Abstract
Objective
To estimate whether racial/ethnic behavioral health service disparities are likely to be reduced through insurance expansion coverage expected through the Affordable Health Care Act.
Data Sources
Pooled data from the nationally representative NIMH Collaborative Psychiatric Epidemiological Studies (2001–2003).
Study Design
We employ a novel reweighting method to estimate service disparities in the presence and absence of insurance coverage.
Data Collection
Access to care was assessed by whether any behavioral health treatment was received in the past year. Need was determined by presence of prior year psychiatric disorder, psychiatric diagnoses, physical comorbidities, gender, and age.
Principal Findings
Improving patient education and availability of community clinics, combined with insurance coverage reduces service disparities across racial/ethnic groups.However, even with expanded insurance coverage, approximately 10 percent fewer African Americans with need for behavioral health services are likely to receive services compared to non-Latino whites while Latinos show no measurable disparity.
Conclusions
Expansion of insurance coverage might have different effects for racial/ethnic groups, requiring additional interventions to reduce disparities for all groups.
Keywords: Disparities, minorities, expanding insurance, behavioral health, mechanisms
Untreated mental illness is linked to job loss, academic failure, delinquency, premature mortality, and suicide attempts (Petry and Kiluk 2002; Galvan and Caetano 2003; Iguchi et al. 2005; Schmidt, Greenfield, and Mulia 2006). Inadequate access to behavioral health services profoundly affects the life trajectory, financial status, and overall welfare of communities of color. Health care reform may reverse this process as planned Medicaid expansions under federal guidelines are expected to heavily impact racial/ethnic minorities (Abrams et al. 2011). Understanding additional constraints due to individual characteristics (e.g., poverty, low education) and institutional resources (e.g., availability of community clinics) is critical if we expect health care reform to lead to better access to care in the estimated 1.15 million new users of behavioral health services (Garfield, Lave, and Donohue 2010; Garfield et al. 2011).
In the last 10 years, there has been mounting attention to disparities in access to and outcomes of psychiatric care (Chow, Jaffee, and Snowden 2003; McGuire et al. 2006; Dobalian and Rivers 2007), with continued evidence (Miranda and Cooper 2004; Alegría et al. 2008) that they pose significant concerns regarding equity for Latinos, Asians, and African Americans. Evidence suggests that these disparities may have been worsening for Latinos and blacks (Blanco et al. 2007; Cook, McGuire, and Miranda 2007). Expectations are high among policy makers that insurance expansions tied to health care reform will increase access to behavioral health care and decrease service disparities.
We utilize the Institute of Medicine (IOM) disparities framework (Institute of Medicine 2002) to estimate disparities in access to behavioral health care between each racial/ethnic minority group and non-Latino whites1 and assess potential mechanisms that could impede reducing disparities. We estimate the potential of health insurance coverage to reduce mental health care disparities (Hargraves and Hadley 2003; Lillie-Blanton and Hoffman 2005). We also assess four additional potential mechanisms underlying access: poverty; education as a proxy for health literacy; presence of a mental health clinic in the neighborhood; and stigma toward mental health care.
State and federal regulations governing insurance coverage, particularly for immigrants, play a direct role in access disparities (Ku and Waidmann 2003; Alegría et al. 2006). Eligibility restrictions have led to loss of public insurance coverage under Medicaid (Ellwood and Ku 1998; Bodenheimer 2005). In addition, employees choosing not to purchase employer health insurance account for a sizeable share of health care access disparities (Lillie-Blanton and Hoffman 2005; Kaiser Family Foundation 2008).
Poverty (measured by the U.S. Census Bureau Federal poverty guidelines 2002), more prevalent among minority groups (U.S. Census Bureau 2010), may serve as a disparities mechanism, particularly since the number of providers accepting new Medicaid patients has declined over the past 10 years (Cunningham and Hadley 2008). The level of poverty within an individual's zip code area (measured by 20 percent or more of the zip code population in poverty) appears to mediate the relationship between race/ethnicity and health care access (Chow, Jaffee, and Snowden 2003). Low education, as a crude proxy for health literacy (Baker 2006), may also impact service access (Balcazar, Castro, and Krull 1995). Low education may inhibit patients’ ability to register for public insurance programs (Gazmararian et al. 2005) or to navigate the health care system (Institute of Medicine 2002) since it limits opportunities to access information, request referrals, understand basic health terminology, and acquire skills to solve bureaucratic barriers to health care. Availability of providers in community health clinics has been linked to increased access to behavioral health services (Sturm, Ringel, and Andreyeva 2003; Wei et al. 2005; McCarthy et al. 2007). For example, augmenting the geographic accessibility to mental health providers has been found to increase the continuity of psychotherapy visits (Wei et al. 2005) as well as living proximal to the clinics (McCarthy et al. 2007). Stigma and attitudes are strongly related to use of services (Mojtabai, Olfson, and Mechanic 2002; Edlund et al. 2008). In this paper, we focus on the contribution of these different factors, among both the insured and the uninsured, as a way to determine what insurance expansions can accomplish given ethnic/racial group characteristics and institutional resources available. We examine whether health insurance coverage could reduce disparities in behavioral health care access, for which subgroups, and how the aforementioned four factors affect mental health care use.
Data and Methods
The CPES Combined Sample
We use the combined data from National Institutes of Mental Health (NIMH) Collaborative Psychiatric Epidemiology Surveys (CPES; Colpe et al. 2004), three large epidemiological studies of adults conducted between 2001 and 2003: the National Latino and Asian American Study (NLAAS; Alegría et al. 2004), the National Comorbidity Survey Replication (NCS-R; Kessler and Merikangas 2004), and the National Survey of American Life (NSAL; Neighbors et al. 2007). The sampling approach allowed for the creation of design-based analysis weights. Using these weights, the three datasets can be combined as though they are a single, nationally representative study (National Institutes of Mental Health Collaborative Psychiatric Epidemiology Surveys [CPES]. Information on the survey sampling design and weighting can be found on the CPES website (http://www.icpsr.umich.edu).
The CPES studies focused on collection of identical epidemiological information on mental and substance use disorders and service usage among the general population with special emphasis on minority groups (Colpe et al. 2004). The NCS-R (Kessler and Merikangas 2004) is a nationally representative sample of non-institutionalized adults ages 18 or older (response rate = 70.9 percent). The NSAL (Neighbors et al. 2007) is a nationally representative survey of household residents (ages 18 or older) in the non-institutionalized black population and included 3,570 African Americans and 1,621 Afro-Caribbeans (response rate = 70.9 percent). The NLAAS (Alegría et al. 2004) is a nationally representative survey of household residents (18 years of age and older) in the non-institutionalized Latino and Asian populations that includes 2,554 Latinos and 2,095 Asian Americans (response rate = 73.2 percent).
All interviews were administered using computer-assisted software. We used a pooled sample that included Latinos from the NLAAS, non-Latino whites from the NCS-R, and African Americans from the NSAL for a sample of 4,172 whites, 1,908 Latinos, and 3,366 African Americans for a total of 9,446 respondents. The Asian or Afro-Caribbean samples were too small to make reliable estimates and were omitted from analysis.
