Abstract
Context:
With regard to intermittent training exercise, the effects of the mode of recovery on subsequent performance are equivocal.
Objective:
To compare the effects of 3 types of recovery intervention on peak torque (PT) and electromyographic (EMG) activity of the knee extensor muscles after fatiguing isokinetic intermittent concentric exercise.
Design:
Crossover study.
Setting:
Research laboratory.
Patients or Other Participants:
Eight elite judo players (age = 18.4 ± 1.4 years, height = 180 ± 3 cm, mass = 77.0 ± 4.2 kg).
Interventions :
Participants completed 3 randomized sessions within 7 days. Each session consisted of 5 sets of 10 concentric knee extensions at 80% PT at 120°/s, with 3 minutes of recovery between sets. Recovery interventions were passive, active, and electromyostimulation. The PT and maximal EMG activity were recorded simultaneously while participants performed isokinetic dynamometer trials before and 3 minutes after the resistance exercise.
Main Outcome Measure(s):
The PT and maximal EMG activity from the knee extensors were quantified at isokinetic velocities of 60°/s, 120°/s, and 180°/s, with 5 repetitions at each velocity.
Results:
The reduction in PT observed after electromyo-stimulation was less than that seen after passive (P < .001) or active recovery (P < .001). The reduction in PT was less after passive recovery than after active recovery (P < .001). The maximal EMG activity level observed after electromyostimulation was higher than that seen after active recovery (P < .05).
Conclusions:
Electromyostimulation was an effective recovery tool in decreasing neuromuscular fatigue after high-intensity, intermittent isokinetic concentric exercise for the knee extensor muscles. Also, active recovery induced the greatest amount of neuromuscular fatigue.
Keywords: peak torque, isokinetic exercises, concentric exercises, high-intensity intermittent exercises
Key Points.
During high-intensity intermittent isokinetic concentric knee extensions, electromyostimulation was more effective than active recovery or passive recovery in reducing neuromuscular fatigue.
At 30% of peak torque, active recovery was inferior to passive recovery in lessening neuromuscular fatigue.
Neuromuscular fatigue has been defined as a reduction in the force-generating capacity of a muscle caused by previous activity.1 A number of methods exist to quantify neuromuscular fatigue in humans during muscular work. Among them, surface electromyography provides noninvasive and objective quantification.2,3 For instance, during maximal-effort contractions, all the motor units are assumed to be active; fatigue decreases muscle force production,4 which may or may not be accompanied by a reduction in the number of active motor units. Therefore, during heavy-resistance and power-loading protocols, decreases in maximal electromyographic (EMG) activity and strength of the loaded muscles have been reported.2,3 The deleterious effects of neuromuscular fatigue have been demonstrated in simple force production5 and in the performance of complex motor tasks, such running,6 jumping,7 and resistance-training exercises.8 Thus, reducing muscle fatigue with an appropriate recovery intervention is an intriguing topic of research.
Many sport activities are characterized by repeated maximal or near-maximal bouts of short-duration exercise alternated with recovery periods, also known as high-intensity intermittent exercise. This type of exercise is often used in strength-training programs9 and corresponds with patterns seen in many sports, including hockey, tennis, and judo. Intermittent exercises are characterized by interactions among multiple factors, such as the intensity of the exercise and the mode of recovery used during rest periods. Because recovery mode may influence neuromuscular fatigue development, an inappropriate recovery modality may prevent the athlete from training at the required intensity or completing the required workload at the next exercise bout. Therefore, we need to adopt effective recovery strategies between the phases of high-intensity exercise. Effective recovery involves completing several key physiologic and metabolic processes that act in concert to prepare the athlete for the next bout of exercise.10
Numerous studies have been conducted to compare the effects of active and passive recovery. Our present knowledge overwhelmingly supports the superiority of active recovery methods over passive methods for removing lactate from the circulation during high-intensity, intermittent exercise.11–14 However, the effects of these recovery modes on subsequent performance are equivocal.15 For instance, although some authors have reported that active recovery is more efficient than passive recovery,11,13,16–19 others found no differences12,20 or better physical performance after passive recovery.14,21–25
Recently, electromyostimulation (EMS) has gained popularity on the athletic field for strength training26 and as a recovery method.15,27,28 In the latter case, a range of settings has been applied, with frequencies ranging from 7 to 10 Hz, pulse width from 300 to 400 μs, and intensity from 20 to 30 mA.15,27,28 Electromyostimulation enhances muscle blood flow by lowering peripheral resistance.29 However, no clear evidence confirms that EMS enhances recovery. For instance, Vanderthommen et al30 concluded that a neuromuscular electric stimulation program applied to the knee flexor muscles for delayed-onset muscle soreness induced by maximal eccentric exercise had no effect on the magnitude of the initial muscle damage when compared with passive recovery. In summary, although the EMS recovery modality is widely used by elite athletes, mainly because of the time constraints that sometimes exist during training or racing periods, no strong scientific evidence demonstrates its efficiency in promoting recovery.31 To our knowledge, the effects of passive, active, and EMS recovery on performance and associated neuromuscular characteristics have not been compared in the context of intermittent, fatiguing isokinetic concentric contractions.
Therefore, the purpose of our study was to compare the effects of these 3 recovery interventions on neuromuscular characteristics of the quadriceps femoris muscle during intermittent, fatiguing isokinetic concentric contractions. This information is important in helping us to prescribe appropriate recovery modalities during concentric isokinetic exercises used for strength-training or rehabilitation programs. Another aim of our study was to gain fundamental knowledge about muscle recovery after purely concentric exercises. We hypothesized that the use of EMS as a recovery mode during intermittent isokinetic concentric contractions would induce a lower level of fatigue, resulting in smaller decreases in isokinetic torque level and EMG signal amplitude (ie, activation level).
