Abstract
Context:
Altered neuromuscular control strategies during fatigue probably contribute to the increased incidence of non-contact anterior cruciate ligament injuries in female athletes.
Objective:
To determine biomechanical differences between 2 fatigue protocols (slow linear oxidative fatigue protocol [SLO-FP] and functional agility short-term fatigue protocol [FAST-FP]) when performing a running-stop-jump task.
Design:
Controlled laboratory study.
Setting:
Laboratory.
Patients or Other Participants:
A convenience sample of 15 female soccer players (age = 19.2 ±0.8 years, height = 1.67±0.05m, mass = 61.7 + 8.1 kg) without injury participated.
Intervention(s):
Five successful trials of a running–stop-jump task were obtained prefatigue and postfatigue during the 2 protocols. For the SLO-FP, a peak oxygen consumption (V˙o2peak) test was conducted before the fatigue protocol. Five minutes after the conclusion of the V˙o2peak test, participants started the fatigue protocol by performing a 30-minute interval run. The FAST-FP consisted of 4 sets of a functional circuit. Repeated 2 (fatigue protocol) × 2 (time) analyses of variance were conducted to assess differences between the 2 protocols and time (prefatigue, postfatigue).
Main Outcome Measure(s):
Kinematic and kinetic measures of the hip and knee were obtained at different times while participants performed both protocols during prefatigue and postfatigue.
Results:
Internal adduction moment at initial contact (IC) was greater during FAST-FP (0.064 ±0.09 Nm/kgm) than SLO-FP (0.024±0.06 Nm/kgm) (F1,14 = 5.610, P=.03). At IC, participants had less hip flexion postfatigue (44.7°±8.1°) than prefatigue (50.1°±9.5°) (F1,14 = 16.229, P=.001). At peak vertical ground reaction force, participants had less hip flexion postfatigue (44.7°±8.4°) than prefatigue (50.4°±10.3°) (F1,14 = 17.026, P=.001). At peak vertical ground reaction force, participants had less knee flexion postfatigue (−35.9°±6.5°) than prefatigue (−38.8°±5.03°) (F1,14 = 11.537, P=.001).
Conclusions:
Our results demonstrated a more erect landing posture due to a decrease in hip and knee flexion angles in the postfatigue condition. The changes were similar between protocols; however, the FAST-FP was a clinically applicable 5-minute protocol, whereas the SLO-FP lasted approximately 45 minutes.
Keywords: anterior cruciate ligament, hip, knee, biomechanics
Key Points.
Both the slow linear oxidative fatigue protocol (SLO-FP) and the functional agility short-term fatigue protocol (FAST-FP) demonstrated that the lower extremity is at a higher risk for sustaining injury when fatigue and unanticipated movement are combined.
Similar lower extremity biomechanical modifications occurred after 5 minutes of fatigue during the FAST-FP and after 45 minutes of fatigue during the SLO-FP.
Fatigue-induced decreases in hip and knee flexion resulted in a more extended landing posture, which can increase anterior tibial translation and thus increase strain on the anterior cruciate ligament.
Current research on anterior cruciate ligament (ACL) injury and the implications of sex continue to reveal an increased incidence in females sustaining noncontact ACL injury.1–4 When comparing the incidence of ACL injury in intercollegiate athletics, Mihata et al2 found the incidence was almost 3 times higher in female than male soccer athletes, whereas it was almost 4 times higher in female than male basketball players. In intercollegiate athletics, Hootman et al5 reported that 3 of the 4 sports with the highest rates of ACL injury were women's sports: gymnastics, soccer, and basketball. Anterior cruciate ligament injury has multiple negative health consequences, including early onset of osteoarthritis, damage to menisci and chondral surfaces, increased probability of additional surgery, and decreased activity level due to functional instability.6,7 In a 20-year follow-up study of operatively repaired ACL ruptures, Maletius and Messner6 found that 87% of patients had signs of osteoarthritis on radiographic examination, 45% of patients had undergone additional surgery, and only 23% of patients were satisfied with their knee function.
The 4 categories of risk factors for ACL injury are anatomical, hormonal, environmental, and neuromuscular.8,9 Of all the risk factors associated with ACL injury, altered neuromuscular control strategies and movement variables are most likely to contribute to the greater incidence of noncontact ACL injury for female athletes.10 Neuromuscular control strategies are altered further when the effects of fatigue combined with unanticipated movements are present.11 Fatigue has been found to increase peak proximal tibial anterior shear force,12 increase knee abduction angle,11,13 decrease knee flexion angle,12 decrease hip flexion angle,11 increase peak valgus angle and maximum valgus angle,11,13 increase knee internal rotation,11,14 and result in a greater knee extension moment.12 Unanticipated movement has been found to induce an increase in knee valgus moment, hip internal rotation, knee abduction, and knee internal rotation.11,15 The combination of fatigue and unanticipated movement typically results in altered lower extremity mechanics in which the foot is planted, the knee is near full extension in an abducted position, and the femur (hip) is rotated internally; all of these are hypothesized mechanisms for ACL injury.7,16–19
The occurrence of the theorized risk factors associated with ACL injury varies depending on the task being analyzed. Various tasks have been used in previous research, including sidestep cutting,11,20 drop-jump,13,21 and stop-jump12,22 tasks. The use of different tasks when analyzing the lower extremity biomechanical variables has yielded conflicting results. Researchers11,20 using the side-step cutting task have reported that fatigue produces changes mainly in frontal-plane kinematics and kinetics. However, researchers12 who analyzed the stop-jump task found that fatigue produces changes in both frontal-plane and sagittal-plane kinematics and kinetics.
Current research on fatigue and its associated relationship between noncontact ACL injuries has been focused on either short-term fatigue or long-term fatigue protocols.11,12,14,20,23–26 Short-term fatigue protocols have induced fatigue through single-leg squats,20 consecutive repetitions of vertical jumps and short sprints,12 and maximum repetitions on a leg-press machine.25 No consensus exists in the literature to indicate which type of fatigue protocol results in greater biomechanical alterations to the lower extremity during unanticipated movement. Furthermore, little research comparing the effects of functional sport-specific fatigue on lower extremity joint kinematics and kinetics is available. Soccer-specific fatigue using various aspects of an actual soccer practice and games should be implemented to accurately and effectively analyze the neuromuscular changes that occur during fatigued states in this specific population. Therefore, the purpose of our study was to determine biomechanical differences between 2 fatigue protocols (slow linear oxidative fatigue protocol [SLO-FP] and functional agility short-term fatigue protocol [FAST-FP]) as measured by various kinematic and kinetic variables. We hypothesized that fatigue would negatively alter lower extremity biomechanics. Specifically, participants would have less hip flexion and knee flexion and more knee valgus, hip abduction, vertical ground reaction force, and posterior ground reaction force. Furthermore, those changes would be more pronounced after the FAST-FP.
