Abstract
Microneedles were first conceptualized for drug delivery many decades ago, but only became the subject of significant research starting in the mid-1990’s when microfabrication technology enabled their manufacture as (i) solid microneedles for skin pretreatment to increase skin permeability, (ii) microneedles coated with drug that dissolves off in the skin, (iii) polymer microneedles that encapsulate drug and fully dissolve in the skin and (iv) hollow microneedles for drug infusion into the skin. As shown in more than 350 papers now published in the field, microneedles have been used to deliver a broad range of different low molecular weight drugs, biotherapeutics and vaccines, including published human studies with a number of small-molecule and protein drugs and vaccines. Influenza vaccination using a hollow microneedle is in widespread clinical use and a number of solid microneedle products are sold for cosmetic purposes. In addition to applications in the skin, microneedles have also been adapted for delivery of bioactives into the eye and into cells. Successful application of microneedles depends on device function that facilitates microneedle insertion and possible infusion into skin, skin recovery after microneedle removal, and drug stability during manufacturing, storage and delivery, and on patient outcomes, including lack of pain, skin irritation and skin infection, in addition to drug efficacy and safety. Building off a strong technology base and multiple demonstrations of successful drug delivery, microneedles are poised to advance further into clinical practice to enable better pharmaceutical therapies, vaccination and other applications.
1. Introduction
Most biotherapeutics and vaccines are injected using a hypodermic needle. Injection provides a low-cost, rapid and direct way to deliver almost any type of molecule into the body. However, hypodermic needles cannot be easily used by patients themselves and are therefore utilized primarily in the clinic or at home by patients who have received special training on correct injection method, safe needle disposal, and other issues [1]. Patient compliance is further limited by pain and needle-phobia experienced by many patients [2–3]. Spread of bloodborne pathogens by needle reuse is also a major concern, especially in developing countries [4–5]. Oral delivery largely overcomes these problems, but many drugs cannot be given by this route due to poor absorption and drug degradation in the gastrointestinal tract and liver [6]. Other routes of administration have also been investigated [7–8], but none offer the broad effectiveness of direct injection using a needle.
Rather than avoiding needles, we and others have proposed shrinking the needle to micron dimensions in order to make use of its powerful delivery capabilities while improving patient compliance and safety. As a micron-scale device, a microneedle should be large enough to deliver almost any drug or small particulate formulation, but still be small enough to avoid pain, fear and the need for expert training to administer. In addition, a microneedle allows precise tissue localization of delivery, such as within the skin, the suprachoroidal space of the eye, and the cell nucleus.
Most applications of microneedles studied to date have emphasized drug and vaccine delivery to the skin. Conventional transdermal delivery is limited by the barrier properties of the outermost skin layer, the stratum corneum [9]. Various chemical, biochemical and physical methods have been studied to increase skin permeability. However, chemical and biochemical methods do not appear to be broadly useful for delivery of biotherapeutics and vaccines across skin. While physical methods have greater promise for delivery of macromolecules, they typically involve the use of sophisticated devices that are relatively large, costly and require training to use. Microneedles, in contrast, can be prepared as a low-cost patch that is simple for patients to apply for delivery of biomacromolecules, as discussed further in this review. Targeting vaccine delivery to antigen-presenting cells in the skin using microneedles is also of particular interest [10].
Other applications of microneedles have also been explored. Drug delivery to the eye, especially via the suprachoroidal space, has received recent attention [11]. As an extension of micropipette techniques, microneedles have been used to deliver molecules into cells and their nuclei, among other laboratory applications [12–13].
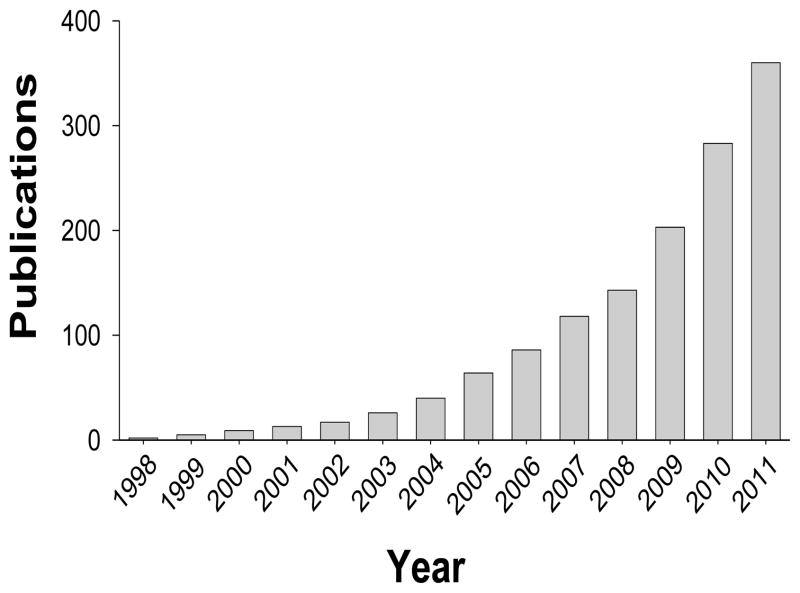
Since the first papers were published on drug delivery using microneedles in the late 1990’s, research activity has grown exponentially (Figure 1), which has lead to published clinical trials, approved products and an active community of academic and industry researchers in the field today. This article reviews this body of work, building upon previous review articles in the field [10, 14–33].
Figure 1.
Cumulative number of publications on microneedles. The number of publications was determined by searching the PubMed database (http://www.ncbi.nlm.nih.gov/pubmed/) and Web of Science (http://apps.webofknowledge.com) on 25 November 2011 using the search terms “microneedle”, “microfabricated needle”, and “nanopatch”. Conference proceedings were excluded.
2. Fabrication of microneedles
Individual small needles have been hand-crafted for research purposes for decades [34] and already in the 1970’s low-cost microneedle arrays were envisioned for drug delivery [35]. However, it was not until the 1990’s that the microelectronics industry provided the microfabrication tools needed to make microneedles suitable for pharmaceutical applications [36].
Given the field’s beginnings using microelectronics industry technology, the first microneedles were fabricated out of silicon. Since then, microneedles have been fabricated out of numerous materials, including metal, polymer, glass and ceramic, and in a variety of shapes and sizes, as needed for different applications. Most microneedle fabrication methods are based on the conventional microfabrication techniques of adding, removing, and copying microstructures utilizing photolithographic processes, silicon etching, laser cutting, metal electroplating, metal electropolishing and micromolding.
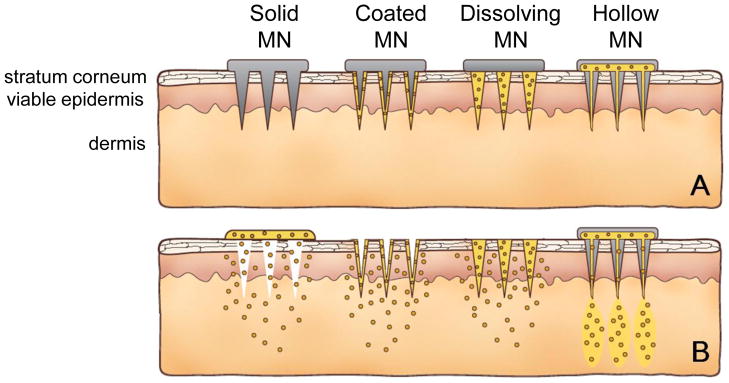
In general, microneedles can be categorized as solid microneedles for tissue pretreatment, drug-coated microneedles, dissolving microneedles, and hollow microneedles. As shown schematically in Fig. 2, each of these microneedle designs enables drug delivery by different mechanisms.
Figure 2.
Methods of drug delivery to the skin using microneedles (MN). Microneedles are first applied to the skin (A) and then used for drug delivery (B). Solid microneedle are used as a pretreatment, after which drug can diffuse through residual holes in skin from a topical formulation (solid MN). After insertion of drug-coated microneedles into the skin, the drug coating dissolves off the microneedles in the aqueous environment of the skin (coated MN). Drug-loaded microneedles are made of water-soluble or biodegradable materials encapsulating drug that is released in the skin upon microneedle dissolution (dissolving MN). Hollow microneedles are used to inject liquid formulations into the skin (hollow MN).
Solid microneedles can be used as a skin pretreatment. After inserting and removing the microneedles to form micron-scale pores in the skin surface, a drug formulation can be applied to the skin for slow diffusion of drug through the pores and into the body.
Microneedles can also be coated with a drug typically using a water-soluble formulation. After insertion of microneedles into the skin, the drug coating is dissolved off the microneedles and into the skin, after which the microneedles are removed.
Alternatively, microneedles can be made completely out of water-soluble or biodegradable polymer that encapsulates the drug within the microneedle matrix. In this way, the microneedles completely dissolve or degrade in the skin, thereby releasing the encapsulated drug payload and leaving behind no sharps waste, (i.e., because the microneedles have dissolved away).
Finally, hollow microneedles can be used for infusion of liquid formulations into the skin or, alternatively, for diffusion into the skin through the needle bore.
These examples all describe delivery of drugs to the skin. However, other compounds, such as vaccines or diagnostic agents, can also be delivered. In addition, other tissues besides the skin can be targeted, such as the eye.
2.1. Solid microneedles for skin pretreatment
Microneedles can be used as a pretreatment for pore formation in the skin (Fig. 2, skin pretreatment). Sharp microneedles penetrate into or scrape the skin in order to make holes through which drugs can transport, either for local effect in the skin or for systemic delivery after uptake by skin capillaries. The drug can be applied to the skin surface over the pores using a drug-loaded patch, as is commonly used in conventional transdermal drug delivery, or using a semi-solid topical formulation, such as an ointment, cream, gel or lotion, as is commonly used for other skin treatments [37].
2.1.1. Fabrication of solid microneedles
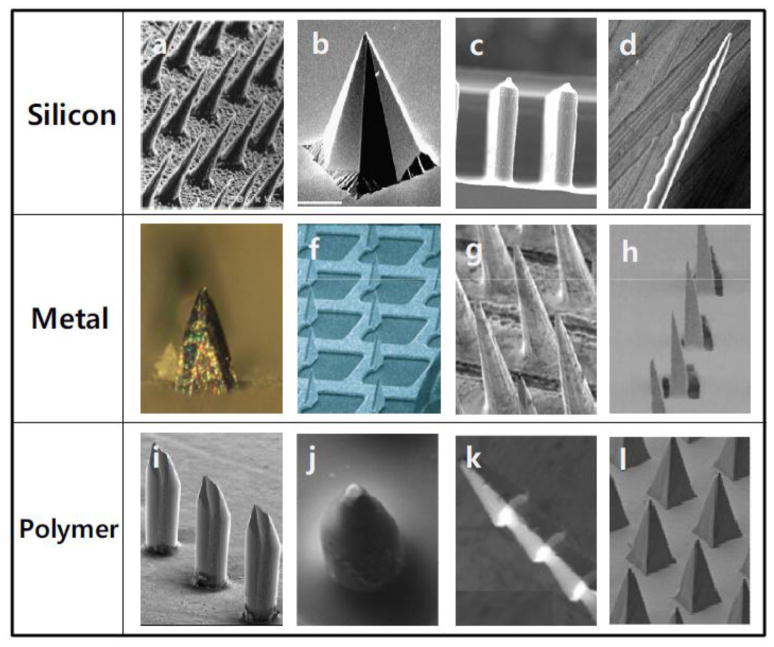
The fabrication of solid microneedles has focused on providing sufficient mechanical strength through choice of microneedle material and geometry and reducing the force needed to insert microneedles into tissue by increasing tip sharpness. Solid microneedles have been fabricated out of various materials, including silicon [38–40]; non-degradable polymers such as photolithographic epoxy {Ami, 2011 #715;Fernández, 2009 #738;Aoyagi, 2008 #688;Yoon, 2006 #537;Park, 2007 #237}, a copolymer of methylvinylether and maleic anhydride (PMVE/MA) [41], polycarbonate [42] and polymethylmethacrylate (PMMA) [43]; biodegradable polymers such as poly-lactic-co-glycolic acid (PLGA), polyglycolic acid (PGA) and polylactic acid (PLA) [44]; water-soluble compounds including maltose [45]; metals including stainless steel [46–47], titanium [48], tantalum [49] and nickel [50]; and ceramics [51–52] (Fig. 3).
Figure 3.
Solid microneedles made of silicon, metal and polymer. Images reproduced with permission from references (a) [39], (b) [343], (c) [59], (d) [344], (e) [312], (f) [53], (g) [67], (h) [52], (i) [49], (j) [71], (k) [43], and (l) [87].
2.1.1.1. Silicon microneedles
The microneedle fabrication process depends on the needle material and geometry. Short silicon microneedles have been prepared using a silicon dry-etching process based on reactive ion etching with a chromium mask [40, 53], as well as isotropic etching in an inductively coupled plasma etcher [54]. Anisotropic wet etching of crystalline silicon using an alkaline solution has also been utilized to obtain solid microneedles [39, 55–56]. Wet-etching methods can lower fabrication cost compared to dry etching, but the geometry of microneedles is restricted by anisotropic etching along crystal planes by the KOH etchant [57]. To overcome this limit of wet etching, isotropic dry etching and anisotropic wet etching methods have been combined [54]. As an additional approach, microneedles have been fabricated to serve as neural probes by dicing a silicon substrate to create a grid pattern of deep grooves and then acid etching the resulting pillars to create sharpened probe tips [58–61].
2.1.1.2. Metal microneedles
Metal microneedles have been prepared by three-dimensional laser ablation [49, 62], laser cutting [63], wet etching [48, 64], and metal electroplating methods [65–66]. Rows of solid metal microneedles were fabricated directly, whereas two-dimensional arrays of microneedles have been made by cutting microneedles into stainless steel and titanium metal sheets and then bending them at a angle out of the plane of the sheet. Two-dimensional metal microneedles have also been prepared by electroplating or electroless-plating of metal onto positive or negative microneedle molds [65].
2.1.1.3. Polymer microneedles
Microneedles have been made by photolithography using optically curable polymers, which are then typically employed as master structures for replication by molding. The ultraviolet (UV)-curable polymer SU-8 has been utilized extensively to fabricate microneedles [67–69]. By using a combination of microlenses on a glass substrate and inclined rotation of the substrate, the path of UV light through the SU-8 was made to taper, thereby defining microneedle structures with sharp tips.
PMMA has also been used to make microneedle arrays by employing an inclined deep X-ray exposure and vertical X-ray exposure known as the lithography, electroplating and molding (LIGA) technique [70–71]. Using these approaches, microneedles can be fabricated as tall as a few millimeters with a high aspect ratio using standard contact lithography equipment due to the low optical adsorption of the polymers in the UV range of 390 nm. A two-photon-initiated polymerization method was utilized to fabricate three-dimensional microstructures including microneedles. In this approach, a near-infrared ultrashort-pulsed laser was focused into a photocurable resin to form three-dimensional microstructures using a sequential layer-by-layer fabrication technique [20, 72–73].
These UV-curable polymers have weaker mechanical strength compared to silicon and metal; thus, they have been used primarily as master structures for making molds. Typically, a silicone polymer (polydimethylsiloxane, PDMS) is poured onto the microneedle master structure to make an inverse mold after curing. Polyvinylalcohol (PVA), silicon and aluminum have also been used as mold materials to replicate polymer microneedles [74–75]. The mold can then be filled at elevated temperature with molten or softened thermoplastics such as polycarbonate [71] and PMMA [76] to produce non-degradable microneedles upon cooling and solidification. In addition, a variety of biodegradable polymers and water-soluble polymers have been micromolded primarily to encapsulate drugs within the microneedle matrix for subsequent release in the skin, as discussed below (see section 2.3. Dissolving Microneedles).
2.1.1.4. Ceramic microneedles
Ceramic microneedles have been fabricated using ceramic micromolding and sintering. Solid ceramic microneedles were prepared by micromolding an alumina slurry using a PDMS microneedle mold and ceramic sintering [51]. Ceramic microneedles have also been made lithographically using a two-photon-induced polymerization approach. A focused laser was scanned within a photosensitive polymer-ceramic hybrid resin using a galvano scanner and a micropositioning system to induce polymerization locally in the shape of the microneedles [52, 77–78].
2.1.1.5. Microneedle rollers
Most solid microneedles have been prepared on flat, planar substrates, such that all microneedles are simultaneously pressed into the skin. Some microneedles have been prepared on a cylindrical surface and applied to the skin as a roller. Microneedle rollers are commercially available and can be used to treat large areas of skin. The microneedle roller was introduced to enhance skin restoration, facilitate collagen induction for cosmetic applications [79–83], and increase skin permeability for drug applications [84–86]. Microneedle rollers have been made by fabrication of planar microneedle arrays and then applying them onto the surface of cylindrical rollers [87] or fabrication of rows of microneedles or individual microneedles and assembling them onto a roller [71].
2.2. Coated microneedles
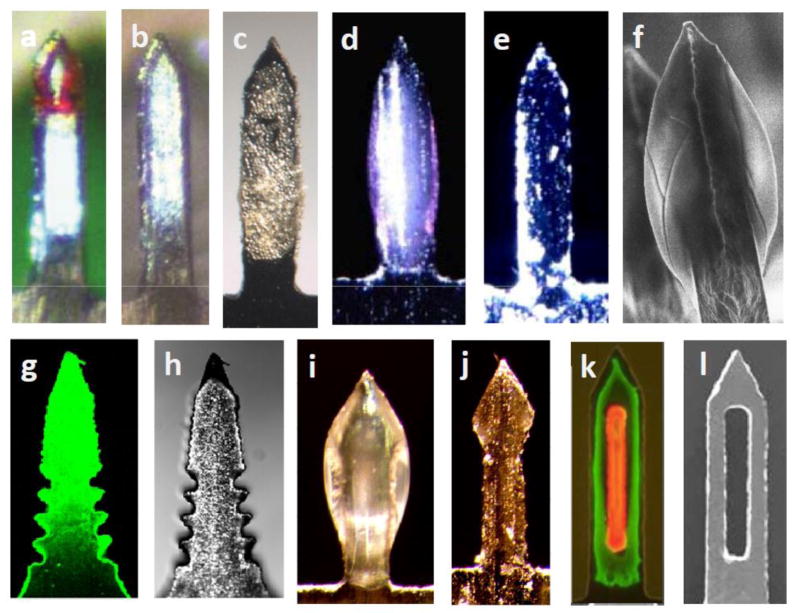
Solid microneedles can be used not only as piercing structures, but also as vehicles to carry and deposit drug within the skin or other tissue (Fig. 2, drug-coated microneedles). This can be done by coating microneedles with a drug in a formulation suitable for coating and subsequent dissolution (Fig. 4). In this way, the desired dose of the drug is delivered into tissue quickly upon insertion of the microneedles. The drug dose that can be administered this way is limited to the amount that can be coated onto the tip and shaft of the microneedles, which is typically less than 1 mg for small microneedle arrays [88].
Figure 4.
Coated microneedles made of metal and polymer after (a,c,d,f,g,i,k) and before (b,e,h,j,l) coating.. Images reproduced with permission from references (a,b) [90], (c) [51], (d,e) [91], (f) [96], (g,f) [98], (i,j) [229], and (k,l) [99].
2.2.1. Microneedle coating methods
Microneedles have been coated by a variety of processes, most of which involve dipping or spraying the microneedles using an aqueous solution often formulated to have increased viscosity to retain more of the formulation on the microneedles during drying; a surfactant to facilitate wetting of the microneedle surface; a drug, vaccine or other active agent; and in some cases a stabilizing agent to protect the drug from damage during drying and storage [46, 88–91]. Coating has been carried out by dipping once or repeatedly into a large bath of coating solution [92], into microwells of coating solution for each individual microneedle [46] and into a thin film of coating solution formed on the surface of a roller [89]. The latter two approaches were designed to better localize the coating to the microneedles or just their tips without contaminating the base substrate.
Layer-by-layer coating techniques have also been applied to microneedle coating [93–94]. DNA or protein molecules were coated onto metal and polymer microneedles by alternately dipping into two solutions containing oppositely charged solutes, such as negatively charged DNA and positively charged polymer, to form a polyelectrolyte multilayer. As another alternative, coating solution has been sprayed onto silicon microneedles. In one approach, an angled gas jet was used to spray the surface of individual microneedle shafts from a reservoir created on the microneedle array substrate at the base of the microneedles [95]. In another approach, spray coating was applied using an atomizer [96].
2.2.2. Microneedle coating formulations
Microneedle coating formulations typically account for the following considerations [46, 88]. First, controlled wetting and spreading of drug solution on the microneedle substrate is critical to obtain a uniform coating on the microneedle surface. Increased viscosity and reduced contact angle of the coating solution to the substrate (e.g., by addition of surfactant) can improve wetting and coating thickness. Second, the coating formulation should be water-soluble, not only for effective coating in an aqueous formulation but also for rapid and complete coating dissolution into the skin, which is an aqueous environment. Third, the mechanical strength of a dried coating should be high enough to keep the coating adherent to the microneedle during insertion into skin. Fourth, coating solution excipients and solvent should be safe for human use and should not damage coated drugs. Finally, the coating process should also not damage the drug and should be compatible with industrial pharmaceutical manufacturing processes.