Measures
Access to Behavioral Health Treatment
Our outcome of interest was use of behavioral health services in the past year for problems related to emotions, nerves, substance use, energy, concentration, sleep, or ability to cope with stress. Use of services was defined as whether respondents received any mental health treatment, being at least one visit to a specialty mental health provider (e.g., psychiatrist, psychologist, social worker, or mental health counselor) or general medical provider (general practitioner, other medical doctor, nurse, occupational therapist, other) for mental health or substance use care in the past year.
Establishing Level of Need for Behavioral Health Care
Need for behavioral health services includes variables found to be closely correlated with need (see McGuire et al. 2006; Kessler et al. 2010). Need was determined by presence of any past year psychiatric disorder, number of psychiatric diagnoses, physical comorbidities, functional impairment, gender, and age. Presence of 12-month psychiatric disorders was evaluated via a modified version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMH-CIDI; Kessler and Ustun 2004), a standardized diagnostic interview assessing current and lifetime psychiatric disorders according to DSM-IV criteria. Findings show good concordance between DSM-IV diagnoses based on the WMH-CIDI and the Structured Clinical Interview for DSM-IV (SCID) (Haro et al. 2006). Functional impairment was measured by the WHO Psychiatric Disability Assessment Schedule (WHO-DAS; Rehm et al. 1999). We also measured the self-reported number of lifetime chronic medical conditions as well as the overall number of psychiatric diagnoses.
Other Measures
Ethnic/racial group affiliation was determined by respondents’ answers to questions identical to those in the 2000 Census. Insurance was operationalized by classifying respondents into one of five categories: not insured, privately insured, Medicare, Medicaid, and other insurance (e.g., Veterans Affairs). If a person reported multiple insurance plans and was enrolled in Medicare, he/she was assigned to the Medicare category. If the person was not in Medicare but had private insurance, he/she was considered privately insured. Other insurance refers to any other type of health care. We elected not to include a measure of whether the insurance covered behavioral health treatments since many respondents did not know the answer, especially those that had never sought behavioral health treatment.
Poverty status was determined using an income-to-needs ratio defined by the U.S. Census Bureau. When household income was less than family needs, as determined by family size and income, a family was considered to be in poverty (U.S. Census Bureau 2002). Low level of education as a proxy for health literacy was defined as having less than a high school education. Stigma toward care was assessed by asking the following: (1) “If you had a serious emotional problem, would you go for professional help?” (2) “How uncomfortable would you feel talking about personal problems with a professional?” and (3) “How embarrassed would you be if your friends knew you were getting professional help for an emotional problem?” Endorsement of any of these three questions was coded as positive for stigma as previously used (Gonzalez, Alegría, and Prihoda 2005). Availability of behavioral health provider was indicated by the presence of a community health center in the respondent's county of residence, with information merged from the 2002–2003 Area Resource File (U.S. Department of Health and Human Services 2010).
Statistical Analysis
Creating Counterfactual Populations
In accordance with the IOM definition, we estimate racial/ethnic differences in access to mental health care that are not due to differences in clinical need or preferences. Preferences are not considered in our modeling strategy, as the dataset has no measure of preferences. To explain our approach, suppose that we have two sets of covariates—variables that are justifiable in causing differences in behavioral health care access (e.g., clinical needs); and variables that are not justifiable in causing differences in access to care (e.g., income). Building upon work by Duan et al. (2008), we will call the former “allowable” covariates denoted by XA, and the latter “non-allowable” covariates denoted by XN. Our outcome of interest is access to care denoted by Y. The goal is to account for differences in access to care that are attributable to the allowable covariates and justifiable in causing differences in use of services, and to investigate the impact of particular nonallowable factors (e.g., uninsurance, lack of community health center, poverty, stigma, and low level of education as proxy for low literacy) on the differences that remain (i.e., disparities).
We aim to estimate the potential outcome of access to care that would manifest if the minority groups had the same characteristics as the non-Latino whites in the allowable covariates. Consider the joint distribution density function f1(Y, XN, XA) for the non-Latino white group and f2(Y, XN, XA) for the minority group of interest, with the subscript for the joint density denoting the group membership (i.e., 1, 2). The joint density for the minority group of interest can be factored into f2 (Y | XN, XA) f2(XA | XN) f2(XN). Here the first factor describes how the allowable and nonallowable covariates affect use of service. The second factor specifies the relationship between the allowable covariates and the nonallowable covariates (e.g., level of clinical need given a particular income level), and the third factor tells us the distribution of the non-allowable covariates (e.g., income distribution). To estimate disparities in access to care, we need to adjust for the level of allowable covariates, but not the level of non-allowable covariates for the minority group of interest. Our approach is to leave the first factor and the third factor untouched but adjust the second factor from that of the minority group to that of the reference group (non-Latino white). The full rationale of this methodology is described in Duan et al. (2008). Intuitively, we leave the first factor untouched because if the impact of the covariates (either allowable or non-allowable) on the use of service is different between the minority group and for the non-Latino whites, then the issue of disparity is far more complex than merely the differences in the distributions of non-allowable covariates (e.g., income level). We leave the third factor unadjusted because it is precisely the difference in use of service due to unallowable variable (e.g., income) that we want to assess.
To adjust for the second factor, we adopt the conceptually straightforward re-weighting method, a common strategy in analyzing survey data (e.g., Kish 1965) or in statistical computing, also known as importance sampling (e.g., Hammersley and Handscomb 1964). For example, suppose among people with annual incomes between $20,000 and $30,000, the minority group has half as many people with clinical need as compared to the non-Latino whites. Then to adjust for this difference, we simply count each minority with clinical need whose income is within the given range twice. The adjustment weight is R = 2. We emphasize here that because we adjust for the allowable covariates after stratifying on the nonallowable covariates, the distribution of the nonallowable attributes is not altered in the minority group, as intended.
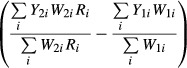
The adjustment weight R can be estimated using the propensity score method described in Elliott and Davis (2005) and Rosenbaum and Rubin (1983). We observe that  can be expressed as the ratio of two propensity scores by Bayes’ theorem. First, we estimate the propensity of being in the non-Latino white group given both the allowable and nonallowable covariates, and the propensity of being in the non-Latino white group given the nonallowable covariate only. Then we estimate the adjustment weight by taking the ratio of the two propensity scores. We fit separate propensity score models for non-Latino whites and Latinos, and for non-Latino whites and African Americans. In addition, the propensity score models are stratified on nativity (U.S. born or immigrant) because the distribution of the covariates is markedly different between the nativity groups. Notice that propensity score estimation does not involve the outcome variable, access to care.
can be expressed as the ratio of two propensity scores by Bayes’ theorem. First, we estimate the propensity of being in the non-Latino white group given both the allowable and nonallowable covariates, and the propensity of being in the non-Latino white group given the nonallowable covariate only. Then we estimate the adjustment weight by taking the ratio of the two propensity scores. We fit separate propensity score models for non-Latino whites and Latinos, and for non-Latino whites and African Americans. In addition, the propensity score models are stratified on nativity (U.S. born or immigrant) because the distribution of the covariates is markedly different between the nativity groups. Notice that propensity score estimation does not involve the outcome variable, access to care.
