Abstract
Objectives
1) To examine the impact of monthly Recovery Management Checkups (RMC) vs. control in the first 90 days post-release from jail on receipt of community-based substance abuse treatment, and 2) To explore the impact of RMC, treatment, and abstinence on HIV risk behaviors and recidivism.
Methods
Of the 480 women randomized, 100% completed the intake and release interviews, and over 90% completed the 30-, 60-, and 90-day post-release interviews. Of the 915 times women assigned to RMC were interviewed (at release, 30, 69 and 90 days post release), 885 (97%) times they attended linkage meetings, 429 (47%) times they were identified as in need of substance abuse treatment, 271 (30%) times they agreed to go to treatment, 149 (16%) times they showed to the treatment intake, and 48 (5%) times they stayed in treatment at least two weeks.
Results
During the 90 days following release from jail, women in the RMC condition (vs. control) were significantly more likely to return to treatment sooner and to participate in substance abuse treatment. Women who received any treatment were significantly more likely than those who did not to be abstinent from any alcohol or other drugs. Those who were abstinent were significantly more likely to avoid HIV risk behaviors and recidivism.
Conclusions
These results demonstrate the feasibility of conducting monthly Recovery Management Checkups with women offenders post-release and provide support for the effectiveness of using RMC to successfully link women offenders to treatment.
Keywords: Substance use disorder, recovery management checkups, women offenders, re-entry, HIV risk behavior, recidivism
1. INTRODUCTION
From 2000 to 2010 about half of incarcerated women were held in local jails and the number of women in local jails has increased by 30% (Minton, 2011). Because most are incarcerated for only a few weeks or months, they also represent the majority of women offenders re-entering the community. Consistent with the reasons for their arrests, 70% of women entering jail in 2002 reported using alcohol or other drugs weekly in the month before their arrest (Adams et al., 2011; Bureau of Justice Statistics, 2005). Women offenders with substance use disorders often suffer from a host of co-occurring conditions (e.g., medical, psychiatric, socioeconomic) that contribute to high relapse and recidivism rates (Adams et al., 2011; Guydish et al., 2011). These women are more likely than other women offenders and women living in the community to live below the poverty line, have no high school degree or GED, be homeless, be single parents, have custodial issues, engage in HIV related risk behaviors, have histories of victimization and its corresponding trauma, experience higher rates of serious mental illness, and have family histories of substance use disorders (Wellisch et al., 1993; Schilling et al., 1994; Singer et al., 1995; Jordon et al., 1996; Teplin et al., 1996; Peters and Hills, 1997; Veysey, 1998; Henderson, 1998; General Accounting Office, 1999; Langan and Pelissier, 2001; Rief et al., 2001; Bloom et al. 2002; Fazel and Danesh, 2002; Teplin et al., 2003; Bloom et al., 2004; Belenko et al., 2004; Adams et al., 2011; Guydish et al., 2011).
The literature suggests that within this vulnerable population, the majority engage in a range of activities that put them at high risk of relapse and either contracting or spreading HIV, with over 90% being sexually active (over half unprotected), 40–55% engaging with multiple sexual partners, 30–50% trading sex for drugs, food, housing or money, and 18–33% injecting drugs prior to incarceration (Adams et al., 2011; Baseman et al., 1999; Belenko et al., 2004; Bond and Semaan, 1996; El-Bassel et al., 1996; Grella et al., 2000, 2005; Guydish et al., 2011; Jordon et al., 1996; Magura et al., 1993; McClelland et al., 2002; Teplin et al., 1996; Wellisch et al., 1993; 1996). These circumstances leave women offenders twice as likely to have HIV/AIDS than male offenders and over 7 times more likely than women in the community (Center for Disease Control and Prevention, 2004; Maruschak, 2004). They also constitute a high-risk group vulnerable to relapse to substance use, HIV, and re-incarceration upon re-entry into the community.
Although dominated by studies with male offenders, several studies show that post-release participation in community-based treatment can sustain and often improve upon post-release outcomes (Harrison and Martin, 2003; Prendergast and Wexler, 2004; Wexler et al., 2004). Unfortunately, while a third of jail-based programs refer women to community-based treatment, only about 1 in 4 programs assist the women in contacting community-based treatment (Taxman et al., 2007). Moreover, the vast array of competing needs women face upon re-entry into the community often devastates and prevents the women from successfully accessing and staying in community-based treatment, resulting in high relapse rates and poor outcomes. For women offenders, when the need for successful linkages and retention in community-based treatment is met, post-release recovery is more likely to be sustained. In one study, Guydish and colleagues (2011) randomly assigned women to probation case management or to standard probation in an attempt to increase post-release treatment participation and reduce relapse and recidivism. There were no significant differences between groups and it was concluded that more treatment was likely needed to achieve successful outcomes.
While it is necessary to link women offenders to community-based treatment upon release and increase retention rates, these strategies alone are likely not sufficient to support the women’s long-term recovery process. A growing body of evidence demonstrates that addiction is often a chronic condition, requiring multiple episodes of care over several years before achieving stable recovery, particularly when accompanied by multiple co-occurring conditions much like the conditions common in the women offender population. To manage other chronic conditions, general public health models utilize ongoing monitoring and early re-intervention techniques to alleviate symptoms, restore physical and psychosocial functioning, and improve social relationships and quality of life (Nicasso and Smith, 1995; Rotter et al., 1996). Drawing on experience from the health care field and responding to calls in the addiction field to shift treatment toward a chronic care model (Dennis and Scott, 2007, 2012; McLellan et al., 2000; Weisner et al., 2004), Scott and colleagues developed and tested a Recovery Management Checkup Model (RMC) designed to manage recovery over time (Dennis et al., 2003, 2012; Scott et al., 2003, 2005a, 2009a, 2011). The theory underlying this work is that long-term monitoring through regular checkups and early re-intervention will facilitate early detection of relapse, reduce the time to treatment re-entry; and consequently, improve long-term outcomes. This approach does not rely on participants to identify their symptoms and return to treatment. Instead, these checkups are pro-active and include quarterly assessments and personalized feedback for participants on the status of their condition. Research personnel used Motivational Interviewing (MI) techniques to involve participants in the decision-making process about their care, and help participants resolve their ambivalence about substance use to help move toward a commitment to change by actively participating in treatment or some other type of recovery support. The Recovery Management Check-up (RMC) model relies on treatment linkage, engagement, and retention protocols to help participants secure the care they need over extended periods of time. This model addresses the chronic nature of addiction and incorporates the following components known to facilitate and sustain long-term recovery: a) sustained client engagement, b) quarterly monitoring and linkage to treatment, c) removing obstacles to treatment admission and recovery, d) enhancing treatment retention and completion, e) teaching participants the skills needed to actively self-manage their condition, and f) pro-actively resolving ambivalence about use and abstinence.
