Abstract
We examined the relationship between personality pathology and the frequency of self-reported psychological and physical partner aggression in a community sample of 872 adults aged 55–64. Previous research suggests that antisocial and borderline personality disorder (PD) symptoms are associated with partner aggression. Controlling for gender, education, alcohol dependence, and other personality pathology, we found that borderline PD symptoms, which include abandonment fears, unstable identity, and affective instability, were significantly related to the frequency of self-reported aggression towards one’s partner. This relationship was observed regardless of whether the participant’s personality was described by a clinical interviewer, the participant themselves, or an informant chosen by the participant. Further, the relationship between borderline PD symptoms and self-reported partner aggression was moderated by gender such that women were driving the association. Conversely, antisocial PD symptoms, which include deceitfulness, irresponsibility, disregard for rules, and lack of remorse did not significantly account for variance in self-reported partner aggression.
Partner aggression in romantic relationships is a troubling yet common phenomenon. Aggressive episodes are often classified as psychological (e.g., shouting, stomping out of the room) or physical (e.g., punching or slapping; Straus, Hamby, Boney-McCoy, & Sugarman, 1996). In a study of 18 US states, 17% of surveyed participants indicated that they had been physically hurt by an intimate partner (Breiding, Black, & Ryan, 2008), whereas over 90% of participants in O’Leary and Slep’s (2006) study reported mild psychological aggression. Although the repercussions of physical aggression can be more devastating, physical and psychological aggression tend to co-occur (e.g., O’Leary, 1999).
Clinical researchers have attempted to identify types of people more prone to partner aggression. Borderline and antisocial personality disorders (PDs) have often been linked to this type of violence (e.g., Dutton & Starzomski, 1993; Holtzworth-Munroe & Stuart, 1994; Mauricio, Tein, & Lopez, 2007). One feature common to borderline and antisocial PDs is impulsivity, which could be partially responsible for partner aggression. Otherwise, borderline and antisocial symptoms probably drive partner violence for different reasons. Borderline symptoms include identity disturbance, disproportionate anger, and fear of abandonment; antisocial symptoms include lack of empathy and remorse, irresponsibility, reckless disregard for the safety of self and others, and a general tendency toward irritability and aggression. Hence, it has been theorized that those with borderline symptoms may perpetrate partner violence due to insecure attachment (e.g., Dutton, Saunders, Starzomski, & Bartholomew, 1994), whereas those with antisocial symptoms might behave in these ways as a consequence of generalized hostility (Holtzworth-Munroe, 2000). Epidemiological studies report a steady decline of partner aggression with age. Despite this decline partner aggression still occurs later in life. A longitudinal study examining middle-aged couples at three yearly time points (Vickerman & Margolin, 2008) found only a small decrease in physical aggression, with no evidence of a decrease in psychological aggression. Similarly, in Pan, Neidig, and O’Leary’s (1994) study of 11,870 White males, age was not a factor in distinguishing between mild and moderate aggression. Conversely, lower levels of education (Cascardi, Langhinrichsen, & Vivian, 1992) and excessive alcohol consumption (Fals-Stewart, 2003; Pan et al., 1994) have consistently been shown to increase episodes of partner aggression.
Partner aggression may decline with age in part because some risk factors (in particular, personality pathology and alcohol use) also fade. The specific features of antisocial and borderline PD seem to decrease in frequency as people get older (Grant et al., 2008; Ullrich & Coid, 2009). Nevertheless, symptoms of these disorders continue to produce impairments later in life. In a sample of borderline patients aged 18 to 52, the only symptom significantly predicted by age was impulsivity (Stevenson, Meares, & Comerford, 2003). Although there is ample evidence that both personality pathology presentation and patterns of partner aggression change across the lifespan, the relationship between personality pathology and partner aggression in older samples has not been systematically investigated. In our study, we examine the relationship between personality disorder symptoms and partner aggression in a late middle-aged community sample adjusting for alcohol use and level of education.
