Abstract
Background
Obesity and depression are closely linked, and each has been associated with disability. However, few studies have assessed inter-relationships between these conditions.
Design and Methods
In this study, 4 641 women aged 40-65 completed a structured telephone interview including self-reported height and weight, the Patient Health Questionnaire (PHQ) assessment of depression, and the World Health Organization Disability Assessment Schedule II (WHODAS II). The survey response rate was 62%. We used multivariable regression models to assess relationships between obesity, depression, and disability.
Results
The mean age was 52 years; 82% were white; and 80% were currently employed. One percent were underweight, 39% normal weight, 27% overweight, and 34% obese. Mild depressive symptoms were present in 23% and moderate-to-severe symptoms were present in 13%. After multivariable adjustment, depression was a strong independent predictor of worse disability in all 7 domains (cognition, mobility, self-care, social interaction, role functioning, household, and work), but obesity was only a significant predictor of greater mobility, role-functioning, household, and work limitations (P<0.05) (overweight was not significantly associated with any disability domain). Overall, the effect on disability was stronger and more pervasive for depression than obesity, and there was no significant interaction between the two conditions (P>0.05). Overweight and obesity were associated with 5 760 days of absenteeism per 1 000 person-years, and depression was associated with 18 240 days of absenteeism per 1 000 person-years.
Conclusions
The strong relationships between depression, obesity and disability suggest that these conditions should be routinely screened and treated among middle-aged women.
Keywords: obesity, depression, disability, absenteeism
Introduction
There is a strong bi-directional relationship between obesity and depression in women(1-5) Our prior work indicates that the prevalence of moderate and severe depression increases four-fold when comparing women with a normal body mass index (BMI 18.5 to 24.9 kg/m2; prevalence of depression 7%) to those with severe obesity (BMI ≥35 kg/m2; prevalence of depression 26%).(1) Similarly, the prevalence of obesity (BMI ≥30 kg/m2) is strongly associated with depression, occurring in 25% of women with no depressive symptoms and in 58% of women with moderate and severe depressive symptoms.
There is also strong evidence that obesity and depression are each associated with disability,(6-12) and the World Health Organization currently ranks depression as the leading cause of disability world-wide.(13) However, few studies have assessed the inter-relationships between obesity, depression, and disability. One study found a relationship between obesity and disability in adults with diabetes, but they found no relationship between depression and disability in the same cohort.(14) Conversely, another study of preretirement adults found that depression was strongly associated with developing activities of daily living disability after adjustment for obesity; however, this study did not report on the inter-relationships between depression, obesity, and disability.(15)
The present paper uses data from a large sample of middle-aged women enrolled in a prepaid health plan to assess (1) whether obesity and depression have independent effects on disability, (2) whether obesity and depression have specific effects on different domains of disability, (3) whether the combination of obesity and depression exacerbates disability (i.e., multiplicative effects), and (4) the overall population impact of obesity and depression on disability and absenteeism.
Materials / subjects and Methods
We conducted this study at Group Health, a mixed-model, health insurance and care delivery system serving approximately 600 000 members in Washington State. Study procedures were approved by the Group Health Institutional Review Board. Group Health enrollment is predominately white (85%), with higher education levels than the regional community. Compared to the rest of the United States, Group Health members are more likely to be Asian or Pacific Islanders (9% versus 4%), but less likely to be African American (4% versus 12%) or report Hispanic ethnicity (4% versus 15%). Group Health has a slightly higher proportion of women (53%) than the regional community (50%) and the nation (51%). Group Health members are also older (46% (39%). To provide a more diverse sample in terms of race and ethnicity, we recruited participants from eight Group Health primary care clinics with higher rates of minority enrollment.
Data used in this paper were obtained through a population-based survey of middle-aged women enrolled in Group Health. All women aged 40 and older enrolled in Group Health are invited to complete periodic breast cancer risk questionnaires,(16) which include questions on self-report of height and weight. For the present study, women who last reported a BMI of 30 kg/m2 or more were sampled at 100%, women who last reported a BMI less than 30 kg/m2 were sampled at 12%, and women with unknown BMI or those who did not complete a screening questionnaire in the last five years were sampled at 25%. This stratified sampling procedure was intended to increase the efficiency of the survey in identifying women with BMI ≥30 kg/m2 and to permit correction for any differences in response rates between sampling strata. All analyses incorporated sampling weights so that results accurately reflect the entire target population.
