Abstract
Objective:
To critically review evidence for the effectiveness of electromyographic biofeedback (EMGB) of the quadriceps femoris muscle in treating various knee conditions.
Data Sources:
Databases used to locate randomized controlled trials included PubMed (1980–2010), Cumulative Index of Nursing and Allied Health Literature (CINAHL, 1995–2007), Web of Science (1986–2010), SPORTDiscus (1990–2007), and Physiotherapy Evidence Database (PEDro). Key words were knee and biofeedback.
Study Selection:
The criteria for selection were clinical randomized controlled trials in which EMGB of the quadriceps femoris was used for various knee conditions of musculoskeletal origin. Trials were excluded because of research designs other than randomized controlled trials, articles published in a non-English language, inclusion of healthy research participants, inability to identify EMGB as the source of clinical improvement, and lack of pain, functional outcome, or quadriceps torque as outcome measures.
Data Extraction:
Twenty specific data points were abstracted from each clinical trial under the broad categories of attributes of the patient and injury, treatment variables for the EMGB group, treatment variables for the control group, and attributes of the research design.
Data Synthesis:
Eight trials yielded a total of 319 participants with patellofemoral pain syndrome (n = 86), anterior cruciate ligament reconstruction (n = 52), arthroscopic surgery (n = 91), or osteoarthritis (n = 90). The average methodologic score of the included studies was 4.6/10 based on PEDro criteria. Pooled analyses demonstrated heterogeneity of the included studies, rendering the interpretation of the pooled data inappropriate. The EMGB appeared to benefit short-term postsurgical pain or quadriceps strength in 3 of 4 postsurgical investigations but was ineffective for chronic knee conditions such as patellofemoral pain and osteoarthritis in all 4 studies. Because the findings are based on limited data, caution is warranted until more randomized controlled trials are conducted to support or refute the general trends observed in this report.
Keywords: exercises, knee, rehabilitation
Key Points.
Electromyographic biofeedback of the quadriceps femoris muscle demonstrated potential improvements in knee extensor torque and functional outcome after anterior cruciate ligament reconstruction or meniscectomy.
Chronic knee conditions, such as patellofemoral pain and osteoarthritis, did not benefit from electromyographic feedback.
However, the number of included studies was small; variability in patient populations, interventions, and outcomes was large; and methodologic problems were identified. Therefore, further investigation is warranted.
Musculoskeletal conditions such as anterior cruciate ligament (ACL) ruptures, meniscal lesions, patellofem-oral pain syndrome, and osteoarthritis of the knee are associated with a loss of quadriceps muscle force production and cross-sectional area.1–4 A combination of limb disuse,5 arthrogenic muscular inhibition,6 and pain avoidance behaviors7 may contribute to quadriceps impairment. Strong evidence indicates that functional outcome of the knee and recovery of the quadriceps are associated8–12 and that knee extensor exercise may improve these outcomes.12–15
Electromyographic biofeedback (EMGB) is a tool for detecting and amplifying the electric activity of muscles and providing the patient with visual or auditory information about the magnitude of muscular tension. The EMGB may be used to modulate muscle contraction by bringing the muscular tension to the level of consciousness, such that a patient may adjust motor output accordingly. This tool has been used therapeutically for incontinence and constipation,16 tension headaches,17 facial paralysis,18 motor function after stroke,19 phonatory performance,20 and temporomandibular joint disorders.21 In general, these reviews demonstrated mixed levels of effectiveness, but a beneficial trend was observed when EMGB was used to decrease muscular tension.
In the domains of orthopaedics and sports medicine, knee conditions have drawn the most attention from authors of clinical trials investigating the effectiveness of EMGB. Perhaps this is the case because quadriceps function is related to knee outcomes8–12; knee dysfunction may cause a neuromuscular imbalance between the heads of the vastus medialis (VM, or more specifically the vastus medialis oblique [VMO]) and the vastus lateralis (VL),22 and this imbalance may be a causative factor for patellofemoral pain.23 Quadriceps atrophy and inhibition are present in various knee conditions, so EMGB may be used as an adjunct to progressive resistive exercises of the quadriceps. Despite common use of biofeedback in knee rehabilitation, we did not find any summaries of its use as an adjunct to therapeutic exercise. Thus, the purpose of our investigation was to answer the following clinical question: Does EMGB of the quadriceps improve patient-oriented outcomes and quadriceps strength after knee dysfunction? Until recently, a critical mass of trials on EMGB had not been published.
METHODS
Data Sources
We performed a search of clinical trials in the following databases: PubMed (1980–2010), Cumulative Index of Nursing and Allied Health Literature (CINAHL, 1995–2007), Web of Science (1986–2010), Sport DISCUS (1990–2007), and the Physiotherapy Evidence Database (PEDro) to gather evidence relating to quadriceps exercise with EMGB for knee rehabilitation. Search terms were limited to knee and biofeedback. For the CINAHL and PubMed searches, we used a sensitive clinical query as advocated by Haynes et al.24 A hand search was used to identify additional trials, particularly those outside the database time frames.
Study Selection
Included in this review were clinical randomized controlled trials in which EMGB of the quadriceps femoris was used for various knee conditions. Exclusion criteria consisted of research designs other than randomized controlled trials, articles published in a non-English language, inclusion of healthy research participants, research designs in which EMGB treatment effects could not be distinguished from other treatment effects, and investigations that did not include pain, functional outcome, or quadriceps torque as outcome measures. We initially screened references by viewing the article title and abstract. If we could not clearly determine that an article met at least one of the criteria for exclusion, we obtained the full-text article for further review. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram25 for the selection of trials for this review is illustrated in Figure 1.
Figure 1.
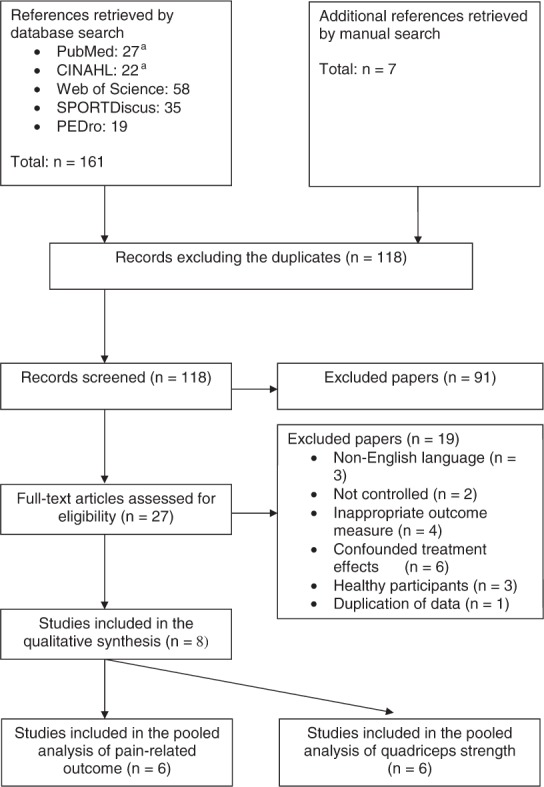
PRISMA flow diagram demonstrating the selection of trials.
a A high-sensitivity clinical query was used to filter the results.24 Abbreviations: CINAHL, Cumulative Index of Nursing and Allied Health Literature; PEDro, Physiotherapy Evidence Database.
