Abstract
Aims
Bleeding complications have been associated with short-term mortality in patients with non-ST-segment elevation myocardial infarction (NSTEMI). Their association with long-term outcomes is less clear. This study examines mortality associated with in-hospital bleeding during NSTEMI over time intervals starting from hospital discharge and extending past 3 years.
Methods and results
We studied 32 895 NSTEMI patients aged ≥65 years, using patient-level data from the CRUSADE registry linked with Medicare claims data. We assessed the association of in-hospital major bleeding with short (30 days), intermediate (1 year), and long-term (3 years) mortality among hospital survivors overall, as well as in those patients treated with or without a percutaneous coronary intervention (PCI). We calculated adjusted hazard ratios (HRs) for mortality for bleeders vs. non-bleeders over time intervals from: (i) discharge to 30 days; (ii) 31 days to 1 year; (iii) 1 year to 3 years; and (iv) beyond 3 years. Overall, 11.9% (n = 3902) had an in-hospital major bleeding event. Cumulative mortality was higher in those who had a major bleed vs. those without at 30 days, 1 year, and 3 years. Even after adjustment, major bleeding continued to be significantly associated with higher mortality over time in the overall population: (i) discharge to 30 days [adjusted HR 1.33; 95% confidence interval (CI) 1.18–1.51]; (ii) 31 days to 1 year (1.19; 95% CI 1.10–1.29); (iii) 1 year to 3 years (1.09; 95% CI 1.01–1.18), and (iv) attenuating beyond 3 years (1.14; 95% CI 0.99–1.31). In-hospital bleeding among patients treated with PCI continued to be significantly associated with higher adjusted mortality even beyond 3 years (1.25; 95% CI 1.01–1.54).
Conclusion
In-hospital major bleeding is associated with short-, intermediate-, and long-term mortality among older patients hospitalized for NSTEMI—this association is strongest within the first 30 days, but remains significant long term, particularly among PCI-treated patients. Despite a probable early hazard related to bleeding, the longer duration of risk in patients who bleed casts doubt on its causal relationship with long-term mortality. Rather, major bleeding likely identifies patients with an underlying risk for mortality.
Keywords: Bleeding, Outcomes, Elderly patients, Acute myocardial infarction, Percutaneous coronary intervention
Introduction
Accumulating evidence from randomized trial cohorts and community-based registries supports the relationship between in-hospital major bleeding and mortality in patients with non-ST-segment elevation myocardial infarction (NSTEMI).1–3 Prior analyses of clinical trials have primarily focused on the association between bleeding and short-term mortality (within 30 days or 6 months of the index event).4–6 Several retrospective studies of trial data found that major bleeding continues to have an adverse association at 1 year.5,7–9 This finding suggests that bleeding may be a marker of a vulnerable group of patients who continue to accumulate adverse events (including mortality) over time. Meanwhile, observational registry data have found either no association or a smaller magnitude of association between bleeding and intermediate-term mortality1 than seen in clinical trials.10,11 It is possible then, that the hazard associated with bleeding may be limited to the bleeding event, and attenuate over time.
To further understand the time course of these relationships, we used data from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the American College of Cardiology/American Heart Association Guidelines (CRUSADE) Quality Improvement Initiative linked to the Centers for Medicare & Medicaid Services (CMS) longitudinal administrative data. We describe the adjusted hazard of mortality associated with in-hospital bleeding during NSTEMI over time from hospital discharge and extending past 3 years in the overall population, as well as in patients treated with or without a percutaneous coronary intervention (PCI). We also describe the effect of in-hospital catheterization, revascularization with PCI, or use of discharge anti-platelet therapies on the observed associations over time.
Methods
The CRUSADE registry is a database of patients with high-risk NSTEMI acute coronary syndromes (ACS) admitted to US hospitals from November 2001 through December 2006.12–15 Inclusion criteria for CRUSADE were patients who presented with: (i) chest pain or anginal equivalent at rest (at least 10min in duration and occurring <24h prior to presentation); (ii) ischaemic electrocardiogram (ECG) changes (ST-segment depression or transient ST-segment elevation); or (iii) elevated biomarker levels with myocardial necrosis (creatine kinase-MB or troponin) above baseline levels. Patients were ineligible if they were transferred into a participating hospital >24h after the last episode of ischaemic symptoms. The CRUSADE hospitals were diverse in size, teaching status, capacity, and region. Participating hospitals collected detailed process of care and in-hospital outcomes data through retrospective chart review, using a standardized data collection form. The institutional review board of each centre approved participation in CRUSADE. As data were collected anonymously, informed consent was not required. Patients ≥65 years of age were linked to CMS longitudinal administrative data (available only for patients 65 years and older) through the end of 2008, using indirect identifiers including site, age, admission date, discharge date, and sex. Details describing the matching algorithm used to match registry data to CMS have been previously described.16 All-cause mortality was available through CMS linkage data. For successfully linked patients, this process provides high-quality information on mortality.
Population
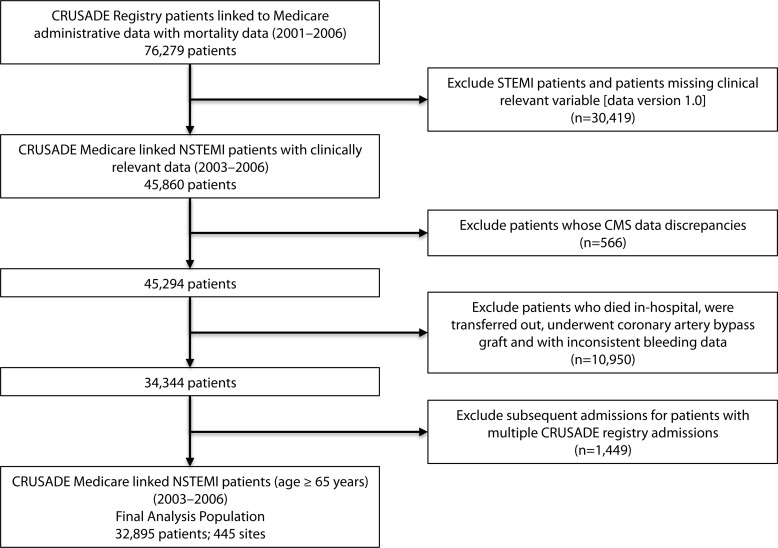
The study population is summarized in Figure 1. Briefly, a total of 76 279 patients ≥65 years of age from 514 CRUSADE hospitals were linked to CMS administrative data through indirect identifiers. Since haematocrit (HCT) and other clinically relevant variables were added to the last version of the data collection form, this analysis population was limited to patients enrolled from 15 February 2003 through 31 December 2006. Also, since only a small number of ST-segment elevation myocardial infarction (STEMI) patients exist in the CRUSADE database, these patients were excluded. Therefore, from the 45 860 NSTEMI patients enrolled in CRUSADE linked to CMS administrative data set with recorded HCT values, we excluded patients whose CMS records did not match for sex (n = 538), who died but were listed as discharged at a later date (n = 28), who died at index hospitalization (n = 2532), who underwent coronary artery bypass grafting (CABG) (n = 3692), who transferred out (n = 4418), who had inconsistent data to determine major bleeding (n = 308), and who had subsequent admissions (non-index) with more than one admission in the CRUSADE registry (n = 1449). Coronary artery bypass grafting patients were excluded, as CABG-associated bleeding is not a part of the in-hospital bleeding definition. The final analysis population included 32 895 patients enrolled from 445 CRUSADE hospitals.