All sampled participants were mailed a letter inviting them to participate in a telephone survey. The letter included a $5 gift card incentive and a phone number through which potential participants could decline further contact. Those who did not decline were contacted by telephone beginning approximately one week after the mailing. Participants received no additional compensation for completing the survey.
Surveys were conducted by certified interviewers from Group Health’s survey research program. Each interviewer received at least 8 h of general interview training and 4 h of project-specific training. Certification required satisfactory performance in two role-play interviews and two observed interviews. Contact protocols required a minimum of nine contact attempts, including attempts during evening and weekend times. A total of 4 641 female health plan enrollees aged 40-65 years completed the interview, which assessed the following:
Demographic measures
The survey included measures of age; ethnicity; and race. Based on the frequency distributions and known associations with obesity, a new race/ethnicity measure with 3 levels was created: (1) White non-Hispanic, (2) Asian/Pacific Islander; and (3) Other (African American, Hispanic, and American Indian/Alaskan Native), where ethnicity took precedence over race.
Height, weight, and BMI measurement
The self-reported height and weight data included in the survey were used to calculate to body mass index scores (kg/m2). Participants were categorized as overweight if the BMI was between 25.0 and 29.9 kg/m2 and obese if their BMI value was 30 kg/m2 or greater.(17) In prior research we assessed the validity of self-reported height and weight information using data from a subsample of 250 women reporting BMI of 30 kg/m2 or more (135 of whom met the American Psychiatric Association DSM-IV diagnostic criteria for clinical depression) who were also invited to participate in an in-person visit to assess eligibility for a treatment study.(18) At this visit, height was measured by stadiometer and weight was measured by triple-beam balance. Comparison of self-reported height and weight with directly measured height and weight obtained on average 26 (SD = 19) days later found that depressed women underestimated their height by 0.002 m (s.e. = 0.003) and underestimated their weight by 1.47 kg (s.e. = 0.04). Underestimates of height and weight in non-depressed women averaged 0.003 m (s.e. = 0.002) and 1.21 kg (s.e. = 0.4), respectively. Differences between the groups were not statistically significant. Additionally, the magnitude of the difference in self-report bias was not large enough to appreciably influence obesity prevalence rate comparisons between obese and non-obese women (i.e., the BMI cut point would change by <0.2%). Pearson’s correlations between measured and self-reported heights and weights were r = 0.92 and 0.95, respectively.(18)
Depressive symptoms
Depression was assessed using the 9-item Patient Health Questionnaire,(19) which examines the nine DSM-IV criteria for major depression.(20) Validation studies have shown excellent agreement between the self-report PHQ and a clinician-administered structured interview in samples of general medical outpatients and medical inpatients.(19, 21) A dimensional score was calculated as the total of all 9 items (possible range 0–27), which was dichotomized at ≥10 (depressed) versus <10 (not depressed) or more, a cut-point previously found to represent a moderate level of depressive symptoms.(22)
Outcome measures – disability, employment status, and absenteeism
We used a modified version of the World Health Organization Disability Assessment Schedule II (WHODAS II), a multidimensional measure of functioning and disability.(8, 23) Standard items in the WHODAS II inquire about functioning in the last 30 days. Using a subset of the standardized WHODAS II questions, we examined disability in the following 7 domains: cognitive functioning, mobility, self-care, social functioning, role functioning, household functioning, and work functioning. For example, a question related to cognitive functioning inquires, “during the past 30 days, how much difficulty did you have concentrating on doing something for ten minutes?” And a question related to work functioning asks, “in the past 30 days how much difficulty did you have in carrying out your day to day activities?” Each domain included 4 questionnaire items like these, and each question was scaled from one (no limitations) to 4 (severe limitations). Domain scores were summed and transformed to a 0 to 100 scale. We also included standard WHODAS II questions related to current employment status and absenteeism (number of days missed work) during the past month.