Methodologic Assessment
The PEDro criteria were used to identify possible biases in the included research. Eight criteria assess internal validity, and 2 criteria evaluate external validity for each trial. These criteria include participant eligibility criteria, random allocation, concealed allocation, baseline similarity, participant blinding, therapist blinding, assessor blinding, adequate follow-up, intention to treat, statistical comparison, and point estimate.26 The cumulative PEDro score demonstrated high intertester reliability (intraclass correlation = 0.91).27
Data Extraction
A priori, we compiled a list of specific data to be drawn from each included article. Abstracted characteristics of the patients and injuries included the type of knee dysfunction, number of patients, age, sex, and duration of symptoms or time since surgery. Data pertinent to the EMGB treatment included location and alignment of the electrodes, feedback type, and patient instructions. Information pertaining to the control group treatment (ie, exercises performed, exercise variables, nonexercise care, and treatment period) was also recorded. Lastly, attributes of the research design were extracted, including follow-up periods, methods for strength testing, functional outcome or pain measures, mean and SD values, and statistical significance among treatment groups.
Consistency of Findings
Study selection, methodologic assessment, and data extraction were independently evaluated by each author. Discrepancies among the findings were discussed until a consensus was reached.
Pooled Analysis
Pooled analyses were performed on all included studies that provided pain-related outcome or quadriceps strength measures. Data necessary for inclusion in the pooled analyses included group sizes, means, and standard deviations collected immediately after the end of the intervention period. When multiple variables were used to assess pain-related outcome, we placed the highest priority on disease-specific, then joint-specific, and lastly global pain or outcome measures. Similarly, quadriceps strength measures were assessed in numerous ways that were prioritized for the analyses. Priority went to isokinetic dynamometry at the slowest velocities, then isometric dynamometry, followed by isotonic tests of maximal intensity. When bilateral dysfunction was present, data from the right limb were analyzed. For each pooled analysis, only one value from each group could be entered into the calculation. The dependent variables were prioritized to ensure “appropriateness”28 of functional outcomes and a greater reflection of maximal torque production capacity with low-velocity isokinetic tests.
Data from the included studies were entered into RevMan Software (version 5.0; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). The analyses were performed across all included data and across subgroups defined by the type of knee dysfunction. A fixed-effects model was used to determine standardized mean differences and 95% confidence intervals. Because the software does not correct for differences in the direction of the scale, the group means had to be multiplied by −1 when higher scores were of clinical benefit.29
RESULTS
Study Selection
The database search yielded 161 citations specific to the search terms used, 50 of which were duplicates. A hand search found an additional 7 publications that had not been identified by the database search. A total of 118 citations were screened by title and abstract, which eliminated 91 of the studies. Each of the remaining 27 articles was examined in full text to determine suitability for inclusion. After the review, additional trials were excluded on the basis of non-English language (n = 3),30–32 no control group (n = 2),33,34 inappropriate outcome measures (n = 4),35–38 confounded treatment effects (n = 6),39–44 inclusion of healthy participants (n = 3),45–47 and duplication of data between studies (n = 1).48 The duplicate trials48,49 shared functional outcome data, but one also provided isokinetic testing of the knee, making it the appropriate choice for inclusion.49 Two trials that were excluded on the basis of inappropriate outcomes investigated quadriceps strength with noninstrumented manual muscle testing36 and while pressing the knee against a sphygmomanometer.38 Eight articles met the criteria for inclusion in this systematic review. Six of these provided the quantitative data for a pooled analysis on pain-related outcomes, and another combination of 6 trials included data for a pooled analysis on quadriceps strength. The selection process is reflected in the PRISMA flow diagram25 in Figure 1.
Study Quality
The 8 included studies had an average PEDro score of 4.625/10, as illustrated in Table 1. These scores represent multiple sources of bias that may skew the results. The most common shortcomings were lack of blinding (patient, therapist, or assessor), concealed allocation, and intention-to-treat analyses. One trial was quasirandomized by birth date, which met the criteria for inclusion in this review but was not considered randomized by PEDro criteria.55 Another trial was described as double blind, but only the assessors were blinded.49
Table 1.
Methodologic Assessment of Included Studies With Physiotherapy Evidence Database (PEDro) Scores
| Author | Random Allocation? | Concealed Allocation? | Baseline Comparability? | Blind Participants? | Blind Therapists? | Blind Assessors? | Follow-Up? | Intention-to-Treat Analysis? | Group Comparisons? | Point and Variability Measures? | Cumulative Score (Maximum = 10) |
| Draper50 | Yes | No | No | No | No | No | Yes | No | Yes | Yes | 4 |
| Draper and Ballard51 | Yes | No | No | No | No | No | Yes | No | Yes | Yes | 4 |
| Durmus et al52 | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| Dursun et al53 | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| Kirnap et al54 | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| Levitt et al55 | No | No | Yes | No | No | No | No | No | Yes | Yes | 3 |
| Yilmaz et al56 | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| Yip and Ng49 | Yes | No | Yes | No | No | Yes | Yes | No | Yes | Yes | 6 |
| Cumulative score | 7/8 | 0/8 | 6/8 | 0/8 | 0/8 | 1/8 | 7/8 | 0/8 | 8/8 | 8/8 | 4.625 |
Two trials failed to meet the “baseline comparability” criterion of PEDro; the postsurgical studies used a posttest-only design when the outcome of interest was quadriceps strength testing.50,51 A third postsurgical study met the baseline comparability PEDro criterion because of the preintervention and postintervention assessment of functional outcome but limited the assessment of quadriceps strength to after the EMGB intervention period.55 This scenario produced uncertainty about the equality of the groups before the intervention with respect to important outcome measures in the study. Therefore, one cannot affirm that differences between groups at follow-up were exclusively due to the study intervention.
Data Synthesis
The 8 studies consisted of a total of 319 participants with patellofemoral pain syndrome (2 trials,49,53 n = 86), ACL reconstruction (2 trials,50,51 n = 52), arthroscopic surgery (2 trials,54,55 n = 91), and osteoarthritis (2 trials,52,55 n = 90). For the trials that used EMGB after arthroscopy54,55 the largest number of patients had a meniscectomy (73.6%), followed by patellar chondromalacia (11.0%), synovitis (5.5%), loose bodies (2.2%), or a combination of the aforementioned conditions (7.7%). The ages of the patients varied according to the knee dysfunction, with ACL reconstruction, patellofemoral pain, arthroscopy, and osteoarthritis representing a spectrum of ages from youngest to oldest, respectively. The respective proportions of female and male patients varied by condition: patellofemoral pain syndrome (74.4% versus 25.6%), ACL reconstruction (40.4% versus 59.6%), arthroscopy (17.6 versus 82.4%), and osteoarthritis (94.4% versus 5.6%). See Table 2 for additional demographic details.
Table 2.