Figure 1.
Study population.
Data definitions
Baseline and nadir (lowest recorded) HCT values were abstracted variables on the data collection form. The CRUSADE bleeding definition10 is comprehensive and based on bleeding variables collected in the registry. CRUSADE major bleeding is defined as intracranial haemorrhage, documented retroperitoneal bleed, absolute HCT decrease ≥12% (baseline to nadir), any red blood cell (RBC) transfusion when baseline HCT ≥28%, or any RBC transfusion when baseline HCT <28% with a witnessed bleed. This HCT cut point of 28% was used to minimize inclusion of transfusions for baseline anaemia at presentation without additional substantiation of witnessed bleeding, which was a variable on the case report form and required evidence of a bleeding site. Blood transfusion was defined as any non-autologous transfusion of whole or packed RBCs. Creatinine clearance (mL/min) was estimated using the Cockcroft–Gault equation.17 Baseline risk for bleeding was presented by the CRUSADE Bleeding Score, where a score of ≤20 represents very low risk of bleeding; 21–30 represents low risk; 31–40, moderate risk; 41–50, high risk; and >50 very high risk.10 To determine the influence of discharge medications on the association between mortality and bleeding, the following discharge medications were included in the regression models: aspirin, clopidogrel, a beta-blocker, a statin, an angiotensin-converting enzyme (ACE)-inhibitor or an angiotensin receptor blocker (ARB), and discharge warfarin.
Statistical analysis
Baseline demographics, clinical presentation, in-hospital therapies (including cardiac medication administered within 24h of hospitalization and in-hospital procedures), and discharge medications were compared between those with major bleeding vs. those without, using the Wilcoxon rank-sum test for comparing continuous variables and Pearson χ2 tests for categorical variables. Continuous variables were presented as medians with inter-quartile ranges, and categorical variables were expressed as frequencies and percentages.
Time to death was calculated from the CRUSADE registry discharge date to the death date. Mortality data were available only through the end of 2008. Therefore, the maximum follow-up time was 5.6 years (February 2003–December 2008) for this study. The primary outcome of interest was death occurring within four different time periods: (i) discharge to 30 days; (ii) 31 days to 1 year; (iii) 1 year to 3 years; and (iv) more than 3 years beyond hospital discharge. Unadjusted event rates were displayed for each of the four time periods. Time-to-event distributions were displayed according to Kaplan–Meier analyses and compared with log-rank tests to illustrate survival among patients who did and did not have in-hospital major bleeding. Cox-proportional hazards modelling was used to examine the association between mortality and in-hospital major bleeding.18 Model 1 investigated the unadjusted association between major bleeding and mortality. Model 2 adjusted for co-variates in the full CRUSADE Long-term Mortality Model19 (plus 10 additional interactions), discharge anti-platelet medications, cardiac catheterization, and revascularization with PCI. The full CRUSADE Long-term Mortality Model is a validated model (c-statistic 0.75) that identified the following variables associated with mortality in this population: age, systolic blood pressure (SBP) on admission, initial serum creatinine, signs of heart failure (HF), prior congestive heart failure (CHF), weight, heart rate on admission, initial HCT, prior stroke, diabetes, initial troponin ratio, prior peripheral artery disease, sex, race, family history of coronary artery disease, hypertension, current/recent smoker, dyslipidaemia, prior myocardial infarction (MI), prior PCI, prior CABG, and ECG findings. The interactions are age by initial serum creatinine, age by SBP on admission, age by signs of HF, age by heart rate on admission, initial serum creatinine by SBP on admission, initial serum creatinine by signs of HF, initial serum creatinine by heart rate on admission, SBP on admission by signs of HF, SBP on admission by heart rate on admission, and signs of HF by heart rate on admission. We controlled for discharge anti-platelet therapies because lack of discharge anti-platelets has been shown to be associated with worse intermediate-term outcomes.20 Revascularization was included in the model, as it has been shown in numerous studies to improve long-term outcomes in the NSTEMI population.
For all variables included in the model, the percentage of missing data was <3%. Missing variables were imputed to the most frequently occurring group for categorical variables and imputed to the median for continuous variables. Missing weight and initial serum creatinine were imputed to the sex-specific median of the non-missing values. Discharge warfarin was missing in ∼10% in our study population. For the unadjusted and adjusted models, a complete case analysis was performed excluding patients with missing discharge warfarin.
To determine whether associations between bleeding and mortality held true for major subgroup populations (age <75 and ≥75 years and males and females), we examined the interaction of age and bleeding, as well as the interactions of sex and bleeding from discharge to 30 days on mortality in the overall population. For statistically significant interactions, hazard ratios (HRs) for mortality from discharge to 30 days among bleeders vs. non-bleeders were calculated. We also analysed the association between in-hospital bleeding and mortality in patients treated with or without PCI.
All comparisons were two-tailed, and a P-value <0.05 was considered statistically significant. All analyses were performed using the SAS software, version 9.2 (SAS Institute, Cary, NC, USA).
