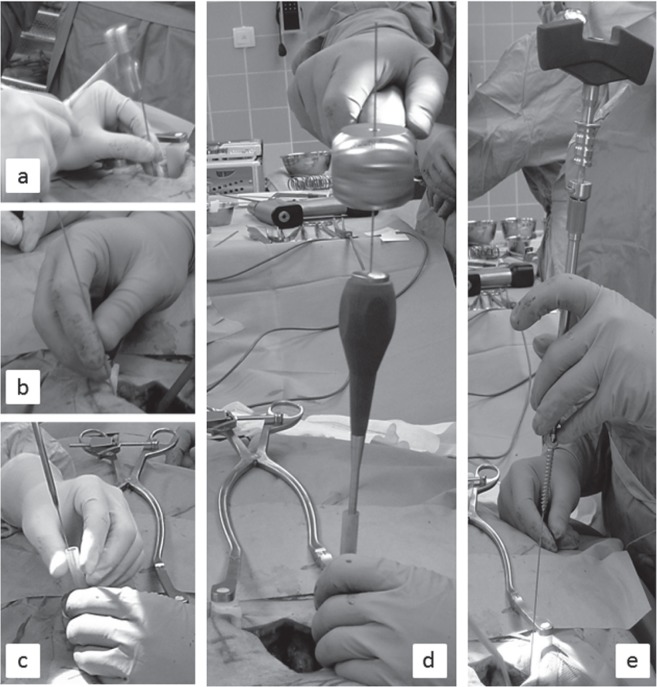
Figure 1.
Photographs of the operation procedure for inserting transpedicular screws with the novel cannulated polyaxial screw system. a) Insertion of the K-wire. b) The K-wire has been replaced by the guidance wire. Widening of the pedicle entrance with c) the cannulated awl and d) slap. e) Bringing in the pedicle screw over the guidance wire.
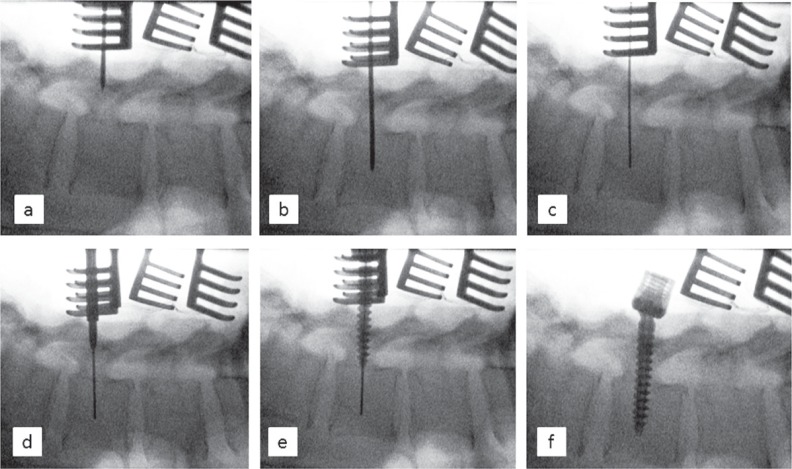
Figure 2.
Radiographic images of the process of inserting the transpedicular screw with the cannulated polyaxial screw system into spinal vertebra L4. a/b) Advancing the K-wire. c) The K-wire has been replaced by the guidance wire. d) Widening of the pedicle entrance with the cannulated awl. e) Insertion of the pedicle screw over the guidance wire. f) Final position of the pedicle screw.
