Abstract
In mice, ovariectomy accelerates the progression of the end-stage renal disease glomerulosclerosis. In women, the incidence of this disease increases after menopause, and estrogen alters its progression. Polymorphisms in the human estrogen receptor α (ERα) gene have been suggested to constitute a genetic predisposition for lupus nephritis. Here we show that by 1 year of age, mice lacking ERα (ERα-/-) but not those lacking ERβ (ERβ-/-) exhibit immune complex-type glomerulonephritis, proteinuria, and destruction of tubular cells with severe infiltration of B lymphocytes in the kidney and the presence of anti-DNA antibodies in serum. No gender difference occurred in the incidence or severity of these symptoms. However, in female but not in male ERα-/- mice there were elevated serum levels of IgG3. Other prominent features of these mice were (i) spontaneous formation of germinal centers in the spleen in the absence of antigen challenge and (ii) infiltration of plasma cells in the kidney and plasmacytosis in the spleen. Immunohistochemistry indicated a selective expression of ERα protein in the germinal centers but not in the follicular mantle zone of murine spleens and human tonsils. Our results indicate that ERα has indispensable functions in the kidney and in germinal centers, and that defective ERα signaling results in glomerulonephritis.
Keywords: kidney, plasma cells, bone marrow, plasmacytosis
The incidence of end-stage renal disease increases after menopause (U.S. Renal Data System, www.usrds.org). These data suggest that estrogen may partially prevent the development or progression of renal diseases. The renal glomerulus has been reported to be a direct-target tissue for estrogen (1, 2), and evidence shows that an estrogen receptor α (ERα) gene polymorphism may be associated with susceptibility to lupus nephritis in males (3). Human and mouse mesangial cells, which are the cells involved in the pathogenesis of the end-stage renal disease glomerulosclerosis, express both ERα and ERβ (1). Renal protective effects of estrogen have been demonstrated both in cultured renal proximal tubular cells (4) and in whole animals. In glomerulosclerosis-prone mice, estrogen treatment results in a reduced prosclerotic response (5) and ovariectomy accelerates its progression (6). Therefore, it has been suggested that estrogen replacement would help in preventing the progression of end-stage renal disease.
Germinal centers (GCs) are sites of Ig class switch, Ig gene V-region somatic hypermutations, and B cell tolerization and are thought to be an important site of immune dysregulation in autoimmune disease (7–9). In NZB × NZW F1 mice (10), a well-characterized model of autoimmunity in mice, GC formation occurs in the absence of antigen challenge (10–12). There is evidence that murine lymphocytes (13) and lymphocytes in GCs of human lymph nodes (14) are ERα-positive. But expression and function of ERα in the GC still remains to be investigated by additional methods.
Estrogen is a Janus-like molecule with contradictory effects in autoimmune diseases. Although it appears to offer protection against end-stage renal disease, during the development of systemic lupus erythematosus (SLE), estrogen blocks the destruction of immature autoreactive B cells in the bone marrow of mice and promotes autoimmunity (15). Furthermore, treatment of lupus-prone mice with estrogen increases the incidence of autoimmune disease (16–18), whereas tamoxifen, an ERα antagonist, seems to suppress SLE (19). With the exception of estrogen treatment of neonatal (NZB × NZW F1) mice (20), it is generally widely accepted that estrogen aggravates lupus nephritis. In direct contrast, estrogen can suppress the development of the autoimmune exocrinopathy, Sjögren's syndrome (SS) (21), and ovariectomy mimics SS in mice of healthy background (22). Interestingly, ovariectomy does not induce apoptotic cell death in the salivary gland of ERα-/- mice (22).
B lymphocytes play an important role in autoimmune diseases, including both SLE and SS. So far, no satisfying explanation has been offered for the apparent contradictory roles of estrogen in SLE and SS, but one possibility is that different B cell populations exist, each with its own unique estrogen sensitivity or dependence during the different stages of cell differentiation. Because the level of ERα seems to increase during differentiation and the level of ERβ to decrease (13), we have used ERα-/- and ERβ-/- mice to help to elucidate the role of the two receptors in the immune system.
We have found that ERα-/- mice develop signs of autoimmunity. This phenotype is spontaneous and involves ERα but not ERβ. Our results indicate that (i) ERα may have an indispensable function during the development of B lymphocytes in splenic GCs and in the kidney, (ii) defects in kidney and immune organs due to aberrant signaling of ERα may play a central role in the development of glomerulonephritis, and (iii) ERα-selective agonists could have beneficial effects in renal disease.