RMC has been tested in two clinical trials involving 894 men and women presenting to community-based treatment. Most reported lifetime involvement with the criminal justice system (75% and 83% respectively) and many reported involvement with the criminal justice system in the 90 days before intake (33% and 45% respectively). In the first trial, participants received quarterly checkups for two years (Dennis et al., 2003; Scott et al., 2005); and in the second, participants received checkups quarterly for four years (Scott and Dennis, 2009, 2012). Results demonstrated that RMC participants were significantly more likely than those in the control condition to receive any treatment and returned to treatment sooner. The size of these effects increased over time. After two years of quarterly checkups, RMC participants in both experiments also reported significantly more days of abstinence and fewer past-month symptoms of abuse/dependence (Scott and Dennis, 2009, 2011).
Given the effectiveness of RMC on successfully linking to and retaining individuals in community-based treatment, it was hypothesized that RMC would provide a viable option for linking women offenders released from jail to community-based treatment. However, given the higher potential for relapse and recidivism during the 90 days post-release, checkups were scheduled for 30, 60, and 90 days post-release and quarterly thereafter. In addition, the high rates of HIV risk in the female offender population clearly highlight the need to expand the previously tested RMC model to include an HIV intervention component. To that end, a gender- specific HIV intervention was added to the existing RMC model.
This article reports the results from the first 90 days of a third clinical trial in which 480 women offenders were randomly assigned to either the RMC condition or a control group upon release from one of the largest single site jails in the U.S. Women participated in checkups at 30, 60, and 90 days post-release. The objectives of this experiment were to examine the impact of monthly Recovery Management Checkups (vs. control) in the first 90 days post-release from jail on receipt of community-based substance abuse treatment, and to explore the impact of RMC, treatment, and abstinence on HIV risk behaviors and recidivism.
2. METHODS
2.1 Recovery Management Checkup (RMC)
Women assigned to the experimental condition received monthly Recovery Management Checkups (RMC; Scott and Dennis, 2008). Women met with a Linkage Manager after completing each research interview at release, 30, 60, and 90 days post-release. Of the 1,847 interviews completed during the first 90 days, 1775 (96%) were completed face-to-face in the research office. During the 30, 60, and 90-day linkage meetings, the Linkage Manager used motivational interviewing to: a) provide feedback regarding her current substance use, HIV risk behavior, or illegal activity; b) discuss barriers that prevented her from stopping each activity and ways to avoid them in the future; and c) discuss her level of motivation for change. For women that reported substance use, Linkage Managers also scheduled treatment appointments and accompanied the women to treatment intake and stayed through the process. After women entered treatment, the Linkage Managers implemented an Engagement and Retention Protocol designed to improve retention rates. Specifically, for women entering detox, the Linkage Manager either called or visited them daily until they moved to the next level of care. After entering treatment (either residential or outpatient), the protocol included a combination of phone calls and face-to-face visits during the first 14 days. If at any point during treatment, a woman threatened to leave or failed to show for an appointment, the treatment staff would contact the Linkage Manager to arrange an intervention to re-engage the woman in treatment. For women who refused the treatment option, the Linkage Manager and participant agreed upon an Alternative Action plan, which included various behaviors the woman planned to engage in to reduce or stop her substance use, HIV risk, or her participation in illegal activity.
For RMC women reporting no involvement in one of the three areas, for instance substance use, the Linkage Manager and participant discussed ways in which her life had changed as a result of being clean (e.g., spending time with family, working), what was working for her, and precisely what she would continue to do in the next 30 or 60 days to maintain her recovery. The same approach was used when women reported no HIV risk behaviors (minimizing her HIV risk by carrying a condom in her purse) or illegal activity (avoiding certain neighborhoods).
As part of the monthly linkage meetings, RMC participants also received a modified gender-focused HIV risk reduction intervention (Wechsberg et al., 2004), which was comprised of: a) assessment and feedback on HIV behavior, HIV knowledge, and condom self-efficacy; b) assistance in understanding related health conditions; c) health promotion skills (assertiveness and communications, self-empowerment and avoiding violence and other unsafe situations); and d) HIV risk reduction materials (e.g., substance abuse and HIV treatment referrals, male and female condoms). The release linkage meeting focused only on substance use and HIV testing.
2.2 Participant Eligibility
The target population for this clinical trial consisted of adult women offenders with substance problems re-entering the community from a county jail substance abuse treatment program. Eligibility for this trial was determined in two phases. In the first phase, women were deemed ineligible if they had not used substances in the 90 days before incarceration, had no abuse/dependence symptoms, were under 18, lived or planned to move outside Chicago within the next 12 months, were not fluent in English or Spanish, were cognitively unable to provide informed consent, or were released before the 14th day of incarceration. At the end of Phase I, a total of 866 women remained eligible and 810 (93%) agreed to participate and completed the initial interview. In the second phase, only women released to the community (vs. those sent to prison or other institutions where the intervention could not be implemented) were invited to participate in the experiment proper. Of the 492 women released to the community, 480 (98%) agreed to participant in the post-release randomized experiment.
2.3 Recruitment Site
Women were recruited from the Department of Women’s Justice Services (DWJS) in the Cook County Jail, in Cook County Illinois, which operates jail- (residential) and furlough- (outpatient) based treatment programs as alternative sentencing for women offenders incarcerated for drug problems and who are considered nonviolent. Cook County Jail is one of the largest single site jails in the U.S. and DWJS is one of the largest jail-based treatment programs for women in the U.S.
2.4 Objectives
The primary objective of this paper is to examine the impact of monthly Recovery Management Checkups (vs. control), in the first 90 days post-release from jail, on receipt of community-based substance abuse treatment. Based on results from two prior trials, we hypothesized that, relative to women in the control group, women assigned to RMC will return to treatment sooner and be more likely to receive any treatment during the first 90 days. This paper reports on the results regarding the impact of RMC, treatment, and abstinence on HIV risk behaviors and recidivism.