METHODS
Participants
Eight male elite judo players participated in this study (age = 18.4 ± 1.4 years, height = 180 ± 3 cm, mass = 77.0 ± 4.2 kg). They were given a thorough explanation of the protocol, including the possible risks and associated discomfort, before providing informed consent. The athletes belonged to the national or regional team (or both teams) of Tunisia, and all were healthy, with no injury to the lower limbs. None was involved in any specific training program for the lower limb musculature at the time of the study. Participants were all right-leg dominant (determined by the leg used to kick a ball). The experimental design of the study was approved by a local research ethics committee, and the investigation was conducted in accordance with the Declaration of Helsinki.
Experimental Procedures
The experimental protocol comprised 3 testing sessions, each with a different mode of recovery. Each session consisted of a fatiguing intermittent exercise and a series of isokinetic test contractions (Figure 1). Muscle activity and torque were measured before and after the exercise. First, the participants reported to the laboratory to become familiar with the protocol for the isokinetic testing and training. Then all volunteers completed 3 testing sessions in random order separated by a 1-week interval. They performed no high-intensity physical activity for 2 days before each session to avoid the effects of cumulative muscular fatigue.
Figure 1.
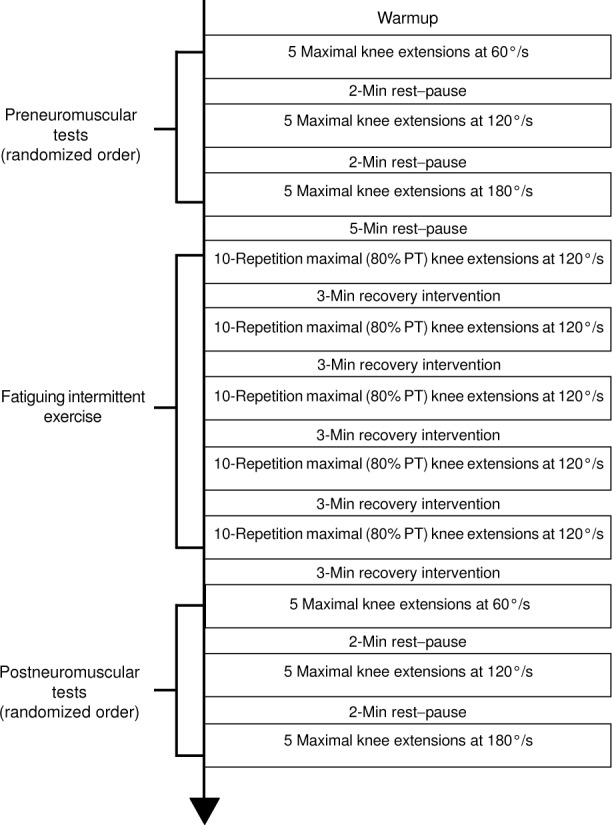
Overview of the experimental protocol. Each session included a pretraining and posttraining maximal test performed before and 3 minutes after the fatiguing exercise, respectively. The tests consisted of 5 maximal isokinetic knee extensions performed at 3 angular velocities (60°/s, 120°/s, and 180°/s) with a 5-second rest period between contractions. A 2-minute rest period was allowed between velocities to minimize muscle fatigue. The order of the 3 velocities was randomized in a balanced design at both the pretraining and the posttraining test. The PT was identified as the highest recorded value among the 5 repetitions at each angular velocity. After the pretraining test and a 5-minute rest period, each participant performed the fatiguing test, which consisted of 5 sets of 10 isokinetic extensions (active phase) and flexions (passive phase) at 120°/s at 80% of the PT recorded at 120°/s during the pretraining test. Abbreviation: PT, peak torque.
The test sessions were designed to investigate 3 recovery interventions after intermittent exercise of isokinetic concentric contractions for the quadriceps. The 3 interventions were active recovery (AR), passive recovery (PR), and EMS (ER). During the first session, AR was performed by 4 athletes, PR by 2, and ER by 2. One week later, AR was performed by 1 athlete, PR by 3 athletes, and ER by 4 athletes. During the last session, AR and ER were performed by 3 athletes each, and PR was performed by 2.
Each session began with a warmup phase, which consisted of submaximal cycling for 5 minutes. The volunteers cycled at a comfortable, self-selected cadence to avoid any significant muscle fatigue. Immediately after cycling, participants were seated on a strength-testing machine that was arranged for right-leg flexion-extension exercises.
Data Collection
Isokinetic Test and Fatigue Exercise. The testing procedure was performed using a Cybex Norm isokinetic dynamometer (Lumex, Inc, New York, NY) from the seated position with the hip fixed at 90°. Hook-and-loop straps stabilized the trunk, the waist, and the upper thigh on the chair. The rotational axis of the dynamometer was carefully aligned with the center of rotation of the knee at the posterior aspect of the lateral femoral condyle. The movable arm of the dynamometer was fixed at the distal end of the tibia, proximal to the medial malleoli. This position was recorded to ensure the same placement for all 3 test sessions. Gravity correction was obtained by measuring the torque exerted on the dynamometer resistance adapter by the relaxed, fully extended knee. Total range of motion (ROM) during the isokinetic contractions was set for all contractions from 0° (full extension) to 90° of flexion.
Each session comprised pretraining and posttraining maximal tests, performed before and 3 minutes after the fatiguing exercise, respectively. The tests consisted of 5 maximal isokinetic knee extensions at 3 angular velocities (60°/s, 120°/s, and 180°/s). A 2-minute rest period was allowed between test levels to minimize muscle fatigue.32 A 5-second rest period between contractions was permitted, during which time the lower limb was passively returned to the starting position.33 The order of the 3 velocities was randomized in a balanced design for both the pretraining and posttraining tests. Torque and EMG measurements were recorded simultaneously and continuously while participants performed the 5 isokinetic knee extensions at each velocity. Peak torque (PT) was identified as the highest recorded value among the 5 repetitions at each angular velocity. During the measurement of isokinetic torque, each participant was required to fold his arms across his chest. As the dynamometer arm moved from 90° to 0°, the participant was verbally encouraged to perform maximally for each contraction throughout the full ROM (ie, the active phase of the contraction cycle). Visual feedback of the produced force was provided via the Cybex computer monitor. All the testing procedures and verbal encouragement were administered by the same investigator to all athletes. The volunteers relaxed as the dynamometer arm moved back to 90° (ie, the passive phase of the contraction cycle).
