Abstract
Context:
Although bloodborne infections are among the most important global health issues, limited data are available on bloodborne infections in athletes.
Objective:
To determine and compare the prevalence of markers of hepatitis B (HBV) and hepatitis C (HCV) viruses and the risk factors for these infections among wrestlers in Tehran and among a control group of athletes in the same geographic area who took part in low- to moderate-contact sports (ie, volleyball and soccer).
Design:
Case-control study.
Setting:
Laboratory.
Patients or Other Participants:
A total of 420 male wrestlers were randomly selected from 28 wrestling clubs in Tehran using a cluster-sample–setting method. The control group (205 volleyball players from 21 clubs and 205 soccer players from 16 clubs) was selected from the same geographic area.
Main Outcome Measure(s):
The risk factors for HBV and HCV and serum levels of anti-HBcAg (antibodies to the HBV core antigen), HBsAg (HBV surface antigen), and anti-HCV (antibodies to HCV) in both groups.
Results:
The prevalence of anti-HBcAg was 13.4% (95% confidence interval [CI] = 10.2%, 16.7%) in wrestlers and 10.9% (95% CI = 7.9%, 14.0%) in the control group. The prevalence of HBsAg was 1.2% (95% CI = 0.2%, 2.2%) in wrestlers and 0.5% (95% CI = −0.2%, 1.2%) in the control group. The prevalence of anti-HCV was 0.5% (95% CI = −0.2%, 1.1%) in wrestlers and 0 in the control group. Some risk factors for bloodborne infections were more common in the wrestlers than in the control group.
Conclusions:
Within the limits of our study, we found no evidence that participation in Tehranian wrestling increased HBV or HCV transmission when compared with transmission in athletes participating in low- to moderate-contact sports. Prevention of bloodborne infections in Tehranian wrestlers should be focused not only on appropriate care for bleeding injuries but also on general risk factors for these conditions.
Keywords: bloodborne infections, communicable diseases, athletes
Key Points.
When compared with athletes in low- to moderate-contact sports such as volleyball and soccer, Tehranian wrestlers demonstrated no greater rates of hepatitis B or hepatitis C virus transmission.
Attention should focus on preventing all bloodborne infections, particularly in athletes who engage in potentially dangerous behaviors, including high-risk sexual activity and sharing razors for shaving.
Bloodborne infections (BBIs) are among the most important health problems in the world.1 Some organizations2 have claimed that BBIs are increasing among athletes and that they create important and complex problems for sports medicine practitioners. Concern exists about the risk of BBIs for athletes in contact and collision sports.
Theoretically, BBIs can be transmitted during sporting activities, from bleeding wounds or the exudative skin injury of an infected athlete to the injured skin or mucous membranes of other athletes.2–8 Case reports9,10 have documented transmission of hepatitis B virus (HBV) during sumo wrestling and American soccer in this way. Although this risk is believed to be low,2–7 it might be higher for athletes in contact and collision sports, especially in combat sports such as wrestling, boxing, and tae kwon do, because of the greater potential risk of bleeding injuries and prolonged close body contact between the athletes in these sports.2,4,11–13
Some authors8,14 have stated that the transmission risks of HBV, followed by hepatitis C virus (HCV), are higher than those for other BBIs in athletes. This is because the concentration of HBV in the blood is higher than the concentrations of agents responsible for other BBIs, and HBV is more stable in the external environment. The risks of transmitting HBV and HCV in the sport setting may also indirectly reveal the risk of transmitting other BBIs. Blood doping and sharing needles or syringes, which may be associated with drug abuse by athletes, also carry the risks of transmitting BBIs.15–17
Requiring testing of athletes for BBIs, vaccinating athletes for HBV, and preventing infected athletes from participating in their sports are controversial topics, especially for players in collision and contact sports. The literature contains only a few case reports.8,15–17 Further epidemiologic research, specifically on high-risk sports such as wrestling and boxing, is needed to evaluate this risk and to help answer some of these questions.
To our knowledge, the prevalence of HBV and HCV markers has not been investigated in the general population of athletes in high-risk sports such as wrestling. Prevalence of HBV and HCV carriers in an athletic population might affect the potential risk of transmission of these infections in that sport and geographic region.