Demographic Characteristics of Patients in the Included Studies
| Authors | Condition or Procedure | Patients, No. | Duration of Dysfunction | Age, y | Sex (Women/Men) |
| Dursun et al53 | Patellofemoral pain | 60 | E: 10.8 ± 7.7 moC:9.7 ± 8.1 mo | E: 36.9 ± 9.2C: 36.6 ± 10.6 | 48/12 |
| Yip and Ng49 | Patellofemoral pain | 26 | NA | T: 32.5 ± 8.8 | 16/10 |
| Draper50 | Acute anterior cruciate ligament reconstruction | 22 | 1 wk postoperatively | T: 23 | 7/15 |
| Draper and Ballard51 | Acute anterior cruciate ligament reconstruction | 30 | Immediately postoperatively | E: 25 ± 8.1C: 24 ± 7.7 | 14/16 |
| Kirnap et al54 | Arthroscopic meniscectomy | 40 | 3 d postoperatively | T: 34.5 ± 10.3 | 0/40 |
| Levitt et al55 | Arthroscopy:Meniscectomy, n = 27Patellar chondromalacia, n = 10Synovitis, n = 5Loose bodies, n = 2Combination, n = 7 | 51 | Immediately postoperatively | E: 45 ± 15C: 48 ± 15 | 16/35 |
| Durmus et al52 | Osteoarthritis (grade I–II) | 50 | NA | E: 54.7 ± 1.8C:54.8 ± 2.0 | 50/0 |
| Yilmaz et al56 | Osteoarthritis (grade I–III) | 40 | E: 17.5 ± 9.1 moC: 15.6 ± 8.5 mo | E: 55.6 ± 7.2C: 59.4 ± 5.6 | 35/5 |
| 8 Trials | 4 General knee conditions | 319 | 186/133 |
Abbreviations: C, control group; E, experimental group; NA, data not available; T, total sample.
The EMGB treatment of the quadriceps was not uniform among studies. Two channels were used to elicit feedback in nearly all the trials. However, in both postoperative ACL reconstruction trials, a single electrode was placed proximal to the patella and offset slightly to the medial side but not described as being placed over any specific muscle.50,51 When 2 electrodes were used, the VL always had an electrode placed superficial to it. The second of the 2 electrodes was placed on either the VM53,56 or, more specifically, the VMO.49,54,55 In another study, the 2 electrodes were vaguely described as being placed over 3 heads of the quadriceps,52 leaving uncertainty about their exact location. When the information was provided, all authors indicated that the active electrodes were aligned with the muscle fibers below. In 6 trials, the EMGB devices provided visual and auditory feedback; one investigation each used units with visual49 or auditory54 feedback alone. Four groups used a threshold function, in which no feedback was provided until a certain amount of electric activity was detected in the muscle. Three of these groups50,51,54 vaguely described the EMGB threshold as near maximum isometric contraction, and another53 clearly described the threshold value as 80% of the average of 3 maximal contractions. Patients treated with EMGB for ACL reconstruction, arthroscopy, or osteoarthritis were encouraged to maximally contract all heads of the quadriceps, whereas those with patellofemoral pain syndrome were instructed to increase the activity of the VM or VMO while maintaining a lower level of activity in the VL.49,53 See Table 3 for additional details of the EMGB treatment.
Table 3.
Attributes of Electromyographic Feedback in Included Studies
| Authors | Biofeedback Device | Electrode Locations | Electrode Orientation | Feedback Type | Threshold Level | Electromyographic Feedback Instructions |
| Dursun et al53 | Myomed 932 (Enraf-Nonius, Rotterdam, Netherlands) | 2: VM and VL, in the areas of greatest muscle bulk | Along the direction of the fibers of each muscle | Visual and auditory | 80% of average of 3 aximal contractions | Contract VM above threshold while attempting to keep VL below threshold |
| Yip and Ng49 | Custom-designed device | 2: Midpoint of VMO, about 4 cm superior and 3 cm medial to the superomedial border of the patella;VL: 10 cm superior and 7 cm lateral to the superior border of the patella | Electrode over the VMO oriented 55° to the diagonalElectrode over the VL oriented 15° to the diagonal | Visual | NA | Increase activity of VMO while maintaining stable activity in VL during exercise |
| Draper50 | Cyborg model J33 portable unit (Autogenic Systems, Chicago, IL) | 1: Placed just proximal to the patella and 2 cm medial | NA | Visual and auditory | Initial threshold value selection different for each patient; threshold settings reevaluated at each session and reset if necessary | NA |
| Draper and Ballard51 | Myotrac electromyographic biofeedback unit (Thought Technology Ltd, West Chazy, NY) | 1: Placed 3–5 cm above the superior border of the patella and 2–3 cm medial | NA | Visual and auditory | Threshold that the patient could achieve only by contracting with maximal effort | NA |
| Kirnap et al54 | Myomed 932 | 2: VMO: placed 4 cm above the upper edge of the patella on the VMO muscle and at 3 cm medial;VL: placed 10 cm above the upper edge of the patella and 6–8 cm lateral | Angle of 55° by the vertical plane Angle 15° from the vertical plane | Auditory | Increase threshold every day | NA |
| Levitt et al55 | BioPrompt portable electromyography unit (EMPI, Inc, St Paul, MN) | 2: VMO and VL described but reference regarding placement described only VM and VL over the muscle bellies, not VMO (Basmajiana) | Reference demonstrates vertical placement of the electrodes over each musclea | Visual and auditory | NA | Maximally contract quadriceps |
| Durmus et al52 | Myomed 432b | 2: “Two superficial electrodes were placed over the patient's rectus femoris, vastus medialis, and vastus lateralis muscles” | NA | Visual and auditory | NA | Increase visual and auditory signals at every contraction |
| Yilmaz et al56 | Myomed 932 | 2: VM and VL | Parallel to the muscle fibers | Visual and auditory | NA | NA |
Abbreviations: NA, not available; VL, vastus lateralis; VM, vastus medialis; VMO, vastus medialis oblique.
aBasmajian JV, ed. Biofeedback: Principles and Practices for Clinicians. 3rd ed. Baltimore, MD: Williams & Wilkins; 1989.
bThis model was not listed on the manufacturer's Web site.
Because EMGB functions as an adjunct to quadriceps exercise in those with knee dysfunction, all patients participated in exercise programs. All authors compared quadriceps exercise and EMGB with quadriceps exercise and no EMGB, but in 2 trials electrotherapy was superimposed during the control groups' exercises.51,52 The exercise programs focused the use of the EMGB device on quadriceps setting and straight-leg– raise exercises, except for one study that used only flexed-knee quadriceps isometric exercises.52 In that same study, the exercises and exercise variables were slightly different between the EMGB and control groups.52 Otherwise, the exercise interventions were the same between the EMGB and control groups. Exercise variables were poorly reported by most authors, so that the sets, repetitions, intensity, and recovery after the exercises are largely unknown. Nonexercise treatments were uncommon but consisted of cryotherapy, patellar mobilization, controlled weight bearing, postoperative bracing, and electro-therapy. The exercise programs varied in duration from 10 days to 12 weeks, 2 to 7 days per week, and 1 to 3 times daily. The settings included outpatient therapy, home exercise programs, and group exercise programs. For additional details about the exercise programs of the included studies, see Table 4.
Table 4.