After the pretest and a 5-minute rest, each participant performed 5 sets of 10 isokinetic extensions (active phase) and flexions (passive phase) at 120°/s for the right-leg knee extensors at 80% of the PT recorded at 120°/s during the pretest. The athletes were instructed to provide an effort corresponding to this intensity. For this purpose, a permanent horizontal line on the computer screen indicated 80% of the PT recorded at 120°/s for each participant. Verbal feedback about the produced output torque was given by the investigator. Each set lasted approximately 25 seconds, and 3 minutes of recovery were allowed between sets.9 After the last 3-minute recovery period following the fifth set, participants were instructed to perform the posttest.
EMG Measurement and Analysis.
The EMG signals were obtained using differential bipolar surface electrodes (model DE-2.1; DelSys, Inc, Boston, MA). The electrode housing is a waterproof polycarbonate plastic case, which is internally shielded to prevent ambient electric noise. The electrodes are fitted with 2 silver bar contacts measuring 1 cm in length and 0.1 cm in diameter, with a fixed interelectrode spacing of 1 cm. Surface electrodes were placed parallel to muscle fibers, longitudinally on the vastus lateralis (VL), rectus femoris (RF), and vastus medialis (VM) muscles of the right leg, in accordance with the European recommendations for surface electromyography.34 For the VM, the electrodes were placed at approximately 20% of the distance between the medial gap of the knee joint and the anterior-superior iliac spine. For the RF, the electrodes were placed at approximately 50% of the distance between the anterior-superior iliac spine and the superior border of the patella. The electrode placements on the VL were at approximately two thirds of the distance between the anterior-superior iliac spine and the lateral aspect of the patella. The electrodes were easily attached to the skin with the electrode interface (Del-Sys, Inc). A reference electrode was placed on the patella of the opposite leg. The exact electrode positions over the 3 muscles were measured carefully for each participant and marked on the skin with a waterproof permanent marker to ensure a consistent location throughout the experiment. Before the electrodes were placed, the skin was shaved, abraded, and cleaned with an alcohol, ether, and acetone solution to minimize skin impedance and ensure adhesion of the electrodes. Before testing began, the participant was asked to contract the muscles to demonstrate good electrode-skin contact and root mean square (RMS) noise levels less than 12 μV.
The EMG signals were preamplified (common mode rejection ratio = 92 dB, input impedance > 1015 Ω, gain = 1000) using a differential amplifier (Bagnoli-4 EMG system; DelSys, Inc). The EMG signals from the recording sites were filtered to a bandwidth between 20 and 450 Hz using a band-pass, second-order Butterworth filter to remove unwanted noise and possible movement artifact in the low-frequency region and to eliminate aliasing and other artifact in the high-frequency region. The signals were analog-to-digital converted (with 16-bit accuracy in the signal range ± 5 V) at a sampling rate of 1000 Hz and stored in a personal computer for subsequent analysis by EMG-works (version 3.0; DelSys, Inc).
For each velocity level (60°/s, 120°/s, and 180°/s) and each muscle, the RMS was calculated over the extension phase (ie, from 90° to 0°) of each of the 5 contractions. The 5 RMS values were then averaged and normalized to the respective values obtained before the fatiguing exercise (pretest) under the same testing conditions. The normalized RMSs for the VL, RF, and VM muscles were summed and averaged to provide an overall representation of muscle activity.
Recovery Interventions
The participants were allowed to recover for 3 minutes between sets. During passive recovery, the knee remained in a relaxed state at the starting position (90° of flexion). Active recovery consisted of 3 minutes of repetitive moderate isokinetic contractions for the right-leg knee extensors from the same ROM. Each athlete executed the active phase in approximately 0.6 seconds (at 180°/s; 30% PT previously recorded at 180°/s) and the passive phase in approximately 1.9 seconds (at 60°/s). To our knowledge, only Andersson et al35 used active recovery calibrated as a percentage of maximal force (<50% of 1-repetition maximum during 30 minutes) between soccer matches. During the familiarization period, we tested our volunteers with different percentages of the PT at 180°/s and observed that active recovery at 30% of this velocity was the value most comfortable for the participants, who were instructed to exert effort corresponding to this intensity. For this purpose, a permanent horizontal line on the computer screen indicated 30% of the PT recorded at 180°/s for the individual. Verbal feedback about the output moment was given by the investigator.
The EMS recovery consisted of electric stimulation of the quadriceps femoris for 3 minutes. The lower limb was in a relaxed state at the starting position. The contractions were produced with a portable and programmable electric stimulator (model Activa 300 PRO; GLOBUS Italia SRL, Codogne, Italy), which delivered rectangular pulses. To elicit a peripheral muscle pump action, as suggested in the literature, low-frequency stimulation (10 Hz) and a 400-μs impulse duration have been used.15,27,28 Electric stimulation was elicited using self-adhesive bipolar electrodes (model MyoTrode, 5 × 5 cm; GLOBUS Italia SRL). Three negative electrodes were placed close to the proximal insertion of the VL, RF, and VM. Three positive electrodes were placed over the motor points of the 3 stimulated muscles (Figure 2). The motor points for these muscles were determined by moving a probe over the skin surface to find the lowest threshold for stimulation. Electrodes were not removed or replaced during the session. During the familiarization period, the current amplitude was gradually increased for each participant until the maximum but comfortable intensity was achieved (24.75 ± 0.71 mA; range, 24–26 mA).15,27,28 Current amplitude was then recorded and kept constant during the 3-minute EMS intervention.
Figure 2.
