Abstract
A multigenerational medical family history graphically recorded as a pedigree or family tree is a cost-effective tool in preconception counseling to identify couples at risk to have offspring with inherited disorders and to identify if either partner has a personal risk for a disorder with a genetic etiology. Interpretation of a medical family history can provide risk assessment for reproductive planning and choices, inform a diagnosis to help identify a patient’s medical screening needs and clinical management, and build rapport with the patient or couple. The use of standardized pedigree nomenclature is paramount to healthcare delivery as electronic medical records become universal. The trend towards having patients prepare a medical family history in advance of the first clinic visit is a way to empower patients to take charge of their health, and also allow health professionals to spend more focused time in confirming and interpreting family history at the visit instead of constructing family history. This article reviews standardized pedigree symbols, clues to identifying “red flags” in family history (with a focus on preconception genetic counseling), the pedigree as a psychosocial tool, and resources for obtaining a medical family history.
Keywords: Electronic medical record, Family history, Genetic counseling, Pedigree, Standardized pedigree nomenclature
Introduction
A medical family history remains the single most cost-effective tool to identify individuals at risk for disorders with a genetic etiology (Bennett 2010). The pedigree has been described as the single best genetic test in preconception care (Hogge and Hogge 1996; Solomon et al. 2008). As highlighted in Box 1, a pedigree is a multifunctional tool for genetic diagnosis, risk-assessment, and for developing patient rapport (Bennett 2004).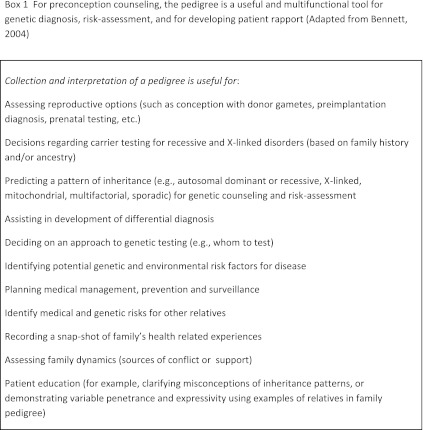
A preconception visit is an optimal time to obtain a medical family history, not just for reproductive counseling but also to identify medical screening needs that might be missed in an otherwise healthy couple. Family history may suggest patterns of inheritance such as autosomal recessive or dominant, X-linked, mitochondrial, multifactorial, or sporadic, and thus provide information for reproductive planning. Analysis of family history can provide information to guide genetic testing and inform reproductive decision making prior to pregnancy, or genetic testing that can be offered early in pregnancy.
Medical family history can also help determine a diagnosis in a patient and identify appropriateness of genetic testing and medical screening needs (Pletcher et al. 2007). Clues from medical family history may alert the practitioner as to health screening that might begin earlier than typical (such as mammography screening for early detection of breast cancer, colonoscopy for identification of precancerous colon polyps, or cardiovascular imaging/screening for person at risk for familial arrhythmias or aneurysms). Interpretation of a pedigree can also readily identify other relatives who may benefit from genetic evaluation.
Families share environmental risk factors too, such as diet and lifestyle. Unhealthy factors that influence wellness and risks during pregnancy may be teased out from a family pedigree (such as tobacco and alcohol use, patterns of dealing with stress, even attitudes about health such as using herbal supplements or decisions about seeking medical care).
In general, the approach to genetic testing involves testing the person at highest risk to have a mutation as compared to starting with a healthy at-risk individual. The pedigree is a quick way to determine the best person in the family to genetically test. For example, if a couple has concerns about passing on a disorder that affects a sibling (such as muscular dystrophy or intellectual disability), that sibling may be the best person to genetically test. Plans for medical management, prevention, and surveillance can be made based on pedigree risk assessment.
A pedigree is a visual snapshot of the person and family's health-related experiences. It is a way of visualizing family dynamics including sources of family support and conflict. It can also serve as a template for patient education such as clarifying misconceptions about patterns of inheritance or causation of disease, and even as a visual demonstration regarding variable expressivity of a disease within a family (such as age of disease onset; Bennett 2010).
Taking a medical family history in the form of a pedigree: a graphical and multifunctional tool
A family history in the form of a pedigree is a quick visual tool for incorporating and interpreting key medical information. A targeted family history and pedigree diagram incorporates reams of key medical and family data at a glance. A medical pedigree truly represents the saying that a picture is worth a thousand words. A pedigree has been described as the “first genetic test.” This is both a historical reference to the fact that pedigrees have been used for over 100 years but also that a pedigree is the first step for genetic evaluation (Resta 1993).
