Abstract
Objective:
Despite recent increases in the volume of research in professional rugby union, there is little consensus on the epidemiology of injury in adolescent players. We undertook a systematic review to determine the incidence, severity, and nature of injury in adolescent rugby union players.
Data Sources:
In April 2009, we performed a computerized literature search on PubMed, Embase, and Cochrane Controlled Trials Register (via Ovid). Population-specific and patient-specific search terms were combined in the form of MEDLINE subject headings and key words (wound$ and injur$, rugby, adolescent$). These were supplemented with related-citation searches on PubMed and bibliographic tracking of primary and review articles.
Study Selection:
Prospective epidemiologic studies in adolescent rugby union players.
Data Synthesis:
A total of 15 studies were included, and the data were analyzed descriptively. Two independent reviewers extracted key study characteristics regarding the incidence, severity, and nature of injuries and the methodologic design.
Conclusions:
Wide variations existed in the injury definitions and data collection procedures. The incidence of injury necessitating medical attention varied with the definition, from 27.5 to 129.8 injuries per 1000 match hours. The incidence of time-loss injury (>7 days) ranged from 0.96 to 1.6 per 1000 playing hours and from 11.4/1000 match hours (>1 day) to 12–22/1000 match hours (missed games). The highest incidence of concussion was 3.3/1000 playing hours. No catastrophic injuries were reported. The head and neck, upper limb, and lower limb were all common sites of injury, and trends were noted toward greater time loss due to upper limb fractures or dislocations and knee ligament injuries. Increasing age, the early part of the playing season, and the tackle situation were most closely associated with injury. Future injury-surveillance studies in rugby union must follow consensus guidelines to facilitate interstudy comparisons and provide further clarification as to where injury- prevention strategies should be focused.
Keywords: injury incidence, injury surveillance, high school athletes
Key Points.
Injury definitions and data collection procedures varied across studies, making comparisons difficult.
The head and neck, upper limb, and lower limb were common sites of injury.
Factors associated most often with injury were increasing age, early playing season, and tackles.
Rugby union is one of the most popular team sports in the world. Figures from the International Rugby Board show that it is increasingly popular with teenagers, who represent 22% to 39% of registered players in the top 5 rugby-playing nations.1 Currently, almost half of officially registered rugby union players in the United States are teenagers.1 In recent years, surveys in the United Kingdom and the United States have shown an increase in the number of young people presenting to emergency departments with rugby-related injuries.2–5
Figure.
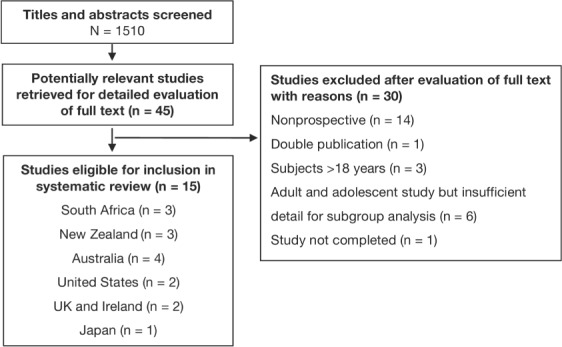
Identification and selection of studies (QUORUM).
Sports injuries can have significant effects on the health and well-being of young athletes. Minimizing their effects is best achieved by developing appropriate injury-prevention strategies based on well-defined epidemiologic studies, which accurately establish the extent of an injury problem and the true risks within a given sport.6,7 Since 1995, when rugby union became a professional sport, the number of injury-surveillance studies in adult players has increased. Injury rates8–11 are highest in professional players, ranging from 91 to 97.9 injuries/1000 match hours.8 In a large study9 of professional players in England, injury to the anterior cruciate ligament and hamstring muscles caused the greatest number of days absent from play. Further evidence indicates that tackles are the most dangerous facet of play in the professional game9,12–14 and carry the highest risk of head and spinal injury.15,16
Currently, the incidence, severity, and nature of injuries in adolescent rugby are unclear. It is difficult to directly extrapolate data from the professional game, given the differences in player physique, game speed, style of play, and rules. High-quality epidemiologic data are essential if we are to determine the levels of injury risk for the adolescent population and, if appropriate, where our future injury-prevention efforts should be focused.17 The aim of this systematic review was to determine the epidemiology of injuries in adolescent rugby players based on the current evidence. Our main objective was to determine the incidence, severity, and nature of injuries recorded in prospective epidemiologic studies of adolescent rugby players. We also considered key characteristics of methodologic design across the current evidence base.
METHODS
Identification and Selection of Studies
In April 2009, we undertook a computerized literature search of the following databases: MEDLINE (from 1966), Embase (from 1980), and Cochrane Controlled Trials Register (from 1982) using Ovid. Population-specific and patient-specific search terms were combined using Boolean operators, in the form of MEDLINE subject headings and key words (wound$ and injur$, rugby, adolescent$). Subject headings were exploded from the mapping display using Ovid to provide a broader and more comprehensive search. The search was further supplemented with 3 related-citation searches on PubMed,18 which retrieved a precalculated set of articles closely related to adolescent rugby injuries. Finally, bibliographic searching of all incoming full-text studies and key review articles (n = 27) was undertaken. Two authors (C.B., M.T.) conducted the searches and assessed trials for eligibility independently; any disparity on the final inclusion or exclusion decision was resolved by consensus discussion. No blinding of study author, place of publication, or results occurred. The following inclusion criteria were used:
Types of Studies.
Prospective cohort or randomized controlled design.
Types of Participants.
Rugby union players, aged 12–18 years, recruited from schools or clubs, with no restrictions placed on sex or level of play. Players defined as under age 19 and high school students were included. Studies involving a mixed sample of adult and adolescent players were also included, provided separate data could be extracted for the adolescent cohort.
Types of Outcome. Any data relating to the incidence, severity, and nature of injuries incurred during rugby union. Studies focusing on one particular injury type (eg, concussion) or risk factor for injury were also included. No restrictions were placed on the definitions of injury, methods of injury reporting and verification, or the duration of follow-up.
Data Extraction
Two authors (C.B., M.T.) independently extracted key study characteristics on the incidence, severity, and nature of injuries using a standardized form. Specific details on the data collection procedure, including the methods of injury reporting and verification and the definition of injury, were also extracted for qualitative discussion. Any disparity was resolved by consensus discussion between the authors or by consultation with the third author (S.O.). Where appropriate, additional figures were extracted for match injury (per 1000 match hours) and practice injury (per 1000 practice hours). Where possible, results were grouped and discussed according to injuries resulting in a player receiving medical attention (medical-attention injury) or injuries resulting in a player being unable to take full part in future rugby training or match play (time-loss injury).