Data on the known risk factors for BBIs in athletic populations (eg, unsafe sexual practices) are scarce and controversial.8 A better understanding of the prevalence of these factors in athletes is needed in order to develop preventive measures. The few published studies2–7,18,19 in this field are mainly case reports, the opinions of experts, and consensus statements. Thus, the objectives of our study were as follows:
To determine the prevalence of HBV markers (ie, antibodies to the hepatitis B core antigen [anti-HBcAg] and antibodies to the hepatitis B surface antigen [HBsAg]) and HCV markers (ie, antibodies to HCV [anti-HCV]) among Tehranian wrestlers and a control group of athletes who took part in low- to moderate-contact sports (ie, volleyball and soccer) in the same geographic area.
To compare any differences in prevalence between these groups. The null hypothesis was “The prevalences of wrestlers ‘ever infected’ with HBV (ie, positive for anti-HBcAg) and ‘ever infected' with HCV (ie, positive for anti-HCV) are similar to those of athletes in low- to moderate-contact sports (ie, volleyball and soccer) in Tehran.”
METHODS
This study was a population-based case-control study. A total of 420 male wrestlers were randomly selected from 28 clubs in Tehran using a cluster-sample–setting method. The city of Tehran was divided into 4 zones based on geography and sociocultural factors such as levels of income. We randomly selected approximately 30% of the wrestling clubs in each of the 4 zones and then approximately 15% of the wrestlers training in each club (Table 1).
Table 1.
Wrestling Clubs in Tehran, Iran, and Area Sport Clubs Randomly Selected for Study
| Tehran Region | Number of Clubs | Number of Selected Clubs |
| Northeast | 14 | 4 |
| Northwest | 21 | 6 |
| Southeast | 29 | 9 |
| Southwest | 31 | 9 |
| Total | 95 | 28 |
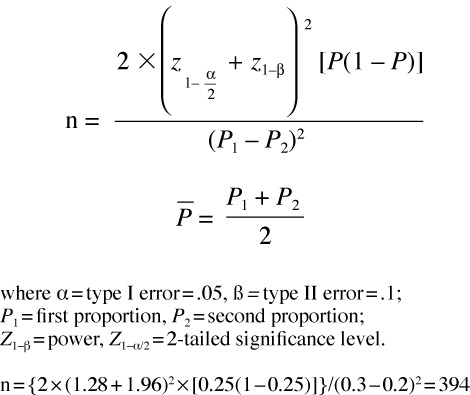
Required sample size was calculated based on the prevalence of HBV markers in Iranians. The following equation has been recommended for the calculation of sample size in a case-control study.20 Based on this equation, we calculated the necessary sample size as 394 participants in each group.
 |
The control group consisted of 205 male volleyball players selected from 21 clubs and 205 male soccer players selected from 16 clubs; both clubs were in Tehran. Volleyball (a low-contact sport) and soccer (a moderate-contact sport) are both popular activities in Iran. When the chosen sport center had wrestling, volleyball, and soccer clubs, we randomly selected participants from these clubs. When the selected sport center had no volleyball or soccer club, we randomly selected athletes from the nearest sport centers that did have volleyball and soccer clubs.
Inclusion criteria were (1) being a member of a wrestling, volleyball, or soccer club in Tehran with at least 1 year of experience training for the sport, (2) not being previously vaccinated against HBV, (3) not participating in both wrestling and a noncontact sport (ie, volleyball or soccer), and (4) age less than 25 years old. Participation in the study was voluntary. The aims and protocol of the research were described to the athletes, who provided verbal consent. The study was approved by the Ethical Committee of the Tehran University of Medical Sciences.
A blood sample was taken from each participant. The samples were sent to the central laboratory of the Iranian Blood Transfusion Organization in Tehran, which is well equipped and one of the highest-quality laboratories in this area of the Middle East. Sera of both wrestlers and control participants were tested for HBsAg, anti-HBcAg and anti-HCV.
To test for anti-HCV, an enzyme immunoassay test was conducted on the sera from all participants. Positive results for anti-HCV were retested using supplemental testing with recombinant immunoblot assay. The finding was considered positive for anti-HCV when both tests were positive.