Boxes 2 and 3 summarize major health and demographic information to include when obtaining a family medical history. When clinicians record family history in text form, it is common to record only “positive” family history information. It is equally important to record the “unremarkable” or “negative” family history. Textual recording may miss key information. Consider the following example, “Ms. Jones age 25, has an uncle and first cousin who died of muscular dystrophy.” What age were these relatives diagnosed with muscular dystrophy? Is the cousin a male or female? Is the cousin a paternal or maternal relative? Did the cousin's parent live to be elderly without developing muscle disease? Knowledge of the age at diagnosis of muscular dystrophy, whether there are other medical findings (such as cardiomyopathy or cataracts), and the exact relationship of these relatives to Ms. Jones can make a substantial difference in determining if her future offspring are at risk for similar problems or even if she remains at risk to develop muscle disease.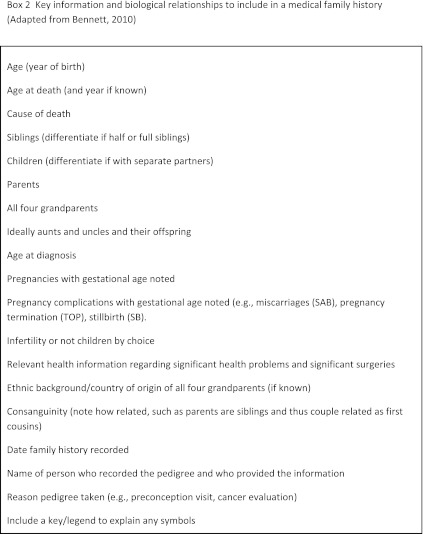
A pedigree is just as useful in determining if a patient does not require genetic testing or differing screening or management recommendations, especially when the patient has a family history of a common disorder such as cancer. Consider the example of Ms. Lee, age 30, she is planning a pregnancy and wondering about the risk of cancer in her family. Assume the following details of her family history: her maternal aunt had breast cancer at age 70; her paternal grandmother had breast cancer diagnosed before menopause; and a maternal first cousin was diagnosed with breast cancer at age 52, but her mother is living at age 80 without breast cancer. This structure of the family history would not require further genetic evaluation with testing for a highly penetrant breast cancer gene such as for BRCA1 or BRCA2. In contrast, if her relatives were premenopausal at the time of breast cancer diagnosis and they are all maternal relatives, the pattern would be suggestive of a high lifetime risk of breast cancer for Ms. Lee and further genetic evaluation would be warranted. She might be offered options for cancer screening and risk reduction at a younger age than typical (e.g., mammograms alternating with breast MRI beginning at age 30 instead of the typical age of 40). If this information is not gathered at a preconception visit, an important opportunity for cancer prevention could be missed.
Although health practitioners have many time constraints, dictating a family history may take more time than drawing a family history or recording an electronic pedigree. Health practitioners routinely triage and prioritize multiple medical issues at each patient visit. A pedigree targeting family history issues can be used as an instrument to help practitioners prioritize patient concerns. For example, if a couple is seen for a preconception visit for reproductive planning but a family history of colon cancer is identified in the male partner's family, the family history can be evaluated to determine if genetic testing may be appropriate or if colon cancer screening should be offered earlier than typical. Again, this is an important opportunity to identify an otherwise healthy person at high risk for a common disorder such as colon cancer, who might otherwise not be identified for many years, at which point cancer may have already developed.
The ideal approach to gathering family history is to have family history information collected by the patient in advance of the first visit. A pedigree begun at one visit can be easily updated at subsequent appointments. Computerized self-administered family medical history questionnaires are becoming more readily available that construct a pedigree in digital form (Bennett 2010). Several free and patient-friendly tools are emerging such as “My Family Health Portrait Tool” offered through the US Surgeon General's Office (http://www.hhs.gov/familyhistory/). Patients should be encouraged to confirm the diagnoses of relatives with medical records, copies of actual genetic test reports, developmental testing, pathology reports, or death certificates. Most people have fairly accurate information about the health history of their parents, children, and often their siblings, but the accuracy of their knowledge tends to decline for more distant relatives; this may be particularly true with family lore about sensitive diagnoses such as a history of mental illness or cancers of female reproductive organs (Bennett 2010).