RESULTS
After review of 45 full-text articles, we excluded 30 studies, leaving 15 eligible studies.13,19–32 In 2 cases,13,27 supplementary articles33,34 were accessed in order to extract the full details of the study methods. The QUORUM statement flow diagram, summarizing the process of study selection and the number of studies excluded at each stage, with explanations, is shown in the Figure. The main reasons for exclusion were nonprospective study design (n = 16), adult population (n = 3), and insufficient data on the adolescent cohort in cases of mixed adolescent and adult populations (n = 6). No studies were excluded based on language of publication.
Methodologic Design
The authors of most studies used a prospective cohort design; 2 groups used a randomized controlled design.27,28 All had at least 1-season follow-up, and 6 groups20–22,25,26,30 investigated only a single team. Participant dropout was clearly accounted for in just 3 studies,13,23,27 and ethical approval was confirmed in only 7.13,22,23,27–29,32 Ten groups20–23,25–29,32 consistently used a qualified medical practitioner to verify injuries, whereas others relied mainly on players or coaches to complete weekly questionnaires19,24,30 or telephone interviews.13 All reported on the anatomical location of injury, and almost all detailed the condition. The majority reported on the injuring event or mechanism,19,21,23–25,27,29,30,31 but few considered the time of injury21,25,29 or whether foul play was a factor.19,25,29–31 Although all authors provided a clear definition of injury, the definitions varied widely across investigations. None of the researchers fully defined or accounted for recurrent injury. A summary of study characteristics and results is provided in Table 1.
Table 1.
Study Characteristics and Results
| Reference No. | Participants | Injury Definition (Method of Injury Reporting) | Incidence of Medical-Attention Injury | Incidence of Time-Loss Injury | Concussion Incidence (Prevalence)a | Other Details of Injury Severity |
| 13 | Rugby clubs, New ZealandN = 356 (data extracted for 54 schoolboys, 23 schoolgirls), 1 season | Seek medical attention or miss at least 1 scheduled game or practice; injuries also graded as minor, moderate, or severe (telephone interview with player) | Boys: 6.2 (95% CI = 4.7, 8.1)/100 player games, 53.4/1000 game h; Girls: 4.7 (95% CI = 1.9, 9.3)/100 player games | NA | NA | |
| 19 | 121 High schools, United StatesAge = 16.5 ± 1.2 y, boys and girls, 2 seasons113641 AEs (81627 practice exposures, 32 014 match exposures) | An injury that resulted from participation in organized high school match or practice, necessitated medical attention from club physician or urgent care facility and resulted in restriction of high school player's regular school or rugby activities for 1 or more days beyond day of injury (medically confirmed in 5% of cases; remainder were reported by player or coach) | NA | >1 d:Overall, 5.2/1000 AEs; boys, 5.5/1000 AEs, 14.8/1000 match exposures,11.4/1000 match hb; girls:4.1/1000 AEs, 19.5/1000 match exposures, 15/1000 match hc | NA (15.8%) | 26.9% of injuries resulted in ≥21 d time loss. 11 career-ending injuries reported (n = 4 fractures, n = 2 dislocations, n = 2 nerve injuries, n = 1 cartilage, n = 1 unknown shoulder injury) |
| 20 | 1 school, Australia11–18 y, males18 seasons82 107 playing h | Injury necessitating attention at school's sports injury clinic; injuries classified as minor or severe based on clinical assessment; severe included most fractures and dislocations (medically confirmed) | 17.6/1000 playing h | NA | 0.19/1000 playing h (1.1%) | 8% of injuries classified as severe (1.4/1000 playing h); 86% of these were fractures; 65%, upper limb fractures; most clinically serious were 1 fractured skull (during tackle), 1 fracture-dislocation of cervical spine (during scrum); both resulted in full recovery; no patient with concussion needed admission to hospital |
| 21 | 1 school, New ZealandN = 442 male players (U19)1 season344 games6880 game h | Injury that forced player to leave field or complain after match; injuries also classified as minor (able to play in 7 d), moderate (unable to play for 1-3 wk), or severe (unable to play >3 wk) (medically confirmed) | 27.5 match injuries per 1000 match h | Missed games: 8.2 match injuries/1000 match h Missed 1-3 wk: 6.5/1000 match injuries/1000 h Missed >3 wk: 1.7 match injuries/1000 match h | 0.87/1000 match h (2.2% of all injuries) | 4% of injuries classified as severe (unable to play for >3 wk), of which 1 (anterior cruciate ligament rupture) may have been at risk for long-term sequelae |
| 22 | 2 high schools, JapanN = 327 15- to 16-y-old boys8 seasons | Atraumatic low back pain (unable to play ≥1 d) (medically confirmed) | NA | At least 1 d: 42% of players | NA | Low back pain prevalence in players with normal radiograph, 44%; ≥1 radiographic abnormality, 41.2%; spondylolysis, 72.5% (odds ratio, 3.36; 95% CI = 2.67, 4.22), P < .01 |
| 23 | 10 schools, New ZealandN = 123 boys, 17 ± 0.84 y1 seasonMean playing exposure = 55.9 ± 15.8 h | Any physical complaint caused by rugby during school training or matches; duration of absence due to injury was also reported and characterized according to severity: no absence, ≤1 wk, 8–21 d, >21 d (medically confirmed) | 129.8 match injuries/1000 h, 2.8/player season | ≤7 d: 5.38/1000 playing h 8–21 d: 3.78/1000 playing h >21 d: 1.16/1000 playing h (≈2.4%) 20.9% of injuries resulted in absences from ≥1 match or training session | 1.45/1000 playing h (2.9%) | 3 injuries (2.4%) ended sport participation (2 shoulder dislocations, 1 anterior cruciate ligament rupture); time frame not specified |
| 24 | 9 schools, ScotlandN = 1705 males, 11–19 y1 season1705 player seasons | An injury sustained on field during competitive match, practice game, or other training activity that prevented athlete from training or playing rugby from time of injury or from end of match or practice session in which injury occurred; severity classified by number of days missed: transient, <7 d; mild, 7–28 d; moderate, 29–84 d; severe, >84 d (player contact and medical records) | NA | Match or practice injury: 80.9 (CI = 68.0, 93.9)/1000 player seasons Match injury: 73.9 (CI = 61.5, 86.3)/1000 player seasons | 10.6/1000 player seasons (CI = 5.7, 15.4) (12.2%) | 9% of match injuries classified as severe (time loss >84 d) 2 players suffered recurrent concussion within 21 d No spinal injuries |
| 25 | 2 youth teams, EnglandN = 45 males, 16 to 18 y old2 seasons | Injury recorded if player needed attention on pitch (other than reassurance) or after completion of game or formal training session (medically confirmed) | 0.7 injuries/game = ≈35 injuries/1000 game h (note this does not take training exposure into consideration) | NA | NA (5%–10%) | |