Methods
Participants
Participants aged 55–64 (57% female) were recruited for a longitudinal study of personality and aging (the St. Louis Personality and Aging Network; see Oltmanns & Gleason, 2011). The 1,630 participants were recruited for this study using listed phone numbers crossed with census data, and form a representative community sample from the St. Louis area (both city and suburbs). All data reported in this paper are taken from the baseline assessment, which included a 2-hour interview as well as a battery of questionnaires. Of all the recruited participants, 981 were in a relationship with a partner at the time of the baseline assessment and thus eligible for the analyses reported in this paper. Subsequently, 7 participants were excluded because they did not complete the partner aggression scale; 13 were excluded because they did not complete the self-assessment of their own personality; and 89 were excluded because they did not have an informant complete an assessment of their personality. We used data from the remaining 872 participants in our analyses (89% of eligible participants). Spouses/romantic partners comprised the largest percentage of these participants’ informants (n = 666, or 76%); other informants were family members, friends, or colleagues.
Males made up 57% of the sample (n = 500), and mean age was 59.5 (SD = 2.7). Most of the participants (679, or 78%) were currently married to their romantic partners, for an average of 27.0 years (SD = 11.1). The racial distribution of the participants reflects that of the greater St. Louis metropolitan area: 71% White/Caucasian (n = 623), 26% Black/African (n = 229), 0.9% Hispanic/Latino (n = 8), and 1.4% from other racial backgrounds (n = 12). Educational achievement varied in the sample: 28% (n = 248) had a high school education or less; 16% (n = 136) had education beyond high school, but not a bachelor degree; 25% (n = 215) had completed a bachelor degree; and 31% (n = 273) had a master’s degree or higher. Median household income was between $60,000 and $79,000, with 18% of households below $40,000 and 20% above $140,000 (32 participants declined to answer).
Measures
Partner Aggression
Self-reported aggression against one’s partner (hereafter referred to as partner aggression) was measured by the 4 psychological aggression events (e.g., “Shouted at partner”) and 9 physical aggression events (e.g., “Beat up partner”) with the highest reliability scores from the Conflict Tactics Scale (Straus et al., 1996). For each question, participants selected one of 8 categorical options regarding the frequency with which each event occurred in the last 12 months. Responses were translated to frequencies indicating the number of times each event had occurred in the past 12 months (frequencies in parentheses): once in the past year (1); twice in the past year (2); 3–5 times in the past year (4); 6–10 times in the past year (8); 11–20 times in the past year (15); more than 20 times in the past year (25); not in the past year, but it did happen before (0); this has never happened (0). The resulting scores were summed across all 13 items to create a self-reported partner aggression frequency variable with a possible range of 0–325; this was used as the dependent variable in the analyses.
Covariates
Gender, education, and alcohol dependence were used as covariates in the regressions. Gender was centered such that male was coded as 0.5 and female as −0.5. For education, participants were asked their highest education degree/certificate. The 9 categorical response options were transformed to a continuous variable with a possible range of 6.5–20 years of education. Response options were as follows (years of education in parentheses): Elementary or Junior High (6.5); GED (12); H.S. Diploma (12); Vocational Tech Degree (14); Associate Degree (14); R.N. Diploma (15); Bachelor Degree (16); Master Degree (18); and Doctorate: M.D., Ph.D., J.D., etc (20).
For alcohol dependence, participants were asked seven yes/no questions about their alcohol usage over the past 12 months, as part of the Mini-international Neuropsychiatric Interview (Sheehan et al., 1998). A score of 3 or more “yes” responses on this scale indicates alcohol dependence. The total number of “yes” responses formed a continuous alcohol dependence variable with a possible range of 0–7. The majority of the sample (732 or 83.9% of participants) did not report any recent alcohol dependence symptoms; 25 (2.9%) qualified for alcohol dependence by reporting at least 3 of the 7 symptoms in the past 12 months. A further 115 (13.2%) reported one or two alcohol dependency characteristics, but did not qualify as dependent on alcohol. On the continuous 0–7 scale, the mean was 0.28 (SD = 0.77). Years of education and alcohol dependence scores were both centered around zero.
Personality Measures
Symptoms of personality disorders were assessed from three sources: an interviewer, the participant themselves, and an informant selected by the participant. Trained interviewers administered the Structured Interview for DSM-IV Personality (SIDP), a semi-structured diagnostic interview that assesses 11 major types of personality disorder (paranoid, schizoid, schizotypal, antisocial, borderline, histrionic, narcissistic, avoidant, dependent, obsessive-compulsive, and passive-aggressive). Participants were rated for each of 7–9 criteria per disorder, on a 4-point scale from 0 (not present) to 3 (strongly present). For each disorder, we summed all responses made on this 4-point scale and divided this sum by the number of criteria assessed for that disorder, to make a scaled score. These scaled scores were calculated for each participant, so that each participant had a scaled score (where 3 was the highest possible score) for each of the 11 personality disorders. The antisocial and borderline portions of the interview each included one criterion concerned specifically with aggression; we excluded these criteria from the scaled score calculations, so that any relationship we found between these disorders and partner aggression could not be attributed to overlap in the assessment measures. This was an especially important precaution given that the partner aggression questionnaire was embedded in the personality interview (see Tables 3 and 4 for analyses that include these criteria).