Characteristics of the Therapeutic Interventions in the Included Trials
| Authors | Control Group Treatment | Exercises Performed | Exercise Variables | Nonexercise Care | Treatment Period and Frequency |
| Dursun et al53 | Exercise only | Quadriceps setting, straight-leg raises, hip adductor strengthening, terminal knee extensions, and closed kinetic chain exercises; hamstrings, triceps surae, iliotibial band, and quadriceps stretching; proprioception training; bicycling | Duty cycle 10:20 s | NA | 4 wk, 5 d/wk (EMGB group wore the device only 3/5 weekly sessions) |
| Yip and Ng49 | Exercise only | Quadriceps, hamstrings, gastrocnemius, hip adductors, and iliotibial band flexibility; quadriceps setting, terminal knee extension, semisquat, wall slide, lunge, step-up, step-down, eccentric hamstrings exercise, and hip adduction exercises; balance and proprioception training; plyometric and agility training | NA | NA | 8-wk daily home exercise program |
| Draper50 | Exercise only | Quadriceps setting, straight-leg raises, active and passive range of motion, isokinetic exercises | 1 wk postoperatively: 10 repetitions2 wk: increased repetitions4 wk: straight-leg raises, 5 sets of 10 each in prone, supine, and side-lying position | Electric stimulation progress to weight bearing tolerated at 12 wk | 12 wk (18 or 26 sessions, depending on the patient's schedule) |
| Draper and Ballard51 | Exercise and electrotherapy | Quadriceps setting, straight-leg raises, active and active-assistive range of motion, hamstrings stretching, isotonic knee extension and flexion exercises | Duty cycle 10:20 s (in conjunction with EMGB or electrotherapy), 3 sets of 10 (wk 1–2), 5 sets of 10 (wk 3–6), progressively increasing intensity | Progress to weight bearing as tolerated at 4 wk | 6 wk total wk 1–4: daily home exercise program, 3×/d wk 5–6: 3 sessions/wk at rehabilitation clinic |
| Kirnap et al54 | Exercise only | Phase 1: quadriceps setting, straight-leg raises Phase 2: hip adductor strengthening and terminal knee extension added Phase 3: closed kinetic chain exercises and lateral step-up exercises added | Duty cycle 5:10 s over 20 cycles | Cryotherapy and patellar mobilization | 2 wk, 5 d/wk |
| Levitt et al55 | Exercise only | Quadriceps setting | Duty cycle 5:10 s | NA | 10-d home exercise program, 3×/d |
| Durmus et al52 | Exercise and electrotherapy | Isometric knee extension (EMGB at 25°–30° knee flexion, electrotherapy at 60° knee flexion) | EMGB duty cycle 10:50 s, electrotherapy duty cycle 10:10 s | NA | 4 wk, 5 d/wk |
| Yilmaz et al56 | Exercise only | Quadriceps isometrics, minisquats, hip adductor isometrics, 4-way straight-leg raises, terminal knee extension | 10 repetitions | NA | 3 wk, 3×/d, both supervised group and home exercise programs |
Abbreviations: EMGB, electromyographic biofeedback; NA, not available.
Three groups50,51,54 found some benefit of EMGB after knee surgery. Two of these were published by the same lead author and demonstrated EMGB as superior for ACL-reconstructed patients in developing quadriceps strength relative to exercise-only50 and electrotherapy-exercise conditions.51 Both studies had below-average PEDro scores (4/10 each) and were post-test-only designs. Therefore, one cannot determine whether the differences between the experimental and control groups were, in fact, due to the intervention. These studies are likely to be more prone to bias and confound, so we must interpret them with great caution. The third study54 that demonstrated positive findings investigated the role of EMGB for 2 weeks after arthroscopic meniscectomy. A disparity in Lysholm knee scores was not present preoperatively or 3 days postoperatively, but at 2 and 6 weeks postoperatively, a difference was noted between the EMGB and exercise-only groups. The methods used in this investigation were slightly above average (5/10) but lacked blinding, concealed allocation, and an intention-to-treat analysis. Despite possible biases, this trial was as sound as any other of the included studies and should be seriously considered as evidence of the effectiveness of EMGB. For further information on the findings of individual studies, see Table 5.
Table 5.
Dependent Variables and Outcomes of Interest From Included Studies
| Authors | Knee Strength Assessment | Pain and Functional Outcomes Assessed | Measurement Intervals | Between-Groups Results at End of Intervention Period |
| Dursun et al53 | NA | 10-point VAS, greatest level of knee discomfort over the past wk Functional Index Questionnaire | Baseline and 1, 2, 3 mo | No differences between groups for VAS or Functional Index Questionnaire |
| Yip and Ng49 | Isokinetic peak torque andtotal work on a Cybex dynamometer (Cybex International, Medway, MA) at 120°/s normalized to body weight | Patellofemoral Pain Syndrome Severity Scale | Baseline and 4, 8 wk | No differences between groups for isokinetic peak torque or the Patellofemoral Pain Syndrome Severity Scale |
| Draper50 | Isometric peak torque on Cybex II dynamometer at 90°, 60°, and 45° of knee flexion, normalized to uninjured limb | NA | Posttest only at 12 wk postoperatively | EMGB group had less side-to-side peak torque difference than the non-EMGB group at all 3 angles |
| Draper and Ballard51 | Isometric peak torque on a Cybex II dynamometer at 60° of knee flexion, normalized to uninjured limb | NA | Posttest only at 6 wk postoperatively | EMGB group had less of a side-to-side peak torque difference than the exercise and electrotherapy group |
| Kirnap et al54 | NA | Lysholm Knee Score | Preoperatively and 3 d and 2 wk, 6 wk postoperatively | Improvement in Lysholm Knee Score of the EMGB group relative to exercise-only control group |
| Levitt et al55 | Isokinetic peak torque on a Biodex II device (Biodex Medical Systems, Shirley, NY) at 120°/s, raw score | Pain Rating Scale (similar to VAS, but lower number represents more severe pain) | Baseline (no baseline knee torque), 14 d | No differences in pain rating scale or isokinetic peak torque between groups |
| Durmus et al52 | 1-, 10-repetition maximum isotonic quadriceps strength | VAS, WOMAC, 50-m walk, ascent and descent of 10-stair flight | Baseline, 4 wk | No differences in the outcomes between EMGB and exercise and electrotherapy control group |
| Yilmaz et al56 | Isokinetic peak torque on a Cybex dynamometer at 60°/s and 180°/s and isometric knee extension torque at 65° knee flexion, raw scores | VAS, WOMAC, Nottingham Health Profile | Baseline, 3 wk | Improvements were noted in the Nottingham Health Profile dimensions of sleep and energy in the EMGB group relative to exercise only-control group |
Abbreviations: EMGB, electromyographic biofeedback; NA, not available; VAS, visual analogue scale; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
For the pooled analyses, pain-related outcome measures and quadriceps strength values were extracted. Six of the 8 trials contained data that could be used in the pooled analysis of pain-related outcomes.49,52–56 The outcomes measures used in the pooled analysis were the Western Ontario and Mc-Master Universities Arthritis Index (WOMAC) pain scale,52,56 Functional Index Questionnaire,53 Patellofemoral Pain Severity Scale,49 Lysholm Knee Score,54 and Pain Rating Scale.55 The data for the pooled analysis of the quadriceps strength measures were derived from 5 studies; factors analyzed were peak knee extensor torque at 60°/s56 and 120°/s,49,55 isometric knee extensor torque at 60°,51 and a 1-repetition maximum effort of the right knee during an isotonic knee extension test.52
The overall pooled analysis for pain-related outcome measures after EMGB demonstrated heterogeneity of the included studies (χ52 = 43.14, P < .01, I2 = 88%), and therefore interpretation of the pooled data was inappropriate. Pooled analyses within the subgroups were also heterogeneous, the exception being the patellofemoral pain syndrome data (χ12 = 0.15, P = .70, I2 = 0%). The overall effect within the patellofemoral pain group was equivocal (z = 1.70, P = .09), despite nearly reaching statistical significance. Standardized effects for the included studies are presented in Figure 2.