Estimating Disparity
We are interested in estimating the disparity in access to behavioral health services in the past year, measured as a dichotomous variable. Our “allowable” covariates that describe behavioral health need include any psychiatric disorders in the past year, number of past year psychiatric disorders, physical comorbidities, functional impairment, gender, and age. Our “non-allowable” covariates include stigma, poverty, low level of education, and the presence of a community health center in the respondent's county. These are considered separately and in combination with insurance coverage in our analyses.
To estimate disparities, we first weigh the observed use of services rates with new weights constructed from multiplying the survey weights by the estimated density ratios R previously described, and then take the difference of the reweighted use of services rates between the minority groups and the non-Latino whites. Since we are not adjusting the distribution of the allowable variables in the non-Latino whites, we only apply the original survey weights to the non-Latino white group. Let W1i and W2i denote the survey weights for individuals i of the non-Latino white and the minority group of interest, respectively. Disparity estimates are calculated as
 |
To estimate the variability associated with use of services and disparity estimates, we apply the bootstrap method described in Rust and Rao (1996). We construct the approximate 95 percent bootstrap confidence intervals by adding and subtracting twice the standard deviation of the weighted bootstrap estimates to and from the weighted point estimates.
Our method does not require modeling the use of services. Use of behavioral health services is a complex behavior and poses challenges in developing predictive models. Instead of relying on parametric models to estimate use rates under different distribution of the nonallowable variables, we take a semi-parametric approach and reweight the existing population. The complex relationship between different individual- and system-level characteristics is inherent in the existing populations. Parametric models are only used in constructing the propensity scores for estimating the ratios R, which involves regressing race/ethnicity group membership on the allowable and non-allowable covariates, and does not require knowledge of the use of services.
Assessing Attributable Sources of Disparity
We are particularly interested in how the presence or absence of insurance coverage, in combination with either individual characteristics of the population or institutional resources, relates to disparities. To investigate the effects of these potential mechanisms, we stratify the sample by insurance status and then by the identified other four factors in combination with insurance status, and compare the estimated racial/ethnic disparities within each of these subpopulations. These comparisons allow us to estimate the level of disparities contingent on certain individual and institutional conditions (e.g., poverty). All sample proportions and means reported are weighted by survey sampling weights to reflect national estimates. Contrasts are made between the minority race/ethnic groups and non-Latino whites using survey design-adjusted chi-square and Wald tests (Rao and Scott 1984; Rao and Thomas 1989; StataCorp 2004).
Results
In Table 1, we observe an age difference across ethnic/racial groups, a likely reason for the observed differences in chronic conditions and functional status. African Americans have lower prevalence of depressive and anxiety disorders but are more likely to reside in areas where there are community clinics, while Latinos are less likely to be English proficient. In addition, Latinos and African Americans have less education, lower household income, and higher poverty rates than non-Latino whites, but they also have different types of insurance. Latinos have the highest uninsurance rate, although they report lower numbers of chronic conditions and less impairment than non-Latino whites and have lower prevalence of past year anxiety disorders.
Table 1.
Sociodemographic, Need Characteristics, Insurance Status, and Mechanisms by Race/Ethnicity (Weighted Estimates)
| White (n = 4,172)% | Latinos (n = 1,908)% | African Americans (n = 3,366)% | |
|---|---|---|---|
| Sociodemographic (nonallowables) | |||
| Marital status | *** | ||
| Not married/divorced/widowed/separated | 44.9 | 48.5 | 66.8 |
| Married | 55.1 | 51.5 | 33.2 |
| Region | *** | *** | |
| Northeast | 21.1 | 18.7 | 16.1 |
| Midwest | 28.6 | 8.7 | 17.6 |
| South | 30.6 | 31.0 | 56.6 |
| West | 19.8 | 41.6 | 9.7 |
| Need for service | |||
| Age | 46.9 (0.57) | 37.9 (0.68)*** | 42.0 (0.53)*** |
| Female | 52.5 | 48.6* | 56.1* |
| Any past year depressive disorder | 8.8 | 9.2 | 6.8** |
| Any past year anxiety disorder | 13.7 | 9.9*** | 10.8** |
| Any past year substance disorder | 3.7 | 2.7 | 2.9 |
| Number of past year diagnosis | ** | ||
| 0 | 80.0 | 83.2 | 84.0 |
| 1 | 11.7 | 9.7 | 9.3 |
| 2 or 3 | 6.4 | 5.7 | 5.0 |
| 4+ | 1.9 | 1.4 | 1.8 |
| Number of chronic conditions | *** | ||
| 0 | 44.7 | 64.8 | 44.4 |
| 1 | 26.7 | 20.8 | 27.7 |
| 2 or 3 | 28.5 | 14.5 | 27.9 |
| 4+ | 1.9 | 1.4 | 1.8 |
| WHO-DAS dysfunction | |||
| Cognition | 10.1 | 6.0*** | 13.6*** |
| Mobility | 18.4 | 10.0*** | 20.3 |
| Selfcare | 4.6 | 3.0** | 5.1 |
| Social | 5.9 | 3.5** | 8.7** |
| Out of role | 35.2 | 21.2*** | 38.1 |
| WHO-DAS dysfunction | |||
| Cognition | 10.1 | 6.0*** | 13.6*** |
| Mobility | 18.4 | 10.0*** | 20.3 |
| Selfcare | 4.6 | 3.0** | 5.1 |
| Social | 5.9 | 3.5** | 8.7** |
| Out of role | 35.2 | 21.2*** | 38.1 |
| Presence of mental health clinic | 40.9 | 56.1 | 58.1* |
| Poverty | 8.9 | 26.3*** | 23.7*** |
| Stigma | 48.3 | 45.5 | |
| English language proficiency | *** | *** | |
| Poor or fair | 0.0 | 49.1 | 0.3 |
| Good or excellent | 100.0 | 50.9 | 99.7 |
Notes. WHO-DAS, WHO Psychiatric Disability Assessment Schedule.
*<0.05, **<0.01, ***<0.001.
Estimates of Service Disparity
The weighted rates of behavioral health-related use of services in the past year for non-Latino whites and counterfactual minority groups with behavioral health need are described in Table 2. In declaring the statistical significance of results, we take into account the approximate nature of bootstrap interval estimates and avoid the practice of taking cut-off points too literally (e.g., interval for differences of rates not covering 0 implies significance). The estimated maximum Monte Carlo error of the bootstrap intervals here is about 3 percent, implying that the end points of the intervals will fluctuate about 3 percent at most on the absolute scale due to simulation error.
Table 2.