Materials and Methods
Mouse Strains and Housing. ERα-/- mice on a C57BL/6J/129 background were kept in the animal facility at Huddinge University Hospital under specific pathogen-free conditions and fed standard laboratory chow.
Human Tissue. Tonsils were obtained from routine tonsillectomies performed at the Karolinska Hospital (Stockholm, Sweden). Informed consent was obtained from the patients. Tissue collection was approved by the ethical committee at the Microbiology and Tumor Biology Center, Karolinska Institute. The specimens were kept on ice immediately after surgical removal.
Proteinuria. The presence of proteins in mouse urine was measured by using Combur 5 test strip (Roche Diagnostics).
Measurement of Serum Ig and Anti-DNA Antibodies by ELISA. Serum Ig was determined by ELISA with mouse Ig isotyping ELISA kit (BD Pharmingen). Serial dilutions (1,000–50,000) of test serum samples were used. Levels of circulating antibodies reactive with single-stranded DNA and double-stranded DNA (dsDNA) were determined with mouse anti-single-stranded DNA and dsDNA ELISA kit (Alpha Diagnostic International, San Antonio, TX).
Histological Methods. Tissues were fixed in 4% paraformaldehyde/PBS overnight and paraffin-embedded. Paraffin sections (4 μm) were dewaxed in xylene, rehydrated through graduated ethanol to water, and stained with hematoxylin/eosin. For immunohistochemistry, endogenous peroxidase was blocked by incubation for 30 min with a solution of 1% hydrogen peroxide, and antigen retrieval was performed by microwaving sections in 0.01 M citrate buffer (pH 6.0) for 20 min at 800 W. Tissue sections were incubated for 1 h at 4°C with normal goat serum diluted at 1/10 in PBS. Antibodies were diluted individually in PBS containing 3% BSA. Dilution was 1:100 for ERα antibody. Sections were incubated with antibodies overnight at 4°C. For negative controls, the primary antibody was replaced with PBS. Before addition of secondary antibody, sections were rinsed in PBS. The ABC method was used to visualize the signal according to the manual provided by the manufacturer (Vector Laboratories). Sections were incubated in biotinylated goat anti-rabbit or goat anti-mouse IgG (1:200 dilution) for 2 h at room temperature, followed by washing with PBS and incubation in avidin–biotin–horseradish peroxidase for 1 h. After thorough washing in PBS, sections were developed with 3,3′-diaminobenzidine tetrahydrochloride (DAKO), slightly counterstained with Mayers hematoxylin, and dehydrated through an ethanol series, followed by exposure to xylene and mounting.
Antibodies. Rabbit anti-human ERα polyclonal (HC-20) antibodies were from Santa Cruz Biotechnology. Biotinylated secondary antibodies (goat anti-mouse IgG and goat anti-rabbit IgG) and avidin-biotin kits were obtained from Vector Laboratories. Cy3-conjugated anti-mouse IgG antibodies were from Jackson ImmunoResearch.
Immunization. Anesthetized mice were immunized with 50 ng of Nonidet 30-keyhole limpet hemocyanin in PBS (Biosearch) by i.p. injection to stimulate an immune response.