Figure 2.
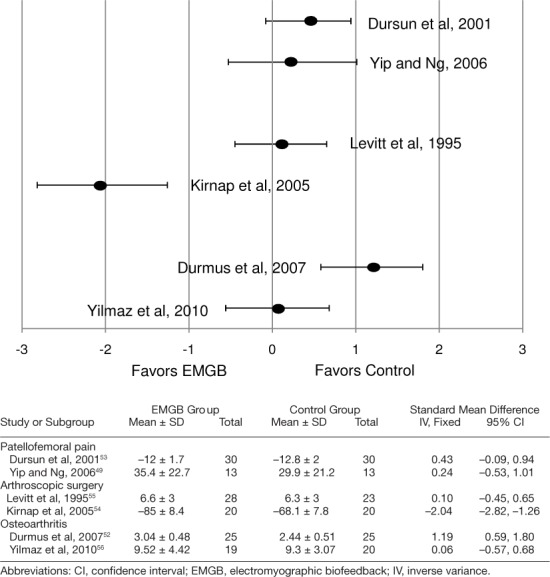
Standardized mean differences for patient-oriented outcomes (ie, functional outcome or pain).
Similarly, the overall pooled effect for quadriceps strength after EMGB yielded heterogeneous data (χ42 = 18.33, P < .01, I2 = 78%), which precluded an analysis of the effect. The pooled analysis within the osteoarthritis subgroup demonstrated both insignificant heterogeneity (χ12 = 1.10, P = .29, I2 = 9%) and an improvement in the strength of the control group relative to the EMGB group (z = 2.99, P = .003). Standardized effects for the included studies are presented in Figure 3.
Figure 3.
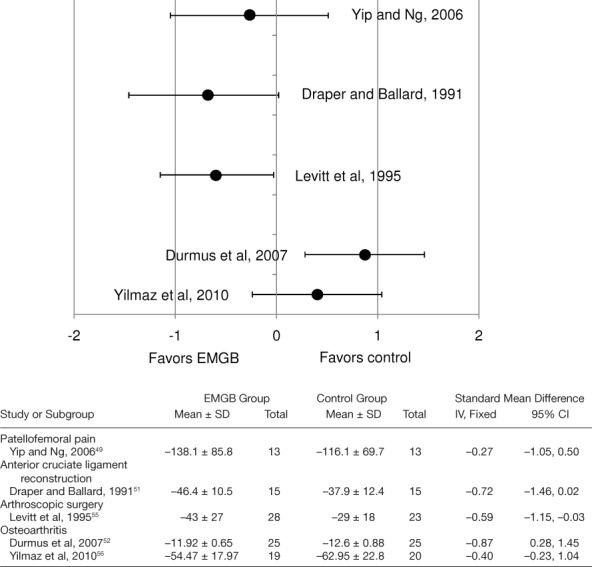
Standardized mean differences for quadriceps muscle strength.
DISCUSSION
Does EMGB of the quadriceps improve patient-oriented outcomes and quadriceps strength after knee dysfunction? Our findings are largely equivocal because of the limited number of trials in this area. However, with great caution we note that EMGB appeared to benefit short-term postsurgical pain and quadriceps strength in 3 of 4 studies.50,51,54,55 Furthermore, EMGB was not effective for chronic knee conditions, such as patellofemoral pain and osteoarthritis, and may border on being less effective than exercise alone for patients in these subgroups.
Surgical Knee Conditions
The evidence in favor of EMGB as an adjunct to exercise postoperatively has substantial limitations. First, the external validity of one of the positive studies50 is severely compromised by its focus on open ACL reconstructions, which are no longer performed. Nonetheless, positive results were noted during arthroscopic meniscectomy54 and arthroscopic ACL reconstruction,51 which are common surgical procedures. Internal validity of the trials that focused on ACL reconstruction35,51 was confounded by the use of posttest-only designs. Therefore, it is unclear whether the differences found between the groups were present immediately after randomization or whether they resulted from the EMGB intervention. The difficulty encountered by the researchers in these studies was that a baseline postoperative isokinetic knee extensor torque measurement after ACL reconstruction was contraindicated because of fragile graft fixation and compromised patellar tendons. Unfortunately, these same authors35,51 failed to include functional outcome or pain scale measurements, which could have been used as evidence for postoperative similarities between the experimental and control groups. Lastly, both postoperative ACL reconstruction studies35,51 had lower than average PEDro methodology scores, potentially skewing the results.
Perhaps improvements in pain and quadriceps strength in postsurgical patients result from extrinsic EMGB competing with intrinsic feedback from nociceptors during painful movements or muscle contractions. Evidence57 suggests that pain is directly related to fear of movement and inversely related to function of the ACL-reconstructed knee. Most pain and fear of movement exist immediately after surgery and progressively decline over time.57 During the early postoperative period, EMGB combined with encouragement from the clinician may sufficiently motivate the patient to overcome the fear of movement and intense pain, subsequently minimizing disuse atrophy of the quadriceps.
Physiologically, it is counterintuitive that EMGB may be effective in increasing quadriceps strength early after surgery. A large effusion tends to occur immediately after knee surgery secondary to the trauma. Several groups22,58,59 have established that even a minimal knee joint effusion may cause arthrogenic muscle inhibition of the quadriceps. Arthrogenic muscle inhibition reduces the ability of the patient to produce a true maximal contraction, either with or without EMGB, because the reflex response is beyond the patient's conscious control.60 Researchers have demonstrated EMGB-related improvements in the electric activity of the quadriceps after arthroscopic knee procedures.54,55 Perhaps quadriceps exercise concurrent with EMGB encourages patients to increase muscle activation, resulting in an improvement in muscular function.
Chronic Knee Conditions
Patients with chronic knee conditions, such as patellofemoral pain syndrome and osteoarthritis, did not appear to derive any benefit from the use of EMGB with exercises. In fact, most data from these subgroups indicated that EMGB might even be a detriment relative to exercise-only or an exercise plus electro-therapy treatment. Whether this trend is an artifact or a result of the EMGB intervention is unclear. Perhaps the novel use of EMGB could be confusing and distracting to some; however, if this were the case, the effect should have been seen across all studies, independent of patients' knee conditions.
Electromyographic feedback is commonly used to increase VMO activation and reduce patellofemoral pain. The VMO is a dynamic stabilizer of the patellofemoral joint and may influence patellar tilt and lateral shift in those with patellofemoral pain.61 Despite this mechanical influence, patellofemoral degeneration in human cadavers does not correspond with structural attributes of the VM62 or VMO.63 A delay of VMO activation onset may or may not exist in patients with patellofemoral pain,64 but if it does, whether the neuromuscular impairment is a cause or effect of patellofemoral pain is unknown.