Statistical Analyses
We used STATA 11.1 (College Station, TX) to examine population characteristics; means and standard deviations were calculated for continuous variables and frequencies and proportions for categorical variables. We used STATA survey commands to generate multivariable linear and logistic regression models to assess relationships between obesity, depression, and disability measures. We ran unadjusted regression models to ascertain the unadjusted effect of both obesity and depression on the disability domains. We then examined fully adjusted models, which included known covariates and the presence of the other risk factors. Finally, we examined whether the interaction of obesity X depression predicted any disability domain beyond main effects. Nineteen underweight women (0.4% of the sample with a BMI <18.5 kg/m2) were excluded from our multivariable analyses. Covariates included age, race, education, smoking status, and a pharmacy-based risk adjuster (RxRisk).(24, 25) The RxRisk is a measure of the burden of comorbid illness that uses automated pharmacy data to predict future health care expenditures. Greater RxRisk scores equate to greater current burden of pharmacy use and greater predicted expenditures in the next year. All analyses incorporate sampling weights to account for the stratified sampling procedure described above and for differential response rates across sampling strata. All statistical tests were two-sided and the significance level was based on p<0.05.
Results and Discussion
Survey response
Of the 8 000 potential participants who were mailed invitation letters, 442 were found to be ineligible (had since died, moved away, or disenrolled from the health plan). Of the remaining 7 558 eligible women, 865 could not be reached by telephone and 2 033 declined to participate, leaving 4 660 participants (62% of those eligible). Nineteen participants had missing data on one or more key variables, so 4 641 were included in analyses presented here. Participation varied significantly across sampling strata (63% among those who reported BMI of 30 kg/m2 or more on the breast cancer screening questionnaire vs. 59% among those reporting BMI less than 30 kg/m2 vs. 34% among those declining to participate in breast cancer screening, (p <0.001).
Population characteristics
Among the 4 641 respondents included in the analyses, the mean age was 52 years; 66% were married; 58% were college graduates; and 9.7% were current smokers (Table I). A total of 3.7% reported Hispanic ethnic origin; and for race categories, 2.5% reported American Indian/Alaskan Native, 8.3% Asian/Pacific Islander (7.4% Asian and 0.9% Native Hawaiian or other Pacific Islander), 7.0% African American, and reported 82.3% White race. The average BMI was 28.5 kg/m2, with 27% of women classified as overweight (BMI 25.0-29.9 kg/m2) and 34% classified as obese (BMI ≥30 kg/m2). Most of the women (64%) had no significant depressive symptoms, while 23% had mild depressive symptoms (PHQ score 5.0-9.9) and 12.9% had moderate-to-severe depressive symptoms (PHQ ≥10). Consistent with the usual demographics of this health plan’s members, 80% of the women in this sample were currently employed full time or part time. Another 2.3% were unemployed, and 3.0% were disabled or on sick leave. Among employed women, nearly one-quarter (23%) of the sample had been absent from work during the past month, and 9% reported work limitations occurring all or most of the time they were at work. Finally, the prevalence of self-reported disability varied by domain, with a low of 7% reporting any limitations in self-care activities and a high of 46% reporting any limitations in household activities (see Table I).
Table I.
Population characteristics – a representative sample of 4641 female health plan enrollees aged 40-65 years
| Characteristic | Result |
|---|---|
| Total Sample, | N 4641 |
| Mean age, years | 52.1 |
| Mean BMI, kg/m2 | 28.5 |
| Mean PHQ score | 4.4 |
| Mean RxRisk score | 1777.2 |
| % White race | 82.3% |
| % Married/living as married | 65.8% |
| % College graduate | 58.2% |
| % Current smoker | 9.7% |
| Depressive Symptoms (PHQ) | |
| % None (PHQ <5) | 63.9% |
| % Mild (PHQ ≥5 to<10) | 23.1% |
| % Moderate-Severe (PHQ ≥10) | 12.9% |