Table 3.
Regression coefficients for three regressions with partner aggression (frequency of reported events for the last 12 months) as the DV and personality disorder scores from three different sources as the IVs. The intercept represents the frequency of partner aggression predicted for the average participant in the sample as all variables were either effect coded (gender) or centered (PD scores, years of education, and alcohol dependence). Antisocial and Borderline PD scores include the aggression criteria that were omitted from the regressions reported in Table 2.
| SIDP (b) | Self-MAPP (b) | Inf-MAPP (b) | |
|---|---|---|---|
| R2 | .15 | .10 | .12 |
|
| |||
| Intercept | 10.35 | 10.44 | 10.36 |
| Gender | −4.11** | −5.29** | −4.31** |
| Years of education | −0.60** | −0.65** | −0.60** |
| Alcohol dependence | 1.79* | 2.69** | 2.38** |
|
| |||
| Antisocial | 1.60 | 2.47 | 2.37 |
| Borderline | 22.63** | 7.63** | 6.13** |
| Histrionic | 2.02 | −0.36 | 0.32 |
| Narcissistic | −0.27 | −1.36 | −0.89 |
p < .05;
p < .005;
Table 4.
Regression coefficients for three regressions with partner aggression (frequency of reported events for the last 12 months) as the DV and personality disorder scores from three different sources as the IVs. The intercept represents the frequency of partner aggression predicted for the average participant in the sample as all variables were either effect coded (gender) or centered (PD scores, years of education, and alcohol dependence).
| SIDP (b) | Self-MAPP (b) | Inf-MAPP (b) | |
|---|---|---|---|
| R2 | .14 | .11 | .13 |
|
| |||
| Intercept | 10.35 | 10.43 | 10.37 |
| Gender | −4.08** | −5.27** | −4.44** |
| Years of education | −0.67** | −0.63** | −0.50** |
| Alcohol dependence | 1.95** | 2.75** | 2.44** |
|
| |||
| Paranoid | −1.70 | 0.16 | 1.24 |
| Schizoid | −1.03 | 0.80 | 0.96 |
| Schizotypal | −3.57 | −2.09 | −0.35 |
| Antisociala | 2.49 | 0.51 | 0.42 |
| Borderlinea | 19.68** | 5.86** | 4.71* |
| Histrionic | 3.23 | 0.29 | 1.11 |
| Narcissistic | 0.29 | −1.28 | −0.71 |
| Obsessive-Compulsive | 1.60 | −0.41 | −2.69* |
| Avoidant | 3.94* | −0.70 | −1.19 |
| Dependent | −5.33 | −1.95 | 0.46 |
| Passive-Aggressive | 6.31* | 5.79** | 2.54 |
p < .05;
p < .005;
One criterion was removed from the scoring of each of these two disorders as it referred explicitly to aggression.
Participants and informants completed the Multi-Source Assessment of Personality Pathology (MAPP; Oltmanns, Turkheimer, & Strauss, 1998), in which each statement relates to one criterion on the SIDP, but worded more colloquially. Participants indicated to what extent each statement applied to them, on a 5-point scale from 0 = I am never like this to 4 = I am always like this. Informants filled out this same questionnaire with the participant’s personality in mind. Scaled scores for each personality disorder were calculated as described above for the SIDP. That is, for each disorder, we summed all responses made on the 5-point scale and divided this sum by the number of criteria assessed for that disorder, to make a scaled score. Self-MAPP and informant-MAPP scaled scores were calculated for each participant, so that each participant had a scaled self- MAPP score and a scaled informant-MAPP score for each of the 11 personality disorders. The antisocial and borderline criteria that directly assessed aggression were also omitted as for the SIDP scaled scores. SIDP and MAPP scaled scores for each disorder were centered around zero.