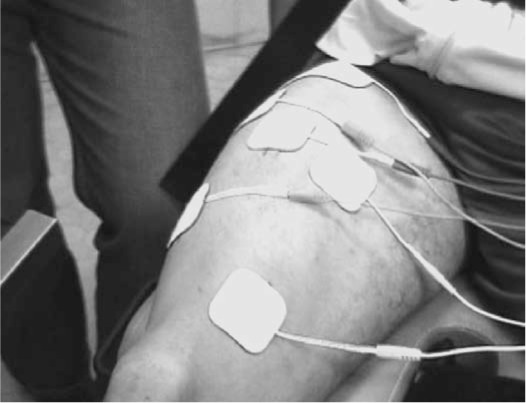
Experimental setup for electromyostimulation. Three negative electrodes were placed close to the proximal insertion of the vastus lateralis, rectus femoris, and vastus medialis muscles. Three positive electrodes were placed over the motor points of the stimulated muscles.
Statistical Analysis
The force measurements were expressed as a percentage of the PT deficit at each velocity. For the neuromuscular variables (PT, RMS), 2-way (contraction velocity × recovery type) analyses of variance (ANOVAs) with repeated measures were used to detect differences among the 3 recovery interventions at 3 angular velocities. When appropriate, the least significant difference post hoc test was used for multiple pairwise comparisons. All data were expressed as mean ± SD. Statistical significance was accepted at P < .05. All statistical analyses were performed with Statistica for Windows software (version 6.0; StatSoft, Inc, Tulsa, OK).
RESULTS
Isokinetic PT
For AR, the fatiguing task induced a decrease in PT ranging from 18.47 ± 7.16% at 60°/s to 15.24 ± 5.02% at 120°/s and 11.20 ± 5.82% at 180°/s (Figure 3). For PR, the decrease in PT ranged from 13.18 ± 7.50% at 60°/s to 8.25 ± 3.84% at 120°/s and 8.79 ± 6.49% at 180°/s. For ER, the decrease in PT ranged from 6.59 ± 7.25% at 60°/s to 4.84 ± 3.87% at 120°/s and 4.24 ± 4.20% at 180°/s. The 2-way repeated-measures ANOVAs revealed differences among the 3 types of recovery intervention for the isokinetic PT data (F2,14 = 47.09, P < .001). Post hoc analysis demonstrated less of a PT deficit after ER than after PR (P < .001) and AR (P < .001) (Figure 3). Moreover, the PT deficit was less after PR than after AR (P < .001; Figure 3).
Figure 3.
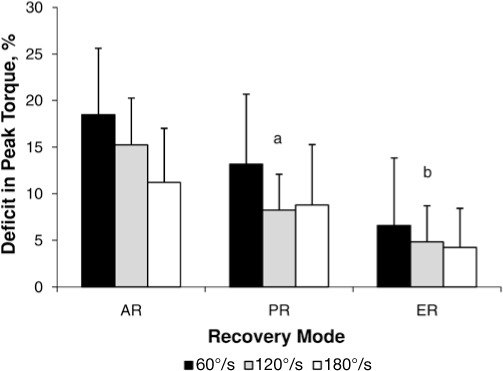
Deficit in isokinetic peak torque measured after the fatiguing exercise at 60°/s, 120°/s, and 180°/s. Values are mean ± SD.
a The deficit in peak torque was less after PR than after AR (P < .001).
b In addition, the deficit in peak torque observed after the ER was lower than after the AR and PR interventions (P < .001). Abbreviations: AR, active recovery; ER, electromyostimulation; PR, passive recovery.
In addition, the ANOVA revealed effects of the contraction velocity (F2,14 = 4.63; P < .05), with interactions of contraction velocity × recovery type (F4,28 = 4.28; P < .01). The PR at 120°/s was different from AR at 180°/s and ER at 120°/s (P < .01). Similarly, we observed differences between AR at 60°/s and 120°/s (P < .01). In addition, PR at 180°/s was different from AR at 180°/s and ER at 60°/s (P < .05). This last condition was also different from ER at 180°/s (P < .05). However, we found no differences between PR at 60°/s and AR at 120°/s (P = .06) or 180°/s (P = .07). Moreover, PR at 120°/s was not different from PR at 180°/s (P = .61) and ER at 60°/s (P = .13). In addition, ER at 120°/s was not different from ER at 60°/s (P = .11) and 180°/s (P = .57). Differences (all P < .001) were noted between all other combinations. The PT reduction was less at 180°/s than at 60°/s (P < .05). However, no difference was seen between 60°/s and 120°/s (P = .055) or between 120°/s and 180°/s (P = .40).
EMG RMS Amplitude
In the time domain, the 2-way repeated-measures ANOVAs revealed differences between the normalized RMS activity recorded after the 3 interventions (F2,46 = 3.60, P < .05). The normalized RMS values seen after ER were higher (P < .05; Figure 4) than those obtained after AR. However, no differences were observed for the normalized RMS of the quadriceps femoris after PR compared with ER (P = .38) or AR (P = .086). In addition, no effect of contraction velocity (F2,46 = 1.17, P = .32) or significant interaction of contraction velocity × recovery type was evident (F4,92 = 0.84, P = .50).
Figure 4.
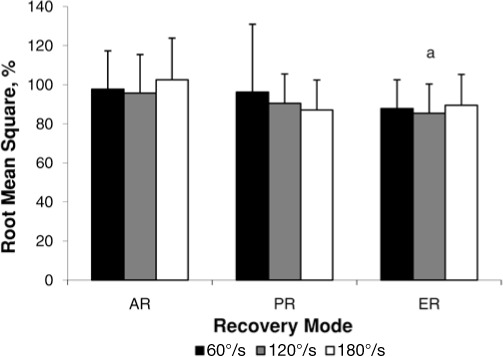
Normalized root mean square of electromyographic amplitude during the 3 sessions at the 3 angular velocities (60°/s, 120°/s, and 180°/s).
a The normalized root mean square values obtained after ER were higher than those obtained after AR (P < .05). Abbreviations: AR, active recovery; ER, electromyostimulation; PR, passive recovery.