Results
Baseline demographics
Of the overall population, 13 090 patients (39.8%) were treated with PCI and 19 578 (59.5%) were not. In-hospital major bleeding occurred in 11.9% (n = 3902) of the overall population, 12.4% (n = 1625) of PCI patients, and 11.6% (n = 2269) of no-PCI patients. Patients who bled were more likely to be female, have co-morbidities, including a history of hypertension, diabetes mellitus, peripheral artery disease, history of HF, prior stroke, higher baseline serum creatinine and lower creatinine clearance, lower baseline HCT, and as expected, had a higher median CRUSADE Bleeding Risk Score (Table 1).10 Those PCI and no-PCI patients who bled were sicker than those who did not bleed, just as observed in the overall study population.
Table 1.
Baseline characteristics according to major bleedinga
| Variable | Overall (n= 32 895) | No major bleed (n= 28 993) | Major bleed (n= 3902) | P-value |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age, years (median, IQR) | 78.0 (72.0, 84.0) | 78.0 (72.0, 84.0) | 79.0 (73.0, 84.0) | 0.0004 |
| Males, n (%) | 16 623 (50.5) | 14 980 (51.7) | 1643 (42.1) | <0.0001 |
| BMI, kg/m2 | 26.6 (23.4, 30.4) | 26.6 (23.4, 30.5) | 26.4 (23.0, 30.4) | 0.0079 |
| Weight, kg | 75.0 (63.5, 87.9) | 75.5 (63.7, 88.0) | 72.6 (61.7, 85.0) | <0.0001 |
| CRUSADE Bleeding Score | 44.0 (32.0, 54.0) | 43.0 (31.0, 53.0) | 52.0 (41.0, 61.0) | <0.0001 |
| Race, n (%) | ||||
| White | 28 136 (85.5) | 24 901 (85.9) | 3235 (82.9) | <0.0001 |
| Black | 2555 (7.8) | 2192 (7.6) | 363 (9.3) | |
| Asian | 233 (0.7) | 189 (0.7) | 44 (1.1) | |
| Hispanic | 913 (2.8) | 794 (2.7) | 119 (3.1) | |
| Other | 525 (1.6) | 458 (1.6) | 67 (1.7) | |
| Medical history, n (%) | ||||
| Hypertension | 25 390 (77.2) | 22 222 (76.7) | 3168 (81.2) | <0.0001 |
| Diabetes mellitus | 11 575 (35.2) | 9937 (34.3) | 1638 (41.9) | <0.0001 |
| PAD | 4876 (14.8) | 4110 (14.2) | 766 (19.6) | <0.0001 |
| Current smoker | 4053 (12.3) | 3546 (12.2) | 507 (13.0) | 0.2094 |
| Dyslipidaemia | 17 004 (51.7) | 14 985 (51.7) | 2019 (51.7) | 0.7442 |
| Prior MI | 10 426 (31.7) | 9216 (31.8) | 1210 (31.0) | 0.2407 |
| Prior PCI | 7069 (21.5) | 6292 (21.7) | 777 (19.9) | 0.0071 |
| Prior CABG | 8396 (25.5) | 7469 (25.8) | 927 (23.8) | 0.0035 |
| Prior CHF | 7929 (24.1) | 6835 (23.6) | 1094 (28.0) | <0.0001 |
| Prior stroke | 4658 (14.2) | 4018 (13.9) | 640 (16.4) | <0.0001 |
| Renal insufficiency | 5945 (18.1) | 4853 (16.7) | 1092 (28.0) | <0.0001 |
| Laboratory results | ||||
| HCT | 38.9 (34.9, 42.5) | 39.1 (35.4, 42.6) | 35.6 (31.3, 41.5) | <0.0001 |
| Serum creatinine | 1.2 (0.9, 1.5) | 1.2 (0.9, 1.5) | 1.3 (1.0, 1.8) | <0.0001 |
| Creatinine clearance (mL/min) by Cockcroft–Gault | 40.1 (28.4, 54.2) | 40.9 (29.2, 55.1) | 34.0 (24.1, 46.5) | <0.0001 |
| Signs and symptoms at presentation | ||||
| Signs of CHF, n (%) | 10 214 (31.1) | 8675 (29.9) | 1539 (39.4) | <0.0001 |
| Heart rate, b.p.m. | 84.0 (70, 101) | 83 (70, 100) | 90 (75, 108) | <0.0001 |
| Systolic blood pressure | 144 (123, 165) | 144 (123, 165) | 141 (118, 165) | <0.0001 |
| ECG findings, n (%) | ||||
| ST depression | 8658 (26.3) | 7388 (25.5) | 1270 (32.6) | <0.0001 |
| Transient ST elevation | 1062 (3.2) | 911 (3.1) | 151 (3.9) | |
BMI, body mass index; b.p.m., beats per minute; CABG, coronary artery bypass grafting; CHF, congestive heart failure; CRUSADE, Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the American College of Cardiology/American Heart Association Guidelines Quality Improvement Initiative; ECG, electrocardiogram; HCT, haematocrit; MI, myocardial infarction; PAD, peripheral arterial disease; PCI, percutaneous coronary intervention.
aVariables presented as median (25th, 75th) unless otherwise indicated.
In-hospital and discharge therapies
Use of unfractionated heparin or glycoprotein IIb/IIIa (GP IIb/IIIa) inhibitors within the first 24h of the hospitalization was associated with an increased likelihood of bleeding (Table 2). Similar results were seen for PCI- and non-PCI-treated patients (data not shown). There was no difference in discharge rates of aspirin or clopidogrel between those who bled vs. those who did not bleed for the overall population and for the no-PCI patients. However, PCI-treated patients were equally likely to get aspirin, but bleeding was associated with a slightly lower likelihood to receive clopidogrel at discharge than no bleeding patients (96.0 vs. 97.2%, respectively, P = 0.002).
Table 2.