The range of scaled SIDP scores was 0–1.75 for borderline and 0–2 for antisocial PD (note that the widest possible range is 0–3), with means of 0.09 (SD = 0.18) and 0.06 (SD = 0.18) respectively1. On the participant MAPP, the range of scaled scores was 0–3.13 for borderline and 0–3.33 for antisocial PD, with means of 0.45 (SD = 0.41) and 0.58 (SD = 0.41) respectively (the widest possible range is 0–4). Similarly, on the informant MAPP the range of scaled scores was 0–3.38 for borderline and 0–3.00 for antisocial PD, with means of 0.55 (SD = 0.53) and 0.61 (SD = 0.52) respectively.
Our primary analyses focused on the dramatic PDs in Cluster B of DSM-IV because descriptions of these disorders involve various types of impulsive or aggressive behavior as well as lack of empathy (Warren & South, 2009). Although the validity of this organizational structure has been criticized (Sheets & Craighead, 2007), it does capture a set of inter-related disorders that share common etiological factors (Torgersen et al., 2008).
Results
Prevalence of Partner Aggression
Table 1 presents descriptive statistics for self-reported partner aggression in our sample. Because psychological aggression was reported much more frequently than was physical aggression, each psychological aggression event is listed separately whereas only the overall frequency is shown for physical aggression. Despite the low mean frequency of physical aggression events, at least one participant reported the occurrence of each of the seven physical aggression events.
Table 1.
Frequencies of self-reported psychological and physical partner aggression over a 12-month period.
| Type of partner aggression | Occurrences in last 12 months
|
N of participants with at least 1 occurrence in last 12 months | |
|---|---|---|---|
| Mean | SD | ||
| Shouted at partner | 4.7 | 7.3 | 542 (62.2%) |
| Insulted or swore at partner | 3.0 | 6.1 | 350 (40.1%) |
| Stomped out of room | 1.9 | 4.4 | 315 (36.1%) |
| Threatened to hit/throw something at partner | 0.2 | 2.0 | 21 (2.4%) |
|
| |||
| Psychological aggression total | 9.8 | 15.0 | 650 (74.5%) |
| Physical aggression total | 0.3 | 2.3 | 53 (6.1%) |
|
| |||
| Partner aggression (DV in regressions) | 10.1 | 15.8 | 653 (74.9%) |
Regressions: The Relationship Between Partner Aggression and Cluster B PD Symptoms
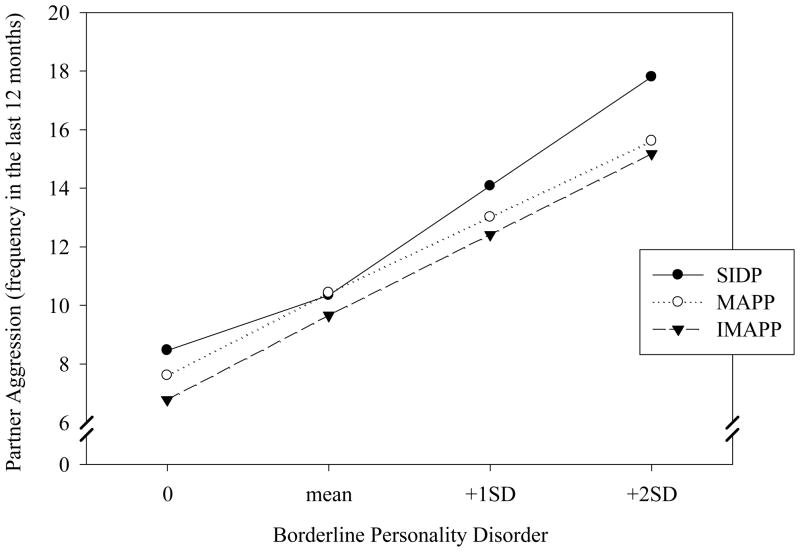
We performed three multiple regressions with self-reported partner aggression frequency over the last 12 months as the dependent variable. The three regressions varied by source of personality assessment (SIDP, participant’s MAPP, and informant’s MAPP). Scaled scores for antisocial PD, borderline PD, histrionic PD, and narcissistic PD from each of these three personality assessments were our predictor variables. All three regressions included the same covariates: gender, years of education, and alcohol dependence over the last 12 months. As can be seen from Table 2, the pattern of results was consistent between the three models. Across all three sources of personality assessment, borderline PD was a significant positive predictor of self-reported partner aggression. Figure 1 shows the predicted frequency of partner aggression in the past year as a function of different levels of borderline pathology, illustrated separately for each source of information (interviewer, self-report, and informant). All three measures produced the same pattern of results. Antisocial PD – the other disorder commonly associated with partner aggression in the literature was not associated with self-reports of partner aggression in any of the three models, nor were histrionic and narcissistic PDs. Note that correlations between the three sources of personality assessment were only moderate (.23–.44 for borderline and .22–.27 for antisocial PD), so each of the three regressions reflects a unique perspective on these problems. Being female, less educated, and more dependent on alcohol also increased the frequency of reported aggression towards one’s partner.