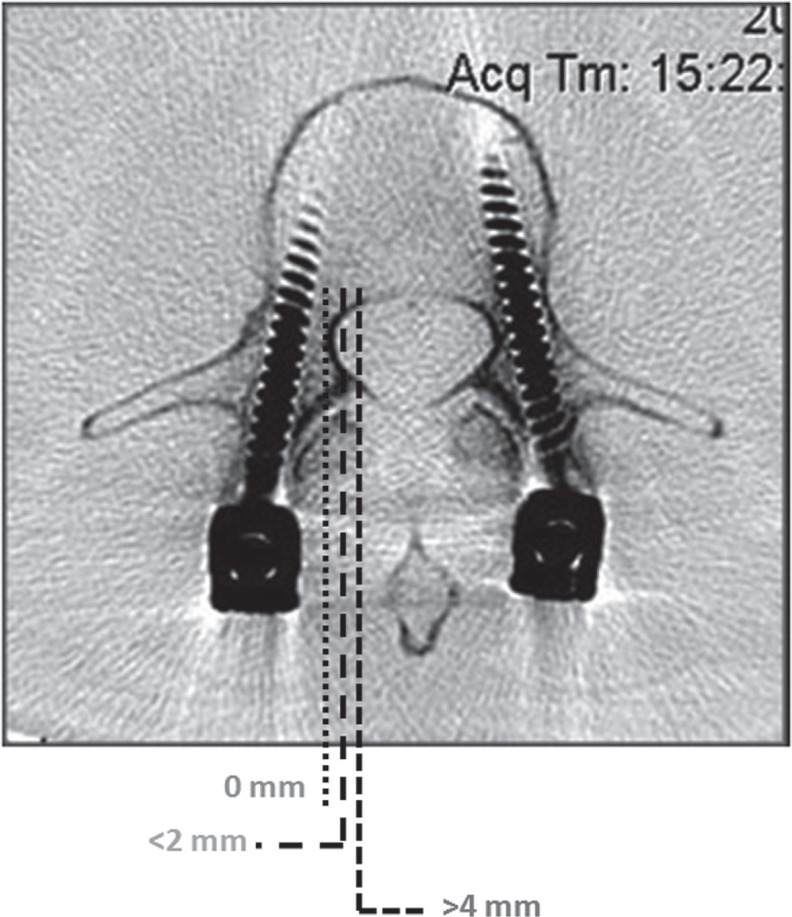
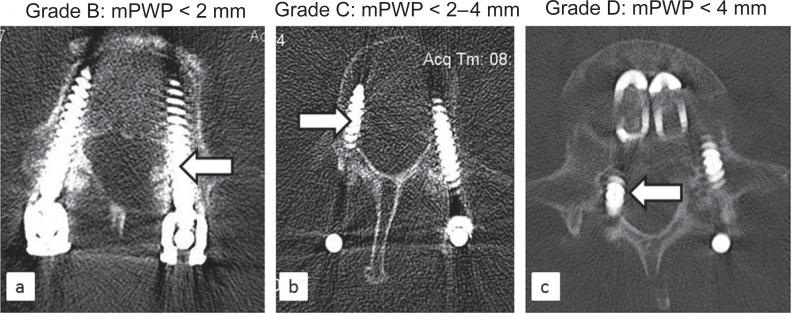
Postoperative verification of the screw position was obtained by CT scan (1 mm axial slices, frontal and sagittal reconstructions). The position of the screw was graded as: A) screw correctly inside the pedicle or lateral entry point with medio-caudal pedicle wall (mcpw) completely intact, B) cortical breakthrough and/or perforation of the mcpw by up to 2 mm, C) perforation of the mcpw by 2 to 4 mm, or D) perforation by more than 4 mm (Figures 3 and 4). As in previous studies, “misplacement” was defined as a pedicular wall perforation of 2 mm or more (grades C and D above) (Grützner et al 2004). The mean follow-up period was 16 months (range: 13–18). The patients were evaluated before and after surgery in terms of pain level and neurological symptoms, and perioperative and postoperative complications were registered.
Figure 3.
Radiographic image of correctly positioned pedicle screws (Grade A; no penetration). The dotted lines show the measurement ranges for pedicle wall perforation (<2 mm: Grade B) and malplacement (2–4 mm: Grade C and >4 mm: Grade D).
Figure 4.
Radiographic images of three grades of medial pedicular wall perforation (mPWP) and screw malposition. a) Grade B: perforation of the medial pedicle wall by up to 2 mm, b) Grade C: perforation of the medial pedicle wall by 2–4 mm, and c) Grade D: perforation by more than 4 mm.
Results
The cannulated screw system was used in 24/67 (35.8%) cases for posterior lumbar interbody fusion (PLIF), in 14/67 (20.9%) for dorsal stabilization, in 13/67 (19.4%) for fusion with laminectomy, in 9/67 (13.4%) for fusion with debridement and/or tumor resection, and in 7/67 cases (10.4%) for dorsoventral fusion (Table 1). The underlying diseases were degenerative in 27/67 cases (40.3%), trauma in 22/67 (32.8%), tumor in 11/67 (16.4%), and spondylithis/spondylodiscitis in 7/67 (10.5%) (Table 2). The mean operating time was 187 minutes (range: 58–454 min) (Table 1).