METHODS
Participants
An a priori power calculation was conducted to estimate the sample needed to establish differences between fatigue protocols. Using data from the literature,11–13 we determined that a sample size of approximately 15 participants was needed for a power level of 80%, an α level of .05, and an anticipated effect size of 0.7. A convenience sample of 15 National Collegiate Athletic Association (NCAA) Division I female soccer players (age=19.2±0.8 years, height =1.67±0.05 m, mass=61.7±8.1 kg) volunteered to participate. Inclusion criteria were no history of cardiovascular or respiratory disease. In addition, clearance from the team physician to practice and play in games was required at the time of data collection. The dominant leg, which was defined as the leg that the participant would use to kick a soccer ball as far as possible, was analyzed. All participants provided written informed consent, and the study was approved by the Institutional Review Board of Old Dominion University.
Instrumentation
The lower extremity was analyzed using 8 high-speed infrared cameras (Vicon, Oxford, United Kingdom) sampling at a rate of 270 Hz. Ground reaction forces were measured via 2 force plates (model 4060-10; Bertec Corporation, Columbus, OH) at a sampling rate of 1080 Hz. A metabolic cart (model Vmax 29c; CareFusion, San Diego, CA) was used during the SLO-FP to measure submaximal oxygen consumption and peak oxygen consumption (V˙o2peak). The flow sensor was calibrated against a 3.0-L syringe, and carbon dioxide and oxygen sensors were calibrated against known gases before the maximum oxygen consumption (V˙o2max) test. The flow sensor and mouthpiece were attached to a headset, which was used to collect expired air. An average of the 3 highest, continuous, 20-s interval oxygen consumption (V˙o2) measurements was used to calculate V˙o2peak. A heart rate monitor (model FS2C; Polar Electro, Inc, Lake Success, NY) was used to collect measurements of resting and exercise heart rates during the entire test.
From the standing (static) trial, a lower extremity kinematic model was created for each participant using Visual3D (C-Motion, Inc, Germantown, MD). Motion at the hip, knee, and ankle joints was quantified using this kinematic model. The standing (dynamic) trial with circular motion of the pelvis was used to estimate a functional hip joint center.27,28 Based on a power spectrum analysis, all kinematic and kinetic data were low-pass filtered through a fourth-order, zero-phase lag, Butterworth filter with a cutoff frequency of 25 Hz.
Experimental Protocol
Participants wore spandex shorts, sports bras, and team running shoes (Supernova; Adidas AG, Herzogenaurach, Germany). The participants were given a 10-minute warmup period, which consisted of self-directed cycling and stretching. After this period, 40 reflective markers were placed on specific anatomical landmarks. Thirty markers were tracking markers consisting of 1 on each posterosuperior iliac crest and anterior iliac crest, clusters of 4 on each thigh and shank, and 5 on each foot. The remaining 10 were calibration markers, which were placed on the greater trochanters, medial and lateral femoral condyles, and medial and lateral malleoli. The same researcher (N.C.) placed the markers on all participants. Pilot testing in our laboratory has shown good to excellent reliability in marker placement and data repeatability for lower extremity biomechanical measures (intraclass correlation coefficient range, 0.620–0.889). Standing and dynamic calibration trials were done to calculate hip joint center. After those trials, the calibration markers were removed.
After the running-stop-jump task was explained, the participants were given time to practice. An infrared beam was placed across and 2 m before the force plates where the participants were running. When the participants crossed and interrupted the light beam, it triggered a software program, which we developed, on the desktop to randomly generate 1 of the soccer athletic tasks (eg, running stop-jump, side step) and project it onto a screen in front of the participants.29 For the purpose of our study, only the running–stop-jump task was used for analysis. Participants had to attain a minimal approach speed of 3.5 m/s,30 which was monitored by a timing system (Brower Timing Systems, Draper, UT). The running–stop-jump task consisted of the participants standing at the beginning of the runway, running and planting onto the force plates with 1 foot on each force plate, and jumping straight into the air as if performing a soccer header. Testing trials were repeated if the participant did not land completely on the force plate or was unable to execute the trials at a minimum speed of 3.5 m/s. After completing 5 successful unanticipated trials, the participants received instructions about the fatigue protocol to be performed. They rested for 1 minute between trials to minimize fatigue during prefatigue assessment.
Functional Agility Short-Term Fatigue Protocol
Before beginning the FAST-FP, 1 investigator (D.Q.) measured the participants' maximal vertical jumps with a measuring tape on the wall. The average of 3 maximal jumps was recorded as the participant's maximal vertical jump for the protocol. Participants began the fatigue protocol by performing a series of step-up and step-down movements onto and off of a 30-cm-high box for 20 seconds in time with a metronome set to 220 beats per minute. Next, the participants immediately performed 1 repetition of an L drill among 3 cones. Participants started in a 3-point stance in front of 3 cones that were set up in an L shape and spaced 4.5 yd (4.05 m) apart. Starting at the first cone, they sprinted 4.5 yd (4.05 m) to the second cone, sprinted back to the first cone, ran to the second cone, ran around the right side of the second cone and to the third cone, ran in a circle around the third cone from the inside to the outside, sprinted back to the second cone, ran around the left side of the second cone, and ran back to the first cone (Figure 1). Immediately after the L drill, participants performed 5 consecutive countermovement jumps, staying within 80% (±2%) of their maximal vertical jump recorded before the start of the protocol. Marks were placed within 80% (±2%) to ensure that they stayed within the range. After the vertical jumps, the participants ran down and back on an agility ladder. When completing the protocol for the first and third times, the participants ran forward, ensuring that both feet touched inside each space of the ladder. When completing the protocol for the second and fourth times, the participants went sideways, ensuring that both feet touched inside each space of the ladder. The metronome also was used for the ladder drill and was set at 220 beats per minute so the participants would maintain a constant speed throughout the protocol. Completing the 4 tasks (step-up and step-down movements, L drill, vertical jumps, and ladder drill) counted as 1 set of the protocol. Participants had to perform 4 sets of the protocols with no rest in between, which took approximately 5 minutes per participant.
Figure 1.
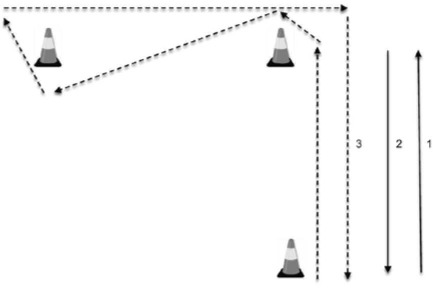
Schematic of the L drill of the functional agility short-term fatigue protocol. The distance between cones was 4.5 yd (4.05 m).