Prevalence of risk factors for transmission of HBV and HCV in all participants was investigated with 2 questionnaires (nonconfidential and confidential) that were designed based on published data in this field2,4,6,8,21,22 and our interview with experts in Iran.
We conducted a test-retest pilot study of the nonconfidential questionnaire on 40 wrestlers in 2 clubs in Tehran. The average reliability coefficients for the questionnaire were ϰ = 0.98 (range, 0.93 to 1.0) and intraclass correlation coefficient = 0.98 (range, 0.93 to 0.99). Reliability of an instrument is considered high when the reliability coefficient is ≥0.9.23 Therefore, these data suggest that the questionnaire is reliable.
The nonconfidential questionnaire was designed to be completed by interviewers. This questionnaire collected information on risk factors for transmission of HBV and HCV, including a history of receiving a blood transfusion, sharing razors for shaving, sharing needles or syringes for injection, sharing needles or syringes to inject doping drugs, family history of HBV or HCV, living with a person with HBV or HCV, having a tattoo, undergoing major surgery, and performing hejamat (a traditional treatment in Iran that involves cupping and bloodletting; a description is provided in the “Results” section). We developed a confidential questionnaire to address sensitive issues such as sexual activity and sharing of needles or syringes to inject doping drugs. The participants were given further explanation about the objectives of the research and the confidential nature of the questionnaire. Then each was given a pen and a questionnaire and asked to fill out the questionnaire and place it in a box. We emphasized that the participant must not write his name or any identifying information on the questionnaire. Our pilot study suggested that this method was appropriate to investigate these sensitive questions.
Vaccination of all children against HBV has been part of the national vaccination program in Iran for 12 years.21 However, wrestlers are generally older than 12. The results of our pilot study suggested that only 2.5% (1/40) of our wrestlers were vaccinated against HBV. Our pilot study and a review of the list of wrestlers in 5 clubs indicated that most of the wrestlers in Tehran were less than 25 years old. In each club, a few wrestlers were between 25 and 55 years. To ensure a more homogeneous group of participants, we limited age to less than 25 years.
Iran is an appropriate country for conducting this type of research because the prevalence of HBV carriers (ie, those with positive HBsAg tests) is moderate at 1.7% to 3.6%.21,24–26 According to Zali et al,24 approximately half of the HBV infections in the general population of Iran occurred between the ages of 10 and 50 years. In countries with moderate endemicity, the prevalence of HBV active disease carriers is high (3% in Iran),24 and transmission can occur during youth and adulthood because of the high percentage of uninfected youths and adults: 65% of the population in Iran was uninfected.21,24 In countries with high endemicity of HBV (more than 8% carriers in the population), most people are infected during childhood,22 and so transmission during adulthood is less likely. In countries with low endemicity (fewer than 2% carriers in the population), transmission during adulthood is a major avenue of infection, but the risk is low because of the low percentage of carriers. Therefore, conducting our research in countries with a high incidence of HBV was not practical because too large a sample size would have been needed.
RESULTS
Blood samples were taken from 420 wrestlers and 410 control participants (205 volleyball players, 205 soccer players). All participants completed both questionnaires.
Participant Characteristics
The age of the participants was 18.4 ± 2.8 years (95% confidence interval [CI] = 18.2, 18.7; range, 13 to 25 years) for the wrestlers and 16.9 ± 2.2 years (95% CI = 16.7, 17.1; range, 14 to 25 years) for the control group. The wrestlers had 3.4 ± 2.5 years of sport training (range, 1 to 16 years). The control group had 3.2 ± 2.2 years of sport training (range, 1 to 10 years). Only 2.5% (n = 11) of the wrestlers and 1% (n = 4) of the control group were married. Most of the wrestlers (81%, n = 340) and the control group (74%, n = 303) were born in Tehran. The majority of the wrestlers (62%, n = 260) and the control group (87%, n = 357) were students.