2.5 Outcome Measures
Table 1 provides the definition for each of the outcome measures. A modified version of the Global Appraisal of Individual Needs (GAIN; Dennis et al., 2003) provided the measures for this study. An on-site urine test protocol (Scott and Dennis, 2009, 2011) was used to minimize the rate of under-reporting by providing women the test results prior to the start of the interview, at the time of the interview, and probing inconsistencies. As a result, false negative rates were low for any alcohol or other drug (4%), opioid use (4%), cocaine (3%), marijuana (2%) and alcohol (1%). For measures of recidivism, we used both Cook County’s information system Incarceration Management and Cost (IMAC) recovery system and the State of Illinois’ Law Enforcement Agencies Data System (LEADS) to check for subsequent arrest and incarceration. As noted in Table 1, the definition of abstinence is based on either urine results or self-reporting, and the definition of re-arrest and incarceration is based on records or self-report.
Table 1.
Definitions of Outcome Measures by Hypothesis
| Days to First Treatment. Days from release to first day of treatment based on staff logs and self-reports at 30, 60, and 90 days post-release. |
| Any Treatment in the first 90 days: Any report of receiving treatment based on staff logs and self-reports at 30, 60, and 90 days post-release. |
| Abstinence: Based on no self-reported use and no dirty urine tests at 30, 60 and 90 days post- release for: a) any alcohol or drugs, b) alcohol, c) cannabis, d) cocaine, and e) opiates. |
| No Needle Use: Based on no self report at 30, 60 and 90 days post-release of any needle use to inject drugs. |
| No Unprotected Sex: Based on no self-report at 30, 60 and 90 days post-release of unprotected sex defined as having vaginal, anal or oral sex without a barrier like a male condom, women’s condom, or dental dam. |
| No Illegal Activity: Based on no self-report at 30, 60 and 90 days post-release of illegal activity other than drug use. |
| No Arrest: Based on no rearrest self-report at 30, 60 and 90 days post-release or in the Jail’s |
| IMAC or State’s LEADS data bases for the first 90 days post-release. |
| No days in Jail/Prison: Based on no days in any kind of jail or prison self-report at 30, 60 and 90 days post-release. |
2.6 Training and Quality Assurance
Tracking for follow-up was done using the model developed by Scott (2004). All staff were trained on the assessment, intervention, and tracking protocols by the authors. Interviews were audio-taped and randomly selected for review to maintain high quality data. A Motivational Interviewing National Trainer (MINT) trained and certified all Linkage Managers. All linkage meetings were audio-taped and the MINT reviewed a random sample of tapes using the Revised Global Scales: Motivational Interviewing Treatment Integrity 3. (Moyers et al., 2010) revised global scales for five areas that reflect the principles of Motivational Interviewing (MI): Evocation, Collaboration, Autonomy/Support, Direction, and Empathy. During the course of this study, 3 individuals served as Linkage Managers, but two individuals conducted 94% of the meetings. The third could not sustain acceptable competency levels and was quickly replaced. The two primary Linkage Managers' performance was exemplary as they averaged between 4.0 and 4.8 on all ratings across all scales.
2.7 Sample Size
The original sample size target of 425 women was sufficient to have 80% power in a two tailed test with p<.05 for 2 group effects of sizes of .36 or more based on prior studies (Dennis et al., 2003, 2012; Scott and Dennis, 2009, 2011) assuming at least 90% follow-up (Dennis et al., 1997). We increased the sample size to 480 to allow for more refined sub-group analyses.
2.8 Randomization
Using gRand Urn Randomization Version1.10 (Charpentier, 2003) women who were eligible at baseline and released to the community were randomly assigned to either RMC or a control condition. Urn randomization uses a Bayesian approach that adjusts the probability of assignment to condition in ways that minimize differences in the stratification variables (Stout et al., 1994). It is conceptually similar to blocked randomization, but more efficient (typically reaching balance within the first 50 cases assigned). In this study, we used a base rate of 50% to each condition and stratified women offenders based on being under 35 (vs. 35+), African American (vs. other race), having any prior treatment (vs. none), recieving jail-based residential program (vs. furlough outpatient program), or scoring high on the substance disorder screener score (3–5 vs. 0–2), HIV risk behavior screener (3–7 vs. 0–2), internalizing disorder screener score (3–5 vs. 0–2), externalizing disorder screener score (3–5 vs. 0–2), and crime/violence screener score (3–7 vs. 0–2). As expected, there were no significant differences by condition on any of the variables used to stratify in urn randomization.
2.9 Statistics
All analyses were conducted using IBM SPSS statistics version 19 and based on an intent to treat design (i.e., participants were analyzed per random assignment regardless of actual services received). Time to event outcomes were analyzed using Cox proportional hazard regression analysis, dichotomous outcomes with logistic regression. In each case (H1, H2 and H3), the initial predictor was random assignment. Where applicable (H2 and H3), this was followed sequentially by models that added variables for “any treatment” and “abstinent for months 1–3” to predict other variables. The latter two variables are for the total sample. To further reduce the impact of missing data, we combined data from multiple data sources (i.e., self report, urine test, justice records) within individual following the Longitudinal, Expert and All Data (LEAD) approach (Kranzler et al., 1997; Lennox et al., 2006).
3. RESULTS
3.1 Participant Flow
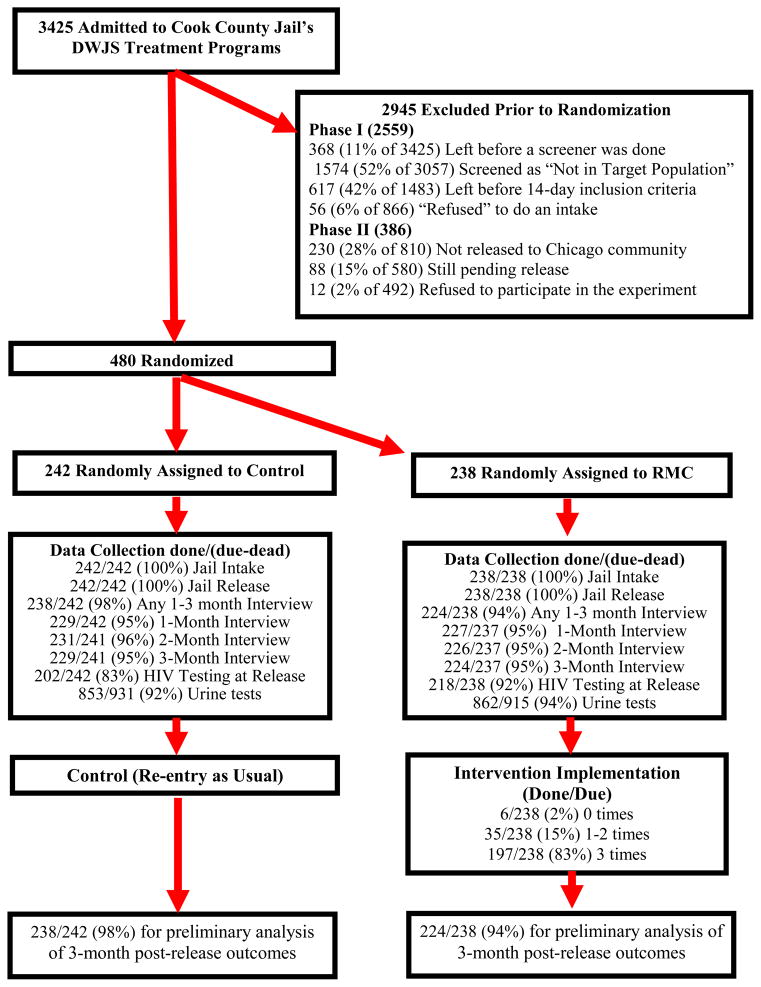
The research team recruited women for the experiment from 8/22/2008 until 4/16/2010. During this time a total of 3,425 women were admitted to the Department of Women’s Justice Services (DWJS). Figure 1 shows the participant flow during recruitment, randomization, data collection and intervention. Prior to randomization:
Figure 1.