| 26 | 1 school, United States high school–age males 3 seasons | Injuries resulting in time lost from games or practices; all fractures and all concussions were reported; concussions graded using the Cantu scale (grade 1, 2, 3)d (medically confirmed) | Time lost from practice and games: 1.5/1000 AEs; 46/100 player seasons (95% CI = 35.1, 56.9) | 3.8 (95% CI = 2.0, 5.7)/1000 AEs; 11.3/100 player seasons (95% CI = 5.9, 16.7) (24.6%) | Concussion accounted for 25.3% of all days lost from rugby (2 grade 2 concussions, 1 grade 3 concussion) | |
| 27 | Data extracted from cluster randomized controlled trials on U13 (≈4046 exposure h), under U15 (≈4624 exposure h), and U18 y (≈7514 exposure h) players, Australia, and from a supplementary article332 seasons | (1) Any injury necessitating on-field treatment or resulting in player being removed from field during rugby game. (2) An injury occurring in rugby game resulting in player missing game the next week (usually at least 7-d absence from competition) (medically confirmed) | Medical attention during game: U13, 43.3/1000 game h (95% CI = 37, 50); U15, 56.2/1000 game h (95% CI = 50, 64); U18, 63/1000 game h (95% CI = 57, 69) | Missed games: U13, 11.8/1000 game h (95% CI = 9, 15); U15, 22.3/1000 game h (95% CI = 18, 27); U18, 22.2/1000 game h (95% CI = 19, 26) | Missed games: incidence per 1000 person h of game timee; front row: U13, 1.2; U15, 2.2; U18, 1.3; back 5: U13, 1.4; U15, 2; U18, 0.8; halfbacks: U13, 1.8; U15, 1.7; U18, 3; inside backs:U13, 0; U15, 0; U18, 3; outside backs: U13, 2.4; U15, 1.1; U18, 3.3 | 1 Odontoid fracture without neurologic injury occurred in ruck, and player's season ended; 20% of concussions resulted in loss of consciousness, none >5 min; 6 players taken to hospital but none admittedf |
| 28 | Data extracted from randomized controlled trials of U15 players from 16 schools, AustraliaN = 294 U15A (first-string) schoolboys1 season1536 player exposures (1179 with headgear, 357 without) | A traumatic event that resulted in player missing game playing or training time (concussion only) (medically confirmed) | NA | NA | 5.76/1000 player exposures; 9 concussions (7 with headgear, 2 without) | 1 player with concussion needed brief hospitalization in emergency department |
| 29 | Squad, Western AustraliaN = 44 (U15 and U16 y; male)26 wk | Minor: able to return to play with no time loss; mild: missed 1 wk; moderate: missed 2 wk; severe, missed >2 wk (medically confirmed) | For injuries of all severity: 13.26/1000 playing h | NA | NA | 40% Received medical attention missed no games; 47% missed 1 game, 11% missed 2 games, 2% missed >2 games; 5 most severe injuries were sustained during tackle; all severe injuries occurred in wk 1 of season |
| 30 | 1 school, South AfricaN = 465 males, U10–U19 y1 season31 185 player h (6075 match h, 25110 training h) | Injury severe enough to prevent player from returning to rugby ≥7 d; injury also classified by absence of ≤7 d, 3 wk, or >3 wk (player questionnaire) | NA | >7 d: 2.5/1000 playing h, 8.4/1000 match h, 1.2/1000 training h | 0.55/1000 playing h (21.5%) | Incidence of injury necessitating expert medical attention: 0.5/1000 playing h, 2.1 match injury/1000 match h; 13.9% of all injuries resulted in absence >21 d; 1 concussion that ended player's rugby career, 1 neck injury with no neurologic damage; 54.5% of severe (>21-d absence) were upper limb fracture-dislocations |
| 31 | 26 schools, South Africa6 schools closely monitored by medical practitioners; 20 schools monitored by correspondence only1 season3350 matches50 250 match h | Severe enough to prevent player from returning to rugby for ≥7 d; all concussions had to be reported, regardless of whether player continued with play (medically confirmed in 6/26 schools) | NA | > 7 d: For all schools: 1.6/1000 playing h, 7/1000 match h; for closely monitored schools: 2.3/1000playing h, mail correspondence only: 1.36/1000 playing h | Average of 5.6 concussions/school/y in closely monitored schools, 1.3/school/y in mail correspondence only (12%) | 68% of fractures and 48% of concussions caused by tackles |
| 32 | 5 high schools, South AfricaN = 1147Schools A and B: grade 12 teams; school C: grades 8–12; schools D and E: grades 8 and 121 season in 3 schools2 seasons in 2 schools | Concussion defined as any alteration in neurologic status occurring as result of head-jarring trauma, with or without loss of consciousness. Patients followed up with neurocognitive testing (ImPACTg)if any (1) loss of consciousness or amnesia, (2) changes in mental and physical status implicating postconcussion symptoms (medically confirmed) | NA | NA | Players needing follow-up by school: A, 11%; B, 10%; C, 13%; D, 6%; E, 4%; concussion management strategies varied; schools A–C deemed to be more proactive | 8 players sustained ≥1 concussion during study |
Abbreviations: AE, athlete-exposure (1 athlete participating in 1 practice or match); CI, confidence interval; NA, data not available; U13, players younger than 13 y; U15, players younger than 15 y; U18, players younger than 18 years; U19, players younger than 19 y.
aAs a percentage of all injuries.
bApproximated value based on 70-min game.
cValues extracted from graph.
d Cantu RC. Guidelines for return to contact sport after cerebral concussion. Physician Sportsmed. 1986;14(10):75–83.
eConcussion definition based on Vienna consensus statement.35
fIncludes data from under-20-years age group.
gImPACT Applications, Inc, Pittsburgh, PA.
Medical-Attention Injury
Seven groups13,20,21,23,25,27,29 focused on injuries resulting in medical attention. However, the definition of medical attention varied. Injuries necessitating medical attention during matches or practice had an incidence of 13.329 to 17.620 per 1000 playing hours. Injuries necessitating on-field treatment or removal from the game were reported at rates of 27.521 to 6327 injuries per 1000 game hours. Similar figures of 3513 to 5325 medical- attention injuries per 1000 game hours were also estimated from other studies based on available data. Junge et al23 reported rates of 129.8/1000 match hours based on a very broad definition of injury as any physical complaints relating to rugby, which might explain the higher figures.
Time-Loss Injury
Injuries necessitating at least 1 day's absence from rugby had incidences of 11.4 injuries/1000 match hours.19 Other figures, based on medically confirmed missed-game injuries, were between 11.8 and 22.2/1000 playing hours27 (depending on player age) and up to 28.3 injuries/1000 match hours.23
The incidence of injuries resulting in absence for at least 7 days ranged from 1.631 to 2.530 injuries/1000 playing hours and from 731 to 8.430 injuries/1000 match hours. In 1 large study,24 injuries preventing a player from training or playing had an incidence of 80.9/1000 player seasons. However, no other details were given as to the duration of players' absences or their playing exposures per season.