A number of different surfactants and thickening agents have been used to facilitate microneedle coating. Surfactants including Lutrol F-68 NF [46], Tween 20 [97], Poloxamer 188 [95], and Quil-A [95] were used to increase spreading on microneedle surfaces. Thickening agents such as carboxymethylcellulose sodium salt (CMC) [46], methylcellulose [95], sucrose [88], hyaluronic acid [88], sodium alginate [88], polyvinylpyrrolidone (PVP) [88], glycerol [88], PLGA [88], alginic acid [98], xanthan gum [88], gum ghatti [98], karaya gum [98], and poly[di(carboxylatophenoxy)phosphazene] [90] were used to increase coating thickness. Stabilizers like trehalose, sucrose, glucose, inulin, and dextrans were added to coating solution formulations to reduce damage to bioactive drugs during the coating/drying process [91].
In addition to optimizing coating formulations, microneedle design was also improved to facilitate delivery from coated microneedles, including development of three-dimensional groove-embedded microneedles to increase coating amounts [99] and pocketed microneedles to facilitate better drug targeting in skin and to administer liquid coatings [100].
2.2.3. Compounds coated onto microneedles
These coating techniques have been shown to be versatile. Small molecules have been coated, including fluorescein [100], sulforhodamine [101], calcein [46], vitamin B [46], pilocarpine [101], and lidocaine [102]. Macromolecules have also been coated, including insulin [88], desmopressin [97], parathyroid hormone PTH(1-34) [89], bovine pancreatic ribonuclease [93], ovalbumin [95], bovine serum albumin [103], horseradish peroxidase [104], Alex Fluor 488-conjugated goat-anti-mouse IgG [99], and antisense oligonucleotises [105]. Vaccines have also been coated, including hepatitis B surface antigen [90], inactivated influenza virus [91], influenza virus-like particle [106], recombinant trimeric soluble influenza hemagglutinin [107], inactivated human papillomavirus [108], inactivated chikungunya virus [109] and bacillus Calmetter-Guérin (BCG) [110]. Different kinds of DNA have been coated, such as plasmid DNA encoding enhanced green fluorescent protein [93], as well as DNA encoding protein vaccines against hepatitis C virus [111], herpes simplex virus [112] and West Nile virus [109]. Finally, microneedles have been coated with micron-scale particles, such as BaSO4 particles (1 μm) and latex particles (10 μm) [46].
2.3. Dissolving microneedles
In contrast to coated microneedles, polymer microneedles have been developed to completely dissolve in the skin and thereby leave behind no biohazardous sharps waste after use (Fig. 2, drug-loaded microneedles). These microneedles are typically made solely of safe, inert, water-soluble materials, such as polymers and sugars that will dissolve in the skin after insertion. While dissolving microneedles can be used as a skin pretreatment to increase permeability, drugs are often encapsulated inside the microneedle for release into the skin similarly to coated microneedles.
2.3.1. Dissolving microneedle fabrication methods
Dissolving microneedles have been fabricated mostly using micromolds filled by solvent casting (with water as the usual solvent), filled with a polymer melt allowed to solidify in the mold, and in-situ polymerization of liquid monomer in the mold (Fig. 5). Drawing methods of fabrication have also been used with polymer/sugar melts and polymer/sugar solutions. Various materials including CMC [113–114], chondroitin sulfate [115–123], dextran [117, 122, 124], dextrin [117, 125–126], PVP [127–130], PVA [129–131], PLGA [44, 132], fibroin [133] and sugars [134] have been dissolved in water, filled into the mold cavities and allowed to dry, sometimes with the additional use of vacuum and/or centrifugal force.
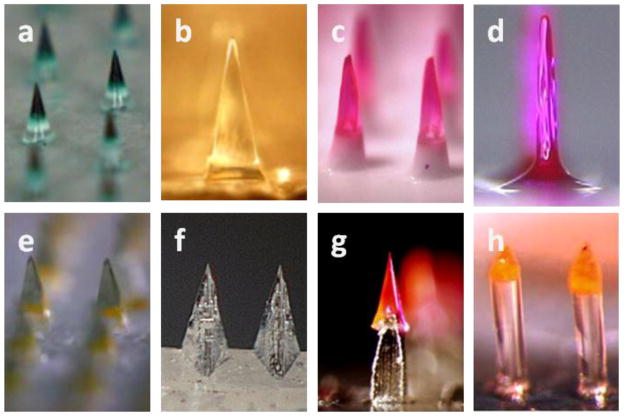
Figure 5.
Dissolving microneedles made of water-soluble polymers and biodegradable polymers. Images reproduced with permission from references (a) [113], (b) [112], (c) [127], (d) [126], (e) [140], (f) [50], (g) [119] and (h) [130].
Melted maltose has been filled in the cavities of a mold and solidified upon cooling [135]. Using a related approach, N-vinylpyrrolidone and/or methacrylic acid were added as liquid monomers into a mold and polymerized under ultraviolet radiation [127]. In contrast to these highly water-soluble, rapidly dissolving microneedles, polymeric microneedles designed for slow biodegradation in the skin have also been fabricated by micromolding polylactic acid, polyglycolic acid and their copolymers as melts using PDMS and silicon molds [44, 74, 136–137].
Another fabrication method draws up liquid formulations to form tapered microneedle structures that solidify in position. Maltose microneedles were formed as multi-needle arrays using a controlled, stepwise drawing technique enabled by a microfabricated device [138]. Microneedles made of dextrin, chondroitin sulfate and albumin were similarly fabricated one-by-one by drawing using pipette tips [125–126]. An ultrasonic welding method was also introduced to form biodegradable polymer microneedles out of polymer particles welded together without bulk heating of the polymer, which resulting in minimal damage to encapsulated compounds [139–140].
2.3.2. Dissolving microneedle formulations and designs
Heat-sensitive compounds like proteins and antigens should be encapsulated in microneedles and solidified at moderate conditions that will not damage their activity. For example, dissolving microneedles were fabricated out of hydrophilic polymers cast in an aqueous solution at room temperature and at atmospheric pressure or under vacuum. CMC microneedles were fabricated under centrifugation to avoid formation of small voids in the microneedle matrix that weaken the structure [113]. Human growth hormone was encapsulated in sodium chondroitin sulfate microneedles in a vacuum dryer [122]. Erythropoietin (EPO) and insulin were encapsulated in other hydrophilic polymers such as dextrin and chondroitin by forming threads using pipette tips at room temperature [125–126].
Most dissolving microneedles in the literature need to be inserted into skin for at least 5 min to fully dissolve. To shorten this time, arrowhead microneedles were designed to separate from the shaft within seconds and remain embedded in the skin for subsequent dissolution [130]. In contrast, biodegradable polymer microneedles must be inserted and remain in the skin for at least several days to effectively utilize their controlled-release degradation properties to provide controlled-release delivery in skin for up to months [132]. Microneedles encapsulating hydrogel microparticles were designed for successful separation of microneedles within less than 1 h of insertion into skin by swelling of the hydrogel microparticles [137].
Because microneedles may not insert fully into skin, it is sometimes desirable to encapsulate drugs only in the microneedle tips. Drug has been localized in microneedle tips by forming multilayered microneedles using sequential applications of different compositions of polymer solutions [122] and using a particle-based molding method [140]. Drug was also localized in tips by the addition of an air bubble at the base of each microneedle during fabrication, which prevented drug diffusion from the microneedles into the patch backing [129].
2.4. Hollow microneedles
Hollow microneedles provide a defined conduit for drug delivery into the skin or other tissue. Similar to hypodermic injection, hollow microneedles enable pressure-driven flow of a liquid formulation (Fig. 2, hollow microneedles). Pressure, and thereby flow rate, can be modulated for a rapid bolus injection, a slow infusion or a time-varying delivery rate. The liquid formulation may simplify use of existing injectable formulations for delivery using microneedles, but misses the opportunity of solid microneedle delivery methods to administer dry-state drug formulations without reconstitution to improve drug stability and the patient convenience of a patch-based delivery method. Hollow microneedles have also been used as a conduit for drug diffusion into the skin from a non-pressurized drug reservoir.
2.4.1. Hollow microneedle fabrication methods
Hollow microneedles have been fabricated directly from a material substrate using microelectromechanical systems (MEMS) techniques including laser micromachining [63], deep reactive ion etching of silicon [141–142], an integrated lithographic molding technique [143], deep X-ray photolithography [144], and wet chemical etching and microfabrication [145] (Fig. 6). Other hollow microneedle fabrication methods require multiple substrates with different chemical or physical properties to serve as sacrificial layers to obtain shell structures indirectly from a microneedle substrate.
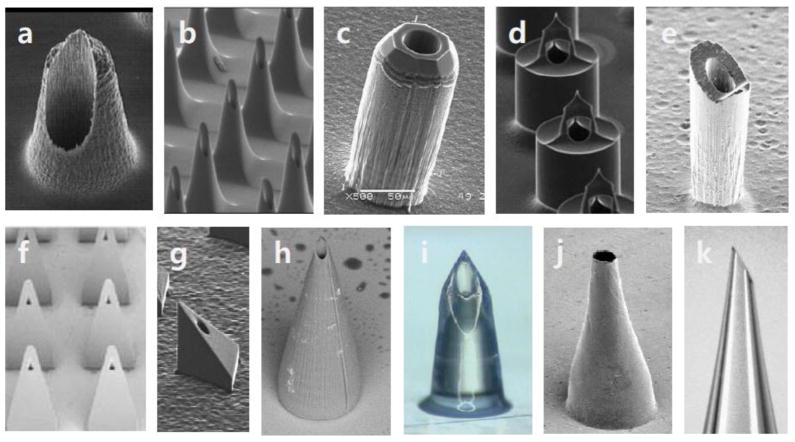
Figure 6.
Hollow microneedles made of silicon and polymers. Images reproduced with permission from references (a) [148], (b) [149], (c) [145], (d) [150], (e) [151], (f) [156], (g) [168], (h) [345], (i) [163], (j) [317], and (k) [167].
Hollow silicon microneedles were fabricated by adapting silicon-based MEMS techniques including lithographic processes, wet etching and micromachining. A SiO2 mask, wet etching and deep reactive ion etching were utilized in combination to fabricate cylindrical hollow microneedles [146] and out-of-plane hollow microneedles [142]. To obtain hollow silicon microneedles, the Bosch process was utilized to create hollow shell structures with high aspect ratio, after which isotropic [145, 146] and wet etching processes [142] were added to obtain shaper tips. Bosch deep reactive ion etching was used to fabricate cylindrical hollow microneedles out of silicon [147]. Isotropic etching and Bosch deep reactive ion etching were used together to fabricate hollow microneedles with a tapered shape [148–149]. Bosch deep reactive ion etching was combined with wet etching to obtain hollow silicon microneedles with sharp tips [145]. Deep anisotropic etching, isotropic etching and mask technique were used to fabricate cylindrical microneedles with a side-opening orifice [150]. In addition to chemical etching methods, a dicing saw was used together with deep reactive ion etching to obtain hollow silicon microneedles with sharp tips [151].
Hollow microneedles made of glass, polymer and metal have been prepared from substrates by conventional fabrication methods. Hollow glass microneedles were made by adapting traditional drawn glass micropipette techniques [152]. Hollow metal microneedle arrays were assembled from commercially available 30 gauge hypodermic needles [145]. Hollow polymer microneedles were formed by drilling to make the bore hole and milling to create the beveled tip shape out of polyphenylsulfone polymer [153]. A digital micromirror stereolithography instrument was used to fabricate hollow polymer microneedles by polymerization of liquid resin [154]. The LIGA technique was utilized to form hollow microneedles by exposing X-ray through a mask onto PMMA [155–156]. Direct two-photon polymerization in a laser-based rapid prototyping system was used to form hollow polymer microneedles [20].
Many hollow metal microneedles were fabricated using indirect methods depending on sacrificial substrates. Hollow metal microneedle arrays were made using a multiple step process, which involved backside exposure of SU-8 photoresist and conformal electroplating [69]. A micromachined polymer mold was prepared using an ultraviolet laser; the mold was then coated with nickel by electrodeposition onto a sputter-deposited seed layer, and the resulting metal microneedle arrays were released by selectively etching the polymer mold [63]. Another design of metal hollow microneedle was made by drawing lithography and metal electroplating [157].
Hot embossing combined with an ultraviolet excimer laser beam technique was introduced to make polymer hollow microneedle arrays with side opening orifices [158]. Another hollow nickel microneedle device was fabricated by a sequential process of electroless copper and nickel plating and copper wet chemical etching [159]. Hollow silicon dioxide microneedles were fabricated based on electrochemical etching of n-type silicon in hydrofluoric acid solutions [160]. Hollow metal microneedles were fabricated from a silica needle template using micro-imprinting, hot embossing, electroplating and polishing [161].
2.4.2. Injection using hollow microneedles
To generate the flow of liquid through hollow microneedles, various methods of actuating flow have been devised [162]. Hollow microneedles are commonly used with a syringe to inject liquid formulations. However, some hollow microneedle systems were integrated with an actuator. Hollow microneedles were attached to a PDMS reservoir filled with a drug [162]. Flow of liquid through hollow microneedles was controlled by CO2 gas pressure [163], a spring [164], a piezoelectric micropump [165], a piezoelectric linear servo motor [166], a syringe pump [167] and a micro-gear pump [168–169].
Currently, there are generally two types of hollow microneedle designs. One type utilizes a single microneedle, which mimics the conventional hypodermic needle [170]. The other type is an array of multiple hollow microneedles [63]. The latter type can deliver liquid formulations to a wide area all at once and, in some cases, more quickly than subcutaneous injection [164] and with higher bioavailability and possible lymphatic targeting [171]. However, if one of the microneedles has a leak, then pressure cannot be equally applied to all of the needles and fluid will not flow through all of the microneedles equally. A microfluidic interconnector was also designed and fabricated out of PMMA, and integrated with a SU-8 hollow microneedle system [172].
Rather than fabricating a microneedle, another approach involves using a 30 gauge hypodermic needle that is housed in a syringe device that exposes only 1.5 mm of the needle, thereby effectively making a short needle [173]. This device consists of this microneedle connected to a prefilled syringe designed for perpendicular insertion into the skin to achieve intradermal localization of the injection. The resulting distribution of fluid in the skin was shown to be larger than the conventional Mantoux injection control. This system also caused less injury to the papillary dermis, less pain than Mantoux injection, and was administered easily by untrained personnel.
In contrast to drug delivery applications, hollow microneedles have also been developed to extract fluids from the body [142, 149, 174–175]. Glass and silicon hollow microneedles were used to obtain interstitial fluid, and stainless steel hollow microneedles were used for blood sampling.
3. Applications of microneedles
When microneedles were first introduced for drug delivery applications, the main goal was either to increase skin permeability through a solid microneedle pretreatment or to make hollow microneedles with advanced functionality over conventional hypodermic needles (see section 5.1 Historical Perspective). Today, the applications of microneedles have been extended to many fields, including transdermal, ocular and intracellular delivery. However, the transdermal route is still the dominant area of application for microneedles, especially for vaccine delivery.
3.1. Delivery to the skin
Drug delivery into the skin for local or systemic effects is extremely difficult due to the highly effective barrier properties of skin’s outer layer, the stratum corneum. The human stratum corneum is only 10 – 15 μm thick, but precludes absorption of most drugs at therapeutic levels [176]. The approximately 20 drugs with approval from the Food and Drug Administration (FDA) as transdermal patches all have molecular weights below 400 Da, are relatively lipophilic and require low doses [177]. Because the barrier layer of skin is just microns thick, microneedles have been developed to cross the stratum corneum without going deeply into the skin, thereby avoiding pain and bleeding. By by-passing the stratum corneum barrier, microneedles have been shown to dramatically increase the number of compounds that can be administered across the skin, including low molecular weight drugs, biotherapeutics, vaccines and other materials.
3.1.1. Low molecular weight drugs
3.1.1.1. Skin pretreatment with microneedles
Most studies on delivery of low molecular weight drugs have emphasized skin pretreatment with microneedles to increase skin permeability. This is because the doses of most drugs for systemic indications are too large to be coated on or encapsulated in microneedles. Larger doses can be delivered by pretreating the skin with microneedles and then administering the drug from a patch for an extended time by diffusion through the resulting skin pores. As another consideration, low molecular weight drugs have larger diffusion coefficients compared to macromolecular drugs and therefore diffuse into the skin more readily. Thus, most small molecule drugs have been administered by microneedle pretreatment of the skin and most microneedle pretreatment of the skin has been used for delivery of small molecule drugs.
Initial studies of this approach involved delivery of small marker compounds. For example, human cadaver skin permeability to calcein (molecular weight of 623 Da) was shown to increase by more than 1,000-fold when microneedles were inserted into the skin and left in place (i.e., thereby partially plugging the pores) and was shown to increase by more than 10,000-fold when microneedles were inserted and immediately removed [40]. Subsequent studies showed that pretreatment with short microneedles (70–80 μm) enhanced the penetration of galanthamine (287 Da) [56]. Formulation of docetaxel in elastic liposomes was also studied as a means to increase delivery into microneedle pretreated skin[55].
Pretreatment with microneedles followed by drug application was used for the delivery of naltrexone across guinea pig and human skin [178–181]. In these studies, microneedle patches were used in the first published study of drug delivery to human subjects and showed elevated and prolonged naltrexone plasma levels for three days after microneedle application. To improve the delivery of naltrexone across microneedle-treated skin, the nonspecific cyclooxygenase enzyme inhibitor diclofenac was applied to the skin, resulting in much longer and greater delivery, believed to be due to delayed recovery of the skin barrier [182]. For the same purpose, a highly water-soluble PEGylated naltrexone pro-drug [183] and a naltrexone formulation including a propylene glycol–water mixture was tested [184]. However, improvement of naltrexone delivery was not achieved because of the nonlinear relationship between pro-drug concentration and transdermal flux, along with the negative effect of increased viscosity by propylene glycol on drug diffusivity.
For topical photodynamic therapy, 5-aminolevulinic acid or 5-aminolevulinic acid methyl ester was delivered through skin pretreated with microneedles [185–186]. Drug-induced production of the photosensitizer protoporphyrin IX was greater after delivery combined with skin pretreatment using microneedles than without microneedle treatment in a human study as well as in rats. Similarly, the preformed photosensitizer meso-tetra(N-methyl-4-pyridyl)porphinetetratosylate was successfully delivered by microneedle pretreatment for topical photodynamic therapy [187]. In a separate human study, a microneedle roller was similarly used for skin pretreatment followed by delivery of aminolevulinic acid and exposure to pulsed light for cosmetic treatment of photodamaged facial skin [188].
Phenylephrine is a drug used to treat fecal incontinence by increasing resting anal sphincter pressure. This drug was delivered locally to the anal sphincter muscle after microneedle pretreatment of the skin. Topical application with microneedle pretreatment increased the mean resting anal sphincter pressure in rats, which was superior to the results in the control group without microneedle pretreatment [189].
While the above studies employed microneedles fabricated as research prototypes, the Dermaroller® and other similar FDA-registered devices are sold commercially for cosmetic purposes and have also been investigated a transdermal drug delivery tool by pretreating the skin with microneedle punctures generated by a cylindrical roller of metal microneedles [190]. Microneedle rollers have also been applied to enhance optical skin clearing by glycerol [85] and increased skin permeability to chondroitin sulfate [191].
Another commercially available microneedle device is sold by Nanomed Devices for skin pretreatment before application of cosmetic agents and acne medication. This solid silicon microneedle array has been used to increase delivery of dyclonine for topical anesthesia after skin pretreatment with microneedles and showed improved cutaneous topical anesthesia in human subjects [192].
3.1.1.2. Lidocaine delivery
While most low molecular weight drugs have been administered using microneedle pretreatment of skin, coated microneedles and hollow microneedles have each been used to administer lidocaine for local anesthesia. In one study, lidocaine was coated on non-dissolving polymer microneedles and administered to pigs [102]. The lidocaine levels in the skin were interpreted as sufficient to cause prolonged local anesthesia.
In a separate study, lidocaine was injected into the skin of human subjects using single, hollow microneedles and compared to conventional intradermal injection of lidocaine [193]. While the local anesthesia caused by lidocaine delivery by either method was the same, the subjects reported significantly less pain associated with delivery using microneedles and expressed strong preference for that method over intradermal injection with a hypodermic needle. As another proof-of-concept study, microinjection of nicotine derivatives with hollow microneedles has also been shown in human subjects [194–195].
3.1.2. Biotherapeutics
Biotherapeutic drugs, such as peptides, proteins, DNA and RNA, are large molecules that cannot easily be administered orally or transdermally and therefore are conventionally given almost exclusively by hypodermic injection. Delivery with a microneedle patch is envisioned as an alternative to hypodermic injection that is less painful, safer and simpler for patients to self administer. Because the doses of biotherapeutics are often low (i.e., microgram doses), many biotherapeutics can be administered either coated onto microneedles or encapsulated within dissolving microneedles. Because of the small size of microneedles, drugs given on or within the microneedles themselves are usually limited to microgram doses, although low milligram doses may be possible.
3.1.2.1. Insulin
Insulin has received by far the most attention among the various biotherapeutics studied for delivery using microneedles, including work with multiple microneedle design types and progressing through animal studies into human trials. In one of the first studies, solid microneedles were pressed into diabetic rat skin as a pretreatment before applying a topical insulin solution, which elicited a significant increase in insulin delivery and reduction in blood-glucose level [47]. Using a similar approach, rat skin was pretreated with a microneedle roller, such that subsequent insulin delivery was shown to lower blood-glucose level [86].
Dissolving microneedles encapsulating insulin have also been studied extensively in mice, diabetic rats and dogs. [115–116, 118, 120, 125]. This approach was shown to enable stable encapsulation of insulin and effective insulin delivery to reduce blood glucose levels.