The extent and location of mcpw perforations are shown in Table 3. From the 326 pedicle screws, there were 19 (5.83%) screws that damaged the mcpw during insertion or perforated the pedicle up to 2 mm (Grade B), 6 (1.84%) that perforated 2 to 4 mm (Grade C), and 5 (1.53%) that perforated over 4 mm (Grade D), for a total mcpw perforation rate of 30/326 (9.2%). According to the definition of “misplacement” (= mcpw perforation >2 mm, Grade C+D), 11/326 screws (3.37%) were misplaced.
There were seven major perioperative or postoperative complications. Three of the complications described were directly associated with the screw insertion. Two of these patients presented with radicular pain correlating to the screw position. One patient with a lumbar L3 fracture presented with a delayed CSF leak to the subcutaneous tissue, two weeks after surgery, probably due to a dural tear from a misplaced screw. This patient simultaneously presented with Guillain-Barré Syndrome affecting the upper and lower limbs, followed by a colitis. Because of that, revision with correction of the screw position and dural closure had to be delayed for 6 weeks after surgery. The remaining complications can be considered as general surgical complications. One patient died in the postoperative period, due to pulmonary embolism on the 6th post-op day. One patient with L1–L5 fusion had to be treated for postoperative pneumothorax. One patient with previously known renal insufficiency suffered from pulmonary edema. One patient presented post-operatively with a bilateral mild paresis for L5 due to epidural hematoma at the L4/5 level. The paresis resolved completely with conservative treatment alone. There were the following minor complications: delayed wound healing in four cases, urinary infection in two cases, diarrhea due to Clostridium difficile in one case, transitory rectal bleeding and colitis in one case. None of the instrumentations has had to be removed, and no pedicular bursts, no dislocations, and no screw breakages have been observed during the follow-up period.
Discussion
The insertion of pedicle screws is a challenging procedure due to the variability in width, height, and orientation of spinal pedicles and the proximity of nerve roots. It is therefore mandatory to aim for a very high accuracy in placing pedicle screws.
Clinical studies on conventional pedicle screw placement with postoperative CT assessment have reported a malpositioning rate of up to 42%: Laine et al demonstrated a rate of 21.1% for pedicle perforation in patients with lower lumbar fusions (Laine et al 2000). In a study on lumbar fusions, Castro et al reported a perforation rate of 39.8% (Castro et al 1996). Gertzbein and Robbins reported a rate of 28.7% (Gertzbein and Robbins 1990). Schnake et al reported a perforation rate of 31.9% in thoracic spine instrumentations without the use of navigation (Schnake et al 2004). Merloz et al reported a perforation rate of 42% in thoracic and lumbar instrumentations (Merloz et al 1998).
In another study evaluating pedicle screw placement in the deformed spine, only 15 out of 789 pedicle screws placed using intraoperative plain radiography showed medial wall violation in the postoperative CT scan. Thirteen of 15 pedicle screws with medial wall violation had radiographical evidence of malpositioning. The authors therefore concluded that evaluation with intraoperative plain radiographs is highly accurate (Kim et al 2005). Previous studies (Schwarzenbach et al 1997; Merloz et al 1998; Amiot et al 2000; Laine et al 2000; Youkilis et al 2001; Schnake et al 2004) have shown that the use of computer-assisted navigation techniques significantly reduces the rate of pedicle perforation and screw malpositioning, compared to conventional screw placement.
Clinical studies using navigation techniques have shown a decrease in malpositioning rates with current rates of 2.7% to 17.5%. Schwarzenbach et al reported a pedicle perforation rate of 2.7% in lumbar instrumentation (Schwarzenbach et al 1997). Amiot et al showed a pedicle perforation rate of 5% (Amiot et al 2000). Schnake et al reported a perforation rate of 17.5% in thoracic spine instrumentations with the use of navigation, compared to 31.9% in the conventional group (Schnake et al 2004). Merloz et al reported a perforation rate of 8% in thoracic and lumbar instrumentations (Merloz et al 1998). Computer-assisted navigation in previously fused lumbar spines has been found to have a malpositioning rate of 4% in a retrospective clinical analysis (Lim et al 2005) and 0% in a cadaver model (Austin et al 2002).
