Abstract
Context:
The reliability of clinical techniques to quantify thoracic spine rotation range of motion (ROM) has not been evaluated.
Objective:
To determine the intratester and intertester reliability of 5 thoracic rotation measurement techniques.
Design:
Descriptive laboratory study.
Setting:
University research laboratory.
Patients or Other Participants:
Forty-six healthy volunteers (age = 23.6±4.3 years, height = 171.0±9.6 cm, mass = 71.4 ±16.7 kg).
Main Outcome Measure(s):
We tested 5 thoracic rotation ROM techniques over 2 days: seated rotation (bar in back and front), half-kneeling rotation (bar in back and front), and lumbar-locked rotation. On day 1, 2 examiners obtained 2 sets of measurements (sessions 1, 2) to determine the within-session intertester reliability and within-day intratester reliability. A single examiner obtained measurements on day 2 (session 3) to determine the intratester reliability between days. Each technique was performed 3 times per side, and averages were used for data analysis. Reliability was determined using intraclass correlation coefficients, standard error of measurement (SEM), and minimal detectable change (MDC). Differences between raters during session 1 were determined using paired t tests.
Results:
Within-session intertester reliability estimates ranged from 0.85 to 0.94. Ranges for the SEM were 1.0° to 2.3° and for the MDC were 2.8° to 6.3°. No differences were seen between examiners during session 1 for seated rotation (bar in front, both sides), half-kneeling rotation (bar in front, left side), or the lumbar locked position (both sides) (all values of P > .05). Within-day intratester reliability estimates ranged from 0.86 to 0.95. Ranges for the SEM were 0.8° to 2.1° and for the MDC were 2.1 ° to 5. 9°. Between-days intratester reliability estimates ranged from 0.84 to 0.91. Ranges for the SEM were 1.4° to 2.0° and for the MDC were 3.9° to 5.6°.
Conclusions:
All techniques had good reliability and low levels of measurement error. The seated rotation, bar in front, and lumbar-locked rotation tests may be used reliably when more than 1 examiner is obtaining measurements.
Keywords: biomechanics, bubble inclinometer, goniometer, scapulothoracic joint
Key Points.
Within-session and between-sessions reliability values for the 2 examiners for each of the 5 thoracic rotation range-of-motion measurement techniques were good.
All measurement techniques showed low SEM (< 3°) and minimal detectable change (< 6°) values for all techniques.
The seated rotation, bar in front, and lumbar-locked rotation tests did not display differences between examiners during session 1. These techniques may be used with confidence by clinicians and researchers.
For the clinician tracking rehabilitation improvements or performance-enhancement interventions in athletes whose sports have a large rotary component (eg, golf, rowing, baseball, gymnastics), it may be necessary to accurately quantify thoracic rotation range of motion (ROM). Accurate assessment of ROM is a fundamental aspect of both injury-evaluation and performance-enhancement screening programs and can help to identify necessary interventions. Additionally, changes in ROM can provide feedback about intervention effectiveness. Established clinical methods measure cervical1–4 and lumbar spine5–8 excursion in all 3 planes (flexion-extension, lateral flexion, and rotation). Clinical techniques have also been established to reliably measure thoracic spine flexion-extension9 and side bending.5 A variety of methods have been proposed to measure thoracic spine rotation,5,10–15 but the reliability of these measures has not been established. Although movement of the vertebrae may be more accurately measured using diagnostic imaging,16–18 this is not a plausible clinical method because of the cost and potential radiation exposure. Rotation has been measured by visual estimation11 and the use of a goniometer or inclinometer.10,14,15
Currently, the selection of clinical techniques to measure thoracic spine rotation ROM depends largely on clinician preference.10,11,14,15 Reliability has not been determined for these measures, which makes it difficult to know whether changes in ROM are caused by measurement error or actual treatment effects. Therefore, the purpose of our study was to identify the most reliable techniques to measure thoracic spine rotation in healthy adults. We selected healthy adults to establish preliminary measurement reliability for the selected measurement techniques.
METHODS
Design
This study involved a descriptive laboratory design. Participants performed 5 variations of thoracic rotation ROM on both the right and left sides. The main outcome measure, ROM (in degrees), was obtained in 5 testing positions: seated rotation test (bar in back), seated rotation test (bar in front), half-kneeling rotation test (bar in back), half-kneeling rotation test (bar in front), and lumbar-locked rotation test. These testing positions were selected because they have been described in previous articles5,10–15 and are commonly used in clinical settings. Two examiners independently obtained measurements twice during the first day (sessions 1, 2), and 1 examiner obtained a third measurement during a follow-up 48 to 72 hours later (session 3).
Participants
Forty-six healthy volunteers (15 men, 31 women: age=23.6± 4.3 years, height=171.0±9.6 cm, mass=71.4± 16.7 kg) participated in this study. Participants were recruited from the university and surrounding community and were eligible if they were healthy adults between 18 and 45 years old. Exclusion criteria were any pathologic condition of the spine, rib, shoulder, hip, or knee within the past 6 months; a history of scoliosis or the presence of spinal hardware; a rheumatologic or respiratory condition at the time of the study; and any chance of pregnancy. Before entering the study, all volunteers signed an informed consent form that was approved by the institutional review board at the university, which also approved the study. Volunteers were screened for inclusion and exclusion criteria using a health history questionnaire.