Standard pedigree symbols
With the advent of electronic medical records, it is important that all types of medical documentation be standardized and family history is no exception (Bennett et al. 2008; Bigley and Feero 2008). A pedigree is of limited utility if the symbols and abbreviations cannot be easily interpreted. By using uniform symbols, there is decreased chance of misinterpretation of patient, family, medical, and genetic information (Bennett et al. 1993; Steinhaus et al. 1995).
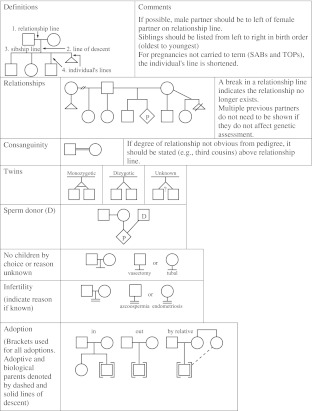
Through a peer-reviewed process, the Pedigree Standardization Task Force of the National Society of Genetic Counselors developed standardized nomenclature for symbolizing pedigrees which have become the international standard (Bennett et al. 1995, 2008). The most common standard pedigree symbols are shown in Figs. 1, 2 and 3.
Fig. 1.
Pedigree line definitions and common pedigree symbols (adapted from Bennett et al. 2008)
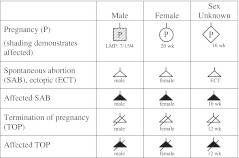
Fig. 2.
Additional pedigree symbols (adapted from Bennett et al. 2008)
Fig. 3.
Pedigree symbols related to pregnancy, miscarriage, and termination of pregnancy (adapted from Bennett et al. 2008)
The approach to recording and obtaining formation for a pedigree and key information to record
It is usually easiest to begin the drawing with the patient or consultand (the person seeking medical attention). The patient may also be the proband (the affected individual who brings the family to medical attention) (Bennett et al. 1995). The drawing then radiates up the page to include relatives by ascent (parents, full siblings, half siblings, grandparents, aunts, uncles, half aunts, and half uncles). Next, include the descendants (children and grandchildren). Clarify with patients the exact relationships because a patient may not distinguish a full sibling from a half sibling. Relationships of cousins may also be confused by a patient (for example, a patient may identify their relationship to the child of their first cousin as a second cousin when the actual relationship is a first cousin once removed; Bennett et al. 2002).
The most practical approach is to begin drawing the pedigree with the consultand (patient) near the middle of the page. Couples are drawn on the pedigree with the male partner (males are represented as square) placed to the left of the female partner (females are represented as circles). Siblings are recorded in birth order (when possible) from left to right, usually beginning with the oldest. An arrow is drawn toward the circle or square representing the patient. For a healthy relative that is related distantly to the patient, the number of relatives can be recorded within the square or circle (for example “5” inside a square would be five males, or “4” inside a circle would be four females). A diamond can be used to represent multiple relatives of either gender. A common error is to put the age of the person inside the pedigree symbol.
The outcomes of pregnancies for your patient and close relatives (siblings, parents, and adult children) should be noted. Miscarriages can be distinguished from termination of pregnancy (a triangle for miscarriage and a triangle with a slash for pregnancy terminations). Less commonly used pedigree symbols can be shown in the key, such as for adoption or a pregnancy conceived by donor gametes.
Diseases affecting relatives can be noted with shading of the pedigree. It is important to include a key so the shading can be easily interpreted. Record who drew the pedigree (e.g., James Spock, MD), the date recorded or updated, the reason for taking the pedigree (such as preconception counseling, cancer risk assessment, etc.), and the name of the informant (for example if a relative or spouse provides the information); this is particularly important if more information is needed at a later date.
Typically, a multigeneration pedigree would include two generations of ascent from the patient (parents, grandparents, siblings and half siblings, aunts and uncles and half aunts/uncles, and sometimes cousins) and two generations of descent (children and grandchildren). For a preconception pedigree, that would be a minimum of three generations. When a condition is suspected of being inherited, it is important to extend the history back as many generations as possible to include any additional affected relatives.
Record the ethnic background/country of origin of both sets of grandparents, if known. Inquire: “Do you know which countries your ancestors are from? What do you consider your ethnic background?” This information is usually placed at the top of the pedigree. Certain genetic disorders are more common in specific populations because individuals are likely to have a common gene mutation inherited from a distant ancestor. For example, the preconception screening that is offered to a couple who is of Ashkenazi Jewish ancestry differs from what would be offered to a couple of Southeast Asian ancestry (Metcalfe, this issue).