In-hospital medications and proceduresa
| Variable | Overall (n= 32 895) | No major bleed (n= 28 993) | Major bleed (n= 3902) | P-value |
|---|---|---|---|---|
| In-hospital acute medication <24h | ||||
| Aspirin | 29 348 (95.3) | 26 034 (95.4) | 3314 (94.7) | 0.0509 |
| Anti-coagulant | 26 018 (80.1) | 22 986 (80.1) | 3032 (79.6) | 0.1314 |
| Heparin | 25 669 (86.9) | 22 672 (86.5) | 2997 (89.8) | <0.0001 |
| Heparin: IV unfractionated | 14 346 (48.5) | 12 411 (47.3) | 1935 (58.0) | <0.0001 |
| Heparin: LMW | 13 119 (44.4) | 11 804 (45.0) | 1315 (39.4) | <0.0001 |
| Beta-blocker | 25 766 (89.8) | 22 843 (89.8) | 2923 (89.8) | 0.7423 |
| Clopidogrel | 15 746 (55.5) | 14 030 (55.4) | 1716 (56.1) | 0.6122 |
| GP IIb/IIIa inhibitors | 10 008 (39.9) | 8728 (39.0) | 1280 (47.7) | <0.0001 |
| Discharge medications | ||||
| Aspirin | 28 166 (93.9) | 25 081 (93.9) | 3085 (94.0) | 0.9192 |
| Clopidogrel | 20 806 (72.9) | 18 531 (72.7) | 2275 (74.7) | 0.0614 |
| Beta-blocker | 27 597 (92.2) | 24 323 (92.0) | 3274 (93.7) | 0.0021 |
| Statin | 23 054 (76.0) | 20 386 (76.0) | 2668 (76.1) | 0.5859 |
| ACE-inhibitor/ARB | 20 581 (67.3) | 18 286 (67.5) | 2295 (65.4) | 0.0021 |
| Warfarin | 3666 (11.4) | 3244 (11.4) | 422 (11.2) | 0.4680 |
| In-hospital procedures | ||||
| Diagnostic catheterization | 20 261 (61.6) | 17 919 (61.8) | 2342 (60.2) | 0.0201 |
| PCI | 13 090 (39.8) | 11 465 (39.5) | 1625 (41.7) | 0.0242 |
| Non-PCI | 19 578 (59.5) | 17 309 (59.7) | 2269 (58.2) | 0.0242 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; GP, glycoprotein; IV, intravenous; LMW, low molecular weight; PCI, percutaneous coronary intervention.
aVariables presented as number (%).
Bleeding and mortality
The individual components of the bleeding definition are shown in Table 3. Bleeding rates were driven primarily by baseline HCT ≥28% and transfusion in both groups, followed by an absolute HCT drop of ≥12% units. Although slightly more retroperitoneal bleeding and HCT drop alone were noted for PCI patients, and more transfusions were noted for no-PCI patients, the results were similar to those seen for the overall population.
Table 3.
Major bleeding component event rates
| Major bleeding components | Event rate (among bleeders) |
||
|---|---|---|---|
| Overall (%) | PCI (%) | No PCI (%) | |
| Absolute HCT drop of ≥12% units | 38.4 | 48.6 | 31.2 |
| Intracranial haemorrhage | 0.5 | 0.0 | 0.8 |
| Retroperitoneal witnessed bleed | 1.5 | 2.5 | 0.8 |
| Baseline HCT ≥28% and transfusion | 71.8 | 68.3 | 74.4 |
| Baseline HCT <28% and transfusion and witnessed a bleed | 3.6 | 1.1 | 5.4 |
HCT, haematocrit; PCI, percutaneous coronary intervention.
Among patients surviving index hospitalization, the cumulative unadjusted mortality rates for the different time periods stratified by patients who bled vs. those who did not, as well as by PCI vs. no-PCI, are presented in Table 4. Cumulative mortality at 30 days was higher in those who had a major bleed than in those without a major bleed (8.4 vs. 5.3%, P < 0.0001) in all groups. Similarly, cumulative mortality at 1 year and 3 years was higher in those who had a major bleed than in those without a major bleed (29.3 vs. 21.0%, P < 0.0001, and 50.5 vs. 38.9%, P < 0.0001, respectively) overall and among patients treated with PCI and no-PCI. Nevertheless, among those who bled, the absolute unadjusted mortality rates were much higher in no-PCI patients when compared with patients who received PCI.
Table 4.
Cumulative mortality rates at 30 days, 1 year, and 3 years according to major bleeding
| Overall (%) |
PCI (%) |
No PCI (%) |
||||
|---|---|---|---|---|---|---|
| No major bleed (n= 28 993) | Major bleed (n= 3902) | No major bleed (n= 11 465) | Major bleed (n= 1625) | No major bleed (n= 17 309) | Major bleed (n= 2269) | |
| Mortality | ||||||
| 30 days | 5.3 | 8.4 | 1.2 | 3.5 | 8.0 | 12.0 |
| 1 year | 21.0 | 29.3 | 7.2 | 15.6 | 30.0 | 39.0 |
| 3 years | 38.9 | 50.5 | 18.8 | 33.9 | 52.0 | 62.4 |
PCI, percutaneous coronary intervention. All unadjusted P < 0.0001.
The overall median follow-up time was 1011 days (1211 days in the PCI group and 834 days in the non-PCI group). The median follow-up time among those patients who died was 389 days (539 days in the PCI group and 257 days in the non-PCI group). Among those patients who died, 86.6% died ≥3 years of discharge and 13.4% died >3 years after discharge. Among those alive at the end of the study, 29.5% had a follow-up time of ≤3 years (median follow-up 929 days) and 70.5% had a follow-up time >3 years.