Injury Severity
In approximately one-third of included studies, the time lost from competition and practice was systematically recorded. Injuries resulting in absences from play for more than 21 days were classified as severe19,21,23 and occurred at rates of 1.2/1000 playing hours23 to 1.7 match injuries/1000 match hours.21 In 2 other investigations,20,30 injury severity was based on the need for expert medical attention30 or clinical diagnosis,20 but the incidences were similar: 0.530 to 1.420/1000 playing hours and 2.1/1000 match hours.30
The body regions most at risk of severe injury were the shoulder and knee,19,21,23 and the most common injury types were fractures,19–21 ligament sprains, and joint dislocations.19–21,23 Other severe injuries were concussions (n = 2) and thigh hematomas (n = 2).21
Catastrophic Injuries
No study reported any catastrophic or nonfatal catastrophic injuries,17 but a small number of injuries had potentially catastrophic consequences. These were a fractured skull sustained during a tackle,20 a cervical spine fracture-dislocation incurred during scrummaging,20 and an odontoid fracture27 (no neurologic injury was sustained, but the patient was unable to return to rugby). Two groups reported that career-ending injuries affected 1.9%19 to 2.4%23 of players, and Nathan et al30 indicated that a concussion ended the player's rugby career.
Concussion
The incidence of concussion ranged from 0.1920 to 1.4523/1000 playing hours and from 3.826 to 5.728/1000 athlete-exposures (AEs). These figures are based on medical practitioners' examinations, yet few authors provided details of concussion definitions or diagnoses.
McIntosh et al27 reported on concussion incidence by both age and playing position, showing that inside backs younger than 18 years tended to have the highest rate of medical-attention concussions: 13/1000 game hours (95% confidence interval [CI] = 9.5, 16.4). Both inside and outside backs of the same age group were at most risk of missing games due to concussions (inside backs: 3/1000 game hours, 95% CI = 1.3, 4.7; outside backs: 3.3/1000 game hours, 95% CI = 1.6, 5.1). Recurrent concussion, which was reported by only 2 groups,24,32 affected 0.1% to 0.7% of players. Two of these cases24 occurred within 3 weeks of the initial injury, and 1 case resulted in retirement from sport.32
One group32 used neurocognitive testing36 to facilitate concussion reporting across 5 schools; however, results varied, with 4% to 14% of players affected. Inconsistent follow-up across schools might explain this variation. Interestingly, Roux et al31 noted that the number of concussions reported by schools with access to medical practitioners (5.6 per school per year) was 4 times higher than by schools self-reporting (ie, those without access to a medical practitioner).
Other Factors Related to Injury
Details on injury incidence and prevalence by age, phase of play, and body region are provided in Tables 2–4. Increasing age was clearly associated with a higher incidence of injury, and tackles were the most dangerous facet of play. Between 40%21 and 59.6%19 of all injuries were sustained in the tackle. Most tackle injuries were to the head or shoulders (63%)29 and accounted for approximately 70%19 of all severe injuries, 48%31 to 64.9%19 of all concussions, and 68% of fractures.31 In Table 4, studies were grouped according to injured body part to facilitate comparison. In general, injuries were evenly distributed among the head and neck, upper limb, and lower limb, with the trunk least often affected. Injury patterns have also been considered by sex,13,19 stage of season,21,24,25,29–31 illegal play,19,29,30 and radiographic abnormality.22
Table 2.
Injury Incidence by Age
| Age, ya | Nathan et al 199830 (per 1000 playing h) | Davidson 198720 (per 1000 player-seasons) | Jones et al 20013 (values extracted from graph) | Lee and Garraway 1996b (per 1000 player-seasons) | Durie and Munroe 2000c (per 1000 match h) | McIntosh et al 2009d (medical-attention or time-loss injury) |
| Under 19 | 7.7d | 25.6e | 2.5 | 230.8f | NA | NA |
| Under 18 | NA | 65.8 | 63/22.2 | |||
| Under 17 | NA | 25 | NA | |||
| Under 16 | 3.4 | 1.6 | 126.1 | 21.8 | NA | |
| Under 15 | 4.8 | 18.4 | 1.1 | 88.9 | 27.9 | 56.2/22.3 |
| Under 14 | 1.7 | 0.7 | 64.2 | 28.5 | NA | |
| Under 13 | 1.0 | 13.6 | NA | 46.4 | 18.5 | 43.3/11.8 |
| Under 12 | NA | NA | NA | 42.0 | NA | NA |
Abbreviation: NA, not available.
aTrend across age groups (χ82 = 55, P < .0001).
bDifferences across groups for both medical-attention (P = .003) and time-loss (P < .001) injuries.24
cSignificant linear increase in risk of injury from U13 to U18 (1st XV) (χ222 = 85.5, P < .0001).21
dParticipants were under age 17 through under age 19.27
e Participants were under age 16 through under age 19.
f Participants were under age 17 through under age 19.
Table 4.
Injury by Body Region as a Percentage of All Injuries
| |
Time Loss (>7 d) |
Medical-Attention Injury |
Unable to Finish Game or >1-d Time Loss |
||||||
| Body Region | Nathan et al 198330 | Roux et al 198731 | Davidson 198720 | Lewis and George 199625 | Durie and Munroe 200021,a | McManus and Cross 200429,b | Junge et al 200423 | Lee and Garraway 199624 | Collins et al 200819 |
| Head and neck | 37.9c | 29 | 36.6 | 15.3 | 15.3 | 28.5 | 15.9 | 20.3 | |
| Head | 3.8 | 20.2 | 9.1 | 21.7 | |||||
| Neck | 11.5 | 8.3 | 6.8 | ||||||
| Upper limbd | 29.1 | 20 | 27.5 | 38.4 | 33.1 | 26.2 | 32.3 | 35.2 | |
| Shoulder | 15.4 | 15.3 | 14.3 | 19.1 | 9.5 | 12.8 | |||
| Arm | 23e | 2.6 | 13.2e | 25.7e | |||||
| Hand and wrist | 15.2 | 11.9 | |||||||
| Trunk | 7.6f | 13g | 6.5 | 7.7 | 10.3 | 11.9 | 7.1 | 8.1 | |
| Lower limbh | 25.3f | 37i | 26.2 | 26.8i | 44.4 | 30.8i | 44.7 | 31.1 | |
| Hip and pelvis | 1.9 | 5 | |||||||
| Thigh | 11.5j | 15.9 | 10.7 | 8.8 | |||||
| Knee | 7.7 | 6.6 | 7.1 | 11.5 | 11.1 | ||||
| Lower leg and shin | 3.8 | 6.3 | 7.1 | 9.1 | |||||
| Ankle | 3.8 | 13.7k | 5.9 | 10.3k | 13.3 | ||||
aA total of 7.4% of injuries were unspecified.
bValues were extracted from graph.
cIncludes face.
dIncludes shoulder, arm, hand, and wrist unless otherwise stated.
eIncludes hand and wrist.
fUnclear whether hip and pelvis were grouped with lower limb.
gIncludes hip and pelvis.
hLower limb includes hip, pelvis, thigh, knee, lower leg and shin, ankle, and foot unless otherwise stated.
iDoes not include hip and pelvis.
jQuadriceps muscles only.
kIncludes foot.