Despite the introduction of computer-assisted navigation techniques for pedicle screw placement and the decrease of perforation rates, the routine use of these systems is not widely accepted. The use of computer-assisted navigation is only safe in the hands of surgeons, who are able to detect system malfunctioning or a systemic error in the planning process. It should be limited to carefully chosen indications. This is partly due to the technical limits of computer-assisted navigation. The time taken for screw insertion is significantly longer with the use of computer-assisted navigation (Girardi et al 1999; Gebhard et al 2000; Laine et al 2000). Most of the systems use an optical system with a camera-based tracking system, which might limit the surgeon in his or her operating field (Gebhard et al 2000). For the purpose of intraoperative point-matching, it is sometimes necessary to perform a larger and therefore more invasive surgical approach (Gebhard et al 2000). Frequently, the navigation determines the starting point and the trajectory. But no guidance is used when the actual pedicle screw is inserted, and this may lead to toggle during manual screw insertion and penetration of the pedicle cortex (Lim et al 2005). Additionally, it has been reported that the use of a CT-based navigation requires higher radiation doses than intraoperative fluoroscopy guidance (Slomczykowski et al 1999; Schaeren et al 2002).
In the here presented study, there was an mcpw perforation rate of 9.2% (30 of 326). Postoperative verification of the screw position was obtained by CT scan in this study. Axial 1 mm scans, as well as frontal and sagittal reconstructions were used equally for the misplacement measurements. It has been shown that CT scans improve accuracy in comparison to plain radiographs (Farber et al 1995; Odgers et al 1996; Berlemann et al 1997). Anatomic dissection studies have shown that postoperative CT scan evaluation provides accurate assessment of titanium screw positioning (Hart et al 2005). Interestingly, the mcpw perforation rate was higher in the lumbar group than in the thoracic group (24/246 = 9.8% vs 6/80 = 7.5%). Misplacement (perforation >2 mm) occurred in 3.37% of all cases (lumbar 9/246 = 3.7%, thoracic 2/80 = 2.5%). This may be caused by several factors: a) The middle and lower lumbar spine has been operated on with a higher frequency in this study (182/326 = 55.8% were placed in L3, L4 or L5). b) There were case specific factors such as traumatic and tumor lesions especially in the lower lumbar spine cases which increased this frequency. c) The screws used within the thoracic spine in general had a smaller diameter (5.5 mm) than in the lumbar spine (6.5 mm), and d) a more lateral approach was used in most of the thoracic spine cases when the surgeon was confronted with a rather narrow pedicle diameter. Complications which led to surgical revision occurred in only 3 cases with misplaced screws >4 mm (group D). Two patients presented with radicular pain corresponding to the misplaced screw and another patient developed CSF leakage from a dural tear close to the misplaced screw. However, the majority of group D screws, as well as all group C and B screws remained asymptomatic. Therefore, misplacement and complication rates of this cannulated screw series were within the range of navigation studies. The described technique therefore seems to be feasible, for there are only a few possible pitfalls.
No deficiency or pedicle screw breakage has been observed so far, indicating stability of the cannulated system. Previous studies have reported a frequency of pedicle screw breakage of 3% to 7% (Dickmann et al 1992; Niu et al 1996). The risk for pedicular burst has been described in previous studies to be elevated when the screw diameter exceeds 80% of the pedicle diameter (Misenhimer et al 1989; Sjostrom et al 1993). No pedicular burst has been observed in our study although the screw/pedicle diameter ratio exceeded 80% in 30% of the implanted screws.
Conclusion
We conclude that the use of this cannulated screw system for the placement of pedicle screws in the thoracic and lumbar spine is accurate and safe. The advantages of this technique include easy handling without a time-consuming setup. Considering the incidence of screw breakage with earlier non-cannulated screw systems (Chen et al 2005), further investigation of the stability of this cannulated screw system should now be performed with a longer follow-up period.
Table 4.
