Abstract
Objective
To compare the distribution of KCNJ11 polymorphisms between elderly Chinese population with and without hypertension.
Methods
We examined the mutation of KCNJ11 gene by directly sequencing. Data for the present study were obtained from 250 hypertensive subjects (60 to 83 years old) as well as 250 normotensive subjects (60 to 86 years old).
Results
We found nine different mutations in KCNJ11, including six novel mutations (I131M, L147I, L147V, L147L, Q235H, G245C). None of the novel mutations were found in the normotensive subjects, and all the residues were conserved in other species. These sequence variants in Chinese population indicate the diversity of the human library and the complexity of hypertension.
Conclusions
The consistent finding of our present study provided a basis for the development of new strategies to diagnosis and treat hypertension in the elderly.
Keywords: Essential hypertension, Phenotype, Genotype, Mutation, The elderly
1. Introduction
Hypertension remains the most common risk factor for cardiovascular morbidity and mortality. Both the prevalence and severity of hypertension increase markedly with aging. Current estimates suggest that approximately 160 million Chinese individuals suffer from hypertension, with a sizable population of elders. The profile of hypertension in older patients differs from that in younger patients and treatment of hypertension in the elderly today leaves much to be desired.[1]–[3] The comprehensive profile of hypertension in older patients is still being elucidated.
ATP-sensitive K+ (KATP) channels are found in many tissues, including heart, vascular smooth muscles, and vascular endothelial cells. KATP channels play especially important roles in the cellular responses of tissues under stress.[4]–[6] In the vascular system, KATP channels regulate the tonus of vascular smooth muscles, playing an important role in blood pressure regulation.[7],[8] The KATP channels are composed of four pore-forming inward rectifier subunits which belong to Kir6.X (Kir6.1 or Kir6.2) subfamily and four regulatory sulfonylurea receptor (SUR1 or SUR2) subunits. The combination Kir6.2/SUR2B is likely the most prevalent in vascular smooth muscle, although Kir6.1/SUR2B may also be present in this tissue.[9] Functional KATP channels are required to secure an optimal stress-adaptation capacity of the organism. They play important roles in the physiology and pathophysiology of various tissues by coupling the metabolic state of the cells with cellular electrical activity.[10] Recent advances in the vascular Kir6.2 channel indicate this channel modulates basal arterial tone and may contribute to vasodilatation in response to flow-induced shear stress.[7]
Previous studies have shown that some polymorphisms or mutations of the Kir6.2 gene were associated with type II diabetes mellitus and acute myocardial infarction.[11]–[14] Knockout of the Kir6.2 gene also causes maladaptive remodeling and heart failure in hypertension.[15] We aimed to explore the distribution of KCNJ11 polymorphisms in elderly Chinese population with and without hypertension to better understand the development and prevention of hypertension in Chinese elderly individuals.
2. Methods
2.1. Study population
Data for this study were obtained from 250 hypertensive subjects (60 to 83 years old) as well as 250 normotensive subjects (60 to 86 years old). Hypertension was defined as a systolic blood pressure ≥ 140 mmHg and/or a diastolic blood pressure ≥ 90 mmHg on repeated measurements, or receiving antihypertensive medication. Secondary hypertension was excluded by history and physical examination. All subjects were apparently healthy, based on the report of their medical history. A positive family history of essential hypertension was defined as the occurrence of hypertension in one or both biological parents. The ethics committee of our institution approved the study protocol. All of the subjects enrolled in this study were Chinese, and all of the subjects gave informed consent to participate in this study.
2.2. Study protocol
The plasma samples were collected between 8:00 and 10:00 am, after an overnight fast and abstinence from alcohol, tea or coffee. Casual blood pressure was measured in supine position over a 15 minutes resting period. Thereafter, blood samples were drawn from the antecubital vein for extracting whole DNA.
2.3. Direct DNA sequencing
DNA was extracted from peripheral blood leukocytes using standard techniques. Polymerse Chain Reaction (PCR) amplification of the Kir 6.2 gene was carried out, using the following primers: forward, 5′-CCGAGAGGACTCTGCAGTGA-3′, reverse, 5′-TGGGCTACATACCACATGGT-3′. The cycling program for PCR consisted of a denaturation step at 95°C for 5 minutes, followed by 35 cycles of denaturation at 95°C for 30 seconds, annealing at 55°C for 30 seconds, and extension at 72°C for 30 seconds, and then a final extension step at 72°C for 5 minutes. The PCR products were directly sequenced on both strands. Sequencing was done using an ABI PRISM Dye Terminator Cycle sequencing kit (Perkin-Elmer, Applied Biosystem, Foster City, Calif., USA) according to the manufacturer's instructions.