| Body Mass Index (BMI) Categories | |
| % Normal Weight (BMI 18.5-24.9) | 39.4% |
| % Overweight (BMI 25.0-29.9) | 26.7% |
| % Obese (BMI ≥30.0) | 33.9% |
| Employment | |
| % Employed (full time or part time) | 79.6% |
| % Unemployed | 2.3% |
| % Temporarily Laid Off | 0.8% |
| % Sick Leave | 0.2% |
| % Disabled | 2.8% |
| % Other work status (student; homemaker, retired) | 14.2% |
| Mean days of work missed in past month | 0.8 |
| % Any absenteeism in past month | 23% |
| % Self-reported work limitations (all or most of time) | 9.3% |
| Self-reported Disability | |
| % Any Cognitive Problem | 26% |
| % Any Mobility Problem | 27% |
| % Any Self Care Problem | 7% |
| % Any Social Problem | 17% |
| % Any Role Functioning Problem | 24% |
| % Any Household Problem | 46% |
| % Any Work Problem | 45% |
BMI = body mass index; PHQ = Patient Health Questionnaire measurement of depression (range of possible scores 0-27); RxRisk = a pharmacy-based risk adjuster (higher RxRisk indicates greater burden of comorbid disease)
Disability outcomes
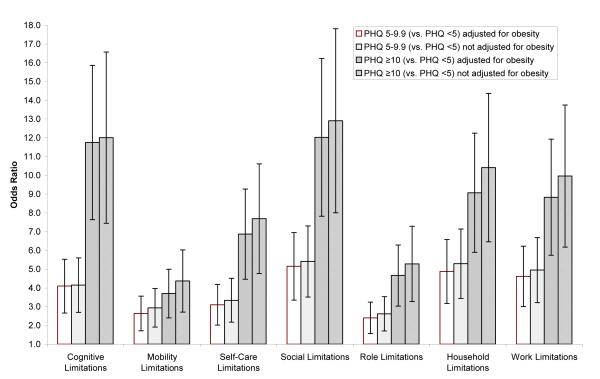
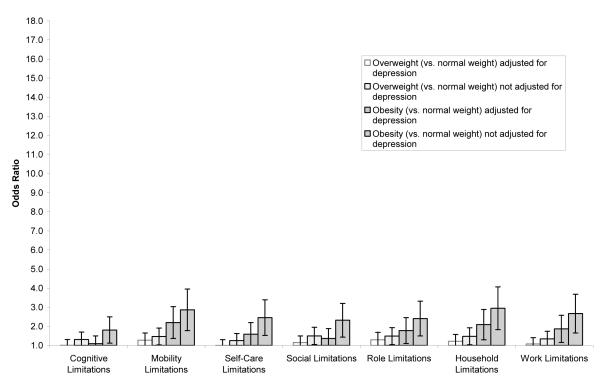
In unadjusted regression models, higher BMI and greater depressive symptoms were both strongly associated with greater self-reported disability in every domain of the WHODAS (P<0.001 for cognitive, mobility, self-care, social, role, household, and work limitation domains; results not shown). After adjusting for age, race, college education, current smoking status, and Rx Risk score (Figure 1), women with PHQ scores indicating mild (5.0-9.9) and moderate-to-severe depressives symptoms (significantly greater odds of reporting any cognitive, mobility, self-care, social, role, household, and work limitation domains compared to women with no depressive symptoms (PHQ <5). The magnitude of the association between PHQ scores and disability outcomes was only slightly reduced after adjusted for BMI categories (1st and 3rd bars). After adjusting for age, race, college education, current smoker, and Rx Risk score (Figure 2), women with a BMI in the overweight range did not have significantly greater odds of reporting disability in any of the domains we examined compared to women with a normal BMI; however, women with a BMI in the obese range did have significantly greater odds of mobility, role, household, and work limitations than women with a normal BMI (P<0.05; Figure 2). In this case however, the magnitude of the association between BMI and disability outcomes was significantly reduced after adjusted for PHQ scores (1st and 3rd bars). Finally, we observed no statistically significant interactions between depressive symptoms and BMI categories in any of our analyses of disability outcomes (P>0.05 for all comparisons).
Figure 1.
Multivariable Adjusted* Odds Ratios of Having Any Limitations in Seven Domains of Disability across Levels of Depressive Symptoms
*First and third bars for each domain are adjusted for BMI, age, race, college education, smoking, and Rx Risk; second and fourth bars for each domain are not adjusted for BMI but are adjusted for age, race, college education, smoking, and Rx Risk; thin lines indicate 95% confidence intervals
Figure 2.
Multivariable Adjusted* Odds Ratios of Having Any Limitations in Seven Domains of Disability across Categories of Body Mass Index
*First and third bars for each domain are adjusted for PHQ, age, race, college education, smoking, and Rx Risk; second and fourth bars for each domain are not adjusted for PHQ but are adjusted for age, race, college education, smoking, and Rx Risk; thin lines indicate 95% confidence intervals
When examining the relationships between obesity and depression with disability, there were notable differences in the patterns of the association. Obese women reported relatively large limitations in mobility, role, household, and work functioning (Figure 2). On the other hand, women with severe depression reported relatively large limitations in cognitive and social functioning in addition to large impacts on household and work functioning (Figure 1). Notably, the magnitude of the associations between severe depression and disability (OR range: 3.7-12.0) were much greater than the associations between obesity and disability (OR range: 1.1-2.2).