Hollow microneedles have been used for insulin delivery. An early study demonstrated insulin diffusion through microneedles into diabetic rat skin [63], but other studies have emphasized active infusion of an insulin solution. The first studies of biotherapeutic delivery using microneedles employed silicon or glass microneedles for insulin delivery [38, 142], which demonstrated drops in blood-glucose levels after microneedle injection. Other hollow microneedle designs have also been developed for effective delivery of insulin, including silicon microneedles made using MEMS-based etching techniques [196–197] and polymer microneedles made by drawing lithography [157].
Hollow microneedles have progressed into human studies of insulin delivery to type 1 diabetes subjects. In addition to showing that subjects found microneedles to be less painful and overall preferred compared to conventional subcutaneous catheters, microneedle-based delivery to the skin increased insulin pharmacokinetics almost two-fold, which may enable better control over postprandial plasma glucose levels [167, 198]. Hollow metal microneedles have also been studied in larger cohorts of type I diabetes patients to show that intradermal insulin delivery not only induced faster insulin absorption but also enabled more rapid onset and offset of metabolic effect on blood glucose levels than subcutaneous injection [199–200]. Expedited pharmacokinetics have been explained by rapid lymphatic uptake and distribution of protein drugs from the skin [171].
3.1.2.2. Other biotherapeutics
A number of other biotherapeutics have been administered to animal models using microneedles. Dissolving microneedles have been used to deliver EPO [121, 126], low molecular weight heparin [117], leuprolide acetate [123], desmopressin [122], and human growth hormone [122, 124, 201]. Coated microneedles have administered desmopressin [97], salmon calcitonin[202], and PTH (1-34) [89, 203–204]. Skin pretreatment with microneedles has been combined with iontophoresis to administer oligonucleotides [105] and human growth hormone [205].
PTH administered with coated microneedles has progressed through Phase I and Phase II clinical trials for osteoporosis treatment [206–207]. Analysis of the pharmacokinetics and pharmacodynamics of PTH delivery showed that the microneedle patch achieved a shorter time to peak concentration and shorter half-life of PTH than injection methods. During the six months of treatment, the microneedle group showed higher (or comparable) lumbar spine bone mineral density change in the total hip and lumbar spine when compared with the injection group, indicating possibly improved drug efficacy in addition to more convenient PTH delivery for patients.
Finally, delivery of plasmid DNA and siRNA have been carried out using microneedles. Plasmid DNA was delivered after microneedle pretreatment and the gene was successfully expressed in a viable human skin ex vivo [208]. Using coated and dissolving microneedles, plasmid DNAs expressing green fluorescence protein (GFP) and luciferase were delivered into the mouse footpad [209]. siRNA delivered by dissolving microneedles silenced reporter gene expression in a transgenic reporter mouse model [210].
3.1.3. Vaccines
Vaccination using microneedles is especially appealing because it not only offers expected advantages that simplify vaccine distribution and improve patient compliance, but also enable vaccine targeting to the skin. It is already known that the skin offers immunologic advantages over conventional intramuscular injection, but until now there have not been simple, reliable methods to vaccinate in the skin [211–212]. Microneedles – both solid microneedle patches and hollow microneedles for intradermal injection – address this limitation and can make skin vaccination a practical clinical reality. Motivated by these opportunities, vaccine delivery has been the most widely investigated use of microneedles.
3.1.3.1. Skin pretreatment with microneedles
Skin pretreatment with microneedles has been employed to vaccinate with diphtheria toxoid adjuvanted with cholera toxin, which generated similar immune responses compared to subcutaneous injection [213–214]. However, a similar approach using microneedle pretreatment did not generate significant immune response to influenza vaccine unless adjuvanted with cholera toxin [214]. Moreover, formulation of the diphtheria toxoid antigen with two types of vesicles (cationic liposomes and anionic surfactant-based vesicles) did not enhance immunogenicity [215].
A model antigen, ovalbumin, and CpG adjuvant were applied to microneedle pretreated skin either in solution or incorporated into cationic liposomes; the antibody response was weaker for the formulation involving liposomes [216]. Using another particulate formulation, N-trimethyl chitosan nanoparticles with the diphtheria toxoid antigen was less effective than the antigen and adjuvant in solution applied to mouse skin pretreated with microneedles [217]. When N-trimethyl chitosan was conjugated with the ovalbumin antigen, it showed better immune response such as higher IgG levels and more antigen trafficking into the lymph nodes compared to a nanoparticle formulation [218]. Solid lipid nanoparticles conjugated with ovalbumin antigen were also transcutaneously delivered using microneedle roller treatment and showed enhanced delivery compared to the antigen alone [219].
Using a related approach, the skin has been scraped with blunt-tipped microneedles to increase delivery of a DNA vaccine against hepatitis B [220], recombinant anthrax vaccine [221], and live-attenuated Japanese encephalitis vaccine [222] in animal models as well as rabies vaccine in human subjects [223]. While this approach was effective, intradermal injection was shown in these studies to be much more effective, probably due to inefficient delivery into skin from the topical formulations.
3.1.3.2. Coated microneedles
To enable more controlled and efficient delivery, coated microneedles have been the most extensively studied technique for vaccination with microneedles. The first studies of microneedle vaccination employed metal microneedles coated with ovalbumin antigen in hairless guinea pigs, which showed a better immune response and significant dose sparing compared to an equivalent subcutaneous or intramuscular injection [48, 224].
3.1.3.2.1. Influenza vaccine
Influenza vaccination with coated microneedles has been extensively studied in recent years, showing complete protection against lethal viral infection after vaccination using H1N1 and H3N2 seasonal strains in mice [225–226]. Incorporation of trehalose into the coating formulation as a stabilizer was shown to prevent antigenicity loss of the influenza vaccine [91, 227]. Microneedles coated with the stabilized vaccine induced similar antibody IgG response, hemagglutination inhibition antibody titer, and neutralizing antibody activity as conventional intramuscular vaccination with the same vaccine at the same dose [228].
A number of studies suggest enhanced memory responses after microneedle vaccination compared to intramuscular injection. For example, microneedle-vaccinated mice had undetectable virus titers in their lungs after viral challenge, suggesting a strong memory response that blocked viral replication in the lung, whereas intramuscularly vaccinated mice had orders of magnitude higher levels of virus in the lung [227, 229]. Interestingly, the microneedle-vaccinated group was also found to have significantly higher levels of total IgG, IgG1, and IgG2 post-challenge than pre-challenge, again indicating a strong memory response [229]. In addition to improved humoral immunity, coated microneedles also induced cellular recall responses, such as MHC–II associated CD4+ T helper cells [227–228]. In addition, microneedle vaccination using the 2009 H1N1 virus vaccine induced protective immunity even six months after vaccination [230].
In addition to the above studies, all of which used whole inactivated influenza virus, other studies have been performed using virus-like particle (VLP) vaccine against the H1 strain of seasonal influenza coated on microneedles. Microneedles coated with VLP vaccine benefitted from formulation with trehalose [98, 231] and were shown to elicit stronger immune responses and enable dose sparing compared to intramuscular injection in mice [106, 232]. Similarly, an avian H5 influenza VLP vaccine was administered with coated microneedles and again showed stronger immunogenicity than the intramuscular route [233–234]. Additional studies showed that the H1 VLPs elicited a stronger Langerhans cell response in an ex vivo human skin model compared to the H5 VLP vaccine [235–236]. Coated microneedles have also been used to administer recombinant subunit vaccine consisting of trimeric influenza hemagglutinin protein, which resulted in improved immunity compared to subcutaneous injection in mice [107].
With the goal of targeting Langerhans cells in the superficial skin layer of viable epidermis, densely packed microneedles close to 100 μm in length have been coated with vaccine and inserted into mouse ear skin at high velocity. While an initial study showed similar immune responses against ovalbumin for this approach compared to intramuscular injection [95], a subsequent study, showed 100-fold dose sparing of influenza vaccine compared to intramuscular injection [237]. In order to improve the delivery of vaccine coated on microneedles, vaccine was site-selectively coated on the tips of microneedles, which resulted in delivery efficiency over 80% within 2 min and induction of strong immune response against influenza in mice. [238]
3.1.3.2.2. Other vaccines
Additional studies using similar coated-microneedle devices have administered bacillus Calmette-Guérin (BCG) vaccine in guinea pigs, which resulted in improved immunity compared to intradermal injection [110]. A DNA vaccine encoding hepatitis C virus protein was coated on microneedles and induced an effective cytotoxic T lymphocyte response in mice [111].
Using a novel approach, hepatitis B surface antigen was coated onto metal microneedles using poly[di(carboxylatophenoxy)phosphazene] as both a coating excipient and as an immuno-adjuvant [239]. Microneedle vaccination in pigs using the adjuvanted coating formulation induced superior antigen-specific IgG compared to intradermal injection by hypodermic needle without adjuvant.
Short, densely packed microneedles were estimated to deliver more than half of the antigen directly to antigen-presenting cells in the skin [237]. Using this type of microneedle patches, mice were vaccinated against human papilloma virus [108], West Nile virus [109], chikungunya virus [109], and herpes simples virus [112, 240].
3.1.3.3. Dissolving microneedles
Influenza vaccination was carried out using dissolving microneedles made of PVP encapsulating lyophilized inactivated influenza vaccine [128]. The microneedles were produced by in situ polymerization of liquid monomeric N-vinylpyrrolidone in a micromold. This solvent-free approach took advantage of the improved stability of lyophilized vaccine and showed improved protective immunity among microneedle-vaccinated mice compared to mice vaccinated by intramuscular injection. A different type of dissolving microneedle patch made of carboxylmethylcellulose and trehalose was used to deliver cell-culture-derived influenza vaccine [241].
Using a related approach, microneedles were formed by casting water-soluble polymer formulations into micromolds and drying to produce microneedles. Ovalbumin and trivalent influenza vaccine were administered using CMC-based dissolving microneedles and induced robust immune responses in mice [114]. A recombinant protective antigen was similarly administered using dissolving microneedles with a different formulation and was shown to generate comparable or better immune response than intramuscular or intradermal injection in rats [131].
Although too large to be called microneedles, dissolving needle structures encapsulating tetanus toxoid or hepatitis B surface antigen have been fabricated and inserted under the skin of mice [242–243]. These needles showed improved stability and immunogenicity compared to intramuscular or subcutaneous injection.
3.1.3.4. Hollow microneedles
Most hollow microneedle vaccination studies have been carried out with 1.5 mm-long, small-gauge hypodermic needles mounted on a syringe. While these needles are arguably too long to be called microneedles and their mounting on a syringe deviates significantly from the patch-like format of solid microneedle devices, the considerable work in this area is worth including. These short needles allow simplified needle insertion and injection normal to the skin surface with reliable intradermal targeting, which contrasts with the conventional Mantoux technique of intradermal injection that requires a precisely controlled, angled insertion and produces unreliable intradermal targeting [173, 244].
These microneedles were first tested for influenza vaccination in rats, which showed that intradermal injection enabled 100-fold dose sparing using inactivated virus vaccine, up to 10-fold dose sparing using a split-virion vaccine, and five-fold dose sparing using a plasmid DNA vaccine when compared to intramuscular delivery [245].
Intradermal vaccination with anthrax recombinant protective antigen generated slightly better or similar immune responses in both the mouse and rabbit [221]. A follow-on study of intradermal anthrax vaccination showed complete protection of immunized rabbits against lethal challenge with anthrax spores and 50-fold dose sparing compared to the intramuscular route [246].
Additional studies using this intradermal microneedle demonstrated effective vaccination with a live attenuated vaccine against Japanese encephalitis in non-human primates [222], plague F1-V vaccine in mice [247], and combination vaccines including anthrax, botulism, plague and staphylococcal toxic shock in rhesus macaques [248]. A study in human subjects showed dose sparing of rabies vaccination in the skin compared to intramuscular injection [223].
3.1.3.4.1. Influenza vaccination clinical trials
A prototype of the hollow microneedle system discussed above was used in a human trial that showed a reduced dose of 6 μg influenza vaccine given in the skin was not significantly different from intramuscular vaccination at a full dose of 15 μg influenza vaccine in non-elderly adults (18 – 60 years old), but showed lower antibody titers in older patients [249].
Further evaluation of the hollow microneedle system now in clinical use in many countries around the world for influenza vaccination was performed in clinical studies of healthy adults (18–57 years) [250–251] and elderly people (> 60 years) [252–253]. For healthy adults, 9 μg of each strain of trivalent influenza vaccine delivered by intradermal injection was as immunogenic as a full 15 μg dose by intramuscular vaccination, whereas lower intradermal doses were inferior in a phase II clinical trial [250–251]. For elderly subjects, full-dose vaccination by the intradermal route was more immunogenic than intramuscular injection of the same dose in phase II and phase III clinical trials [252–253].
Finally, a human trial of influenza vaccination in healthy adults was carried out using a needle array of four silicon microneedles measuring 450 μm in length [254]. Intradermal vaccination using 3 μg or 6 μg of influenza vaccine induced similar immune responses compared to intramuscular injection of 15 μg of vaccine.
3.1.4. Blood and interstitial fluid extraction
Microneedles have been used mainly for delivery into the skin, but several studies have investigated the role of microneedles as a diagnostic tool to extract analytes from the skin for ex vivo analysis or by integrating a sensor into the microneedle for in situ sensing in the skin. In one approach, up to a few microliters of interstitial fluid were extracted under suction from skin pretreated with microneedles; measured glucose concentrations in the extracted interstitial fluid showed excellent correlation with corresponding blood glucose levels in rats and human subjects [175, 255].
A microneedle for microdialysis has also been developed to selectively collect analytes below a molecular weight cut off to prevent biosensor fouling with high molecular weight compounds [256]. Integrated diagnostic systems including a microneedle, as well as supporting microactuators, microfluidic controls and sensors, have also been developed to collect blood from the skin for glucose monitoring [257–258].
Rather than extracting fluid containing biomarkers, microneedles have been surface-modified to specifically bind biomarkers of interest and, in that way, selectively extract those compounds for analysis [259]. Other approaches have involved building sensors into the microneedle itself. For example, microneedles have been developed as sensors for hydrogen peroxide, lactate, dissolved oxygen and glutamate [260–262]. Microneedles have also been used as bioelectrical interfaces, especially for neural recording and stimulation [263–271], as well as for electrocardiography (ECG) and electroencephalography (EEG) measurements [146, 272].
3.1.5. Combination of microneedles and other methods
Microneedle technology has been combined with iontophoresis, electroporation and other methods to provide synergistic effects. In one of the first papers on drug delivery using microneedles, skin was pretreated with microneedles and then oligonucleotides were driven through the permeabilized skin by iontophoresis in hairless guinea pigs [105]. This approach reduces the skin barrier using microneedles and then provides a driving force for enhanced transport by iontophoresis. In follow-on studies, this approach was effective for delivery of dextrans up to 200 kDa in molecular weight in vitro [273] and for delivery of the 13 kDa protein daniplestim in vitro and in vivo [274–275]. Nanovesicles containing insulin were delivered by iontophoresis across microneedle pretreated skin, which lowered blood-glucose levels in diabetic rats [276]. The combination of microneedle pretreatment with iontophoresis has been proposed for local anesthetic delivery across the oral mucosa for dental applications [277].
Microneedles have also been developed as micro-electrodes for skin electroporation. In one study, insertion of microneedles combined with application of short electrical pulses designed to cause skin electroporation increased delivery of dextran into the skin [278]. In other studies, arrays of independently addressable, solid microneedle electrodes were fabricated by a novel metal-transfer micromolding technique and shown to electroporate cells to increase uptake of calcein and bovine serum albumin and to increase DNA transfection [66, 279]. A hollow microneedle electrode was also developed as a proof-of-concept for simultaneous intradermal injection and electroporation [153] and for temperature monitoring during electroporation [148]. Using the drawing technique, a dissolving maltose microneedle tip was combined with a metal microelectrode for transdermal delivery of the p2CMVmIL-12 gene. This hybrid electro-microneedle resulted in the successful treatment of B16F10 subcutaneous tumors in a mouse model [280].
Microneedle electrode arrays have also been used for DNA vaccination, where a microneedle coated with the smallpox DNA vaccine was employed; a high antibody response and complete protection against lethal challenge were the results [281–283].
3.1.6. Approved microneedle products
There are a number of approved medical and cosmetic products using microneedles that are sold around the world. The first product was the Dermaroller®, which is a cylindrical roller covered on its surface with solid, metal microneedles that measure 0.2 – 2.5 mm in length. The shorter needles are designed especially for home use by patients to improve skin texture and the longer ones are used in clinics to treat scars and hyperpigmentation. First sold in Europe in 1999, the Dermaroller is now sold around the world (http://dermaroller.com/). A number of other companies sell similar products as microneedle rollers (http://www.hansderma.net, http://www.whitelotus.com.au/) as well as a flat microneedle patch (http://www.henryschein.com/microchannel).
More recently, MicroHyala® was developed as a patch covered with dissolving microneedles containing hyaluronic acid that is released in the skin to treat wrinkles (http://www.cosmed-pharm.co.jp/). This product was introduced in 2008 and is currently sold in Japan. LiteClear® was also recently introduced in China for acne treatment and worldwide for cosmetic blemish treatment (http://www.nanomed-skincare.com/). This family of products uses solid silicon microneedles as a skin pretreatment followed by application of the active agents topically.
Soluvia® is a single hollow microneedle that is 1.5 mm long and is attached to a syringe (http://www.bd.com/pharmaceuticals/products/microinjection.asp). It is marketed worldwide prefilled with influenza vaccine for intradermal vaccination as IDflu®, Intanza® and Fluzone Intradermal® (http://en.sanofi.com/press/press_releases/2009/ppc_24214.asp).
Finally, MicronJet® recently received FDA clearance (http://www.nanopass.com/content-c.asp?cid=22). This device contains a row of four hollow, silicon microneedles mounted on a plastic adapter compatible with standard syringes,
3.2. Delivery to the eye
In addition to applications in the skin, microneedles have also been used for drug delivery to the eye. In the first study of ocular drug delivery, coated microneedles were used to administer model compounds into the sclera and corneal stroma [101]. Administration of pilocarpine to the corneal stroma in this way achieved a bioavailablity almost two orders of magnitude greater than topical delivery and induced significant and extended constriction of the pupil in the rabbit eye.
A subsequent study showed that hollow microneedles can be used to make minimally invasive injections of soluble molecules, as well as nano- and microparticles, into the sclera [284]. Intrascleral injection was influenced by scleral thickness, infusion pressure, microneedle retraction depth, and concomitant use of enzymes. By inserting hollow microneedles to the base of the sclera, fluid injection could be targeted to the suprachoroidal space, which is a potential space between the sclera and choroid of the eye [285]. Fluid injected in this way was able to flow circumferentially around the eye and even reach the macula after injection near the limbus. Soluble molecules, as well as nano- and microparticles, were injected, which was influenced by microneedle length, intraocular pressure, infusion pressure, and particle size.
An implantable microneedle made of biodegradable polymer and methotrexate was developed for treatment of primary vitreo-retinal lymphoma [286]. In a preliminary toxicity test, in vivo implantation into the rabbit eye resulted in no inflammatory response.
3.3. Delivery into cells
Single, hollow microneedles have been used for intracellular injection for decades, facilitating applications in the bioscience laboratory, animal cloning and clinical medicine (e.g., in vitro fertilization) [287–289]. This extremely low-throughput approach uses pulled glass micropipettes that are carefully inserted into individual cells under a microscope for intracytoplasmic or intranuclear injection of proteins, DNA, spermatozoa or other materials.
As an alternative approach, modified atomic force microscopy (AFM) tips have been developed into nanoneedles of 200–300 nm in diameter and 6–8 μm in length for intracellular penetration and delivery [290–292]. By immobilizing DNA molecules on the surface of the nanoneedle, DNA was delivered and expressed in human stem cells and cancer cells [293–295]. This type of nanoneedle was also adapted for use as a sensor of mRNA or insulin-like growth factor-II in cells [296–297].
Nanoneedles have also been made from single multiwalled carbon nanotubes (MWCNT) mounted on an AFM tips, glass micropipettes and macroscopic needles. In this way, quantum dots adhered to the nanotube surface were delivered into human cells [298–299]. Fluid and nanoparticles were also delivered through the bore of MWCNT [300].
Microneedle arrays have been adapted to facilitate higher-throughput delivery into cells, in contrast to the single-cell approaches described above. In an early study, nematodes were allowed to locomote across an array of DNA-coated microneedles, which pierced through the nematode cuticle to transfect nematode cells [301]. About 8% of the total progeny tested expressed the foreign gene. Similarly, microneedle arrays have been pressed into a monolayer of prostate cancer cells bathed in a solution of calcein, a small fluorescent marker compound [38]. This led to intracellular uptake of the calcein at high cell viability. Hollow microneedle arrays have also been developed for intracellular injection [302]. In a different way, nanoneedle-shaped particles were developed for intracellular delivery on encapsulated molecules [303].
3.4. Other applications
For medical applications, solid microneedles have been developed for drug delivery into blood vessel walls, for example to treat restenosis [304]. Such microneedles were shown to puncture across the internal elastic lamina in rabbit arteries ex vivo. To aid tissue engineering, hollow microneedles were developed to improve cell viability in tissue culture by better perfusing slices of harvested brain tissue [305].
For biofuels applications, gold-plated microneedle electrodes were functionalized to electrochemically detect p-cresol for high-throughput analysis of biochemical species in plants for biofuels research [306].
4. Use of microneedles
4.1. Biomechanics of delivery using microneedles
4.1.1. Microneedle insertion into skin
Most applications require insertion of microneedles into the skin or other tissue of interest. Because skin is composed of nonlinear viscoelastic layers, it is easily deformed when microneedles are applied to its surface [307–311]. This means that microneedle design and insertion method can influence whether microneedles fully penetrate, partially penetrate or do not penetrate at all into the skin.