Results
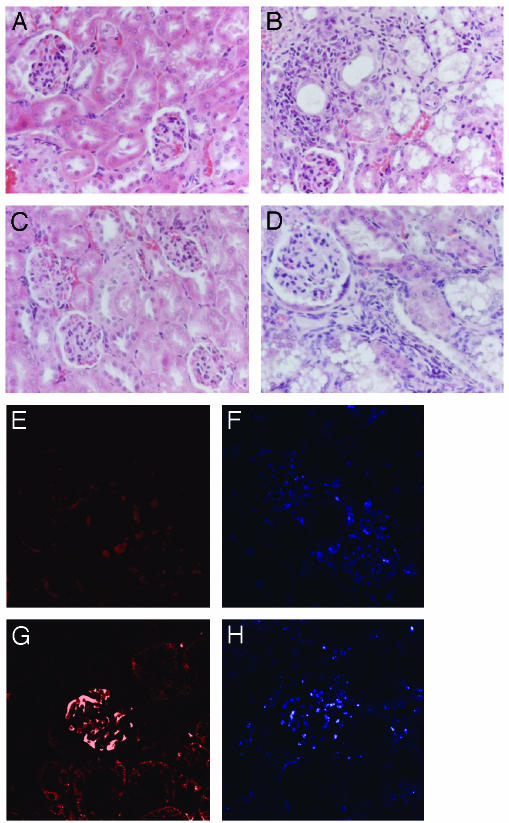
ERα-/- Mice Show Histological Signs of Glomerulonephritis. By 1 year of age, male and female ERα-/- mice show glomerulonephritis and some degree of mesangial sclerosis characterized by tubular epithelial cellular proliferation and inflammatory cell infiltrates (Fig. 1B). Whereas the kidneys of WT and ERβ-/- mice (Fig. 1 A and C) are normal, mice in which both estrogen receptor genes are inactivated, ERαβ-/- mice (Fig. 1D), have a phenotype similar to that of ERα-/- mice. Apparently, no increase occurred in cellularity in the glomeruli. The ERα-/- mice had significant depositions of IgG (Fig. 1G) in renal glomeruli, but no positive signals for IgM or IgA were detected when the appropriate antibodies were used (data not shown). These abnormalities were not seen in age-matched WT or ERβ-/- mice, suggesting that it is specifically the loss of the ERα-/- gene in vivo that results in development of glomerulonephritis. Impaired renal function was confirmed by the presence of significant proteinuria in ERα-/- mice (Table 1). Nine of 10 WT mice had proteinuria levels <30 mg/dl, whereas all ERα-/- mice, female and male, had protein levels >30 mg/dl; 30% of ERα-/- mice had levels >100 mg/dl.
Fig. 1.
One-year-old ERα-/- mice develop autoimmune glomerulonephritis. Kidney sections from 1-year-old ERα-/- (B) and ERαβ-/- (D) mice stained with hematoxylin/eosin show glomerulonephritis, but WT (A) and ERβ-/- (C) mice do not. Deposition of IgG was detected by immunofluorescence with kidney sections from WT (E and F) and ERα-/- (G and H) mice. IgG deposition in the kidney is shown in ERα-/- (G) but not WT (E) mice. Counterstained nuclei with DAPI are shown in F and H. Fifteen ERα-/- and 15 WT animals were evaluated.
Table 1. Number of mice with proteinuria.
| Strains | <30 mg/dl | >30 mg/dl | >100 mg/dl |
|---|---|---|---|
| WT female | 4 | 1 | 0 |
| WT male | 5 | 0 | 0 |
| ERα-/- female | 0 | 4 | 1 |
| ERα-/- male | 0 | 3 | 2 |
Ten- to 12-month-old ERα-/- mice and WT littermates were tested for proteinuria. Data show numbers of mice for each group.
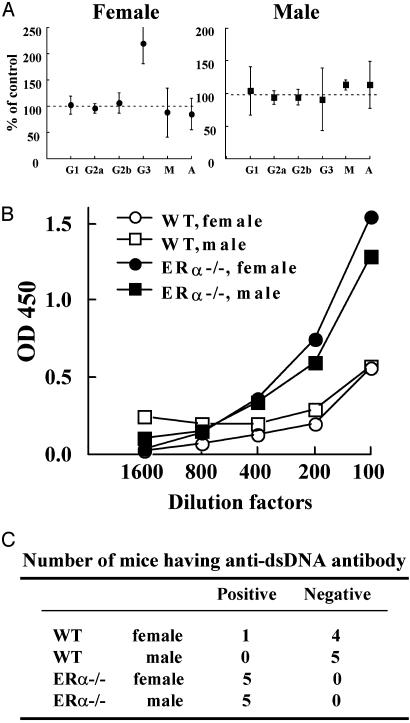
Autoantibody Development in ERα-/- Mice. To further characterize the autoimmune glomerulonephritis-like phenotype in ERα-/- mice, concentrations of immunoglobulins and antibodies against DNA were determined. The data show that, compared with their WT littermates, female but not male ERα-/- mice have a significant increase in the T helper 1-dependent Ig isotype, IgG3 (Fig. 2A). Both female and male ERα-/- mice developed high concentrations of autoantibodies against dsDNA, whereas most age-matched WT mice were negative (Fig. 2 B and C). This result suggests that ERα controls B cell tolerance and autoimmunity during nephritis. No antibodies against single-stranded DNA existed in any of the mouse strains (total, 20 mice; data not shown).