Participant Case Flow Chart
368 (11% of 3425) women left before a screener was done
1574 (52% of 3057) women were screened and deemed “Not in Target Population”
617 (42% of 1483) women were in the jail’s custody for less than 14 days
56 (6% of 866) women “refused” to do an intake
230 (28% of 810) women were not released to the Chicago community
88 (15% of 580) women were still pending release at the time recruitment ended on 4/16/2010
12 (2% of 492) refused to participate in the experiment
As shown in Figure 1, the remaining 480 were randomized at the time of release to either the experimental condition (RMC; n=238) or to control condition (n=242). Of the 480 women, 100% completed the intake and release interviews, and over 90% completed all 3 of the 30, 60, and 90 day post-release interviews. Urine test data was collected during 93% of the release 30-, 60- and 90-day interviews. Of the women assigned to RMC (n=238), 95% participated in the linkage meeting at 30 days, 95% at 60 days, and 95% at 90 days. This includes 83% who attended all 3 linkage meetings, 15% attended 1–2 linkage meetings, and 2% who failed to attend any linkage meetings. Analyses in this paper are based on women with one or more follow-up and include data from 238 (98% of the 242) women randomized to the control group and 224 (94% of 238) women randomized to RMC condition. Of the 915 times women assigned to RMC were interviewed (at release, 30, 69 and 90 days post release), 885 (97%) times they attended linkage meetings, 429 (47%) times they were identified as in need of substance abuse treatment, 271 (30%) times they agreed to go, 149 (16%) times they showed to the treatment intake, and 48 (5%) times they stayed in treatment at least two weeks.
3.2 Participant Characteristics
Eighty-three percent of the women described themselves as African American, 8% Caucasian, 5% Hispanic, and 4% as “other/mixed.” Average age was 36.7 years (SD = 10.02, range 18–63 years). Seventy-one percent of the women reported being never married; 17% divorced, separated, or widowed; and 12% married or living with someone. Approximately 63% of the women had children under age 21, and most had custody of all (41%) or some (27%) of their children. Twenty-two percent of the women started using alcohol or drugs before the age of 15, 94% reported prior addiction treatments, and 80% met criteria for dependence, including 14% for alcohol, 10% for cannabis, 41% for cocaine, 45% for opioids, and 24% for other substances. During the year prior to incarceration, 43% of the women reported symptoms consistent with one or more other mental disorders, including 32% for mood disorders, 11% for generalized anxiety, 19% for a trauma related disorder, 38% for borderline personality disorder, and 10% with antisocial personality disorder. Four percent of the women were first arrested under age 15, 52% reported five or more prior arrests, 86% had prior incarcerations. Current charges included 63% related to alcohol or drugs, 25% property crime, 5% prostitution, 4% violent crime, 3% criminal justice system violation, and 8% other. At release, 30% of the women were on probation or parole and 26% were mandated to treatment. As shown in Table 2, there were no significant differences between conditions across all of the above characteristics.
Table 2.
Participant Characteristics by Randomized Condition
| RMCWO
|
|||||
|---|---|---|---|---|---|
| Characteristics | Control (n=242) | RMC (n=238) | Total (n=480) | Chi-sq. | p |
| Race/Ethnicity | |||||
| African American | 81% | 85% | 83% | 2.84 | 0.416 |
| Caucasian | 8% | 8% | 8% | ||
| Hispanic | 5% | 4% | 5% | ||
| Mixed/Other | 5% | 3% | 4% | ||
| Age (mean) | 37.2 | 36.3 | 36.7 (10.4) | F=0.92 | 0.339 |
| Married/living with someone | 11% | 13% | 12% | 1.06 | 0.589 |
| Divorced/separated/widowed | 18% | 15% | 17% | ||
| Never married | 71% | 72% | 71% | ||
| Number of Children under age 21 | |||||
| None | 41% | 33% | 37% | 3.47 | 0.320 |
| 1 | 16% | 18% | 17% | ||
| 2 | 15% | 18% | 17% | ||
| 3+ | 27% | 31% | 29% | ||
| Child/Custody | (n=141) | (n=158) | (n=299) | ||
| Self Only | 43% | 39% | 41% | 0.54 | 0.768 |
| Self + Others | 28% | 27% | 27% | ||
| Others Only | 30% | 34% | 32% | ||
| Age of first use under 15 | 21% | 22% | 22% | 0.05 | 0.817 |
| Prior Substance Abuse Treatment | |||||
| 0 times | 6% | 5% | 6% | 0.51 | 0.776 |
| 1 time | 31% | 34% | 32% | ||
| 2+ times | 63% | 61% | 62% | ||
| Weekly Use in the 90 days before incarceration | 89% | 90% | 89% | 0.01 | 1.000 |
| Dependence (lifetime) | |||||
| Any | 81% | 79% | 80% | 0.10 | 0.820 |
| Alcohol | 15% | 13% | 14% | 0.20 | 0.653 |
| Cannabis | 10% | 10% | 10% | 0.05 | 0.831 |
| Cocaine | 43% | 39% | 41% | 0.76 | 0.384 |
| Opioid | 45% | 45% | 45% | 0.03 | 0.869 |
| Other | 22% | 27% | 24% | 1.37 | 0.242 |
| Any Co-occurring Disorder (Past Year) | 40% | 45% | 43% | 1.38 | 0.268 |
| Depression | 29% | 34% | 32% | 1.46 | 0.228 |
| Anxiety | 10% | 11% | 11% | 0.13 | 0.718 |
| Traumatic Related | 20% | 18% | 19% | 0.53 | 0.467 |
| Borderline Personality | 36% | 40% | 38% | 1.17 | 0.301 |
| Antisocial Personality Behavior | 12% | 9% | 10% | 0.70 | 0.456 |
| First arrest under age 15 | 4% | 4% | 4% | 0.00 | 1.000 |
| 5+ arrests | 52% | 51% | 52% | 0.05 | 0.855 |
| Prior incarceration of a week or more | 88% | 85% | 86% | 0.52 | 0.506 |
| Moderate/High Crime or Violence | 50% | 55% | 53% | 1.12 | 0.289 |
| Types of Current Charges | |||||
| AOD Crime | 64% | 63% | 63% | 0.11 | 0.777 |
| Property Crime | 28% | 21% | 25% | 2.86 | 0.092 |
| Prostitution | 5% | 5% | 5% | 0.06 | 0.840 |
| Violent Crime | 2% | 5% | 4% | 2.18 | 0.156 |
| Criminal Justice Violations | 3% | 2% | 3% | 0.31 | 0.772 |
| Other | 8% | 8% | 8% | 0.05 | 0.868 |
| At the time of Release\a | |||||
| On Probation or Parole | 31% | 29% | 30% | 0.23 | .692 |
| Mandated to Treatment | 23% | 30% | 26% | 3.04 | .096 |
Note: No differences statistically significant
Random assignment happened just after the time of release
3.3 Post-Release Relapse and the Need for Substance Abuse Treatment
Over 68% of the women relapsed to alcohol or drug use within the first 30 days post-release, 74% relapsed within 60 days, post-release and 77% relapsed within 90 days post-release. There were no significant differences by condition in relapse rates at 30 days (67% RMC vs. 69% control; OR=0.92, nsd), 60 days (73% RMC vs. 75% control; OR=0.86, nsd) or 90 days post-release (76% RMC vs. 77% Control, OR=.96, nsd). This demonstrates the high need for additional substance abuse treatment after release.