Serologic Markers
The cumulative prevalence of HBV infection (ie, “all those who have been in a disease state during their lives”27 = all those positive for anti-HBcAg = all those who have been infected with HBV) among wrestlers was 13.4% (95% CI = 10.2%, 16.7%) and in the control group was 10.9% (95% CI = 7.9%, 14.0%) (Table 2). The difference in cumulative prevalence of HBV infection between the wrestlers and the control group was not significant.
Table 2.
Hepatitis B and Hepatitis C Serologic Markers in Wrestlers and the Control Group
| Serologic Marker | Group | Subgroup | Positive Result, No. (%) | 95% Confidence Interval |
| Anti-HBcAg (antibodies to hepatitis B core antigen) | Wrestlers | 13.4 | 10.2, 16.9 | |
| Control group | 10.9 | 7.9, 14.0 | ||
| Volleyball players | 7.8 | 4.9, 12.3 | ||
| Soccer players | 14.1 | 10.0, 19.6 | ||
| HBsAg (hepatitis B surface antigens) | Wrestlers | 1.2 | 0.5, 2.7 | |
| Control group | 0.5 | 0.1, 1.8 | ||
| Volleyball players | 0 | 0, 1.8 | ||
| Soccer players | 1.0 | 0.3, 3.5 | ||
| Anti-HCV (antibodies to hepatitis C) | Wrestlers | 0.5 | 0.1, 1.7 | |
| Control group | 0 | 0, 0.9 | ||
| Volleyball players | 0 | 0, 1.8 | ||
| Soccer players | 0 | 0, 1.8 |
The risk ratio (ie, ratio of the prevalence of disease in 2 population groups27) for being positive for anti-HBcAg (ie, cumulative prevalence of HBV) in wrestlers compared with the control group was 1.2 (95% CI = 0.7, 2.1). The prevalence of being HBsAg positive in wrestlers (1.2) was 2.4 times as high as in the control group (0.5). However, this difference was not significant.
The cumulative prevalence of HCV infection was 0.5% (95% CI = 0.1%, 1.7%) in the wrestlers and 0% (95% CI = 0%, 0.9%) in the control group.
Risk Factors for HBV and HCV
Common risk factors for BBIs in wrestlers were high-risk sexual activity (24.3% [n = 102] of wrestlers), undergoing major surgery (13.6% [n = 57] of wrestlers), and sharing razors for shaving (11.9% [n = 50] of wrestlers) (Table 3). In the control group, common risk factors for BBIs were sharing razors for shaving (18.8% [n = 77]), high-risk sexual activity (15.8% [n = 65]), and undergoing major surgery (13.7% [n = 56]).
Table 3.
Risk Factors for Hepatitis B and Hepatitis C in Wrestlers and Control Groups
| Risk Factor | Wrestlers |
Control Group |
||
| % | 95% Confidence Interval | % | 95% Confidence Interval | |
| High-risk sexual activitya,b,c | 24.3 | 20.2, 28.4 | 15.8 | 12.3, 19.3 |
| Blood transfusion | 2.1 | 0.68, 3.52 | 3 | 1.32, 4.68 |
| Sharing razors for shaving | 11.9 | 8.68, 15.12 | 18.8 | 14.94, 22.66 |
| Sharing needles or syringes for injection | 2.1 | 0.68, 3.52 | 1 | 0.4, 2.5 |
| Sharing needles or syringes for doping b | 1.8 | 0.5, 3.1 | 1 | 0.4, 2.5 |
| Family history of hepatitis B | 1.4 | 0.23, 2.57 | 1.8 | 0.49, 3.11 |
| Family history of hepatitis C | 2.2 | 0.74, 3.66 | 1 | 0.4, 2.5 |
| Living with a person with hepatitis B or C | 0.8 | 0.2, 2.0 | 1.1 | 0.07, 2.13 |
| Tattoo | 2.8 | 1.16, 4.44 | 0.8 | 0.2, 2.1 |
| Hejamatc,d | 11.4 | 8.24, 14.56 | 4.2 | 2.22, 6.18 |
| Major surgery | 13.6 | 10.19, 17.01 | 13.7 | 10.30, 17.10 |
| High-risk job (eg, health care worker) | 0.5 | 0.1, 1.7 | 0 | 0.0, 0.9 |
| Doping (during the previous year)b,c | 7 | 4.6, 9.4 | 2.7 | 1.1, 4.3 |
a Extramarital sex or sex with a man.
b Results from confidential questionnaire.
c The difference between wrestlers and the control group is statistically significant (P < .05).
d A traditional treatment in Iran that involves cupping and bloodletting.