In preconception counseling, documenting if the patient is related as a blood relative to his/her partner is important because couples who are closely related are more likely to share the same deleterious genes in common than a nonrelated couple. Specific recommendations for genetic counseling of consanguineous couples can be found in Bennett et al. (2002) and Hanamy (this issue).
The best way to obtain a range of health information from a patient is to ask open-ended questions. It is better to begin a query with “Describe any medical problems that affect your parents” than to ask “Are your parents healthy?” You can follow with questions using a review of systems approach going from “top to bottom” with questioning about blood relatives who might have problems with eyesight, hearing, bones, skin conditions, cancer, etc. (Bennett 2010). Inquire about any potential environmental or occupational exposures in the patient and extended relatives such as tobacco, drug, and alcohol abuse, or occupational exposure such as lead and asbestos. Questions should be asked one at a time without jumping from one topic to another. Begin with general questions and then move to more complex questions or ones that may seem more threatening (McCarthy Veach et al. 2003). The ultimate test of the appropriateness of a question is: Will this information be helpful to my patient? (Hill and O'Brien 1999). Consider closing the interview with, “Are there any other conditions that you think ‘run’ in your family? Is there anything else that I have not asked about that you feel is important for me to know” (Bennett 2010).
Dealing with sensitive information
A genetic family history inquires about the very essence of an individual; queries are made not only about the patient's personal health but about intimate relationships and the health of relatives with whom the patient may have little contact (Bennett 2010). Before beginning to record a family history, it is helpful to warn the patient: “I will be asking you some personal questions about your health and the health of your family. Your answers to these questions are an important part of providing you with appropriate medical care.” (Bennett 2010). Emphasize to the patient that there is no choice in the genetic conditions that are passed in a family and that the diseases are nobody's fault. Listen to the patient's story and acknowledge significant life events (such as the death of a relative in an accident or sensitive information such as suicide). Even a simple statement to the patient “You have been through so much” will be greatly appreciated by the client (Bennett 2010).
Questioning should focus on “people-first-language” (www.disabilityisnatural.com). Inquiries should focus on the medical condition and not a label (e.g., a person with autism not an autistic). Be sensitive and respectful of cultural issues and differences. Individuals have different customs and beliefs based on race, socioeconomic status, gender, religious beliefs, sexual orientation, education, and health status (Bennett 2010). For example, if a couple has experienced multiple miscarriages, they may have cultural notions regarding the cause, such as eating forbidden foods, breaking social or religious taboos, “misconduct by the woman or by her partner”, even witchcraft or angering ancestral spirits (Laurino et al. 2005). When taking a family history, acknowledge belief systems that are different from one's own. An individual's belief system is likely to influence the type of health information he or she shares with the healthcare provider. Avoid stereotypes that assume that all persons from the same culture share the same views of health and disease causation.
The collection of family history information should be collected and maintained with the utmost protection for privacy and confidentiality. Initials or first names (in lieu of full names) may be enough to identify persons where medical records are documented and for orientation of discussion with the patient (Bennett et al. 2008).
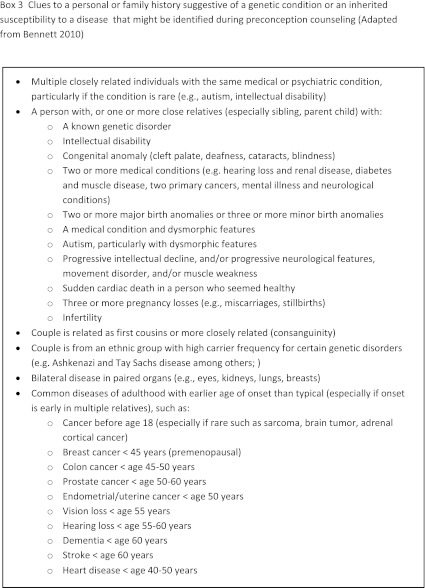
Red flags of family history
The key to teasing out potential genetic variables in a patient's family history is to look for unusual and infrequent features against a background of common diseases and normal physical variation. Box 3 reviews some of the clues to determine that a patient may have a higher risk of disease and that further genetic evaluation is appropriate. A “positive” family history for a particular condition would be followed up with more targeted questions (Bennett 2010).
A pedigree can be a useful tool for preconception counseling even if a diagnosis cannot be established. In the case of Ms. Jones, who has an uncle and cousin with muscular dystrophy, if her uncle is maternal uncle and her male cousin is related through a maternal aunt, then this could be an x-linked inheritance pattern, and therefore Ms. Jones would potentially be at risk to have a child with similar problems. If the male cousin is the son of the patient's maternal uncle, then this could be an autosomal dominant condition and therefore if Ms. Jones and her mother have no symptoms of the disease as adults, then it is unlikely that Ms. Jones and her partner are at risk to have a child with the muscular dystrophy. Of course the ideal approach would be to arrange for a genetic evaluation of the uncle and/or cousin, if this has not been done.