3.3.1 Effect of RMC
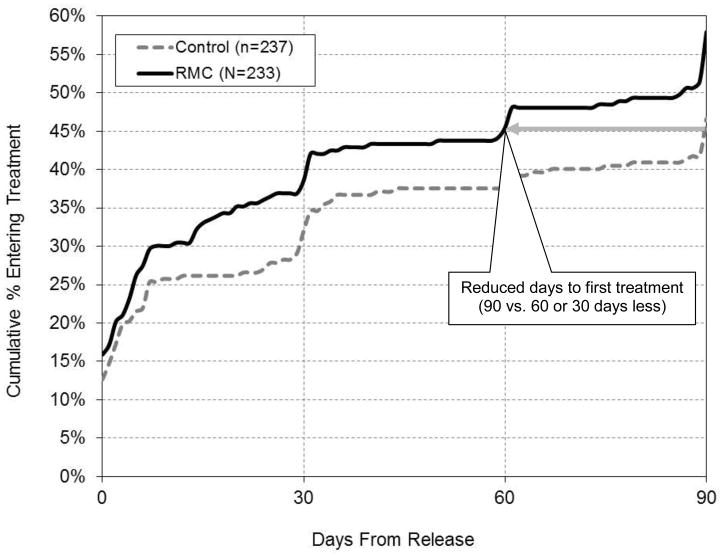
During the first 90 days post-release, women in the RMC condition (vs. control) returned to treatment significantly sooner (60 vs. 90 days; OR=1.33, p<.05; 95% CI 1.02 to 1.72; See Figure 2) and were significantly more likely to participate in any substance abuse treatment (55% vs. 45%; OR=1.53, p<.05, 95% CI=1.06 to 2.20; See Table 3). Thus, RMC was associated with linking women to treatment sooner and with higher treatment admission rates during the first 90 days. We also explored the potential impact of mandates to treatment and found no main effect (OR=1.49, p = .136; 95% CI 0.88, 2.50) or interaction with assignment to RMC (OR=0.87, p = .711; 95% CI 0.42, 1.82). While associated with treatment, RMC was not significantly associated with increased abstinence or reduced HIV risk or recidivism (see Table 3). These findings are consistent with the previous two clinical trials.
Figure 2.
Time from Release to Treatment Re-entry by Condition
Table 3.
Effect of RMC on Treatment, Abstinence, HIV Risk Behaviors and Recidivism in the First 90 Days Post-Release
| Dependent Variable | Control (n=238) | RMC (n=224) | Odds Ratio (95% CI) |
|---|---|---|---|
| Any Treatment Participation | 45% | 55% | 1.53* (1.06, 2.20) |
| Alcohol and Other Drugs (AOD) Abstinence | 23% | 24% | 1.05 (0.68, 1.61) |
| No Needle Use | 95% | 96% | 1.23 (0.50, 3.02) |
| No Unprotected Sex | 44% | 43% | 0.96 (0.67,1.38) |
| No Illegal Activity | 83% | 77% | 0.69 (0.44, 1.09) |
| No Arrests | 80% | 75% | 0.73 (0.47, 1.13) |
| No Days in Jail | 77% | 76% | 0.92 (0.60, 1.43) |
p<.05
3.3.2 Effects of RMC and Treatment on Abstinence
Part 1 of Table 4 repeats the relationship between RMC and increased treatment participation. Part 2 of Table 4 shows the impact of RMC and treatment on abstinence. During the first 90 days post-release, women who received any treatment were significantly more likely than those who did not, to be abstinent from any alcohol or other drugs (34% vs. 12%; OR=3.74, p<.001), alcohol (58% vs. 31%; OR=3.12, p<.001), marijuana (74% vs. 46%; OR=3.44; p<.001), and cocaine (65% vs. 52%). The differences were in a similar direction for abstinence from opiates, but did not reach significance (67% vs. 62%; OR=1.22, nsd). There were no significant effects of RMC on abstinence in the multivariate model.
Table 4.