2.4. Statistical analysis
Statistical analyses were performed with SPSS 10.0. The gender ratio among hypertensive subjects, history of diabetes and family history of hypertension were compared by χ2 test. Values for continuous variables were presented as adjusted mean ± SD. P < 0.05 was deemed statistically significant.
3. Results
3.1. General characteristics
The mean body mass indexes were 25.0 ± 3.26 kg/m2 and 23.5 ± 3.14 kg/m2 in the hypertensive and normotensive subjects respectively. Body surface area of hypertensive subjects was higher than that of normotensive subjects (P < 0.01). Hypertensive subjects were more likely to have a positive family history of essential hypertension and clinical history of diabetes than normotensive subjects.
3.2. Identification of sequence variants in the Kir 6.2 gene
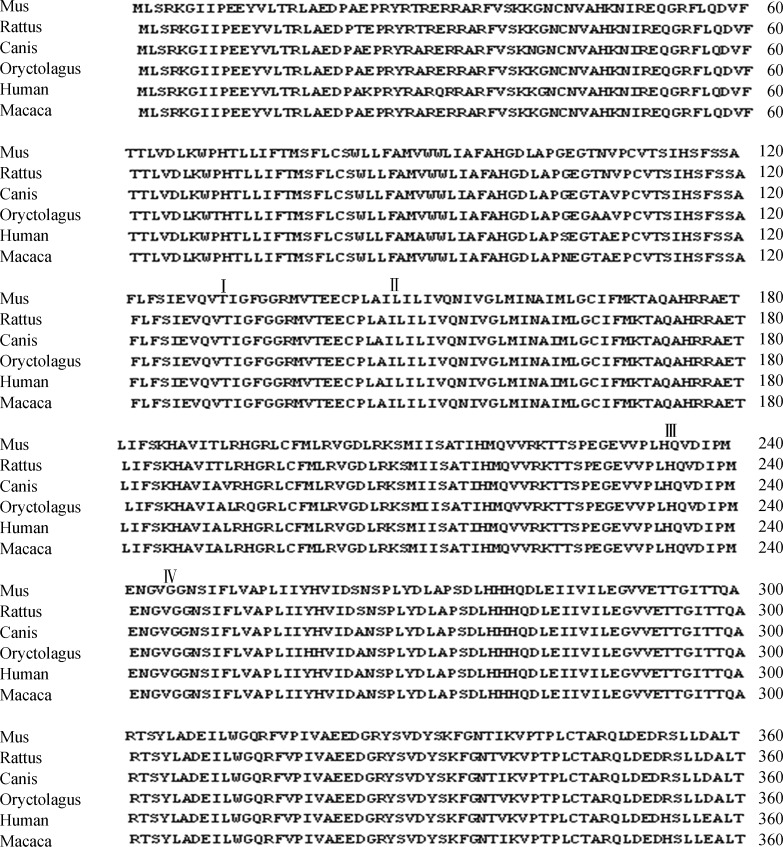
Analysis of the complete coding region of the Kir6.2 gene extracted from 250 unrelated, essential hypertensive individuals revealed several alterations of the nucleotide sequence in comparison to the wild type sequence. We found nine different missense mutations, of which six were novel: I131M (c.392 G>T), L147I (c.438 A>C), L147V (c.438 G>C), L147L (c.438 T>C), Q235H (c.704 T>G), G245C (c.731 T>G). Those novel mutations were not found in 250 normotensive individuals. All the mutations are conserved in rats, mice, rabbits, dogs, and macaques (Figure 1). As shown in Table 2, three mutations occurred in more than one individuals, that was, L147I (n = 2), L147V (n = 2) and Q235H (n = 2). Two individuals carried more than one mutation, one of which carried Q235H and G245C, and another carried L147L and Q235H.
Figure 1. Comparison of KCNJ11 protein sequences among different species.
I-IV indicates the position correspond to the amino acid substition of I131M, L147I (L147V, L147L), Q235H and G245C, respectively.
Table 2. Phenotypes of patients with the novel mutations of KCNJ11.
| Patient | Base substitution | Amino acid substitution | Age at diagnosis (year) | Blood pressure (mmHg) |
| 1 | T704G,T731G | Q235H,G245C | 35 | 180/110 |
| 2 | T438C | L147L | 42 | 168/97 |
| 3 | G438C | L147V | 37 | 175/105 |
| 4 | A438C | L147L | 46 | 182/96 |
| 5 | G438C | L147V | 41 | 192/113 |
| 6 | A438C,T704g | L147L,Q245H | 34 | 172/104 |
| 7 | G392T | I131M | 38 | 183/95 |
Table 1. General characteristics and blood pressure of normotensive subjects and hypertensive subjects.