The pedigree as a psychosocial tool
The pedigree can be a powerful tool for anticipating a patient's potential psychosocial needs (Bennett 2010; McCarthy Veach et al. 2003). Table 1 lists some of the psychosocial clues that can be gleaned from the patient's family history portrait. For example, if a couple is planning a pregnancy and one of their siblings has experienced multiple miscarriages or infertility, they may be particularly concerned about such issues even when their change to have similar reproductive complications is low. If a woman in a preconception setting is identified to have an increased risk for cancer based on family history, and it is evident from her family pedigree that she is approaching the age that cancer developed in a close relative (such as a mother or sister), she may experience increased anxiety about developing cancer or feel compelled to have children “sooner than she is psychologically ready” based on the experience of her relative being diagnosed with cancer at a young age.
Table 1.
Listing of some of the clues from a pedigree that can help anticipate a patient's psychosocial needs in preconception counseling (adapted from Bennett 2010)
| Family history clue | Anticipatory guidance |
|---|---|
| Patient is approaching the age of relatives in the family who have developed disease or had life-threatening complications | May be reason that patient is seeking medical care at this time |
| Patient may have escalating anxiety about developing condition in family | |
| Patient may be experiencing chronic sorrow | |
| Patient is only a relative affected with the condition in immediate or extended family | Patient may have feelings of anger, disbelief and bewilderment, asking “Why me?” |
| Patient may have misconceptions about patterns of inheritance given perception of pattern of disease in family | |
| Patient is only an unaffected relative in immediate or extended family | Patient may experience survivor guilt |
| Patient may have hard time believing that risk for disease is “average” | |
| Patient may have misconceptions about patterns of inheritance given perception of pattern of disease in family | |
| Patient/couple is experiencing infertility and another close relative is pregnant or has recently given birth | Patient may have emotional conflicts regarding simultaneous family experience |
| Degree that medical interventions have been successful or well tolerated by relative(s) | If relatives have had successful medical interventions or screening the patient may be more trustful of the medical system, or the converse maybe true if the relatives have done poorly or screening has not detected disease early |
| Family history of depression or suicide | This could be a clue to risk factor for antepartum depression or need for extra assistance in coping with disease in family or outcome of test results |
| What is the structure of the family history? (e.g., are there relatives to turn to for support) | Are there siblings, adult children, parents or a step-parent who are available for support? |
Future areas of research: the clinical utility of medical family history
As electronic medical records become standard, the future may be a pedigree that travels from “birth to grave” through a person's electronic health record (Bennett 2010). Family history is dynamic; diseases occur with time, relatives are born and die. The pedigree would need to be updated and referenced to time as medical recommendations would be made in reference to the family history data available at a set time point. Ideally, this would include electronic risk assessment and recommendations for health screening and medical management (Valdez et al. 2010). A record would need to remain simple and not too cluttered with excess information, with data that is interpretable through the continuum of patient care (Bennett 2010; Feero et al. 2008). There may be information that is too sensitive to include in a pedigree but yet that information may be important for risk assessment (such as a history of depression or suicide). As noted in the proceedings of the National Institute of Health State-of-the-Science Conference: Family History and Improving Health (http://consensus.nih.gov/2009/familyhistorystatement.htm), continued research is needed to determine the best approaches to collecting family history, how to provide precise and timely risk assessment, and patient as well as provider satisfaction with these processes.
Conclusions
All primary care practitioners should have basic competence in obtaining and interpreting a family medical history and pedigree. Standardized pedigree symbols are used to record a medical family history. A family pedigree is a graphical reference to the diseases that run in a family and can be used in preconception counseling to inform risk assessment and guide discussions about reproductive decision making. A pedigree is also a base for identifying individuals at increased risk for genetic disorders, particularly disorders that are common such as heart disease, stroke, muscle disease, familial dementia, gait and movement disorders, and cancers. Interpretation of a pedigree can help to establish a pattern of inheritance and guide the practitioner to provide information to a couple making reproductive choices and when further genetic counseling and genetic testing may be appropriate. Medical geneticists and genetic counselors are experts in recording and interpreting family history and are a resource to health practitioners in making decisions about referrals for genetic counseling and testing. In addition to being a base for diagnostic evaluation and for surveillance recommendations, a pedigree is a primary method for patient education and for developing patient rapport. A pedigree remains a critical tool in the armamentarium of genomic medicine.