Next, we examined the relationships between BMI categories, depressive symptoms, current employment status and absenteeism (Table II). Once again, in unadjusted regression models, higher BMI and greater depressive symptoms were both strongly associated with a higher prevalence of disabled work status (P<0.05). Similarly, among employed women, higher BMI and depressive symptoms were associated with the number of days absent from work (P<0.05). Overall, 22% of overweight women and 31% of obese women reported any absenteeism in the past month, compared with 17% of normal weight women. Furthermore, 32% of women with mild depressive symptoms and 47% of women with moderate-to-severe depressive symptoms reported any absenteeism in the past month, compared to 16% of women with no depressive symptoms. After adjusting for BMI, age, race, college education, current smoker, and Rx Risk score (data not shown), women with PHQ scores in the mild or moderate-to-severe depressive symptom range had significantly greater odds of reporting any disability leave and absenteeism compared to women with no depressive symptoms (PHQ <5). After adjusting for PHQ, age, race, college education, current smoker, and Rx Risk score (data not shown), overweight and obese women had significantly greater odds of reporting any days absent from work compared to normal weight women; however, overweight and obese status were no longer significantly associated with unemployment/disability/sick leave.
Table II.
Trends in unadjusted work-related unemployment, sick leave, disability, absenteeism, and work limitations among employed women, by BMI and PHQ categories*
| Work Status | Normal Weight |
Over- weight |
Obese | P value for trend* |
PHQ <5 |
PHQ 5.0-9.9 |
PHQ ≥10 |
P value for trend* |
|---|---|---|---|---|---|---|---|---|
| % Unemployed | 1.4% | 3.9% | 2.2% | 0.30 | 1.2% | 4.0% | 4.8% | 0.05 |
| % Temporarily Laid Off |
1.1% | 0.5% | 0.6% | 0.16 | 0.7% | 0.4% | 1.7% | 0.23 |
| % Sick Leave | 0.1% | 0.3% | 0.2% | 0.68 | 0.0% | 0.1% | 1.2% | 0.07 |
| % Disabled | 1.1% | 2.9% | 4.9% | <0.05 | 1.7% | 3.7% | 7.3% | <0.05 |
| Mean days of work missed in past month |
0.5 | 0.8 | 1.1 | <0.05 | 0.4 | 1.2 | 2.0 | <0.05 |
| % Any absenteeism in past month |
17.4% | 22.9% | 31.0% | <0.05 | 16.1% | 31.7% | 47.4% | <0.05 |
| % Work limitations (all or most of time) |
7.5% | 8.2% | 12.3% | 0.03 | 6.6% | 10.7% | 21.3% | <0.05 |
BMI = body mass index; Normal Weight = BMI 18.5-24.9, Overweight = BMI 25.0-29.9, and Obese = BMI possible scores 0-27); P-values indicate the unadjusted trend across BMI and PHQ categories separately
Population-attributable calculations for absenteeism
We also estimated the population-level impact of excess body weight and depressive symptoms among employed women in this cohort (Table 3). After adjusting for PHQ, age, and race, the 2 166 overweight and obese employed women in this cohort averaged 0.48 more days of absenteeism per month than normal weight employed women. Thus, excess body weight was associated with 5 760 days of absenteeism per 1 000 person-years. Women with mild, moderate, and severe depressive symptoms averaged 1.52 more days of absenteeism per month than non-depressed women. Thus, depressive symptoms were associated with 18 240 days of absenteeism per 1 000 person-years. Our cohort of 4 641 women reported a total of 6 990 days absent from work per month, which annualizes to approximately 83 000 absentee days per year. Based on our calculations, roughly 35 000 (42%) of days absent from work may be attributed to excess weight and depressive symptoms.
Table III.