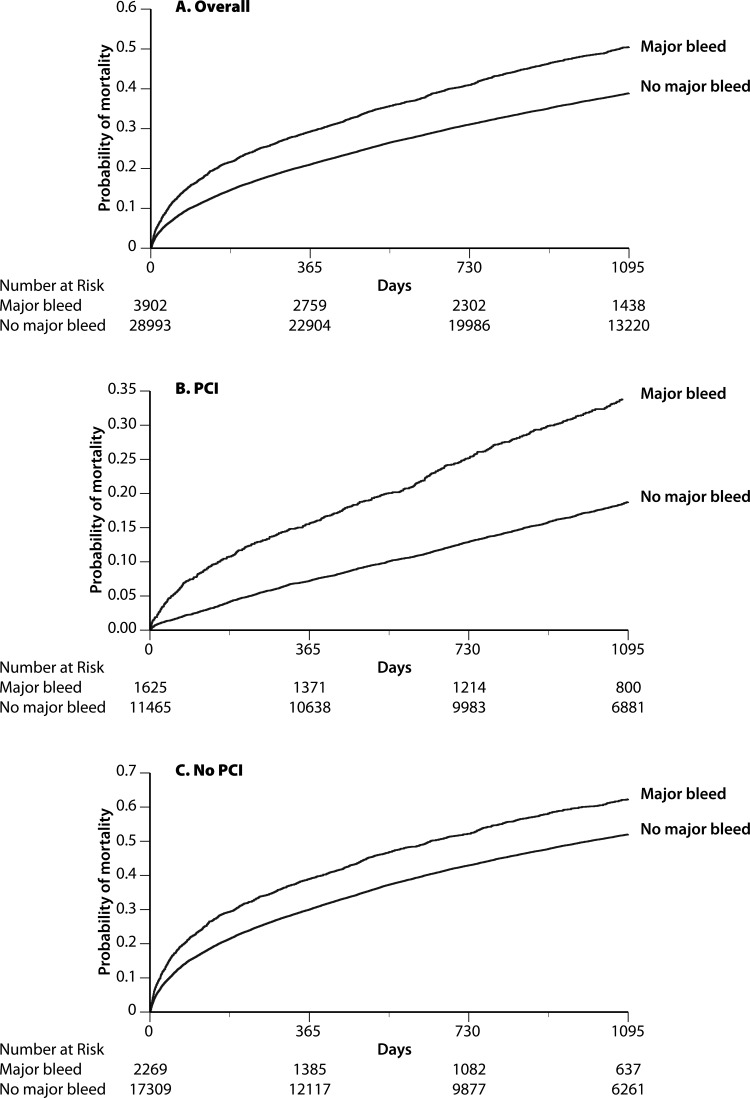
In Figure 2A–C, unadjusted Kaplan–Meier curves of 3-year post-discharge mortality among patients who bled vs. those who did not are presented for the overall, PCI, and no-PCI populations. Major bleeding remained independently associated with mortality up to 3 years (Table 5) after adjustment for co-variates in the full CRUSADE Long-term Mortality Model (including interaction terms), discharge medications, catheterization, and PCI. The strongest association between bleeding and mortality was within the first 30 days after index event [HR 1.33, 95% confidence interval (CI) 1.18–1.51], after which the hazard dropped, but remained significant: (i) for 31 days to 1 year after index event (HR 1.19; 95% CI 1.10–1.29); (ii) for 1 to 3 years (HR 1.09; 95% CI 1.01–1.18); and (iii) attenuating beyond 3 years (HR 1.14; 95% CI 0.99–1.31). Similar results were seen in the PCI patients, but the association between bleeding and mortality remained significant even beyond 3 years. For the no-PCI-treated patients, the association between in-hospital major bleeding and higher mortality became non-significant after 1 year.
Figure 2.
(A–C) Unadjusted Kaplan–Meier curves of 3-year post-discharge mortality among patients who bled vs. those who did not are presented for the (A) overall, (B) PCI (percutaneous coronary intervention), and (C) no-PCI populations.
Table 5.
Major bleeding and adjusted short-, intermediate-, and long-term mortality among hospital survivorsa
| Variable | Overall (n= 29 768) |
PCI (n= 11 968) |
No PCI (n= 17 694) |
|||
|---|---|---|---|---|---|---|
| HR (95% CI for lower/upper) | P-value | HR (95% CI for lower/upper) | P-value | HR (95% CI for lower/upper) | P-value | |
| Major bleed (1–30 days) | 1.33 (1.18–1.51) | <0.0001 | 2.00 (1.44–2.77) | <0.0001 | 1.27 (1.11–1.46) | 0.0006 |
| Major bleed (31 days–1 year) | 1.19 (1.10–1.29) | <0.0001 | 1.48 (1.25–1.75) | <0.0001 | 1.11 (1.02–1.22) | 0.0211 |
| Major bleed (1–3 years) | 1.09 (1.01–1.18) | 0.0318 | 1.23 (1.07–1.42) | 0.0031 | 1.00 (0.91–1.10) | 0.9936 |
| Major bleed (>3 years) | 1.14 (0.99–1.31) | 0.0595 | 1.25 (1.01–1.54) | 0.0404 | 1.02 (0.85–1.23) | 0.8004 |
CI, confidence interval; HR, hazard ratio; PCI, percutaneous coronary intervention.
aAdjusted for the full CRUSADE Long-term Mortality Model co-variates (plus 10 additional interactions), discharge medications (aspirin, clopidogrel, beta-blocker, statin, ACE-inhibitor or ARB, and warfarin), in-hospital catheterization, and in-hospital PCI.
For the overall population, we tested the interaction between age (<75 years and ≥75 years) and bleeding, as well as sex and bleeding, on the outcome of mortality and did not find differential hazards in these subgroups (results not shown).
Discussion
The present analysis demonstrates, in an NSTEMI population, an association between in-hospital major bleeding and long-term mortality (beyond 1 year) after adjustment—well after the effects of the bleeding event itself should have resolved. This supports a persisting hazard which is unlikely due to the actual bleeding event. Our study found that older NSTEMI patients who experienced a major bleed during their index hospitalization but survived to hospital discharge had a 33% increased risk of 30-day mortality. Similar patterns were seen for patients treated with or without PCI. This mortality risk attenuates over time, but remains significant up to 3 years after adjusting for clinical variables, cardiac catheterization, in-hospital revascularization, and discharge medications—particularly among patients treated with PCI.
Our study adds clarity to the long-term implications of bleeding from a registry population. Previous secondary analyses from the Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) and Harmonizing Outcomes with RevascularIZation and Stents in Acute Myocardial Infarction (HORIZONS-AMI) trials have demonstrated the association between bleeding and short-term mortality.5,7,21 More recently, the same group reported a significant association between in-hospital major bleeding and higher mortality and greater morbidity at 3 years in patients with STEMI treated with PCI.22 Other analyses in trial populations have demonstrated the association between bleeding and intermediate-term mortality (1-year mortality).5,8,9 Although these secondary analyses of randomized trial data demonstrated a greater association between major bleeding and 1-year mortality (adjusted HRs between 2.04 and 2.70), our analysis found a more modest association (adjusted HR 1.19).5,7,9 A possible explanation is that our population (with or without bleeding) may have had more co-morbidities (e.g. advanced age, prior stroke, and renal insufficiency) than previously studied clinical trial populations. A greater co-morbidity burden would predispose the non-bleeding population in our cohort to competing mortality risk, thereby lessening the observed effect of bleeding itself. Indeed, the 1-year mortality rates among those who did not bleed was 3.3% compared with 14.1% among patients who bled within 30 days after PCI in a pooled analysis of four Intracoronary Stenting and Antithrombotic Regimen (ISAR) trials,5 and 3.3 vs. 14.4%, respectively, in the ACUITY trial.9 In a subgroup analysis of the latter trial, those patients who did not bleed and were aged from 65 to 74, or ≥75 years, presented 1-year mortality rates of 3.5 and 7.9%, respectively—both of which are substantially lower than what we found in our study.23 As a result, it seems that the hazard of major bleeding is affected by the clinical complexity of the population under study. Nevertheless, despite analysing a population with greater co-morbidities, our analysis demonstrates that major bleeding continues to be associated with mortality beyond 1 year and after fully adjusting with available variables.