Observed Rates of Services Use in Non-Latino Whites and Estimated Rates Use for Latinos and African Americans If They Had the Same Need for Behavioral Services as Non-Latino Whites Stratified by Insurance Status (bootstrap intervals presented in square brackets)†
| Non-Latino Whites | Latinos | African Americans | Difference: Latinos - Non-Latino Whites | Difference: African Americans - Non-Latino Whites | |
|---|---|---|---|---|---|
| Services use rates | N = 2,310; n = 918 0.38 [0.35, 0.41] | N = 1,153; n = 213 0.39 [0.17, 0.61] | N = 2,463; n = 408 0.28 [0.22, 0.34] | 0.02 [−0.21, 0.24]‡ | −0.10 [−0.17, −0.04] |
| Minorities adjusted to have same insurance as non-Latino whites | N = 2,310; n = 918 0.38 [0.35, 0.41] | N = 1,153; n = 213 0.41 [0.25, 0.56] | N = 2,463; n = 408 0.27 [0.20, 0.34] | 0.03 [−0.13, 0.18] | −0.11 [−0.18, −0.04] |
| Among uninsured | N = 237; n = 124 0.27 [0.20, 0.33] | N = 369; n = 60 0.20 [0.00, 0.47] | N = 443; n = 102 0.18 [0.10, 0.27] | −0.06 [−0.34, 0.22] | −0.08 [−0.19, 0.02] |
| Among insured | N = 2,074; n = 797 0.39 [0.36, 0.42] | N = 789; n = 155 0.43 [0.26, 0.59] | N = 2,020; n = 305 0.28 [0.21, 0.35] | 0.04 [−0.13, 0.20] | −0.11 [−0.19, −0.04] |
| Private insured | N = 1,565; n = 604 0.37 [0.34, 0.40] | N = 488; n = 75 0.39 [0.17, 0.60] | N = 1,337; n = 167 0.28 [0.17, 0.38] | 0.02 [−0.20, 0.23] | −0.09 [−0.20, 0.02] |
| Medicare | N = 395; n = 91 0.43 [0.33, 0.53] | N = 102; n = 28 0.47 [0.18, 0.77] | N = 372;n = 64 0.30 [0.14, 0.45] | 0.04 [−0.27, 0.36] | −0.13 [−0.32, 0.06] |
| Medicaid | N = 109; n = 69 0.55 [0.40, 0.69] | N = 194; n = 53 0.53 [0.25, 0.81] | N = 243; n = 63 0.26 [0.12, 0.40] | −0.02 [−0.33, 0.29] | −0.29 [−0.48, −0.09] |
| Other | N = 48; n = 33 0.43 [0.27, 0.60] | N = 24; n = 4 1.00 [0.50, 1.00] | N = 80; n = 14 0.13 [0.00, 0.35] | 0.57 [0.03, 1.00] | −0.30 [−0.58, −0.02] |
Notes. N = effective sample size for that cell.
n = effective sample size for those with need for behavioral services in that cell.
The bootstrap intervals are estimated as 2*SD of bootstrap estimates.
Note that due to rounding the point estimate of disparity is 0.02 instead of 0.01 from subtracting 0.38 from 0.39.
Table 2 is adjusted by the need for behavioral services. Our definition of need includes the following variables that the literature has found to be closely correlated with need (see McGuire et al. 2006; Kessler et al. 2010): gender, age, any past year psychiatric disorders, number of last year psychiatric disorders, number of chronic conditions, and measures of functional impairment.
The estimated use of services rates for those with any past year behavioral health need according to our reweighting method are shown in Table 2 row 1. When comparing Latinos to non-Latino whites, we find no evidence of service disparities in access to behavioral health care (disparity estimate = 0.02, bootstrap interval [−0.21, 0.24]; Table 2 row 1, column 4) while we find statistically significant disparities in access for African Americans (−0.10 [−0.17, −0.04]; Table 2 row 1 column 5). Our method estimates that about 10 percent fewer African Americans with need for care will receive any related services as contrasted to non-Latino whites. This pattern persists even when the distribution of health insurance status is adjusted (Table 2, row 2).
Exploring Potential Mechanisms to Reduce Disparities
Insurance Coverage
Aggregating insured and uninsured respondents shows no significant disparities in access to care between Latinos and non-Latino whites. This pattern remains even when we look at the insured and uninsured respondents separately. We find disparities between African Americans and non-Latino whites among the insured (−0.11 [−0.19, −0.04]); Table 2, row 4 column 5) and uninsured (−0.08 [−0.19, 0.02]); Table 2 row 3 column 5). Note that we do not take the difference between [−0.19, −0.04] and [−0.19, 0.02] literally, because statistically they provide similar evidence. This suggests that the disparity in African Americans is contributed by both the insured and the uninsured groups. When we stratify the groups by insurance type, we see evidence of greatest disparity in African Americans with Medicaid compared to their non-Latino white counterparts with the same insurance (−0.29 [−0.48, −0.09]); Table 2 row 7 column 5). We also find evidence of a large disparity in African Americans with other types of insurance (−0.30 [−0.58, −0.02]), although the sample sizes are too small to produce reliable estimates.
Presence of Neighborhood Clinic
Our estimates show significant disparities in the rates of use of service for insured persons with behavioral health need and without access to neighborhood clinics between Latinos and non-Latino whites (−0.22 [−0.37, −0.06]); Table 3 block A row 3 column 4), and between African Americans and non-Latino whites (−0.19 [−0.31, −0.07]); Table 3 block A row 3 column 5). However, there were no statistically significant differences between the minority racial/ethnic groups and non-Latino whites among insured individuals with access to neighborhood clinics.
Table 3.