Microneedles have been inserted into the skin by hand or using mechanical insertion devices. One study showed that longer microneedle and lower microneedle density made insertion into the skin easier by overcoming this deformation [53]. Another approach uses a cylindrical roller with protruding microneedles, which inserts just one row of microneedles at a time as the device rolls across the skin surface [85–87, 190, 219, 312–314]. Using a different approach, blunt-tipped microneedles have been scraped across the skin surface to form micro-trenches [220].
To facilitate microneedle insertion into skin, a vibratory actuator helped microneedles penetrate the skin with less insertion force [153, 315–316] and an electrically driven applicator that inserted microneedles at high velocity helped assure microneedle penetration to increase skin permeability [317]. In a related study, a spring-loaded applicator inserted densely packed, extremely short (< 70 μm) microneedles into the skin and determined the effect of insertion speed on perforating area, penetration depth, and amount of vaccine delivered from coated microneedles [318]. Microneedle insertion by drilling enabled precise control over the depth of microneedles insertion, allowing localization of injection through hollow microneedles to within the viable epidermis or specific depths within the dermis [152].
To supplement histological imaging that requires invasive skin sampling and processing, non-invasive imaging methods have been used for real-time visualization of microneedle penetration. Optical coherence tomography (OCT) has been used by a number of groups to image microneedle insertion depth, skin resealing and the influence of microneedle geometry and application force on insertion depth [319–320]. Real-time dissolution of a microneedle in the skin was also imaged by OCT [321]. Injection into skin with a hollow microneedle was imaged by X-ray and 3D ultrasound echography to show intradermal localization of the injection and to visualize the distribution of injected fluid within the skin [173].
Microneedles must be strong enough to insert into skin without bending or breaking. While solid metal microneedles tend to be very strong, hollow microneedles are susceptible to fracture if not designed properly [322], whereas polymer microneedles have mostly been shown to fail by plastic deformation [44, 201, 323]. Experimental measurements coupled with biomechanical modeling have shown that the force required to insert a microneedle into the skin decreases in proportion to microneedle tip sharpness and is affected by skin tension and curvature, and that both microneedle material and geometry affect microneedle mechanical strength [44, 201, 322–327].
4.1.2. Infusion through hollow microneedles
Hollow microneedles require control not only over the microneedle insertion process, but also over fluid infusion into the skin. Experimental and finite-element modeling of fluid flow through microneedles showed that while geometry of the microneedle tip largely controlled pressure drop for fluid infusion through the microneedle, these pressures were much less than those required for injection into skin, meaning that the primary resistance to flow was associated with infusion into the skin and not through the microneedle itself [328].
In human cadaver skin, fluid flow rate into skin was increased by greater insertion depth, larger infusion pressure, use of a beveled microneedle tip, and the presence of hyaluronidase as a tissue spreading factor [163]. Partial retraction of the microneedle also increased infusion rate by allowing skin compressed during microneedle insertion to return to its original state, which resulted in an enhanced flow rate [163, 307]. A similar study in human subjects that assessed infusion pressure and pain associated with infusion at a set of flow rates showed that microneedle insertion depth had little effect, partial microneedle retraction lowered infusion pressure but increased pain, slower infusion rate reduced infusion pressure and kept pain low, and use of hyaluronidase also lowered infusion pressure and kept pain low [329].
In the eye, infusion pressures during injection using microneedles have been reported over a similar range as in the skin, i.e., up to one or a few atmospheres [284–285]. Intrascleral injection benefitted strongly from partial microneedle retraction, but infusion pressure had little effect on the volume injected, which was generally up to a few tens of microliters [284]. Suprachoroidal injection required precise placement of the microneedle at the base of the sclera (i.e., just above the choroid) for infusion of up to a few tens of microliters, which depended on microneedle insertion depth and infusion pressure [285].
4.1.3. Skin recovery process
Micron-scale holes remain in the skin after removing microneedles. When microneedles are used as a pretreatment for subsequent drug delivery through these holes, a long pore lifetime is ideal. However, in other scenarios, quick resealing of the pores is beneficial for safety reasons to avoid possible infection. The kinetics of pore resealing after microneedle insertion were studied by electrical impedance measurement in human subjects, which showed that pores formed by microneedles recovered their barrier properties within 2 h when the skin was not occluded, but took 3 to 40 h to recover when the skin was occluded, depending on the geometry of the microneedles [180, 330]. The kinetics of pore resealing were also assayed in hairless rats using TEWL and tissue staining, and showed similar timeframes for pore resealing [314].
Application of a non-specific COX inhibitor to the skin after microneedle pretreatment was shown to maintain skin permeability for up to 7 days by inhibiting the skin recovery process [182]. This was achieved by applying an FDA-approved topical formulation of diclofenac sodium (Solaraze® gel) to hairless guinea pigs.
4.2. Biopharmaceutical stability in microneedles
Molecules, and especially biopharmaceuticals, need to be protected during incorporation into microneedles and during subsequent storage, possibly at elevated temperature. While many of the studies mentioned throughout this review implicitly demonstrate retained bioactivity based on pharmacokinetic measurements and pharmacodynamic responses, some studies specifically examined biomolecule stability and developed methods to enhance it.
4.2.1. Stability of biotherapeutics
In an early study, bovine serum albumin was encapsulated in biodegradable PLGA polymer microneedles. During microneedle fabrication, heat exposure for less than 10 min did not significantly damage protein stability, but heat exposure longer than 20 min induced protein aggregation [132]. Lysozyme and human growth hormone were stably encapsulated and stored at room temperature for two months and 15 months, respectively, in carboxymethylcellulose microneedles fabricated by casting and drying at low temperature [113, 201]. Insulin, low molecular-weight heparin, human growth hormone, and desmopressin were also embedded in dissolving microneedles and retained their activity for at least one month, even at −80°C or +40°C [117, 122, 125]. Horseradish peroxidase was stably coated onto microneedles and maintained much of its enzymatic activity even after one month storage at 70°C [104].
In a detailed set of studies, destabilization of PTH (1-34)-coated microneedles was shown to be due primarily to aggregation and oxidation [203]. Interestingly, the plastic retainer ring in the microneedle packaging was the main component that had a negative effect on PTH stability. After optimizing storage conditions, PTH coated on microneedles retained its bioactivity up to 18 months at room temperature and 60% humidity. Terminal sterilization of PTH-coated microneedles by γ-irradiation or e-beam irradiation caused PTH oxidation, which was reduced but not eliminated by lowering irradiation dose and temperature, as well as minimizing moisture and oxygen levels in the packaging [204]. However, these measures were not able to maintain product stability for a two-year shelf life at room temperature, so aseptic manufacturing was used instead.
4.2.2. Stability of vaccines
Vaccine stability has also received considerable attention, in part because long-term vaccine storage without refrigeration would significantly benefit developing country vaccination efforts. Vaccine stability can be damaged during coating onto solid microneedles or encapsulation within dissolving microneedles, largely due to the drying process. A number of different vaccine formulations have been studied for coating influenza vaccines onto metal microneedles, which showed that including trehalose was critical to preserving vaccine antigenicity [91, 98]. Inclusion of trehalose, as well as surfactant, was also important to stabilizing BCG vaccine on coated microneedles [110]. Inactivated influenza vaccine was shown to maintain immunogenicity in the presence of UV-mediated polymerization of monomeric N-vinylpyrrolidone to encapsulate the vaccine in PVP microneedles [128].
Microneedles coated with an inactivated influenza vaccine and stored at room temperature for one month had approximately 20% loss of antigenicity in vitro, but mice immunized using these microneedles in vivo produced similar IgG responses to mice immunized using freshly coated microneedles [331]. An influenza subunit vaccine coated onto microneedles using a different formulation produced antibody responses in mice after six months storage that were similar to the response from freshly coated microneedles [332]. In another study, BCG vaccine lost approximately 30% viability after storage on coated microneedles at room temperature for 7 weeks [110]. A mechanistic study of influenza vaccine stability in microneedle coatings showed that phase transformation and especially crystallization of trehalose in the coating was strongly associated with loss of vaccine antigenicity [333].
4.3. Patient compliance and safety
In focus group studies of the opinions of the public as well as healthcare professionals, microneedle patches were generally viewed positively compared to hypodermic needle injections [334]. Perceived benefits included reduced pain, tissue damage and risk of infections, as well as possible self administration. Concerns focused on delayed onset, cost, accurate and reliable dosing and the potential for misuse. In separate vaccination surveys associated with hollow microneedle injection of influenza vaccine, most physicians and the general public preferred microneedles over conventional intramuscular injection largely due to the smaller needle size, as well as the increased immunogenicity of intradermal vaccination [335]. Physicians and patients alike thought that microneedle-based vaccination could increase vaccination coverage rates.
4.3.1. Pain
Patients may find microneedles appealing because of their minimally invasive delivery mechanism. Blinded pain studies in human subjects showed that pressing an array of 400 microneedles measuring 150 μm in length into the skin was much less painful than inserting a 26 gauge hypodermic needle [336]. A more detailed study showed that microneedle length strongly affected pain scores, number of microneedles also affected pain scores, and microneedle thickness and tip angle had weak effects on pain score over the range of conditions studied [337]. All microneedles studied induced significantly less pain than the hypodermic needle control. Other studies similarly showed that microneedles shorter than 400 μm did not cause reported pain [338–339].
Possible pain from hollow microneedles can be caused by microneedle insertion as well as liquid infusion during injection. A detailed study in human subjects showed that insertion of a single microneedle even as deep as 1 mm into the skin was generally not perceived as painful [329]. Infusion of up to a few hundred microliters of saline caused minimal sensation that was reported by most subjects as painless. Infusion up to 1 ml sometimes caused mild pain, especially at high flow rate and after partial microneedle retraction. In two separate studies, injection of lidocaine and injection of insulin with a microneedle was generally reported as painless and was overwhelmingly preferred by subjects over a hypodermic needle or subcutaneous catheter control, respectively [167, 193, 198]. In a human trial of influenza vaccination using a hollow microneedle array, pain associated with microneedles was not significantly different from that by IM injection in healthy adults [254].
4.3.2. Skin irritation
Microneedles can cause mild, transient skin irritation, primarily in the form of highly localized, mild and often punctuate erythema. The length of solid microneedles was found to be important, where 400 μm-long microneedles induced greater erythema and blood flow than 200 μm-long microneedles [338]. Other studies using solid microneedles have similarly found mild erythema that disappears within hours or, in some cases, days [340].
Hollow microneedles can also cause mild erythema [167, 193, 198, 250–251, 253, 329]. Edema can also be seen, although this swelling is not believed to be an inflammatory reaction, but rather direct visual evidence of the bleb of fluid injected into the skin characteristic of conventional intradermal injections as well. Unlike after hypodermic needle injection, blood is not characteristically seen on the skin surface after hollow microneedle injection. Influenza vaccination using hollow microneedles has shown more local inflammatory reactions than hypodermic injection in human subjects [249–250, 252–254]. This may be due to inflammatory reactions being more easily visible in the skin than those that may occur after intramuscular injection deeper in the body.
4.3.3. Skin infection
It is important to consider whether residual holes left by microneedles in the skin may be sites for infection. Clinical experience with hypodermic needles suggests that residual holes left by sterile needles is not a significant source of infection [341], in large part because the skin has a host of pathogen defense mechanisms to protect it from infection [342]. Experience to date with microneedles is consistent with the expectation that infection of skin after microneedle treatment is unlikely; there have been no reports of skin infection in the many human and animal studies cited throughout this review, which amounts to many thousands of microneedle insertions in hundreds of people and thousands of animals.
A study that specifically examined the issue of microbial penetration through residual holes left by microneedles in pig skin in vitro found that microneedle puncture resulted in significantly less microbial penetration than did hypodermic needle puncture and that no microorganisms crossed the viable epidermis in microneedle-punctured skin [343]. In another study, pretreatment of mouse skin with a microneedle roller making 150 holes resulted in similar levels of E. coli penetration as a single hole made by a hypodermic needle [219].
5. Perspectives and conclusions
5.1. Historical perspective
Active research in the field of microneedles for drug delivery began in the mid-1990’s, largely through three isolated efforts operated in parallel at Becton Dickinson (BD), Alza Corporation and the Georgia Institute of Technology.
In the early 1990’s, BD was interested to improve upon the well-established hypodermic needle for parenteral injection that formed a large part of their business and envisioned that microfabrication technology could enable smaller needles with enhanced clinical or pharmacological outcomes. They sponsored research at the University of California at Berkeley and the University of Utah to explore alternative manufacturing processes and designs enabled by microfabrication [344–346]. As the program matured, BD continued internal development of scalable manufacturing processes, preclinical testing, and clinical device evaluation. Primary focus was on short hollow steel needles [347] and blunt-tipped, solid microneedles that scrape the skin to increase skin permeability to topical vaccines [220]. The former project has matured into a commercial product platform (Soluvia®) [223] that is widely used for intradermal injection of influenza vaccine (IDflu®, Intanza®, Fluzone Intradermal®) [348].
In the early 1990’s, Alza Corporation had a historical interest in microneedles dating back to the early days of the company in the 1970’s [35], as well as an active engagement in developing iontophoresis for transdermal drug delivery [349]. Seeing the opportunity to combine these technologies, the company initially teamed with ISIS Pharmaceuticals to study iontophoresis of oligonucleotides across the skin after pretreatment by puncturing the skin with solid metal microneedles [105]. Additional work included coated metal microneedles; this technology was spun out of Alza and into a new company originally called The Macroflux Company and now called Zosano Pharma. This technology has been carried through a Phase II clinical trial for administration of PTH (1-34) to treat osteoporosis [206].
The third group to pioneer microneedles for drug delivery in the 1990’s was Georgia Tech, through collaboration between Mark Prausnitz, with expertise in transdermal drug delivery, and Mark Allen, with expertise in microfabrication. This group produced the first journal article on drug delivery using microneedles [40] and has continued to perform microneedles research since then.
In the late 1990’s and early 2000’s, a number of other companies began microneedles research programs. In academia, the microfabrication community also became interested in microneedles and developed a variety of different microneedle designs and fabrication methods. However, most of these microneedles were never used for drug delivery, but rather served as vehicles for advancing microfabrication research. The academic drug delivery community did not become very involved in microneedles research during this early stage, other than at Georgia Tech.
As the 2000’s progressed, industrial activity continued to grow, academic microfabrication activity slowed, and academic drug delivery research grew dramatically. It appears that academic research on drug delivery was delayed because most drug delivery researchers did not have the ability to make microneedles and most microfabrication researchers did not have the ability (or interest) to carry out drug delivery studies. Eventually, the interdisciplinary divide was crossed and the field blossomed as pharmaceutical labs gained access to microneedles.
Today, the field is at an important transitional point. It has matured far enough that many viable microneedle systems exist in dozens of industry and academic labs, and numerous applications of microneedles have been demonstrated in vitro and in animals, with a few progressing into human trials. The field is now fertile for more extensive translation into the clinic and introduction of microneedle products into medical practice.
5.2. Selection of microneedle designs for applications
Many microneedle designs and delivery strategies have been developed. For a given application, it is critical to identify the best microneedle design from among the many options. In general, drug delivery strategies can be divided into three major categories, each with different strengths and weaknesses: (i) skin pretreatment with microneedles followed by drug application as a topical formulation or patch for slow delivery over time, (ii) drug coating on or encapsulation in microneedles for bolus delivery into the skin and (iii) injection of a liquid drug formulation through one or more hollow microneedles for bolus injection or controlled infusion over time (Table I).
Table I.
Characteristics of different microneedle-based drug delivery system designs.
| Microneedle design | Simplicity of design and manufacturing | Simplicity of use by patient | Maximum possible drug dose | Control over drug delivery profile |
|---|---|---|---|---|
| Microneedle pretreatment | + + + | + + | + + | + + |
| Microneedle patch | + + | + + + | + | + + |
| Hollow microneedles | + | + | + + + | + + + |
5.2.1. Skin pretreatment with microneedles
Skin pretreatment with microneedles followed by drug application as a topical formulation or patch is arguably the simplest design for microneedle-based drug delivery. In this way, microneedles only need to be designed for biomechanical function, can be terminally sterilized without damaging bioactives, and need not remain in the skin for more than a fraction of a second. Moreover, such drug-free microneedles might be obtained from existing manufacturers who currently sell microneedles for cosmetic and other purposes. Drug delivery can then be carried out possibly using a conventional topical ointment, cream or gel or a transdermal patch. A downside, however, to this approach is that it is a two-step process, wherein the patient must first apply and discard microneedles and then apply the drug formulation to the treated skin site. A more successful approach might involve designing a device that integrates this two-step process into a single step procedure for the patient.
Another feature of the skin pretreatment approach is that it involves sustained-release drug delivery by diffusion through long-lived pores in the skin. For drugs that would benefit from a sustained-release delivery profile, this is an advantage. For scenarios where bolus delivery is desirable, this is a disadvantage. This approach also facilitates combination of microneedle-based delivery with other methods, such as iontophoresis. Because the skin pretreatment method relies on long-lived pores in the skin, the duration of drug delivery is limited by the lifetime of these pores. Finally, because drug delivery occurs over a long time (i.e., hours to days), milligram doses per day should be possible for many drugs, depending on treated skin area, drug solubility in the delivery vehicle, drug diffusivity in pores, and other factors.
5.2.2. Coated and dissolving microneedle patch
The use of a microneedle patch, either coated with or encapsulating drugs, is arguably the simplest method of microneedle-based drug delivery for patients. In this scenario, the patient applies the patch to the skin, possibly using an applicator, and then leaves the patch in place probably for a few minutes before discarding it. While coated microneedles may be considered biohazardous sharps waste, dissolving microneedles should be discarded as non-sharps waste.
This patient convenience, however, requires more sophisticated microneedle design and manufacturing. Microneedles must be designed for biomechanical function with the added constraints of including bioactives; have to be formulated using safe excipients that quickly dissolve in the fluids of the skin and protect drug stability during fabrication and storage; and may need to be manufactured under aseptic conditions. Biomechanical constraints are still greater for dissolving microneedles, which are generally weaker than metal or non-dissolving polymer microneedles suitable for coating.
A microneedle patch enables rapid bolus delivery. If sustained-release delivery is preferred, the microneedle formulation can be adjusted to have slow drug release from a skin depot formed by the dissolution products of the microneedle or its coating. Perhaps the greatest limitation of the microneedle patch is the small dose that can be coated on or encapsulated in microneedles. Although it depends strongly on drug properties – especially water solubility, since dissolving microneedles and microneedle coatings are typically prepared in aqueous solution – a general rule of thumb is that on the order of 0.1 – 1 μg of drug can be administered per microneedle, which corresponds to 10 – 1000 μg for a patch containing 100 – 1000 microneedles. Some of the very small microneedles may not support so much drug per microneedle, but can generally be packed at higher density such that this same dose range applies for a patch of up to a few square centimeters in size.
5.2.3. Hollow microneedles
Injection of drugs through hollow microneedles is arguably the most powerful method of microneedle-based drug delivery that enables the greatest control over the amount and timing of drug delivery. Hollow microneedles can be briefly inserted into the skin for bolus injection or can be left in place for sustained infusion. When coupled with a microprocessor-controlled pump, a wide variety of delivery profiles can be achieved, possibly in response to real-time patient or biosensor input.
Microneedle design is simplified by separation of the microneedle from the bioactive during manufacturing and drug formulation is simplified by use of liquid formulations that may need little or no changes from drug formulations already in clinical use. However, hollow microneedles have to be designed not only for mechanical strength during insertion, but also to enable leak-free infusion into skin and coupling to a drug reservoir. Single hollow microneedles have been shown to be sufficient for a number of applications, but multiple microneedles may be desirable in other scenarios. In addition to the design and manufacture of the microneedle, hollow microneedle systems typically require design and manufacture of a drug reservoir, pump, microfluidic netoworks and possible electronic controller, making the whole system much more complex than a microneedle patch.
5.3. Conclusions
The field of microneedles has dramatically grown over the past 15 years. Microfabrication technology has enabled a variety of different microneedle designs for drug delivery to the skin and other targets. Microneedles have been fabricated out of many different materials including silicon, metals, polymers, and ceramics using a variety of different fabrication methods including lithography, wet and dry etching, laser cutting and micromolding.
Solid microneedles, either on planar substrates or assembled as rollers, can be used to pretreat the skin and thereby increase skin permeability by orders of magnitude. A drug formulation or patch can then be applied to treated skin for sustained drug delivery. Alternatively, drugs can be encapsulated within a water-soluble matrix that is either applied as a coating onto metal or polymer microneedles or used as the matrix material of the microneedles themselves. Upon insertion into skin, the matrix dissolves and releases the encapsulated drug. Finally, hollow microneedles can be used to infuse liquid formulations of drug into the skin.
Microneedles have been studied for a diversity of medical applications, where delivery of bioactives to the skin has been the primary focus. Animal and human studies have demonstrated microneedle-based delivery of low molecular weight drugs including naltrexone, lidocaine, phenylephrine and compounds for photodynamic therapy; biotherapeutics including parathyroid hormone and insulin among other protein and peptide drugs; and vaccines including influenza, rabies, BCG, West Nile virus, HPV and other vaccines. Ocular delivery has been targeted to the cornea, sclera and suprachoroidal space using solid and hollow microneedles. Microneedles have been used for intracellular delivery of DNA and other compounds as well. Finally, microneedles have been used to collect bodily fluids and make bioelectric measurements as diagnostic sensors.