Table 2.
Regression coefficients for three regressions with partner aggression (frequency of reported events for the last 12 months) as the DV and Cluster B disorder scores from three different sources as the IVs. The intercept represents the frequency of partner aggression predicted for the average participant in the sample as all variables were either effect coded (gender) or centered (PD scores, years of education, and alcohol dependence).
| SIDP (b) | Self-MAPP (b) | Inf-MAPP (b) | |
|---|---|---|---|
| R2 | .13 | .09 | .11 |
|
| |||
| Intercept | 10.35 | 10.42 | 10.35 |
| Gender | − 4.10** | − 5.14** | − 4.14** |
| Years of education | −0.63** | − 0.67** | − 0.61** |
| Alcohol dependence | 1.89** | 2.73** | 2.42** |
|
| |||
| Antisociala | 2.53 | 1.20 | 1.60 |
| Borderlinea | 20.15** | 6.32** | 5.19** |
| Histrionic | 2.69 | 0.52 | 1.07 |
| Narcissistic | 0.87 | −0.71 | −0.26 |
p < .05;
p < .005;
One criterion was removed from the scoring of each of these two disorders as it referred explicitly to aggression.
Figure 1.
Predicted number of aggressive events in the past 12 months at each level of borderline pathology, as defined by each of the three personality assessments (SIDP clinical interview, participant’s own assessment, and informant’s assessment using the MAPP). These data relate to the average person in the sample in terms of covariates (gender, education, and alcohol dependence) and severity of other Cluster B disorders.
We also ran two further sets of regressions. The first set is identical to those presented here but includes the explicit aggression items in borderline and antisocial PDs (see Table 3). The results are nearly identical to those reported above: borderline PD is still a significant predictor whereas antisocial PD is not. The second set of regressions includes all DSM-IV forms of PD (see Table 4). These regressions look very similar to those reported above: Including all 11 PDs does not change our overall finding that borderline PD is related to aggressive behaviors. A few other disorders were significantly related to aggression, but these results differ depending on the source of personality assessment (interviewer/participant/informant). In particular, avoidant PD symptoms were positively related to partner aggression, but only when PD symptoms were measured by the SIDP; obsessive-compulsive PD symptoms according to the informant MAPP were negatively related to partner aggression; and passive-aggressive PD symptoms were positively related to partner aggression, on both the SIDP and the participant MAPP. Given lack of a priori hypotheses regarding these PDs and the number of contrasts involved in these analyses, increasing our Type I error rate, we have chosen not to interpret these findings. It is important to note that the inclusion of all disorders does not change the finding that symptoms of borderline PD, regardless of the source, is related to aggressive behavior.
Finally, we also repeated the Cluster B regressions separately for psychological and physical aggression. For psychological aggression results, the direction and significance of the comparisons were the same, but not surprisingly coefficients varied slightly across the analyses. The physical aggression results were also quite similar, with two exceptions. First, there was a significant relationship between antisocial PD symptoms and physical aggression, but only on the informant-MAPP; and second, the relationship between borderline PD symptoms and partner aggression was significant for two out of three sources but was at p = .11 on the self-MAPP. To check for multicollinearity, we calculated variance inflation for each variable in each regression. No variables had a variance inflation of above 3.3 (all tolerances > .31), indicating that multicollinearity was not a problem in our sample.