Possible Mechanisms of Disparities in Services Use in Those with Need for Behavioral Services in the Past Year (bootstrap intervals presented in square brackets)†
| Non-Latino Whites | Latinos | African Americans | Latinos - Non-Latino Whites | Non-Latino Whites - African Americans | |
|---|---|---|---|---|---|
| A. Community health clinic | |||||
| Insurance No Clinic No | N = 142; n = 66 0.28 [0.21, 0.35] | N = 151; n = 26 0.20 [0.00, 0.76] | N = 199; n = 43 0.37 [0.15, 0.59] | −0.08 [−0.65, 0.49] | 0.09 [−0.14, 0.32] |
| Insurance No Clinic Yes | N = 98; n = 71 0.24 [0.14, 0.34] | N = 218; n = 34 0.37 [0.06, 0.68] | N = 245; n = 60 0.13 [0.04, 0.22] | 0.13 [−0.19, 0.46] | −0.11 [−0.25, 0.03] |
| Insurance Yes Clinic No | N = 1,172; n = 415 0.41 [0.37, 0.45] | N = 332; n = 57 0.19 [0.05, 0.34] | N = 878; n = 121 0.22 [0.11, 0.33] | −0.22 [−0.37, −0.06] | −0.19 [−0.31, −0.07] |
| Insurance Yes Clinic Yes | N = 906; n = 406 0.38 [0.33, 0.43] | N = 462; n = 99 0.41 [0.27, 0.56] | N = 1,144; n = 185 0.34 [0.25, 0.43] | 0.03 [−0.12, 0.18] | −0.04 [−0.14, 0.07] |
| B. Literacy | |||||
| Insurance No HS Edu No | N = 43; n = 24 0.21 [0.05, 0.37] | N = 204; n = 32 0.11 [0.00, 0.24] | N = 147; n = 40 0.12 [0.00, 0.25] | −0.11 [−0.32, 0.10] | −0.10 [−0.31, 0.11] |
| Insurance No HS Edu Yes | N = 196; n = 101 0.28 [0.21, 0.35] | N = 168; n = 28 0.13 [0.00, 0.32] | N = 296; n = 63 0.22 [0.09, 0.35] | −0.15 [−0.34, 0.05] | −0.06 [−0.21, 0.09] |
| Insurance Yes HS Edu No | N = 240; n = 102 0.43 [0.30, 0.57] | N = 264; n = 66 0.48 [0.22, 0.75] | N = 495; n = 100 0.21 [0.12, 0.30] | 0.05 [−0.25, 0.35] | −0.22 [−0.39, −0.06] |
| Insurance Yes HS Edu Yes | N = 1,835; n = 695 0.39 [0.36, 0.42] | N = 527; n = 89 0.39 [0.13, 0.65] | N = 1,531; n = 205 0.31 [0.23, 0.40] | −0.00 [−0.26, 0.26] | −0.08 [−0.17, 0.01] |
| C. Poverty | |||||
| Insurance No Poverty No | N = 210; n = 95 0.27 [0.20, 0.34] | N = 240; n = 42 0.11 [0.00, 0.27] | N = 288; n = 63 0.21 [0.10, 0.32] | −0.16 [−0.34, 0.01] | −0.06 [−0.19, 0.08] |
| Insurance No Poverty Yes | N = 29; n = 31 0.25 [0.09, 0.41] | N = 129; n = 18 0.25 [0.01, 0.49] | N = 156; n = 43 0.04 [0.00, 0.10] | 0.00 [−0.29, 0.29] | −0.22 [−0.38, −0.05] |
| Insurance Yes Poverty No | N = 1,899; n = 703 0.39 [0.36, 0.42] | N = 637; n = 110 0.35 [0.16, 0.54] | N = 1,551; n = 194 0.26 [0.18, 0.34] | −0.04 [−0.23, 0.16] | −0.13 [−0.22, −0.04] |
| Insurance Yes Poverty Yes | N = 175; n = 93 0.47 [0.36, 0.58] | N = 153; n = 45 0.55 [0.32, 0.78] | N = 471; n = 112 0.33 [0.20, 0.46] | 0.08 [−0.17, 0.34] | −0.14 [−0.31, 0.03] |
| D. Stigma | |||||
| Insurance No Stigma No | N = 129; n = 70 0.36 [0.26, 0.46] | N = 201; n = 31 0.28 [0.06, 0.51] | −0.08 [−0.32, 0.17] | ||
| Insurance No Stigma Yes | N = 111; n = 57 0.18 [0.10, 0.25] | N = 169; n = 30 0.21 [0.00, 0.48] | 0.03 [−0.25, 0.31] | ||
| Insurance Yes Stigma No | N = 1,103; n = 404 0.52 [0.48, 0.56] | N = 455; n = 86 0.50 [0.30, 0.70] | −0.02 [−0.22, 0.18] | ||
| Insurance Yes Stigma Yes | N = 972; n = 393 0.28 [0.23, 0.33] | N = 335; n = 74 0.25 [0.13, 0.37] | −0.03 [−0.16, 0.11] | ||
Notes. Table 3 is adjusted by the need for behavioral services. Our definition of need includes the following variables that the literature has found to be closely correlated with need (see McGuire et al. 2006; Kessler et al. 2010): gender, age, any past year psychiatric disorders, number of last year psychiatric disorders, number of chronic conditions, and measures of functional impairment.
N = effective sample size for that cell.
n = effective sample size for those with any past year disorders in that cell.
The bootstrap intervals are estimated as 2*SD of bootstrap estimates.
Low Education
Our estimates show that among African Americans who are insured, the magnitude of disparity was greater for the subgroup without a high school education (−0.22 [−0.39, −0.06]); Table 3 block B row 3 column 5) than the group with at least a high school education (−0.08 [−0.17, 0.01]); Table 3 block B row 4 column 5).
Poverty
There is evidence suggesting significant service disparity for non-poor Latinos without insurance (−0.16 [−0.34, 0.01]); Table 3 block C row 1 column 4), but we find no disparity in non-poor Latinos with insurance (−0.04 [−0.23, 0.16]); Table 3 block C row 3 column 4) compared to their non-Latino white counterparts with similar levels of behavioral health need. Among non-poor African Americans without insurance the estimated use of services is not significantly different from non-Latino whites with similar behavioral health needs and no insurance (estimated disparity −0.06 [−0.19, 0.08]); Table 3 block C row 1 column 5). However, without insurance, poverty seems to play an important role. The estimated disparity for African Americans without insurance and in poverty is significant (−0.22 [−0.38, −0.05]); Table 3 block C row 2 column 5).
Stigma
We were only able to explore how stigma was associated with disparities in seeking professional help for non-Latino whites and Latinos since stigma questions were not asked in the NSAL. Our estimates suggest that stigma does play a strong role in determining differential access to behavioral health services, although it has a similar effect for both Latinos and non-Latino whites.
Discussion
Universal health coverage has been viewed as an important factor in reducing disparities in access to behavioral health services. However, ethnic/racial groups might benefit differently from this access-expanding policy. Expansion of insurance coverage could increase access for Latinos and non-Latino whites, but it may have modest effects for African Americans, implying that policy making might need to look beyond health coverage alone to effectively increase access. We found considerable service disparities for African Americans, even among those with insurance coverage, which confirms the findings of the 2009 National Healthcare Disparities Report from Agency for Health Research and Quality (AHRQ) (2009). Furthermore, service disparities were more pronounced among African Americans with Medicaid as compared with non-Latino whites with the same insurance coverage. We conclude that caution should be exercised in generalizing the effect that expansion of insurance coverage could have on increased use of services for racial/ethnic vsubgroups, since insurance coverage without adequate providers to offer behavioral health services is unlikely to decrease service disparities. Highlighting this issue is the finding that only one-third of primary care physicians (PCPs) report that they were able to successfully obtain outpatient mental health services for their primary care patients (Cunningham and Hadley 2008). This lack of providers might be especially severe in areas where African Americans reside (Waidmann and Rajan 2000). Given the importance of provider supply on treatment, referral, and engagement (Lindrooth, LoSasso, and Lurie 2006), having a sufficient workforce of service providers must be addressed in order to truly implement the Affordable Health Care Act. In addition, attention to the effect of socio-cultural factors and patient preferences for service delivery is particularly important for ethnic/racial minority populations (Mulvaney-Day et al. 2011) and must be considered if we are to close the disparities gap.