DISCUSSION
The aim of our study was to compare the effectiveness of 3 recovery modalities (AR, PR, and ER) during an intermittent isokinetic concentric exercise on maximal voluntary force-generating capacity and the activity level of the quadriceps femoris. In accordance with our hypothesis, the results suggest that the most appropriate and effective recovery mode is ER. These findings enhance our knowledge about the effects of different modalities of recovery applied during the rest periods of intermittent isokinetic concentric contractions for the knee extensors and will allow clinicians and coaches to better prescribe the most effective recovery mode during this specific training modality.
Our major finding was that the reduction in the normalized PT at the 3 programmed angular velocities (60°/s, 120°/s, and 180°/s) was lower after ER than after AR or PR. Based on the classic definition of neuromuscular fatigue,1 our results show that the EMS intervention reduced fatigue more than did AR or PR. This result is in line with the higher EMG activity level recorded after ER when compared with AR. To our knowledge, previous studies15,27,28 of EMS as a mode of recovery have been performed mainly after eccentric contractions. Yet fatigue induced by eccentric exercise differs from fatigue induced by a concentric (or mainly concentric) exercise. In fact, eccentric exercise leads to delayed-onset muscle soreness and causes muscle damage and soreness36,37; long-term recovery occurs over several days.27 Thus, one reason for differences in fatigue after concentric and eccentric exercise is the rightward shift in the ascending force-length relationship after the latter, probably from the presence of damaged sarcomeres.36,37 Therefore, the delayed and long-lasting decline in muscle force caused by a short burst of maximal exercise is more profound after concentric exercise but lasts longer after eccentric exercise.38 For these reasons, direct comparison with our results is very difficult.
The smaller amount of fatigue reported with EMS recovery might be explained by the fact that specific electric stimulation increases regional blood flow, especially when stimulation at low frequencies is used at intensities sufficient to cause skeletal muscle contraction in the exhausted muscles.29 Thus, increasing blood flow could improve oxygen delivery and the efflux of noxious substances and, consequently, enhance recovery. The EMS might also improve performance by accelerating the restoration of ionic balance across the sarcolemma of fatigued fibers. The greater maximal EMG activity recorded after the fatiguing exercise for ER compared with AR indicates that neural drive is less affected with ER.39 In fact, the smaller RMS amplitude accompanied by the greatest decrease in PT after the series interspersed by AR may have resulted from reductions in the number of participating motor units,40,41 the discharge rate of the recruited motor units,42 the amplitude of motor unit action potentials,43 or a combination of these causes. These changes can result from an accumulation of metabolites (ie, H+ and extracellular K+)44 and reduction in the intracellular pH,45 thus decreasing sarcolemma excitability after the fatiguing exercise interspersed by AR. The voluntary contractions at the intensity in our protocol probably exacerbated fatigue instead of assisting muscle recovery from fatigue induced by the intermittent exercise. Although the decrease in PT was less after ER than after PR, we found no differences between EMG activity recorded during these conditions. This lack of difference in the electric manifestations associated with the greater force-generating capacity is probably caused by greater peripheral fatigue in PR (ie, deficit in contractility from the fatigued motor units). However, the methods we used did not permit us to test this hypothesis. Finally, the better performances observed with ER might also be due to a placebo effect. In fact, some authors15,28 claimed that EMS recovery intervention could have a beneficial effect on the psychological state of the athlete, which might help to maintain maximal performance. Yet our main result was that the most appropriate and effective recovery mode during intermittent isokinetic concentric knee extensions was ER. The reasons for this efficiency, including the possible placebo effect, should be explored in further research.
The second main result of our study was the smaller deficit in PT after PR compared with AR. This finding is consistent with previously reported studies (Table). Dupont et al22 stated that the longer time to exhaustion of a high-intensity intermittent exercise resulting from the use of PR could be attributed to less metabolic power and a slower decline in oxyhemoglobin than during active recovery. The latter recovery intervention probably permitted greater reoxygenation of myoglobin and phosphorylcreatine (PCr) resynthesis, leading to the observed longer time to exhaustion.22 This suggestion was recently investigated by Spencer et al,24 who reported a strong trend toward lower postexercise PCr concentrations during AR. In light of these results, the mechanisms explaining the maintenance of a higher level of PT after exercise interspersed with PR were probably related to a possible slower rate of PCr depletion and greater rate of PCr resynthesis. The increased energetic cost of AR versus PR may be a factor22 because PCr resynthesis depends on oxidative processes, and during AR, PCr resynthesis and lactate oxidation compete for limited oxygen supplies.
Table.