Footnotes
This is a contribution to the special issue “Genetic Aspects of Preconception Counseling in Primary Care.”
References
- Bennett RL. The family medical history. Prim Care Clin Off Pract. 2004;31:479–495. doi: 10.1016/j.pop.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Bennett RL. The practical guide to the genetic family history. Hoboken: Wiley-Blackwell; 2010. [Google Scholar]
- Bennett RL, Steinhaus KA, Uhrich SB, O'Sullivan C. The need for developing standardized family pedigree nomenclature. J Genet Couns. 1993;2:261–273. doi: 10.1007/BF00961575. [DOI] [PubMed] [Google Scholar]
- Bennett RL, Steinhaus KA, Uhrich SB, et al. Recommendations for standardized pedigree nomenclature. Am J Hum Genet. 1995;56(3):745–752. [PMC free article] [PubMed] [Google Scholar]
- Bennett RL, Motulsky AG, Bittles A, et al. Genetic evaluation of consanguineous couples and their offspring: recommendation of the National Society of Genetic Counselors. J Genet Couns. 2002;11(2):97–119. doi: 10.1023/A:1014593404915. [DOI] [PubMed] [Google Scholar]
- Bennett RL, French KA, Resta RG, Doyle DL. Update and review of the standardized pedigree nomenclature of the National Society of Genetic Counselors. J Genet Couns. 2008;17(5):424–433. doi: 10.1007/s10897-008-9169-9. [DOI] [PubMed] [Google Scholar]
- Bigley MB, Feero WG (2008). United States Department of Health and Human Services. A report of the Family Health History Multi-Stakeholder Workgroup. October 25, 2007. Available at www.hhs.gov/healthit/ahic/materials/10_07/phc/report.html
- Feero WG, Bigley MB, Brinner KM. New standards and enhanced utility for family health history information in the electronic health record: an update from the American Health Information Community's Family Health History Multi-Stakeholder Workgroup. J Am Med Inform Assoc. 2008;15(6):723–728. doi: 10.1197/jamia.M2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill CE, O'Brien KM. Helping skills: facilitating exploration, insight, and action. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- Hogge JS, Hogge WA. Preconception genetic counseling. Clin Obstet Gynecol. 1996;39:751–762. doi: 10.1097/00003081-199612000-00004. [DOI] [PubMed] [Google Scholar]
- Laurino MY, Bennett RL, Saraiya DS, Baumeister L, Doyle DL, Leppig K, Pettersen B, Resta R, Shields L, Uhrich S, Varga EA, Raskind WH. Genetic evaluation and counseling of couples with recurrent miscarriage: recommendations of the National Society of Genetic Counselors. J Genet Couns. 2005;14(3):165–181. doi: 10.1007/s10897-005-3241-5. [DOI] [PubMed] [Google Scholar]
- McCarthy Veach P, LeRoy BS, Bartels DM. Facilitating the genetic counseling process: a practice manual. New York: Springer; 2003. [Google Scholar]
- Pletcher BA, Toriello HV, Noblin SJ, Seaver LH, Driscool DA, Bennett RL, Gross SJ. Indications for genetic referral: a guide for health care professionals. Genet Med. 2007;9:385–389. doi: 10.1097/GIM.0b013e318064e70c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resta RG. The crane's foot: the risk of the pedigree in human genetics. J Genet Couns. 1993;2(4):1284–1285. doi: 10.1007/BF00961574. [DOI] [PubMed] [Google Scholar]
- Solomon BD, Jack BW, Ferro WG. The clinical content of preconception care: genetics and genomics. Am J Obstet Gynecol. 2008;199(6):S340–S344. doi: 10.1016/j.ajog.2008.09.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhaus KA, Bennett RL, Uhrich SB, et al. Inconsistencies in pedigree nomenclature in human genetics publications: a need for standardization. Am J Med Genet. 1995;56(3):291–295. doi: 10.1002/ajmg.1320560314. [DOI] [PubMed] [Google Scholar]
- Valdez R, Yoon PW, Quershi N, Green RF, Khoury MJ. Family history in public health practice: a genomic tool for disease prevention and health promotion. Annu Rev Public Health. 2010;31:69–87. doi: 10.1146/annurev.publhealth.012809.103621. [DOI] [PubMed] [Google Scholar]