Odds Ratios for Direct and Indirect Effects of RMC on Treatment and Abstinence in the First 90 Days Post-Release
| Predictors Cells=Odds Ratio (95% confidence intervals) |
|||
|---|---|---|---|
| Dependent Variable | Recovery Management Checkups (RMC ) | Any Treatment | Any AOD Abstinence |
| Sample sizes for each predictor | n=234, RMC | n=235, Any Treatment | n=109; 90 days of AOD Abstinence |
| n=238, Control | n=237, No Treatment | n=363; 0–89 days AOD Abstinence | |
|
| |||
| Part 1 Effect of RMC on Treatment | |||
| Any Treatment Participation | 1.53*(1.06, 2.20) | -- | |
|
| |||
| Part 2. Effect of RMC and Treatment on Abstinence | |||
|
| |||
| Alcohol and Other Drugs (AOD) Abstinence | 0.91 (0.58, 1.43) | 3.74*** (2.32, 6.02) | -- - |
| Alcohol Abstinence | 0.79 (0.54, 1.15) | 3.12*** (2.13, 4.57) | -- |
| Marijuana Abstinence | 0.83 (0.56, 1.22) | 3.44*** (2.33, 5.10) | -- |
| Cocaine Abstinence | 1.12 (0.77, 1.62) | 1.68** (1.16, 2.43) | -- |
| Opiate Abstinence | 1.15 (0.79, 1.68) | 1.22 (0.83, 1.78) | -- |
|
| |||
| Part 3. Effect of RMC, Treatment and AOD Abstinence on HIV Risk Behaviors and Recidivism | |||
|
| |||
| No Needle Use | 1.34 (0.54, 3.35) | 0.32* (0.12, 0.87) | 8.02* (1.05, 61.43) |
| No Unprotected Sex | 0.95 (0.65, 1.38) | 1.01 (0.69, 1.49) | 2.70*** (1.71, 4.26) |
| No Illegal Activity | 0.66 (0.42, 1.06) | 1.19 (0.73, 1.89) | 6.61*** (2.58, 16.92) |
| No Arrests | 0.69 (0.44, 1.08) | 0.99 (0.63, 1.56) | 3.58*** (1.77, 7.26) |
| No Days in Jail | 0.94 (0.60, 1.46) | 0.70 (0.44, 1.10) | 2.94** (1.54, 6.52) |
p < .05,
p<.01,
p<.001 bolded
Notes. RMC=random assignment to Recovery Management Check-ups; Any treatment and Any alcohol or other drug (AOD) abstinence based on total sample (regardless of condition).
3.3.3 Effects of RMC, Treatment, and Abstinence on HIV Risk Behaviors and Recidivism
Part 3 of Table 4 shows the effects of RMC, treatment and abstinence during the first 90 days post-release on HIV risk behaviors, illegal activity, and recidivism. Women who were abstinent during the first 90 days post-release (regardless of condition or treatment) were significantly more likely to avoid needle use (99% vs. 95%; OR=8.02, p < .05) and unprotected sex (62% vs. 38%; OR=2.70, p<.001). In the multivariate model, any treatment decreased the odds of no needle use (94% vs. 97%; OR=0.32, p < .05), but was not related to unprotected sex. RMC was not significantly related to reduced HIV risk in the multivariate model. Women who were abstinent during the first 90 days post-release (regardless of condition or treatment) were also significantly more likely to avoid any illegal activity (95% vs. 75%; OR=6.61, p<.001), re-arrest (91% vs. 73%; OR=3.58, p<.001), or time in jail or prison (87% vs. 73%; OR=2.94; p<.01).
4. DISCUSSION
The current study tested the impact of one of the first non-corrections involved re-entry interventions implemented with women offenders released from jail. The Recovery Management Checkups for Women Offenders (RMC-WO) intervention tested in this study utilized a Mixed strategy for providing continuity of care between corrections and community-based treatment. In line with components of Taxman and colleague’s (2007) evidence-based supervision model, the RMC-WO intervention was explicitly designed to: a) engage the offender in the process of change, b) assist the offender in understanding her behavior and become committed to behavioral change, and c) assist the offender in learning to manage her behavior over time.
The high follow-up and intervention participation rates observed in this trial demonstrate the feasibility of engaging women offenders, without the threat of punishment, in monthly checkups following release from jail. Consistent with earlier studies of women offenders (Guydish et al 2011), results also document the high substance relapse rates during the first 90 days post-release demonstrating the need for aggressive linkages to community based treatment. The rates of follow-up, intervention and relapse are similar to prior experiments with RMC (Dennis et al., 2003; Dennis and Scott, 2012; Scott et al., 2005; Scott and Dennis, 2009, 2010, 2011). The rates of treatment participation were actually higher than these prior studies in both conditions.
Women who received Recovery Management Checkups were significantly more likely to participate in community-based substance abuse treatment and return to treatment significantly sooner than women in the control group. These findings provide support for using RMC as a non-criminal justice involved intervention to successfully link women offenders to post-release community-based treatment.
While there were no significant effects during the first 90 days following release of RMC on abstinence, HIV risk behavior, or recidivism, it is unknown whether continued receipt of the checkups beyond the first 90 days will eventually impact these important outcomes. Given that for many addiction is a chronic relapsing condition it may be that additional treatment or a different type of treatment may be needed. In the previous two RMC experiments, it required multiple exposures to RMC over 12 to 18 months before RMC was associated with increased abstinence. The current trial will continue to conduct RMCs quarterly through 3 years post-release, which may produce an effect similar to the prior two trials. As more data becomes available, we will be able to test these associations with temporal order and explore the extent to which they mediate an effect of RMC on the abstinence, HIV risk behaviors and recidivism, should those be observed over 3 years.
4.1 Generalizability and Limitations
While the study has several strengths including large sample size, high follow-up rates, excellent implementation, multiple sources of data, and standardized measures, it is also important to recognize its limitations. It is based on a single-site trial from a large urban jail with a predominately minority female population; thus, needs to be replicated in more diverse sites and populations. The current study focused on a short time period, the first 90 days post-release, which may not provide adequate exposure to the intervention. In addition, this intervention did not target the many women who were released from jail within 14 days or fewer days limiting its generalizability.
4.2 Conclusions and Next Steps
Substance use appears to lock women into patterns of criminal activity that are severe and dynamic (Inciardi et al., 1997) and it, too often, prevents them from completing their education, securing employment, obtaining adequate housing, and providing parental support to their children. Recovery management checkups provided during the first 90 days of this trial successfully linked women to treatment upon release to the community. For those who received treatment, their subsequent abstinence was linked to reduced illegal activity and HIV risk.
Access to and retention in community-based treatment post-release would be adequate if the nature of addiction was acute. However, evidence suggests that many, if not most, substance users who enter publicly-funded treatment suffer from a more chronic condition whereby they cycle through periods of relapse, treatment reentry, incarceration and recovery (Scott and Dennis, 2009, 2011). These cyclical periods often last for several years, particularly when accompanied by multiple co-occurring conditions. While these findings were positive, the next challenge is to determine the feasibility of providing quarterly checkups over longer periods of time and observe whether this model remains an effective intervention for linking the women to treatment and whether, over time, RMC affects abstinence, HIV risk behaviors and recidivism. Moreover, as with any intervention the knowing more about the costs associated with it is critical. While results are not available at this time, there is a cost and cost effectiveness study currently underway.