Gender as a Possible Moderator
We further investigated the possibility of gender moderating the relationship between Cluster B symptoms and partner aggression. To do this, we re-ran the Cluster B regressions including two interaction variables: gender by borderline scaled score and gender by antisocial scaled score. The interaction between borderline PD and gender was significant across all three sources of personality disorder. The interaction between antisocial PD and gender was also significant but only on one source (the SIDP). Further analyses of the consistent interactions between borderline PD and gender revealed that across all three sources of personality assessment, borderline symptoms were significantly related to partner aggression only for women (coefficients of 37.5, 10.2, and 8.9 for the SIDP, the self-MAPP, and the informant-MAPP respectively), but not for men (highest p-value of .10 for the self-MAPP, although note that all coefficients were positive). This result cannot be explained by sample size differences, since men outnumbered women in this sample, or differences in variability of borderline symptoms between genders, since men (mean scaled borderline score = .11, SD = .18) were no different to women (mean scaled borderline score = .11, SD = .22) in terms of borderline symptoms.
Discussion
We examined the connection between personality pathology and self-reported partner aggression in a community sample of late middle-aged adults. By using three complementary measures of personality disorders, we avoided limitations associated with any particular assessment instrument or source of information. Consistent with the literature linking borderline PD to partner aggression (e.g., Holtzworth-Munroe & Stuart, 1994; Mauricio, Tein, & Lopez, 2007), we found that borderline PD symptoms were significantly related to self-reported partner aggression, although this relationship was moderated by gender (as discussed below). Conversely, contrary to the extant literature on antisocial PD and partner aggression (e.g., Ehrensaft et al., 2006), we did not find a consistent relationship between partner aggression and features of antisocial PD. This relationship was absent even when we included the antisocial criterion that refers specifically to aggression. Holtzworth-Munroe and Stuart (1994) identified two main types of pathological abusers (although note that they specifically looked at men, whereas our sample includes both genders). Borderline/dysphoric batterers were identified as those with insecure attachment patterns, moodiness, and fear of abandonment. Generally violent/antisocial batterers, on the other hand, are those who perpetrate partner aggression as part of a larger pattern of violence that is associated with a lack of empathy. Our results suggest that, in a community sample, the generally violent/antisocial batterer style does not persist into later middle-age, whereas the borderline/dysphoric style still causes significant problems in females.
Our finding that borderline symptoms were related to partner aggression was moderated by gender, such that the relationship was only significant for women. Most previous research showing a link between borderline symptoms and partner violence has focused on male batterers, but Hines (2008) found that gender did not moderate the association between borderline personality organization (a less severe form of borderline PD) and intimate partner aggression in a community sample. Our results appear to contradict this finding, pointing to a stronger relationship between borderline PD symptoms and partner aggression in females than in males.
Both borderline and antisocial PDs have been linked to partner aggression; why, then, did we only find a significant relationship between partner aggression and symptoms of borderline PD in our sample? Both disorders have been found to decrease in severity with age. In a community sample of adults aged under versus over 55, Cohen et al. (1994) reported a three-fold decrease in the older group in terms of the number of people who met diagnostic criteria for borderline, antisocial, narcissistic, and histrionic PDs. Links, Heslegrave, and Reekum (1998) also found that 53% of patients diagnosed with borderline PD no longer met criteria for full diagnosis of the disorder 7 years later. Indeed, we had very few participants in our sample who met full criteria for either disorder (three participants met full clinical criteria for diagnosis of borderline PD, and five for antisocial PD). In spite of this, subclinical borderline symptoms were related to self-reported partner aggression, whereas antisocial symptoms were not. Restricted range is unlikely to account for this differential finding, since the standard deviations of the scaled borderline and antisocial scores were identical.
There are various possible explanations for the observed decrease in personality pathology with age; aside from genuine abatement, this pattern of data could also result from selective mortality, either due to suicide, violent death, or other health complications; or other selection biases such as unavailability of pathological individuals due to incarceration (see Cohen et al., 1994, for a discussion). While our results do not speak to these explanations, they challenge the prevalent idea that borderline personality pathology is no longer a risk factor in older age. One possible criticism of our study is that we relied on self-reported aggression. Although self-reports are used commonly to investigate partner aggression, there is some evidence that people tend to under-report aggression as compared with their partners’ reports (e.g., Marshall et al., 2011; Simpson & Christensen, 2005). An important follow-up to our study would thus include both self and partner reports of aggression, in order to investigate how PDs interact with the tendency to report incidence of aggression. Another possible limitation of our study is that psychological aggression was much more frequent than physical aggression, with 75% of participants reporting psychological aggression but only 6% reporting any physical aggression. This is to be expected of an older community sample; furthermore, our substantive findings did not change when physical and psychological aggression were considered separately.