Additional BBI risk factors are somewhat unique to the athletes participating in this study. For example, hejamat is a traditional therapy practiced in Iran that involves the use of a glass cup placed on the skin to create a vacuum. After a few minutes, shallow incisions are made to the area of the skin that has been cupped, and bloodletting is induced by replacing the cup after a vacuum has been created. If practitioners share unsterile devices, BBIs and other infections may be transmitted. According to our participants, hejamat had been performed using sterile devices in all of the control group (n = 410) and 98% (n = 412) of the wrestlers. Tattooing was performed using sterile devices in 73% (8 of 11) of wrestlers and 67% (1 of 3) of the control group.
DISCUSSION
The prevalence of HBV markers (ie, anti-HBcAg and HB-sAg) and HCV (ie, anti-HCV) infections in Tehranian wrestlers was not different from that in athletes practicing low- to moderate-contact sports (ie, volleyball and soccer) of the same sex and the same geographic area. The risk of being previously infected with HBV (ie, positive for anti-HBcAg) in wrestlers was slightly higher (risk ratio = 1.2) than in the control group, but this difference was not significant.
On average, the wrestlers were 1.5 years older than the control group (mean = 18.4, 95% CI = 18.2, 18.7 for wrestlers, mean = 16.9, 95% CI = 16.7, 17.1 for the control group). However, this small difference in age could result in a slightly higher prevalence of serologic markers in our wrestlers than in the control group.
In Iran, the prevalence of hepatitis B carriers (ie, being HB-sAg positive) in the 10- to 29-year age group is reported to be 1.5% to 1.6%, and it is 1.3% to 1.4% among students.24 Most of the wrestlers (62%) in our study were students, and the prevalence of being HBsAg positive among wrestlers in this study was 1.2%. Therefore, the likelihood of a wrestler in Tehran being an HBV carrier was no more than in the general Iranian population of the same age range.
The limited data available indicate that the prevalence of HCV infections in the general population of Iran was 0.12% to 0.5%.25,26,28 The prevalence of HCV infection was quite high in high-risk groups such as injected-drug users (60% to 90%), hemophiliacs (50% to 70%), and hemodialysis patients (15% to 60%).29 Our results suggest that the prevalence of anti-HCV in Tehranian wrestlers was 0.5%. Thus, the likelihood of wrestlers being HCV carriers in Tehran, as in the case of HBV, was no more than in the general Iranian population and far less than in high-risk groups.
The prevalences of most known risk factors for HBV and HCV transmission in Tehranian wrestlers were not detectably different from those of athletes participating in low- to moderate-contact sports (ie, volleyball and soccer) of the same sex and in the same geographic area. However, participating in unsafe sexual activity, doping, and undergoing hejamat were more common practices in wrestlers than in the control group.
Hejamat was relatively common among our wrestlers (11%). Those who performed hejamat were considered to be at high risk for BBIs by the Iranian Blood Transfusion Organization,30 either because of the possibility of using unsterile instruments or because of the low sociocultural and financial levels of these people. In Iran, hejamat is offered both by general practitioners in clinics that use disposable sterile equipment and by traditional therapists, who may or may not use disposable sterile equipment. Sterile devices were used for all of the control group who underwent hejamat and for 98% of the wrestlers who did so. Therefore, hejamat is unlikely to be a major risk factor for BBIs in wrestlers in Tehran.
Sharing razors for shaving was common among participants in this study (12% in wrestlers, 19% in the control group). Therefore, it is clear that both the wrestlers and the control group needed to be educated in the modes of BBIs transmission, including sharing razors.
Sharing needles or syringes to inject doping drugs was rare (2% [n = 8] in wrestlers and 1% [n = 4] in the control group). Syringes and needles are cheap and can be purchased from pharmacies without prescription. Therefore, sharing probably resulted from ignorance rather than need, and this behavior should be addressed by an appropriate educational program.