Table. Comparison of Active and Passive Recovery as Reported in the Literature
| Study | Population | Fatiguing Protocol | Recovery Strategies | Results |
| Thiriet et al (1993)13,a | 16 untrained participants | Repeated bouts (2 min) of maximal pedaling exercise | 5 min after each exercise bout: PR and AR (pedaling at 30% of MAS) | AR preserved better performance during repeated maximal exercise |
| Ahmaidi et al (1996)11,a | 10 untrained participants | Repeated bouts (6 s) of intense cycling exercise against increasing braking forces | 5 min after each exercise bout: PR and AR (cycling at 32% of MAS) | AR resulted in greater anaerobic power output than PR |
| Bogdanis et al (1996)16,a | 13 untrained participants | 2 maximal (30-s) cycle ergometer sprints | 4 min between sprints, with PR and AR (cycling at 40% of V˙o2max) | AR resulted in greater mean power output than PR |
| McEniery et al (1997)18,a | 5 untrained participants | 4 × 30-s sprints (cycling) interspersed with 4-min intervals | 15 min after exercise: PR and AR (cycling at 30% and 60% of V˙o2max) | AR at 30% of V˙o2max resulted in greater peak torque than PR and AR at 60% of V˙o2max |
| Dorado et al (2004)17,a | 10 untrained participants | High-intensity intermittentexercise (4 cycling bouts until exhaustion at 110% maximal power) | 5 min after each exercise bout: PR, AR (pedaling at 20% of V˙o2max) and stretching exercises | AR improved performance by increasing aerobic energy yield |
| Spierer et al (2004)19,a | 6 untrained, 9 moderately trained hockey players | 2 × 30-s Wingate anaerobic power tests | 4 min between tests with PR and AR (pedaling at 28% of V˙o2max) | AR increased total work achieved during repeated Wingate anaerobic power tests |
| Franchini et al (2003)20,b | 17 judo players | 5-min judo combat followed by 15-min recovery and 4 bouts of upper body Wingate tests (3-min rests in between) | 15 min after judo combat: PR and AR (running at ≈50% of V˙o2max) | No difference in performance of subsequent intermittent anaerobic exercises |
| Coffey et al (2004)12,b | 14 trained participants | 2 treadmill runs to exhaustion at 120% and 90% of PRS over 4 h | 15 min after the firsttreadmill run: PR and AR (40% of PRS) and CTW | No difference |
| Dupont et al (2004)22,c | 12 soccer players | High-intensity intermittentcycling exercise (15 s) to exhaustion | 15 s after each exercise bout: PR and AR (cycling at 40% of V˙o2max) | PR resulted in greater time power, and slower rate to exhaustion, less metabolic of decrease in oxyhemoglobin |
| Spencer et al (2006)24,c | 9 moderately trained participants | Repeated sprint cycling (6 × 4 s) | 25 s after each exercise bout: PR and AR (cycling at 32% of V˙o2max) | PR resulted in less power decrement and greater final peak power |
| Toubekis et al (2005)14,c | 9 trained swimmers | 8 × 25-m sprints (swimming) interspersed with 45-s intervals | 45 s after each exercise bout: PR and AR (50% and 60% of 100-m velocity) | PR resulted in better performance than AR |
| Thevenet et al (2007)25,c | 8 endurance-trained adolescents | Intermittent runs (30 s) at 105% of MAS to exhaustion | 30 s after each exercise bout: PR and AR (running at 50% of MAS) | PR resulted in greater time to exhaustion than AR |
| Castagna et al (2008)21,c | 16 basketball players | Repeated sprint ability (10 × 30-m shuttle-run sprints) | 30 s after each exercise bout: PR and AR (running at 50% of MAS) | PR resulted in lower fatigue index than AR |
| Jougla et al (2009)23,c | 7 male rugby players | Repeated-sprint rugby tests completed before and after a 30-min rugby match | 30 s after each repetition of the tests: PR and AR (running at 50% of MAS) | Scrum forces were greater in PR; fatigue index and total sprint time were greater in AR |
Abbreviations: AR: active recovery; CTW, contrast-temperature water immersion; MAS, maximal aerobic speed; PR, passive recovery; PRS, peak running speed.
a Better results for AR than for PR.
b No difference between AR and PR.
c Better results for PR than for AR.
However, several authors12,20 found no differences between these types of recovery on subsequent performance, and others11,13,16–19 reported that AR allowed better performance. Some of the discrepancies among these studies might be due to differences in the duration of recovery and the intensity at which the exercise bouts were performed.17 If so, the contrast between our results and those of the studies mentioned earlier can be explained by the intensity programmed during our AR (30% of the PT recorded at 180°/s during 3 minutes), which could reduce the rate of PCr resynthesis and delay recovery. In addition, although we studied well-trained participants, the other authors studied AR interventions in untrained participants (Table). Thus, sedentary people seem to benefit from AR interventions, whereas athletes show similar or better performance after PR.19,46
Implications
Because concentric isokinetic exercises are used in both injury rehabilitation and strength training, our results have practical applications. More precisely, recovery modalities can enhance performance by enabling athletes or patients to tolerate greater training loads or by increasing the performance-enhancing effect of training at a given load. Consequently, clinicians and coaches should consider prescribing the appropriate recovery intervention during concentric isokinetic strength training of the knee extensors in elite young athletes. Therefore, based on our results, we would recommend that certified athletic trainers and clinicians use EMS rather than AR or PR during high-intensity intermittent concentric isokinetic exercise.
Limitations
Our investigation had several possible limitations that must be considered. In fact, our findings are limited to the concentric isokinetic strength training of an isolated muscle group (ie, knee extensors) and to the specific settings selected for the different recovery interventions. Moreover, because training may affect the response to neuromuscular fatigue, these results should not be generalized to sedentary people. Despite these limitations, the present study offers fundamental knowledge about muscle recovery after purely concentric exercises that could serve as the basis for future research.
CONCLUSIONS
Electromyostimulation was better than AR or PR for decreasing neuromuscular fatigue during intermittent isokinetic concentric knee extensions. Moreover, PR seemed to be more effective than AR performed at 30% of PT.
In order to better understand the physiologic phenomenon that could explain these results, future authors should investigate additional settings. First, it is very important to measure blood flow during the different modalities of recovery to confirm our suggestions. Second, some biochemical markers, such as lactate and ammonia, can provide more information about metabolism. Third, peripheral and central fatigue should be quantified by measuring twitch torque and voluntary activation (superimposed stimulation). Finally, further studies are needed to optimize electric stimulation settings before we evaluate the efficiency of this method in recovery and explore the putative placebo effect.