In our community sample of 55–64 year olds, we found borderline symptoms in women to be significantly related to partner aggression regardless of who provided the personality assessment. The three sources (interviewer, participant, and informant) each offer a unique perspective on the individual, but all point to the role of borderline personality pathology and its characteristics of abandonment fears, unstable identity, and affective instability in increased female partner aggression and a trend in this direction for men. This relationship was also stable regardless of whether we controlled only for the other Cluster B disorders, or for all 11 personality disorders. Our consistent borderline result echoes recent findings that borderline symptoms continue to be related to health (Powers & Oltmanns, in press) as well as the frequency of stressful life events (Gleason, Powers, & Oltmanns, in press) in later middle-age.
Acknowledgments
This research was supported by a grant from NIMH (RO1-MH077840). We are extremely grateful to Merlyn Rodrigues for managing this project and indebted to Amber Wilson, Josh Oltmanns, Rickey Louis, Tami Curl, and Andy Shields for their conscientious efforts in recruiting and interviewing our participants.
Footnotes
Raw, or total, scores on the SIDP for these symptom counts are, perhaps, easier to understand. Each participant’s score on BPD, for example, would be the sum of ratings (0–3) across 8 symptoms of BPD (1 of the 9 was excluded because it referred to aggression). The possible range would therefore be 0–24, and the actual range was 0–14. For ASPD, there are 6 symptoms (again, 1 of the 7 was excluded), so the possible range would be 0–18 and the actual range was 0–12.
Contributor Information
Yana Weinstein, Washington University in St. Louis.
Marci E. J. Gleason, University of Texas at Austin
Thomas F. Oltmanns, Washington University in St. Louis
References
- Breiding MJ, Black MC, Ryan GW. Prevalence and risk factors of intimate partner violence in eighteen U.S. states/territories, 2005. American Journal of Preventive Medicine. 2008;34(2):112–8. doi: 10.1016/j.amepre.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Cascardi M, Langhinrichsen J, Vivian D. Marital aggression: Impact, injury, and health correlates for husbands and wives. Archives of Internal Medicine. 1992;152(6):1178–84. doi: 10.1001/archinte.152.6.1178. [DOI] [PubMed] [Google Scholar]
- Cohen BJ, Nestadt G, Samuels JF, Romanoski AJ, McHugh PR, Rabins PV. Personality disorder in later life: A community study. The British Journal of Psychiatry. 1994;165(4):493–499. doi: 10.1192/bjp.165.4.493. [DOI] [PubMed] [Google Scholar]
- Dutton DG, Saunders K, Starzomski A, Bartholomew K. Intimacy anger and insecure attachment as precursors of abuse in intimate relationships. Journal of Applied Social Psychology. 1994;24(15):1367–1386. [Google Scholar]
- Dutton DG, Starzomski AJ. Borderline personality in perpetrators of psychological and physical abuse. Violence and Victims. 1993;8(4):327–337. [PubMed] [Google Scholar]
- Ehrensaft MK, Cohen P, Johnson JG. Development of personality disorder symptoms and the risk for partner violence. Journal of Abnormal Psychology. 2006;115(3):474–83. doi: 10.1037/0021-843X.115.3.474. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W. The occurrence of partner physical aggression on days of alcohol consumption: A longitudinal diary study. Journal of Consulting and Clinical Psychology. 2003;71(1):41–52. doi: 10.1037/0022-006X.71.1.41. [DOI] [PubMed] [Google Scholar]
- Gleason MEJ, Powers AD, Oltmanns TF. Personality pathology and threatening life events: Stress generation or enhanced subjective experience? Journal of Abnormal Psychology (in press) [Google Scholar]
- Grant B, Chou S, Goldstein R, Huang B, Stinson F, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69(4):533–45. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines DA. Borderline personality traits and intimate partner aggression: An international multisite, cross-gender analysis. Psychology of Women Quarterly. 2008;32(3):290–302. doi: 10.1111/j.1471-6402.2008.00437.x. [DOI] [Google Scholar]