Table 3.
Injury by Phase of Play as a Percentage of All Injuries
| Phase of Play | Nathan et al 198330 | Roux et al 198731 | Lee and Garraway 199624 | Lewis and George 199625,a | Bird et al 199813 | Durie and Munroe 200021 | McManus and Cross 200429,b | Junge et al 200423 | Collins et al 200819 | McIntosh et al 200927,b |
| Tackling | 22 | 25 | 40 | 19 | 19 | 18.5 | 52.3 | NA | 28.8 | 25/30/32 |
| Being tackled | 25 | 30 | 24 | 23 | 22 | 22 | NA | NA | 30.8 | 25/23/25 |
| Scrum | 18 | 8 | 2 | 4 | NA | 13.7 | 5.9 | NA | NA | 10/4/3 |
| Ruck | 6 | 18 | 13 | 26.9 | 26.9 | 31.5 | 4.7 | NA | 14 | NA |
| Maul | NA | NA | 2 | NA | NA | NA | 9.5 | NA | NA | NA |
| Line out | 4 | 1 | 1.6 | NA | NA | 8.3 | 1.2 | NA | NA | NA |
| Open play | 11 | 8 | 9.5 | 11 | NA | 5.9 | 13 | NA | 9.9 | NA |
| Other | 6 | 7 | 8.8 | NA | NA | NA | 15.5 | NA | NA | NA |
| Foul play | 8 | 4 | NA | NA | NA | NA | 1.2 | NA | 4.9 | NA |
| Contact/noncontact | NA | NA | NA | NA | NA | NA | NA 66.8/33.2 | NA | NA |
Abbreviation: NA, not available.
aValues extracted from graphs.
bHead, face, and neck injury for under age 18 players only.
Few studies involved female athletes. Bird et al13 reported a lower incidence of injury (4.7/100 game hours) in school-age girls than in school-age boys (6.2/100 game hours). In contrast, Collins et al19 described higher injury rates per 1000 match exposures in girls (risk ratio [RR] = 1.3, 95% CI = 1.0, 1.7). Boys had higher injury rates based on total AEs (RR = 1.3, 95% CI = 1.1, 1.7) and time-loss injuries lasting more than 10 days (RR = 1.5, 95% CI = 1.1, 2), and all reported career-ending injuries were in male players.19
Six groups21,24,25,29–31 focused on the stage of season at which injuries occurred, with all reporting a higher incidence in the early stages. Interestingly, 2 sets of authors30,31 found that incidences peaked again immediately after a midseason break. Two groups21,29 included a statistical analysis and showed decreases in injury rate (χ221 = 43.39, P < .0001)21 and injury severity (χ2 = 36.51, P < .001; degrees of freedom not reported)29 over the course of the season.
Illegal play was associated with 1.2%29 to 8%30 of injuries, with high and late tackles noted as the most common type in one study.30 In particular, foul play increased the risk of severe injury and was related to 42% of concussions and a large number of fractures (12.5%) and dislocations (12.5%).19
As part of a preparticipation sport screening, Iwamoto et al22 found that 243/327 players had at least 1 radiographic abnormality (eg, spinal instability, Schmorl node, balloon disc, spina bifida), but only spondylolysis was associated with a higher incidence of low back pain (odds ratio = 3.36, 95% CI = 2.7, 4.2).
DISCUSSION
Despite recent increases in the volume of research on professional rugby union players, little consensus exists as to the epidemiology of injuries in the adolescent playing population. We undertook a systematic review to determine injury patterns in adolescent rugby union players. A total of 15 studies involving players from 5 continents were included. Wide variations in study methods restricted comparisons among investigations.
Injury Definition
One of the primary differences across studies was the tendency to report on either medical-attention or time-loss injuries. It would be erroneous to use these definitions interchangeably. In some cases, medical-attention injury referred to “any physical complaint resulting from rugby,”23 which starkly contrasts with other, less inclusive definitions such as “absence from play for at least 1 week.”31 Although a definition involving medical attention captures a large number of “injuries,” some of these data may be of limited reliability and clinical interest.37 In one case,23 79.1% of medical-attention injuries did not result in absence from play, and the use of time-loss definitions seemed to provide a more direct indication of injury morbidity.
Injury Severity
It is interesting that most of the injuries causing time loss of more than 21 days were caused by upper limb fractures or dislocations or knee ligament injuries.19–21,23,30 This pattern certainly merits further research. Unfortunately, the current evidence base does not include a discrete measure of the number of days lost for each injury beyond 21 days. Such data could provide further quantification as to which injury has the greatest effect in terms of time and cost; however, the challenges of such rigorous follow-up in an amateur sporting environment are acknowledged.33
An estimated 8% of adolescents drop out of sport activities each year because of injury.38 A small number of career-ending injuries were reported in the current review. A “career” may be more difficult to define in an amateur athlete, and these data alone may offer little in describing the long-term implications. By contrast, the consequences of a catastrophic sport injury are widespread and devastating. No catastrophic injuries were reported in the current review, but we noted small numbers of potentially catastrophic events. This finding provides further clarification of the importance of having high-quality acute management strategies and emergency care available for adolescent athletes.
Concussion
Until recently, no universal agreement existed on the standard definition or nature of sport concussion,35,39–40 and few evidence-based guidelines for return to sport were available.41 These facts may be reflected in the current review, and because few authors provided details as to how concussion was diagnosed, it is difficult to determine the accuracy of the reporting. Underreporting of concussion seemed to occur in 2 studies31,32 and was most likely in schools using less proactive data collection procedures. Underreporting has been identified in other adolescent contact sports42 and even remains a concern in international rugby union.8,43
Also of concern was that recurrent concussions were reported,24,32 some within a 3-week period.24 International guidelines suggest that premature return to competition after concussion seems to carry a higher risk of delayed-onset symptoms in children and adolescents.39 Previously, return to play after concussion followed a mandatory 3-week rule, which prevented players from returning to competition before this time.39 Recently, a shift has occurred toward a more individualized approach to diagnosis and return to play after concussion, which sometimes incorporates computerized neurocognitive testing.39 The results of one study32 clarified that although neurocognitive testing may be of benefit, such testing must be accompanied by a pro-active approach to injury management. Unfortunately, this may be particularly challenging in youth rugby, given the inherent dearth of qualified medical staff and the young players' limited knowledge of concussion guidelines.44
Comparison With Adult Rugby Union Players
Three of the eligible studies13,24,25 in this review also included a cohort of amateur adult rugby players; in all cases, the adults had consistently higher injury rates than did the adolescents. Similar trends seem to exist in the data from professional athletes. Epidemiologic studies of professional players using a “missed-match” definition of injury yielded injury rates between 43.2 (95% CI = 34.9, 53.6)43 and 7412 injuries/1000 player- hours. By comparison, McIntosh et al27 used the same definition for injury and described lower rates in adolescent players of 11.8 to 22.2/1000 playing hours. Similarly, the risk of severe injury is greater in the professional game. In a study43 defining severe as an absence from rugby for more than 28 days, incidences of 15.1 severe injuries/1000 match hours (95% CI = 10.5, 21.7) have been recorded in professional players. We found that injuries necessitating 21 days of time loss occurred at a rate of just 1.1623 to 1.721/1000 playing hours.