REFERENCES
- 1.West W, Hicks A, Clements L, Dowling J. The relationship between voluntary electromyogram, endurance time and intensity of effort in isometric handgrip exercise. Eur J Appl Physiol Occup Physiol. 1995;71(4):301–305. doi: 10.1007/BF00240408. [DOI] [PubMed] [Google Scholar]
- 2.Linnamo V, Newton RU, Häkkinen K. Neuromuscular responses to explosive and heavy resistance loading. J Electromyogr Kinesiol. 2000;10(6):417–424. doi: 10.1016/s1050-6411(00)00029-8. et al. [DOI] [PubMed] [Google Scholar]
- 3.Walker S, Ahtiainen JP, Häkkinen K. Acute neuromuscular and hormonal responses during contrast loading: effect of 11 weeks of contrast training. Scand J Med Sci Sports. 2009;20(2):226–234. doi: 10.1111/j.1600-0838.2009.00914.x. [DOI] [PubMed] [Google Scholar]
- 4.Komi PV, Rusko H. Quantitative evaluation of mechanical and electrical changes during fatigue loading of eccentric and concentric work. Scand J Rehabil Med Suppl. 1974;3:121–126. [PubMed] [Google Scholar]
- 5.Merton AR. Voluntary strength and fatigue. J Physiol. 1954;123(3):553–564. doi: 10.1113/jphysiol.1954.sp005070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christina KA, White SC, Gilchrist LA. Effect of localized muscle fatigue on vertical ground reaction forces and ankle joint motion during running. Hum Mov Sci. 2001;20(3):257–276. doi: 10.1016/s0167-9457(01)00048-3. [DOI] [PubMed] [Google Scholar]
- 7.Chappell JD, Herman DC, Knight BS, Kirkendall DT, Garrett WE, Yu B. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2005;33(7):1022–1029. doi: 10.1177/0363546504273047. [DOI] [PubMed] [Google Scholar]
- 8.Babault N, Desbrosses K, Fabre MS, Michaut A, Pousson M. Neuromuscular fatigue development during maximal concentric and isometric knee extensions. J Appl Physiol. 2006;100(3):780–785. doi: 10.1152/japplphysiol.00737.2005. [DOI] [PubMed] [Google Scholar]
- 9.American College of Sports Medicine. Position stand: progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41(3):687–708. doi: 10.1249/MSS.0b013e3181915670. [DOI] [PubMed] [Google Scholar]
- 10.Hooper SL, Mackinnon LT, Howard A, Gordon RD, Bachmann AW. Markers for monitoring overtraining and recovery. Med Sci Sports Exerc. 1995;27(1):106–112. [PubMed] [Google Scholar]
- 11.Ahmaidi S, Granier P, Taoutaou Z, Mercier J, Dubouchaud H, Prefaut C. Effects of active recovery on plasma lactate and anaerobic power following repeated intensive exercise. Med Sci Sports Exerc. 1996;28(4):450–456. doi: 10.1097/00005768-199604000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Coffey V, Leveritt M, Gill N. Effect of recovery modality on 4-hour repeated treadmill running performance and changes in physiological variables. J Sci Med Sport. 2004;7(1):1–10. doi: 10.1016/s1440-2440(04)80038-0. [DOI] [PubMed] [Google Scholar]
- 13.Thiriet P, Gozal D, Wouassi D, Oumarou T, Gelas H, Lacour JR. The effect of various recovery modalities on subsequent performance, in consecutive supramaximal exercise. J Sports Med Phys Fitness. 1993;33(2):118–129. [PubMed] [Google Scholar]
- 14.Toubekis AG, Douda HT, Tokmakidis SP. Influence of different rest intervals during active or passive recovery on repeated sprint swimming performance. Eur J Appl Physiol. 2005;93(5–6):694–700. doi: 10.1007/s00421-004-1244-9. [DOI] [PubMed] [Google Scholar]
- 15.Lattier G, Millet GY, Martin A, Martin V. Fatigue and recovery after high-intensity exercise, part II: recovery interventions. Int J Sports Med. 2004;25(7):509–515. doi: 10.1055/s-2004-820946. [DOI] [PubMed] [Google Scholar]
- 16.Bogdanis GC, Nevill ME, Lakomy HK, Graham CM, Louis G. Effects of active recovery on power output during repeated maximal sprint cycling. Eur J Appl Physiol Occup Physiol. 1996;74(5):461–469. doi: 10.1007/BF02337727. [DOI] [PubMed] [Google Scholar]
- 17.Dorado C, Sanchis-Moysi J, Calbet JA. Effects of recovery mode on performance, O2 uptake, and O2 deficit during high-intensity intermittent exercise. Can J Appl Physiol. 2004;29(3):227–244. doi: 10.1139/h04-016. [DOI] [PubMed] [Google Scholar]
- 18.McEniery CM, Jenkins DG, Barnett C. The relationship between plasma potassium concentration and muscle torque during recovery following intense exercise. Eur J Appl Physiol Occup Physiol. 1997;75(5):462–466. doi: 10.1007/s004210050189. [DOI] [PubMed] [Google Scholar]
- 19.Spierer DK, Goldsmith R, Baran DA, Hryniewicz K, Katz SD. Effects of active vs. passive recovery on work performed during serial supramaximal exercise tests. Int J Sports Med. 2004;25(2):109–114. doi: 10.1055/s-2004-819954. [DOI] [PubMed] [Google Scholar]
- 20.Franchini E, Yuri Takito M, Yuzo Nakamura F, Ayumi Matsushigue K, Peduti Dal'Molin Kiss MA. Effects of recovery type after a judo combat on blood lactate removal and on performance in an intermittent anaerobic task. J Sports Med Phys Fitness. 2003;43(4):424–431. [PubMed] [Google Scholar]
- 21.Castagna C, Abt G, Manzi V, Annino G, Padua E, D'Ottavio S. Effect of recovery mode on repeated sprint ability in young basketball players. J Strength Cond Res. 2008;22(3):923–929. doi: 10.1519/JSC.0b013e31816a4281. [DOI] [PubMed] [Google Scholar]
- 22.Dupont G, Moalla W, Guinhouya C, Ahmaidi S, Berthoin S. Passive versus active recovery during high-intensity intermittent exercises. Med Sci Sports Exerc. 2004;36(2):302–308. doi: 10.1249/01.MSS.0000113477.11431.59. [DOI] [PubMed] [Google Scholar]