Although evidence against the effectiveness of EMGB for patellofemoral pain is modest, quadriceps exercise alone does reduce patellofemoral pain.15,65 The mechanism of pain reduction is unknown, but it is unlikely that the quadriceps exercises preferentially activate the VMO.66 In a randomized controlled trial, Syme et al44 found that VMO-specific exercises were no better than general quadriceps exercises for reducing patellofemoral pain. Furthermore, arthroscopic debridement of the patellofemoral joint and subsequent quadriceps exercises were no better than quadriceps exercise alone,67 and the surgical intervention may lead to prolonged quadriceps inhibition.68
Limitations to the Systematic Review
Several limitations to this systematic review exist. First, a small number of trials was included in the review. Also, patient populations, interventions, and outcomes in the included studies varied significantly, making comparisons very difficult. In particular, the exercise variables were conspicuously absent from most of the investigations. Allocation was inadequately concealed, and adequate blinding of the participants, therapists, and assessors was lacking, which often positively biases outcomes.69 In addition, intention-to-treat analyses were not performed; these assessments may yield biased data, but the magnitude and direction of the bias are variable.70,71 As more research becomes available and journals become more stringent about the reporting of trial methods, the effect of bias will be reduced and the true clinical effectiveness of EMGB will become clearer.
Suggestions for Future Research
We can make several recommendations for researchers who want to study the clinical effectiveness of EMGB. First, the possible trends noted in surgical and nonsurgical knee conditions in this review should be challenged. Although the postoperative use of EMGB may indicate effectiveness in reducing pain and increasing quadriceps strength, the recommendation is cautious and tentative. With greater conviction, we can suggest that EMGB is ineffective for chronic knee conditions, such as patellofemoral pain syndrome and osteoarthritis. However, the basis for these recommendations is 8 trials, which is clearly insufficient for a confident conclusion.
Contemporary approaches to rehabilitation should be attempted in future research. The included studies used primarily straight-leg raises and quadriceps setting. These exercises are noninvasive and can be performed by most patients, but a criterion-based progression of functional exercises may better reflect current clinical practice.
Methodologic bias is a concern that must be addressed by future authors. Nearly all investigators failed to conceal patient allocation; analyze intention to treat; and blind patients, therapists, or assessors. Using the Consolidated Standards of Reporting Trials (CONSORT) guidelines to plan future trials may reduce many of these shortcomings.
CONCLUSIONS
This review yielded preliminary trends in the effectiveness of EMGB and quadriceps exercise. Potential improvements in knee extensor torque and functional outcome with EMGB were demonstrated in participants with surgical knee conditions, such as ACL reconstructions and meniscectomies, albeit from a limited data pool. However, participants with chronic knee conditions, such as patellofemoral pain and osteoarthritis, did not appear to benefit from EMGB. These recommendations are tentative and warrant further examination of the topic.
REFERENCE
- 1.Akima H, Hioki M, Furukawa T. Effect of arthroscopic partial meniscectomy on the function of quadriceps femoris. Knee Surg Sports Traumatol Arthrosc. 2008;16(11):1017–1025. doi: 10.1007/s00167-008-0601-3. [DOI] [PubMed] [Google Scholar]
- 2.Brandt KD, Heilman DK, Slemenda C. A comparison of lower extremity muscle strength, obesity, and depression scores in elderly subjects with knee pain with and without radiographic evidence of knee osteoarthritis. J Rheumatol. 2000;27(8):1937–1946. et al. [PubMed] [Google Scholar]
- 3.Callaghan MJ, Oldham JA. Quadriceps atrophy: to what extent does it exist in patellofemoral pain syndrome? Br J Sports Med. 2004;38(3):295–299. doi: 10.1136/bjsm.2002.002964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gerber C, Hoppeler H, Claassen H, Robotti G, Zehnder R, Jakob RP. The lower-extremity musculature in chronic symptomatic instability of the anterior cruciate ligament. J Bone Joint Surg Am. 1985;67(7):1034–1043. [PubMed] [Google Scholar]
- 5.Jones SW, Hill RJ, Krasney PA, O'Conner B, Peirce N, Greenhaff PL. Disuse atrophy and exercise rehabilitation in humans profoundly affects the expression of genes associated with the regulation of skeletal muscle mass. FASEB J. 2004;18(9):1025–1027. doi: 10.1096/fj.03-1228fje. [DOI] [PubMed] [Google Scholar]
- 6.Hopkins JT, Ingersoll CD, Krause BA, Edwards JE, Cordova ML. Effect of knee joint effusion on quadriceps and soleus motoneuron pool excitability. Med Sci Sports Exerc. 2001;33(1):123–126. doi: 10.1097/00005768-200101000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Piva SR, Fitzgerald GK, Irrgang JJ. Associates of physical function and pain in patients with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2009;90(2):285–295. doi: 10.1016/j.apmr.2008.08.214. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ericsson YB, Roos EM, Dahlberg L. Muscle strength, functional perfor- mance, and self-reported outcomes four years after arthroscopic partial meniscectomy in middle-aged patients. Arthritis Rheum. 2006;55(6):946–952. doi: 10.1002/art.22346. [DOI] [PubMed] [Google Scholar]
- 9.Kannus P, Natri A, Niittymaki S, Jarvinen M. Effect of intraarticular glycosaminoglycan polysulfate treatment on patellofemoral pain syndrome: a prospective, randomized double-blind trial comparing glycosaminoglycan polysulfate with placebo and quadriceps muscle exercises. Arthritis Rheum. 1992;35(9):1053–1061. doi: 10.1002/art.1780350910. [DOI] [PubMed] [Google Scholar]
- 10.Liikavainio T, Lyytinen T, Tyrväinen E, Sipilä S, Arokoski JP. Physical function and properties of quadriceps femoris muscle in men with knee osteoarthritis. Arch Phys Med Rehabil. 2008;89(11):2185–2194. doi: 10.1016/j.apmr.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Natri A, Kannus P, Jarvinen M. Which factors predict the long-term outcome in chronic patellofemoral pain syndrome? A 7-yr prospective follow-up study. Med Sci Sports Exerc. 1998;30(11):1572–1577. doi: 10.1097/00005768-199811000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A. Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29(7):400–412. doi: 10.2519/jospt.1999.29.7.400. [DOI] [PubMed] [Google Scholar]