Fig. 2.
Levels of circulating Igs and autoantibodies in 1-year-old ERα-/- mice. Level of circulating Igs in 1-year-old mice was assayed by ELISA. (A) ODs at 450 nM were compared between ERα-/- and WT mice (four mice per group). (B) Serum titers of anti-dsDNA IgG in 1-year-old mice were analyzed by using an ELISA kit, and OD values of a step-wise dilution factor from one set of representative results are shown. (C) Summary of preference of anti-dsDNA IgG in 10 ERα-/- mice is shown.
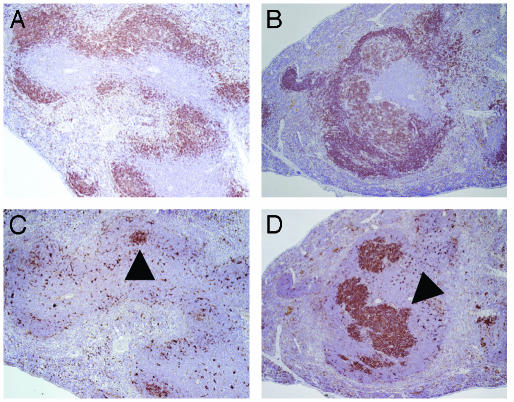
Spontaneous Formation of GCs in ERα-/- Mice. In many cases of autoimmunity, persistent GC formation may contribute to the development of disease. The mice in these studies were maintained in a specific pathogen-free animal facility. Histological analysis of spleens revealed that GCs were either absent or poorly formed in B cell follicles of WT mice (Fig. 3 A and C). Minor changes were apparent in B220 positive B cells of follicular mantle zones (Fig. 3 A and B). In contrast, ERα-/- mice spontaneously developed GCs together with nephritis (Fig. 3 B and D).
Fig. 3.
Spontaneous GC formation in ERα-/- mice in the absence of antigen challenge. Sections obtained from the spleens of 1-year-old WT (A and C) and ERα-/- (B and D) mice revealed lymphoid follicles (B220 positive, A and B). In ERα-/- mice, spontaneous formation of PNA-positive GC occurs (D), whereas WT mice exhibit poorly formed GCs (C). Arrowheads point to GC.
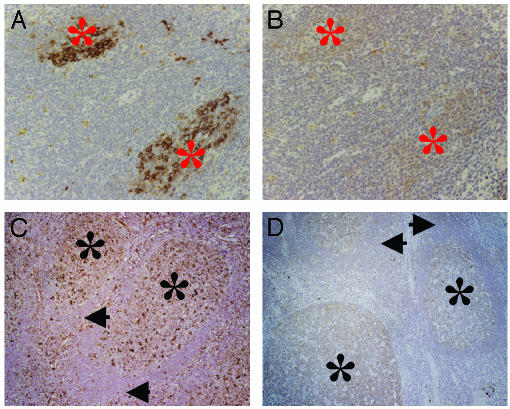
ERα Is Expressed in Splenic GCs. To investigate the expression of ER in GCs in response to a challenge with a TD antigen, C57BL/6 WT mice were immunized with keyhole limpet hemocyanin. Ten days after immunization, peanut agglutinin (PNA) was used in histological sections to detect GCs. Clusters of PNA-positive cells were observed in immunized WT mice, indicating formation and expansion of GCs (Fig. 4A). On immunohistochemistry with ERα antibodies, no ERα-positive signals occurred in the follicular zone, but positive (although weak) staining did occur for ERα in the areas that were PNA-positive (Fig. 4B).
Fig. 4.
ERα protein is expressed in mouse and human GCs. The formation of GCs was induced by immunization of mice with keyhole limpet hemocyanin for 10 days. Mouse spleens and human tonsil sections were stained with biotin-labeled PNA (A and C) and anti-ERα antibody (B and D). Arrows point to follicular mantle zone, and asterisks indicate GCs.
Unlike the mouse spleen, a human tonsil has well defined secondary follicles with GCs and a follicular mantle zone. On immunohistochemistry with ERα antibodies, the expression of ERα was found to be strictly confined to the GC area only with no expression in the follicular mantle zone (Fig. 4 C and D).