- 23.Jougla A, Micallef JP, Mottet D. Effects of active vs. passive recovery on repeated rugby-specific exercises. J Sci Med Sport. 2010;13(3):350–355. doi: 10.1016/j.jsams.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 24.Spencer M, Bishop D, Dawson B, Goodman C, Duffield R. Metabolism and performance in repeated cycle sprints: active versus passive recovery. Med Sci Sports Exerc. 2006;38(8):1492–1499. doi: 10.1249/01.mss.0000228944.62776.a7. [DOI] [PubMed] [Google Scholar]
- 25.Thevenet D, Tardieu-Berger M, Berthoin S, Prioux J. Influence of recovery mode (passive vs. active) on time spent at maximal oxygen uptake during an intermittent session in young and endurance-trained athletes. Eur J Appl Physiol. 2007;99(2):133–142. doi: 10.1007/s00421-006-0327-1. [DOI] [PubMed] [Google Scholar]
- 26.Brocherie F, Babault N, Cometti G, Maffiuletti N, Chatard JC. Electro-stimulation training effects on the physical performance of ice hockey players. Med Sci Sports Exerc. 2005;37(3):455–460. doi: 10.1249/01.mss.0000155396.51293.9f. [DOI] [PubMed] [Google Scholar]
- 27.Martin V, Millet GY, Lattier G, Perrod L. Effects of recovery modes after knee extensor muscles eccentric contractions. Med Sci Sports Exerc. 2004;36(11):1907–1915. doi: 10.1249/01.mss.0000145526.43208.08. [DOI] [PubMed] [Google Scholar]
- 28.Tessitore A, Meeusen R, Cortis C, Capranicla L. Effects of different recovery interventions on anaerobic performances following preseason soccer training. J Strength Cond Res. 2007;21(3):745–750. doi: 10.1519/R-20386.1. [DOI] [PubMed] [Google Scholar]
- 29.Miller BF, Gruben KG, Morgan BJ. Circulatory responses to voluntary and electrically induced muscle contractions in humans. Phys Ther. 2000;80(1):53–60. [PubMed] [Google Scholar]
- 30.Vanderthommen M, Soltani K, Maquet D, Crielaard JM, Croisier JL. Does neuromuscular electrical stimulation influence muscle recovery after maximal isokinetic exercise? Isokinet Exerc Sci. 2007;15(2):143–149. [Google Scholar]
- 31.Millet G, Perrey S, Divert C, Foissac M. The role of engineering in fatigue reduction during human locomotion: a review. Sports Eng. 2006;9(4):209–220. [Google Scholar]
- 32.Pua YH, Koh MTH, Teo YY. Effects of allometric scaling and isokinetic testing methods on the relationship between countermovement jump and quadriceps torque and power. J Sports Sci. 2006;24(4):423–432. doi: 10.1080/02640410500189124. [DOI] [PubMed] [Google Scholar]
- 33.Symons TB, Vandervoort AA, Rice CL, Overend TJ, Marsh GD. Effects of maximal isometric and isokinetic resistance training on strength and functional mobility in older adults. J Gerontol A Biol Sci Med Sci. 2005;60(6):777–781. doi: 10.1093/gerona/60.6.777. [DOI] [PubMed] [Google Scholar]
- 34.Hermens HJ, Feriks B, Merletti R. SENIAM 8: European Recommendations for Surface Electromyography. Enschede, The Netherlands: Roessingh Research and Development; 1999. et al. [Google Scholar]
- 35.Andersson H, Raastad T, Nilsson J, Paulsen G, Garthe I, Kadi F. Neuromuscular fatigue and recovery in elite female soccer: effects of active recovery. Med Sci Sports Exerc. 2008;40(2):372–380. doi: 10.1249/mss.0b013e31815b8497. [DOI] [PubMed] [Google Scholar]
- 36.Morgan DL, Gregory JE, Proske U. The influence of fatigue on damage from eccentric contractions in the gastrocnemius muscle of the cat. J Physiol. 2004;561(pt 3):841–850. doi: 10.1113/jphysiol.2004.069948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Proske U, Allen TJ. Damage to skeletal muscle from eccentric exercise. Exerc Sport Sci Rev. 2005;33(2):98–104. doi: 10.1097/00003677-200504000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Smith IC, Newham DJ. Fatigue and functional performance of human biceps muscle following concentric or eccentric contractions. J Appl Physiol. 2006;102(1):207–213. doi: 10.1152/japplphysiol.00571.2006. [DOI] [PubMed] [Google Scholar]
- 39.Enoka RM, Stuart DG. Neurobiology of muscle fatigue. J Appl Physiol. 1992;72(5):1631–1648. doi: 10.1152/jappl.1992.72.5.1631. [DOI] [PubMed] [Google Scholar]
- 40.Grimby L, Hannerz J, Hedman B. The fatigue and voluntary discharge properties of single motor units in man. J Physiol. 1981;316:545–554. doi: 10.1113/jphysiol.1981.sp013805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peters EJ, Fuglevand AJ. Cessation of human motor unit discharge during sustained maximal voluntary contraction. Neurosci Lett. 1999;274(1):66–70. doi: 10.1016/s0304-3940(99)00666-7. [DOI] [PubMed] [Google Scholar]
- 42.Bigland-Ritchie B, Johansson R, Lippold OC, Smith S, Woods JJ. Changes in motoneurone firing rates during sustained maximal voluntary contractions. J Physiol. 1983;340:335–346. doi: 10.1113/jphysiol.1983.sp014765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fitts RH. Cellular mechanisms of muscle fatigue. Physiol Rev. 1994;74(1):49–94. doi: 10.1152/physrev.1994.74.1.49. [DOI] [PubMed] [Google Scholar]
- 44.Bigland-Ritchie B, Donovan EF, Roussos CS. Conduction velocity and EMG power spectrum changes in fatigue of sustained maximal efforts. J Appl Physiol. 1981;51(5):1300–1305. doi: 10.1152/jappl.1981.51.5.1300. [DOI] [PubMed] [Google Scholar]
- 45.Brody LR, Pollock MT, Roy SH, De Luca CJ, Celli B. pH-induced effects on median frequency and conduction velocity of the myoelectric signal. J Appl Physiol. 1991;71(5):1878–1885. doi: 10.1152/jappl.1991.71.5.1878. [DOI] [PubMed] [Google Scholar]
- 46.Barnett A. Using recovery modalities between training sessions in elite athletes: does it help? Sports Med. 2006;36(9):781–796. doi: 10.2165/00007256-200636090-00005. [DOI] [PubMed] [Google Scholar]