Acknowledgments
We gratefully acknowledge Rachael Bledsaw, Nancy Dudley, Rod Funk Lilia Hristova, Lisa Nicholson, Joan Unsicker, and Belinda Willis for assistance in preparing the manuscript, as well as the Chestnut research staff, Cook County Jail Division 17 staff, Haymarket clinical staff and families who participated in the study..
Role of Funding Source: Financial assistance for this study was provided by the National Institute on Drug Abuse (NIDA; grant number R01 DA 021174). The opinions represented here are those of the authors and to not represent official positions of the government. Comments can be directed Dr. Christy K Scott, Chestnut Health Systems, 221 W. Walton; Chicago, IL60610; Phone: (312) 664-4321; Fax: 312-664-4324; Email: cscott@chestnut.org .
Footnotes
ClinicalTrials.gov ID: NCT01334164
Contributors: Dr. Scott led the design and implementation of the intervention and the field work. Dr. Dennis led the instrumentation and analysis. They both participated in all aspects of developing this paper.
Conflicts of Interests: No conflicts of interest declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams SM, Peden AR, Hall LA, Rayens MK, Staten RR, Leukefeld CG. Predictors of retention of women offenders in a community-based residential substance abuse treatment program. J Addict Nurs. 2011;22:103–116. [Google Scholar]
- Abram KM, Teplin LA, McClelland GM. Comorbidity of severe psychiatric disorders and substance use disorders among women in jail. Am J Psychiatry. 2003;160:1007–1010. doi: 10.1176/appi.ajp.160.5.1007. [DOI] [PubMed] [Google Scholar]
- Baseman J, Ross M, Williams M. Sale of sex for drugs and drugs for sex: an economic context of sexual behavior for STDs. Sex Transm Dis. 1999;26:444–449. doi: 10.1097/00007435-199909000-00005. [DOI] [PubMed] [Google Scholar]
- Belenko S, Langley S, Crimmins S, Chaple M. HIV risk behaviors, knowledge, and prevention education among offenders under community supervision: a hidden risk group. AIDS Educ Prev. 2004;16:367–385. doi: 10.1521/aeap.16.4.367.40394. [DOI] [PubMed] [Google Scholar]
- Bloom B, Owen B, Covington S. A Theoretical Basis for Gender-Responsive Strategies in Criminal Justice. Paper presented at the American Society of Criminology Annual Meeting; Chicago, IL. 2002. [Google Scholar]
- Bloom B, Owen B, Covington S. Women offenders and the gendered effects of public policy. Rev Policy Res. 2004;21:31–48. [Google Scholar]
- Bond L, Semaan S. At risk for HIV infection: incarcerated women in a county jail in Philadelphia. Women Health. 1996;24:27–45. doi: 10.1300/j013v24n04_02. [DOI] [PubMed] [Google Scholar]
- Bureau of Justice Statistics. Prison statistics: Summary Findings. U.S. Department of Justice; Washington D.C: 2005. [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS surveillance report, 2003. 15. U.S. Department of Health and Human Services; Georgia: 2004. [Google Scholar]
- Charpentier PA. Urn randomization program gRand v1.10. Yale University; Connecticut: 2003. [Google Scholar]
- Dennis ML, Dawud-Noursi S, Muck RD, McDermeit IM. The need for developing and evaluating adolescent treatment models. In: Steven SJ, Morral AR, editors. Adolescent Substance Abuse Treatment in the United States: Exemplary Models from a National Evaluation Study. Haworth Press; New York: 2003. pp. 3–34. [Google Scholar]
- Dennis ML, Lennox RD, Foss M. Practical power analysis for substance abuse health services research. In: Bryant KJ, Windle M, West SG, editors. The Science of Prevention: Methodological Advances from Alcohol and Substance Abuse Research. American Psychological Association; Washington, D.C: 1997. pp. 367–404. [Google Scholar]
- Dennis ML, Scott CK. Managing addiction as a chronic but treatable condition. Addict Sci Clin Pract. 2007;4:45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Scott CK. Four-year outcomes from the Early Re-Intervention Experiment (ERI) with recovery management checkups (RMC) Drug Alcohol Depend. 2012;121:10–17. doi: 10.1016/j.drugalcdep.2011.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Eval Program Plann. 2003;26:339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Titus JC, White M, Unsicker J, Hodgkins D. Global Appraisal of Individual Needs (GAIN): Administration Guide for the GAIN and Related Measures. Chestnut Health Systems; Illinois: 2003. Version 5 ed. [Google Scholar]
- El-Bassel N, Gilbert L, Schilling RF, Ivanoff A, Borne D. Correlates of crack abuse among drug-using incarcerated women: psychological trauma, social support, and coping behavior. Am J Drug Alcohol Abuse. 1996;22:41–56. doi: 10.3109/00952999609001644. [DOI] [PubMed] [Google Scholar]
- Fazel S, Danesh J. Serious mental disorder in 23 000 prisoners: a systematic review of 62 surveys. Lancet. 2002;359:545–550. doi: 10.1016/S0140-6736(02)07740-1. [DOI] [PubMed] [Google Scholar]
- General Accounting Office. Women in prison: Issues and challenges confronting US correctional systems. United States General Accounting Office; Washington D.C: 1999. [Google Scholar]
- Grella CE, Annon JJ, Anglin MD. Drug use and risk for HIV among women arrestees in California. AIDS Behav. 2000;4:289–295. [Google Scholar]
- Grella CE, Scott CK, Foss MA. Gender differences in long-term drug treatment outcomes in Chicago PETS. J Subst Abuse Treat. 2005;28 (Suppl 1):S3–S12. doi: 10.1016/j.jsat.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Guydish J, Chan M, Bostrom A, Jessup MA, Davis TB, Marsh C. A randomized trial of probation case management for drug-involved women offenders. Crime Delinq. 2011;57:167–198. doi: 10.1177/0011128708318944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison L, Martin SS. Residential Substance Abuse Treatment for State Prisoners: Implementation Lessons Learned. National Institute of Justice; Washington, D.C: 2003. [Google Scholar]
- Henderson DJ. Drug abuse and incarcerated women: a research review. J Subst Abuse Treat. 1998;15:579–587. doi: 10.1016/s0740-5472(97)00319-x. [DOI] [PubMed] [Google Scholar]
- Inciardi JA, Martin SS, Butzin CA, Hooper RM, Harrison LD. An effective model of prison-based treatment for drug involved offenders. J Drug Issues. 1997;27:261–278. [Google Scholar]