Summary of complications after spinal instrumentation in n = 67 patients
| N | Misplacement Grades | Screw associated | Surgical revision | ||
|---|---|---|---|---|---|
| Major complications | Radicular pain | 2 | D,D | Yes | Yes |
| CSF leak | 1 | D | Yes | Yes | |
| Epidural hematoma | 1 | B | No | No | |
| Pneumothorax | 1 | B | No | No | |
| Guillain-Barré-Syndrome | 1 | D | No | – | |
| Death | 1 | C | No | – | |
| Minor complications | Delayed wound healing | 4 | B,B,B,C | No | No |
| Urinary infection | 2 | B,C | No | – | |
| Colitis | 2 | B,D | No | – |
Footnotes
Disclosures
The authors have no conflicts of interest to disclose.
References
- Amiot LP, Lang K, Putzier M, et al. Comparative Results Between Conventional and Computer Assisted Pedicle Screw Installation in the Thoracic, Lumbar, and Sacral Spine. Spine. 2000;25:606–14. doi: 10.1097/00007632-200003010-00012. [DOI] [PubMed] [Google Scholar]
- Austin MS, Vaccaro AR, Brislin B, et al. Image-guided spine surgery: a cadaver study comparing conventional open laminoforaminotomy and two image-guided techniques for pedicle screw placement in posterolateral fusion and nonfusion models. Spine. 2002;27:2503–8. doi: 10.1097/01.BRS.0000031274.34509.1E. [DOI] [PubMed] [Google Scholar]
- Berlemann U, Heini P, Muller U, et al. Reliability of pedicle screw assessment utilizing plain radiographs versus CT reconstruction. Eur Spine J. 1997;6:406–10. doi: 10.1007/BF01834069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro WH, Halm H, Jerosch J, et al. Accuracy of pedicle screw placemnent in lumbar vertebrae. Spine. 1996;21:1320–24. doi: 10.1097/00007632-199606010-00008. [DOI] [PubMed] [Google Scholar]
- Chen CS, Chen WJ, Cheng CK, et al. Failure analysis of broken pedicle screws on spinal instrumentation. Med Eng Phys. 2005;27:487–96. doi: 10.1016/j.medengphy.2004.12.007. [DOI] [PubMed] [Google Scholar]
- Coe JD, Warden KE, Herzig MA, et al. Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine. 1990;15:902–7. doi: 10.1097/00007632-199009000-00012. [DOI] [PubMed] [Google Scholar]
- Dickman CA, Fessler RG, MacMillan M, et al. Transpedicular screw-rod fixation of the lumbar spine: operative technique and outcome in 104 cases. J Neurosurg. 1992;77:860–70. doi: 10.3171/jns.1992.77.6.0860. [DOI] [PubMed] [Google Scholar]
- Dvorak M, MacDonald S, Gurr KR, et al. An anatomic, radiographic, and biomechanical assessment of extrapedicular screw fixation in the thoracic spine. Spine. 1993;18:1689–94. doi: 10.1097/00007632-199309000-00018. [DOI] [PubMed] [Google Scholar]
- Ebmeier K, Giest K, Kalff R. Intraoperative computerized tomography for improved accuracy of spinal navigation in pedicle screw placement of the thoracic spine. Acta Neurochir Suppl. 85:105–13. doi: 10.1007/978-3-7091-6043-5_15. [DOI] [PubMed] [Google Scholar]
- Farber GL, Place HM, Mazur RA, et al. Accuracy of pedicle screw placement in lumbar fusions by plain radiographs and computed tomography. Spine. 1995;20:1494–99. doi: 10.1097/00007632-199507000-00010. [DOI] [PubMed] [Google Scholar]
- Gebhard F, Kinzl L, Arand M. Grenzen der CT-basierten Computer-navigation in der Wirbelsäulenchirurgie. Unfallchirurg. 2000;103:696–701. doi: 10.1007/s001130050605. [DOI] [PubMed] [Google Scholar]
- Gertzbein S, Robbins S. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–4. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- Girardi FP, Cammisa FP, Jr, Sandhu HS, et al. The placement of lumbar pedicle screws using computerised stereotactic guidance. Bone Joint Surg Br. 1999;81:825–9. doi: 10.1302/0301-620x.81b5.9244. [DOI] [PubMed] [Google Scholar]
- Grützner PA, Beutler T, Wendl K, et al. Navigation an der Brust-und Lendenwirbelsäule mit dem 3D-Bildwandler. Chirurg. 2004;75:967–75. doi: 10.1007/s00104-004-0944-3. [DOI] [PubMed] [Google Scholar]