- Holtzworth-Munroe A. A typology of men who are violent toward their female partners: Making sense of the heterogeneity in husband violence. Current Directions in Psychological Science. 2000;9(4):140–143. [Google Scholar]
- Holtzworth-Munroe A, Stuart GL. Typologies of male batterers: Three subtypes and the differences among them. Psychological Bulletin. 1994;116(3):476–497. doi: 10.1037/0033-2909.116.3.476. [DOI] [PubMed] [Google Scholar]
- Links PS, Heslegrave R, van Reekum R. Prospective follow-up study of borderline personality disorder: prognosis, prediction of outcome, and Axis II comorbidity. Canadian Journal of Psychiatry. 1998;43(3):265–70. doi: 10.1177/070674379804300305. [DOI] [PubMed] [Google Scholar]
- Marshall AD, Panuzio Jillian, Makin-Byrd Kerry N, Taft Casey T, Holtzworth-Munroe Amy. A multilevel examination of interpartner intimate partner violence and psychological aggression reporting concordance. Behavior Therapy. 2011;42:364–77. doi: 10.1016/j.beth.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauricio AM, Tein JY, Lopez FG. Borderline and antisocial personality scores as mediators between attachment and intimate partner violence. Violence and Victims. 2007;22(2):139–57. doi: 10.1891/088667007780477339. [DOI] [PubMed] [Google Scholar]
- Oltmanns TF, Gleason MEJ. Personality, health, and social adjustment in later life. In: Cottler LB, editor. Mental health in public health: The next 100 years. New York: Oxford University Press; 2011. [Google Scholar]
- Oltmanns TF, Turkheimer E, Strauss ME. Assessment. 1. Vol. 5. Sage Publications; 1998. Peer assessment of personality traits and pathology in female college students; pp. 53–55. [DOI] [PubMed] [Google Scholar]
- O’Leary KD. Psychological abuse: A variable deserving critical attention in domestic violence. Violence and Victims. 1999;14(1):3–23. [PubMed] [Google Scholar]
- O’Leary SG, Slep AMS. Precipitants of partner aggression. Journal of Family Psychology. 2006;20(2):344–7. doi: 10.1037/0893-3200.20.2.344. [DOI] [PubMed] [Google Scholar]
- Pan HS, Neidig PH, O’Leary KD. Predicting mild and severe husband-to-wife physical aggression. Journal of Consulting and Clinical Psychology. 1994;62(5):975–81. doi: 10.1037//0022-006x.62.5.975. [DOI] [PubMed] [Google Scholar]
- Powers AD, Oltmanns TF. Personality pathology as a risk factor for negative health perception. Journal of Personality Disorders. doi: 10.1521/pedi_2013_27_083. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Sheets E, Craighead W. Toward an empirically based classification of personality pathology. Clinical Psychology: Science And Practice. 2007;14(2):77–93. [Google Scholar]
- Simpson LE, Christensen A. Spousal agreement regarding relationship aggression on the Conflict Tactics Scale-2. Psychological Assessment. 2005;17(4):423–32. doi: 10.1037/1040-3590.17.4.423. [DOI] [PubMed] [Google Scholar]
- Stevenson J, Meares R, Comerford A. Diminished impulsivity in older patients with borderline personality disorder. The American Journal of Psychiatry. 2003;160(1):165–6. doi: 10.1176/appi.ajp.160.1.165. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. doi: 10.1177/019251396017003001. [DOI] [Google Scholar]
- Torgersen SS, Czajkowski NN, Jacobson KK, Reichborn-Kjennerud TT, Røysamb EE, Neale MC, Kendler KS. Dimensional representations of DSM-IV cluster B personality disorders in a population-based sample of Norwegian twins: A multivariate study. Psychological Medicine: A Journal Of Research In Psychiatry And The Allied Sciences. 2008;38(11):1617–1625. doi: 10.1017/S0033291708002924. [DOI] [PubMed] [Google Scholar]
- Ullrich S, Coid J. The age distribution of self-reported personality disorder traits in a household population. Journal of Personality Disorders. 2009;23(2):187–200. doi: 10.1521/pedi.2009.23.2.187. [DOI] [PubMed] [Google Scholar]
- Vickerman KA, Margolin G. Trajectories of physical and emotional marital aggression in midlife couples. Violence and Victims. 2008;23(1):18–34. doi: 10.1891/0886-6708.23.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren JI, South SC. A symptom level examination of the relationship between Cluster B personality disorders and patterns of criminality and violence in women. International Journal Of Law And Psychiatry. 2009;32(1):10–17. doi: 10.1016/j.ijlp.2008.11.005. [DOI] [PubMed] [Google Scholar]