Comparison With Other Adolescent Sports
One of the included studies19 used data collection methods that closely model those of the National Collegiate Athletic Association Injury Surveillance System,45 and therefore direct comparison with injury-surveillance studies undertaken in other youth sports in the United States is possible.46–48 Injury incidences in high school basketball (1.94/1000 AEs),46 soccer (2.4/1000 AEs),48 and football (gridiron, 3.5/1000 AEs)47 were all lower than those reported by Collins et al19 (5.2/1000 AEs). Despite using a slightly different definition of time loss as more than 48 hours, studies of high school lacrosse (2.89/1000 playing hours)49 and youth soccer (11.2/1000 match hours)50 players also showed lower injury rates than did rugby players.
It is also useful to consider the risk of severe injuries across adolescent sports. In one of the included studies,23 compared with age-matched soccer players, rugby players sustained more fractures, dislocations, and concussions (P < .05), injuries resulting in 8- to 21-day absences (P < .05), and career-ending injuries (n = 3 in rugby, n = 0 in soccer). However, with the exception of Collins et al,19 the prevalence of severe injuries in adolescent rugby players in the current evidence base21,24,29,30 was lower than or comparable with data from high school football (8.6%47 to 11.2%51), soccer (10.4%),51 and wrestling (14.8%)51 athletes.
Other Factors Related to Injury
In conjunction with evidence from other adolescent sports,50,52 we found a clear trend of increased injury incidence with age. Perhaps the most likely reason for this is the greater strength and power that older players develop, contributing to a faster game tempo and, ultimately, harder collisions. As in the professional game,9,14 contact was the most dangerous facet of play. In the professional game, high-speed and high-impact tackles carry a greater propensity for injury, particularly collision-type tackles with head-to-head or neck contact.14,53 Future researchers should ascertain whether these risks are equivalent in adolescent rugby players. Specifically, we should consider the influences of mismatches in player physiques and strengths at certain ages and whether certain types of tackles are more prevalent in the adolescent game.
Similar to evidence from other adolescent sports,50 the incidence of injury was higher at the start of each season. This may be attributed to early-season deconditioning and merits further investigation. Studies of adult rugby players54 and other physically active populations55,56 have highlighted poor fitness levels as a risk factor for injury; structured preseason training regimens have prevented lower limb injuries in other adolescent athletes.57
Preseason physical screening assessments were undertaken in a small number of included studies13,22–24,29; however, only 1 group22 considered the results in relation to the injury patterns reported. Consequently, few intrinsic risk factors for injury are known for adolescent rugby players. As was noted in adolescent soccer players,58 Iwamoto et al22 found that radiologic evidence of lumbar spondylolysis was commonly associated with back pain in adolescent rugby players. Yet because they22 failed to provide discrete data for the duration of time loss beyond 1 day, it is difficult to ascertain whether radiographs are an ethical and cost-effective preseason screening tool.
Future Study
Our primary objective was to provide an indication of the incidence, severity, and nature of injuries sustained by adolescent rugby players, but it was difficult to gain a consensus in some areas. The primary reasons for this difficulty were the different methods of data collection and inconsistent definitions of definition of injury. Recently, the International Rugby Board produced consensus guidelines59 for epidemiologic studies in rugby. This consensus provides guidance on study design and data collection procedures and, most importantly, a standardized definition of injury, specifically for rugby union. Given the current problems associated with comparing studies of adolescent rugby union players, it is essential that authors of future injury-surveillance studies follow these recommendations.
It is also important to recognize that potentially important injury trends or inciting events were not taken into account in many studies. Similarly, many authors overlooked injury severity, when the gold standard should include medical verification of injury and a discrete measure of the associated time loss.59 Collating this level of detail in future research will help to clarify the true morbidity and effects of adolescent rugby injury and will streamline decisions as to where injury-prevention strategies are best focused.
CONCLUSIONS
Injury definitions differed across the included studies, which made comparisons challenging. The incidence of time-loss injury in adolescent rugby union players was lower than in adult professionals but higher than in adolescent athletes in other sports. The head and neck, upper limb, and lower limb were common sites of injury; greater time loss seemed to be associated with upper limb fractures and dislocations and knee ligament injuries. Increasing age, the early part of the playing season, and the tackle situation were closely linked with injury.
Future investigators pursuing injury-surveillance studies in rugby union must follow consensus guidelines provided by the International Rugby Board. This will facilitate comparisons among studies and provide further clarification as to where injury-prevention strategies should be focused.
REFERENCES
- 1.International Rugby Board. USA unions. http://www.irb.com/unions/union=11000012/index.html. Accessed August 26, 2009.