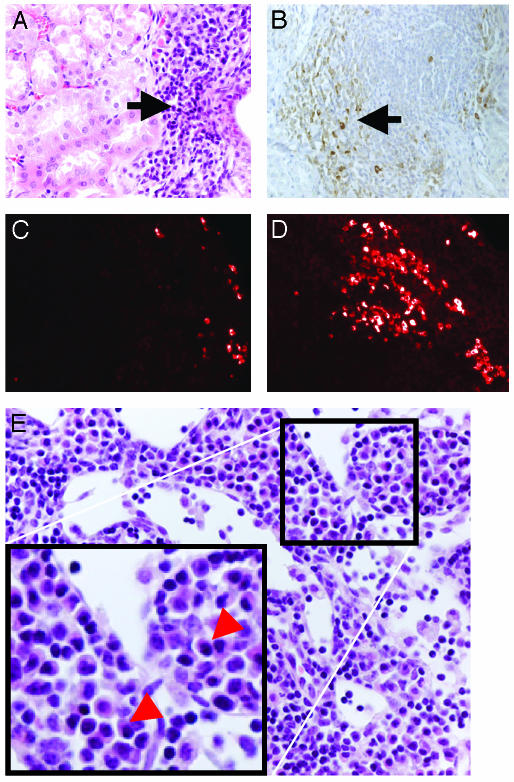
ERα-/- Mice Show Plasmacytosis in Kidney and Spleen. ERα-/- mice often show well developed lymph nodes occupied with plasma B cells, which arise from the GC and play critical roles in autoimmune diseases. Histological sections of kidneys from ERα-/- mice showed the presence of massive infiltration of B lymphocytes (Fig. 5A), many of which were identified as plasma cells based on the presence of IgG in their cytoplasm (Fig. 5B). Whereas the number of plasma cells is very low in the spleen of WT mice (Fig. 5C), increased cytosolic IgG-positive plasma cells in ERα-/- mice indicate plasmacytosis in the spleen (Fig. 5D), probably because of enhanced GC formation. This result indicates that loss of ERα may allow accumulation of plasma cells in nonhematopoietic tissues. In addition, lymph nodes in ERα-/- mice showed accumulating plasma cells characterized by eccentrically placed nuclei with prominent speckles of chromatin and cytoplasm with marked peripheral basophilia (Fig. 5E).
Fig. 5.
Lack of ERα causes an accumulation of plasma B cells in the kidney and spleen. (A) Severe infiltration of B lymphocytes in kidneys from ERα-/- mice (hematoxylin/eosin-stained). Some of these lymphocytes are characterized as a plasma B cells with bigger cytosolic areas (A) and cytosolic IgG signals (anti-IgG positive, B). Increased numbers of plasma B cells bearing cytosolic IgG are found in spleens from ERα-/- mice (D) but not in WT mice (C). Plasma B cells also accumulate in lymph nodes from ERα-/- mice (E). Arrowheads point to plasma B cells.
Discussion
Autoimmune diseases occur more frequently in females than in males, and estrogen alters the course of these diseases (23). So far, the exact role of estrogen in autoimmune diseases is not understood. The aim of our study was to determine whether lack of either of the two estrogen receptors is involved in autoimmunity. For these studies we used mice in which either or both estrogen receptor genes were inactive, i.e., ERα-/-, ERβ-/-, and ERαβ-/- mice. We found that, by 1 year of age, ERα-/- mice spontaneously exhibit signs of autoimmune nephritis with IgG deposition and destruction of tubular epithelial cells in the kidney, whereas age-matched WT and ERβ-/- mice were normal. Impaired renal function was confirmed by the presence of significant proteinuria in ERα-/- mice. This previously unpublished evidence shows that development of signs of spontaneous renal disease in mice involves ERα but not ERβ.
Involvement of estrogen in renal diseases has been well demonstrated in many studies (U.S. Renal Data System, www.usrds.org; refs. 5 and 16–20). Our results support the notion that ERα is required for the renal protective effect of estrogen (4–6). Human and mouse mesangial cells and glomeruli, which are the cells involved in the pathogenesis of the end-stage renal disease called glomerulosclerosis, express both ERα and ERβ (1). Thus, although estrogen plays an important role in regulating the immune system, ERα may also be important in glomerular functions and in the protective effects of estrogen on the kidney.