Population-level impact of excess body weight and depressive symptoms on absenteeism in our study sample
| Average Number of Days Missed from Work per Month Compared with Normal Weight and Non-depressed Women* |
|
| BMI ≥25 kg/m2* | 0.48 |
| PHQ ≥5 | 1.52 |
| Average Number of Days Missed from Work per 1000 person-years Compared with Normal Weight and Non-depressed |
|
| Women* BMI ≥25 kg/m2* | 5,760 |
| PHQ ≥5 | 18,240 |
| Number of Employed Women With the Condition in Our Sample | |
| BMI ≥25 kg/m2* | 2,166 |
| PHQ ≥5 | 1,260 |
| Total Number of Days Missed from Work Per Month Among Employed Women With the Condition in Our Sample |
|
| BMI ≥25 kg/m2* | 1,040 |
| PHQ ≥5 | 1,915 |
| Total Number of Days Missed from Work Per Year Among Employed Women With the Condition in Our Sample |
|
| BMI ≥25 kg/m2* | 12,476 |
| PHQ ≥5 | 22,982 |
Restricted to employed women only and adjusted for age, race, college education, current smoker, and Rx Risk score; BMI = body mass index; PHQ = Patient Health Questionnaire measurement of depression (range of possible scores 0-27)
Finally, to further illustrate the impact of impact of increasing BMI and depressive symptoms on presenteeism (work performance) among employed women, Figure 3 presents the associations between BMI categories, PHQ categories, and the proportions of employed women reporting mild, moderate, and severe difficulty with day-to-day work activities. Once again, the larger magnitude of the relationship between increasing depressive symptoms and disability is clearly illustrated.
Figure 3.
Proportions of employed women (80% of total sample) reporting mild, moderate, and severe difficulty carrying out their day-to-day work, by BMI category and PHQ score*
*adjusted for age, race, education, smoking status, and a pharmacy-based risk adjuster (RxRisk)
Discussion
Obesity and depression are both very common health conditions among middle age women. In this large, representative cohort from a single health plan in Washington State, we found that obesity was a significant predictor of greater disability in the areas of mobility, role functioning, household functioning, and work, but not the cognition, self-care, and social domains. Notably, women who were overweight, but not obese, were no more likely to report disability than normal weight women after adjusting for depression and other covariates. We also found that depressive symptoms were a strong independent predictor of worse disability in all 7 domains that were examined, and that both mild and moderate levels of depression were associated with worse levels of disability. The associations between obesity or depression and disability persisted after adjusting for age, race, education, smoking status, and a pharmacy-based risk adjuster. The strong independent relationships between these health conditions and disability suggest that obesity and depression should be routinely screened and treated in this population.
Our analyses also indicate that obesity and depression have differential effects on disability. Obesity appears to have its strongest effects on mobility limitations, which may also be reflected in measures of household and work disability. For example, the area of household limitations that was most commonly endorsed was “getting household work done quickly as needed,” an area in which mobility limitations may reduce the speed at which work can be performed. On the other hand, depressive symptoms were most strongly associated with cognitive and social limitations and least strongly associated with mobility problems. It is notable, however, that the magnitude of the effect of depressive symptoms on mobility appeared to be at least as strong as the effect of obesity on mobility. Women reporting depressive symptoms were much more likely, however, to endorse “difficulties in concentrating,” “remembering to do important things,” and “starting or maintaining conversations.”
Notably, we found that there were no significant interactions between obesity and depression in any of the disability domains examined in this cohort. This finding suggests that the effects of obesity and depression on disability are independent and do not require the presence of the other health condition to be manifested. In other words, the independent effects of obesity and depression on disability are likely to be additive, rather than multiplicative, in this population. However, we also observed that much of the effect of obesity on disability was explained by co-morbid depression (the odds ratios were significantly reduced in Figure 2 when we adjusted for PHQ), but that obesity explained very little of the effect of depression on disability (the odds ratios were not impacted much in Figure 1 when we adjusted for BMI). The main clinical implication of this finding is that each of these conditions needs to be treated and reduced in this population to most effectively reduce the prevalence of disability, but that depression has the larger independent effect.
Another important finding in our study was that obesity and depression were each associated with significant absenteeism. The overweight and obese women in this study population were absent one-half day more per month than normal weight women, and women with mild-or-greater depressive symptoms were absent one-and-a-half days more per month than women without depressive symptoms. Thus, among middle-aged women, excess body weight is associated with 5 760 days of absenteeism per 1 000 person-years, and depression is associated with 18 240 days of absenteeism per 1 000 person-years. To further illustrate the effect, in this modest-sized cohort of 4 641 women, these two health conditions were associated with over 35 000 days of absenteeism annually, representing roughly 42% of all absentee days experienced each year. Absenteeism of this magnitude is likely to have significant economic consequences for employers.(26-28) Indeed, prior research by Cawley and colleagues estimated the annual cost of obesity-related absenteeism at $4.3 billion annually in the United States (2 004 dollars).(29) Given that both obesity and depression are potentially treatable (and reversible) health conditions, we believe these findings should be a call to action among employers to place greater emphasis on prevention, screening, and treatment of obesity and depression in their wellness programs.