- 2.Abernethy L, MacAuley D. Impact of school sports injury. Br J Sports Med. 2003;37(4):354–355. doi: 10.1136/bjsm.37.4.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones SJ, Lyons RA, Sibert J, Evans R, Palmer SR. Changes in sports injuries to children between 1983 and 1998: comparison of case series. J Public Health Med. 2001;23(4):268–271. doi: 10.1093/pubmed/23.4.268. [DOI] [PubMed] [Google Scholar]
- 4.O'Rourke KP, Quinn F, Mun S. A comparison of paediatric soccer, Gaelic football and rugby injuries presenting to an emergency department in Ireland. Injury. 2007;38(1):104–111. doi: 10.1016/j.injury.2006.06.010. et al. [DOI] [PubMed] [Google Scholar]
- 5.Yard EE, Comstock RD. Injuries sustained by rugby players presenting to United States emergency departments, 1978 through 2004. J Athl Train. 2006;41(3):325–331. [PMC free article] [PubMed] [Google Scholar]
- 6.Van Mechelen W, Hlobil H, Kemper HCG. Incidence, severity, aetiology and prevention of sports injuries: a review of concepts. Sports Med. 1992;14(2):82–99. doi: 10.2165/00007256-199214020-00002. [DOI] [PubMed] [Google Scholar]
- 7.Brooks JH, Fuller CW. The influence of methodological issues on the results and conclusions from epidemiological studies of sports injuries: illustrative examples. Sports Med. 2006;36(6):459–472. doi: 10.2165/00007256-200636060-00001. [DOI] [PubMed] [Google Scholar]
- 8.Best JP, McIntosh AS, Savage TN. Rugby World Cup 2003 injury surveil-lance project. Br J Sports Med. 2005;39(11):812–817. doi: 10.1136/bjsm.2004.016402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brooks JHM, Fuller CW, Kemp SPT, Reddin DB. Epidemiology of injuries in English professional rugby union, part 1: match injuries. Br J Sports Med. 2005;39(10):757–766. doi: 10.1136/bjsm.2005.018135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brooks JHM, Fuller CW, Kemp SPT, Reddin DB. Epidemiology of injuries in English professional rugby union, part 2: training injuries. Br J Sports Med. 2005;39(10):767–775. doi: 10.1136/bjsm.2005.018408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dallalana RJ, Brooks JHM, Kemp SPT, Williams AM. The epidemiology of knee injuries in English professional rugby union. Am J Sports Med. 2007;35(5):818–830. doi: 10.1177/0363546506296738. [DOI] [PubMed] [Google Scholar]
- 12.Bathgate A, Best JP, Craig G, Jamieson M. A prospective study of injuries to elite Australian rugby union players. Br J Sports Med. 2002;36(4):265–269. doi: 10.1136/bjsm.36.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bird YN, Waller AE, Marshall SW, Alsop JC, Chalmers DJ, Gerrard DF. The New Zealand Rugby Injury and Performance Project, V: epidemiology of a season of rugby injury. Br J Sports Med. 1998;32(4):319–325. doi: 10.1136/bjsm.32.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fuller CW, Brooks JH, Cancea RJ, Hall J, Kemp SP. Contact events in rugby union and their propensity to cause injury. Br J Sports Med. 2007;41(12):862–867. doi: 10.1136/bjsm.2007.037499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haylen PT. Spinal injuries in rugby union, 1970– 2003: lessons and responsibilities. Med J Aust. 2004;181(1):48–50. doi: 10.5694/j.1326-5377.2004.tb06161.x. [DOI] [PubMed] [Google Scholar]
- 16.Shelly MJ, Butler JS, Timlin M. Spinal injuries in Irish rugby: a ten-year review. J Bone Joint Surg Br. 2006;88(6):771–775. doi: 10.1302/0301-620X.88B6.17388. et al. [DOI] [PubMed] [Google Scholar]
- 17.Fuller CW. Managing the risk of injury in sport. Clin J Sport Med. 2007;17(3):182–187. doi: 10.1097/JSM.0b013e31805930b0. [DOI] [PubMed] [Google Scholar]
- 18.National Center for Biotechnology Information, U.S. National Library of Medicine. Home page. http://www.ncbi.nlm.nih.gov/pubmed. Accessed April 2009.
- 19.Collins CL, Micheli LJ, Yard EE, Comstock RD. Injuries sustained by high school rugby players in the United States, 2005– 2006. Arch Pediatr Adolesc Med. 2008;162(1):49–54. doi: 10.1001/archpediatrics.2007.1. [DOI] [PubMed] [Google Scholar]
- 20.Davidson RM. Schoolboy rugby injuries, 1969–1986. Med J Aust. 1987;147(3):119–120. doi: 10.5694/j.1326-5377.1987.tb133299.x. [DOI] [PubMed] [Google Scholar]
- 21.Durie RM, Munroe AD. A prospective survey of injuries in a New Zealand schoolboy population. N Z J Sports Med. 2000;28(4):84–90. [Google Scholar]
- 22.Iwamoto J, Abe H, Tsukimura Y, Wakano K. Relationship between radiological abnormalities of lumbar spine and incidence of low back pain in high school rugby players: a prospective study. Scand J Med Sci Sports. 2005;15(3):163–168. doi: 10.1111/j.1600-0838.2004.00414.x. [DOI] [PubMed] [Google Scholar]
- 23.Junge A, Cheung K, Edwards T, Dvorak J. Injuries in youth amateur soccer and rugby players: comparison of incidence and characteristics. Br J Sports Med. 2004;38(2):168–172. doi: 10.1136/bjsm.2002.003020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee AJ, Garraway WM. Epidemiological comparison of injuries in school and senior club rugby. Br J Sports Med. 1996;30(3):213–217. doi: 10.1136/bjsm.30.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lewis ER, George KP. An initial investigation of injuries in women, men and youth playing rugby union football at the same club. Sport Exerc Injury. 1996;2:186–191. [Google Scholar]
- 26.Marshall SW, Spencer RJ. Concussion in rugby: the hidden epidemic. J Athl Train. 2001;36(3):334–338. [PMC free article] [PubMed] [Google Scholar]
- 27.McIntosh AS, McCrory P, Finch CF, Best JP, Chalmers DJ, Wolfe R. Does padded headgear prevent head injury in rugby union football? Med Sci Sports Exerc. 2009;41(2):306–313. doi: 10.1249/MSS.0b013e3181864bee. [DOI] [PubMed] [Google Scholar]
- 28.McIntosh AS, McCrory P. Effectiveness of headgear in a pilot study of under 15 rugby union football. Br J Sports Med. 2001;35(3):167–169. doi: 10.1136/bjsm.35.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McManus AS, Cross DS. Incidence of injury in elite junior rugby union: a prospective descriptive study. J Sci Med Sport. 2004;7(4):438–445. doi: 10.1016/s1440-2440(04)80261-5. [DOI] [PubMed] [Google Scholar]
- 30.Nathan M, Goedeke R, Noakes TD. The incidence and nature of rugby injuries experienced at one school during the 1982 rugby season. S Afr Med J. 1983;64(4):132–137. [PubMed] [Google Scholar]
- 31.Roux CE, Goedeke R, Visser GR, Van Zyl WA, Noakes TD. The epidemiology of schoolboy rugby injuries. S Afr Med J. 1987;71(5):307–313. [PubMed] [Google Scholar]