- Jordon L Missouri Coalition of Community Mental Health Centers. The Future of Comprehensive Alcohol and Substance Abuse Treatment for Medicaid Eligible Women and Children in Missouri. Missouri Coalition of Community Mental Health Centers; Missouri: 1996. [Google Scholar]
- Kranzler HR, Tennen H, Babor TF, Kadden RM, Rounsaville BJ. Validity of the longitudinal, expert, all data procedure for psychiatric diagnosis in patients with psychoactive substance use disorders. Drug Alcohol Depend. 1997;45:93–104. doi: 10.1016/s0376-8716(97)01349-5. [DOI] [PubMed] [Google Scholar]
- Langan NP, Pelissier BMM. Gender differences among prisoners in drug treatment. J Subst Abuse. 2001;13:291–301. doi: 10.1016/s0899-3289(01)00083-9. [DOI] [PubMed] [Google Scholar]
- Lennox RD, Dennis ML, Scott CK, Funk RR. Combining psychometric and biometric measures of substance use. Drug Alcohol Depend. 2006;83:95–103. doi: 10.1016/j.drugalcdep.2005.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magura S, Rosenblum A, Lewis C, Joseph H. The effectiveness of in jail methadone maintenance. J Drug Issues. 1993;23:75–99. [Google Scholar]
- Maruschak LM. HIV in prisons, 2001. Bureau of Justice Statistics; Washington D.C: 2004. [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- McClelland GM, Teplin LA, Abram KM, Jacobs N. HIV and AIDS risk behaviors among female jail detainees: implications for public health policy. Am J Public Health. 2002;92:818–825. doi: 10.2105/ajph.92.5.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minton TD. Jail Inmates at Midyear 2010 – Statistical Tables. Bureau of Justice Statistics; Washington, D.C: [Accessed on 2/14/12]. http://www.bjs.gov/index.cfm?ty=pbdetail&iid=2375. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Revised Global Scales: Motivational Interviewing Treatment Integrity 3.1.1. University of New Mexico Center on Alcoholism, Substance Abuse and Addictions (CASAA); New Mexico: 2010. [Accessed on 3/26/12]. from http://casaa.unm.edu/download/MITI3_1.pdf. [Google Scholar]
- Nicassio PM, Smith TW, editors. Managing Chronic iIlness: A Biopsychosocial Perspective. American Psychological Association; Washington, D.C: 1995. [Google Scholar]
- Prendergast M, Wexler HK. Correctional substance abuse programs in California: a historical perspective. Prison J. 2004;84:8–35. [Google Scholar]
- Reif S, Wechsberg WM, Dennis ML. Reduction of co-occurring distress and HIV risk behaviors among women substance abusers. J Prev Interv Community. 2001;22:61–80. [Google Scholar]
- Rotter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36:1138–1161. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- Schilling R, El-Bassel N, Ivanoff A, Gilbert L, Su K, Safyer SM. Sexual risk behavior of incarcerated, drug-using women, 1992. Public Health Rep. 1994;109:539–547. [PMC free article] [PubMed] [Google Scholar]
- Scott CK. A replicable model for achieving over 90% follow-up rates in longitudinal studies of substance abusers. Drug Alcohol Depend. 2004;74:21–36. doi: 10.1016/j.drugalcdep.2003.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CK, Dennis ML. Recovery Management Check-ups (RMC) Procedure Manual. Chestnut Health Systems; Illinois: 2008. [Google Scholar]
- Scott CK, Dennis ML. Results from two randomized clinical trials evaluating the impact of quarterly recovery management checkups with adult chronic substance users. Addiction. 2009;104:959–971. doi: 10.1111/j.1360-0443.2009.02525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CK, Dennis ML. Recovery management checkups with adult chronic substance users. In: Kelly JF, White William L, editors. Addiction Recovery Management: Theory, Science, and Practice. Springer Science; New York: 2011. pp. 87–102. [Google Scholar]
- Scott CK, Dennis ML, Foss MA. Utilizing recovery management checkups to shorten the cycle of relapse, treatment reentry, and recovery. Drug Alcohol Depend. 2005;78:325–338. doi: 10.1016/j.drugalcdep.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CK, Foss MA, Dennis ML. Pathways in the relapse, treatment, and recovery cycle over three years. J Subst Abuse Treat. 2005;28:S63–S72. doi: 10.1016/j.jsat.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Drugs Suppl. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Singer MI, Bussey J, Song LY, Lunghofer L. The psychosocial issues of women serving time in jail. Soc Work. 1995;40:103–113. [PubMed] [Google Scholar]
- Taxman FS, Perdoni ML, Harrison LD. Drug treatment services for adult offenders: the state of the art. J Subst Abuse Treat. 2007;32:329–254. doi: 10.1016/j.jsat.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM. Prevalence of psychiatric disorders among incarcerated women. I pretrial jail detainees. Arch Gen Psychiatry. 1996;53:505–12. doi: 10.1001/archpsyc.1996.01830060047007. [DOI] [PubMed] [Google Scholar]
- Veysey BM. Specific Needs of Women Diagnosed with Mental Illnesses in US jails. Sage Publications; Tousand Oaks: 1997. [Google Scholar]
- Wechsberg WM, Lam WKK, Zule WA, Bobashev G. Efficacy of a woman-focused intervention to reduce HIV risk and increase self-sufficiency among African American crack abusers. Am J Public Health. 2004;94:1165–1173. doi: 10.2105/ajph.94.7.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, McLellan T, Barthwell A, Blitz C, Catalano R, Chalk M, Chinnia L, Collins RL, Compton W, Dennis ML, Frank R, Hewitt W, Inciardi JA, Lightfoot M, Montoya I, Sterk CE, Wood J, Pintello D, Volkow M, Michaud SE. Report of the Blue Ribbon Task Force on Health Services Research at the National Institute on Drug Abuse. National Institute on Drug Abuse; Baltimore, Maryland: 2004. [Google Scholar]
- Wellisch J, Anglin MD, Prendergast ML. Numbers and characteristics of drug-using women in the criminal justice system: implications for treatment. J Drug Issues. 1993;23:7–30. [Google Scholar]
- Wellisch J, Prendergast ML, Anglin MD. Needs assessment and services for drug-abusing women offenders: results from a national survey of community-based treatment programs. Women Crim Justice. 1996;8:27–61. [Google Scholar]
- Wexler HK, Prendergast ML, Melnick G. Introduction to a special issue: correctional drug treatment outcomes-Focus on California. Prison J. 2004;84:3–7. [Google Scholar]