Estrogen is a Janus-like molecule with contradictory effects in two typical autoimmune diseases, SLE and the exocrinopathy SS. During the development of SLE, estrogen-treated lupus-prone mice have higher incidence of autoimmune disease in general (16). It is a well accepted fact that estrogen aggravates lupus nephritis (16–18). On the other hand, during the development of SS, estrogen suppresses the disease (21), and ovariectomy mimics SS in mice of healthy background (22). B lymphocytes play an important role in autoimmune diseases, including both SLE and SS.
The relative level of ERα increases during differentiation of B lymphocytes, and the level of ERβ decreases (13). This finding suggests that ERα and ERβ may have different functions during the development of B lymphocytes. To better understand the seemingly contradictory actions of estradiol, we also investigated the effect of estrogen receptor deficiency in salivary glands of mice as they age, with reference to development of SS. Surprisingly, we found no significant signs of exocrinopathy of the salivary glands in 1-year-old mice of either genotype (data not shown). Thus, even though ovariectomy mimics SS in mice of healthy background, neither ERα nor ERβ seems to be directly involved in the development of SS.
In general, females exhibit higher levels of serum Ig than males and mount more vigorous humoral immune responses (24). Estrogen enhances survival of autoreactive B cells (15) and number of plasma cells in mouse (25). It seems that ERα is essential in these positive actions of estrogen in adult mice (26). In very old ERα-/- mice (1.5–2 years of age), the frequency of IgA and IgG secreting B lymphocytes in the spleen increased (27). According to our results, both male and female ERα-/- mice develop IgG but not IgA and IgM deposition in their kidneys and have a significant increase in anti-dsDNA antibodies in their serum. Clearly, lack of ERα in the mouse mimics signs of autoimmune nephritis. Many observations show that estrogen treatment can accelerate the onset of lupus nephritis and decrease the lifespan of mice with lupus nephritis. Moreover, estrogen treatment induces the production of autoantibodies in some nonautoimmune-prone mouse strains (25). In addition, many independent studies in humans clearly demonstrate that estrogen enhances the progression of lupus nephritis (28).
Our results, showing an increase in autoimmunity in the absence of ERα, appear at first glance to be opposite to the evidence of a worsening effect of estrogen in lupus nephritis. The autoimmunity in ERα-/- mice is different from human lupus nephritis and from the animal model of this disease. In general, human lupus nephritis strikes young females after puberty and is associated with systemic disease, including skin and joints. We have found that nephritis in ERα-/- mice appears when mice are ≈9 months of age. In addition, after careful examination of many other tissues, including skin, salivary glands, liver, and joints, we found no signs of autoimmune-like symptoms in these tissues.
The GC may be an important site of immune dysregulation and disruption of B cell tolerance in autoimmune diseases (7–9). GC formation occurs in mice that spontaneously develop autoimmunity (10–12). Here we report that mice lacking ERα spontaneously develop GCs in the absence of an antigen challenge. This persistent GC formation may contribute to the development of autoantibodies and autoimmune nephritis in ERα-/- mice. It has been reported that lymphocytes in GCs of human and mouse lymph nodes are weakly positive for ERα (13, 14). In the present study, we found that selective expression of ERα protein occurs in the GC but not in the follicular mantle zone of murine spleen and human tonsils.
It is well known that estrogen treatment inhibits B and T lymphopoiesis in the bone marrow and thymus (27, 29–31). From the studies of ERα-/- mice, it has become clear that both ERs are responsible for mediating estrogen-regulated B lymphopoiesis in vivo (29, 30). In ERα-/- mice, the number of total B cells, including pro/pre B lymphocytes (B220low/IgM-) and mature B lymphocytes (B220high/IgM+) in bone marrow, decreases (29), and estrogen treatment can still reduce the number of mature B lymphocytes in the bone marrow of ERα-/- mice. These results indicate that both ERα and ERβ are needed for the inhibitory effects of estrogen on B lymphopoiesis after estrogen treatment (29, 30). We have observed (unpublished work) that tamoxifen, but not 17β-estradiol, inhibits spontaneous DNA synthesis in GCs under nonstimulated conditions. In contrast, the formation of GCs induced by immunization can be inhibited by estrogen. These observations suggest that estrogen normally inhibits immunization-induced proliferation of lymphocytes in developing GCs. The effect of ERα deficiency in the formation of GCs might, therefore, be a reflection of the inhibitory effects of 17β-estradiol on lymphopoiesis in bone marrow. The exaggerated formation of GCs in ERα-/- mice, which we have reported in the present study, is consistent with an antiproliferative role for ERα.