- 32.Shuttleworth-Edwards AB, Noakes TD, Radloff SE. The comparative incidence of reported concussions presenting for follow-up management in South African rugby union. Clin J Sport Med. 2008;18(5):403–409. doi: 10.1097/JSM.0b013e3181895910. et al. [DOI] [PubMed] [Google Scholar]
- 33.McIntosh AS, McCrory P, Finch CF, Wolfe R. Head, face and neck injury in youth rugby: incidence and risk factors. Br J Sports Med. 2010;44(3):188–193. doi: 10.1136/bjsm.2007.041400. [DOI] [PubMed] [Google Scholar]
- 34.Waller AE, Feehan M, Marshall SW, Chalmers DJ. The New Zealand Rugby Injury and Performance Project, I: design and methodology of a prospective follow-up study. Br J Sports Med. 1994;28(4):223–228. doi: 10.1136/bjsm.28.4.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aubry M, Cantu R, Dvorak J. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001: recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36(1):6–10. doi: 10.1136/bjsm.36.1.6. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lovell MR, Collins MW, Podell K. ImPACT: Immediate Post-Concussion Assessment and Cognitive Testing. Pittsburgh, PA: NeuroHealth Systems, LLC; 2000. et al. [Google Scholar]
- 37.Orchard J, Hoskins W. For debate: consensus injury definitions in team sports should focus on missed playing time. Clin J Sport Med. 2007;17(3):192–196. doi: 10.1097/JSM.0b013e3180547527. [DOI] [PubMed] [Google Scholar]
- 38.Grimmer KA, Jones D, Williams J. Prevalence of adolescent injury from recreational exercise: an Australian perspective. J Adolesc Health. 2000;27(4):266–272. doi: 10.1016/s1054-139x(00)00120-8. [DOI] [PubMed] [Google Scholar]
- 39.McCrory P, Meeuwisse W, Johnston K. Consensus statement on concussion in sport: The Third International Conference on Concussion in Sport held in Zurich, November 2008. J Sci Med Sport. 2009;12(3):340–351. doi: 10.1016/j.jsams.2009.02.004. et al. [DOI] [PubMed] [Google Scholar]
- 40.McCrory P, Johnston K, Meeuwisse W. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Br J Sports Med. 2005;39(4):196–204. doi: 10.1136/bjsm.2005.018614. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McCrory P. Who should retire after repeated concussions? In: MacAuley DC, Best TM, editors. Evidence Based Sports Medicine. Oxford, United Kingdom: Blackwell Publishing Ltd; 2006. pp. 93–108. [Google Scholar]
- 42.Williamson IJ, Goodman D. Converging evidence for the under-reporting of concussions in youth ice hockey. Br J Sports Med. 2006;40(2):128–132. doi: 10.1136/bjsm.2005.021832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fuller CW, Laborde F, Leather RJ, Molloy MG. International Rugby Board Rugby World Cup 2007 injury surveillance study. Br J Sports Med. 2008;42(6):452–459. doi: 10.1136/bjsm.2008.047035. [DOI] [PubMed] [Google Scholar]
- 44.Sye G, Sullivan JS, McCrory P. High school players' understanding of concussion and return to play guidelines. Br J Sports Med. 2006;40(12):1003–1005. doi: 10.1136/bjsm.2005.020511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.National Collegiate Athletic Association. NCAA Injury Surveillance System data summary. http://www.ncaa.org/wps/portal/ncaahome?WCM_GLOBAL_CONTEXT=/ncaa/NCAA/Academics+and+Athletes/Personal+Welfare/Iss/Report_SelectionByYear. Accessed April 15, 2009.
- 46.Borowski LA, Yard EE, Fields SK, Comstock RD. The epidemiology of US high school basketball injuries, 2005– 2007. Am J Sports Med. 2008;36(12):2328–2335. doi: 10.1177/0363546508322893. [DOI] [PubMed] [Google Scholar]
- 47.Knowles SB, Marshall SW, Bowling MJ. Risk factors for injury among high school football players. Epidemiology. 2009;20(2):302–310. doi: 10.1097/EDE.0b013e318193107c. et al. [DOI] [PubMed] [Google Scholar]
- 48.Yard EE, Schroeder MJ, Fields SK, Collins CL, Comstock RD. The epidemiology of United States high school soccer injuries, 2005– 2007. Am J Sports Med. 2008;36(10):1930–1937. doi: 10.1177/0363546508318047. [DOI] [PubMed] [Google Scholar]
- 49.Hinton RY, Lincoln AE, Almquist JL, Douoquih WA, Sharma KM. Epidemiology of lacrosse injuries in high school-aged girls and boys: a 3-year prospective study. Am J Sports Med. 2005;33(9):1305–1314. doi: 10.1177/0363546504274148. [DOI] [PubMed] [Google Scholar]
- 50.Le Gall F, Carling C, Reilly T, Vandewalle H, Church J, Rochcongar P. Incidence of injuries in elite French youth soccer players: a 10-season study. Am J Sports Med. 2006;34(6):928–938. doi: 10.1177/0363546505283271. [DOI] [PubMed] [Google Scholar]
- 51.Powell JW, Barber-Foss KD. Injury patterns in selected high school sports: a review of the 1995– 1997 seasons. J Athl Train. 1999;34(3):277–284. [PMC free article] [PubMed] [Google Scholar]
- 52.Knowles SB, Marshall SW, Bowling JM. A prospective study of injury incidence among North Carolina high school athletes. Am J Epidemiol. 2006;164(12):1209–1221. doi: 10.1093/aje/kwj337. et al. [DOI] [PubMed] [Google Scholar]
- 53.Quarrie KL, Hopkins WG. Tackle injuries in professional rugby union. Am J Sports Med. 2008;36(9):1705–1716. doi: 10.1177/0363546508316768. [DOI] [PubMed] [Google Scholar]
- 54.Quarrie KL, Alsop JC, Waller AE, Bird YN, Marshall SW, Chalmers DJ. The New Zealand Rugby Injury and Performance Project, VI: a prospective cohort study of risk factors for injury in rugby union football. Br J Sports Med. 2001;35(3):157–166. doi: 10.1136/bjsm.35.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Knapik JJ, Jones SB, Darakjy S. Injuries and injury risk factors among members of the United States Army Band. Am J Ind Med. 2007;50(12):951–961. doi: 10.1002/ajim.20532. et al. [DOI] [PubMed] [Google Scholar]
- 56.Knapik JJ, Sharp MA, Canham-Chervak M, Hauret K, Patton JF, Jones BH. Risk factors for training-related injuries among men and women in basic combat training. Med Sci Sports Exerc. 2001;33(6):946–954. doi: 10.1097/00005768-200106000-00014. [DOI] [PubMed] [Google Scholar]
- 57.Abernethy L, Bleakley C. Strategies to prevent injury in adolescent sport: a systematic review. Br J Sports Med. 2007;41(10):627–638. doi: 10.1136/bjsm.2007.035691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Micheli LJ, Wood R. Back pain in young athletes: significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995;149(1):15–18. doi: 10.1001/archpedi.1995.02170130017004. [DOI] [PubMed] [Google Scholar]
- 59.Fuller CW, Molloy MG, Bagate C. Consensus statement on injury definitions and data collection procedures for studies of injuries in rugby union. Clin J Sport Med. 2007;17(3):177–181. doi: 10.1097/JSM.0b013e31803220b3. et al. [DOI] [PubMed] [Google Scholar]