Contrary to the AHRQ's Report (2009), our results provide no evidence of service disparities for Latinos when examined in the aggregate. This inconsistency may be due to how we adjust for differences in need for care. Since there were a significant number of immigrants in the Latino sample, and immigrant Latinos tend to have lower levels of behavioral health needs (Alegría et al. 2008), results may differ from other studies that only include English-proficient minority populations. In some subgroup analyses, we found estimates of behavioral health services access that are suggestive of potential disparities between Latinos and non-Latino whites but not statistically significant. Although not statistically significant, the notable disparity estimates are still of practical interest and warrant further investigation.
These results also suggest potential mechanisms through which ethnic/racial disparities in access could increase, given the limited focus on disparities reduction in the Affordable Care Act (Weinick and Hasnain-Wynia 2011). Assuming that use of services is widely similar to the patterns observed here, our estimation of disparities suggests that with full insurance coverage, African Americans would see access to services improved, but they may nonetheless encounter service disparities in comparison to non-Latino whites with insurance coverage. In other words, universal insurance coverage could increase access across populations, but it would have only a modest effect in decreasing service disparities. One potential explanation may be that the emphasis in behavioral health care on psychopharmacological treatments is not aligned with treatment preferences of African Americans (Cooper-Patrick et al. 1997). Another potential reason is that the South, with a greater concentration of African Americans, might have fewer options for care in public insurance programs than the West, where many Latinos reside (Waidmann and Rajan 2000; Chow, Jaffee, and Snowden 2003). Federal stimulus funds devoted to community health centers may counteract these factors and facilitate access to behavioral health care for minorities (Felland et al. 2010).
Neighborhood clinics, combined with universal coverage, appear to be able to reduce access disparities. Community clinics may reach out to minorities who may have limited transportation or offer culturally sensitive care to marginalized populations. Both Latinos and African Americans utilize community health centers at rates much higher than that of non-Latino whites (Smedley, Stith, and Nelson 2003).
However, access problems would not be completely resolved even if all our findings are substantiated and all remedial solutions are implemented. Even in the presence of universal insurance coverage and the resolution of barriers like stigma, 50 percent or more of people with significant behavioral health needs will not access any behavioral health care, independent of race/ethnicity. The treatment system may be failing racial/ethnic minorities as currently configured.
Also relevant is the absence of a significant difference in access to behavioral health care for Latinos or African Americans (as compared to non-Latino whites) who did not complete high school and had no insurance. A parallel pattern is observed for poor Latinos who are not insured. For disadvantaged individuals, regardless of racial/ethnic group, there might be few service options beyond public insurance. This suggests the importance of monitoring states that raise eligibility thresholds for Medicaid in the presence of poverty, with no alternative low-cost options, making everyone, independent of race/ethnicity, vulnerable for unmet needs.
There are limitations to the present study. The cross-sectional nature of the study design does not permit identification of causal effects, so that the findings are suggestive of potential mechanisms to be tested in future studies. Both diagnostic and use of service data are based on self-report that may be subject to incomplete information, particularly if respondents who have accessed services do not know they are being treated for behavioral health problems, as could be the case in primary care settings when providers might not specify they are prescribing antidepressants. Another limitation is the exclusion of other racial/ethnic groups (e.g., Asians) and geographical areas given the small sample sizes. The precision of disparity estimates was limited in that confidence bounds in Table 2 suggest that lack of significant findings do not rule out important disparities. Our disparity estimates are dependent on the ratios constructed from the estimated propensity scores that enable us to adjust minority mental health need characteristics so they are similar to those of non-Latino whites. Therefore, the disparity estimates may be sensitive to the assumed propensity score models. However, we emphasize that the propensity score model does not involve the use of services as an outcome variable, but only the race/ethnic group membership, behavioral health needs, and sociodemographic covariates. Thus, our reweighting method may actually provide more robust disparity estimates than other methods that require parametric assumptions of the relationship between use of services and other covariates.
Our findings stress that universal coverage alone may not be sufficient for eliminating disparities, especially when targeted approaches may be needed for specific racial/ethnic groups. Certain interventions, including increasing the community health clinic availability, augmenting patient education, and addressing stigma, should be tested. Furthermore, health system interventions may be needed to better align services to needs, including substantially improving geographical shortages of behavioral health professionals in certain African American communities (Merwin 2003), particularly for those who prefer counseling and psychotherapeutic interventions or voluntary support networks (Snowden 2001), not necessarily available in community health clinics. Similarly, we might need community interventions to help minority patients with behavioral disorders advocate for services not covered by typical insurance plans (Garfield, Lave, and Donohue 2010). Although insurance provides coverage for services, it is not sufficient to eliminate disparities. The system must attend to individual, family, and socio-cultural factors that weigh on accessing care. Additional interventions beyond extending insurance coverage will be needed to eliminate racial and ethnic disparities in access to behavioral health services.
Acknowledgments
This project was supported by funding from the National Institute of Mental Health grant P50 MHO73469, Advanced Center for Latino and Mental Health Systems Research; the National Center on Minority Health and Health Disparities grant P60 MD002261, UPR-CHA Research Center of Excellence: Making a Difference for Latino Health; and the Robert Wood Johnson Foundation (RWJF) grant 5-8678, Improving the Quality of Depression Treatment for Ethnic/Racial Minorities.
Disclosures: None.
Note
The Institute of Medicine defines a racial/ethnic health care disparity as all racial/ethnic differences except those due to clinically appropriate need and patient preferences. Estimating service disparities according to this framework requires the adjustment of variables related to need and preferences while allowing differences due to all other factors into the disparities calculation (McGuire et al. 2006).