In addition, our findings also extend observations from prior registry analyses. In an analysis from the Global Registry of Acute Coronary Events (GRACE), major bleeding was no longer associated with 6-month mortality after adjustment for the known co-morbidities. Those who bled in GRACE had a 6-month mortality of 7.9%, much lower than the 6-month mortality rate of 20.9% seen in our population.1 The authors concluded that co-morbidities associated with major bleeding accounted for the higher rate of mortality in patients who bled.1 There were differences in the two populations. Specifically, our analysis was limited to older patients (age ≥65 years: median age 78 years), and included only US patients with NSTEMI. The median age in the GRACE population was nearly a decade younger, and GRACE included a population from 14 countries with both STEMI and NSTEMI. In the Canadian Acute Coronary Syndromes (Canadian ACS) registry, major bleeding continued to be associated with a greater 1-year mortality after adjustment—even more than that observed in clinical trials [adjusted odds ratio (OR) 3.92 (2.07–7.41)].24 The Canadian ACS trial was limited to only 79 bleeding patients out of the total 5763 and used a different statistical approach. Different bleeding definitions can substantially influence the bleeding rates and association with outcomes.25 Therefore, the observed relationships may be dependent on the population and the definitions used; however, there continues to be confirmation that long-term hazards with major bleeding exist. On the other hand, the rates of bleeding in no-PCI patients are higher (when compared with PCI patients) and the association between bleeding and longer term clinical outcomes is weaker and less sustained. This finding may suggest that in the medically treated population, bleeding provides less additional or unique prognostic information. Alternatively, this finding could be due to differential survival, shorter follow-up, and a smaller percentage of events in medically treated patients.
In our study, there was a stronger association between bleeding and mortality within the first 30 days. Certainly, the negative consequences of a blood transfusion may be limited to the short-term period. Rao et al.26 demonstrated that among NSTEMI patients, transfusion was associated with an increased hazard for 30-day mortality. Similarly, mortality in the short-term could be a direct consequence of a haemodynamically significant bleeding event or subsequent anaemia. Additionally, patients who have major in-hospital bleeding tend to have anti-platelet therapies held upon hospital discharge, but have these therapies resumed in the near future.3 Consequently, withholding these important therapies in the short-term may contribute to increased mortality.20 In our study, there was no significant difference in the use of aspirin at discharge between patients who bled and those who did not. Overall, patients who bled were slightly more likely to have undergone PCI and to receive clopidogrel at discharge. Despite accounting for these potential confounders in our analysis, PCI patients who bled were slightly less likely to receive clopidogrel at discharge, which also could have played some role in the longer hazard associated with bleeding in this subgroup of patients.
The present analysis is the first to demonstrate in a real-world setting among elderly patients that major bleeding continues to be associated with higher mortality at 3 years post-NSTEMI, despite adjustment for multiple factors. In patients with STEMI who are treated with PCI and in a clinical trial setting, in-hospital major bleeding is associated with worse 3-year clinical outcomes.22 Our findings confirm these results and expand them to the NSTEMI elderly population, treated both with and without PCI in clinical practice. As a result, we conclude that major bleeding is most likely a marker of residual unmeasured co-morbidity (i.e. bone marrow suppression, frailty, infection, malignancy, malnutrition, etc.), which increases a person's risk for bleeding during hospitalization, as well as late mortality. Although our study demonstrates an association, it remains to be seen whether preventing bleeding in this at-risk population will translate into improved long-term outcomes.
Limitations
The present analysis was an observational study design limited to patients aged 65 years and older. This long-term association between in-hospital bleeding and long-term mortality needs to be confirmed in a younger cohort. Though we found an association between major bleeding and long-term mortality, causality should not be inferred. Further analyses demonstrating whether minimization of bleeding events in the patients with NSTEMI will result in a reduction of long-term mortality rates are warranted. Of note, The Fifth Organization to Assess Strategies in Acute Ischemic Syndromes (OASIS-5) trial of a newer anti-thrombotic agent suggests that improvement in intermediate survival (6 months) may be achieved by minimizing bleeding complications27; however, this needs to be investigated in the long-term setting and verified, particularly in patients at highest risk for bleeding, who also tend to be at highest risk for ischaemic events. Adjustments for co-variates in our study were limited to those collected in the data collection form. We did not stratify the severity of bleeding events. Prior analysis demonstrated that there is an increasing association between bleeding and mortality with increasing severity of bleeding, as measured by either the Thrombolysis in Myocardial Infarction (TIMI) or Global Use of Strategies to Open Occluded Coronary Arteries (GUSTO) definitions.25 In addition, the Bleeding Academic Research Consortium (BARC) has recently published recommendations on a consensus bleeding definition.28 Unfortunately, we could not apply the BARC definition in the present work. In our study, the bleeding events were site-reported and not adjudicated; therefore, there may be residual confounding. Furthermore, we were unable to control for post-discharge clinical events and their contribution to mortality over time. We also did not have information on long-term medication adherence among patients who did and did not bleed. Among those patients alive at the end of the study, 30% have follow-up ≥3 years. Nonetheless, the median follow-up time among these patients was 929 days (which is ∼2 years, 7 months). Finally, the Medicare administrative claims data that were linked to the CRUSADE registry data contains only information regarding all-cause mortality and does not contain cause-specific mortality.