Our data suggest that at least 7% (n = 29) of the general population of wrestlers in Tehran undertook doping in the year before the study, a percentage that is significantly higher than that of volleyball and football players in the same area (3%, n = 12). This figure is especially notable because most of these wrestlers were not highly competitive athletes. We did not investigate age, level of performance, or type of abused drug in these athletes. More research and preventive measures are needed.
High-risk sexual activity was a common risk factor among both wrestlers and the control group but more common among the former. Limited and controversial evidence on high-risk sexual activities among athletes is available in the literature. However, some high-risk sexual activities might be more common among male athletes than nonathletes, and athletes may be more sexually active,31 practice less safe sex,32,33 have more sexually transmitted diseases,34 and have a greater number of sexual partners.32–34 More investigation is needed to help us elucidate the relationship between high-risk sexual activity and sports, including wrestling. Regarding sexual activity, preventive plans should focus on the ABC strategy35:
Abstain and delay sexual initiation.
Be safer by Being faithful or reducing the number of sexual partners.
Use Condoms Correctly and Consistently.
Sports have been categorized as high, moderate, or low risk for BBIs based on the potential risk of bleeding injuries and body contact.2,4,11,12 Globally, the most common method of HBV transmission during adulthood is heterosexual contact with an infected partner (because this exposure occurs most often), followed by injected-drug abuse and then homosexual contact. 22,36 Therefore, the main methods of transmission of BBIs in athletes are probably not associated with sporting activity but similar to those for the general population, such as unsafe sexual activity and sharing needles. 2,3,37,38 High risk for BBIs might be determined based not on the risk of bleeding injuries in a given sport but on the prevalence of these high-risk behaviors that are related to other factors, such as sociocultural factors and pressures within sports to abuse injected drugs. According to our limited data, when compared with volleyball and soccer players in the same area, Tehranian wrestlers were at greater risk for BBIs because of the prevalence of unsafe sexual activity.
CONCLUSIONS
We found no evidence that wrestlers in Tehran had higher HBV or HCV transmission rates than athletes in low- to moderate- contact sports (ie, volleyball, soccer) of the same sex and in the same geographic area. Therefore, preventive measures, such as screening of Tehranian wrestlers for HBV and HCV, do not seem justified. Vaccination of wrestlers might be justified to provide personal protection, but transmission of HBV and HCV does not appear to pose a major public health problem in Tehranian wrestlers.
Athletes should be classified by their level of risk for BBI based on the rates of bleeding injures and other risk factors, such as unsafe sexual activities and sharing needles and syringes. Prevention of BBIs in Tehranian wrestlers should focus on general risk factors for BBIs, especially high-risk sexual activity and the sharing of razors for shaving. However, appropriate care of bleeding injuries could also be beneficial to reduce the transmission risk of BBIs, even though this rarely occurs.
More studies are needed to investigate the prevalence and risk of transmission of BBIs in other high-risk athletes, both those who are at high risk because of a large number of bleeding injuries, such as boxers, and those who are high risk because of other factors for BBIs, such as sexual activity and sharing needles for doping. More study is needed to investigate the rate of risk factors for BBIs, including unsafe sexual activity in athletes of different sports.
Acknowledgments
The Iranian Blood Transfusion Organization, a nonprofit government network of blood centers in Iran, funded this study. The Sports Medicine Research Centre of the Tehran University of Medical Sciences also provided support.
REFERENCES
- 1.World Health Organization. HIV/AIDS. http://www.who.int/hiv/en/. Accessed November 28, 2003.
- 2.American Medical Society for Sports Medicine and the American Orthopaedic Society for Sports Medicine. Human immunodeficiency virus (HIV) and other blood-borne pathogens in sports. http://www.amssm.org/hiv.html. Accessed November 25, 2003.
- 3.Centers for Disease Control and Prevention. National AIDS Clearinghouse. HIV/AIDS and sports. http://www.caps.ucsf.edu/toolbox/HIV&sports.html. Accessed November 25, 2003.