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Abrams M, Nuzum R, Mika S, Lawlor G. “Realizing Health Reform's Potential: How the Affordable Care Act Will Strengthen Primary Care and Benefit Patients, Providers, and Payers”. Commonwealth Fund. 2011;1466((1)):1–7. [PubMed] [Google Scholar]
- Agency for Health Research and Quality (AHRQ) National Healthcare Disparities Report 2009. Rockville, MD: 2009. [Google Scholar]
- Alegría M, Takeuchi D, Canino G, Duan N, Shrout P, Meng X-L, Vega W, Zane N, Vila D, Woo M, Vera M, Guarnaccia P, Aguilar-Gaxiola S, Sue S, Escobar J, Lin KM, Gong F. “Considering Context, Place and Culture: The National Latino and Asian American Study”. International Journal of Methods in Psychiatric Research. 2004;13((4)):208–20. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Cao Z, McGuire TG, Ojeda VD, Sribney B, Woo M, Takeuchi D. “Health Insurance Coverage for Vulnerable Populations: Contrasting Asian Americans and Latinos in the United States”. National Institutes of Health Public Access. 2006;43((3)):231–54. doi: 10.5034/inquiryjrnl_43.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Chatterji P, Wells K, Cao Z, Chen C, Takeuchi D, Jackson J, Meng XL. “Disparity in Depression Treatment among Racial and Ethnic Minority Populations in the United States”. Psychiatric Services. 2008;59((11)):1264. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker C. Foundations of Bilingual Education and Bilingualism. 4th edition. Tonawanda, NY: Multilingual Matters Ltd; 2006. [Google Scholar]
- Balcazar H, Castro F, Krull JL. “Cancer Risk Reduction in Mexican American Women: The Role of Acculturation, Education, and Health Risk Factors”. Health Education Quarterly. 1995;22((1)):61–84. doi: 10.1177/109019819502200107. [DOI] [PubMed] [Google Scholar]
- Blanco C, Patel SR, Liu L, Jiang H, Lewis-Fernández R, Schmidt AB, Liebowitz MR, Olfson M. “National Trends in Ethnic Disparities in Mental Health Care”. Medical Care. 2007;45((11)):1012–9. doi: 10.1097/MLR.0b013e3180ca95d3. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T. “High and Rising Health Care Costs. Part 1: Seeking an Explanation”. Annals of Internal Medicine. 2005;142((10)):847–54. doi: 10.7326/0003-4819-142-10-200505170-00010. [DOI] [PubMed] [Google Scholar]
- Chow JC, Jaffee K, Snowden L. “Racial/Ethnic Disparities in the Use of Mental Health Services in Poverty Areas”. American Journal of Public Health. 2003;93((5)):792–7. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collaborative Psychiatric Epidemiology Surveys (CPES). n.d. “Welcome to CPES” [accessed on November 9, 2010]. Available at http://www.icpsr.umich.edu/icpsrweb/CPES/
- Colpe L, Merikangas KR, Cuthbert B, Bourdon K. Guest Editorial. International Journal of Methods in Psychiatric Research. 2004;13((4)):193–4. [Google Scholar]
- Cook B, McGuire T, Miranda J. “Measuring Trends in Mental Health Care Disparities, 2000–2004”. Psychiatric Services. 2007;58((12)):1533–9. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- Cooper-Patrick L, Powe N, Jenckes M, Gonzales J, Levine D, Ford D. “Identification of Patient Attitudes and Preferences Regarding Treatment of Depression”. Journal of General Internal Medicine. 1997;12((7)):431–8. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham PJ, Hadley J. “Effects of Changes in Incomes and Practice Circumstances on Physicians’ Decisions to Treat Charity and Medicaid Patients”. Millbank Quarterly. 2008;86((1)):91–123. doi: 10.1111/j.1468-0009.2007.00514.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobalian A, Rivers P. “Racial and Ethnic Disparities in the Use of Mental Health Services”. Journal of Behavioral Health Services and Research. 2007;35((2)):128–41. doi: 10.1007/s11414-007-9097-8. [DOI] [PubMed] [Google Scholar]
- Duan N, Meng X-L, Lin JY, Chen C-n, Alegría M. “Disparities in Defining Disparities: Statistical Conceptual Frameworks”. Statistics in Medicine. 2008;27:3941–56. doi: 10.1002/sim.3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Fortney JC, Reaves CM, Pyne JM, Mittal D. “Beliefs about Depression and Depression Treatment among Depressed Veterans”. Medical Care. 2008;46((6)):581–9. doi: 10.1097/MLR.0b013e3181648e46. [DOI] [PubMed] [Google Scholar]
- Elliott M, Davis W. “Obtaining Cancer Risk Factor Prevalence Estimates in Small Areas: Combining Data from Two Surveys”. Journal of the Royal Statistical Society: Series C (Applied Statistics) 2005;54((3)):595–609. [Google Scholar]
- Ellwood MR, Ku L. “Welfare and Immigration Reforms: Unintended Side Effects for Medicaid”. Health Affairs. 1998;17((3)):137–51. doi: 10.1377/hlthaff.17.3.137. [DOI] [PubMed] [Google Scholar]
- Felland LE, Cunningham PJ, Cohen GR, November EA, Quinn BC. “The Economic Recession: Early Impacts on Health Care Safety Net Providers”. Research Brief. 2010;((15)):1–8. Jan. [PubMed] [Google Scholar]
- Galvan FH, Caetano R. “Alcohol Use and Related Problems among Ethnic Minorities in the United Status”. Alcohol Research and Health. 2003;27((1)):87–94. [PMC free article] [PubMed] [Google Scholar]
- Garfield R, Lave J, Donohue JM. “Health Reform and the Scope of Benefits for Mental Health and Substance Use Disorder Services”. Psychiatric Services. 2010;61((11)):1081–6. doi: 10.1176/ps.2010.61.11.1081. [DOI] [PubMed] [Google Scholar]
- Garfield R, Zuvekas S, Lave J, Donohue J. “The Impact of National Health Reform on Adults with Mental Disorders”. American Journal of Psychiatry. 2011;168((5)):486–94. doi: 10.1176/appi.ajp.2010.10060792. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Curran JW, Parker RM, Bernhardt JM, DeBuono BA. “Public Health Literacy in America: An Ethical Imperative”. American Journal of Preventive Medicine. 2005;28((3)):317–22. doi: 10.1016/j.amepre.2004.11.004. [DOI] [PubMed] [Google Scholar]
- Gonzalez J, Alegría M, Prihoda T. “How do Attitudes toward Mental Health Treatment Vary by Age, Gender and Ethnicity/Race in Young Adults?”. Journal of Community Psychology. 2005;33((5)):611–29. [Google Scholar]
- Hammersley JM, Handscomb DM. Monte Carlo Methods. London: Methuen; 1964. [Google Scholar]
- Hargraves JL, Hadley J. “The Contribution of Insurance Coverage and Community Resources to Reducing Racial/Ethnic Disparities in Access to Care”. Health Services Research. 2003;38((3)):809–29. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haro J, Arbabzadeh-Bouchez S, Brugha T, Girolamo G, Guyer M, Jin R. “Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with Standardized Clinical Assessments in the WHO World Mental Health Surveys”. International Journal of Methods in Psychiatric Research. 2006;15((4)):167–80. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iguchi MY, Fain T, Ramchand RN, Bell J. “How Criminal System Racial Disparities may Translate into Health Disparities”. Journal of Health Care for the Poor and Underserved. 2005;16((4)):48–56. doi: 10.1353/hpu.2005.0114. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- Kaiser Family Foundation. 2008. “Health Insurance Coverage in America, 2008” [accessed on November 11, 2010]. Available at http://facts.kff.org/chart.aspx?cb=57&sctn=161&p=1.