Conclusions
In-hospital major bleeding in older NSTEMI patients is independently associated with mortality for 3 years among those who survive to hospital discharge. Although this association is strongest in the first 30 days, it remains significant up to 3 years. The association between bleeding and mortality is less sustained among patients with no-PCI. This may represent an association between those who bleed and increased risk of long-term mortality rather than a causal relationship. Nevertheless, major bleeding identifies patients with an increased hazard for mortality beyond the direct result of the bleeding event itself. Consequently, further studies are necessary to determine whether prevention of bleeding may decrease long-term adverse outcomes in this vulnerable population.
Funding
CRUSADE is funded by the Schering-Plough Corporation. Bristol-Myers Squibb/Sanofi Pharmaceuticals Partnership provides additional funding support. Millennium Pharmaceuticals, Inc., also funded this work. This work was also supported in part by a grant from the National Institute on Aging (R01 AG025312-01A1, E.D.P.).
Conflict of interest: R.D.L.: research grants from BMS; T.Y.W.: research grants from BMS/Sanofi Partnership and Merck/Schering-Plough. S.V.R.: consultant for Sanofi-Aventis; E.M.O.: research grants from BMS, Sanofi-Aventis, Merck/Schering-Plough; M.T.R.: research grants from BMS/Sanofi-Aventis and Merck/Schering-Plough, speakers bureau for BMS/Sanofi-Aventis and Merck/Schering-Plough, consulting for Merck/Schering-Plough. E.D.P.: research grants from BMS/Sanofi Pharmaceuticals Partnership, Merck/Schering, and Schering Plough Corporation. Erin LoFrese, who made editorial contributions to this manuscript, did not receive compensation for her assistance, apart from her employment at the institution where the study was conducted.
Acknowledgements
The authors would like to thank Erin LoFrese for her editorial contributions to this manuscript.
References
- 1.Spencer FA, Moscucci M, Granger CB, Gore JM, Goldberg RJ, Steg PG, Goodman SG, Budaj A, FitzGerald G, Fox KA GRACE Investigators. Does comorbidity account for the excess mortality in patients with major bleeding in acute myocardial infarction? Circulation. 2007;116:2793–2801. doi: 10.1161/CIRCULATIONAHA.107.694273. [DOI] [PubMed] [Google Scholar]
- 2.Rao SV, Eikelboom JA, Granger CB, Harrington RA, Califf RM, Bassand JP. Bleeding and blood transfusion issues in patients with non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007;28:1193–1204. doi: 10.1093/eurheartj/ehm019. [DOI] [PubMed] [Google Scholar]
- 3.Wang TY, Xiao L, Alexander KP, Rao SV, Kosiborod MN, Rumsfeld JS, Spertus JA, Peterson ED. Antiplatelet therapy use after discharge among acute myocardial infarction patients with in-hospital bleeding. Circulation. 2008;118:2139–2145. doi: 10.1161/CIRCULATIONAHA.108.787143. [DOI] [PubMed] [Google Scholar]
- 4.Eikelboom JW, Mehta SR, Anand SS, Xie C, Fox KA, Yusuf S. Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation. 2006;114:774–782. doi: 10.1161/CIRCULATIONAHA.106.612812. [DOI] [PubMed] [Google Scholar]
- 5.Ndrepepa G, Berger PB, Mehilli J, Seyfarth M, Neumann FJ, Schömig A, Kastrati A. Periprocedural bleeding and 1-year outcome after percutaneous coronary interventions: appropriateness of including bleeding as a component of a quadruple end point. J Am Coll Cardiol. 2008;51:690–697. doi: 10.1016/j.jacc.2007.10.040. [DOI] [PubMed] [Google Scholar]
- 6.Manoukian SV, Feit F, Mehran R, Voeltz MD, Ebrahimi R, Hamon M, Dangas GD, Lincoff AM, White HD, Moses JW, King SB, III, Ohman EM, Stone GW. Impact of major bleeding on 30-day mortality and clinical outcomes in patients with acute coronary syndromes: an analysis from the ACUITY Trial. J Am Coll Cardiol. 2007;49:1362–1368. doi: 10.1016/j.jacc.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 7.Mehran R, Pocock SJ, Nikolsky E, Clayton T, Dangas GD, Kirtane AJ, Parise H, Fahy M, Manoukian SV, Feit F, Ohman ME, Witzenbichler B, Guagliumi G, Lansky AJ, Stone GW. A risk score to predict bleeding in patients with acute coronary syndromes. J Am Coll Cardiol. 2010;55:2556–2566. doi: 10.1016/j.jacc.2009.09.076. [DOI] [PubMed] [Google Scholar]
- 8.Feit F, Voeltz MD, Attubato MJ, Lincoff AM, Chew DP, Bittl JA, Topol EJ, Manoukian SV. Predictors and impact of major hemorrhage on mortality following percutaneous coronary intervention from the REPLACE-2 Trial. Am J Cardiol. 2007;100:1364–1369. doi: 10.1016/j.amjcard.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 9.Mehran R, Pocock SJ, Stone GW, Clayton TC, Dangas GD, Feit F, Manoukian SV, Nikolsky E, Lansky AJ, Kirtane A, White HD, Colombo A, Ware JH, Moses JW, Ohman EM. Associations of major bleeding and myocardial infarction with the incidence and timing of mortality in patients presenting with non-ST-elevation acute coronary syndromes: a risk model from the ACUITY trial. Eur Heart J. 2009;30:1457–1466. doi: 10.1093/eurheartj/ehp110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Subherwal S, Back RG, Chen AY, Gage BF, Rao SV, Newby LK, Wang TY, Gibler WB, Ohman EM, Roe MT, Pollack CV, Jr, Peterson ED, Alexander KP. Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction: the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA Guidelines) Bleeding Score. Circulation. 2009;119:1873–1882. doi: 10.1161/CIRCULATIONAHA.108.828541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moscucci M, Fox KA, Cannon CP, Klein W, López-Sendón J, Montalescot G, White K, Goldberg RJ. Predictors of major bleeding in acute coronary syndromes: the Global Registry of Acute Coronary Events (GRACE) Eur Heart J. 2003;24:1815–1823. doi: 10.1016/s0195-668x(03)00485-8. [DOI] [PubMed] [Google Scholar]