In normal mice, estrogen up-regulates the anti-apoptotic protein, Bcl-2, in splenic B cells (15) and increases the number of plasma cells and their antibody production capacity (25). Mice deficient in Bcl-2 have few B cells in their bone marrow and none in the splenic GC. Reintroduction of Bcl-2 into these mice restores bone marrow B cells but does not restore B cells to GCs (32). Our observation of an accumulation of plasma cells in diseased kidneys and spleens in the absence of ERα and the report of a significant elevation in the number of IgA- and IgG-producing cells in the spleens of ERα-/- mice by 18 months of age (27) are compatible with the previous conclusion (32) that regulation of Bcl2 levels is not a decisive factor in regulation of the number of B cells in the GC.
Our results suggest a role of ERα in the development of autoimmune nephritis. In addition to the role of ERα in lymphopoiesis, ERα may affect the kidney directly. It is still not clear whether the nephritis in ERα-/- mice is directly caused by loss of ERα from immune cells or whether insufficiency of estrogen-supported cytoprotection in the kidney exacerbates glomerulonephritis and leads to death of mesangial cells. Tissue-specific knock-out of ERα could be useful in future studies to resolve these issues. If the loss of ERα from the kidney is important in the progression of glomerulonephritis, ERα agonists could be of use clinically to alter the course this disease. Bone marrow transplantation of ERα-/- lymphocytes into WT mice will provide useful answers to this question. One other aspect of the role of estrogen in kidney disease, which may be of value in diagnosis and treatment in the clinic, is whether mutations in the ERα gene are responsible for and constitute a genetic risk factor for nephritis.
Acknowledgments
We thank Sandra Andersson for valuable advice on immunohistochemical techniques, Patricia Humire and Ann-Marie Witte for excellent animal care and genotyping, and Christina Tuhlin Andersson for magical Western blots. This study was supported by grants from the Swedish Cancer Fund and Karo Bio AB.
Abbreviations: ER, estrogen receptor; SLE, systemic lupus erythematosus; GC, germinal center; SS, Sjögren's syndrome; dsDNA, double-stranded DNA; PNA, peanut agglutinin.
References
- 1.Potier, M., Elliot, S. J., Tack, I., Lenz, O., Striker, G. E., Striker, L. J. & Karl, M. (2001) J. Am. Soc. Nephrol. 12, 241-251. [DOI] [PubMed] [Google Scholar]
- 2.Jelinsky, S. A., Harris, H. A., Brown, E. L., Flanagan, K., Zhang, X., Tunkey, C., Lai, K., Lane, M. V., Simcoe, D. K. & Evans, M. J. (2003) Endocrinology 144, 701-710. [DOI] [PubMed] [Google Scholar]
- 3.Liu, Z. H., Cheng, Z. H., Gong, R. J., Liu, H., Liu, D. & Li, L. S. (2002) Nephron 90, 174-180. [DOI] [PubMed] [Google Scholar]
- 4.Han, H. J., Park, S. H., Park, H. J., Park, K. M., Kang, J. W., Lee. J. H., Lee, B. C. & Hwang, W. S. (2002) Clin. Exp. Pharmacol. Physiol. 29, 60-67.11906461 [Google Scholar]
- 5.Potier, M., Karl, M., Zheng, F., Elliot, S. J., Striker, G. E. & Striker, L. J. (2002) Am. J. Pathol. 160, 1877-1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elliot, S. J., Karl, M., Berho, M., Potier, M., Zheng, F., Leclercq, B., Striker, G. E. & Striker, L. J. (2003) Am. J. Pathol. 162, 1441-1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wen, L., Pao, W., Wong, F. S., Peng, Q., Craft, J., Zheng, B., Kelsoe, G., Dianda, L., Owen, M. J. & Hayday, A. C. (1996) J. Exp. Med. 183, 2271-2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelsoe, G. (1996) Semin. Immunol. 8, 179-184. [DOI] [PubMed] [Google Scholar]