Several limitations of this study should be noted. Height and weight were assessed by self-report. Previous methodological research suggests that self-reported height and weight are highly correlated with direct physical measurements, but self-report tends to consistently underestimate weight and overestimate height. In a sub sample of participants in this study, weight was underreported by less than 1.5 kg on average, and correlation between self-reported and measured weight was 0.98. We would not expect that a general tendency to underreport weight would affect the association between obesity and depression. Previous studies demonstrating an association between obesity and depression have included both self-report and physical measurements of height and weight. Second, depression was assessed by non-clinicians using a structured research interview rather than by a full clinical assessment. Compared to the gold standard of a clinician assessment, the validity of the PHQ is as good as or better than alternative measures used in previous studies.(22, 30, 31) This cross-sectional study cannot establish the direction of the causal relationship between obesity, depression, and disability or the mechanisms underlying those relationships. The link between obesity, depression, and disability is likely mediated through numerous mechanisms, including the related chronic health condition such as low back pain, osteoarthritis, cardiovascular disease, and diabetes.(32-34) One possible limitation of this study is the potential for overlap on a few of the individual items on the PHQ and WHODAS (e.g., items related to difficulty concentrating and moving slowly); however, the overwhelming majority of items do not overlap and, overall, we believe that only a very small amount of the association between disability and depression seen in this study is likely to be attributable to overlap in symptoms. Another limitation is our use of disability measures that were drawn from a longer self-report survey, the WHODAS II. While the WHODAS II has been previously validated in the full version, our modified (shorter) version may misclassify women with disabilities in this modified format. Finally our sample only included middle-age women, so we are unable to assess these relationships among other age ranges and among men.
In conclusion, in this large, population-based sample of middle aged women, we find strong evidence for independent effects of obesity and depression on disability. Disability has been linked to greater work absenteeism, and in our multidimensional assessment of disability, we find that the primarily physical impacts of obesity are associated with less absenteeism than the more globally disabling aspects of depression. However, the greater prevalence of overweight and obesity translate into significant population-level impacts. We believe that these findings have important implications for employers and health insurance organizations as they consider the optimal design of employee wellness programs.
Acknowledgments
This project was supported by NIH Research Grant #MH68127 funded by the National Institute of Mental Health and the Office of Behavioral Social Sciences Research. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Dr. Arterburn had full access to the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors declare no conflict of interest.
References
- 1.Simon GE, Ludman EJ, Linde JA, et al. Association between obesity and depression in middle-aged women. Gen Hosp Psychiatry. 2008;30:32–9. doi: 10.1016/j.genhosppsych.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Linde JA, Jeffery RW, Finch EA, et al. Relation of body mass index to depression and weighing frequency in overweight women. Prev Med. 2007;45:75–9. doi: 10.1016/j.ypmed.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faubel M. Body image and depression in women with early and late onset obesity. J Psychol. 1989;123:385–95. doi: 10.1080/00223980.1989.10542993. [DOI] [PubMed] [Google Scholar]
- 4.Atlantis E, Baker M. Obesity effects on depression: systematic review of epidemiological studies. Int J Obes (Lond) 2008;32:881–91. doi: 10.1038/ijo.2008.54. [DOI] [PubMed] [Google Scholar]
- 5.Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 6.Alley DE, Chang VW. The changing relationship of obesity and disability, 1988-2004. JAMA. 2007;298:2020–7. doi: 10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- 7.Bell MP, McLaughlin ME, Sequeira JM. Age, disability, and obesity: Similarities, differences, and common threads. In: Stockdale MS, Crosby, Faye J, editors. The psychology and management of workplace diversity. 2004. [Google Scholar]
- 8.Chwastiak LA, Von Korff M. Disability in depression and back pain: evaluation of the World Health Organization Disability Assessment Schedule (WHO DAS II) in a primary care setting. J Clin Epidemiol. 2003;56:507–14. doi: 10.1016/s0895-4356(03)00051-9. [DOI] [PubMed] [Google Scholar]
- 9.Gregg EW, Guralnik JM. Is disability obesity’s price of longevity? JAMA. 2007;298:2066–7. doi: 10.1001/jama.298.17.2066. [DOI] [PubMed] [Google Scholar]
- 10.Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures. Results from the WHO Collaborative Study on Psychological Problems in General Health Care. Jama. 1994;272:1741–8. doi: 10.1001/jama.272.22.1741. [DOI] [PubMed] [Google Scholar]
- 11.Simon GE. Social and economic burden of mood disorders. Biol Psychiatry. 2003;54:208–15. doi: 10.1016/s0006-3223(03)00420-7. [DOI] [PubMed] [Google Scholar]
- 12.Sturm R, Ringel JS, Andreyeva T. Increasing Obesity Rates and Disability Trends. Health Aff (Millwood) 2004;23:199–205. doi: 10.1377/hlthaff.23.2.199. [DOI] [PubMed] [Google Scholar]
- 13.Mental Health: Depression. World Health Organization; 2011. [Google Scholar]
- 14.Gregg EW, Mangione CM, Cauley JA, et al. Diabetes and incidence of functional disability in older women. Diabetes Care. 2002;25:61–7. doi: 10.2337/diacare.25.1.61. [DOI] [PubMed] [Google Scholar]
- 15.Dunlop DD, Manheim LM, Song J, Lyons JS. Chang RW. Incidence of disability among preretirement adults: the impact of depression. Am J Public Health. 2005;95:2003–8. doi: 10.2105/AJPH.2004.050948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taplin SH, Thompson RS, Schnitzer F, Anderman C, Immanuel V. Revisions in the risk-based Breast Cancer Screening Program at Group Health Cooperative. Cancer. 1990;66:812–8. doi: 10.1002/1097-0142(19900815)66:4<812::aid-cncr2820660436>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 17.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 18.Jeffery RW, Finch EA, Linde JA, et al. Does clinical depression affect the accuracy of self-reported height and weight in obese women? Obesity (Silver Spring) 2008;16:473–5. doi: 10.1038/oby.2007.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 20.The Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association; 1994. [Google Scholar]
- 21.Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer RL. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med. 2001;63:679–86. doi: 10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization Disability Assessment Schedule II. World Health Organization; 1999. [Google Scholar]
- 24.Sloan KL, Sales AE, Liu CF, et al. Construction and characteristics of the RxRisk-V: a VA-adapted pharmacy-based case-mix instrument. Med Care. 2003;41:761–74. doi: 10.1097/01.MLR.0000064641.84967.B7. [DOI] [PubMed] [Google Scholar]
- 25.Fishman PA, Goodman MJ, Hornbrook MC, Meenan RT, Bachman DJ, Rosetti MC O’Keeffe. Risk adjustment using automated ambulatory pharmacy data: the RxRisk model. Med Care. 2003;41:84–99. doi: 10.1097/00005650-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the “top 10” physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med. 2003;45:5–14. doi: 10.1097/00043764-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Ricci JA, Chee E. Lost productive time associated with excess weight in the U.S. workforce. J Occup Environ Med. 2005;47:1227–34. doi: 10.1097/01.jom.0000184871.20901.c3. [DOI] [PubMed] [Google Scholar]
- 28.Finkelstein E, Fiebelkorn C, Wang G. The costs of obesity among full-time employees. Am J Health Promot. 2005;20:45–51. doi: 10.4278/0890-1171-20.1.45. [DOI] [PubMed] [Google Scholar]
- 29.Cawley J, Rizzo JA, Haas K. Occupation-specific absenteeism costs associated with obesity and morbid obesity. J Occup Environ Med. 2007;49:1317–24. doi: 10.1097/JOM.0b013e31815b56a0. [DOI] [PubMed] [Google Scholar]
- 30.Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90:251–7. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heo M, Pietrobelli A, Fontaine KR, Sirey JA, Faith MS. Depressive mood and obesity in US adults: comparison and moderation by sex, age, and race. Int J Obes (Lond) 2006;30:513–9. doi: 10.1038/sj.ijo.0803122. [DOI] [PubMed] [Google Scholar]
- 32.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. Jama. 1999;282:1523–9. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 33.Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988;109:18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- 34.Peltonen M, Lindroos AK, Torgerson JS. Musculoskeletal pain in the obese: a comparison with a general population and long-term changes after conventional and surgical obesity treatment. Pain. 2003;104:549–57. doi: 10.1016/S0304-3959(03)00091-5. [DOI] [PubMed] [Google Scholar]