- Kessler R, Merikangas K. “The National Comorbidity Survey Replication (NCS-R): Background and Aims”. International Journal of Methods in Psychiatric Research. 2004;13((2)):60–8. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Ustun T. “The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI)”. International Journal of Methods in Psychiatric Research. 2004;13((2)):93. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, Furukawa TA, Gureje O, Hinkov H, Hu C, Lara C, Lee S, Mneimneh Z, Myer L, Oakley-Brown M, Posada-Villa J, Sagar R, Viana MC, Zaslavsky AM. “Screening for Serious Mental Illness in the General Population with the K6 Screening Scale: Results from the WHO World Mental Health (WMH) Survey Initiative”. International Journal of Methods in Psychiatric Research. 2010;19(suppl 1):4–22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kish L. Survey Sampling. New York: Wiley and Sons; 1965. [Google Scholar]
- Ku L, Waidmann T. How Race/Ethnicity, Immigration Status, and Language Affect Health Insurance Coverage, Access to Care and Quality of Care Among the Low-Income Population. Washington D C: The Henry J. Kaiser Family Foundation; 2003. [Google Scholar]
- Lillie-Blanton M, Hoffman C. “The Role of Health Insurance Coverage in Reducing Racial/Ethnic Disparities in Health Care”. Health Affairs. 2005;24((2)):398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- Lindrooth R, LoSasso A, Lurie I. “The Effect of Distance to Provider on Employee Response to Changes in Mental Health Benefits”. Health Economics. 2006;15:1133–41. doi: 10.1002/hec.1118. [DOI] [PubMed] [Google Scholar]
- McCarthy J, Blow F, Valenstein M, Fischer E, Owen R, Barry K, Hudson TJ, Ignacio RV. “Veterans Affairs Health System and Mental Health Treatment Retention among Patients with Serious Mental Illness: Evaluating Accessibility and Availability Barriers”. Health Services Research. 2007;42((3)):1042–60. doi: 10.1111/j.1475-6773.2006.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire T, Alegría M, Cook B, Wells K, Zaslavsky A. “Implementing the Institute of Medicine Definition of Disparities: An Application to Mental Health Care”. Health Services Research. 2006;41((5)):1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merwin E. “Shortages of Rural Mental Health Professionals”. Archives of Psychiatric Nursing. 2003;17((1)):42–51. doi: 10.1053/apnu.2003.1. [DOI] [PubMed] [Google Scholar]
- Miranda J, Cooper LA. “Disparities in Care for Depression among Primary Care Patients”. Journal General Internal Medicine. 2004;19:120–6. doi: 10.1111/j.1525-1497.2004.30272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, Mechanic D. “Perceived Need and Help-Seeking in Adults with Mood, Anxiety, or Substance Use Disorders”. Archives of General Psychiatry. 2002;59((1)):77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- Mulvaney-Day N, Earl T, Diaz-Linhart Y, Alegria M. “Preferences for Relational Style with Mental Health Clinicians: A Qualitative Comparison of African American, Latino and non-Latino White Patients”. Journal of Clinical Psychology. 2011;67((1)):31–44. doi: 10.1002/jclp.20739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Mental Health Collaborative Psychiatric Epidemiology Surveys (CPES) 2007. “Integrated Weights and Sampling Error Codes for Design-based Analysis” [accessed on November 9, 2010]. Available at http://www.icpsr.umich.edu/cocoon/cpes/using.xml?section-Weighting.
- Neighbors H, Caldwell C, Williams D, Nesse R, Taylor R, Torres M, Jackson JS. “Race Ethnicity, and the Use of Services for Mental Disorders: Results from the National Survey of American Life (NSAL)”. Archives of General Psychiatry. 2007;64:1–10. doi: 10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]
- Petry NM, Kiluk BD. “Suicidal Ideation and Suicide Attempts in Treatment-Seeking Pathological Gamblers”. Journal of Nervous Mental Disorders. 2002;190((7)):462–9. doi: 10.1097/01.NMD.0000022447.27689.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao JNK, Scott AJ. “On Chi-Squared Tests for Multiway Contingency Tables with Cell Proportions Estimated from Survey Data”. Annals of Statistics. 1984;12:46–60. [Google Scholar]
- Rao JNK, Thomas DR. “Chi-Squared Tests for Contingency Tables”. In: Skinner CJ, Holt D, Smith TMF, editors. Analysis of Complex Surveys. New York: John Wiley and Sons; 1989. pp. 89–114. [Google Scholar]
- Rehm J, Ustun T, Saxena S, Nelson C, Chatterji S, Ivis F. “On the Development and Psychometric Testing of the WHO Screening Instrument to Assess Disablement in the General Population”. International Journal of Methods in Psychiatric Research. 1999;8:110–23. [Google Scholar]
- Rosenbaum PR, Rubin DB. “The Central Role of the Propensity Score in Observational Studies for Causal Effects”. Biometrika. 1983;70((1)):41–55. [Google Scholar]
- Rust K, Rao J. “Variance Estimation for Complex Surveys Using Replication Techniques”. Statistical Methods in Medical Research. 1996;5((3)):283–310. doi: 10.1177/096228029600500305. [DOI] [PubMed] [Google Scholar]
- Schmidt L, Greenfield T, Mulia N. “Unequal Treatment: Racial and Ethnic Disparities in Alcoholism Treatment Services”. Alcohol Research and Health. 2006;29((1)):49–54. [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press, Institute of Medicine of the National Academies; 2003. [PubMed] [Google Scholar]
- Snowden L. “Barriers to Effective Mental Health Services for African Americans”. Mental Health Services Research. 2001;3((4)):181–7. doi: 10.1023/a:1013172913880. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata (release 8.2) Statistical Software. College Station, TX: Stata Corporation; 2004. [Google Scholar]
- Sturm R, Ringel J, Andreyeva T. “Geographic Disparities in Children's Mental Health Care”. Pediatrics. 2003;112((4)):e308. doi: 10.1542/peds.112.4.e308. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. 2002. “Poverty in the United States, 2001” [accessed on November 11, 2010]. Available at http://www.census.gov/prod/2002pubs/p60-219.pdf.
- U.S. Census Bureau. 2010. “Income, Poverty, and Health Insurance Coverage in the United States: 2009” [accessed on November 11, 2010]. Available at http://www.census.gov/prod/2010pubs/p60-238.pdf.
- U.S. Department of Health and Human Services. 2010. “Health Resources and Services Administration Bureau of Primary Health Care” [accessed on November 11, 2010]. Available at http://www.hrsa.gov/grants/apply/assistance/SAC/sacdataguidepdf.pdf. [DOI] [PubMed]
- Waidmann TA, Rajan S. “Race and Ethnic Disparities in Health Care Access and Utilization: An Examination of State Variation”. Medical Care Research and Review. 2000;57(4 suppl):55–84. doi: 10.1177/1077558700057001S04. [DOI] [PubMed] [Google Scholar]
- Wei W, Sambamoorthi U, Olfson M, Walkup J, Crystal S. “Use of Psychotherapy for Depression in Older Adults”. American Journal of Psychiatry. 2005;162((4)):711–7. doi: 10.1176/appi.ajp.162.4.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinick RM, Hasnain-Wynia R. “Quality Improvement Efforts Under Health Reform: How To Ensure That They Help Reduce Disparities Not Increase Them”. Health Affairs. 2011;30((10)):1837–43. doi: 10.1377/hlthaff.2011.0617. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