- 9.Thorbecke, G. J., Amin, A. R. & Tsiagbe, V. K. (1994) FASEB J. 8, 832-840. [DOI] [PubMed] [Google Scholar]
- 10.Carteron, N. L., Schimenti, C. L. & Wofsy, D. (1989) J. Immunol. 142, 1470-1475. [PubMed] [Google Scholar]
- 11.Miyamoto, A., Nakayama, K., Imaki, H., Hirose, S., Jiang, Y., Abe, M., Tsukiyama, T., Nagahama, H., Ohno, S., Hatakeyama, S. & Nakayama, K. (2002) Nature 416, 865-869. [DOI] [PubMed] [Google Scholar]
- 12.Wang, J. H., Avitahl, N., Cariappa, A., Friedrich, C., Ikeda, T., Renold, A., Andrikopoulos, K., Liang, L., Pillai, S., Morgan, B. A. & Georgopoulos, K. (1998) Immunity 9, 543-553. [DOI] [PubMed] [Google Scholar]
- 13.Grimaldi, C. M., Cleary, J., Dagtas, A. S., Moussai, D. & Diamond, B. J. (2002) J. Clin. Invest. 109, 1625-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maia, D. M., Sciarrotta, J., Abendroth, K. & Blatt, J. (2002) Leuk. Lymphoma 39, 365-371. [DOI] [PubMed] [Google Scholar]
- 15.Bynoe, M. S., Grimaldi, C. M. & Diamond, B. (2000) Proc. Natl. Acad. Sci. USA 97, 2703-2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carlsten, H., Tarkowski, A., Holmdahl, R. & Nilsson, L. A. (1990) Clin. Exp. Immunol. 80, 467-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carlsten, H., Nilsson, N., Jonsson, R., Backman, K., Holmdahl, R. & Tarkowski, A. (1992) Cell Immunol. 144, 190-202. [DOI] [PubMed] [Google Scholar]
- 18.Peeva, E., Grimaldi, C., Spatz, L. & Diamond, B. (2000) J. Clin. Invest. 106, 1373-1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu, W. M., Lin, B. F., Su, Y. C., Suen, J. L. & Chiang, B. L. (2000) Scand. J. Immunol. 52, 393-400. [DOI] [PubMed] [Google Scholar]
- 20.Yamaguchi, K., Inoue, Y., Hisano, M., Unten, S. & Shimamura, T. (2003) Lupus 12, 332-334. [DOI] [PubMed] [Google Scholar]
- 21.Ishimaru, N., Saegusa, K., Yanagi, K., Haneji, N., Saito, I. & Hayashi, Y. (1999) Am. J. Pathol. 155, 173-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishimaru, N., Arakaki, R., Watanabe, M., Kobayashi, M., Miyazaki, K. & Hayashi, Y. (2003) Am. J Pathol. 163, 1481-1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vidaver, R. (2002) Trends Immunol. 23, 229-230. [DOI] [PubMed] [Google Scholar]
- 24.Butterworth, M., McClellan, B. & Allansmith, M. (1967) Nature 13, 483-488. [PMC free article] [PubMed] [Google Scholar]
- 25.Verthelyi, D. I. & Ahmed, S. A. (1998) Cell. Immunol. 189, 125-134. [DOI] [PubMed] [Google Scholar]
- 26.Erlandsson, M. C., Jonsson, C. A., Islander, U., Ohlsson, C. & Carlsten, H. (2003) Immunology 108, 346-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Islander, U., Erlandsson, M. C., Hasseus, B., Jonsson, C. A., Ohlsson, C., Gustafsson, J.-Å., Dahlgren, U. & Carlsten, H. (2003) Immunology 110, 149-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mok, C. C., Lau, C. S. & Wong, R. W. (2001) Semin. Arthritis. Rheum. 30, 426-435. [DOI] [PubMed] [Google Scholar]
- 29.Thurmond, T. S., Murante, F. G., Staples, J. E., Silverstone, A. E., Korach, K. S. & Gasiewicz, T. A. (2000) Endocrinology 141, 2309-2318. [DOI] [PubMed] [Google Scholar]
- 30.Erlandsson, M. C., Ohlsson, C., Gustafsson, J.-Å. & Carlsten, H. (2001) Immunology 103, 17-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shim, G.-J., Wang, L., Andersson, S., Nagy, N., Kis, L. L., Zhang, Q., Makela, S., Warner, M. & Gustafsson, J.-Å. (2003) Proc. Natl. Acad. Sci. USA 100, 6694-6699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brunner, C., Marinkovic, D., Klein, J., Samardzic, T., Nitschke, L. & Wirth, T. (2003) J. Exp. Med. 197, 1205-1211. [DOI] [PMC free article] [PubMed] [Google Scholar]