- 4.Committee on Sports Medicine and Fitness. American Academy of Pediatrics. Human immunodeficiency virus and other. blood-borne viral pathogens in the athletic setting. Pediatrics. 1999;104(6):1400–1403. doi: 10.1542/peds.104.6.1400. [DOI] [PubMed] [Google Scholar]
- 5.Robinson J. Position statement: HIV as it relates to sport, February 1994. Canadian Academy of Sports Medicine. http://www.casm-acms.org/. Accessed November 18, 2003.
- 6.International Federation of Sports Medicine. AIDS and sports: FIMS position statement. http://www.fims.org/fims/frames.asp. Accessed November 25, 2003.
- 7.Mast EE, Goodman RA, Bond WW, Favero MS, Drotman DP. Transmission of blood-borne pathogens during sports: risk and prevention. Ann Intern Med. 1995;122(4):283–285. doi: 10.7326/0003-4819-122-4-199502150-00008. [DOI] [PubMed] [Google Scholar]
- 8.Kordi R, Wallace WA. Blood borne infections in sport: risks of transmission, methods of prevention, and recommendations for hepatitis B vaccination. Br J Sports Med. 2004;38(6):678–684. doi: 10.1136/bjsm.2004.011643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kashiwagi S, Hayashi J, Ikematsu H, Nishigori S, Ishihara K, Kaji M. An outbreak of hepatitis B in members of a high school sumo wrestling club. JAMA. 1982;248(2):213–214. [PubMed] [Google Scholar]
- 10.Tobe K, Matsuura K, Ogura T. Horizontal transmission of hepatitis B virus among players of an American football team. Arch Intern Med. 2000;160(16):2541–2545. doi: 10.1001/archinte.160.16.2541. et al. [DOI] [PubMed] [Google Scholar]
- 11.National Collegiate Athletic Association. 2003–04 NCAA Sports Medicine Handbook. http://www.ncaa.org/library/sports_sciences/sports_med_handbook/2003-04/index.html. Accessed November 18, 2003.
- 12.Goldsmith MF. When sports and HIV share the bill: smart money goes on common sense. JAMA. 1992;267(10):1311–1314. [PubMed] [Google Scholar]
- 13.Bereket-Yucel S. Risk of hepatitis B infections in Olympic wrestling. Br J Sports Med. 2007;41(5):306–310. doi: 10.1136/bjsm.2006.032847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGrew CA. Blood-borne pathogens and sports. In: Fields KB, Fricker PA, editors. Medical Problems in Athletes. Malden, MA: Oxford: Blackwell Science; 1997. pp. 64–69. [Google Scholar]
- 15.Henrion R, Mandelbrot L, Delfieu D. [HIV contamination after injections of anabolic steroids] Presse Med. 1992;21(5):218. [PubMed] [Google Scholar]
- 16.Rich JD, Dickinson BP, Merriman NA, Flanigan TP. Hepatitis C virus infection related to anabolic-androgenic steroid injection in a recreational weight lifter. Am J Gastroenterol. 1998;93(9):1598. doi: 10.1111/j.1572-0241.1998.01598.x. [DOI] [PubMed] [Google Scholar]
- 17.Sklarek HM, Mantovani RP, Erens E, Heisler D, Niederman MS, Fein AM. AIDS in a bodybuilder using anabolic steroids. N Engl J Med. 1984;311(26):1701. doi: 10.1056/NEJM198412273112615. [DOI] [PubMed] [Google Scholar]
- 18.Siebert DJ, Lindschau PB, Burrell CJ. Lack of evidence for significant hepatitis B transmission in Australian rules footballers. Med J Aust. 1995;162(6):312–313. doi: 10.5694/j.1326-5377.1995.tb139908.x. [DOI] [PubMed] [Google Scholar]
- 19.Hamilton BH, Paoloni JA, Chalabi H. Epidemiology of hepatitis B among professional male athletes in Qatar. Saudi Med J. 2010;31(6):678–683. [PubMed] [Google Scholar]
- 20.Bashardoust N. Sample setting and sample size. In: Malecafzali H, Majdzadeh SR, Fotohi A, Tavakoli S, editors. Methodology of Practical Research in Medical Sciences. Tehran, Iran: Tehran University of Medical Sciences Publishing; 2004. pp. 297–316. [Google Scholar]
- 21.Malekzadeh R, Khatibian M, Resvan H. Viral hepatitis in the world and Iran. J Med Counc Islam Republic Iran. 1997;15:188–200. [Google Scholar]
- 22.World Health Organization. Hepatitis B. http://www.who.int/emc. Accessed December 11, 2003.