Slow Linear Oxidative Fatigue Protocol
Participants started the fatigue protocol by performing a V˙o2max test. The protocol was explained to the participants, and they were fitted with a mouthpiece and headset, which they were required to wear for the V˙o2max test. Running shorts were placed over the tracking markers, and skin lubricant was applied to any areas on the participants' thighs that might rub and cause irritation during the prolonged run. The protocol for the V˙o2max test has been used in previous research31,32 and required the participants to run at 9 km/h for 5 minutes followed by 1-km/h speed increments every 2 minutes until exhaustion. Participants were instructed to grab the sides of the treadmill when they felt they were fatigued maximally and could not continue running, at which point the treadmill was slowed down to a walk (Figure 2). A participant was considered to have reached maximal fatigue when she met 2 of the following criteria: (1) her heart rate reached 90% of her age-calculated maximum heart rate, (2) her respiratory quotient was more than 1.1, (3) she reached the plateau in the V˙o2max curve, and (4) she was unable to continue running. The treadmill gradient was kept at 0° for the entire V˙o2max test. After completing the V˙o2max test, the participants rested for 5 minutes. Immediately after the rest period, the participants alternated between 2 running speeds throughout the 30-minute treadmill run. Six intervals consisting of running at a speed of 70% of the final V˙o2max speed for 4 minutes followed by running at a speed of 90% of their final V˙o2max speed for 1 minute were conducted. The estimated time for the V˙o2max test was 15 minutes, which, when combined with the 30-minute treadmill run, equaled 45 minutes and simulated 1 half of a collegiate soccer match.
Figure 2.
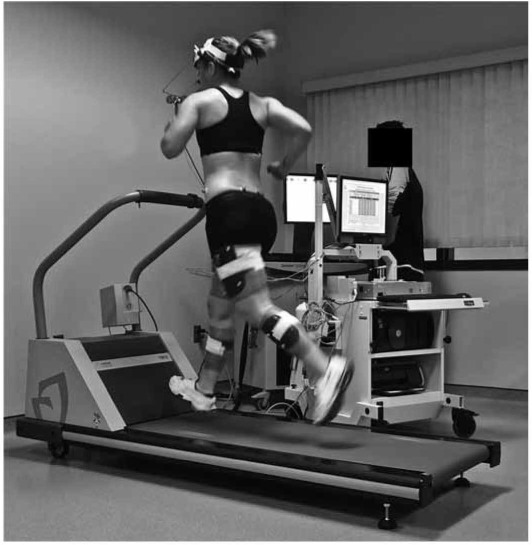
A maximum oxygen consumption test was conducted before the 30-minute running protocol for the slow linear oxidative fatigue protocol.
Posttest Fatigue Assessment
After completing each fatigue protocol, the participants again were required to perform 5 successful unanticipated trials of the running–stop-jump task. After each running–stop-jump task, participants immediately ran back to the start of the runway and performed another trial until 5 successful running–stop-jump tasks were completed. After completing the FAST-FP, participants were required to complete 3 vertical jumps between dynamic trials to maintain fatigue throughout the posttest fatigue assessment. The fatigue protocols (SLO-FP, FAST-FP) were counterbalanced between participants, with a 1-week break between fatigue and data collection sessions.
Statistical Analysis
Prefatigue conditions (SLO-FP, FAST-FP) were compared with a paired t test to assess the baseline assumption (prefatigue was equal between protocols) for possible comparison of post-fatigue conditions between the SLO-FP and FAST-FP. The independent variables were fatigue protocols and time. Separate repeated-measures 2 (fatigue protocols: SLO-FP, FAST-FP) × 2 (time: prefatigue, postfatigue) analyses of variance were conducted for each dependent variable and time instant. Kinematic variables were knee flexion, knee abduction, knee rotation, hip flexion, and hip abduction. Kinetic variables were vertical and posterior ground reaction forces, knee flexion-extension moment, knee abduction-adduction moment, hip flexion moment, and hip abduction-adduction moment; these were measured at various time instants: initial contact, peak vertical and posterior ground reaction forces, peak knee flexion, and peak during the stance phase. Kinematic variables were measured in degrees, internal joint moments were normalized to height and mass, and ground reaction forces were normalized to body weight. Initial contact was defined as the time at which vertical ground reaction force was greater than 10 N. Peak was defined as the maximum value obtained between initial contact and 50% of stance phase. We used Visual3D and a custom-made MATLAB (The MathWorks, Inc, Natick, MA) for data reduction to export data into SPSS (version 16.0; SPSS Inc, Chicago, IL). The average of 5 trials was used for all analyses. The α level was set a priori at .05.
RESULTS
Descriptive statistics are presented in Tables 1–4. Participants had an approach speed of 3.6±0.19 m/s before SLO-FP, 3.5±0.14 m/s after SLO-FP, 3.6±0.12 m/s before FAST-FP, and 3.5±0.12 m/s after FAST-FP. We found no differences between approach speeds for either protocol or fatigue condition (P>.05).
Table 1.
Descriptive Statistics for Kinematic Variables Between 2 Fatigue Protocols at Initial Contact, Peak Vertical Ground Reaction Force, Peak Posterior Ground Reaction Force, Peak Knee Flexion, and Peak Stance (Mean±SD)
| Kinematic Variable | Slow Linear Oxidative Fatigue Protocol |
Functional Agility Short-Term Fatigue Protocol |
||
| Pretest | Posttest | Pretest | Posttest | |
| Initial contact, ° | ||||
| Knee flexion (−)/extension (+) | −27.4 ±8.5 | −24.5 ±9.2 | −25.9 ±8.1 | −25.2 ±9.1 |
| Knee abduction (−)/adduction (+) | −0.9 ±3.2 | −1.0±3.9 | −1.3 ±4.2 | −2.3 ±5.6 |
| Knee internal rotation (+)/external rotation (−) | 8.8 ±7.3 | 8.8±6.5 | 7.9±7.8 | 11.9±9.8 |
| Hip flexion | 50.3 ±10.5 | 46.5±6.6 | 49.9±8.4 | 42.9±9.6 |
| Hip abduction (−)/adduction (+) | −5.0 ±5.2 | −5.6 ±4.6 | −5.5 ±4.5 | −6.4 ±5.8 |
| Peak vertical ground reaction force, ° | ||||
| Knee flexion (−)/extension (+) | −39.1 ±5.1 | −36.1 ±7.4 | −38.4 ±5.0 | −35.7 ±5.6 |
| Hip flexion | 50.4 ±11.5 | 46.9 ±7.3 | 50.5 ±9.1 | 42.5±9.5 |
| Peak posterior ground reaction force, ° | ||||
| Knee flexion (−)/extension (+) | −38.3 ±5.7 | −36.6 ±7.8 | −38.5 ±5.5 | −34.9 ±6.7 |
| Knee abduction (−)/adduction (+) | −0.4 ±4.7 | −1.1 ±5.2 | −1 8±5.1 | −2.5 ±6.6 |
| Hip flexion | 51.3 ±12.0 | 46.9 ±7.3 | 50.8±9.5 | 43.4±9.9 |
| Peak knee flexion, ° | ||||
| Knee flexion (−)/extension (+) | −55.9 ±7.8 | −53.3 ±5.6 | −57.61 ±8.9 | −51.6 ±10.1 |
| Knee abduction (−)/adduction (+) | −2.4 ±5.9 | −3.7 ±6.2 | −5.2 ±5.3 | −5.6 ±6.4 |
| Hip flexion | 44.6 ±12.8 | 40.5 ±7.6 | 45.6±10.4 | 36.8±9.7 |
| Hip abduction (−)/adduction (+) | −1.8±4.1 | −1.9 ±3.7 | −3.1 ±4.6 | −4.4±4.7 |
| Peak stance, ° | ||||
| Knee abduction (−)/adduction (+) | −4.6±3.9 | −5.5±5.1 | −6.1 ±4.9 | −7.0 ±5.9 |
| Hip flexion | 53.3 ±11.9 | 49.1 ±6.7 | 53.3±10.0 | 45.6±9.8 |
Table 2.
Descriptive Statistics for Kinetic Variables Between 2 Fatigue Protocols at Initial Contact, Peak Vertical Ground Reaction Force, Peak Posterior Ground Reaction Force, Peak Knee Flexion, and Peak Stance (Mean±SD)
| Kinetic Variable | Slow Linear Oxidative Fatigue Protocol |
Functional Agility Short-Term Fatigue Protocol |
||
| Pretest | Posttest | Pretest | Posttest | |
| Initial contact, Nm/kgm | ||||
| Knee abduction (−)/adduction (+) moment | −0.006 ±0.28 | −0.03 ±0.24 | 0.05 ±0.20 | 0.071 ±0.23 |
| Knee flexion (−)/extension (+) moment | 0.08±0.21 | 0.02±0.15 | 0.04±0.18 | 0.06 ±0.23 |
| Peak vertical ground reaction forcea | ||||
| Vertical ground reaction force | 5.1 ±1.3 | 5.2±1.1 | 4.6 ±1.2 | 4.9 ±1.3 |
| Peak posterior ground reaction forcea | ||||
| Posterior ground reaction force | 1.9 ±0.5 | 1.8 ±0.4 | 1.8 ±0.4 | 1.8 ±0.3 |
| Peak knee flexiona | ||||
| Posterior ground reaction force | 1.3±0.3 | 1.3±0.3 | 1.2 ±0.4 | 1.3 ±0.3 |
| Peak stance, Nm/kgm | ||||
| Knee flexion (−)/extension (+) moment | 2.09 ±0.33 | 2.08 ±0.30 | 1.98 ±0.33 | 1.92 ±0.39 |
| Knee abduction (−)/adduction (+) moment | 0.34±0.16 | 0.37±0.25 | 0.33±0.13 | 0.41 ±0.22 |
aIndicates ground reaction forces measures are given in multiples of body weight.
Table 3.
Descriptive Statistics for Kinematic Variables by Protocol and Fatigue at Initial Contact, Peak Vertical Ground Reaction Force, Peak Posterior Ground Reaction Force, Peak Knee Flexion, and Peak Stance (Mean ± SD)
| Kinematic Variable | Protocol |
Fatigue |
||
| Slow Linear Oxidative Fatigue | Functional Agility Short-Term Fatigue | Pretest | Posttest | |
| Initial contact, ° | ||||
| Knee flexion(−)/extension(+) | −25.9 ±8.9 | −25.6 ±8.6 | −26.6 ±8.3 | −24.9 ±9.2 |
| Knee abduction (−)/adduction (+) | −0.96 ±3.5 | −1.8 ±4.9 | −1.1 ±3.7 | −1.7±4.7 |
| Hip flexion | 48.4±8.6 | 46.4±9.0 | 50.1 ±9.5 | 44.7±8.1 |
| Hip abduction (−)/adduction (+) | −5.3 ±4.9 | −5.9±5.1 | −5.2 ±4.9 | −6.0 ±5.2 |
| Knee internal rotation (+)/external rotation (−) | 8.8 ±6.9 | 9.9±8.8 | 8.4±7.5 | 10.3 ±8.2 |
| Peak vertical ground reaction force, ° | ||||
| Knee flexion (−)/extension (+) | −37.6 ±6.3 | −37.0 ±5.3 | −38.8 ±5.0 | −35.9 ±6.5 |
| Hip flexion | 48.7±9.4 | 46.5±9.3 | 50.4±10.3 | 44.7±8.4 |
| Peak posterior ground reaction force, ° | ||||
| Knee flexion (−)/extension (+) | −37.5 ±6.7 | −36.7 ±6.1 | −38.4 ±5.6 | −35.8 ±7.2 |
| Knee abduction (−)/adduction (+) | ||||
| Hip flexion | 49.1 ±9.7 | 47.1 ±9.7 | 51.1 +10.8 | 45.2±8.6 |
| Peak knee flexion, ° | ||||
| Knee flexion (−)/extension (+) | −54.6 ±6.7 | −54.6 ±9.5 | −56.8 ±8.3 | −52.5 ±7.9 |
| Knee abduction (−)/adduction (+) | −3.0 ±6.0 | −5.4 ±5.8 | −3.8 ±5.6 | −4.7±6.3 |
| Hip flexion | 42.6 ±10.2 | 41.2 + 10.1 | 45.1 ±11.6 | 38.7±8.7 |
| Hip abduction (−)/adduction (+) | −1.8 ±3.9 | −3.8 ±4.6 | −2.4 ±4.4 | −3.1 ±4.2 |
| Peak stance, ° | ||||
| Knee abduction (−)/adduction (+) | −5.0 ±4.5 | −6.5 ±5.4 | −3.8 ±4.4 | −4.7±5.5 |
| Hip flexion | 51.2±9.3 | 49.5±9.9 | 53.3±11.0 | 47.3±8.2 |
Table 4.
Descriptive Statistics for Kinetic Variables by Protocol and Fatigue at Initial Contact, Peak Vertical Ground Reaction Force, Peak Posterior Ground Reaction Force, Peak Knee Flexion, and Peak Stance (Mean±SD)
| Kinetic Variable | Protocol |
Fatigue |
||
| Slow Linear Oxidative Fatigue | Functional Agility Short-Term Fatigue | Pretest | Posttest | |
| Initial contact, Nm/kgm | ||||
| Knee flexion (−)/extension (+) moment | 0.051 ±0.18 | 0.050 ±0.20 | 0.057±0.19 | 0.044±0.19 |
| Knee abduction (−)/adduction (+) moment | 0.024 ±0.06 | 0.064 ±0.09 | 0.037 ±0.06 | 0.048 ±0.09 |
| Peak vertical ground reaction forcea | ||||
| Vertical ground reaction force | 5.1 ±1.2 | 4.8 ±1.2 | 4.9 ±1.2 | 5.1 ±1.2 |
| Peak posterior ground reaction forcea | ||||
| Posterior ground reaction force | 1.9 ±0.42 | 1.8 ±0.36 | 1.9 ±0.45 | 1.8 ±0.34 |
| Peak knee flexiona | ||||
| Posterior ground reaction force | 1.3 ±0.30 | 1.2 ±0.33 | 1.2 ±0.35 | 1.3 ±057 |
| Peak stance, Nm/kgm | ||||
| Knee flexion (−)/extension (+) moment | 2.01 ±0.32 | 1.9 ±0.36 | 2.0±0.33 | 2.0±0.35 |
| Knee abduction (−)/adduction (+) moment | 0.36±0.21 | 0.37±0.18 | 0.34±0.14 | 0.39 ±0.24 |
aIndicates ground reaction forces measures are given in multiples of body weight.
Fatigue
The primary differences attained due to the fatigue main effect were observed at the sagittal plane of the knee and hip at the different time instants. Participants landed with less hip flexion at postfatigue than prefatigue at all time instants analyzed. At initial contact, the participants landed in less hip flexion post-fatigue (44.7°±8.1°) than prefatigue (50.1°±9.5°) (F1,14= 16.229, P=.001, Cohen d=0.57). At peak vertical ground reaction force, participants landed in less hip flexion postfatigue (44.7° ±8.4°) than prefatigue (50.4° ±10.3°) (F1,14 = 17.026, P=.001, Cohen d=0.55). At peak posterior ground reaction force, participants had less hip flexion postfatigue (45.2° ± 8.6°) than prefatigue (51.1°±10.8°) (F1,14 =18.533, P=.001, Cohen d=0.55) (Figure 3). At peak knee flexion, participants landed in less hip flexion postfatigue (38.7° ±8.7°) than prefatigue (45.1°±11.6°) (F1,14= 17.331, P=.001, Cohen d=0.55) (Figure 3). Lastly, at peak hip flexion, participants landed in less hip flexion postfatigue (47.3° ±8.2°) than prefatigue (53.3°± 10.95°) (F1,14 = 16.616, P=.001, Cohen d=0.55).
Figure 3.
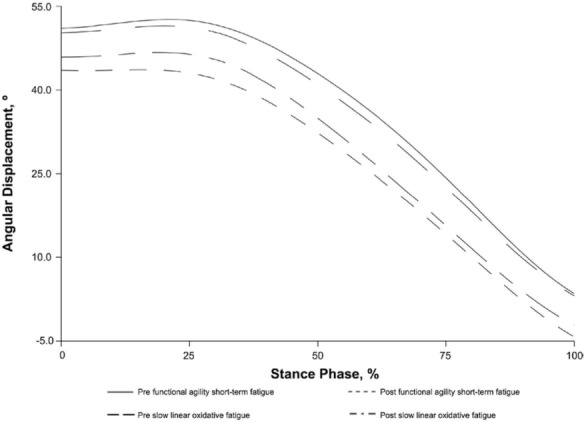
Hip flexion angle during the slow linear oxidative fatigue protocol and functional agility short-term fatigue protocol (prefatigue and postfatigue conditions) in a running–stop-jump task.
For knee flexion, the following differences were obtained. At peak knee flexion participants landed in less knee flexion postfatigue (−52.5° ±7.9°) than prefatigue (56.8° ±8.3°) (F1,14=24.346, P<.001, Cohend=0.52) (Figure 4). At peak vertical ground reaction force, participants landed in less knee flexion postfatigue (−35.9° ± 6.5°) than prefatigue (−38.8° ± 5.03°) (F1,14 =11.537, P=.001, Cohen d=0.48). Lastly, at peak posterior ground reaction force, participants landed in less knee flexion postfatigue (−35.8°±7.2°) than prefatigue (−38.4°±5.6°) (F1,14 =9.300, P=.009, Cohen d=0.39).
Figure 4.
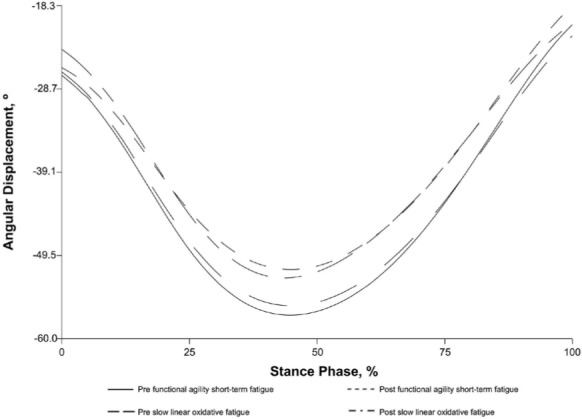
Knee flexion angle during the slow linear oxidative fatigue protocol and functional agility short-term fatigue protocol (prefatigue and postfatigue conditions) in a running–stop-jump task.
Protocol
At peak knee flexion, hip abduction was greater during the posttest of FAST-FP (−3.8° ±4.6°) than the SLO-FP (−1.8°±3.9°) (F1,14 = 13.086, P=.003, Cohen d=0.41). At initial contact, internal knee adduction moment was greater during the FAST-FP (0.064 ±0.09 Nm/kgm) than the SLO-FP (0.024 ±0.06 Nm/kgm) (F1,14 =5.610, P=.03, Cohen d=0.44). At peak stance (maximum value), internal knee extension moments were greater during the SLO-FP (2.01 ±0.32 Nm/kgm) than the FAST-FP (1.9±0.36 Nm/kgm) (F1,14 =6.486, P=.02, Cohen d=0.31).
The only interaction attained was at initial contact. We found that knee internal rotation was greater after the FAST-FP (11.9°±9.8°) than before the FAST-FP (7.9°±7.8°) (F1,14 =7.025, P=.02, Cohen d=0.41).
DISCUSSION
We evaluated the effects of 2 fatigue protocols (SLO-FP, FAST-FP) on lower extremity biomechanics during an unanticipated running–stop-jump task in female NCAA Division I soccer players. We hypothesized that fatigue would induce lower extremity biomechanical alterations in the hip and knee during the landing phase of the running–stop-jump task. One of our main results was a decrease in knee and hip flexion after the 2 types of fatigue protocols. The participants presented a more erect or extended position after being fatigued. Landing with the knee in a more extended position is thought to increase anterior shear force on the proximal end of the tibia via an increased patellar tendon–tibia shaft angle.33 Researchers have suggested that increased tibial anterior shear force results in increased loads being placed on the ACL.12,21 Blackburn and Padua34 showed that landing in a more erect posture results in increased ground reaction forces and subsequent quadriceps activation. Therefore, our participants might have increased the strain placed on the ACL and consequently increased ACL loading because of their erect positions. The decreased joint angles (eg, knee flexion) are thought to produce a mechanical disadvantage for the hamstring muscles by decreasing their angles of pull and reducing the amount of posterior force that can be applied to the tibia.35 This decreased posterior force allows increased anterior translation, which also could increase the load placed on the ACL.35 The combination of lower knee and hip joint angles during an unanticipated task (decision-making process) under a fatigued condition might increase the likelihood of injury.
The fatigue protocols created for our study were based on previous research; however, various aspects of each protocol are unique to our study. The FAST-FP used tasks, including vertical jumps12 and step-ups,13 from previous research. To our knowledge, the L drill and agility ladder have not been used to induce fatigue; we chose both activities to reproduce the functional demands of soccer. The V˙o2max protocol used in the SLO-FP was based on previous research.31,32 The 30-minute treadmill run was based on the fatigue protocol of Sanna and O'Connor.14 Fatigue has been shown to alter hip and knee kinematics during various athletic tasks.13,20,21,36 Our results, which showed that fatigue changes lower extremity biomechanics during a landing task, are similar to those of other investigators.11,12,20 Chappell et al12 found a decrease in knee flexion angle at peak proximal tibial anterior shear force in a stop-jump task similar to the one we used. Their participants had a knee flexion angle at prefatigue of 26.3° and at postfatigue of 23.1°, representing a 12% decrease between fatigue states.12
We analyzed knee flexion at peak posterior ground reaction force and peak vertical ground reaction force, both of which have been shown to be correlated with peak proximal tibial anterior shear force,37 and found a decrease of 6.9% (prefatigue=−38.4°, postfatigue=−35.8°) and 7.4% (prefatigue= −38.8°, postfatigue=−35.9°), respectively. The percentage change for our study was smaller than the change reported by Chappell et al.12 The smaller decrease in knee flexion angle in our study could be a result of the increased level of conditioning and athletic ability present in our participants. However, the reduced knee flexion angle at peak posterior ground reaction force still might be increasing the load on the ACL, thereby increasing its likelihood of rupture. Cerulli et al38 analyzed the strain placed on the ACL during rapid deceleration and found ACL strain to be highest during peak ground reaction force. Anterior displacement of the tibia via the quadriceps is most pronounced between 15° and 45° of knee flexion, with the peak anterior translation occurring at 30° of knee flexion.39 With fatigue, knee flexion decreased from −38.8° to −35.9° at peak vertical ground reaction force and decreased from −38.4 to −35.8° at peak posterior ground reaction force. In effect, fatigue is moving the knee closer to 30° of knee flexion, where peak anterior translation of the tibia is thought to occur. However, this change in flexion of approximately 3° might not appear to be clinically relevant. From our standpoint, we cannot precisely say whether the 3° change is clinically important; however, we believe it is relevant and important when analyzing how the lower extremity responds to the demands of fatigue. This small change can represent the difference between injury and no injury occurring.
We and others11,13,14,20 analyzed lower extremity biomechanics during the performance of various unanticipated tasks. Although each task performed was unanticipated, the participant knew the task had to be 1 of 3 options and was never exposed to repeated unanticipated movements. Therefore, to complete a successful trial, the participant was required only to complete 1 unanticipated movement without being concerned with what would happen next. In real-life game situations, athletes are exposed to a constantly evolving environment in which they are required to perform multiple unanticipated movements in conjunction with each other. This collection of unanticipated movements along with a combination of motion in the sagittal, frontal, and transverse planes might be what produces the abnormal out-of-plane motion commonly seen during an ACL injury. In the future, researchers should examine the effects that multiple unanticipated movements have on lower extremity biomechanics.
Landing in a more extended position possibly decreases the capability of the lower extremity to effectively absorb shock through decreased flexion of the joints.40 This increased force on the knee joint could decrease the stability of the joint, making it more susceptible to out-of-plane motions and increasing the likelihood of ACL injury. Researchers have analyzed the landing phase of single-legged jumps both prefatigue and postfatigue and have found the following frontal-plane changes: increased knee abduction and internal rotation,11,13,20,41 increased hip internal rotation,11,20,42 and increased hip internal rotation moment from prefatigue to postfatigue.20 The task used in those studies differed from the running–stop-jump task we used. The lower extremity biomechanical adaptation for the demands of different tasks partially might explain the difference in results. With the running–stop-jump task, the demands occur primarily in the sagittal plane with full deceleration to perform a vertical jump, whereas the side-step cutting task combines a deceleration with an acceleration phase and a change in direction (eg, 45° angle). Characteristics of both tasks have been observed during ACL tear events; however, the difference between these tasks makes comparison challenging. How each task (running stop, side-step cut, single-legged landing, and double-legged landing) is modified by increasing or decreasing the lower extremity biomechanical variables is important and should be the focus of future research.
Although the differences between the 2 fatigue protocols were minimal, we found that the FAST-FP induced changes in frontal-plane hip and knee biomechanics when compared with the SLO-FP. Hip abduction at peak knee flexion was greater during the FAST-FP than during the SLO-FP. The multidirectional movements associated with the FAST-FP possibly induced greater amounts of fatigue to the hip musculature of our participants, resulting in greater hip abduction after FAST-FP. The multidirectional functional protocol recruited various muscle groups (eg, flexors and extensors, abductors and adductors), whereas the SLO-FP affected primarily the flexors and extensors. This increased hip abduction angle during landing has been associated with excessive knee valgus and abduction moments.21,43 Furthermore, at initial contact participants had greater knee adduction moments during the FAST-FP than the SLO-FP. In the transverse plane, knee internal rotation increased from prefatigue to postfatigue in the FAST-FP. Fatigue has been shown to alter knee abduction and adduction moments20 and knee internal rotation11 during landing tasks. We assume that a relationship exists between the increase in internal knee adduction moment induced by the FAST-FP and the increased knee internal rotation present postfatigue during the FAST-FP. The increased internal knee adduction moment probably is a response to an increased external valgus load attempting to force the knee into an abducted position. Our assumption is based on the premise that an external knee abduction moment tends to produce an abducted knee angle that would be resisted by an internal knee adduction moment.
Our results indicated that both the SLO-FP and FAST-FP induced similar kinematic and kinetic changes to the lower extremity during the running–stop-jump task. The fatigue protocols elicited the largest variations in sagittal-plane lower extremity kinematics. Specifically, participants landed with less hip flexion at all time instances analyzed. Sagittal-plane knee mechanics were altered with fatigue; specifically, a decrease in knee flexion was seen at peak vertical ground reaction force, peak posterior ground reaction force, and peak knee flexion. Researchers who did not completely use a SLO-FP or FAST-FP but induced lower extremity fatigue found similar results for these kinematic variables.11,12,20
An interesting result to note is the lack of difference between fatigue protocols (SLO-FP and FAST-FP). Most prefatigue to postfatigue changes were observed regardless of the fatigue protocol used, with minimal differences noted between the 2 protocols. One possible reason for the similarities between the SLO-FP and FAST-FP was that our participant population was accustomed to a wide range of activity, including short-term, high-intensity exercise and long-duration, low-intensity exercise. During competition, elite female soccer athletes change activity an average of 1459 times. The changes in activity range from standing to walking, low-intensity running, and high-intensity running.44 Krustrup et al44 reported that elite female soccer players had an average heart rate during a competitive match that was 87% of their maximum heart rates. The average heart rate for our participants during both fatigue protocols was 89.6% of their maximum heart rates, which was similar to what is experienced during competition. Therefore, our participant population of elite soccer athletes appears to have been able to adjust accordingly to both the SLO-FP and FAST-FP because both protocols are similar to what is experienced during a game.
We initially hypothesized that the FAST-FP would create greater changes on the lower extremity biomechanics because of its functional drills performed at high intensity. However, the SLO-FP with moderate intensity produced similar biomechanical adaptations in our participants. When ACL injury-prevention programs are developed, feedback on proper mechanics should be stressed early because fatigue-related lower extremity modifications occur in as few as 5 minutes of intense multidirectional movements. Both fatigue protocols appear to be anaerobic; that is, the participants were at or above their anaerobic threshold at the end of both. Furthermore, the finding that the most severe neuromuscular changes, which include increased hip abduction, increased knee internal rotation, and increased internal knee adduction moment, occurred after 5 minutes of exercise (FAST-FP) when compared with 45 minutes of exercise (SLO-FP) is clinically relevant. A 5-minute fatigue protocol similar to the FAST-FP could be used to induce fatigue. A quick and effective screening process similar to the Landing Error Scoring System45 could be implemented to analyze lower extremity biomechanics in a fatigued state. This tool could be used to identify lower extremity movement patterns that place people at high or low risk for ACL injury. This would be an inexpensive and efficient process to determine which risk factors are modified during fatigue conditions and, therefore, which areas should be the focus of an ACL injury-prevention program. Individualized prevention programs that consider specific neuromechanical characteristics with and without fatigue should be developed. This would allow people to adjust their specific risk factors in an unfatigued state. The same prevention program would be completed again near the end of practice, when participants are fatigued. Each participant would be given proper feedback on how to improve her previously identified neuromechanical risk factors. Therefore, this instruction could carry over to game situations that take place during fatigued states.
CONCLUSIONS
One of our main outcomes was the similarity of the 2 fatigue protocols. Both demonstrated that when fatigue and unanticipated movement are combined, the lower extremity is at a higher risk for sustaining injury. Similar lower extremity bio-mechanical modifications occurred after 5 minutes of fatigue with the FAST-FP and after 45 minutes of fatigue with the SLO-FP. Altered lower extremity biomechanical movement patterns are known risk factors for ACL injury. Our results indicated that fatigue, regardless of type, makes these biomechanical risk factors more pronounced. Therefore, ACL injury-prevention programs should be designed to prevent the detrimental effects of fatigue. To accomplish this, people need to be trained and instructed on proper mechanics while in a fatigued state. During this fatigued state, feedback on proper mechanics should be given early and often and should be continued throughout the injury-prevention program. We found fatigue-induced decreases in hip and knee flexion, resulting in a more extended landing posture. Landing in a more extended position is thought to increase anterior tibial translation and thus increase the strain placed on the ACL. The FAST-FP produced increases in hip abduction, internal knee adduction moment, and knee internal rotation, all of which are either a cause or result of increased valgus loading on the knee joint.
REFERENCES
- 1.Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in National Collegiate Athletic Association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33(4):524–530. doi: 10.1177/0363546504269937. [DOI] [PubMed] [Google Scholar]
- 2.Mihata LC, Beutler AI, Boden BP. Comparing the incidence of anterior cruciate ligament injury in collegiate lacrosse, soccer, and basketball players: implications for anterior cruciate ligament mechanism and prevention. Am J Sports Med. 2006;34(6):899–904. doi: 10.1177/0363546505285582. [DOI] [PubMed] [Google Scholar]
- 3.Mountcastle SB, Posner M, Kragh JF, Jr, Taylor DC. Gender differences in anterior cruciate ligament injury vary with activity: epidemiology of anterior cruciate ligament injuries in a young, athletic population. Am J Sports Med. 2007;35(10):1635–1642. doi: 10.1177/0363546507302917. [DOI] [PubMed] [Google Scholar]
- 4.Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31(6):831–842. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 5.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(1):311–319. [PMC free article] [PubMed] [Google Scholar]
- 6.Maletius W, Messner K. Eighteen- to twenty-four-year follow-up after complete rupture of the anterior cruciate ligament. Am J Sports Med. 1999;27(6):711–717. doi: 10.1177/03635465990270060501. [DOI] [PubMed] [Google Scholar]
- 7.Yu B, Garrett WE. Mechanisms of non-contact ACL injuries. Br J Sports Med. 2007;41(suppl 1):i47–i51. doi: 10.1136/bjsm.2007.037192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Griffin LY, Agel J, Albohm MJ. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150. doi: 10.5435/00124635-200005000-00001. et al. [DOI] [PubMed] [Google Scholar]
- 9.Schulz BW, Ashton-Miller JA, Alexander NB. The effects of age and step length on joint kinematics and kinetics of large out-and-back steps. Clin Biomech (Bristol, Avon) 2008;23(5):609–618. doi: 10.1016/j.clinbiomech.2008.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech (Bristol, Avon) 2001;16(5):438–445. doi: 10.1016/s0268-0033(01)00019-5. [DOI] [PubMed] [Google Scholar]
- 11.Borotikar BS, Newcomer R, Koppes R, McLean SG. Combined effects of fatigue and decision making on female lower limb landing postures: central and peripheral contributions to ACL injury risk. Clin Biomech (Bristol, Avon) 2008;23(1):81–92. doi: 10.1016/j.clinbiomech.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 12.Chappell JD, Herman DC, Knight BS, Kirkendall DT, Garrett WE, Yu B. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2005;33(7):1022–1029. doi: 10.1177/0363546504273047. [DOI] [PubMed] [Google Scholar]
- 13.McLean SG, Fellin RE, Suedekum N, Calabrese G, Passerallo A, Joy S. Impact of fatigue on gender-based high-risk landing strategies. Med Sci Sports Exerc. 2007;39(3):502–514. doi: 10.1249/mss.0b013e3180d47f0. [DOI] [PubMed] [Google Scholar]
- 14.Sanna G, O'Connor KM. Fatigue-related changes in stance leg mechanics during sidestep cutting maneuvers. Clin Biomech (Bristol, Avon) 2008;23(7):946–954. doi: 10.1016/j.clinbiomech.2008.03.065. [DOI] [PubMed] [Google Scholar]
- 15.Besier TF, Lloyd DG, Ackland TR, Cochrane JL. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33(7):1176–1181. doi: 10.1097/00005768-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 17.Hewett TE, Myer GD, Ford KR. Reducing knee and anterior cruciate ligament injuries among female athletes: a systematic review of neuromuscular training interventions. J Knee Surg. 2005;18(1):82–88. doi: 10.1055/s-0030-1248163. [DOI] [PubMed] [Google Scholar]
- 18.Liederbach M, Dilgen FE, Rose DJ. Incidence of anterior cruciate ligament injuries among elite ballet and modern dancers: a 5-year prospective study. Am J Sports Med. 2008;36(9):1779–1788. doi: 10.1177/0363546508323644. [DOI] [PubMed] [Google Scholar]
- 19.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 20.McLean SG, Samorezov JE. Fatigue-induced ACL injury risk stems from a degradation in central control. Med Sci Sports Exerc. 2009;41(8):1661–1672. doi: 10.1249/MSS.0b013e31819ca07b. [DOI] [PubMed] [Google Scholar]
- 21.Kernozek TW, Torry MR, Iwasaki M. Gender differences in lower extremity landing mechanics caused by neuromuscular fatigue. Am J Sports Med. 2008;36(3):554–565. doi: 10.1177/0363546507308934. [DOI] [PubMed] [Google Scholar]
- 22.Chappell JD, Creighton RA, Giuliani C, Yu B, Garrett WE. Kinematics and electromyography of landing preparation in vertical stop-jump: risks for noncontact anterior cruciate ligament injury. Am J Sports Med. 2007;35(1):235–241. doi: 10.1177/0363546506294077. [DOI] [PubMed] [Google Scholar]
- 23.McLean SG, Huang X, van den Bogert AT. Investigating isolated neuromuscular control contributions to non-contact anterior cruciate ligament injury risk via computer simulation methods. Clin Biomech (Bristol, Avon) 2008;23(7):926–936. doi: 10.1016/j.clinbiomech.2008.03.072. [DOI] [PubMed] [Google Scholar]
- 24.Melnyk M, Gollhofer A. Submaximal fatigue of the hamstrings impairs specific reflex components and knee stability. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):525–532. doi: 10.1007/s00167-006-0226-3. [DOI] [PubMed] [Google Scholar]
- 25.Gehring D, Melnyk M, Gollhofer A. Gender and fatigue have influence on knee joint control strategies during landing. Clin Biomech (Bristol, Avon). 2009;24(1):82–87. doi: 10.1016/j.clinbiomech.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 26.McLean SG, Borotikar B, Lucey SM. Lower limb muscle pre-motor time measures during a choice reaction task associate with knee abduction loads during dynamic single leg landings. Clin Biomech (Bristol, Avon). 2010;25(6):563–569. doi: 10.1016/j.clinbiomech.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 27.Begon M, Monnet T, Lacouture P. Effects of movement for estimating the hip joint centre. Gait Posture. 2007;25(3):353–359. doi: 10.1016/j.gaitpost.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Schwartz MH, Rozumalski A. A new method for estimating joint parameters from motion data. J Biomech. 2005;38(1):107–116. doi: 10.1016/j.jbiomech.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 29.Cortes N, Blount E, Ringleb S, Onate JA. Soccer-specific video simulation for improving movement assessment. Sports Biomech. 2011;10(1):22–34. doi: 10.1080/14763141.2010.547591. [DOI] [PubMed] [Google Scholar]
- 30.Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Neuromuscular and lower limb biomechanical differences exist between male and female elite adolescent soccer players during an unanticipated run and crosscut maneuver. Am J Sports Med. 2007;35(11):1901–1911. doi: 10.1177/0363546507307400. [DOI] [PubMed] [Google Scholar]
- 31.Flouris AD, Koutedakis Y, Nevill A, Metsios GS, Tsiotra G, Parasiris Y. Enhancing specificity in proxy-design for the assessment of bioenergetics. J Sci Med Sport. 2004;7(1):197–204. doi: 10.1016/s1440-2440(04)80009-4. [DOI] [PubMed] [Google Scholar]
- 32.Metsios GS, Flouris AD, Koutedakis Y, Theodorakis Y. The effect of performance feedback on cardiorespiratory fitness field tests. J Sci Med Sport. 2006;9(3):263–266. doi: 10.1016/j.jsams.2006.03.027. [DOI] [PubMed] [Google Scholar]
- 33.Hughes G, Watkins J. A risk-factor model for anterior cruciate ligament injury. Sports Med. 2006;36(5):411–428. doi: 10.2165/00007256-200636050-00004. [DOI] [PubMed] [Google Scholar]
- 34.Blackburn JT, Padua DA. Sagittal-plane trunk position, landing forces, and quadriceps electromyographic activity. J Athl Train. 2009;44(1):174–179. doi: 10.4085/1062-6050-44.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pandy MG, Shelburne KB. Dependence of cruciate-ligament loading on muscle forces and external load. J Biomech. 1997;30(10):1015–1024. doi: 10.1016/s0021-9290(97)00070-5. [DOI] [PubMed] [Google Scholar]
- 36.MacDonald SW, Hultsch DF, Dixon RA. Performance variability is related to change in cognition: evidence from the Victoria Longitudinal Study. Psychol Aging. 2003;18(3):510–523. doi: 10.1037/0882-7974.18.3.510. [DOI] [PubMed] [Google Scholar]
- 37.Yu B, Lin CF, Garrett WE. Lower extremity biomechanics during the landing of a stop-jump task. Clin Biomech (Bristol, Avon). 2006;21(3):297–305. doi: 10.1016/j.clinbiomech.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 38.Cerulli G, Benoit DL, Lamontagne M, Caraffa A, Liti A. In vivo anterior cruciate ligament strain behaviour during a rapid deceleration movement: case report. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):307–311. doi: 10.1007/s00167-003-0403-6. [DOI] [PubMed] [Google Scholar]
- 39.Hirokawa S, Solomonow M, Lu Y, Lou ZP, D'Ambrosia R. Anterior-posterior and rotational displacement of the tibia elicited by quadriceps contraction. Am J Sports Med. 1992;20(3):299–306. doi: 10.1177/036354659202000311. [DOI] [PubMed] [Google Scholar]
- 40.Decker MJ, Torry MR, Wyland DJ, Sterett WI, Steadman JR. Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech (Bristol, Avon). 2003;18(7):662–669. doi: 10.1016/s0268-0033(03)00090-1. [DOI] [PubMed] [Google Scholar]
- 41.McNair PJ, Hewson DJ, Dombroski E, Stanley SN. Stiffness and passive peak force changes at the ankle joint: the effect of different joint angular velocities. Clin Biomech (Bristol, Avon). 2002;17(7):536–540. doi: 10.1016/s0268-0033(02)00062-1. [DOI] [PubMed] [Google Scholar]
- 42.Baca A. A comparison of methods for analyzing drop jump performance. Med Sci Sports Exerc. 1999;31(3):437–442. doi: 10.1097/00005768-199903000-00013. [DOI] [PubMed] [Google Scholar]
- 43.Chappell JD, Yu B, Kirkendall DT, Garrett WE. A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med. 2002;30(1):261–267. doi: 10.1177/03635465020300021901. [DOI] [PubMed] [Google Scholar]
- 44.Krustrup P, Mohr M, Ellingsgaard H, Bangsbo J. Physical demands during an elite female soccer game: importance of training status. Med Sci Sports Exerc. 2005;37(7):1242–1248. doi: 10.1249/01.mss.0000170062.73981.94. [DOI] [PubMed] [Google Scholar]
- 45.Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE, Jr, Beutler AI. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: the JUMP-ACL study. Am J Sports Med. 2009;37(10):1996–2002. doi: 10.1177/0363546509343200. [DOI] [PubMed] [Google Scholar]