| Phenotypes | Overall (n = 500) | No Event (n = 250) | Event (n = 250) | P Value |
| Age at testing (year) | 72.1 (6.0) | 71.8 (6.1) | 72.4 (5.5) | 0.254 |
| Age at onset (year) | − | − | 53.9 (14.5) | − |
| Men, n(%) | 280 (56) | 150 (60) | 130 (52) | 0.232 |
| Women, n(%) | 220 (44) | 100 (40) | 120 (48) | 0.178 |
| BMI (Kg/m2) | 24.5 (3.3) | 23.5 (3.1) | 25.3 (3.3) | P < 0.001 |
| BSA (m2) | 1.78 (0.15) | 1.85 (0.14) | 1.71 (0.13) | P < 0.001 |
| HR (bpm) | 72.7 (10.2) | 71.7 (9.7) | 73.8 (10.3) | 0.184 |
| SBP (mmHg) | 135.7 (20.3) | 124.1 (12.8) | 147.3 (19.8) | P < 0.001 |
| DBP (mmHg) | 80.3 (14.3) | 75 (9.8) | 85.6 (15.9) | P < 0.001 |
| Diabetes, n(%) | 64 (12.8) | 19 (7.5) | 45 (18) | 0.001 |
| Family history of HT, n(%) | 214 (42.8) | 42 (16.8) | 172 (68.8) | P < 0.001 |
Values are mean ± SD, whereas indicated otherwise. P values are based on the difference between normotensive subjects and hypertensive subjects. BMI: body mass index; BSA: body surface area; HR: heart rate; SBP: systolic blood pressure; DBP: diastolic blood pressure.
Two previously reported missense variants (E23K, I337V) and one silent change (A190A) were shown in Table 3. As shown in Table 3, a G-to-A change resulted in a glutamic acid-to-lysine substitution at codon 23 of KCNJ11 (E23K), and an A-to-G change resulted in an isoleucine-to-valine change at codon 337 KCNJ11 (I337V), while a T-to-C change did not result in an amino acid change at codon 190 (A190A). Neither genotypic nor allelic frequencies of E23K, ISS7V, and A190A differed between hypertension and control groups.
Table 3. Genotypic and allelic frequencies of variants between hypertensive patients and normal subjects.
| Hypertension Patients (n = 250) | Control subjects (n = 250) | P value | |
| E23K | |||
| Genotype | |||
| G/G | 104 (0.42) | 119 (0.48) | |
| G/A or A/A | 146 (0.58) | 131 (0.52) | 0.177 |
| Allele | |||
| G | 320 (0.64) | 346 (0.69) | |
| A | 180 (0.36) | 134 (0.31) | 0.213 |
| A190A | |||
| Genotype | |||
| T/T | 92 (0.37) | 102 (0.41) | |
| T/C or C/C | 158 (0.63) | 148 (0.59) | 0.359 |
| Allele | |||
| T | 288 (0.58) | 310 (0.62) | |
| C | 212 (0.42) | 190 (0.38) | 0.156 |
| 1337V | |||
| Genotype | |||
| AA | 121 (0.48) | 107 (0.43) | |
| AG or GG | 129 (0.52) | 143 (0.57) | 0.209 |
| Allele | |||
| A | 354 (0.71) | 338 (0.68) | |
| G | 146 (0.29) | 162 (0.32) | 0.273 |
Data are number of subjects with each genotype or number of alleles (% of each group).
All subjects with KCNJ11 mutation were diagnosed with hypertension at the age of forty or under the median age of diagnosis at age thirty-five.
4. Discussion
In the present study, a positive family history of essential hypertension occurred more commonly in hypertensive subjects than in normotensive subjects, indicating that hypertensive subjects may have a pre-existing genetic predisposition to blood pressure elevation.
We found nine different mutations in KCNJ11, identified by directly sequencing 250 patients with hypertension. We described six novel mutations (I131M, L147I, L147V, L147L, Q235H, G245C). None of the novel mutations was found in the normotensive subjects, and all the residues are conserved in other species. Therefore, these mutations may be pathogenic, although functional studies have not been performed. L147P, mutated at the same amino acid as L147I, L147V and L147L, has previously been reported, thus highlighting the functional importance of the residues.[16] Previous studies have revealed the altered response to ATP by KATP channels with mutations in Kir6.2 at several residues, reducing the ability of the channel to close in response to elevated levels of ATP, and functional analysis of those mutations shows that mutated residues within the Kir6.2 protein correlates with the observed phenotype.
In summary, the present study evaluated the genetic profile in Chinese older hypertensive subjects. The study provides important evidence for novel mutations in association with the pathogenesis of hypertension. These sequence variants in the Chinese population indicate the diversity of the human library and the complexity of hypertension. Further confirmatory studies on the functional effect of those novel mutations should further reveal the real contribution of this gene to hypertension.