- 13.Ericsson YB, Dahlberg LE, Roos EM. Effects of functional exercise training on performance and muscle strength after meniscectomy: a randomized trial. Scand J Med Sci Sports. 2009;19(2):156–165. doi: 10.1111/j.1600-0838.2008.00794.x. [DOI] [PubMed] [Google Scholar]
- 14.Jenkinson CM, Doherty M, Avery AJ. Effects of dietary intervention and quadriceps strengthening exercises on pain and function in over-weight people with knee pain: randomised controlled trial. BMJ. 2009;339:b3170. doi: 10.1136/bmj.b3170. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Linschoten R, van Middelkoop M, Berger MY. Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open label randomised controlled trial. BMJ. 2009;339:b4074. doi: 10.1136/bmj.b4074. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Enck P, Van der Voort IR, Klosterhalfen S. Biofeedback therapy in fecal incontinence and constipation. Neurogastroenterol Motil. 2009;21(11):1133–1141. doi: 10.1111/j.1365-2982.2009.01345.x. [DOI] [PubMed] [Google Scholar]
- 17.Nestoriuc Y, Rief W, Martin A. Meta-analysis of biofeedback for tension-type headache: efficacy, specificity, and treatment moderators. J Consult Clin Psychol. 2008;76(3):379–396. doi: 10.1037/0022-006X.76.3.379. [DOI] [PubMed] [Google Scholar]
- 18.Cardoso JR, Teixeira EC, Moreira MD, Favero FM, Fontes SV, Bulle de Oliveira AS. Effects of exercises on Bell's palsy: systematic review of randomized controlled trials. Otol Neurotol. 2008;29(4):557–560. doi: 10.1097/MAO.0b013e31816c7bf1. [DOI] [PubMed] [Google Scholar]
- 19.Woodford H, Price C. EMG biofeedback for the recovery of motor function after stroke. Cochrane Database Syst Rev. 2007;(2):CD004585. doi: 10.1002/14651858.CD004585.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maryn Y, De Bodt M, Van Cauwenberge P. Effects of biofeedback in phonatory disorders and phonatory performance: a systematic literature review. Appl Psychophysiol Biofeedback. 2006;31(1):65–83. doi: 10.1007/s10484-006-9005-7. [DOI] [PubMed] [Google Scholar]
- 21.Crider A, Glaros AG, Gevirtz RN. Efficacy of biofeedback-based treatments for temporomandibular disorders. Appl Psychophysiol Biofeedback. 2005;30(4):333–345. doi: 10.1007/s10484-005-8420-5. [DOI] [PubMed] [Google Scholar]
- 22.Torry MR, Decker MJ, Viola RW, O'Connor DD, Steadman JR. Intraarticular knee joint effusion induces quadriceps avoidance gait patterns. Clin Biomech (Bristol, Avon) 2000;15(3):147–159. doi: 10.1016/s0268-0033(99)00083-2. [DOI] [PubMed] [Google Scholar]
- 23.Van Tiggelen D, Cowan S, Coorevits P, Duvigneaud N, Witvrouw E. Delayed vastus medialis obliquus to vastus lateralis onset timing contributes to the development of patellofemoral pain in previously healthy men: a prospective study. Am J Sports Med. 2009;37(6):1099–1105. doi: 10.1177/0363546508331135. [DOI] [PubMed] [Google Scholar]
- 24.Haynes RB, Wilczynski N, McKibbon KA, Walker CJ, Sinclair JC. Developing optimal search strategies for detecting clinically sound studies in MEDLINE. J Am Med Inform Assoc. 1994;1(6):447–458. doi: 10.1136/jamia.1994.95153434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 26.Sherrington C, Herbert RD, Maher CG, Moseley AM. PEDro. A database of randomized trials and systematic reviews in physiotherapy. Man Ther. 2000;5(4):223–226. doi: 10.1054/math.2000.0372. [DOI] [PubMed] [Google Scholar]
- 27.Foley NC, Bhogal SK, Teasell RW, Bureau Y, Speechley MR. Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys Ther. 2006;86(6):817–824. [PubMed] [Google Scholar]
- 28.Bent NP, Wright CC, Rushton AB, Batt ME. Selecting outcome measures in sports medicine: a guide for practitioners using the example of anterior cruciate ligament rehabilitation. Br J Sports Med. 2009;43(13):1006–1012. doi: 10.1136/bjsm.2009.057356. [DOI] [PubMed] [Google Scholar]
- 29.Higgins JPT, Green S. London, England: The Cochrane Collaboration; 2009. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.2. [Google Scholar]
- 30.Durmuş D, Alayli G, Cantürk F. [Diz osteoartritli hastalarda biofeedback yardimli izometrik egzersiz ve elektrik stimulasyon programinin agri, anksiyete ve depresyon uzerine etkisi.] Fizik Tedavi Rehabilitasyon Dergisi. 2005;51(4):142–145. [Google Scholar]
- 31.Hernandez Mendo A. El biofeedback electromiografico en la rehabilitacion de lesiones deportivas de la rodilla. Lecturas: Educacion Fisica y Deportes. 1999;4(15) http://www.efdeportes.com/efd15/lesion.htm. Accessed March 14, 2011. [Google Scholar]
- 32.Ma L, Shen B. The effects of EMG biofeedback training on some muscular functions after knee injuries. Chin J Sport Med. 1990;9(4):216–220. [Google Scholar]
- 33.Sprenger CK, Carlson K, Wessman HC. Application of electromyographic biofeedback following medial meniscectomy: a clinical report. Phys Ther. 1979;59(2):167–169. doi: 10.1093/ptj/59.2.167. [DOI] [PubMed] [Google Scholar]
- 34.Wise HH, Fiebert I, Kates JL. EMG biofeedback as treatment for patellofemoral pain syndrome. J Orthop Sports Phys Ther. 1984;6(2):95–103. doi: 10.2519/jospt.1984.6.2.95. [DOI] [PubMed] [Google Scholar]
- 35.Draper V, Lyle L, Seymour T. EMG biofeedback versus electrical stimulation in the recovery of quadriceps surface EMG. Clin Kinesiol. 1997;51(2):28–32. [Google Scholar]
- 36.Krebs DE. Clinical electromyographic feedback following meniscectomy: a multiple regression experimental analysis. Phys Ther. 1981;61(7):1017–1021. doi: 10.1093/ptj/61.7.1017. [DOI] [PubMed] [Google Scholar]
- 37.Ng GY, Zhang AQ, Li CK. Biofeedback exercise improved the EMG activity ratio of the medial and lateral vasti muscles in subjects with patellofemoral pain syndrome. J Electromyogr Kinesiol. 2008;18(1):128–133. doi: 10.1016/j.jelekin.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 38.Nitz JC, Luparia L. The use of EMG biofeedback in quadriceps strengthening exercise for rheumatoid arthritis patients: a clinical trial. Aust J Physiother. 1983;29(4):127–132. doi: 10.1016/S0004-9514(14)60669-3. [DOI] [PubMed] [Google Scholar]
- 39.Bennell K, Duncan M, Cowan S, McConnell J, Hodges P, Crossley K. Effects of vastus medialis oblique retraining versus general quadriceps strengthening on vasti onset. Med Sci Sports Exerc. 2010;42(5):856–864. doi: 10.1249/MSS.0b013e3181c12771. [DOI] [PubMed] [Google Scholar]
- 40.Cowan SM, Bennell KL, Crossley KM, Hodges PW, McConnell J. Physical therapy alters recruitment of the vasti in patellofemoral pain syndrome. Med Sci Sports Exerc. 2002;34(12):1879–1885. doi: 10.1097/00005768-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Crossley K, Bennell K, Green S, Cowan S, McConnell J. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002;30(6):857–865. doi: 10.1177/03635465020300061701. [DOI] [PubMed] [Google Scholar]