- 23.Hopkins W. A new view of statistics. http://www.sportsci.org/resource/stats/index.html. Accessed May 4, 2004.
- 24.Zali MR, Mohammad K, Farhadi A, Masjedi MR, Zargar A, Nowroozi A. Epidemiology of hepatitis B in the Islamic Republic of Iran. East Mediterr Health J. 1996;2(2):290–298. [Google Scholar]
- 25.Alizadeh AH, Alavian SM, Jafari K, Yazdi N. Prevalence of hepatitis C virus infection and its related risk factors in drug abuser prisoners in Hamedan: Iran. World J Gastroenterol. 2005;11(26):4085–4089. doi: 10.3748/wjg.v11.i26.4085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghavanini AA, Sabri MR. Hepatitis B surface antigen and anti-hepatitis C antibodies among blood donors in the Islamic Republic of Iran. East Mediterr Health J. 2000;6(5–6):1114–1116. [PubMed] [Google Scholar]
- 27.Silman AJ, Macfarlane GJ. Epidemiological Studies: A Practical Guide. 2nd ed. Cambridge, UK: Cambridge University Press; 2002. p. xiv.p. 241. [Google Scholar]
- 28.Ansar MM, Kooloobandi A. Prevalence of hepatitis C virus infection in thalassemia and haemodialysis patients in north Iran– Rasht. J Viral Hepat. 2002;9(5):390–392. doi: 10.1046/j.1365-2893.2002.00368.x. [DOI] [PubMed] [Google Scholar]
- 29.Kew M, Francois G, Lavanchy D. Prevention of hepatitis C virus infection. J Viral Hepat. 2004;11(3):198–205. doi: 10.1111/j.1365-2893.2004.00492.x. et al. [DOI] [PubMed] [Google Scholar]
- 30.Iranian Blood Transfusion Organization. Hejamat. http://www.ibto.ir/. Accessed February 3, 2006.
- 31.Trost SG, Levin S, Pate RR. Sport, physical activity and other health behaviours in children and adolescents. In: Armstrong N, Van Mechelen W, editors. Paediatric Exercise Science and Medicine. Oxford, UK: Oxford University Press; 2000. pp. 295–310. [Google Scholar]
- 32.Wetherill RR, Fromme K. Alcohol use, sexual activity, and perceived risk in high school athletes and non-athletes. J Adolesc Health. 2007;41(3):294–301. doi: 10.1016/j.jadohealth.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nattiv A, Puffer JC, Green GA. Lifestyles and health risks of collegiate athletes: a multi-center study. Clin J Sport Med. 1997;7(4):262–272. doi: 10.1097/00042752-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Nattiv A, Puffer JC. Lifestyles and health risks of collegiate athletes. J Fam Pract. 1991;33(6):585–590. [PubMed] [Google Scholar]
- 35.Joint United Nations Programme on HIV/AIDS. 2004 report on the global HIV/AIDS epidemic: 4th global report. http://www.unaids.org. Accessed March 1, 2005. [PubMed]
- 36.Harrington DW. Viral hepatitis and exercise. Med Sci Sports Exerc. 2000;32(7 suppl):S422–430. doi: 10.1097/00005768-200007001-00007. [DOI] [PubMed] [Google Scholar]
- 37.National Collegiate Athletic Association. Wrestling, 2004 Rules and Interpretations. Indianapolis, IN: National Collegiate Athletic Association; 2003. [Google Scholar]
- 38.Passos AD, Figueiredo JF, Martinelli Ade L, Villanova M, Nascimento MM, Secaf M. Hepatitis C among former athletes: association with the use of injectable stimulants in the past. Mem Inst Oswaldo Cruz. 2008;103(8):809–812. doi: 10.1590/s0074-02762008000800011. [DOI] [PubMed] [Google Scholar]