Functional use of microneedles has also received extensive attention. Optimization of microneedle sharpness, length, insertion force and velocity, and other parameters has enabled reliable microneedle insertion into skin. Fluid infusion through hollow microneedles depends on geometry of the microneedle (especially at the tip), infusion pressure, and possible partial retraction of the microneedle. Skin undergoes substantial recovery of barrier properties after microneedle treatment within hours if skin is not occluded, within about one day if skin is occluded and within up to one week if agents inhibiting skin repair are added. Stability of biomolecules encapsulated in microneedles and microneedle coatings has been facilitated by storage in a dry state in a formulation often containing trehalose among other excipients.
Patients and healthcare workers have seen value and expressed preference for microneedle-based delivery compared to hypodermic injections in surveys. Human subjects report little or no pain associated with most microneedle designs. After microneedle treatment, the skin often shows mild, transient erythema, but there is currently no evidence for increased risk of infection at the treatment site.
Microneedle research and development has progress tremendously over the past 15 years. Microfabrication tools have been adapted to the needs of microneedles as drug delivery devices. A variety of drug and vaccine applications have been shown in animals and humans. Patients, healthcare providers and companies have demonstrated interest in the technology. Microneedles are poised to make expanded impact on clinical medicine over the coming years.
Acknowledgments
We thank Dr. Jun Ki Jung in KRIBB and Dr. Jin Ho Choy in Ehwa Womens’ University for helpful discussions and support. We also thank Min-Ji Kim for drawing the images in Fig. 2. This work was carried out with support from the US National Institutes of Health and the Basic Science Research Program of the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2011-0022214). Mark Prausnitz serves as a consultant to companies, is a founding share-holder of companies and is an inventor on patents licensed to companies developing microneedle-based products.
Footnotes
This possible conflict of interest has been disclosed and is being managed by Georgia Tech and Emory University.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Giudice EL, Campbell JD. Needle-free vaccine delivery. Adv Drug Del Rev. 2006;58:68–89. doi: 10.1016/j.addr.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 2.Nir Y, Paz A, Sabo E, Potasman I. Fear of injections in young adults: Prevalence and associations. Am J Trop Med Hyg. 2003;68:341–344. [PubMed] [Google Scholar]
- 3.Hamilton JG. Needle phobia - a neglected diagnosis. J Fam Pract. 1995;41:169–175. [PubMed] [Google Scholar]
- 4.Drucker E, Alcabes PG, Marx PA. The injection century: massive unsterile injections and the emergence of human pathogens. Lancet. 2001;358:1989–1992. doi: 10.1016/S0140-6736(01)06967-7. [DOI] [PubMed] [Google Scholar]
- 5.Kermode M. Unsafe injections in low-income country health settings: need for injection safety promotion to prevent the spread of blood-borne viruses. Health Promot Int. 2004;19:95–103. doi: 10.1093/heapro/dah110. [DOI] [PubMed] [Google Scholar]
- 6.Singh R, Singh S, Lillard JW. Past, present, and future technologies for oral delivery of therapeutic proteins. J Pharm Sci. 2008;97:2497–2523. doi: 10.1002/jps.21183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amorij JP, Hinrichs WLJ, Frijlink HW, Wilschut JC, Huckriede A. Needle-free influenza vaccination. Lancet Infect Dis. 2010;10:699–711. doi: 10.1016/S1473-3099(10)70157-2. [DOI] [PubMed] [Google Scholar]
- 8.Mitragotri S. Immunization without needles. Nat Rev Immunol. 2005;5:905–916. doi: 10.1038/nri1728. [DOI] [PubMed] [Google Scholar]
- 9.Bronaugh RL, Maibach HI. Percutaneous absorption: Drugs-cosmetics-mechanisms-methodology. Marcel Dekker; New York: 2005. [Google Scholar]
- 10.Prausnitz MR, Mikszta JA, Cormier M, Andrianov AK. Microneedle-based vaccines. CurrTopMicrobiol Immunol. 2009:369–393. doi: 10.1007/978-3-540-92165-3_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel SR, Edelhauser HF, Prausnitz MR. Targeted drug delivery to the eye enabled by microneedles. In: Kompella UB, Edelhauser HF, editors. Drug product development for the back of the eye. American Association of Pharmaceutical Sciences; Arlington: 2011. pp. 331–360. [Google Scholar]
- 12.Yum K, Yu MF, Wang N, Xiang YK. Biofunctionalized nanoneedles for the direct and site-selective delivery of probes into living cells. Biochim Biophys Acta. 2011;1810:330–338. doi: 10.1016/j.bbagen.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yum K, Wang N, Yu MF. Nanoneedle: A multifunctional tool for biological studies in living cells. Nanoscale. 2010;2:363–372. doi: 10.1039/b9nr00231f. [DOI] [PubMed] [Google Scholar]
- 14.Arora A, Prausnitz MR, Mitragotri S. Micro-scale devices for transdermal drug delivery. Int J Pharm. 2008;364:227–236. doi: 10.1016/j.ijpharm.2008.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banga AK. Microporation applications for enhancing drug delivery. Expert Opin Drug Deliv. 2009;6:343–354. doi: 10.1517/17425240902841935. [DOI] [PubMed] [Google Scholar]
- 16.Birchall JC. Microneedle array technology: the time is right but is the science ready? Expert Rev Med Devic. 2006;3:1–4. doi: 10.1586/17434440.3.1.1. [DOI] [PubMed] [Google Scholar]
- 17.Coulman S, Allender C, Birchall J. Microneedles and other physical methods for overcoming the stratum corneum barrier for cutaneous gene therapy. Crit Rev Ther Drug Carrier Syst. 2006;23:205–258. doi: 10.1615/critrevtherdrugcarriersyst.v23.i3.20. [DOI] [PubMed] [Google Scholar]
- 18.Donnelly RF, Singh TRR, Woolfson AD. Microneedle-based drug delivery systems: Microfabrication, drug delivery, and safety. Drug Deliv. 2010;17:187–207. doi: 10.3109/10717541003667798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garland MJ, Migalska K, Mazlelaa T, Mahmood T, Raghu T, Singh R, Woolfson AD, Donnelly RF. Microneedle arrays as medical devices for enhanced transdermal drug delivery. Expert Rev Med Devic. 2011;8:459–482. doi: 10.1586/erd.11.20. [DOI] [PubMed] [Google Scholar]
- 20.Gittard SD, Ovsianikov A, Chichkov BN, Doraiswamy A, Narayan RJ. Two-photon polymerization of microneedles for transdermal drug delivery. Expert Opin Drug Deliv. 2010;7:513–533. doi: 10.1517/17425241003628171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalluri H, Banga AK. Microneedles and transdermal drug delivery. J Drug Deliv Sci Tec. 2009;19:303–310. [Google Scholar]
- 22.Khanna P, Strom JA, Malone JI, Bhansali S. Microneedle-based automated therapy for diabetes mellitus. J Diabetes Sci Technol. 2008;2:1122–1129. doi: 10.1177/193229680800200621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McAllister DV, Allen MG, Prausnitz MR. Microfabricated microneedles for gene and drug delivery. Annu Rev Biomed Eng. 2000;2:289–313. doi: 10.1146/annurev.bioeng.2.1.289. [DOI] [PubMed] [Google Scholar]
- 24.Milewski M, Brogden NK, Stinchcomb AL. Current aspects of formulation efforts and pore lifetime related to microneedle treatment of skin. Expert Opin Drug Deliv. 2010;7:617–629. doi: 10.1517/17425241003663228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prausnitz MR. Microneedles for transdermal drug delivery. Adv Drug Del Rev. 2004;56:581–587. doi: 10.1016/j.addr.2003.10.023. [DOI] [PubMed] [Google Scholar]
- 26.Reed ML, Lye WK. Microsystems for drug and gene delivery. Proc IEEE. 2004;92:56–75. [Google Scholar]
- 27.Sachdeva V, Banga AK. Microneedles and their applications. Recent Pat Drug Deliv Formul. 2011;5:95–132. doi: 10.2174/187221111795471445. [DOI] [PubMed] [Google Scholar]
- 28.Shah UU, Roberts M, Orlu Gul M, Tuleu C, Beresford MW. Needle-free and microneedle drug delivery in children: A case for disease-modifying antirheumatic drugs (DMARDs) Int J Pharm. 2011;416:1–11. doi: 10.1016/j.ijpharm.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 29.Singh TRR, Dunne NJ, Cunningham E, Donnelly RF. Review of patents on microneedle applicators. Recent Pat Drug Deliv Formul. 2011;5:11–23. doi: 10.2174/187221111794109484. [DOI] [PubMed] [Google Scholar]
- 30.Singh TRR, Garland MJ, Cassidy CM, Migalska K, Demir YK, Abdelghany S, Ryan E, Woolfson AD, Donnelly RF. Microporation techniques for enhanced delivery of therapeutic agents. Recent Pat Drug Deliv Formul. 2010;4:1–17. doi: 10.2174/187221110789957174. [DOI] [PubMed] [Google Scholar]
- 31.Sivamani RK, Liepmann D, Malbach HI. Microneedles and transdermal applications. Expert Opin Drug Deliv. 2007;4:19–25. doi: 10.1517/17425247.4.1.19. [DOI] [PubMed] [Google Scholar]
- 32.Vandervoort J, Ludwig A. Microneedles for transdermal drug delivery: a minireview. Front Biosci. 2008;13:1711–1715. doi: 10.2741/2794. [DOI] [PubMed] [Google Scholar]
- 33.Bariya SH, Gohel MC, Mehta TA, Sharma OP. Microneedles: an emerging transdermal drug delivery system. J Pharm Pharmacol. 2012;64:11–29. doi: 10.1111/j.2042-7158.2011.01369.x. [DOI] [PubMed] [Google Scholar]
- 34.Park HA, Roy S, Khanna S, Sen CK. Current technologies in single-cell microinjection and application to study signal transduction. In: Das DK, editor. Methods in Redox Signaling. Mary Ann Liebert; New Rochelle: 2010. pp. 71–77. [Google Scholar]
- 35.Gerstel MS, Place VA. U.S. Patent 3,964,482. Drug delivery device. 1976
- 36.Madou MJ. Fundamentals of microfabrication and nanotechnology. CRC Press; Boca Raton, FL: 2011. [Google Scholar]
- 37.Williams A. Transdermal and topical drug delivery. Pharmaceutical Press; London: 2003. [Google Scholar]
- 38.McAllister DV, Wang PM, Davis SP, Park JH, Canatella PJ, Allen MG, Prausnitz MR. Microfabricated needles for transdermal delivery of macromolecules and nanoparticles: Fabrication methods and transport studies. Proc Natl Acad Sci U S A. 2003;100:13755–13760. doi: 10.1073/pnas.2331316100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wilke N, Mulcahy A, Ye SR, Morrissey A. Process optimization and characterization of silicon microneedles fabricated by wet etch technology. Microelectron J. 2005;36:650–656. [Google Scholar]
- 40.Henry S, McAllister DV, Allen MG, Prausnitz MR. Microfabricated microneedles: A novel approach to transdermal drug delivery. J Pharm Sci. 1998;87:922–925. doi: 10.1021/js980042+. [DOI] [PubMed] [Google Scholar]
- 41.Donnelly RF, Majithiya R, Singh TRR, Morrow DIJ, Garland MJ, Demir YK, Migalska K, Ryan E, Gillen D, Scott CJ, Woolfson AD. Design, optimization and characterisation of polymeric microneedle arrays prepared by a novel laser-based micromoulding technique. Pharm Res. 2011;28:41–57. doi: 10.1007/s11095-010-0169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jin CY, Han MH, Lee SS, Choi YH. Mass producible and biocompatible microneedle patch and functional verification of its usefulness for transdermal drug delivery. Biomed Microdevices. 2009;11:1195–1203. doi: 10.1007/s10544-009-9337-1. [DOI] [PubMed] [Google Scholar]
- 43.Moon SJ, Lee SS, Lee HS, Kwon TH. Fabrication of microneedle array using LIGA and hot embossing process. Microsyst Technol. 2005;11:311–318. [Google Scholar]
- 44.Park JH, Allen MG, Prausnitz MR. Biodegradable polymer microneedles: Fabrication, mechanics and transdermal drug delivery. J Controlled Release. 2005;104:51–66. doi: 10.1016/j.jconrel.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 45.Li GH, Badkar A, Nema S, Kolli CS, Banga AK. In vitro transdermal delivery of therapeutic antibodies using maltose microneedles. Int J Pharm. 2009;368:109–115. doi: 10.1016/j.ijpharm.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 46.Gill HS, Prausnitz MR. Coated microneedles for transdermal delivery. J Controlled Release. 2007;117:227–237. doi: 10.1016/j.jconrel.2006.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martanto W, Davis SP, Holiday NR, Wang J, Gill HS, Prausnitz MR. Transdermal delivery of insulin using microneedles in vivo. Pharm Res. 2004;21:947–952. doi: 10.1023/b:pham.0000029282.44140.2e. [DOI] [PubMed] [Google Scholar]
- 48.Matriano JA, Cormier M, Johnson J, Young WA, Buttery M, Nyam K, Daddona PE. Macroflux (R) microprojection array patch technology: A new and efficient approach for intracutaneous immunization. Pharm Res. 2002;19:63–70. doi: 10.1023/a:1013607400040. [DOI] [PubMed] [Google Scholar]
- 49.Omatsu T, Chujo K, Miyamoto K, Okida M, Nakamura K, Aoki N, Morita R. Metal microneedle fabrication using twisted light with spin. Optics Express. 2010;18:17967–17973. doi: 10.1364/OE.18.017967. [DOI] [PubMed] [Google Scholar]
- 50.Jung PG, Lee TW, Oh DJ, Hwang SJ, Jung ID, Lee SM, Ko JS. Nickel microneedles fabricated by sequential copper and nickel electroless plating and copper chemical wet etching. Sensors Mater. 2008;20:45–53. [Google Scholar]
- 51.Bystrova S, Luttge R. Micromolding for ceramic microneedle arrays. Microelectron Eng. 2011;88:1681–1684. [Google Scholar]
- 52.Ovsianikov A, Chichkov B, Mente P, Monteiro-Riviere NA, Doraiswamy A, Narayan RJ. Two photon polymerization of polymer-ceramic hybrid materials for transdermal drug delivery. Int J Appl Ceram Tec. 2007;4:22–29. [Google Scholar]
- 53.Yan G, Warner KS, Zhang J, Sharma S, Gale BK. Evaluation needle length and density of microneedle arrays in the pretreatment of skin for transdermal drug delivery. Int J Pharm. 2010;391:7–12. doi: 10.1016/j.ijpharm.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 54.Ji J, Tay FEH, Miao JM, Iliescu C. Microfabricated silicon microneedle array for transdermal drug delivery. International Mems Conference; 2006; Bristol: Iop Publishing Ltd; 2006. pp. 1127–1131. [Google Scholar]
- 55.Qiu YQ, Gao YH, Hu KJ, Li F. Enhancement of skin permeation of docetaxel: A novel approach combining microneedle and elastic liposomes. J Controlled Release. 2008;129:144–150. doi: 10.1016/j.jconrel.2008.04.019. [DOI] [PubMed] [Google Scholar]
- 56.Wei-Ze L, Mei-Rong H, Jian-Ping Z, Yong-Qiang Z, Bao-Hua H, Ting L, Yong Z. Super-short solid silicon microneedles for transdermal drug delivery applications. Int J Pharm. 2010;389:122–129. doi: 10.1016/j.ijpharm.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 57.Chen YT, Hsu CC, Tsai CH, Kang SW. Fabrication of microneedles. J Mar Sci Technol. 2010;18:243–248. [Google Scholar]
- 58.Suner S, Fellows MR, Vargas-Irwin C, Nakata GK, Donoghue JP. Reliability of signals from a chronically implanted, silicon-based electrode array in non-human primate primary motor cortex. IEEE Trans Neural Syst Rehab Eng. 2005;13:524–541. doi: 10.1109/TNSRE.2005.857687. [DOI] [PubMed] [Google Scholar]
- 59.Rousche PJ, Normann RA. Chronic intracortical microstimulation of cat auditory cortex using a 100 penetrating electrode array. J Physiol. 1997;499:87–88. [Google Scholar]
- 60.Rousche PJ, Normann RA. Chronic recording capability of the Utah Intracortical Electrode Array in cat sensory cortex. J Neurosci Methods. 1998;82:1–15. doi: 10.1016/s0165-0270(98)00031-4. [DOI] [PubMed] [Google Scholar]
- 61.Kelly RC, Smith MA, Samonds JM, Kohn A, Bonds AB, Movshon JA, Lee TS. Comparison of recordings from microelectrode arrays and single electrodes in the visual cortex. J Neurosci. 2007;27:261–264. doi: 10.1523/JNEUROSCI.4906-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gower MC. Industrial applications of laser micromachining. Optics Express. 2000;7:56–67. doi: 10.1364/oe.7.000056. [DOI] [PubMed] [Google Scholar]
- 63.Davis SP, Martanto W, Allen MG, Prausnitz MR. Hollow metal microneedles for insulin delivery to diabetic rats. IEEE Trans Biomed Eng. 2005;52:909–915. doi: 10.1109/TBME.2005.845240. [DOI] [PubMed] [Google Scholar]
- 64.Yuzhakov VV. The AdminPen microneedle device for painless & convenient drug delivery. Drug Deliv Technol. 2010;10:32–36. [Google Scholar]
- 65.Fomani AA, Mansour RR. Fabrication and Characterization of Flexible Neural Microprobes with Improved Structural Design. Sens Actuators A Phys. 2011;168:233–241. [Google Scholar]
- 66.Choi SO, Kim YC, Park JH, Hutcheson J, Gill HS, Yoon YK, Prausnitz MR, Allen MG. An electrically active microneedle array for electroporation. Biomed Microdevices. 2010;12:263–273. doi: 10.1007/s10544-009-9381-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yoon YK, Park JH, Allen MG. Multidirectional UV lithography for complex 3-D MEMS structures. J Microelectromech Sys. 2006;15:1121–1130. [Google Scholar]
- 68.Park JH, Yoon YK, Choi SO, Prausnitz MR, Allen MG. Tapered conical polymer microneedles fabricated using an integrated lens technique for transdermal drug delivery. IEEE Trans Biomed Eng. 2007;54:903–913. doi: 10.1109/TBME.2006.889173. [DOI] [PubMed] [Google Scholar]
- 69.Kim K, Park DS, Lu HM, Che W, Kim K, Lee JB, Ahn CH. A tapered hollow metallic microneedle array using backside exposure of SU-8. J Micromech Microeng. 2004;14:597–603. [Google Scholar]
- 70.Sugiyama S, Khumpuang S, Kawaguchi G. PCT technique for deep x-ray lithography and applications. J Micromech Microeng. 2004;14:1399–1404. [Google Scholar]
- 71.Han M, Hyun DH, Park HH, Lee SS, Kim CH, Kim C. A novel fabrication process for out-of-plane microneedle sheets of biocompatible polymer. J Micromech Microeng. 2007;17:1184–1191. [Google Scholar]
- 72.Gittard SD, Ovsianikov A, Monteiro-Riviere NA, Lusk J, Morel P, Minghetti P, Lenardi C, Chichkov BN, Narayan RJ. Fabrication of polymer microneedles using a two-photon polymerization and micromolding process. J Diabetes Sci Technol. 2009;3:304–311. doi: 10.1177/193229680900300211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lee K-S, Kim RH, Yang D-Y, Park SH. Advances in 3D nano/microfabrication using two-photon initiated polymerization. Prog Polym Sci. 2008;33:631–681. [Google Scholar]
- 74.Aoyagi S, Izumi H, Fukuda M. Biodegradable polymer needle with various tip angles and consideration on insertion mechanism of mosquito’s proboscis. Sens Actuators A Phys. 2008;143:20–28. [Google Scholar]
- 75.Matteucci M, Fanetti M, Casella M, Gramatica F, Gavioli L, Tormen M, Grenci G, De Angelis F, Di Fabrizio E. Poly vinyl alcohol re-usable masters for microneedle replication. Microelectron Eng. 2009;86:752–756. [Google Scholar]
- 76.Moon SJ, Lee SS. A novel fabrication method of a microneedle array using inclined deep x-ray exposure. J Micromech Microeng. 2005;15:903–911. [Google Scholar]
- 77.Gittard SD, Narayan RJ, Jin C, Ovsianikov A, Chichkov BN, Monteiro-Riviere NA, Stafslien S, Chisholm B. Pulsed laser deposition of antimicrobial silver coating on Ormocer (R) microneedles. Biofabrication. 2009;1:041001. doi: 10.1088/1758-5082/1/4/041001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Doraiswamy A, Jin C, Narayan R, Mageswaran P, Mente P, Modi R, Auyeung R, Chrisey DB, Ovsianikov A, Chichkov B. Two photon induced polymerization of organic-inorganic hybrid biomaterials for microstructured medical devices. Acta Biomater. 2006;2:267–275. doi: 10.1016/j.actbio.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 79.Aust MC, Fernandes D, Kolokythas P, Kaplan HM, Vogt PM. Percutaneous collagen induction therapy: an alternative treatment for scars, wrinkles, and skin laxity. Plast Reconstr Surg. 2008;121:1421. doi: 10.1097/01.prs.0000304612.72899.02. [DOI] [PubMed] [Google Scholar]
- 80.Aust MC, Fernandes D, Kolokythas P, Kaplan HM, Vogt PM. Percutaneous collagen induction therapy: an alternative treatment for scars, wrinkles, and skin laxity. Plast Reconstr Surg. 2008;121:1421. doi: 10.1097/01.prs.0000304612.72899.02. [DOI] [PubMed] [Google Scholar]
- 81.Doddaballapur S. Microneedling with dermaroller. J Cutan Aesthet Surg. 2009;2:110. doi: 10.4103/0974-2077.58529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fabbrocini G, Fardella N, Monfrecola A, Proietti I, Innocenzi D. Acne scarring treatment using skin needling. Clin Exp Dermatol. 2009;34:874–879. doi: 10.1111/j.1365-2230.2009.03291.x. [DOI] [PubMed] [Google Scholar]
- 83.Majid I. Microneedling therapy in atrophic facial scars: An objective assessment. J Cutan Aesthet Surg. 2009;2:26. doi: 10.4103/0974-2077.53096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.So JW, Park HH, Lee SS, Kim DC, Shin SC, Cho CW. Effect of microneedle on the pharmacokinetics of ketoprofen from its transdermal formulations. Drug Deliv. 2009;16:52–56. doi: 10.1080/10717540802518082. [DOI] [PubMed] [Google Scholar]
- 85.Yoon J, Son T, Choi EH, Choi B, Nelson JS, Jung B. Enhancement of optical skin clearing efficacy using a microneedle roller. J Biomed Opt. 2008;13:021103. doi: 10.1117/1.2907483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhou CP, Liu YL, Wang HL, Zhang PX, Zhang JL. Transdermal delivery of insulin using microneedle rollers in vivo. Int J Pharm. 2010;392:127–133. doi: 10.1016/j.ijpharm.2010.03.041. [DOI] [PubMed] [Google Scholar]
- 87.Park JH, Choi SO, Seo S, Choy YB, Prausnitz MR. A microneedle roller for transdermal drug delivery. Eur J Pharm Biopharm. 2010;76:282–289. doi: 10.1016/j.ejpb.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 88.Gill HS, Prausnitz MR. Coating formulations for microneedles. Pharm Res. 2007;24:1369–1380. doi: 10.1007/s11095-007-9286-4. [DOI] [PubMed] [Google Scholar]
- 89.Ameri M, Fan SC, Maa Y-F. Parathyroid hormone PTH(1-34) formulation that enables uniform coating on a novel transdermal microprojection delivery system. Pharm Res. 2010;27:303–313. doi: 10.1007/s11095-009-0019-8. [DOI] [PubMed] [Google Scholar]
- 90.Andrianov AK, DeCollibus DP, Gillis HA, Kha HH, Marin A, Prausnitz MR, Babiuk LA, Townsend H, Mutwiri G. Poly [di(carboxylatophenoxy)phosphazene] is a potent adjuvant for intradermal immunization. Proc Natl Acad Sci U S A. 2009;106:18936–18941. doi: 10.1073/pnas.0908842106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kim YC, Quan FS, Compans RW, Kang SM, Prausnitz MR. Formulation and coating of microneedles with inactivated influenza virus to improve vaccine stability and immunogenicity. J Control Release. 2010;142:187–195. doi: 10.1016/j.jconrel.2009.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Stokes RJ, Evans DF, Errico M. Liquid coating processes. Wiley-VCH; Weinheim, Germany: 1997. [Google Scholar]
- 93.Saurer EM, Flessner RM, Sullivan SP, Prausnitz MR, Lynn DM. Layer-by-layer assembly of DNA- and protein-containing films on microneedles for drug delivery to the skin. Biomacromolecules. 2010;11:3136–3143. doi: 10.1021/bm1009443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.DeMuth PC, Su XF, Samuel RE, Hammond PT, Irvine DJ. Nano-layered microneedles for transcutaneous delivery of polymer nanoparticles and plasmid DNA. Adv Mat. 2010;22:4851–4856. doi: 10.1002/adma.201001525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chen XF, Prow TW, Crichton ML, Jenkins DWK, Roberts MS, Frazer IH, Fernando GJP, Kendall MAF. Dry-coated microprojection array patches for targeted delivery of immunotherapeutics to the skin. J Controlled Release. 2009;139:212–220. doi: 10.1016/j.jconrel.2009.06.029. [DOI] [PubMed] [Google Scholar]
- 96.McGrath MG, Vrdoljak A, O’Mahony C, Oliveira JC, Moore AC, Crean AM. Determination of parameters for successful spray coating of silicon microneedle arrays. Int J Pharm. 2011;415:140–149. doi: 10.1016/j.ijpharm.2011.05.064. [DOI] [PubMed] [Google Scholar]
- 97.Cormier M, Johnson B, Ameri M, Nyam K, Libiran L, Zhang DD, Daddona P. Transdermal delivery of desmopressin using a coated microneedle array patch system. J Controlled Release. 2004;97:503–511. doi: 10.1016/j.jconrel.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 98.Kim YC, Quan FS, Compans RW, Kang SM, Prausnitz MR. Formulation of microneedles coated with influenza virus-like particle vaccine. AAPS PharmSciTech. 2010;11:1193–1201. doi: 10.1208/s12249-010-9471-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Han M, Kim DK, Kang SH, Yoon HR, Kim BY, Lee SS, Kim KD, Lee HG. Improvement in antigen-delivery using fabrication of a grooves-embedded microneedle array. Sens Actuat B Chem. 2009;137:274–280. [Google Scholar]
- 100.Gill HS, Prausnitz MR. Pocketed microneedles for drug delivery to the skin. J Phys Chem Solids. 2008;69:1537–1541. doi: 10.1016/j.jpcs.2007.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jiang J, Gill HS, Ghate D, McCarey BE, Patel SR, Edelhauser HF, Prausnitz MR. Coated microneedles for drug delivery to the eye. Invest Ophthalmol Vis Sci. 2007;48:4038–4043. doi: 10.1167/iovs.07-0066. [DOI] [PubMed] [Google Scholar]
- 102.Zhang Y, Brown K, Siebenaler K, Determan A, Dohmeier D, Hansen K. Development of lidocaine-coated microneedle product for rapid, safe, and prolonged local analgesic action. Pharm Res. 2012;29:170–177. doi: 10.1007/s11095-011-0524-4. [DOI] [PubMed] [Google Scholar]
- 103.Marin A, Andrianov AK. Carboxymethylcellulose-Chitosan-Coated microneedles with modulated hydration properties. J Appl Polym Sci. 2011;121:395–401. [Google Scholar]
- 104.Andrianov AK, Marin A, DeCollibus DP. Microneedles with intrinsic immunoadjuvant properties: microfabrication, protein stability, and modulated release. Pharm Res. 2011;28:58–65. doi: 10.1007/s11095-010-0133-7. [DOI] [PubMed] [Google Scholar]
- 105.Lin WQ, Cormier M, Samiee A, Griffin A, Johnson B, Teng CL, Hardee GE, Daddona PE. Transdermal delivery of antisense oligonucleotides with microprojection patch (Macroflux (R)) technology. Pharm Res. 2001;18:1789–1793. doi: 10.1023/a:1013395102049. [DOI] [PubMed] [Google Scholar]
- 106.Quan FS, Kim YC, Vunnava A, Yoo DG, Song JM, Prausnitz MR, Compans RW, Kang SM. Intradermal vaccination with influenza virus-like particles by using microneedles induces protection superior to that with intramuscular immunization. J Virol. 2010;84:7760–7769. doi: 10.1128/JVI.01849-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Weldon WC, Martin MP, Zarnitsyn V, Wang BZ, Koutsonanos D, Skountzou I, Prausnitz MR, Compans RW. Microneedle vaccination with stabilized recombinant influenza virus hemagglutinin induces improved protective immunity. ClinVaccine Immunol. 2011;18:647–654. doi: 10.1128/CVI.00435-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Corbett HJ, Fernando GJP, Chen XF, Frazer IH, Kendall MAF. Skin vaccination against cervical cancer associated human papillomavirus with a novel micro-projection array in a mouse model. PLoS One. 2010;5:e13460. doi: 10.1371/journal.pone.0013460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Prow TW, Chen X, Prow NA, Fernando GJ, Tan CS, Raphael AP, Chang D, Ruutu MP, Jenkins DW, Pyke A, Crichton ML, Raphaelli K, Goh LY, Frazer IH, Roberts MS, Gardner J, Khromykh AA, Suhrbier A, Hall RA, Kendall MA. Nanopatch-targeted skin vaccination against West Nile virus and Chikungunya virus in mice. Small. 2010;6:1776–1784. doi: 10.1002/smll.201000331. [DOI] [PubMed] [Google Scholar]
- 110.Hiraishi Y, Nandakumar S, Choi SO, Lee JW, Kim YC, Posey JE, Sable SB, Prausnitz MR. Bacillus Calmette-Guerin vaccination using a microneedle patch. Vaccine. 2011;29:2626–2636. doi: 10.1016/j.vaccine.2011.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gill HS, Sõderholm J, Prausnitz MR, Sällberg M. Cutaneous vaccination using microneedles coated with hepatitis C DNA vaccine. Gene Ther. 2010;17:811–814. doi: 10.1038/gt.2010.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chen XF, Kask AS, Crichton ML, McNeilly C, Yukiko S, Dong LC, Marshak JO, Jarrahian C, Fernando GJP, Chen DX, Koelle DM, Kendall MAF. Improved DNA vaccination by skin-targeted delivery using dry-coated densely-packed microprojection arrays. J Controlled Release. 2010;148:327–333. doi: 10.1016/j.jconrel.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 113.Lee JW, Park JH, Prausnitz MR. Dissolving microneedles for transdermal drug delivery. Biomaterials. 2008;29:2113–2124. doi: 10.1016/j.biomaterials.2007.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Raphael AP, Prow TW, Crichton ML, Chen XF, Fernando GIP, Kendall MAF. Targeted, needle-free vaccinations in skin using multi layered, densely-packed dissolving microprojection arrays. Small. 2010;6:1785–1793. doi: 10.1002/smll.201000326. [DOI] [PubMed] [Google Scholar]
- 115.Ito Y, Hagiwara E, Saeki A, Sugioka N, Takada K. Sustained-release self-dissolving micropiles for percutaneous absorption of insulin in mice. J Drug Target. 2007;15:323–326. doi: 10.1080/10611860701349794. [DOI] [PubMed] [Google Scholar]
- 116.Ito Y, Ohashi Y, Saeki A, Sugioka N, Takada K. Antihyperglycemic effect of insulin from self-dissolving micropiles in dogs. Chem Pharm Bull. 2008;56:243–246. doi: 10.1248/cpb.56.243. [DOI] [PubMed] [Google Scholar]
- 117.Ito Y, Murakami A, Maeda T, Sugioka N, Takada K. Evaluation of self-dissolving needles containing low molecular weight heparin (LMWH) in rats. Int J Pharm. 2008;349:124–129. doi: 10.1016/j.ijpharm.2007.07.036. [DOI] [PubMed] [Google Scholar]
- 118.Fukushima K, Yamazaki T, Hasegawa R, Ito Y, Sugioka N, Takada K. Pharmacokinetic and pharmacodynamic evaluation of insulin dissolving microneedles in dogs. Diabetes Technol The. 2010;12:465–474. doi: 10.1089/dia.2009.0176. [DOI] [PubMed] [Google Scholar]
- 119.Ito Y, Maeda T, Fukushima K, Sugioka N, Takada K. Permeation Enhancement of Ascorbic Acid by Self-Dissolving Micropile Array Tip through Rat Skin. Chem Pharm Bull. 2010;58:458–463. doi: 10.1248/cpb.58.458. [DOI] [PubMed] [Google Scholar]
- 120.Ito Y, Yamazaki T, Sugioka N, Takada K. Self-dissolving micropile array tips for percutaneous administration of insulin. J Mater Sci Mater Med. 2010;21:835–841. doi: 10.1007/s10856-009-3923-x. [DOI] [PubMed] [Google Scholar]
- 121.Ito Y, Hasegawa R, Fukushima K, Sugioka N, Takada K. Self-dissolving micropile array chip as percutaneous delivery system of protein drug. Biol Pharm Bull. 2010;33:683–690. doi: 10.1248/bpb.33.683. [DOI] [PubMed] [Google Scholar]
- 122.Fukushima K, Ise A, Morita H, Hasegawa R, Ito Y, Sugioka N, Takada K. Two-layered dissolving microneedles for percutaneous delivery of peptide/protein drugs in rats. Pharm Res. 2011;28:7–21. doi: 10.1007/s11095-010-0097-7. [DOI] [PubMed] [Google Scholar]
- 123.Ito Y, Murano H, Hamasaki N, Fukushima K, Takada K. Incidence of low bioavailability of leuprolide acetate after percutaneous administration to rats by dissolving microneedles. Int J Pharm. 2011;407:126–131. doi: 10.1016/j.ijpharm.2011.01.039. [DOI] [PubMed] [Google Scholar]
- 124.Ito Y, Ohashi Y, Shiroyama K, Sugioka N, Takada K. Self-dissolving micropiles for the percutaneous absorption of recombinant human growth hormone in rats. Biol Pharm Bull. 2008;31:1631–1633. doi: 10.1248/bpb.31.1631. [DOI] [PubMed] [Google Scholar]
- 125.Ito Y, Hagiwara E, Saeki A, Sugioka N, Takada K. Feasibility of microneedles for percutaneous absorption of insulin. Eur J Pharm Sci. 2006;29:82–88. doi: 10.1016/j.ejps.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 126.Ito Y, Yoshimitsu JI, Shiroyama K, Sugioka N, Takada K. Self-dissolving microneedles for the percutaneous absorption of EPO in mice. J Drug Target. 2006;14:255–261. doi: 10.1080/10611860600785080. [DOI] [PubMed] [Google Scholar]
- 127.Sullivan SP, Murthy N, Prausnitz MR. Minimally invasive protein delivery with rapidly dissolving polymer microneedles. Adv Mater. 2008;20:933–938. doi: 10.1002/adma.200701205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sullivan SP, Koutsonanos DG, Martin MD, Lee JW, Zarnitsyn V, Choi SO, Murthy N, Compans RW, Skountzou I, Prausnitz MR. Dissolving polymer microneedle patches for influenza vaccination. Nat Med. 2010;16:915–920. doi: 10.1038/nm.2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chu LY, Choi SO, Prausnitz MR. Fabrication of dissolving polymer microneedles for controlled drug encapsulation and delivery: Bubble and pedestal microneedle designs. J Pharm Sci. 2010;99:4228–4238. doi: 10.1002/jps.22140. [DOI] [PubMed] [Google Scholar]
- 130.Chu LY, Prausnitz MR. Separable arrowhead microneedles. J Controlled Release. 2011;149:242–249. doi: 10.1016/j.jconrel.2010.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wendorf JR, Ghartey-Tagoe EB, Williams SC, Enioutina E, Singh P, Cleary GW. Transdermal delivery of macromolecules using solid-state biodegradable microstructures. Pharm Res. 2011;28:22–30. doi: 10.1007/s11095-010-0174-y. [DOI] [PubMed] [Google Scholar]
- 132.Park JH, Allen MG, Prausnitz MR. Polymer microneedles for controlled-release drug delivery. Pharm Res. 2006;23:1008–1019. doi: 10.1007/s11095-006-0028-9. [DOI] [PubMed] [Google Scholar]
- 133.You X, Chang J-h, Ju B-K, Pak JJ. Rapidly dissolving fibroin microneedles for transdermal drug delivery. Mat Sci Eng C. 2011;31:1632–1636. [Google Scholar]
- 134.Martin CJ, Allender CJ, Brain KR, Morrissey A, Birchall JC. Low temperature fabrication of biodegradable sugar glass microneedles for transdermal drug delivery applications. J Controlled Release. 2012;158:93–101. doi: 10.1016/j.jconrel.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 135.Miyano T, Tobinaga Y, Kanno T, Matsuzaki Y, Takeda H, Wakui M, Hanada K. Sugar micro needles as transdermic drug delivery system. Biomed Microdevices. 2005;7:185–188. doi: 10.1007/s10544-005-3024-7. [DOI] [PubMed] [Google Scholar]
- 136.Aoyagi S, Izumi H, Isono Y, Fukuda M, Ogawa H. Laser fabrication of high aspect ratio thin holes on biodegradable polymer and its application to a microneedle. Sens Actuat A Phys. 2007;139:293–302. [Google Scholar]
- 137.Kim M, Jung B, Park J-H. Hydrogel swelling as a trigger to release biodegradable polymer microneedles in skin. Biomaterials. 2012;33:668–678. doi: 10.1016/j.biomaterials.2011.09.074. [DOI] [PubMed] [Google Scholar]
- 138.Lee K, Lee CY, Jung H. Dissolving microneedles for transdermal drug administration prepared by stepwise controlled drawing of maltose. Biomaterials. 2011;32:3134–3140. doi: 10.1016/j.biomaterials.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 139.Min J, Park J-H, Yoon H, Choy Y. Ultrasonic welding method to fabricate polymer microstructure encapsulating protein with minimum damage. Macromol Res. 2008;16:570–573. [Google Scholar]
- 140.Park JH, Choi SO, Kamath R, Yoon YK, Allen MG, Prausnitz MR. Polymer particle-based micromolding to fabricate novel microstructures. Biomed Microdevices. 2007;9:223–234. doi: 10.1007/s10544-006-9024-4. [DOI] [PubMed] [Google Scholar]
- 141.Roxhed N, Gasser TC, Griss P, Holzapfel GA, Stemme G. Penetration-enhanced ultrasharp microneedles and prediction on skin interaction for efficient transdermal drug delivery. J Microelectromech S. 2007;16:1429–1440. [Google Scholar]
- 142.Gardeniers HJGE, Luttge R, Berenschot EJW, de Boer MJ, Yeshurun SY, Hefetz M, van’t Oever R, van den Berg A. Silicon micromachined hollow microneedles for transdermal liquid transport. J Microelectromech S. 2003;12:855–862. [Google Scholar]
- 143.Luttge R, Berenschot EJW, de Boer MJ, Altpeter DM, Vrouwe EX, van den Berg A, Elwenspoek M. Integrated lithographic molding for microneedle-based devices. J Microelectromech S. 2007;16:872–884. [Google Scholar]
- 144.Perennes F, Marmiroli B, Matteucci M, Tormen M, Vaccari L, Di Fabrizio E. Sharp beveled tip hollow microneedle arrays fabricated by LIGA and 3D soft lithography with polyvinyl alcohol. J Micromech Microeng. 2006;16:473–479. [Google Scholar]
- 145.Ma B, Liu S, Gan Z, Liu G, Cai X, Zhang H, Yang Z. A PZT insulin pump integrated with a silicon microneedle array for transdermal drug delivery. Microfluid Nanofluid. 2006;2:417–423. [Google Scholar]
- 146.Yu LM, Tay FEH, Guo DG, Xu L, Yap KL. A microfabricated electrode with hollow microneedles for ECG measurement. Sens Actuat A Phys. 2009;151:17–22. [Google Scholar]
- 147.Teo MAL, Shearwood C, Ng KC, Lu J, Moochhala S. In vitro and in vivo characterization of MEMS microneedles. Biomed Microdevices. 2005;7:47–52. doi: 10.1007/s10544-005-6171-y. [DOI] [PubMed] [Google Scholar]
- 148.Wilke N, Hibert C, O’Brien J, Morrissey A. Silicon microneedle electrode array with temperature monitoring for electroporation. Sens Actuat A Phys. 2005;123–24:319–325. [Google Scholar]
- 149.Mukerjee E, Collins SD, Isseroff RR, Smith RL. Microneedle array for transdermal biological fluid extraction and in situ analysis. Sens Actuat A Phys. 2004;114:267–275. [Google Scholar]
- 150.Zhang PY, Dalton CL, Jullien G. Design and fabrication of MEMS-based microneedle arrays for medical applications. Microsyst Technol. 2009;15:1073–1082. [Google Scholar]
- 151.Baron N, Passave J, Guichardaz B, Cabodevila G. Investigations of development process of high hollow beveled microneedles using a combination of ICP RIE and dicing saw. Microsyst Technol. 2008;14:1475–1480. [Google Scholar]
- 152.Wang PM, Cornwell M, Hill J, Prausnitz MR. Precise microinjection into skin using hollow microneedles. J Invest Dermatol. 2006;126:1080–1087. doi: 10.1038/sj.jid.5700150. [DOI] [PubMed] [Google Scholar]
- 153.Daugimont L, Baron N, Vandermeulen G, Pavselj N, Miklavcic D, Jullien M-C, Cabodevila G, Mir L, Préat V. Hollow microneedle arrays for intradermal drug delivery and DNA electroporation. J Membr Biol. 2010;236:117–125. doi: 10.1007/s00232-010-9283-0. [DOI] [PubMed] [Google Scholar]
- 154.Miller PR, Gittard SD, Edwards TL, Lopez DM, Xiao X, Wheeler DR, Monteiro-Riviere NA, Brozik SM, Polsky R, Narayan RJ. Integrated carbon fiber electrodes within hollow polymer microneedles for transdermal electrochemical sensing. Biomicrofluidics. 2011;5:013415. doi: 10.1063/1.3569945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Khumpuang S, Horade M, Fujioka K, Sugiyama S. Geometrical strengthening and tip-sharpening of a microneedle array fabricated by X-ray lithography. Microsyst Technol. 2007;13:209–214. [Google Scholar]
- 156.Moon SJ, Lee SS, Lee HS, Kwon TH. Fabrication of microneedle array using LIGA and hot embossing process. Microsyst Technol. 2005;11:311–318. [Google Scholar]
- 157.Lee K, Lee HC, Lee DS, Jung H. Drawing lithography: Three-dimensional fabrication of an ultrahigh-aspect-ratio microneedle. AdvMat. 2010;22:483–486. doi: 10.1002/adma.200902418. [DOI] [PubMed] [Google Scholar]
- 158.Bodhale DW, Nisar A, Afzulpurkar N. Structural and microfluidic analysis of hollow side-open polymeric microneedles for transdermal drug delivery applications. Microfluid Nanofluid. 2010;8:373–392. [Google Scholar]
- 159.Jung P, Lee TW, Oh DJ, Hwang SJ, Jung I, Lee S, Ko J. Nickel microneedles fabricated by sequential copper and nickel electroless plating and copper chemical wet etching. Sens Mater. 2008;20:45–53. [Google Scholar]
- 160.Rodriguez A, Molinero D, Valera E, Trifonov T, Marsal LF, Pallares J, Alcubilla R. Fabrication of silicon oxide microneedles from macroporous silicon. Sensor Actuat B Chem. 2005;109:135–140. [Google Scholar]
- 161.Zhu MW, Li HW, Chen XL, Tang YF, Lu MH, Chen YF. Silica needle template fabrication of metal hollow microneedle arrays. J Micromech Microeng. 2009;19:115010. [Google Scholar]
- 162.Hafeli UO, Mokhtari A, Liepmann D, Stoeber B. In vivo evaluation of a microneedle-based miniature syringe for intradermal drug delivery. Biomed Microdevices. 2009;11:943–950. doi: 10.1007/s10544-009-9311-y. [DOI] [PubMed] [Google Scholar]
- 163.Martanto W, Moore JS, Kashlan O, Kamath R, Wang PM, O’Neal JM, Prausnitz MR. Microinfusion using hollow microneedles. Pharm Res. 2006;23:104–113. doi: 10.1007/s11095-005-8498-8. [DOI] [PubMed] [Google Scholar]
- 164.Burton S, Ng C-Y, Simmers R, Moeckly C, Brandwein D, Gilbert T, Johnson N, Brown K, Alston T, Prochnow G, Siebenaler K, Hansen K. Rapid intradermal delivery of liquid formulations using a hollow microstructured array. Pharm Res. 2011;28:31–40. doi: 10.1007/s11095-010-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ashraf M, Tayyaba S, Nisar A, Afzulpurkar N, Bodhale D, Lomas T, Poyai A, Tuantranont A. Design, fabrication and analysis of silicon hollow microneedles for transdermal drug delivery system for treatment of hemodynamic dysfunctions. Cardiovasc Eng. 2010;10:91–108. doi: 10.1007/s10558-010-9100-5. [DOI] [PubMed] [Google Scholar]
- 166.Ali WG, Nagib G. Embedded control design for insulin pump. Adv Mat Res. 2011;201:2399–2404. [Google Scholar]
- 167.Gupta J, Felner EI, Prausnitz MR. Minimally invasive insulin delivery in subjects with type 1 diabetes using hollow microneedles. Diabetes Technol The. 2009;11:329–337. doi: 10.1089/dia.2008.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Amirouche F, Zhou Y, Johnson T. Current micropump technologies and their biomedical applications. Microsyst Technol. 2009;15:647–666. [Google Scholar]
- 169.Matteucci M, Casella M, Bedoni M, Donetti E, Fanetti M, De Angelis F, Gramatica F, Di Fabrizio E. A compact and disposable transdermal drug delivery system. Microelectron Eng. 2008;85:1066–1073. [Google Scholar]
- 170.Wonglertnirant N, Todo H, Opanasopit P, Ngawhirunpat T, Sugibayashi K. Macromolecular delivery into skin using a hollow microneedle. Biol Pharm Bull. 2010;33:1988–1993. doi: 10.1248/bpb.33.1988. [DOI] [PubMed] [Google Scholar]
- 171.Harvey A, Kaestner S, Sutter D, Harvey N, Mikszta J, Pettis R. Microneedle-based intradermal delivery enables rapid lymphatic uptake and fistribution of protein drugs. Pharm Res. 2011;28:107–116. doi: 10.1007/s11095-010-0123-9. [DOI] [PubMed] [Google Scholar]
- 172.Kim K, Lee JB. High aspect ratio tapered hollow metallic microneedle arrays with microfluidic interconnector. Microsyst Technol. 2007;13:231–235. [Google Scholar]
- 173.Laurent PE, Bonnet S, Alchas P, Regolini P, Mikszta JA, Pettis R, Harvey NG. Evaluation of the clinical performance of a new intradermal vaccine administration technique and associated delivery system. Vaccine. 2007;25:8833–8842. doi: 10.1016/j.vaccine.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 174.Li T, Barnett A, Rogers KL, Gianchandani YB. A blood sampling microsystem for pharmacokinetic applications: Design, fabrication, and initial results. Lab Chip. 2009;9:3495–3503. doi: 10.1039/b910508e. [DOI] [PubMed] [Google Scholar]
- 175.Vesper HW, Wang PM, Archibold E, Prausnitz MR, Myers GL. Assessment of trueness of a glucose monitor using interstitial fluid and whole blood as specimen matrix. Diabetes Technol The. 2006;8:76–80. doi: 10.1089/dia.2006.8.76. [DOI] [PubMed] [Google Scholar]
- 176.Prausnitz MR, Langer R. Transdermal drug delivery. Nat Biotechnol. 2008;26:1261–1268. doi: 10.1038/nbt.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Choy YB, Prausnitz MR. The rule of five for non-oral routes of drug delivery: ophthalmic, inhalation and transdermal. Pharm Res. 2011;28:943–948. doi: 10.1007/s11095-010-0292-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Banks SL, Pinninti RR, Gill HS, Crooks PA, Prausnitz MR, Stinchcomb AL. Flux across of microneedle-treated skin is increased by increasing charge of naltrexone and naltrexol in vitro. Pharm Res. 2008;25:1677–1685. doi: 10.1007/s11095-008-9578-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Banks SL, Pinninti RR, Gill HS, Paudel KS, Crooks PA, Brogden NK, Prausnitz MR, Stinchcomb AL. Transdermal delivery of naltrexol and skin permeability lifetime after microneedle treatment in hairless guinea pigs. J Pharm Sci. 2010;99:3072–3080. doi: 10.1002/jps.22083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Wermeling DP, Banks SL, Huclson DA, Gill HS, Glupta J, Prausnitz MR, Stinchcom AL. Microneedles permit transdermal delivery of a skin-impermeant medication to humans. Proc Natl Acad Sci U S A. 2008;105:2058–2063. doi: 10.1073/pnas.0710355105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Yerramreddy TR, Milewski M, Penthala NR, Stinchcomb AL, Crooks PA. Novel 3-O-pegylated carboxylate and 3-O-pegylated carbamate prodrugs of naltrexone for microneedle-enhanced transdermal delivery. Bioorg Med Chem Lett. 2010;20:3280–3283. doi: 10.1016/j.bmcl.2010.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Banks S, Paudel K, Brogden N, Loftin C, Stinchcomb AL. Diclofenac enables prolonged delivery of naltrexone through microneedle-treated skin. Pharm Res. 2011;28:1211–1219. doi: 10.1007/s11095-011-0372-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Milewski M, Yerramreddy TR, Ghosh P, Crooks PA, Stinchcomb AL. In vitro permeation of a pegylated naltrexone prodrug across microneedle-treated skin. J Controlled Release. 2010;146:37–44. doi: 10.1016/j.jconrel.2010.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Milewski M, Stinchcomb AL. Vehicle composition influence on the microneedle-enhanced transdermal flux of naltrexone hydrochloride. Pharm Res. 2011;28:124–134. doi: 10.1007/s11095-010-0191-x. [DOI] [PubMed] [Google Scholar]
- 185.Donnelly RF, Morrow DIJ, McCarron PA, Woolfson AD, Morrissey A, Juzenas P, Juzeniene A, Iani V, McCarthy HO, Moan J. Microneedle-mediated intradermal delivery of 5-aminolevulinic acid: Potential for enhanced topical photodynamic therapy. Journal of Controlled Release. 2008;129:154–162. doi: 10.1016/j.jconrel.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 186.Mikolajewska P, Donnelly RF, Garland MJ, Morrow DIJ, Singh TRR, Iani V, Moan J, Juzeniene A. Microneedle pre-treatment of human skin improves 5-aminolevulininc acid (ALA)- and 5-aminolevulinic acid methyl ester (MAL)-induced PpIX production for topical photodynamic therapy without increase in pain or erythema. Pharm Res. 2010;27:2213–2220. doi: 10.1007/s11095-010-0227-2. [DOI] [PubMed] [Google Scholar]
- 187.Donnelly RF, Morrow DIJ, McCarron PA, David Woolfson A, Morrissey A, Juzenas P, Juzeniene A, Iani V, McCarthy HO, Moan J. Microneedle arrays permit enhanced intradermal delivery of a preformed photosensitizer. Photochem Photobiol. 2009;85:195–204. doi: 10.1111/j.1751-1097.2008.00417.x. [DOI] [PubMed] [Google Scholar]
- 188.Clementoni MT, Roscher MB, Munavalli GS. Photodynamic photorejuvenation of the face with a combination of microneedling, red light, and broadband pulsed light. Lasers Surg Med. 2010;42:150–159. doi: 10.1002/lsm.20905. [DOI] [PubMed] [Google Scholar]
- 189.Baek C, Han M, Min J, Prausnitz MR, Park J-H, Park JH. Local transdermal delivery of phenylephrine to the anal sphincter muscle using microneedles. J Controlled Release. 2011;154:138–147. doi: 10.1016/j.jconrel.2011.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Badran MM, Kuntsche J, Fahr A. Skin penetration enhancement by a microneedle device (Dermaroller (R)) in vitro: Dependency on needle size and applied formulation. Eur J Pharm Sci. 2009;36:511–523. doi: 10.1016/j.ejps.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 191.Kim YT, Il Ahn S, Park HJ, Jung SH, Hong HK, Lee HK, Lee D, Rhee JM, Lee KH, Khang G. Microneedle-mediated transdermal delivery of chondroitin sulfate. Tissue Eng Regen Med. 2009;6:756–761. [Google Scholar]
- 192.Li X, Zhao R, Qin Z, Zhang J, Zhai S, Qiu Y, Gao Y, Xu B, Thomas SH. Microneedle pretreatment improves efficacy of cutaneous topical anesthesia. Am J Emerg Med. 2010;28:130–134. doi: 10.1016/j.ajem.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 193.Gupta J, Denson DD, Felner EI, Prausnitz MR. Rapid local anesthesia in humans using minimally invasive microneedles. Clin J Pain. 2012;28:129–135. doi: 10.1097/AJP.0b013e318225dbe9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Sivamani RK, Stoeber B, Wu GC, Zhai HB, Liepmann D, Maibach H. Clinical microneedle injection of methyl nicotinate: stratum corneum penetration. Skin Res Technol. 2005;11:152–156. doi: 10.1111/j.1600-0846.2005.00107.x. [DOI] [PubMed] [Google Scholar]
- 195.Sivamani RK, Stoeber B, Liepmann D, Maibach HI. Microneedle penetration and injection past the stratum corneum in humans. J Dermatol Treat. 2009;20:156–159. doi: 10.1080/09546630802512679. [DOI] [PubMed] [Google Scholar]
- 196.Roxhed N, Samel B, Nordquist L, Griss P, Stemme G. Painless drug delivery through microneedle-based transdermal patches featuring active infusion. IEEE Trans Biomed Eng. 2008;55:1063–1071. doi: 10.1109/TBME.2007.906492. [DOI] [PubMed] [Google Scholar]
- 197.Nordquist L, Roxhed N, Griss P, Stemme G. Novel microneedle patches for active insulin delivery are efficient in maintaining glycaemic control: An initial comparison with subcutaneous administration. Pharm Res. 2007;24:1381–1388. doi: 10.1007/s11095-007-9256-x. [DOI] [PubMed] [Google Scholar]
- 198.Gupta J, Felner EI, Prausnitz MR. Rapid pharmacokinetics of intradermal insulin administered using microneedles in type 1 diabetes subjects. Diabetes TechnolThe. 2011;13:451–456. doi: 10.1089/dia.2010.0204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Pettis RJ, Ginsberg B, Hirsch L, Sutter D, Keith S, McVey E, Harvey NG, Hompesch M, Nosek L, Kapitza C, Heinemann L. Intradermal microneedle delivery of insulin lispro achieves faster insulin absorption and insulin action than subcutaneous injection. Diabetes TechnolThe. 2011;13:435–442. doi: 10.1089/dia.2010.0184. [DOI] [PubMed] [Google Scholar]
- 200.Pettis RJ, Hirsch L, Kapitza C, Nosek L, Hovelmann U, Kurth HJ, Sutter DE, Harvey NG, Heinemann L. Microneedle-based intradermal versus subcutaneous administration of regular human insulin or insulin lispro: pharmacokinetics and postprandial glycemic excursions in patients with type 1 diabetes. Diabetes TechnolThe. 2011;13:443–450. doi: 10.1089/dia.2010.0183. [DOI] [PubMed] [Google Scholar]
- 201.Lee JW, Choi SO, Felner EI, Prausnitz MR. Dissolving microneedle patch for transdermal delivery of human growth hormone. Small. 2011;7:531–539. doi: 10.1002/smll.201001091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Tas C, Mansoor S, Kalluri H, Zarnitsyn VG, Choi S-O, Banga AK, Prausnitz MR. Delivery of salmon calcitonin using a microneedle patch. Int J Pharm. 2012;423:257–263. doi: 10.1016/j.ijpharm.2011.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Ameri M, Daddona PE, Maa Y-F. Demonstrated solid-state stability of parathyroid hormone PTH(1-34) coated on a novel transdermal microprojection delivery system. Pharm Res. 2009;26:2454–2463. doi: 10.1007/s11095-009-9960-9. [DOI] [PubMed] [Google Scholar]
- 204.Ameri M, Wang X, Maa Y-F. Effect of irradiation on parathyroid hormone PTH(1-34) coated on a novel transdermal microprojection delivery system to produce a sterile product-adhesive compatibility. J Pharm Sci. 2010;99:2123–2134. doi: 10.1002/jps.21985. [DOI] [PubMed] [Google Scholar]
- 205.Cormier M, Daddona PE. Macroflux technology for transdermal delivery of therapeutic proteins and vaccines. In: Rathbone MJ, Hadgraft J, Roberts MS, editors. Modified-Release Drug Delivery Technology. Marcel Dekker; New York: 2003. [Google Scholar]
- 206.Cosman F, Lane NE, Bolognese MA, Zanchetta JR, Garcia-Hernandez PA, Sees K, Matriano JA, Gaumer K, Daddona PE. Effect of transdermal teriparatide administration on bone mineral density in postmenopausal women. J Clin Endocrinol Metab. 2010;95:151–158. doi: 10.1210/jc.2009-0358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Daddona P, Matriano J, Mandema J, Maa Y-F. Parathyroid hormone (1-34)-coated microneedle patch system: Clinical pharmacokinetics and pharmacodynamics for treatment of osteoporosis. Pharm Res. 2011;28:159–165. doi: 10.1007/s11095-010-0192-9. [DOI] [PubMed] [Google Scholar]
- 208.Pearton M, Allender C, Brain K, Anstey A, Gateley C, Wilke N, Morrissey A, Birchall J. Gene delivery to the epidermal cells of human skin explants using microfabricated microneedles and hydrogel formulations. Pharm Res. 2008;25:407–416. doi: 10.1007/s11095-007-9360-y. [DOI] [PubMed] [Google Scholar]
- 209.Gonzalez-Gonzalez E, Kim Y-C, Speaker TJ, Hickerson RP, Spitler R, Birchall JC, Lara MF, Hu R-h, Liang Y, Kirkiles-Smith N, Prausnitz MR, Milstone LM, Contag CH, Kaspar RL. Visualization of plasmid delivery to keratinocytes in mouse and human epidermis. Sci Rep. 2011;1:158. doi: 10.1038/srep00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Gonzalez-Gonzalez E, Speaker TJ, Hickerson RP, Spitler R, Flores MA, Leake D, Contag CH, Kaspar RL. Silencing of reporter gene expression in skin using siRNAs and … of plasmid DNA delivered by a soluble protrusion array device (PAD) Mol Ther. 2010;18:1667–1674. doi: 10.1038/mt.2010.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Kim YC, Prausnitz M. Enabling skin vaccination using new delivery technologies. Drug Deliv Trans Res. 2011;1:7–12. doi: 10.1007/s13346-010-0005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Mikszta JA, Laurent PE. Cutaneous delivery of prophylactic and therapeutic vaccines: historical perspective and future outlook. Expert RevVaccines. 2008;7:1329–1339. doi: 10.1586/14760584.7.9.1329. [DOI] [PubMed] [Google Scholar]
- 213.Ding Z, Van Riet E, Romeijn S, Kersten GFA, Jiskoot W, Bouwstra JA. Immune modulation by adjuvants combined with diphtheria toxoid administered topically in BALB/c mice after microneedle array pretreatment. Pharm Res. 2009;26:1635–1643. doi: 10.1007/s11095-009-9874-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Ding Z, Verbaan FJ, Bivas-Benita M, Bungener L, Huckriede A, van den Berg DJ, Kersten G, Bouwstra JA. Microneedle arrays for the transcutaneous immunization of diphtheria and influenza in BALB/c mice. J Controlled Release. 2009;136:71–78. doi: 10.1016/j.jconrel.2009.01.025. [DOI] [PubMed] [Google Scholar]
- 215.Ding Z, Van Riet E, Romeijn S, Kersten GFA, Jiskoot W, Bouwstra JA. Immune modulation by adjuvants combined with diphtheria toxoid administered topically in BALB/c mice after microneedle array pretreatment. Pharm Res. 2009;26:1635–1643. doi: 10.1007/s11095-009-9874-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Slutter B, Bal SM, Zhi D, Jiskoot W, Bouwstra JA. Adjuvant effect of cationic liposomes and CpG depends on administration route. J Control Release. 2011;154:123–130. doi: 10.1016/j.jconrel.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 217.Bal S, Ding Z, Kersten G, Jiskoot W, Bouwstra J. Microneedle-based transcutaneous immunisation in mice with N-trimethyl chitosan adjuvanted diphtheria toxoid formulations. Pharm Res. 2010;27:1837–1847. doi: 10.1007/s11095-010-0182-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Bal SM, Slütter B, Jiskoot W, Bouwstra JA. Small is beautiful: N-trimethyl chitosan-ovalbumin conjugates for microneedle-based transcutaneous immunisation. Vaccine. 2011;29:4025–4032. doi: 10.1016/j.vaccine.2011.03.039. [DOI] [PubMed] [Google Scholar]
- 219.Kumar A, Li XR, Sandoval MA, Rodriguez BL, Sloat BR, Cui ZR. Permeation of antigen protein-conjugated nanoparticles and live bacteria through microneedle-treated mouse skin. Int J Nanomed. 2011;6:1253–1264. doi: 10.2147/IJN.S20413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Mikszta JA, Alarcon JB, Brittingham JM, Sutter DE, Pettis RJ, Harvey NG. Improved genetic immunization via micromechanical disruption of skin-barrier function and targeted epidermal delivery. Nat Med. 2002;8:415–419. doi: 10.1038/nm0402-415. [DOI] [PubMed] [Google Scholar]
- 221.Mikszta JA, Sullivan VJ, Dean C, Waterston AM, Alarcon JB, Dekker JP, Brittingham JM, Huang J, Hwang CR, Ferriter M, Jiang G, Mar K, Saikh KU, Stiles BG, Roy CJ, Ulrich RG, Harvey NG. Protective immunization against inhalational anthrax: A comparison of minimally invasive delivery platforms. J Infect Dis. 2005;191:278–288. doi: 10.1086/426865. [DOI] [PubMed] [Google Scholar]
- 222.Dean C, Alarcon HJ, Waterston BA, Draper MK, Early R, Guirakhoo F, Monath T, Mikszta PJA. Cutaneous delivery of a live, attenuated chimeric flavivirus vaccine against Japanese encephalitis (ChimeriVax)-JE) in non-human primates. Human vaccines. 2005;1:106–111. doi: 10.4161/hv.1.3.1797. [DOI] [PubMed] [Google Scholar]
- 223.Laurent PE, Bourhy H, Fantino M, Alchas P, Mikszta JA. Safety and efficacy of novel dermal and epidermal microneedle delivery systems for rabies vaccination in healthy adults. Vaccine. 2010;28:5850–5856. doi: 10.1016/j.vaccine.2010.06.062. [DOI] [PubMed] [Google Scholar]
- 224.Widera G, Johnson J, Kim L, Libiran L, Nyam K, Daddona PE, Cormier M. Effect of delivery parameters on immunization to ovalbumin following intracutaneous administration by a coated microneedle array patch system. Vaccine. 2006;24:1653–1664. doi: 10.1016/j.vaccine.2005.09.049. [DOI] [PubMed] [Google Scholar]