- 42.Crossley KM, Cowan SM, McConnell J, Bennell KL. Physical therapy improves knee flexion during stair ambulation in patellofemoral pain. Med Sci Sports Exerc. 2005;37(2):176–183. doi: 10.1249/01.mss.0000152676.13197.49. [DOI] [PubMed] [Google Scholar]
- 43.Harrison E, Sheppard M, McQuarrie A. A randomised controlled trial of physical therapy treatment programs in patellofemoral pain syndrome. Physiother Can. 1999;51(2):93–106. [Google Scholar]
- 44.Syme G, Rowe P, Martin D, Daly G. Disability in patients with chronic patellofemoral pain syndrome: a randomised controlled trial of VMO selective training versus general quadriceps strengthening. Man Ther. 2009;14(3):252–263. doi: 10.1016/j.math.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 45.Ingersoll CD, Knight KL. Patellar location changes following EMG biofeedback or progressive resistive exercises. Med Sci Sports Exerc. 1991;23(10):1122–1127. [PubMed] [Google Scholar]
- 46.LeVeau BF, Rogers C. Selective training of the vastus medialis muscle using EMG biofeedback. Phys Ther. 1980;60(11):1410–1415. doi: 10.1093/ptj/60.11.1410. [DOI] [PubMed] [Google Scholar]
- 47.Lucca JA, Recchiuti SJ. Effect of electromyographic biofeedback on an isometric strengthening program. Phys Ther. 1983;63(2):200–203. doi: 10.1093/ptj/63.2.200. [DOI] [PubMed] [Google Scholar]
- 48.Qi Z, Ng G. EMG analysis of vastus medialis obliquus/vastus lateralis activities in subjects with patellofemoral pain syndrome before and after a home exercise program. J Phys Ther Sci. 2007;19(2):131–137. [Google Scholar]
- 49.Yip SL, Ng GY. Biofeedback supplementation to physiotherapy exercise programme for rehabilitation of patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. 2006;20(12):1050–1057. doi: 10.1177/0269215506071259. [DOI] [PubMed] [Google Scholar]
- 50.Draper V. Electromyographic biofeedback and recovery of quadriceps femoris muscle function following anterior cruciate ligament reconstruction. Phys Ther. 1990;70(1):11–17. doi: 10.1093/ptj/70.1.11. [DOI] [PubMed] [Google Scholar]
- 51.Draper V, Ballard L. Electrical stimulation versus electromyographic biofeedback in the recovery of quadriceps femoris muscle function following anterior cruciate ligament surgery. Phys Ther. 1991;71(6):455–461. doi: 10.1093/ptj/71.6.455. [DOI] [PubMed] [Google Scholar]
- 52.Durmus D, Alayli G, Canturk F. Effects of quadriceps electrical stimulation program on clinical parameters in the patients with knee osteoarthritis. Clin Rheumatol. 2007;26(5):674–678. doi: 10.1007/s10067-006-0358-3. [DOI] [PubMed] [Google Scholar]
- 53.Dursun N, Dursun E, Kilic Z. Electromyographic biofeedback– controlled exercise versus conservative care for patellofemoral pain syndrome. Arch Phys Med Rehabil. 2001;82(12):1692–1695. doi: 10.1053/apmr.2001.26253. [DOI] [PubMed] [Google Scholar]
- 54.Kirnap M, Calis M, Turgut AO, Halici M, Tuncel M. The efficacy of EMG-biofeedback training on quadriceps muscle strength in patients after arthroscopic meniscectomy. N Z Med J. 2005;118(1224):U1704. [PubMed] [Google Scholar]
- 55.Levitt R, Deisinger JA, Remondet Wall J, Ford L, Cassisi JE. EMG feedback– assisted postoperative rehabilitation of minor arthroscopic knee surgeries. J Sports Med Phys Fitness. 1995;35(3):218–223. [PubMed] [Google Scholar]
- 56.Yilmaz OO, Senocak O, Sahin E. Efficacy of EMG-biofeedback in knee osteoarthritis. Rheumatol Int. 2010;30(7):887–892. doi: 10.1007/s00296-009-1070-9. et al. [DOI] [PubMed] [Google Scholar]
- 57.Chmielewski TL, Jones D, Day T, Tillman SM, Lentz TA, George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther. 2008;38(12):746–753. doi: 10.2519/jospt.2008.2887. [DOI] [PubMed] [Google Scholar]
- 58.Fahrer H, Rentsch HU, Gerber NJ, Beyeler C, Hess CW, Grunig B. Knee effusion and reflex inhibition of the quadriceps: a bar to effective retraining. J Bone Joint Surg Br. 1988;70(4):635–638. doi: 10.1302/0301-620X.70B4.3403614. [DOI] [PubMed] [Google Scholar]
- 59.Jensen K, Graf BK. The effects of knee effusion on quadriceps strength and knee intraarticular pressure. Arthroscopy. 1993;9(1):52–56. doi: 10.1016/s0749-8063(05)80343-3. [DOI] [PubMed] [Google Scholar]
- 60.Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45(1):87–97. doi: 10.4085/1062-6050-45.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lin YF, Lin JJ, Jan MH, Wei TC, Shih HY, Cheng CK. Role of the vastus medialis obliquus in repositioning the patella. Am J Sports Med. 2008;36(4):741–746. doi: 10.1177/0363546507312171. [DOI] [PubMed] [Google Scholar]
- 62.Peeler J, Anderson JE. Structural parameters of the vastus medialis muscle and its relationship to patellofemoral joint deterioration. Clin Anat. 2007;20(3):307–314. doi: 10.1002/ca.20375. [DOI] [PubMed] [Google Scholar]
- 63.Hubbard JK, Sampson HW, Elledge JR. The vastus medialis oblique muscle and its relationship to patellofemoral joint deterioration in human cadavers. J Orthop Sports Phys Ther. 1998;28(6):384–391. doi: 10.2519/jospt.1998.28.6.384. [DOI] [PubMed] [Google Scholar]
- 64.Chester R, Smith TO, Sweeting D, Dixon J, Wood S, Song F. The relative timing of VMO and VL in the aetiology of anterior knee pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2008;9:64. doi: 10.1186/1471-2474-9-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Heintjes E, Berger MY, Bierma-Zeinstra SM, Bernsen RM, Verhaar JA, Koes BW. Exercise therapy for patellofemoral pain syndrome. Cochrane Database Syst Rev. 2003;(4):CD003472. doi: 10.1002/14651858.CD003472. [DOI] [PubMed] [Google Scholar]
- 66.Smith TO, Bowyer D, Dixon J, Stephenson R, Chester R, Donell ST. Can vastus medialis oblique be preferentially activated? A systematic review of electromyographic studies. Physiother Theory Pract. 2009;25(2):69–98. doi: 10.1080/09593980802686953. [DOI] [PubMed] [Google Scholar]
- 67.Kettunen JA, Harilainen A, Sandelin J. Knee arthroscopy and exercise versus exercise only for chronic patellofemoral pain syndrome: a randomized controlled trial. BMC Med. 2007;5:38. doi: 10.1186/1741-7015-5-38. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Suter E, Herzog W, Bray RC. Quadriceps inhibition following arthros-copy in patients with anterior knee pain. Clin Biomech (Bristol, Avon) 1998;13(4–5):314–319. doi: 10.1016/s0268-0033(98)00098-9. [DOI] [PubMed] [Google Scholar]
- 69.Egger M, Ebrahim S, Smith GD. Where now for meta-analysis? Int J Epidemiol. 2002;31(1):1–5. doi: 10.1093/ije/31.1.1. [DOI] [PubMed] [Google Scholar]
- 70.Nuesch E, Trelle S, Reichenbach S. The effects of excluding patients from the analysis in randomised controlled trials: meta-epidemiological study. BMJ. 2009;339:b3244. doi: 10.1136/bmj.b3244. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tierney JF, Stewart LA. Investigating patient exclusion bias in meta-analysis. Int J Epidemiol. 2005;34(1):79–87. doi: 10.1093/ije/dyh300. [DOI] [PubMed] [Google Scholar]