- 12.Hoekstra JW, Pollack CV, Jr, Roe MT, Peterson ED, Brindis R, Harrington RA, Christenson RH, Smith SC, Ohman EM, Gibler WB. Improving the care of patients with non-ST-elevation acute coronary syndromes in the emergency department: the CRUSADE initiative. Acad Emerg Med. 2002;9:1146–1155. doi: 10.1111/j.1553-2712.2002.tb01569.x. [DOI] [PubMed] [Google Scholar]
- 13.Ohman EM, Roe MT, Smith SC, Jr, Brindis RG, Christenson RH, Harrington RA, Gibler WB, Peterson ED CRUSADE Investigators. Care of non-ST-segment elevation patients: insights from the crusade national quality improvement initiative. Am Heart J. 2004;148:S34–S39. doi: 10.1016/j.ahj.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Bhatt DL, Roe MT, Peterson ED, Li Y, Chen AY, Harrington RA, Greenbaum AB, Berger PB, Cannon CP, Cohen DJ, Gibson CM, Saucedo JF, Kleiman NS, Hochman JS, Boden WE, Brindis RG, Peacock WF, Smith SC, Jr, Pollack CV, Jr, Gibler WB, Ohman EM CRUSADE Investigators. Utilization of early invasive management strategies for high-risk patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE Quality Improvement initiative. JAMA. 2004;292:2096–2104. doi: 10.1001/jama.292.17.2096. [DOI] [PubMed] [Google Scholar]
- 15.Roe MT, Ohman EM, Pollack CV, Jr, Peterson ED, Brindis RG, Harrington RA, Christenson RH, Smith SC, Jr, Califf RM, Gibler WB. Changing the model of care for patients with acute coronary syndromes. Am Heart J. 2003;146:605–612. doi: 10.1016/S0002-8703(03)00388-0. [DOI] [PubMed] [Google Scholar]
- 16.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to Medicare claims data using indirect identifiers. Am Heart J. 2009;157:995–1000. doi: 10.1016/j.ahj.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 18.Allison PD. Survival Analysis Using SAS: A Practical Guide. Cary, NC: SAS Institute, Inc.; 1995. [Google Scholar]
- 19.Roe MT, Chen AY, Thomas L, Wang TY, Alexander KP, Hammill BG, Gibler WB, Ohman EM, Peterson ED. Predicting long-term mortality in older patients after non-ST-segment elevation myocardial infarction: the CRUSADE long-term mortality model and risk score. Am Heart J. 2011;162:875 e1–883 e1. doi: 10.1016/j.ahj.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 20.Chan MY, Sun JL, Wang TY, Lopes RD, Jolicoeur ME, Pieper KS, Rao SV, Newby LK, Mahaffey KW, Harrington RA, Peterson ED. Patterns of discharge antiplatelet therapy and late outcomes among 8,582 patients with bleeding during acute coronary syndrome: a pooled analysis from PURSUIT, PARAGON-A, PARAGON-B, and SYNERGY. Am Heart J. 2010;160:1056.e1–1064.e2. doi: 10.1016/j.ahj.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Rao SV, O'Grady K, Pieper KS, Granger CB, Newby LK, Van de Werf F, Mahaffey KW, Califf RM, Harrington RA. Impact of bleeding severity on clinical outcomes among patients with acute coronary syndromes. Am J Cardiol. 2005;96:1200–1206. doi: 10.1016/j.amjcard.2005.06.056. [DOI] [PubMed] [Google Scholar]
- 22.Suh JW, Mehran R, Claessen BE, Xu K, Baber U, Dangas G, Parise H, Lansky AJ, Witzenbichler B, Grines CL, Guagliumi G, Kornowski R, Wöhrle J, Dudek D, Weisz G, Stone GW. Impact of in-hospital major bleeding on late clinical outcomes after primary percutaneous coronary intervention in acute myocardial infarction the HORIZONS-AMI (Harmonizing Outcomes with RevascularIZation and Stents in Acute Myocardial Infarction) trial. J Am Coll Cardiol. 2011;58:1750–1756. doi: 10.1016/j.jacc.2011.07.021. [DOI] [PubMed] [Google Scholar]
- 23.Lopes RD, Alexander KP, Manoukian SV, Bertrand ME, Feit F, White HD, Pollack CV, Jr, Hoekstra J, Gersh BJ, Stone GW, Ohman EM. Advanced age, antithrombotic strategy, and bleeding in non-ST-segment elevation acute coronary syndromes: results from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol. 2009;53:1021–1030. doi: 10.1016/j.jacc.2008.12.021. [DOI] [PubMed] [Google Scholar]
- 24.Segev A, Strauss BH, Tan M, Constance C, Langer A, Goodman SG Canadian Acute Coronary Syndromes Registries Investigators. Predictors and 1-year outcome of major bleeding in patients with non-ST-elevation acute coronary syndromes: insights from the Canadian Acute Coronary Syndrome Registries. Am Heart J. 2005;150:690–694. doi: 10.1016/j.ahj.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 25.Rao SV, O'Grady K, Pieper KS, Granger CB, Newby LK, Mahaffey KW, Moliterno DJ, Lincoff AM, Armstrong PW, Van de Werf F, Califf RM, Harrington RA. A comparison of the clinical impact of bleeding measured by two different classifications among patients with acute coronary syndromes. J Am Coll Cardiol. 2006;47:809–816. doi: 10.1016/j.jacc.2005.09.060. [DOI] [PubMed] [Google Scholar]
- 26.Rao SV, Jollis JG, Harrington RA, Granger CB, Newby LK, Armstrong PW, Moliterno DJ, Lindblad L, Pieper K, Topol EJ, Stamler JS, Califf RM. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA. 2004;292:1555–1562. doi: 10.1001/jama.292.13.1555. [DOI] [PubMed] [Google Scholar]
- 27.Yusuf S, Mehta SR, Chrolavicius S, Afzal R, Pogue J, Granger CB, Budaj A, Peters RJ, Bassand JP, Wallentin L, Joyner C, Fox KA Fifth Organization to Assess Strategies in Acute Ischemic Syndromes Investigators. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med. 2006;354:1464–1476. doi: 10.1056/NEJMoa055443. [DOI] [PubMed] [Google Scholar]
- 28.Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, Kaul S, Wiviott SD, Menon V, Nikolsky E, Serebruany V, Valgimigli M, Vranckx P, Taggart D, Sabik JF, Cutlip DE, Krucoff MW, Ohman EM, Steg PG, White H. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123:2736–2747. doi: 10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]