Acknowledgments
The authors declare no conflict of interest. This work was supported by the grant from the National Natural Science Foundation of China (81170249, 30700305 and 30400549), the Key Project of National Natural Science Foundation of China (81030002), the 10th Five-Year Plan for Scientific and Technological Progress of the military (01MA104), Chinese Postdoctoral Science Foundation (20080431356), and Beijing Nova Program (2008A064).
References
- 1.Staessen JA, Fagard R, Thijs L, et al. Subgroup and per- protocol analysis of the Randomization European Trial on Isolated Systolic Hypertension in the Elderly. Arch Intern Med. 1998;158:1681–1691. doi: 10.1001/archinte.158.15.1681. [DOI] [PubMed] [Google Scholar]
- 2.Gambassi G, Lapane K, Sgadari A, et al. Prevalence, clinical correlates, and treatment of hypertension in elderly nursing home residents. Arch Intern Med. 1998;158:2377–2385. doi: 10.1001/archinte.158.21.2377. [DOI] [PubMed] [Google Scholar]
- 3.Borghi C, Dormi A, D'Addato S, et al. Trends in blood pressure control and antihypertensive treatment in clinical practice: the Brisighella Heart Study. J Hypertens. 2004;22:1707–1716. doi: 10.1097/00004872-200409000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Babenko AP, Aguilar-Bryan L, Bryan J. A view of Sur/KIR6.X, KATP channels. Annu Rev Physiol. 1998;60:667–687. doi: 10.1146/annurev.physiol.60.1.667. [DOI] [PubMed] [Google Scholar]
- 5.Haider S, Antcliff JF, Proks P, et al. Focus on Kir6.2: a key component of the ATP-sensitive potassium channel. J Mol Cell Cardiol. 2005;38:927–936. doi: 10.1016/j.yjmcc.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Zingman LV, Hodgson DM, Bast PH, et al. Kir6.2 is required for adaptation to stress. Proc Natl Acad Sci USA. 2002;99:13278–13283. doi: 10.1073/pnas.212315199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chrissobolis S, Sobey CG. Inwardly rectifying potassium channels in the regulation of vascular tone. Curr Drug Targets. 2003;4:281–289. doi: 10.2174/1389450033491046. [DOI] [PubMed] [Google Scholar]
- 8.Kane GC, Behfar A, Dyer RB, et al. KCNJ11 gene knockout of the Kir6.2 KATP channel causes maladaptive remodeling and heart failure in hypertension. Hum Mol Genet. 2006;15:2285–2297. doi: 10.1093/hmg/ddl154. [DOI] [PubMed] [Google Scholar]
- 9.Gögelein H, Hartung J, Englert HC. Molecular basis, pharmacology and physiological role of cardiac K(ATP) channels. Cell Physiol Biochem. 1999;9:227–241. doi: 10.1159/000016319. [DOI] [PubMed] [Google Scholar]
- 10.Seino S, Miki T. Physiological and pathophysiological roles of ATP-sensitive K+ channels. Prog Biophys Mol Biol. 2003;81:133–176. doi: 10.1016/s0079-6107(02)00053-6. [DOI] [PubMed] [Google Scholar]
- 11.Hansen JB. Towards selective Kir6.2/SUR1 potassium channel openers, medicinal chemistry and therapeutic perspectives. Curr Med Chem. 2006;13:361–376. doi: 10.2174/092986706775527947. [DOI] [PubMed] [Google Scholar]
- 12.Jeron A, Hengstenberg C, Holmer S, et al. KCNJ11 polymorphisms and sudden cardiac death in patients with acute myocardial infarction. J Mol Cell Cardiol. 2004;36:287–293. doi: 10.1016/j.yjmcc.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Koo BK, Cho YM, Park BL, et al. Polymorphisms of KCNJ11 (Kir6.2 gene) are associated with Type 2 diabetes and hypertension in the Korean population. Diabet Med. 2007;24:178–186. doi: 10.1111/j.1464-5491.2006.02050.x. [DOI] [PubMed] [Google Scholar]
- 14.Shimomura K. The K(ATP) channel and neonatal diabetes. Endocr J. 2009;56:56165–56175. doi: 10.1507/endocrj.k08e-160. [DOI] [PubMed] [Google Scholar]
- 15.Yamada S, Kane GC, Behfar A, et al. Protection conferred by myocardial ATP-sensitive K+ channels in pressure overload- induced congestive heart failure revealed in KCNJ11 Kir6.2-null mutant. J Physiol. 2006;577:1053–1065. doi: 10.1113/jphysiol.2006.119511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas P, Ye Y, Lightner E. Mutation of the pancreatic islet inward rectifier Kir 6.2 also leads to familial persistent hyperinsulinemic hypoglycemia of infancy. Hum Mol Genet. 1996;5:1809–1812. doi: 10.1093/hmg/5.11.1809. [DOI] [PubMed] [Google Scholar]