- Hart RA, Hansen BL, Shea M, et al. Pedicle screw placement in the thoracic spine: a comparison of image-guided and manual techniques in cadavers. Spine. 2005;30:E326–31. doi: 10.1097/01.brs.0000166621.98354.1d. [DOI] [PubMed] [Google Scholar]
- Kim YJ, Lenke LG, Cheh G. Evaluation of pedicle screw placement in the deformed spine using intraoperative plain radiographs: a comparison with computerized tomography. Spine. 2005;30:2084–88. doi: 10.1097/01.brs.0000178818.92105.ec. [DOI] [PubMed] [Google Scholar]
- Laine T, Lund T, Ylikoski M, et al. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J. 2000;9:235–40. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–45. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- Lim MR, Girardi FP, Yoon SC, et al. Accuracy of computerized frameless stereotactic image-guided pedicle screw placement into previously fused lumbar spines. Spine. 2005;30:1793–98. doi: 10.1097/01.brs.0000171905.38459.b7. [DOI] [PubMed] [Google Scholar]
- Merloz P, Tonetti J, Pittet L, et al. Pedicle screw placement using image guided techniques. Clin Orthop Relat Res. 1998;354:39–48. doi: 10.1097/00003086-199809000-00006. [DOI] [PubMed] [Google Scholar]
- Misenhimer GR, Peek RD, Wiltse LL, et al. Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine. 1989;14:367–72. doi: 10.1097/00007632-198904000-00004. [DOI] [PubMed] [Google Scholar]
- Niu CC, Chen WJ, Chen LH, et al. Reduction-fixation spinal system in spondylolisthesis. Am J Orthop. 1996;25:418–24. [PubMed] [Google Scholar]
- Odgers CJ, 4th, Vaccaro AR, Pollack ME, et al. Accuracy of pedicle screw placement with the assistance of lateral plain radiography. J Spinal Disord. 1996;9:334–8. [PubMed] [Google Scholar]
- Roy-Camille R, Saillant G, Mazel C. Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986;17:147–59. [PubMed] [Google Scholar]
- Schaeren S, Roth J, Dick W. Effektive In-vivo-Strahlendosis bei bildwandlerkontrollierter Pedikelinstrumentation vs CT-basierter Navigation. Orthopade. 31:392–6. doi: 10.1007/s00132-001-0281-x. [DOI] [PubMed] [Google Scholar]
- Schnake KJ, König B, Berth U, et al. Genauigkeit der CT-basierten Navigation von Pedikelschrauben an der Brustwirbelsäule im Vergleich zur konventionellen Technik. Unfallchirurg. 2004;107:104–22. doi: 10.1007/s00113-003-0720-8. [DOI] [PubMed] [Google Scholar]
- Schwarzenbach O, Berlemann U, Jost B, et al. Accuracy of Computer-Assisted Pedicle Screw Placement: An In Vivo Computed Tomography Analysis. Spine. 1997;22:452–8. doi: 10.1097/00007632-199702150-00020. [DOI] [PubMed] [Google Scholar]
- Sjostrom L, Jacobsson O, Karlstrom G, et al. CT analysis of pedicles and screw tracts after implant removal in thoracolumbar fractures. J Spinal Disord. 1993;6:225–31. doi: 10.1097/00002517-199306030-00007. [DOI] [PubMed] [Google Scholar]
- Slomczykowski M, Roberto M, Schneeberger P, et al. Radiation dose for pedicle screw insertion. Fluoroscopic method versus computer-assisted surgery. Spine. 1999;24:975–82. doi: 10.1097/00007632-199905150-00009. [DOI] [PubMed] [Google Scholar]
- Suk SI, Lee CK, Min HJ, et al. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18:341–6. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- Weinstein J, Spratt KF, Spengler D, et al. Spinal pedicle fixation: Reliability and validity of roentgenogramm-based assessment and surgical factos on successful screw placement. Spine. 1988;13:1012. doi: 10.1097/00007632-198809000-00008. [DOI] [PubMed] [Google Scholar]
- Youkilis AS, Quint DJ, McGillicuddy JE, et al. Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery. 2001;48:771–8. doi: 10.1097/00006123-200104000-00015. [DOI] [PubMed] [Google Scholar]