- 225.Zhu QY, Zarnitsyn VG, Ye L, Wen ZY, Gao YL, Pan L, Skountzou I, Gill HS, Prausnitz MR, Yang CL, Compans RW. Immunization by vaccine-coated microneedle arrays protects against lethal influenza virus challenge. Proc Natl Acad Sci U S A. 2009;106:7968–7973. doi: 10.1073/pnas.0812652106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Koutsonanos DG, Martin MdP, Zarnitsyn VG, Sullivan SP, Compans RW, Prausnitz MR, Skountzou I. Transdermal influenza immunization with vaccine-coated microneedle arrays. PLoS ONE. 2009;4:e4773. doi: 10.1371/journal.pone.0004773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Quan FS, Kim YC, Yoo DG, Compans RW, Prausnitz MR, Kang SM. Stabilization of influenza vaccine enhances protection by microneedle delivery in the mouse skin. PLoS One. 2009;4:e7152. doi: 10.1371/journal.pone.0007152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Kim YC, Quan FS, Yoo DG, Compans RW, Kang SM, Prausnitz MR. Improved influenza vaccination in the skin using vaccine coated-microneedles. Vaccine. 2009;27:6932–6938. doi: 10.1016/j.vaccine.2009.08.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Kim YC, Quan FS, Yoo DG, Compans RW, Kang SM, Prausnitz MR. Enhanced memory responses to seasonal H1N1 influenza vaccination of the skin with the use of vaccine-coated microneedles. J Infect Dis. 2010;201:190–198. doi: 10.1086/649228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Koutsonanos DG, del Pilar Martin M, Zarnitsyn VG, Jacob J, Prausnitz MR, Compans RW, Skountzou I. Serological memory and long-term protection to novel H1N1 influenza virus after skin vaccination. J Infect Dis. 2011;204:582–91. doi: 10.1093/infdis/jir094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Kim YC, Quan FS, Song JM, Vunnava A, Yoo DG, Park KM, Compans RW, Kang SM, Prausnitz MR. Influenza immunization with trehalose-stabilized virus-like particle vaccine using microneedles. Proc Vaccinol. 2010;2:17–21. doi: 10.1016/j.provac.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Quan FS, Kim YC, Compans RW, Prausnitz MR, Kang SM. Dose sparing enabled by skin immunization with influenza virus-like particle vaccine using microneedles. J Control Release. 2010;147:326–332. doi: 10.1016/j.jconrel.2010.07.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Song JM, Kim YC, Barlow PG, Hossain MJ, Park KM, Donis RO, Prausnitz MR, Compans RW, Kang SM. Improved protection against avian influenza H5N1 virus by a single vaccination with virus-like particles in skin using microneedles. Antiviral Res. 2010;88:244–247. doi: 10.1016/j.antiviral.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Song JM, Kim YC, Lipatov AS, Pearton M, Davis CT, Yoo DG, Park KM, Chen LM, Quan FS, Birchall JC, Donis RO, Prausnitz MR, Compans RW, Kang SM. Microneedle delivery of H5N1 influenza virus-like particles to the skin induces long-lasting B- and T-cell responses in mice. Clin Vaccine Immunol. 2010;17:1381–1389. doi: 10.1128/CVI.00100-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Ng KW, Pearton M, Coulman S, Anstey A, Gateley C, Morrissey A, Allender C, Birchall J. Development of an ex vivo human skin model for intradermal vaccination: Tissue viability and Langerhans cell behaviour. Vaccine. 2009;27:5948–5955. doi: 10.1016/j.vaccine.2009.07.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Pearton M, Kang SM, Song JM, Kim YC, Quan FS, Anstey A, Ivory M, Prausnitz MR, Compans RW, Birchall JC. Influenza virus-like particles coated onto microneedles can elicit stimulatory effects on Langerhans cells in human skin. Vaccine. 2010;28:6104–6113. doi: 10.1016/j.vaccine.2010.05.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Fernando GJP, Chen XF, Prow TW, Crichton ML, Fairmaid EJ, Roberts MS, Frazer IH, Brown LE, Kendall MAF. Potent immunity to low doses of influenza vaccine by probabilistic guided micro-targeted skin delivery in a mouse model. PLoS One. 2010;5:e10266. doi: 10.1371/journal.pone.0010266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Chen XF, Corbett HJ, Yukiko SR, Raphael AP, Fairmaid EJ, Prow TW, Brown LE, Fernando GJP, Kendall MAF. Site-selectively coated densely-packed microprojection array patches for targeted delivery of vaccines to skin. Adv Funct Mater. 2011;21:464–473. [Google Scholar]
- 239.Andrianov AK, DeCollibus DP, Gillis HA, Kha HH, Marin A, Prausnitz MR, Babiuk LA, Townsend H, Mutwiri G. Poly [di(carboxylatophenoxy)phosphazene] is a potent adjuvant for intradermal immunization. Proc Natl Acad Sci USA. 2009;106:18936–18941. doi: 10.1073/pnas.0908842106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Kask AS, Chen X, Marshak JO, Dong L, Saracino M, Chen D, Jarrahian C, Kendall MA, Koelle DM. DNA vaccine delivery by densely-packed and short microprojection arrays to skin protects against vaginal HSV-2 challenge. Vaccine. 2010;28:7483–7491. doi: 10.1016/j.vaccine.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 241.Kommareddy S, Baudner BC, Oh S, Kwon S-y, Singh M, O’Hagan DT. Dissolvable microneedle patches for the delivery of cell-culture-derived influenza vaccine antigens. J Pharm Sci. 2012;101:1021–1027. doi: 10.1002/jps.23019. [DOI] [PubMed] [Google Scholar]
- 242.Hirschberg HJHB, de Wijdeven GGPV, Kelder AB, van den Dobbelsteen GPJM, Kerstena GFA. Bioneedles (TM) as vaccine carriers. Vaccine. 2008;26:2389–2397. doi: 10.1016/j.vaccine.2008.02.067. [DOI] [PubMed] [Google Scholar]
- 243.Hirschberg H, de Wijdeven G, Kraan H, Amorij JP, Kersten GFA. Bioneedles as alternative delivery system for hepatitis B vaccine. J Controlled Release. 2010;147:211–217. doi: 10.1016/j.jconrel.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 244.Flynn PM, Shenep JL, Mao L, Crawford R, Williams BF, Williams BG. Influence of needle gauge in Mantoux skin testing. Chest. 1994;106:1463–1465. doi: 10.1378/chest.106.5.1463. [DOI] [PubMed] [Google Scholar]
- 245.Alarcon JB, Hartley AW, Harvey NG, Mikszta JA. Preclinical evaluation of microneedle technology for intradermal delivery of influenza vaccines. ClinVaccine Immunol. 2007;14:375–381. doi: 10.1128/CVI.00387-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Mikszta JA, Dekker JP, Harvey NG, Dean CH, Brittingham JM, Huang J, Sullivan VJ, Dyas B, Roy CJ, Ulrich RG. Microneedle-based intradermal delivery of the anthrax recombinant protective antigen vaccine. Infect Immun. 2006;74:6806–6810. doi: 10.1128/IAI.01210-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Huang J, D’Souza AJ, Alarcon JB, Mikszta JA, Ford BM, Ferriter MS, Evans M, Stewart T, Amemiya K, Ulrich RG, Sullivan VJ. Protective immunity in mice achieved with dry powder formulation and alternative delivery of plague F1-V vaccine. ClinVaccine Immunol. 2009;16:719–725. doi: 10.1128/CVI.00447-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Morefield GL, Tammariello RF, Purcell BK, Worsham PL, Chapman J, Smith LA, Alarcon JB, Mikszta JA, Ulrich RG. An alternative approach to combination vaccines: intradermal administration of isolated components for control of anthrax, botulism, plague and staphylococcal toxic shock. J Immune Based Ther Vaccines. 2008;6:5. doi: 10.1186/1476-8518-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Belshe RB. Current status of live attenuated influenza virus vaccine in the US. Virus Res. 2004;103:177–185. doi: 10.1016/j.virusres.2004.02.031. [DOI] [PubMed] [Google Scholar]
- 250.Beran J, Ambrozaitis A, Laiskonis A, Mickuviene N, Bacart P, Calozet Y, Demanet E, Heijmans S, Van Belle P, Weber F, Salamand C. Intradermal influenza vaccination of healthy adults using a new microinjection system: a 3-year randomised controlled safety and immunogenicity trial. BMC Medicine. 2009;7:13. doi: 10.1186/1741-7015-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Leroux-Roels I, Vets E, Freese R, Seiberling M, Weber F, Salamand C, Leroux-Roels G. Seasonal influenza vaccine delivered by intradermal microinjection: A randomised controlled safety and immunogenicity trial in adults. Vaccine. 2008;26:6614–6619. doi: 10.1016/j.vaccine.2008.09.078. [DOI] [PubMed] [Google Scholar]
- 252.Holland D, Booy R, De Looze F, Eizenberg P, McDonald J, Karrasch J, McKeirnan M, Salem H, Mills G, Reid J, Weber F, Saville M. Intradermal influenza vaccine administered using a new microinjection system produces superior immunogenicity in elderly adults: A randomized controlled trial. J Infect Dis. 2008;198:650–658. doi: 10.1086/590434. [DOI] [PubMed] [Google Scholar]
- 253.Arnou R, Icardi G, De Decker M, Ambrozaitis A, Kazek MP, Weber F, Van Damme P. Intradermal influenza vaccine for older adults: A randomized controlled multicenter phase III study. Vaccine. 2009;27:7304–7312. doi: 10.1016/j.vaccine.2009.10.033. [DOI] [PubMed] [Google Scholar]
- 254.Van Damme P, Oosterhuis-Kafeja F, Van der Wielen M, Almagor Y, Sharon O, Levin Y. Safety and efficacy of a novel microneedle device for dose sparing intradermal influenza vaccination in healthy adults. Vaccine. 2009;27:454–459. doi: 10.1016/j.vaccine.2008.10.077. [DOI] [PubMed] [Google Scholar]
- 255.Wang PM, Cornwell M, Prausnitz MR. Minimally invasive extraction of dermal interstitial fluid for glucose monitoring using microneedles. Diabetes Technology & Therapeutics. 2005;7:131–141. doi: 10.1089/dia.2005.7.131. [DOI] [PubMed] [Google Scholar]
- 256.Zahn JD, Trebotich D, Liepmann D. Microdialysis microneedles for continuous medical monitoring. Biomed Microdevices. 2005;7:59–69. doi: 10.1007/s10544-005-6173-9. [DOI] [PubMed] [Google Scholar]
- 257.Gattiker GE, Kaler K, Mintchev MP. Electronic Mosquito: designing a semi-invasive Microsystem for blood sampling, analysis and drug delivery applications. Microsyst Technol. 2005;12:44–51. [Google Scholar]
- 258.Smart WH, Subramanian K. The use of silicon microfabrication technology in painless blood glucose monitoring. Diabetes Technol The. 2000;2:549–559. doi: 10.1089/15209150050501961. [DOI] [PubMed] [Google Scholar]
- 259.Corrie SR, Fernando GJP, Crichton ML, Brunck MEG, Anderson CD, Kendall MAF. Surface-modified microprojection arrays for intradermal biomarker capture with low non-specific protein binding. Lab Chip. 2010;10:2655–2658. doi: 10.1039/c0lc00068j. [DOI] [PubMed] [Google Scholar]
- 260.Windmiller JR, Zhou ND, Chuang MC, Valdes-Ramirez G, Santhosh P, Miller PR, Narayan R, Wang J. Microneedle array-based carbon paste amperometric sensors and biosensors. Analyst. 2011;136:1846–1851. doi: 10.1039/c1an00012h. [DOI] [PubMed] [Google Scholar]
- 261.Lee J-H, Seo Y, Lim T-S, Bishop PL, Papautsky I. MEMS needle-type sensor array for in situ measurements of dissolved oxygen and redox potential. Environ Sci Technol. 2007;41:7857–7863. doi: 10.1021/es070969o. [DOI] [PubMed] [Google Scholar]
- 262.Wassum KM, Tolosa VM, Wang J, Walker E, Monbouquette HG, Maidment NT. Silicon wafer-based platinum microelectrode array biosensor for near real-time measurement of glutamate in vivo. Sensors. 2008;8:5023–5036. doi: 10.3390/s8085023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Bai Q, Wise KD, Anderson DJ. A high-yield microassembly structure for three-dimensional microelectrode arrays. IEEE Trans Biomed Eng. 2000;47:281–289. doi: 10.1109/10.827288. [DOI] [PubMed] [Google Scholar]
- 264.Chen C-H, Yao D-J, Tseng S-H, Lu S-W, Chiao C-C, Yeh S-R. Micro-multi-probe electrode array to measure neural signals. Biosens Bioelectron. 2009;24:1911–1917. doi: 10.1016/j.bios.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 265.Hoogerwerf AC, Wise KD. A three-dimensional microelectrode array for chronic neural recording. IEEE Trans Biomed Eng. 1994;41:1136–1146. doi: 10.1109/10.335862. [DOI] [PubMed] [Google Scholar]
- 266.Normann RA, Maynard EM, Rousche PJ, Warren DJ. A neural interface for a cortical vision prosthesis. Vision Res. 1999;39:2577–2587. doi: 10.1016/s0042-6989(99)00040-1. [DOI] [PubMed] [Google Scholar]
- 267.Rajaraman S, Bragg JA, Ross JD, Allen MG. Micromachined three-dimensional electrode arrays for transcutaneous nerve tracking. J Micromech Microeng. 2011;21:085014. [Google Scholar]
- 268.Rajaraman S, Choi S-O, McClain MA, Ross JD, LaPlaca MC, Allen MG. Metal-Transfer-Micromolded Three-Dimensional Microelectrode Arrays for in-vitro Brain-Slice Recordings. J Microelectromech S. 2011;20:396–409. [Google Scholar]
- 269.Rousche PJ, Pellinen DS, Pivin DP, Williams JC, Vetter RJ, Kipke DR. Flexible polyimide-based intracortical electrode arrays with bioactive capability. IEEE Trans Biomed Eng. 2001;48:361–371. doi: 10.1109/10.914800. [DOI] [PubMed] [Google Scholar]
- 270.Vetter RJ, Williams JC, Hetke JF, Nunamaker EA, Kipke DR. Chronic neural recording using silicon-substrate microelectrode arrays implanted in cerebral cortex. IEEE Trans Biomed Eng. 2004;51:896–904. doi: 10.1109/TBME.2004.826680. [DOI] [PubMed] [Google Scholar]
- 271.Wise KD, Sodagar AM, Yao Y, Gulari MN, Perlin GE, Najafi K. Microelectrodes, microelectronics, and implantable neural microsystems. Proc, IEEE. 2008;96:1184–1202. [Google Scholar]
- 272.Griss P, Tolvanen-Laakso HK, Merilainen P, Stemme G. Characterization of micromachined spiked biopotential electrodes. IEEE Trans Biomed Eng. 2002;49:597–604. doi: 10.1109/TBME.2002.1001974. [DOI] [PubMed] [Google Scholar]
- 273.Wu XM, Todo H, Sugibayashi K. Enhancement of skin permeation of high molecular compounds by a combination of microneedle pretreatment and iontophoresis. J Controlled Release. 2007;118:189–195. doi: 10.1016/j.jconrel.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 274.Katikaneni S, Badkar A, Nema S, Banga AK. Molecular charge mediated transport of a 13 kD protein across microporated skin. Int J Pharm. 2009;378:93–100. doi: 10.1016/j.ijpharm.2009.05.050. [DOI] [PubMed] [Google Scholar]
- 275.Katikaneni S, Li GH, Badkar A, Banga AK. Transdermal delivery of a similar to 13 kDa protein-an in vivo comparison of physical enhancement methods. J Drug Target. 2010;18:141–147. doi: 10.3109/10611860903287164. [DOI] [PubMed] [Google Scholar]
- 276.Chen HB, Zhu HD, Zheng JN, Mou DS, Wan JL, Zhang JY, Shi TL, Zhao YJ, Xu HB, Yang XL. Iontophoresis-driven penetration of nanovesicles through microneedle-induced skin microchannels for enhancing transdermal delivery of insulin. J Controlled Release. 2009;139:63–72. doi: 10.1016/j.jconrel.2009.05.031. [DOI] [PubMed] [Google Scholar]
- 277.Wilson JR, Kehl LJ, Beiraghi S. Enhanced topical anesthesia of 4% lidocaine with microneedle pretreatment and iontophoresis. Northwest Dent. 2008;87:40–41. [PubMed] [Google Scholar]
- 278.Yan K, Todo H, Sugibayashi K. Transdermal drug delivery by in-skin electroporation using a microneedle array. Int J Pharm. 2010;397:77–83. doi: 10.1016/j.ijpharm.2010.06.052. [DOI] [PubMed] [Google Scholar]
- 279.Choi SO, Kim YC, Lee JW, Park JH, Prausnitz MR, Allen MG. Intracellular protein delivery and gene transfection by electroporation using a microneedle electrode array. Small. 2012 doi: 10.1002/smll.201101747. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Lee K, Kim JD, Lee CY, Her S, Jung H. A high-capacity, hybrid electro-microneedle for in-situ cutaneous gene transfer. Biomaterials. 2011;32:7705–7710. doi: 10.1016/j.biomaterials.2011.06.058. [DOI] [PubMed] [Google Scholar]
- 281.Hooper JW, Golden JW, Ferro AM, King AD. Smallpox DNA vaccine delivered by novel skin electroporation device protects mice against intranasal poxvirus challenge. Vaccine. 2007;25:1814–1823. doi: 10.1016/j.vaccine.2006.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Brave A, Gudmundsdotter L, Sandstrom E, Haller BK, Hallengard D, Maltais A-K, King AD, Stout RR, Blomberg P, Hoglund U, Hejdeman B, Biberfeld G, Wahren B. Biodistribution persistence and lack of integration of a multigene HIV vaccine delivered by needle-free intradermal injection and electroporation. Vaccine. 2010;28:8203–8209. doi: 10.1016/j.vaccine.2010.08.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Roos A-K, Eriksson F, Walters DC, Pisa P, King AD. Optimization of skin electroporation in mice to increase tolerability of DNA vaccine delivery to patients. Mol Ther. 2009;17:1637–1642. doi: 10.1038/mt.2009.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Jiang J, Moore JS, Edelhauser HF, Prausnitz MR. Intrascleral drug delivery to the eye using hollow microneedles. Pharm Res. 2009;26:395–403. doi: 10.1007/s11095-008-9756-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Patel SR, Lin ASP, Edelhauser HF, Prausnitz MR. Suprachoroidal drug delivery to the back of the eye using hollow microneedles. Pharm Res. 2011;28:166–176. doi: 10.1007/s11095-010-0271-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Palakurthi NK, Correa ZM, Augsburger JJ, Banerjee RK. Toxicity of a biodegradable microneedle implant loaded with methotrexate as a sustained release device in normal rabbit eye: a pilot study. J Ocul Pharmacol Ther. 2011;27:151–156. doi: 10.1089/jop.2010.0037. [DOI] [PubMed] [Google Scholar]
- 287.Navarro J, Risco R, Toschi M, Schattman G. Gene therapy and intracytoplasmatic sperm injection (ICSI) - a review. Placenta. 2008;29:193–199. doi: 10.1016/j.placenta.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 288.Zhang Y, Yu LC. Single-cell microinjection technology in cell biology. Bioessays. 2008;30:606–610. doi: 10.1002/bies.20759. [DOI] [PubMed] [Google Scholar]
- 289.Niemann H, Kues WA. Transgenic farm animals: an update. Reprod Fertil Dev. 2007;19:762–770. doi: 10.1071/rd07040. [DOI] [PubMed] [Google Scholar]
- 290.Obataya I, Nakamura C, Han S, Nakamura N, Miyake J. Nanoscale operation of a living cell using an atomic force microscope with a nanoneedle. Nano Lett. 2005;5:27–30. doi: 10.1021/nl0485399. [DOI] [PubMed] [Google Scholar]
- 291.Obataya F, Nakamura C, Han SW, Nakamura N, Miyake J. Mechanical sensing of the penetration of various nanoneedles into a living cell using atomic force microscopy. Biosens Bioelectron. 2005;20:1652–1655. doi: 10.1016/j.bios.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 292.Han SW, Nakamura C, Obataya I, Nakamura N, Miyake J. Gene expression using an ultrathin needle enabling accurate displacement and low invasiveness. Biochem Biophys Res Commun. 2005;332:633–639. doi: 10.1016/j.bbrc.2005.04.059. [DOI] [PubMed] [Google Scholar]
- 293.Han SW, Nakamura C, Obataya I, Nakamura N, Miyake J. A molecular delivery system by using AFM and nanoneedle. Biosens Bioelectron. 2005;20:2120–2125. doi: 10.1016/j.bios.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 294.Han SW, Nakamura C, Kotobuki N, Obataya I, Ohgushi H, Nagamune T, Miyake J. High-efficiency DNA injection into a single human mesenchymal stem cell using a nanoneedle and atomic force microscopy. Nanomed-Nanotechnol Biol Med. 2008;4:215–225. doi: 10.1016/j.nano.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 295.Han SW, Nakamura C, Imai Y, Nakamura N, Miyake J. Monitoring of hormonal drug effect in a single breast cancer cell using an estrogen responsive GFP reporter vector delivered by a nanoneedle. Biosens Bioelectron. 2009;24:1219–1222. doi: 10.1016/j.bios.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 296.Kihara T, Yoshida N, Kitagawa T, Nakamura C, Nakamura N, Miyake J. Development of a novel method to detect intrinsic mRNA in a living cell by using a molecular beacon-immobilized nanoneedle. Biosens Bioelectron. 2010;26:1449–1454. doi: 10.1016/j.bios.2010.07.079. [DOI] [PubMed] [Google Scholar]
- 297.Han SW, Mieda S, Nakamura C, Kihara T, Nakamura N, Miyake J. Successive detection of insulin-like growth factor-II bound to receptors on a living cell surface using an AFM. J Mol Recognit. 2011;24:17–22. doi: 10.1002/jmr.994. [DOI] [PubMed] [Google Scholar]
- 298.Chen X, Kis A, Zettl A, Bertozzi CR. A cell nanoinjector based on carbon nanotubes. Proc Natl Acad Sci U S A. 2007;104:8218–8222. doi: 10.1073/pnas.0700567104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Yum K, Na S, Xiang Y, Wang N, Yu MF. Mechanochemical delivery and dynamic tracking of fluorescent quantum dots in the cytoplasm and nucleus of living cells. Nano Lett. 2009;9:2193–2198. doi: 10.1021/nl901047u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Singhal R, Orynbayeva Z, