Abstract
Context:
The female athlete triad describes the interrelatedness of energy availability, menstrual function, and bone density. Although associations between triad components and musculoskeletal injury (INJ) have been reported in collegiate athletes, limited information exists about menstrual irregularity (MI) and INJ in the high school population.
Objective:
To determine the prevalence of and relationship between MI and INJ in high school athletes.
Design:
Cross-sectional study.
Setting:
High schools.
Patients or Other Participants:
The sample consisted of 249 female athletes from 3 high schools who competed in 33 interscholastic, school-sponsored sport teams, dance teams, and cheerleading or pom-pon squad during the 2006–2007 school year. Each athlete remained on the roster throughout the season.
Main Outcome Measure(s):
Participants completed a survey regarding injury type, number of days of sport participation missed, and menstrual history in the past year.
Results:
The prevalences of MI and INJ were 19.7% and 63.1%, respectively. Athletes who reported MI sustained a higher percentage of severe injuries (missing ≥22 days of practice or competition) than did athletes who reported normal menses. Although the trend was not significant, athletes with MI were almost 3 times more likely to sustain an injury resulting in 7 or more days of time lost from sport (odds ratio = 2.7, 95% confidence interval = 0.8, 8.8) than those who sustained an injury resulting in 7 or fewer days of time lost.
Conclusions:
The incidences of MI and INJ in this high school population during the study period were high. Athletes who reported MI sustained a higher percentage of severe injuries than did athletes who reported normal menses. Education programs to increase knowledge and improve management of MI and its potential effects on injury in female high school athletes are warranted.
Keywords: female athlete triad, sports injuries, musculoskeletal disorders
Key Points.
The overall prevalence of menstrual irregularity was 19.7%; values were similar for athletes in different sport types.
The overall prevalence of musculoskeletal injury was 63.1%; athletes participating in aesthetic sports reported more injuries.
Athletes with menstrual irregularity reported a greater percentage of severe musculoskeletal injuries than did athletes with normal menses.
According to the 2007 American College of Sports Medicine position stand, the female athlete triad is defined as the interrelatedness of energy availability, menstrual function, and bone mineral density (BMD).1 Clinically, energy availability is defined as dietary energy intake minus exercise energy expenditure, or the amount of dietary energy remaining for other body functions after exercise training.1 Energy availability can be affected by disordered eating (DE) behaviors, anorexia, and bulimia nervosa.1 Abnormal menstrual function may manifest as oligomenorrhea or amenorrhea; changes in BMD may present as stress fractures, osteopenia, or osteoporosis.2–9
Abnormal menstrual function is often called menstrual irregularity (MI) and may include primary amenorrhea, secondary amenorrhea, or oligomenorrhea.1 A higher prevalence of MI has been reported in the athletic population than in the general population.1,9–11 Few authors10,12–14 have reported the prevalence of MI in the high school athletic population, with estimates ranging from 20% to 54%. Menstrual irregularity is concerning because of its negative consequences, including an association with decreased BMD, which has been reported in the adolescent population.1,15
Although musculoskeletal injuries (INJ) in the adolescent population are fairly common, the adolescent female may be more susceptible to certain musculoskeletal injuries, such as patellofemoral pain syndrome and anterior cruciate ligament injury.16,17 Additionally, recent prospective studies18–20 have demonstrated higher injury rates in females than in males in similar high school sports. Although the short-term effects of injuries may limit sport participation for the female athlete, the long-term effects may include chronic impairments that limit her exercise and fitness participation, which may then negatively affect her overall quality of life across her lifespan.21
Hormones, particularly estrogen, have a significant influence on bone development. Higher estrogen levels increase calcium levels, leading to elevated calcium storage in bone.22 Because peak bone mass in females occurs during adolescence, the more time spent without adequate estrogen levels (as seen in oligomenorrhea and amenorrhea) during growth, the lower the peak bone mass, ultimately leading to a lower lifetime bone density.22,23 Menstrual irregularity has been associated primarily with stress fractures in collegiate and competitive athletes and military recruit populations.24–26 The relationship between MI and INJ in the adolescent population, including the development of stress fractures, has been reported in only 2 studies.12,27 Rauh et al27 noted that 37.4% of 163 (n=61) high school female athletes had at least 1 musculoskeletal injury and that athletes who reported MI were 3 times more likely to sustain a musculoskeletal injury than were athletes with normal menses. In a study of 62 female high school cross-country runners, Austin et al12 found that athletes with abnormal menstrual function were at 4 times greater risk of experiencing exercise-related leg pain. As in previous studies,18,28–31 the definition of injury used by both Rauh et al27 and Austin et al12 required the athlete to miss sport participation. However, athletes may sustain low-grade injuries that do not require them to completely miss practice or competition, and they may continue modified participation. Thus, these athletes are participating in activity at less than 100% effort but may not be identified as injured.12,18,27–31
Although the prevalence of MI among adolescent athletes is suggested to be high,12–15,32 and the rate of injuries among adolescent females can be high depending on the sport played,14,16,17,20,31,33 research on the relationship between MI and INJ in the adolescent population is limited.12,27 Therefore, our purpose was to determine the prevalence of and relationship between MI and INJ rates in a high school multisport population.
METHODS
Participants
Of the 850 female athletes who participated in school-sponsored sports at 3 local high schools in the Madison, Wisconsin, area during the 2006–2007 school year, 334 athletes (39.3% response rate) completed a study survey. The schools were selected by convenience. Athletes were grouped into the 3-sport classification system described by Beals and Manore.9 Aesthetic (AES) sports were those that used a subjective scoring component and included diving, gymnastics, dance team, cheerleading, and pom-pon squad. Endurance (END) sports were those in which intense exercise lasted beyond several minutes and aerobic metabolism was the primary energy source.34 The END sports included basketball, cross-country, soccer, and track (middle distance and distance). Team/anaerobic (T/A) sports were those that required maximal exercise for up to 3 minutes; the primary energy sources were almost exclusively adenosine triphosphate and phosphocreatine,34 and they included tennis, volleyball, swimming, softball, golf, and track (field events and sprints). No athletes were excluded because of inability to understand written and spoken English. Before the study began, written parental consent and participant assent were obtained. The study was approved by the institutional review boards at the University of Wisconsin, Madison, and Rocky Mountain University of Health Professions.
Procedures
Participant data were collected at the end of the respective season for each sport, dance, cheer, or pom-pon group. Each subject completed the Healthy Wisconsin High School Female Athlete Survey (HWHSFAS). The questionnaire, which has been demonstrated to be reliable, was developed by our research team and asked about the athlete's menstrual status over the past 12 months (frequency and length of menstrual cycles), age at menarche, and oral contraceptive (OCP) use. The questionnaire was administered in a group format with teammates and took each athlete 5 minutes, on average, to complete. The injury section of the questionnaire asked the athlete to recall any traumatic or overuse injury that occurred during the current sports season. For example, volleyball players were asked to report any injury that incurred during the current volleyball season, the body part that was injured, and the number of days of practice or competition missed because of the injury. If an athlete began the sport season with an injury sustained in a different sport, the athlete was excluded from the sport being surveyed. The survey did not differentiate between athletes who participated in full practice or had practice modified because of injury. Overuse injury was defined as a condition in which the pain began gradually and was not the result of falling, running into another athlete, or slipping or twisting the body. Traumatic injury was defined as an injury caused by running into another player, tripping, or falling. Examples of both injury types were provided on the survey next to the specific body part. For each injury, the athlete reported whether the injury was related to overuse or occurred traumatically. Our study injury definition included injuries that did not cause the athlete to miss any participation time. The survey also asked whether any injuries were not reported to a coach or certified athletic trainer (AT) and, if so, why the athlete chose not to report the injury.
Before the survey, general instructions were given to the group, and participants were directed to sit far apart from one another to protect the confidentiality of their responses. All research assistants were trained in a standardized written procedure to ensure consistency in data collection. When the athlete returned her survey, a research assistant reviewed it to identify unanswered questions. An athlete who submitted an incomplete survey was asked whether she needed clarification of any unanswered questions and was provided an opportunity to answer the questions.
Menstrual Irregularity.
Menstrual irregularity was defined as 9 or fewer menstrual cycles in the past 12 months in an athlete who had started menstruation (identified as all athletes experiencing secondary amenorrhea or oligomenorrhea).1 Primary amenorrhea was defined as the lack of menstruation by age 15 years4 and was also considered a form of MI. Athletes were then classified into 2 menstrual status groups: those with MI (having 9 or fewer menstrual cycles in the past 12 months for athletes who were postmenarche or had not begun menstruating by age 15) and those with normal menses.
Musculoskeletal Injury.
Musculoskeletal injury was defined as an injury from either overuse or direct trauma that occurred during participation in the current sport season. All injuries were classified according to days missed from participation: A minor injury resulted in no missed days, a mild injury resulted in 1 to 7 missed days, a moderate injury resulted in 8 to 21 missed days, and a major injury resulted in 22 or more missed days. Lastly, we also examined the greatest time lost (GTL) injury, which was defined as the injury that required the most days missed from participation, regardless of whether the injury was caused by overuse or trauma, for the current sport season.
Data Analysis
During the 2006–2007 school year, 311 female athletes participated in our study, including 23 multisport athletes (6.9%) who participated in the study twice. Therefore, our total number of completed questionnaires was 334. The study design required athletes to complete questionnaires about injuries that they had incurred during the current sport season and their eating habits in the past 28 days. Because responses from the same person could differ depending on the sport season, each survey completed by a multisport athlete was counted as a separate person. Athletes reported only injuries incurred in the current season; injuries were not carried over to another sport season. Surveys with incomplete responses (n=42) were excluded from the analysis. Additionally, 43 surveys in which athletes reported OCP use were excluded, because these medications can regulate menstruation in a female who may otherwise have MI.35–38 More athletes reported using OCPs (37%, n=8) than T/A athletes (15%, n=23) or END athletes (6.6%, n=5) (P=.03). A total of 249 surveys were used in the final analysis: AES = 21, END=77, and T/A=151. Of these, only 16 (6.4%) responses were from athletes who participated in the study twice.
Means and standard deviations of the participants' age, age of menarche, gynecologic age (time since the onset of menses), height, weight, and body mass index were determined. Statistical comparisons of mean values by sport type were performed using 1-way analysis of variance and Bonferroni post hoc pair-wise comparisons. Chi-square analysis was used to determine relationships between MI and sport type, INJ and sport type, and primary and secondary amenorrhea and oligomenorrhea and the effect of training on menstruation. Statistical significance was set at the .05 level.
Odds ratios and 95% confidence intervals were calculated to compare the severity of INJ between athletes with MI and athletes with normal menses. Odds ratios were then calculated separately for each sport type. The GTL injuries were categorized as minor (causing the athlete to miss 7 or fewer days of participation) or severe (causing the athlete to miss 8 or more days of participation).
All study analyses were conducted using SPSS software (version 16.0; SPSS Inc, Chicago, IL).
RESULTS
Pilot studies were conducted 8 days apart to assess the test-retest reliability of the menstrual history questions of the HWHSFAS on a convenience sample of 11 high school athletes. The intraclass correlation coefficients (3,1) for questions on age at menarche and number of periods during the past year were 0.95 and 0.99, respectively. The κ value for OCP use was 1.0.
Characteristics of the study sample are presented in Table 1. Although AES and T/A athletes differed in height and weight, body mass index was not different between the groups. The percentages of athletes who reported MI and INJ are shown in the Figure. Although the greatest percentages of MI and INJ were reported by AES athletes, no statistical differences were found among sport types. The percentages of athletes classified as having primary amenorrhea, secondary amenorrhea, and oligomenorrhea are provided in Table 2. Although no differences were found among sport types for any menstrual condition, the T/A athletes tended to report a higher percentage (23.8%, n=36) of oligomenorrhea (P=.08).
Table 1.
Characteristics of Study Participants (Mean±SD)
| Characteristic | Total (N = 249) | Aesthetic Sport Athletesa (n = 21) | Endurance Sport Athletesb (n = 77) | Team/Anaerobic Sport Athletesc (n = 151) | P Valued |
| Age, y | 15.3 ± 1.1 | 15.6 ± 1.2 | 15.3 ± 1.0 | 15.3 ± 1.1 | .32 |
| Age at menarche, y | 12.4 ± 1.1 | 12.6 ± 0.9 | 12.4 ± 1.1 | 12.3 ± 1.1 | .61 |
| Gynecologic age,e y | 2.9 ± 1.4 | 3.1 ± 1.7 | 3.0 ± 1.3 | 2.9 ± 1.4 | .92 |
| Height, cm | 166.7± 6.6 | 163.5 ± 5.0f | 165.6 ± 6.3 | 167.6 ± 6.8f | .01 |
| Weight, kg | 59.0 ± 9.5 | 54.1 ± 7.2f | 57.8 ± 8.2 | 60.3 ± 10.2f | .01 |
| Body mass index, kg/m2 | 21.2 ± 2.9 | 20.2 ± 2.3 | 21.0 ± 2.4 | 21.4 ± 3.2 | .16 |
aAesthetic sports consisted of diving, gymnastics, dance team, cheerleading, and pom-pon squad.
bEndurance sports consisted of basketball, cross-country, soccer, and track (middle distance and distance).
cTeam/anaerobic sports consisted of tennis, volleyball, swimming, softball, golf, and track (field events and sprints).
dMean differences between sport types (1-way analysis of variance).
eGynecologic age = chronologic age–years since menarche.
fDifferences noted for height and weight between the aesthetic and team/anaerobic groups (P=.02).
Figure.
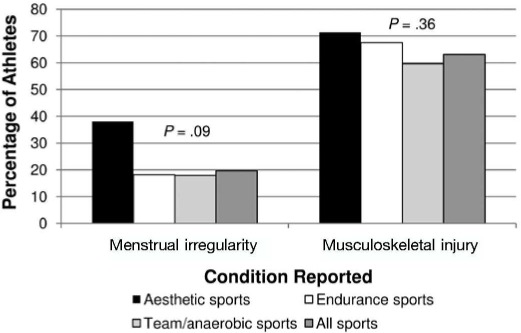
Aesthetic sports consisted of cheerleading, pom-pon squad, dance team, diving, and gymnastics. Endurance sports consisted of basketball, cross-country, soccer, and track (middle distance and distance). Team/anaerobic sports consisted of tennis, volleyball, swimming, softball, golf, and track (field events and sprints). Menstrual irregularity was defined as ≤9 menses in the past 12 months or menses not started by age 15 years. Musculoskeletal injury was defined as an injury that was the direct result of sport participation during the season. P values reflect the results of χ2 tests.
Table 2.
Athletes with Primary Amenorrhea, Secondary Amenorrhea, and Oligomenorrhea
| Condition | Total, n (%) (N = 249) | Aesthetic Sport Athletes,a n (%) (n = 21) | Endurance Sport Athletes,b n (%) (n = 77) | Team/Anaerobic Sport Athletes,c n (%) (n=151) | P Valued |
| Primary amenorrheae | 0.8 | 0.0 | 1.3 | 0.7 | .80 |
| Secondary amenorrheaf | 7.2 | 9.5 | 9.1 | 6.0 | .63 |
| Oligomenorrheag | 20.1 | 19.0 | 13.0 | 23.8 | .08 |
aAesthetic sports consisted of diving, gymnastics, dance team, cheerleading, and pom-pon squad..
bEndurance sports consisted of basketball, cross-country, soccer, and track (middle distance and distance).
cTeam/anaerobic sports consisted of tennis, volleyball, swimming, softball, golf, and track (field events and sprints).
d Frequency differences between sport types (χ2 test).
eDefined as the onset of menses at age 15 years or later.
fDefined as the lack of menstruation for 3 or more months after the onset of menses.
gDefined as menstrual cycles occurring 35 or more days apart.
The percentages of athletes with MI within each sport type and within the overall sample are presented in Table 3. The highest percentage of athletes within their sport type reporting MI were participants in pom-pon squad (66.7%, n=2) for AES, cross-country (21.4%, n=6) for END sports, and field events in track (33.3%, n=1) for T/A. Across all sports, the highest percentages of MI were in athletes participating in volleyball (20.4%, n=51), swimming (14.3%, n=36), cross-country (12.2%, n=30), and tennis (12.2%, n=30).
Table 3.
Athletes With Menstrual Irregularity Within Sport Types and in Overall Sample
| Sport Type | Menstrual Irregularitya in Each Sport, n (%) | Menstrual Irregularity in Overall Sample (N = 249), n (%) |
| Aesthetic (n = 21) | ||
| Diving | 1 (50.0) | 5 (2.0) |
| Gymnastics | 0 (0.0) | 0 (0.0) |
| Dance team | 2 (40.0) | 10 (4.1) |
| Cheerleading | 3 (33.3) | 15 (6.1) |
| Pom-pon squad | 2 (66.7) | 10 (4.1) |
| Endurance (n = 77) | ||
| Basketball | 4(16.7) | 20 (8.2) |
| Cross-country | 6(21.4) | 30 (12.2) |
| Soccer | 4(19.0) | 20 (8.2) |
| Track (middle distance and distance) | 0 (0.0) | 0 (0.0) |
| Team/anaerobic (n = 151) | ||
| Tennis | 6(13.6) | 30 (12.2) |
| Volleyball | 10(18.2) | 51 (20.4) |
| Swimming | 7 (23.3) | 36 (14.3) |
| Softball | 1 (16.7) | 5 (2.0) |
| Golf | 1 (14.3) | 5 (2.0) |
| Track (field events) | 1 (33.3) | 5 (2.0) |
| Track (sprints) | 1 (16.7) | 5 (2.0) |
aMenstrual irregularity was defined as 9 or fewer menses in the past 12 months or no menarche by age 15 years.
Age at the onset of training, the effect of training on menstruation, and the training regimen of participants are described in Table 4. Although a slightly higher percentage of T/A athletes reported that their periods became farther apart or lighter as a result of training, no differences were found among sport types. More than half of all athletes (58.6%, n=146) reported training outside organized practice, but the percentages did not differ by sport type.
Table 4.
Training and Menstruation
| Variable | Total (N = 249) | Aesthetic Sport Athletesa (n = 21) | Endurance Sport Athletesb (n = 77) | Team/Anaerobic Sport Athletesc (n = 151) | P Value |
| Age training started, y | 9.3 ± 2.9 | 10.4 ± 2.8 | 9.4 ± 3.0 | 9.1 ± 2.8 | .12d |
| During training, my periods, n (%) | |||||
| Stop | 8 (3.2) | 1 (4.8) | 3 (3.9) | 4 (2.6) | .55e |
| Get farther apart or lighter | 117 (47.0) | 7 (33.3) | 33 (42.9) | 77 (51.0) | |
| Get closer together or heavier | 16(6.4) | 2 (9.5) | 3 (3.9) | 11 (7.3) | |
| Do not change | 108(43.4) | 11 (52.4) | 38 (49.4) | 59 (39.1) | |
| Athletes who trained outside practice, n (%) | 146 (58.6) | 15 (71.4) | 47 (61.0) | 84 (55.6) | .34e |
aAesthetic sports consisted of diving, gymnastics, dance team, cheerleading, and pom-pon squad.
bEndurance sports consisted of basketball, cross-country, soccer, and track (middle distance and distance).
cTeam/anaerobic sports consisted of tennis, volleyball, swimming, softball, golf, and track (field events and sprints).
dOne-way analysis of variance.
eχ2 test.
Overall, 63.1% (n= 157) of the athletes reported an INJ. The reports of injury among AES (71.4%, n=15), END (67.5%, n=52), and T/A (59.6%, n=90) sport types were not different (P=.36). The percentages for severity of injury by menstrual status are shown in Table 5. For athletes in both groups (MI and normal menses), more than 50% of total injuries sustained were classified as minor, meaning that the athlete did not miss any days of sport participation because of the injury. Fewer than 6% of total injuries in either group were classified as major, which was defined as missing 22 or more days of sport participation because of the injury. For the overall sample, athletes who reported MI sustained a higher percentage of major injuries than did athletes who reported normal menses. The incidence of GTL injuries by menstrual status is presented in Table 6. Although athletes with MI were almost 3 times as likely to sustain a GTL injury causing the athlete to miss 8 or more days as were athletes with normal menses, the association was not significant (odds ratio=2.7, 95% confidence interval=0.8, 8.8).
Table 5.
Severity of Injury in Athletes With or Without Menstrual Dysfunction by Sport Type
| Sport Type | Menstrual Status | Overuse Injuries, n (%) |
Traumatic Injuries, n (%) |
Total Injuries, n (%) |
|||||||||
| Minora | Mildb | Moderatec | Majord | Minor | Mild | Moderate | Major | Minor | Mild | Moderate | Major | ||
| Aesthetice | |||||||||||||
| Irregularf | 16 (94.1) | 1 (5.9) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 17 (89.5) | 1 (5.3) | 0 (0.0) | 1 (5.3) | |
| Normal | 42 (87.5) | 6 (12.5) | 0 (0.0) | 0 (0.0) | 6 (60.0) | 3 (30.0) | 1 (10.0) | 0 (0.0) | 48 (82.8) | 9 (15.5) | 1 (1.7) | 0 (0.0) | |
| Endurancesg | |||||||||||||
| Irregular | 13 (61.9) | 8 (38.1) | 0 (0.0) | 0 (0.0) | 5 (45.5) | 2 (18.2) | 3 (27.3) | 1 (9.1) | 19 (57.6) | 10 (30.3) | 3 (9.1) | 1 (3.0) | |
| Normal | 50 (64.1) | 24 (30.8) | 3 (3.8) | 1 (1.3) | 18 (52.9) | 15 (44.1) | 1 (2.9) | 0 (0.0) | 69 (61.1) | 39 (34.5) | 4 (3.5) | 1 (0.9) | |
| Team/anaerobich | |||||||||||||
| Irregular | 26 (74.3) | 8 (22.9) | 0 (0.0) | 1 (2.9) | 16(76.2) | 4 (19.0) | 0 (0.0) | 1 (4.8) | 42 (75.0) | 12 (21.4) | 0 (0.0) | 2 (3.6) | |
| Normal | 123 (72.8) | 42 (24.9) | 3 (1.8) | 1 (0.6) | 31 (68.9) | 13 (28.9) | 0 (0.0) | 1 (2.2) | 154 (72.0) | 55 (25.7) | 3(1.4) | 2 (0.9) | |
aThe athlete reported missing 0 days of sport participation because of the injury.
bThe athlete reported missing 1–7 days of sport participation because of the injury.
cThe athlete reported missing 8–21 days of sport participation because of the injury.
dThe athlete reported missing 22 or more days of sport participation because of the injury.
eAesthetic sports consisted of diving, gymnastics, dance team, cheerleading, and pom-pon squad.
fMenstrual irregularity was defined as 9 or fewer menses in the past 12 months or no menarche by age 15 years.
gEndurance sports consisted of basketball, cross-country, soccer, and track (middle distance and distance).
hTeam/anaerobic sports consisted of tennis, volleyball, swimming, softball, golf, and track (field events and sprints).
Table 6.
Incidence of Greatest Time Lost Injuries by Menstrual Status and Days Lost from Sport
| Sport Type | Menstrual Status | Incidence of Greatest Time Lost Injuries |
Odds Ratio | 95% Confidence Interval | |
| ≤7 d Lost, n (%) | ≥8 d Lost, n (%) | ||||
| Aesthetic sport athletesa | |||||
| Irregulara | 3 (75.0) | 1 (25.0) | 0.0 | NA | |
| Normal | 10 (100.0) | 0 (0.0) | 1.0 | Reference | |
| Endurance sport athletesc | |||||
| Irregular | 13 (92.9) | 1 (7.1) | 1.1 | 0.1, 10.1 | |
| Normal | 71 (93.4) | 5 (6.6) | 1.0 | Reference | |
| Team/anaerobic sport athletesd | |||||
| Irregular | 8 (72.7) | 3 (27.3) | 3.4 | 0.6, 18.1 | |
| Normal | 36 (90.0) | 4 (10.0) | 1.0 | Reference | |
| Total | |||||
| Irregular | 24 (82.8) | 5(17.2) | 2.7 | 0.8, 8.8 | |
| Normal | 117 (92.9) | 9(7.1) | 1.0 | Reference | |
Abbreviation: NA, not applicable.
aAesthetic sports consisted of diving, gymnastics, dance team, cheerleading, and pom-pon squad.
bMenstrual irregularity was defined as 9 or fewer menses in the past 12 months or no menarche by age 15 years.
cEndurance sports consisted of basketball, cross-country, soccer, and track (middle distance and distance).
dTeam/anaerobic sports consisted of tennis, volleyball, swimming, softball, golf, and track (field events and sprints).
DISCUSSION
Prevalence of MI
Overall, the prevalence of MI in our study was 19.7% among athletes from multiple sports, which is similar to prevalence estimates reported by several authors12–14 but lower than estimates in another study.10 In an investigation of multiple sports, Nichols et al13 found that 20.1% of 423 high school athletes reported MI. Interestingly, despite some differences in sports studied (we included 3 additional AES sports [gymnastics, dance team, and pom-pon squad]; they included lacrosse), the overall prevalence of MI was similar to our findings. However, when they categorized their sports by lean-build or nonlean-build status, lean-build athletes had a higher prevalence of MI (26.7%) than did nonlean-build athletes (16.6%).13 Although we classified our athletes differently, our T/A classification (tennis, volleyball, swimming, softball, golf) is similar to their nonlean-build classification (tennis, volleyball, basketball, softball, soccer). The prevalence of MI in our T/A athletes (17.9%) was similar to the 16.6% observed in their nonlean-build sport group.13 Because their lean-build group classification was dissimilar from our AES and END groups, we were unable to make appropriate comparisons. Our AES group had a prevalence of MI of 38.1%, but Nichols et al13 did not study these sports.
Using a definition of MI similar to ours, Hoch et al10 reported an overall much higher prevalence of MI in the athletic population (54%).10 The difference in their findings compared with ours and those of other studies13,14 cannot be explained. Interestingly, Hoch et al10 reported the prevalence of MI in their sedentary control population as 21%, which is similar to that in our population of female athletes and in other studies of female athletes.13,14 Hoch et al10 stated that the high MI prevalence in sedentary controls was probably related to the high frequency of low energy availability observed in that population in their study.
Austin et al12 reported a much higher MI prevalence of 34.9%. Their estimate was derived solely from a sample of 62 high school cross-country runners, so comparisons should be made cautiously because we studied athletes in numerous sports. For direct comparisons, however, only 21.4% of the cross-country runners in our study reported MI. The reasons for the lower estimate in our study are unknown but may be related in part to the differences in design used (ie, retrospective versus prospective).
In our study, the prevalence of oligomenorrhea was 20.1%, which is similar to the 17.1% to 21% prevalence shown by other authors.10,14 Our prevalences of primary and secondary amenorrhea were 0.8% and 7.2%, respectively, similar to the findings of 1.2% and 5.3% by Nichols et al.14 In contrast, Hoch et al10 reported a higher frequency of amenorrhea (36%) than oligomenorrhea (18%) in their athletic population. The authors did not indicate whether the amenorrhea was primary, secondary, or both.10 In collegiate athletes, Beals and Manore9 found that the prevalence of primary amenorrhea was 7.4%, which is much higher than our finding. This difference may reflect the populations studied. Beals and Manore9 examined National Collegiate Athletic Association Division I athletes, whereas we investigated high school athletes. Although we found a 7.2% prevalence of secondary amenorrhea in our population, Hoch et al10 noted a prevalence of 15% in sedentary controls, which they attributed to the high frequency of low energy availability without DE. The prevalence of secondary amenorrhea ranges from 3.4% to 66.0%.1,35,39,40 This wide range of estimates can be explained largely by methodologic variations among studies, including differences in the athletic populations studied, the levels of competition, and the ages of the athletes. 1,35,39,40
Our prevalence estimate for MI of 19.7%, which is similar to previous findings,13,14 suggests that MI may be a medical problem among high school athletes. However, reports pertaining to the prevalence of MI in the adolescent population should be interpreted cautiously. Although MI immediately after menarche is common, nearly 90% of females have normal menstrual cycles within 2 years of menarche.41 Our confidence in our reported MI estimate was high because 63.5% of our participants were 2 or more years postmenarche, by which time the normal fluctuations commonly observed immediately after menarche are typically no longer present.
We found no difference in the prevalence of MI among sport types, which is in direct contrast to Beals and Manore,9 who studied collegiate women and noted that AES athletes experienced greater prevalences of primary and secondary amenorrhea and oligomenorrhea than END and T/A athletes. Our results demonstrate that the occurrence of MI among athletes in END and T/A sports is similar to that among athletes participating in AES sports in the high school population. Therefore, health care professionals should screen for MI in all female athletes at the high school level, regardless of sport.
In our study, half (50.2%) of the athletes reported that their periods stopped, became farther apart, or were lighter during training. This high prevalence may be partially related to the hormonal alterations that occur with strenuous exercise, which may lead to a decrease in energy availability.42 The exercise itself is not fully responsible for the modulation in the reproductive system; rather, the reproductive system undergoes changes because of the decreased acute available energy. This theory has been supported by Loucks et al,43 who examined reproductive function alterations in exercising women by assaying blood samples during menstrual cycles while controlling for exercise intensity and caloric intake. They found that reproductive function was not disrupted by exercise stress but was affected by low energy availability.43 In a subsequent study, Loucks et al44 determined that reproductive disruption may occur when negative energy balance falls below a very specific threshold of 20 to 30 kcal/kg of lean body mass per day.44 In a similar study, De Souza et al45 grouped 49 women according to exercise status (exercising versus sedentary) and menstrual status (menstrual disturbance versus normal ovulation). All groups with menstrual disturbances had lower resting energy expenditures than did groups with normal ovulation, demonstrating an attempt to conserve energy in the presence of a chronic negative energy balance. De Souza et al45 also noted that as the magnitude of negative energy balance increases, alterations in the reproductive system become more severe.45 The results of these studies43–45 and others39,40,46–48 indicate that alterations in reproductive function appear to be related to acute energy availability, not body mass or exercise intensity.
The fact that 50% of athletes in our study reported menstruation alterations is concerning; irregular menses during adolescence have been associated with decreased bone mineral density.1,15 Approximately 50% of peak bone mass is accrued during adolescence, which is a critical time to attain maximal bone mass.49
The age at which athletes in our study started organized training was 9.3 ± 2.9 years, and the average age of menarche was 12.4 ± 1.1 years, which is considered normal.50 These results are in contrast to those of other authors,41,51 who reported delayed menarche in exercising adolescents. Warren51 found that menarche in 15 ballet dancers occurred at 15.4 years, which was significantly different from that in the control group. No identified ballet dancers participated in our study, and we did not characterize activity intensity or the amount of supervision that occurred during training. It may be that the level and frequency of activity were appropriate for the athletes in our study, thereby allowing them to maintain a positive energy balance, establishing an environment for normal menarche. Further research in this area is warranted.
Incidence of INJ
We found that the overall incidence of INJ was 63.1%, similar to the 65.9% reported by Beals and Manore9 in a study of DE, menstrual status, and INJ among athletes in multiple collegiate sports. They calculated injury risks of 80.6%, 65.2%, and 62.4% for AES, END, and T/A athletes, respectively.9 The similarity of our injury estimates of 71.4%, 67.5%, and 59.6% for AES, END, and T/A athletes, respectively, probably resulted from our use of identical sport classifications. However, although Beals and Manore9 used the phrase musculoskeletal injury, they did not define it in their study. Our incidence of MI of 63.1% is higher than that of other studies of high school athletes.18,28–30,52,53 This difference may result from the definition of injury. Many previous authors12,18,27–30,53 included only injuries that required the athlete to miss sport participation, whereas we included injured athletes who did not miss any participation time. To date, only one group52 has examined injury occurrence among high school athletes using a definition that did not require the athlete to miss any participation time. Beachy et al52 found that the overall incidence of injury in female athletes was 46%. Our injury estimate of 63.1% may be higher because we included all injuries, regardless of whether they were reported to the AT, whereas Beachy et al52 included only those reported to the AT. In addition, we investigated 1 sport season of injury data, whereas Beachy et al52 collected injury data for 9 years. Lastly, we sampled different sports in our studies, which probably affected injury incidence; Beachy et al52 followed athletes in additional sports that generally have a lower occurrence of injury.
Using the same definitions for injury severity in terms of time lost from participation, we found a similar pattern. Beachy et al52 reported 64.5%, 30.3%, 3.1%, and 1.9% for 0 days lost, 1–7 days lost, 8–21 days lost, and 22 or more days lost from participation; we found 56.8%, 35.9%, 3.9%, and 3.4%, respectively, for the same classifications. Although our findings are similar to those of Beachy et al,52 they must be interpreted cautiously because the latter included both male and female athletes in their estimates, whereas our findings are restricted to female athletes.
In our study, the highest incidence of injury was minor injuries, so the athlete did not miss any participation time. Part of our rationale for including athletes who reported an injury but did not miss practice or competition was to capture those who competed but at less than 100% effort. If the athlete reported the injury to the AT, and appropriate participation modifications were instituted, the risk of incurring a more severe injury probably decreased. However, more than one-third (37%) of athletes sustained an injury that was unreported. Almost 20% of athletes stated that they did not report the injury because they believed it would affect their position on the team. These findings are concerning in that athletes who continue to play with an undiagnosed injury, without proper guidance and recommendations related to their sport participation from the AT or another health care professional, may predispose themselves to a subsequent or more severe injury.14,15,33
Overall, of the GTL injuries, 141/155 (91%) resulted in athletes missing 7 days or fewer from sport participation. Only 14 (9%) athletes missed 8 or more days of participation due to a GTL injury. Of these, 5 (35%) met the criteria for MI. Regarding the 9 severe injuries in athletes with normal menses, 7 were overuse and 2 were traumatic. Because of the small sample size, it is difficult to draw any conclusions from this information. Future authors may want to assess time lost from activity as it relates to menstrual status.
One theory that may support the high prevalence of INJ is low energy availability, which can cause alterations in cellular maintenance, growth, and thermoregulation.1,54 Therefore, just as a female with low energy availability may not have enough caloric support for normal menstruation, she may also not have enough caloric support for growth and repair of injured tissues. In addition, levels of leptin, a modulator of hormones such as growth hormone, cortisol, and thyroid-stimulating hormone, are known to be low in undernourished states55 and may ultimately affect tissue growth and repair.55 We did not examine the association between leptin and injury risk, so future studies are needed to examine this relationship.
The common theory supporting the MI and INJ prevalences seen in our study is low energy availability, which may manifest as DE. Previous studies of female high school athletes have demonstrated prevalences of DE ranging from 18.2% to 35.4%.14,56 Although we did not assess the presence of DE in our sample, it is possible that the females with MI and INJ (or both) also suffered from DE, specifically those who sustained INJ resulting in more time lost. Rauh et al33 reported associations among DE, BMD levels >1 SD, and musculoskeletal injuries considered major (>21 days lost). Furthermore, they found a trend between major injuries and amenorrheic and oligomenorrheic athletes. They suggested that athletes with DE may also exhibit low energy availability, which may adversely affect the athlete's bone, muscle, and connective tissues.
One strength of our study is the large sample size (n=249). In addition, we excluded participants with incomplete data and those who reported OCP use, which may affect a female athlete's menstrual status. In addition, we evaluated the relationship between MI and INJ in high school female athletes who participated in school-sponsored activities and not elite athletes, which increases the generalizability of the study for this population. Currently, very few studies10,12–14 have been dedicated to this population. Lastly, similar to the findings of Nichols et al, the reliabilities of the variables of menstrual irregularity from the HWHSFAS were also high (0.95–0.99), which increased our confidence in the athletes' reports of their menstrual histories in the past year.
Although the HWHSFAS had good reliability, the use of recall in survey research may be a potential limitation of our findings. However, the recall accuracy of medical information has been examined in the athletic population and been shown to be accurate,29,57,58 even at the high school level.29 Because we asked participants to report injuries from the past 2 to 3 months only, we believe that their ability to recall injury information was reasonably accurate. Yet literature directly related to the injury recall ability of the female high school athlete does not exist. Finally, although our menstrual questions proved to be reliable, we did not have clinical or laboratory data to accurately assess the participants' menstrual status, thereby limiting our results.
We also recognize that our findings may be limited because of the low participation rate (39.3%). Several factors probably affected our response rate: the inability to obtain parental or athlete consent and lack of support from coaches to encourage the athletes to participate in the study.
We suggest that future authors examine the relationship between MI and INJ at the high school level. Suggested topics include determining the relationship among menstrual status and days missed from sport participation, injury type (overuse versus traumatic), and timing of injury during the sport event (first half versus second half). In addition, a prospective cohort study in which the AT establishes the diagnosis is recommended.
In conclusion, we observed a high prevalence of MI that was similar among sport types. This finding adds to the growing body of evidence10,12–14 about this health problem in high school female athletes. More than half of the athletes reported that their periods stopped or became lighter during training and competition. Furthermore, we found a high incidence of INJ, with more cases among athletes participating in AES sports. Most injuries that caused the athlete the greatest time lost during the current sport season resulted in the athlete missing 7 or fewer days of practice or competition.
Our data suggest that MI may increase the risk of injury in female athletes during their high school sport participation. Based on recent reports, the acute change in energy availability may play a key role in this risk relationship. Although more longitudinal data are needed to elucidate the effects of oligomenorrhea (the most common form of MI in this study population) on long-term health, directing educational efforts at helping teen female athletes improve their caloric intake to better balance their energy availability and thus prevent or correct menstrual dysfunction may be warranted. These efforts may help reduce major injuries in female athletes, in that our data showed more major injuries in athletes who reported MI. Lastly, because of the association between irregular menses and decreased bone mineral density1,15 during adolescence, referral to a physician for examination of the adolescent with MI is warranted.
Acknowledgments
This research was supported in part by a doctoral research grant from the NATA Research & Education Foundation.
REFERENCES
- 1.Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP, American College of Sports Medicine American College of Sports Medicine position stand: the female athlete triad. Med Sci Sports Exerc. 2007;39(10):1867–1882. doi: 10.1249/mss.0b013e318149f111. [DOI] [PubMed] [Google Scholar]
- 2.Beals KA. Eating behaviors, nutritional status, and menstrual function in elite female adolescent volleyball players. J Am Diet Assoc. 2002;102(9):1293–1296. doi: 10.1016/s0002-8223(02)90285-3. [DOI] [PubMed] [Google Scholar]
- 3.Black DR, Larkin LJ, Coster DC, Leverenz LJ, Abood DA. Physiologic Screening Test for Eating Disorders/ Disordered Eating among female collegiate athletes. J Athl Train. 2003;38(4):286–297. [PMC free article] [PubMed] [Google Scholar]
- 4.Cobb KL, Bachrach LK, Greendale G. Disordered eating, menstrual irregularity, and bone mineral density in female runners. Med Sci Sports Exerc. 2003;35(5):711–719. doi: 10.1249/01.MSS.0000064935.68277.E7. et al. [DOI] [PubMed] [Google Scholar]
- 5.Greydanus DE, Patel DR. The female athlete: before and beyond puberty. Pediatr Clin North Am. 2002;49(3):553–580. vi. doi: 10.1016/s0031-3955(02)00005-6. [DOI] [PubMed] [Google Scholar]
- 6.Khan KM, Liu-Ambrose T, Sran MM, Ashe MC, Donaldson MG, Wark JD. New criteria for female athlete triad syndrome? As osteoporosis is rare, should osteopenia be among the criteria for defining the female athlete triad syndrome? Br J Sports Med. 2002;36(1):10–13. doi: 10.1136/bjsm.36.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smolak L, Murnen SK, Ruble AE. Female athletes and eating problems: a meta-analysis. Int J Eat Disord. 2000;27(4):371–380. doi: 10.1002/(sici)1098-108x(200005)27:4<371::aid-eat1>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 8.Beals KA. Eating disorder and menstrual dysfunction screening, education, and treatment programs. Phys Sportsmed. 2003;31(7):33–41. doi: 10.3810/psm.2003.07.434. [DOI] [PubMed] [Google Scholar]
- 9.Beals KA, Manore MM. Disorders of the female athlete triad among collegiate athletes. Int J Sport Nutr Exerc Metab. 2002;12(3):281–293. doi: 10.1123/ijsnem.12.3.281. [DOI] [PubMed] [Google Scholar]
- 10.Hoch AZ, Pajewski NM, Moraski L. Prevalence of the female athlete triad in high school athletes and sedentary students. Clin J Sport Med. 2009;19(5):421–428. doi: 10.1097/JSM.0b013e3181b8c136. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiksten-Almstromer M, Hirschberg AL, Hagenfeldt K. Menstrual disorders and associated factors among adolescent girls visiting a youth clinic. Acta Obstet Gynecol Scand. 2007;86(1):65–72. doi: 10.1080/00016340601034970. [DOI] [PubMed] [Google Scholar]
- 12.Austin TM, Reinking MF, Hayes AM. Menstrual function in female high school cross-country athletes. Int J Adolesc Med Health. 2009;21(4):555–565. doi: 10.1515/ijamh.2009.21.4.555. [DOI] [PubMed] [Google Scholar]
- 13.Nichols JF, Rauh MJ, Barrack MT, Barkai HS, Pernick Y. Disordered eating and menstrual irregularity in high school athletes in lean-build and nonlean-build sports. Int J Sport Nutr Exerc Metab. 2007;17(4):364–377. doi: 10.1123/ijsnem.17.4.364. [DOI] [PubMed] [Google Scholar]
- 14.Nichols JF, Rauh MJ, Lawson MJ, Ji M, Barkai HS. Prevalence of the female athlete triad syndrome among high school athletes. Arch Pediatr Adolesc Med. 2006;160(1):137–142. doi: 10.1001/archpedi.160.2.137. [DOI] [PubMed] [Google Scholar]
- 15.Nichols JF, Rauh MJ, Barrack MT, Barkai HS. Bone mineral density in female high school athletes: interactions of menstrual function and type of mechanical loading. Bone. 2007;41(3):371–377. doi: 10.1016/j.bone.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Huston LJ, Greenfield ML, Wojtys EM. Anterior cruciate ligament injuries in the female athlete: potential risk factors. Clin Orthop Relat Res. 2000;372:50–63. doi: 10.1097/00003086-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Loud KJ, Micheli LF. Common athletic injuries in adolescent girls. Curr Opin Pediatr. 2001;13(4):317–322. doi: 10.1097/00008480-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Knowles SB, Marshall SW, Bowling JM. A prospective study of injury incidence among North Carolina high school athletes. Am J Epidemiol. 2006;164(12):1209–1221. doi: 10.1093/aje/kwj337. et al. [DOI] [PubMed] [Google Scholar]
- 19.Powell JW, Barber-Foss KD. Sex-related injury patterns among selected high school sports. Am J Sports Med. 2000;28(3):385–391. doi: 10.1177/03635465000280031801. [DOI] [PubMed] [Google Scholar]
- 20.Rauh MJ, Koepsell TD, Rivara FP, Margherita AJ, Rice SG. Epidemiology of musculoskeletal injuries among high school cross-country runners. Am J Epidemiol. 2006;163(1):151–159. doi: 10.1093/aje/kwj022. [DOI] [PubMed] [Google Scholar]
- 21.Garrick JG, Requa RK. Sports and fitness activities: the negative consequences. J Am Acad Orthop Surg. 2003;11(6):439–443. doi: 10.5435/00124635-200311000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Drinkwater BL, Nilson K, Ott S, Chesnut CH., III. Bone mineral density after resumption of menses in amenorrheic athletes. JAMA. 1986;256(3):380–382. [PubMed] [Google Scholar]
- 23.Myburgh KH, Hutchins J, Fataar AB, Hough SF, Noakes TD. Low bone density is an etiologic factor for stress fractures in athletes. Ann Intern Med. 1990;113(10):754–759. doi: 10.7326/0003-4819-113-10-754. [DOI] [PubMed] [Google Scholar]
- 24.Bennell KL, Malcolm SA, Thomas SA. Risk factors for stress fractures in track and field athletes: a twelve-month prospective study. Am J Sports Med. 1996;24(6):810–818. doi: 10.1177/036354659602400617. et al. [DOI] [PubMed] [Google Scholar]
- 25.Nattiv A, Puffer JC, Green GA. Lifestyles and health risks of collegiate athletes: a multi-center study. Clin J Sport Med. 1997;7(4):262–272. doi: 10.1097/00042752-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Rauh MJ, Macera CA, Trone DW, Shaffer RA, Brodine SK. Epidemiology of stress fracture and lower-extremity overuse injury in female recruits. Med Sci Sports Exerc. 2006;38(9):1571–1577. doi: 10.1249/01.mss.0000227543.51293.9d. [DOI] [PubMed] [Google Scholar]
- 27.Rauh MJ, Nichols JF, Barrack MT. Relationships among injury and disordered eating, menstrual dysfunction, and low bone mineral density in high school athletes: a prospective study. J Athl Train. 2010;45(3):243–252. doi: 10.4085/1062-6050-45.3.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernandez WG, Yard EE, Comstock RD. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emerg Med. 2007;14(7):641–645. doi: 10.1197/j.aem.2007.03.1354. [DOI] [PubMed] [Google Scholar]
- 29.Garrick JG, Requa RK. Injuries in high school sports. Pediatrics. 1978;61(3):465–469. doi: 10.1542/peds.61.3.465. [DOI] [PubMed] [Google Scholar]
- 30.Powell JW, Barber-Foss KD. Injury patterns in selected high school sports: a review of the 1995–1997 seasons. J Athl Train. 1999;34(3):277–284. [PMC free article] [PubMed] [Google Scholar]
- 31.Rauh MJ, Macera CA, Ji M, Wiksten DL. Subsequent injury patterns in girls' high school sports. J Athl Train. 2007;42(4):486–494. [PMC free article] [PubMed] [Google Scholar]
- 32.Barrack MT, Rauh MJ, Barkai HS, Nichols JF. Dietary restraint and low bone mass in female adolescent endurance runners. Am J Clin Nutr. 2008;87(1):36–43. doi: 10.1093/ajcn/87.1.36. [DOI] [PubMed] [Google Scholar]
- 33.Rauh MJ, Margherita AJ, Rice SG, Koepsell TD, Rivara FP. High school cross country running injuries: a longitudinal study. Clin J Sport Med. 2000;10(1):110–116. doi: 10.1097/00042752-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 34.McArdle WD, Katch FI, Katch VL. Exercise Physiology: Energy, Nutrition and Human Performance. Baltimore, MD: Lippincott Williams & Wilkins; 2001. p. 138. [Google Scholar]
- 35.Loucks AB, Horvath SM. Athletic amenorrhea: a review. Med Sci Sports Exerc. 1985;17(1):56–72. [PubMed] [Google Scholar]
- 36.Fenichel RM, Warren MP. Anorexia, bulimia, and the athletic triad: evaluation and management. Curr Osteoporos Rep. 2007;5(4):160–164. doi: 10.1007/s11914-007-0011-3. [DOI] [PubMed] [Google Scholar]
- 37.Warren MP, Brooks-Gunn J, Fox RP. Persistent osteopenia in ballet dancers with amenorrhea and delayed menarche despite hormone therapy: a longitudinal study. Fertil Steril. 2003;80(1):398–404. doi: 10.1016/s0015-0282(03)00660-5. et al. [DOI] [PubMed] [Google Scholar]
- 38.Warren MP, Miller KK, Olson WH, Grinspoon SK, Friedman AJ. Effects of an oral contraceptive (norgestimate/ethinyl estradiol) on bone mineral density in women with hypothalamic amenorrhea and osteopenia: an open-label extension of a double-blind, placebo-controlled study. Contraception. 2005;72(3):206–211. doi: 10.1016/j.contraception.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 39.Loucks AB. Effects of exercise training on the menstrual-cycle: existence and mechanisms. Med Sci Sports Exerc. 1990;22(3):275–280. [PubMed] [Google Scholar]
- 40.Warren MP, Perlroth NE. The effects of intense exercise on the female reproductive system. J Endocrinol. 2001;170(1):3–11. doi: 10.1677/joe.0.1700003. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization Task Force on Adolescent Reproductive Health. World Health Organization multicenter study on menstrual and ovulatory patterns in adolescent girls, II: longitudinal study of menstrual patterns in the early postmenarcheal period, duration of bleeding episodes and menstrual cycles. J Adolesc Health Care. 1986;7(4):236–244. [PubMed] [Google Scholar]
- 42.Loucks AB, Mortola JF, Girton L, Yen SS. Alterations in the hypothalamic-pituitary-ovarian and the hypothalamic-pituitary-adrenal axes in athletic women. J Clin Endocrinol Metab. 1989;68(1):402–411. doi: 10.1210/jcem-68-2-402. [DOI] [PubMed] [Google Scholar]
- 43.Loucks AB, Verdun M, Heath EM. Low energy availability, not stress of exercise, alters LH pulsatility in exercising women. J Appl Physiol. 1998;84(1):37–46. doi: 10.1152/jappl.1998.84.1.37. [DOI] [PubMed] [Google Scholar]
- 44.Loucks AB. Energy availability, not body fatness, regulates reproductive function in women. Exerc Sport Sci Rev. 2003;31(3):144–148. doi: 10.1097/00003677-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 45.De Souza MJ, Lee DK, VanHeest JL, Scheid JL, West SL, Williams NI. Severity of energy-related menstrual disturbances increases in proportion to indices of energy conservation in exercising women. Fertil Steril. 2007;88(4):971–975. doi: 10.1016/j.fertnstert.2006.11.171. [DOI] [PubMed] [Google Scholar]
- 46.Eliakim A, Beyth Y. Exercise training, menstrual irregularities and bone development in children and adolescents. J Pediatr Adolesc Gynecol. 2003;16(4):201–206. doi: 10.1016/s1083-3188(03)00122-0. [DOI] [PubMed] [Google Scholar]
- 47.Loucks AB. Introduction to menstrual disturbances in athletes. Med Sci Sports Exerc. 2003;35(9):1551–1552. doi: 10.1249/01.MSS.0000084531.33556.7B. [DOI] [PubMed] [Google Scholar]
- 48.Warren MP, Stiehl AL. Exercise and female adolescents: effects on the reproductive and skeletal systems. J Am Med Womens Assoc. 1999;54(3):115–120. 138. [PubMed] [Google Scholar]
- 49.Loud KJ, Gordon CM. Adolescent bone health. Arch Pediatr Adolesc Med. 2006;160(10):1026–1032. doi: 10.1001/archpedi.160.10.1026. [DOI] [PubMed] [Google Scholar]
- 50.Chumlea WC, Schubert CM, Roche AF. Age at menarche and racial comparisons in US girls. Pediatrics. 2003;111(1):110–113. doi: 10.1542/peds.111.1.110. et al. [DOI] [PubMed] [Google Scholar]
- 51.Warren MP. The effects of exercise on pubertal progression and reproductive function in girls. J Clin Endocrinol Metab. 1980;51(5):1150–1157. doi: 10.1210/jcem-51-5-1150. [DOI] [PubMed] [Google Scholar]
- 52.Beachy G, Akau CK, Martinson M, Olderr TF. High school sports injuries: a longitudinal study at Punahou School, 1988 to 1996. Am J Sports Med. 1997;25(5):675–681. doi: 10.1177/036354659702500515. [DOI] [PubMed] [Google Scholar]
- 53.Brooks MA, Schiff MA, Rivara FP. Identifying previous sports injury among high school athletes. Clin Pediatr (Phila). 2009;48(5):548–550. doi: 10.1177/0009922808330777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Loucks AB, Thuma JR. Luteinizing hormone pulsatility is disrupted at a threshold of energy availability in regularly menstruating women. J Clin Endocrinol Metab. 2003;88(1):297–311. doi: 10.1210/jc.2002-020369. [DOI] [PubMed] [Google Scholar]
- 55.Misra M, Miller KK, Kuo K. Secretory dynamics of leptin in adolescent girls with anorexia nervosa and healthy adolescents. Am J Physiol Endocrinol Metab. 2005;289(3):E373–E381. doi: 10.1152/ajpendo.00041.2005. et al. [DOI] [PubMed] [Google Scholar]
- 56.Thein-Nissenbaum JM, Rauh MJ, Carr KE, Loud KJ, McGuine TA. Associations between disordered eating, menstrual dysfunction and musculoskeletal injury among high school athletes. J Orthop Sports Phys Ther. 2011;41(1):60–69. doi: 10.2519/jospt.2011.3312. [DOI] [PubMed] [Google Scholar]
- 57.Gabbe BJ, Finch CF, Bennell KL, Wajswelner H. How valid is a self reported 12 month sports injury history? Br J Sports Med. 2003;37(6):545–547. doi: 10.1136/bjsm.37.6.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hahn T. Criterion related validity of self-reported knee symptoms among athletes. Scand J Med Sci Sports. 2002;12(5):282–287. doi: 10.1034/j.1600-0838.2002.10215.x. [DOI] [PubMed] [Google Scholar]