Examiners
Two examiners (both certified athletic trainers) obtained thoracic rotation ROM measurements but were blinded to goniometer and inclinometer readings. The examiners were blinded to goniometer measurements with the use of a piece of paper to cover the numbers associated with the axis of the goniometer; blinding for the inclinometer was accomplished by having the examiner face away from the numbers on the inclinometer. The third examiner recorded the goniometer or inclinometer angle obtained during each trial. Training for the examiners consisted of practice with measurement procedures, participant positioning, palpation of bony landmarks (T1 and T2 vertebral levels, spine of the scapula) and familiarization with the use of the goniometer and bubble inclinometer for measuring thoracic rotation.
Instrumentation
A standard 8-in (20-cm) clear plastic goniometer was used to measure both components (bar in back or front) of the seated and half-kneeling rotation tests. A fluid-filled bubble inclinometer (model Baseline Bubble; Fabrication Enterprises, Inc, White Plains, NY) was used to measure thoracic ROM during the lumbar-locked rotation test.
Procedures
After we obtained consent and health history information, we used a piece of athletic tape to mark the point on the spine between T1 and T2 that served as a reference point for ROM measurements. The T1 and T2 were identified by palpating inferiorly from C7. The T1-T2 level was selected because these segments have the greatest amount of motion19 and the greatest amount of excursion due to rotation of the caudal thoracic vertebral segments. Thoracic rotation ROM was measured using 5 measurement techniques: (1) seated rotation test (bar in back), (2) seated rotation test (bar in front), (3) half-kneeling rotation test (bar in back), (4) half-kneeling rotation test (bar in front), and (5) lumbar-locked rotation test.15 Each technique was performed 3 times per side, with the order of testing technique, side, and examiner counterbalanced using a Latin square. Both examiners independently obtained measurements twice during the first day (sessions 1, 2). Participants were given a 5-minute rest period between sessions 1 and 2. A third measurement session (session 3) was conducted by a single examiner 48 to 72 hours later (Figure 1). Specific criteria for each test are provided in subsequent paragraphs and have also been described in greater detail in a previous article.15
Figure 1.
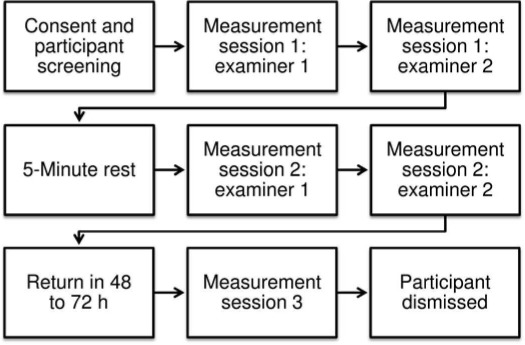
Flow chart of participant progression.
Seated Rotation Test.
The participant was seated, with hips and knees flexed to 90° and a ball (21-cm diameter) placed between the knees to minimize motion of the lower extremities during thoracic rotation. A 105-cm-long, 2.5-cm-diameter polyvinyl chloride pipe (bar), with a piece of tape marking the midpoint, was used to standardize the position of the upper extremity. In the bar-in-back position (Figure 2A), the bar was placed across the back, at approximately the level of the inferior border of the scapulae. The elbows were placed behind the bar and the hands across the stomach; interlocking of the fingers was not necessary. The bar-in-front position was performed with a bar placed across the chest and the arms crossed over the bar (Figure 2B). In both positions, the goniometer was aligned parallel to the ground at the midpoint between the T1 and T2 spinous processes, with the spine of the scapula as a reference point. The stationary arm was pointed away from the rotating side and remained parallel to the starting position. The participant was instructed to continue looking forward at an eye-level mark on the wall while maximally rotating to one side. The examiner followed this motion with the moving arm of the goniometer (Figure 3). Once the participant reached end range, the angle of the goniometer was maintained, and another examiner read and recorded the measurement. Each measurement was obtained 3 times on both the right and left sides.
Figure 2.
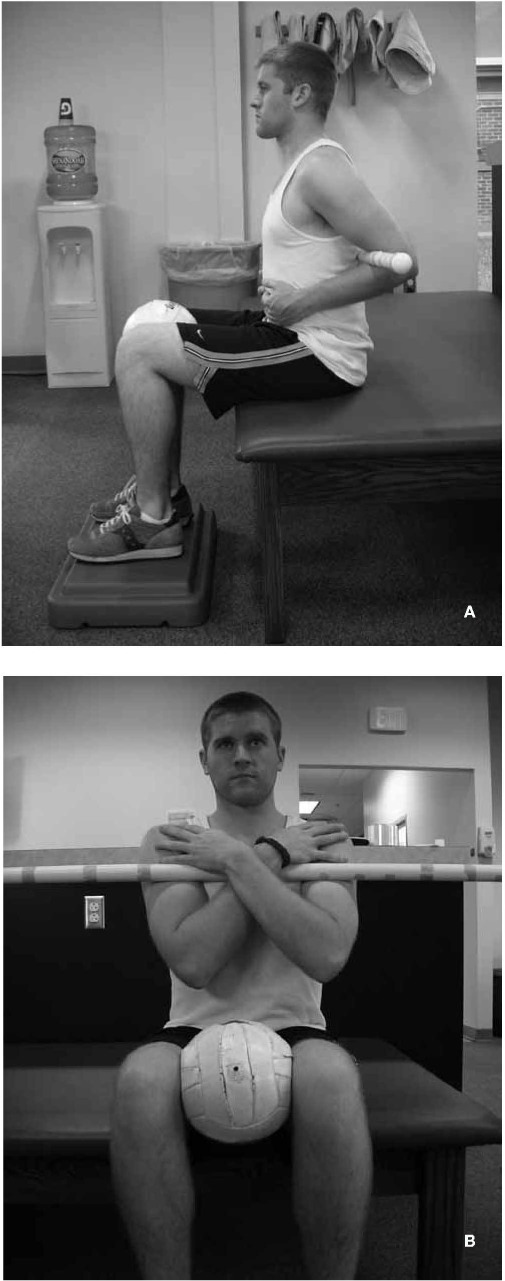
Seated rotation test. The hips and knees are at 90° with a ball placed between the knees. A, Bar-in-back position with the bar behind the back and hands resting on the stomach. B, Bar-in-front position with arms crossed over the bar and in front of the chest.
Figure 3.

Goniometer placement. The goniometer is placed parallel to the ground at the level of T1-T2, using the spine of the scapula as a reference point. (Right rotation is shown.) The stationary arm is pointed away from the rotating side and remains parallel to the starting position. The mobile arm follows the rotary motion of the thoracic spine and remains parallel to the spine of the scapula.
Half-Kneeling Rotation Test.
The participant was placed in the half-kneeling (lunge) position (Figure 4A). Bar position (back and front) and goniometer alignment and measurement techniques were identical to those in the seated rotation test. The direction of rotation was dictated by the forward leg of the lunge (ie, left leg forward, rotation to the left; Figure 4B). Each measurement was obtained 3 times on both the right and left sides.
Figure 4.
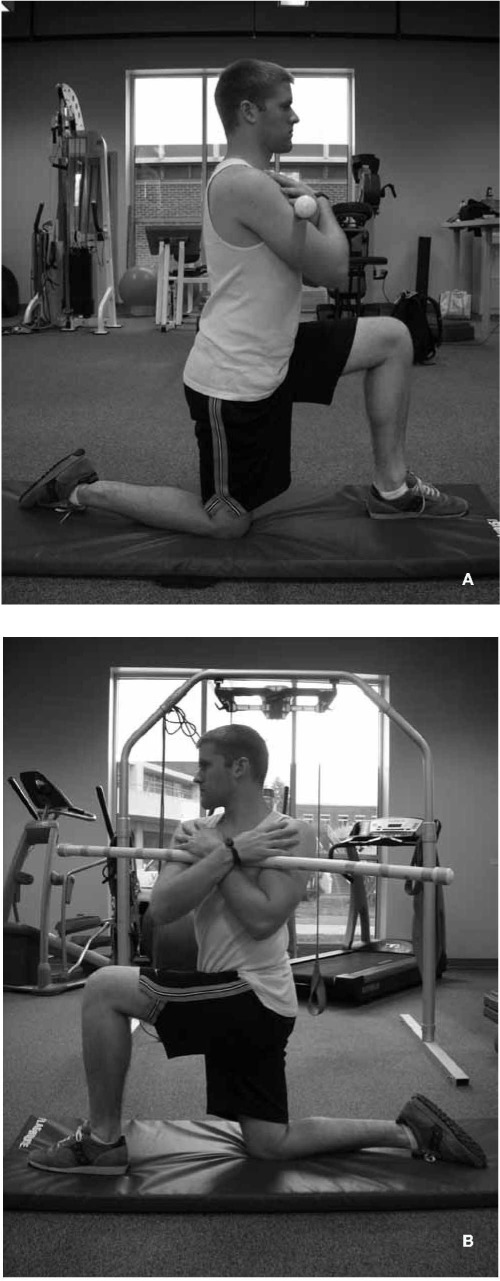
Half-kneeling rotation test. The hip and knee are flexed to 90°, and the forward foot is in line with the knee. A, Starting position for left rotation (left leg forward). B, The participant is asked to rotate toward the forward leg (left rotation).
Lumbar-Locked Rotation Test.
The participant was in the quadruped position (Figure 5A) and maintaining upper extremity support with the elbows and forearms. This position was thought to place the hips and lumbar spine into maximal flexion, reducing the contributions of the pelvis and lumbar spine during thoracic rotation. The bubble inclinometer was positioned between the scapular spines at the T1-T2 level. Rotation was performed with the participant placing the ipsilateral hand on the posterior aspect of the neck and rotating the thoracic spine while maintaining the kneeling position (Figure 5B). Once the participant reached end range, the angle of the inclinometer was maintained, and a separate examiner read and recorded the measurement. Each measurement was obtained 3 times on both the right and left sides.
Figure 5.
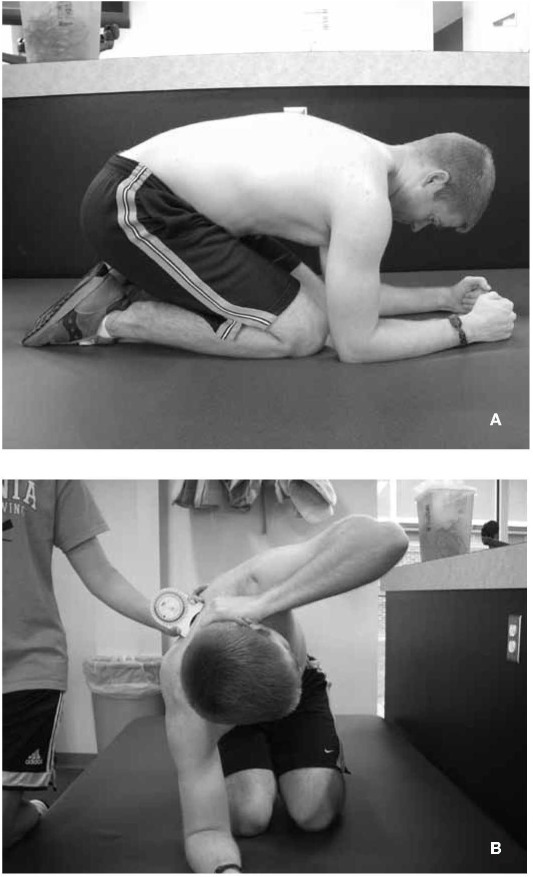
Lumbar-locked rotation test. A, Starting position with the shoulders and elbows at 90°, participant sitting back on heels as far as possible, and neck in neutral position. B, Left rotation; right forearm remains in contact with the ground while the neck remains in a neutral position.
Criteria for Failed Trials.
In the seated rotation test position (bar in front and back), if the participant was unable to maintain knees and feet together, forward gaze with head and neck, upright posture, contact with the bar, or the bar parallel to the ground, the trial was considered a failure. Similar to the seated rotation test position, the half-kneeling rotation test position required monitoring of knee and feet shifting during rotation, head and neck rotation, contact of the bar, hip level, and bar angle. Lumbar-locked rotation test failure criteria were inability to maintain maximum hip flexion (sitting on heels) during motion, a change in elbow angle, inability to keep the contralateral forearm on the floor during rotation, and inability to keep the hand on the back of the neck while rotating.
Statistical Analysis
The mean for each session (position and side) was used for data analysis. Reliability was determined using an intraclass correlation coefficient (ICC) and associated 95% confidence intervals (CIs). Calculations were also made for the standard error of measurement (SEM; SEM=SD√1–ICC)20 and the minimal detectable change (MDC; MDC=SEM * 1.96* √2).20 The SEM was calculated to determine measurement error, and the MDC was calculated to determine the minimum threshold of measurement to ensure that differences between measurements were real and outside the error range. Alternatively stated, the SEM provides an “absolute index of reliability”20 or “typical error”21 associated with a measurement. The MDC incorporates the SEM but provides clinicians and researchers with an index of differences between measurements that can be considered real and not due to measurement variability.20 Intertester reliability (ICC [2,3]) and intratester reliability (ICC [2,3]) were calculated for both the right and left sides for each measurement technique. Initial assessment data were used to determine within-session (session 1) intertester reliability. Differences between raters during session 1 were determined using paired t tests. Data from the second session (session 2) during day 1 and the follow-up data obtained 48 to 72 hours after the initial assessment (session 3) were used to calculate the within-day and between-days intratester reliability. Criteria ranges for reliability were as follows: <0.50, poor; 0.50 to 0.75, moderate; and >0.75, good.22 Statistical analyses were performed with SPSS (version 17.0; SPSS Inc, Chicago, IL).
Results
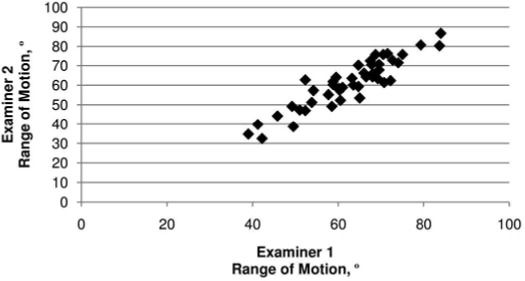
Session 1 means and standard deviations for both examiners for each of the 5 techniques are presented in Table 1. The lumbar-locked position (40.8° ± 10.7°) produced the smallest ROM value; the greatest amount of motion occurred in the half-kneeling rotation (bar-in-front) position (60.6° ± 10.8°). Means and standard deviations for thoracic spine rotation ROM measurements by examiner, session, and side are shown in Table 2. Scatterplots (Figures 6–10) were constructed for each of the 5 measurement techniques using data (average of right and left sides) obtained from both examiners during session 1. All participants were able to complete testing in all positions.
Table 1.
Thoracic Spine Range-of-Motion Measurements Obtained on Day 1, °
| Test | Mean ± SDa |
| Seated rotation, bar in back | 41.6±8.7 |
| Seated rotation, bar in front | 55.4±9.2 |
| Half-kneeling rotation, bar in back | 48.2±10.7 |
| Half-kneeling rotation, bar in front | 60.6±10.8 |
| Lumbar-locked rotation | 40.8±10.7 |
aAverages were determined using data from both examiners and each side (right and left) during sessions 1 and 2.
Table 2.
Thoracic Spine Range-of-Motion Measurements by Side, Examiner, and Session, ° (Mean±SD)
| Test | Side | Examiner 1 |
Examiner 2 |
Session 1 P Value | |||
| Session 1 | Session 2 | Session 3 | Session 1 | Session 2 | |||
| Seated rotation, bar in back | |||||||
| Right | 45.4±10.0 | 43.0±9.6 | 45.4±8.2 | 39.3±10.4a | 36.8±9.9 | <.001 | |
| Left | 47.2±9.1 | 43.6±8.4 | 45.9±8.7 | 40.2±10.9a | 37.7±9.8 | <.001 | |
| Average | 46.2±9.1 | 43.3±8.5 | 45.6±7.6 | 39.7±10.0a | 37.3±9.2 | <.001 | |
| Seated rotation, bar in front | |||||||
| Right | 56.7±9.3 | 54.4±10.5 | 57.0±8.7 | 55.2±10.7 | 53.4±11.0 | .16 | |
| Left | 56.7±9.4 | 53.7±9.0 | 56.1 ±8.4 | 57.64±11.4 | 55.28±11.1 | .38 | |
| Average | 56.7±9.0 | 54.0±9.1 | 56.6±8.0 | 56.44±10.6 | 54.32±10.7 | .78 | |
| Half-kneeling rotation, bar in back | |||||||
| Right | 53.1±11.4 | 51.0±10.9 | 51.7±11.1 | 45.7±11.7a | 44.4±13.2 | <.001 | |
| Left | 51.7±10.6 | 49.5±10.0 | 51.6±9.8 | 46.3±13.6a | 44.1±12.3 | <.001 | |
| Average | 52.4±10.6 | 50.3±10.1 | 51.6±10.2 | 46.0±12.1a | 44.2±12.1 | <.001 | |
| Half-kneeling rotation, bar in front | |||||||
| Right | 63.7±11.5 | 60.6±11.1 | 63.6±10.4 | 61.0±12.4a | 58.9±12.3 | .002 | |
| Left | 61.9±10.0 | 58.7±10.7 | 60.6±11.0 | 61.6±13.2 | 58.5±12.8 | .74 | |
| Average | 62.8±10.4 | 59.6±10.3 | 62.1±10.2 | 61.3±12.3a | 58.7±12.1 | .04 | |
| Lumbar-locked rotation | |||||||
| Right | 41.1±14.6 | 39.0±13.6 | 45.7±14.3 | 39.5±11.2 | 39.0±12.7 | .23 | |
| Left | 43.9±12.9 | 40.4±10.3 | 46.4±12.2 | 42.0±10.6 | 41.2±10.1 | .11 | |
| Average | 42.5±13.2 | 39.7±11.4 | 46.0±12.8 | 40.8±10.3 | 40.1±10.9 | .09 | |
aSignificant difference between examiners during session 1 measurements (P<.05).
Figure 6.
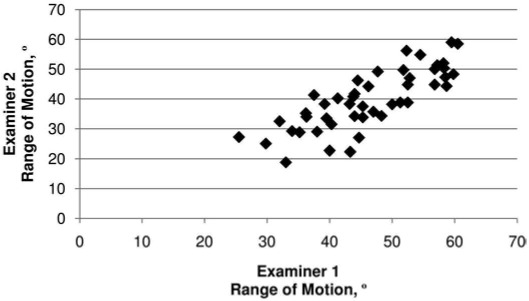
Scatterplot for data from the seated rotation test with bar in the back.
Figure 7.
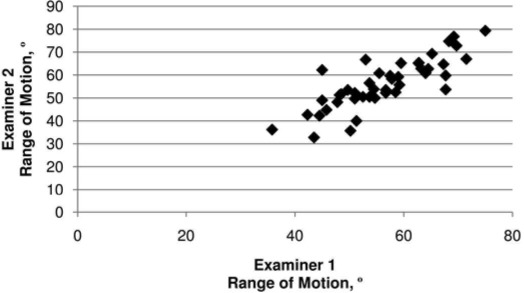
Scatterplot for data from the seated rotation test with bar in the front.
Figure 8.
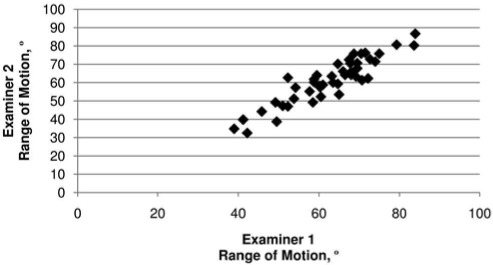
Scatterplot for data from the half-kneeling rotation test with bar in the back.
Figure 9.
Scatterplot for data from the half-kneeling rotation test with bar in the front.
Figure 10.
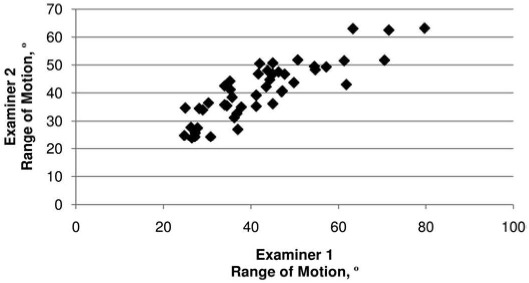
Scatterplot for data from the lumbar-locked rotation test.
The within-session intertester reliability estimates ranged from 0.85 to 0.94 (Table 3). The SEM ranged from 1.0° to 2.3°, and the MDC ranged from 2.8° to 6.3°. Differences were noted between examiners for measurements obtained during session 1 (Table 2). Specifically examiner 1's ROM values were approximately 4° to 8° higher for the seated rotation test (bar in back, both right and left sides) and the half-kneeling rotation test (bar in back, both right and left sides, and bar in front, right side). Values for the seated rotation test (bar in front) and lumbar-locked rotation tests were not different between examiners during session 1.
Table 3.
Within-Session Intertester Reliability (ICC [2,3]) and Measurement Error for Thoracic Spine Range-of-Motion Measurements
| Test | Right Side |
Left Side |
||||
| ICC (95% Confidence Interval) | Standard Error of Measurement, ° | Minimal Detectable Change, ° | ICC (95% Confidence Interval) | Standard Error of Measurement, ° | Minimal Detectable Change, ° | |
| Seated rotation, bar in back | 0.85 (0.73, 0.92) | 2.03 | 5.61 | 0.85 (0.73, 0.92) | 1.96 | 5.42 |
| Seated rotation, bar in front | 0.87 (0.77, 0.93) | 1.72 | 4.77 | 0.87 (0.76, 0.93) | 1.82 | 5.05 |
| Half-kneeling rotation, bar in back | 0.92 (0.86, 0.96) | 1.26 | 3.49 | 0.89 (0.80, 0.94) | 1.79 | 4.97 |
| Half-kneeling rotation, bar in front | 0.94 (0.89, 0.97) | 1.03 | 2.84 | 0.91 (0.83, 0.95) | 1.49 | 4.13 |
| Lumbar-locked rotation | 0.87 (0.77, 0.93) | 2.25 | 6.25 | 0.87 (0.77, 0.93) | 2.00 | 5.54 |
Abbreviation: ICC, intraclass correlation coefficient.
The within-day intratester reliability estimates ranged from 0.86 to 0.95 (Table 4); the SEMs ranged from 0.8° to 2.1°, and the MDCs ranged from 2.1° to 5.9°. The between-days intratester reliability estimates ranged from 0.84 to 0.91 (Table 5); the SEMs ranged from 1.4° to 2.0°, and the MDCs ranged from 3.9° to 5.6°.
Table 4.
Within-Day Intratester Reliability (ICC [2,3]) and Measurement Error for Thoracic Spine Range-of-Motion Measurements
| Test | Right Side |
Left Side |
||||
| ICC (95% Confidence Interval) | Standard Error of Measurement, ° | Minimal Detectable Change, ° | ICC (95% Confidence Interval) | Standard Error of Measurement, ° | Minimal Detectable Change, ° | |
| Seated rotation, bar in back | 0.94 (0.90, 0.97) | 0.76 | 2.10 | 0.90 (0.81, 0.94) | 1.21 | 3.37 |
| Seated rotation, bar in front | 0.87 (0.76, 0.93) | 1.74 | 4.83 | 0.91 (0.84, 0.95) | 1.12 | 3.10 |
| Half-kneeling rotation, bar in back | 0.95 (0.91, 0.97) | 0.78 | 2.16 | 0.94 (0.90, 0.97) | 0.81 | 2.24 |
| Half-kneeling rotation, bar in front | 0.92 (0.86, 0.96) | 1.18 | 3.27 | 0.90 (0.82, 0.95) | 1.38 | 3.82 |
| Lumbar-locked rotation | 0.90 (0.81, 0.94) | 2.00 | 5.53 | 0.86 (0.75, 0.92) | 2.12 | 5.89 |
Abbreviation: ICC, intraclass correlation coefficient.
Table 5.
Between-Days Intratester Reliability (ICC [2,3]) and Measurement Error for Thoracic Spine Range-of-Motion Measurements
| Test | Right Side |
Left Side |
||||
| ICC (95% Confidence Interval) | Standard Error of Measurement, ° | Minimal Detectable Change, ° | ICC (95% Confidence Interval) | Standard Error of Measurement, ° | Minimal Detectable Change, ° | |
| Seated rotation, bar in back | 0.84 (0.70, 0.91) | 5.48 | 2.10 | 0.87 (0.76, 0.93) | 1.59 | 4.42 |
| Seated rotation, bar in front | 0.84 (0.72, 0.91) | 5.15 | 4.83 | 0.87 (0.76, 0.93) | 1.60 | 4.43 |
| Half-kneeling rotation, bar in back | 0.91 (0.84, 0.95) | 3.85 | 2.16 | 0.90 (0.82, 0.94) | 1.40 | 3.88 |
| Half-kneeling rotation, bar in front | 0.88 (0.77, 0.93) | 5.09 | 3.27 | 0.87 (0.76, 0.93) | 1.89 | 5.24 |
| Lumbar-locked rotation | 0.90 (0.83, 0.95) | 5.23 | 5.53 | 0.88 (0.78, 0.93) | 2.01 | 5.56 |
Abbreviation: ICC, intraclass correlation coefficient.
Discussion
The purpose of our study was to determine the reliability of 5 thoracic rotation ROM measurement techniques. The thoracic spine rotation ROM values (Table 1) we obtained were similar to previously reported normative values.12,23 These findings indicate that the proposed techniques are reliable methods for measuring thoracic rotation in the seated, half-kneeling, and lumbar-locked positions. All intratester and intertester ICC values were greater than 0.85, which can be described as good.22 Additionally, all techniques had low measurement error (SEMs less than 3° and MDC values less than 6°).
Despite good reliability values, differences were seen between examiners during session 1 for the seated rotation test (bar in back, both right and left sides) and the half-kneeling rotation test (bar in back, both right and left sides, and bar in front, right side). Examiner l's values were approximately 4° to 8° higher for measures obtained with the bar in back. It is possible that systematic error was present for one of the examiners. Only the values for the seated rotation test with the bar in front and the lumbar-locked rotation test were not different between examiners during session 1. Both examiners underwent a brief training session to ensure standardization of the measurement techniques, and both examiners were certified athletic trainers with less than 3 years of clinical experience. Whether more experienced raters would obtain consistent measurement values within the same session is unknown. Despite the differences between examiners for values obtained during session 1, both examiners had good within-day intratester reliability, and examiner 1 had good between-days intratester reliability. Measurements for both examiners during sessions 2 and 3 were below the MDC for each technique. This indicates that any of the 5 techniques may be used if the same examiner (with good intrarater reliability) obtains measures at all follow-up sessions. When other examiners are obtaining follow-up measures, the seated rotation test with the bar in front and the lumbar-locked rotation test may be the best choices.
Perceived advantages and disadvantages are associated with each method and may have also contributed to differences between raters during session 1. The bar-in-front variations of both the seated and half-kneeling test positions allowed easier visualization of anatomical landmarks such as the spine of the scapula. The seated rotation test (both bar in front and bar in back) may have provided greater stability for those who had difficulty maintaining balance in the half-kneeling position; however, some participants had difficulty keeping the ball between their knees. We did not determine whether this was caused by actual muscle weakness of the hip adductor muscles or possibly the inability to perform trunk rotation while maintaining a stable pelvis. During the seated rotation test with the bar in front, the combination of easier visualization of anatomical landmarks and greater stability may have contributed to the examiners obtaining similar values. The half-kneeling positions (both bar in front and bar in back) posed challenges for participants who had trouble maintaining balance; this was evident in the participant's wavering or shaking, which made measurement acquisition more difficult. The inability to maintain balance in this position may indicate a number of trunk or lower extremity impairments. Further examination by the clinician may be needed to determine the specific reason for the inability to complete testing in this position. The presence of any condition that precluded kneeling (eg, anterior knee pain) would also make this position problematic. Furthermore, verbal cuing from the examiner was often needed to minimize movement of the hip and pelvis during testing.
Although both the seated and half-kneeling test positions required multiple pieces of equipment (bar, ball, and goniometer) to obtain the measurement, the lumbar-locked position required only a bubble inclinometer. This factor, along with ease of position and speed of measurement recording capability, may have contributed to the similar values obtained by the examiners. Thus, this technique is a viable choice for clinicians who have restrictions on available equipment, times, and settings and when multiple people are obtaining measurements. Some participants were not able to sit all the way back on their heels in the lumbar-locked position, but they were able to maintain maximal hip flexion ROM (even if that did not involve reaching their heels). The lumbar-locked position may pose difficulties for people with hip or knee joint conditions (eg, osteoarthritis) that become painful at end range. Because the ROM values for each of the 5 techniques were similar, each technique may provide similar information about thoracic spine rotation ROM.
For some populations (eg, golfers, rowers, gymnasts, throwers, swimmers, other athletes whose sports entail repetitive rotation), the excursion of thoracic rotation may be an important variable to measure. The ability to reliably measure ROM within the same session and between days is important; clinicians can better monitor rehabilitation effectiveness when they are confident that changes are due to intervention and not measurement error. All measurement techniques showed low SEM (<3°) and MDC (<6°) values for all techniques, a finding that is consistent with other spine rotation ROM measurement techniques.2–4,24 Thus, changes in motion that are greater than 2° to 6° MDC (depending on technique) can be attributed to actual changes in motion and not to measurement error. As a result, the techniques can be used in clinical settings and intervention studies to document changes in thoracic spine rotation ROM.
A limitation of this study was that we examined healthy adults aged 18 to 45 years with no history of spinal conditions within the last 6 months. Therefore, our findings may not be generalized to people outside this age range or to people with spine injuries. Future authors should examine the reliability of these techniques in people with limitations in thoracic spine rotation ROM and thoracic spine injuries.
Radiographs, computed tomography scans, and ultrasound images have all been used to measure thoracic rotation16–18 and are thought to be valid methods of measuring spine motion.25 However, not only are these methods expensive, but they potentially pose risks to the participants (ie, radiation exposure). The validity of clinical measures of thoracic spine rotation ROM has not been established, and we were not able to definitively determine that all motion was isolated to the thoracic spine. Motion from adjacent joints (eg, scapulothoracic, lumbar, hip) may have contributed to the total rotation ROM measured. Measures of thoracic rotation with the bar-in-back position are believed to limit the contribution from the shoulder joints to spine rotation. The bar-in-front position tended to allow approximately 12° to 14° more rotation than the bar-in-back position (Table 1). The bar-in-back positions (seated and half kneeling) and the lumbar-locked rotation test are thought to best minimize the contribution of adjacent joints to total thoracic ROM. Although we were not able to specifically confirm that motion was occurring only at the thoracic spine, the values we obtained were consistent with previously reported normative thoracic spine rotation ROM values,12,23 thus indicating face validity of these measurement techniques. Future research on the validity of noninvasive measurement approaches is needed.
Another limitation of this study is that it was performed in a controlled laboratory setting with specific participant positioning and instrument placement. A follow-up period of 48 to 72 hours was selected to minimize the effects of uncontrolled factors (eg, exercise) on thoracic spine ROM. We cannot generalize our findings beyond 48 to 72 hours, but examiners were blinded to measurement values and order was counterbalanced, so the effects of multiple days between sessions on the ability to accurately obtain consistent measurements may be negligible.
CONCLUSIONS
Our results indicate that the 5 techniques can be measured reliably by the same clinician within a day and between days. The seated rotation test with the bar in front and the lumbar-locked rotation test produced values that were not different between examiners during session 1. These 2 techniques are recommended when 2 examiners are working with the same patient or participant. Measurements were taken in a standardized manner, and the results of these methods were consistent between the examiners. Additionally, the SEM and MDC scores were low for all techniques, indicating that changes in motion (MDC > 2° to 6°, depending on technique) can be consistently identified with these techniques.
REFERENCES
- 1.Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion: comparison of three methods. Phys Ther. 1991;71(1):98–104. doi: 10.1093/ptj/71.2.98. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther. 2008;38(10):640–645. doi: 10.2519/jospt.2008.2680. [DOI] [PubMed] [Google Scholar]
- 3.Audette I, Dumas JP, Cote JN, De Serres SJ. Validity and between-day reliability of the cervical range of motion (CROM) device. J Orthop Sports Phys Ther. 2010;40(5):318–323. doi: 10.2519/jospt.2010.3180. [DOI] [PubMed] [Google Scholar]
- 4.Prushansky T, Deryi O, Jabarreen B. Reproducibility and validity of digital inclinometry for measuring cervical range of motion in normal subjects. Physiother Res Int. 2010;15(1):42–48. doi: 10.1002/pri.443. [DOI] [PubMed] [Google Scholar]
- 5.Klein AB, Snyder-Mackler L, Roy SH, DeLuca CJ. Comparison of spinal mobility and isometric trunk extensor forces with electromyographic spectral analysis in identifying low back pain. Phys Ther. 1991;71(6):445–454. doi: 10.1093/ptj/71.6.445. [DOI] [PubMed] [Google Scholar]
- 6.Olson KA, Goehring MT. Intra and inter-rater reliability of a goniometric lower trunk rotation measurement. J Back Musculoskelet Rehabil. 2009;22(3):157–164. doi: 10.3233/BMR-2009-0229. [DOI] [PubMed] [Google Scholar]
- 7.Myers J, Shanks G, Watson T, Hudson D. Single inclinometer vs. double inclinometer measures of lumbar spine range of motion. Orthop Phys Ther Pract. 2009;21(4):146–148. [Google Scholar]
- 8.Kachingwe AF, Phillips BJ. Inter- and intrarater reliability of a back range of motion instrument. Arch Phys Med Rehabil. 2005;86(12):2347–2353. doi: 10.1016/j.apmr.2005.07.304. [DOI] [PubMed] [Google Scholar]
- 9.Mannion AF, Knecht K, Balaban G, Dvorak J, Grob D. A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: reliability of measurements and comparison with data reviewed from the literature. Eur Spine J. 2004;13(1):122–136. doi: 10.1007/s00586-003-0618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoogenboom BJ, Voight ML, Cook G, Gill L. Using rolling to develop neuromuscular control and coordination of the core and extremities of athletes. N Am J Sport Phys Ther. 2009;4(1):70–82. [PMC free article] [PubMed] [Google Scholar]
- 11.Burton L, Kiesel K, Cook G. Mobility screening for the core. Athl Ther Today. 2004;9(6):38–41. [Google Scholar]
- 12.Willems JM, Jull GA, Ng JF. An in vivo study of the primary and coupled rotations of the thoracic spine. Clin Biomech (Bristol, Avon) 1996;11(6):311–316. doi: 10.1016/0268-0033(96)00017-4. [DOI] [PubMed] [Google Scholar]
- 13.Schenkman M, Laub KC, Kuchibhatla M, Ray L, Shinberg M. Measures of shoulder protraction and thoracolumbar rotation. J Orthop Sports Phys Ther. 1997;25(5):329–335. doi: 10.2519/jospt.1997.25.5.329. [DOI] [PubMed] [Google Scholar]
- 14.Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. Philadelphia, PA: FA Davis; 1995. pp. 212–213. [Google Scholar]
- 15.Johnson KD, Grindstaff TL. Thoracic rotation measurement techniques: clinical commentary. N Am J Sport Phys Ther. 2010;5(4):252–256. [PMC free article] [PubMed] [Google Scholar]
- 16.Ho EK, Upadhyay SS, Ferris L. A comparative study of computed tomographic and plain radiographic methods to measure vertebral rotation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 1992;17(7):771–774. doi: 10.1097/00007632-199207000-00008. et al. [DOI] [PubMed] [Google Scholar]
- 17.Russell GG, Raso VJ, Hill D, McIvor J. A comparison of four computerized methods for measuring vertebral rotation. Spine (Phila Pa 1976). 1990;15(1):24–27. doi: 10.1097/00007632-199001000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Suzuki S, Yamamuro T, Shikata J, Shimizu K, Iida H. Ultrasound measurement of vertebral rotation in idiopathic scoliosis. J Bone Joint Surg Br. 1989;71(1):252–255. doi: 10.1302/0301-620X.71B2.2647754. [DOI] [PubMed] [Google Scholar]
- 19.White AA., III. Analysis of the mechanics of the thoracic spine in man: an experimental study of autopsy specimens. Acta Orthop Scand Suppl. 1969;127:1–105. doi: 10.3109/ort.1969.40.suppl-127.01. [DOI] [PubMed] [Google Scholar]
- 20.Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–240. doi: 10.1519/15184.1. [DOI] [PubMed] [Google Scholar]
- 21.Hopkins WG. Measures of reliability in sports medicine and science. Sports Med. 2000;30(1):1–15. doi: 10.2165/00007256-200030010-00001. [DOI] [PubMed] [Google Scholar]
- 22.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. Upper Saddle River, NJ: Prentice Hall Health; 1999. p. 565. [Google Scholar]
- 23.Magee DJ. Orthopedic Physical Assessment. 4th ed. Philadelphia, PA: WB Saunders; 2002. p. 440. [Google Scholar]
- 24.Heneghan NR, Hall A, Hollands M, Balanos GM. Stability and intra-tester reliability of an in vivo measurement of thoracic axial rotation using an innovative methodology. Man Ther. 2009;14(4):452–455. doi: 10.1016/j.math.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Loebl WY. Measurement of spinal posture and range of spinal movement. Ann Phys Med. 1967;9(3):103–110. doi: 10.1093/rheumatology/9.3.103. [DOI] [PubMed] [Google Scholar]


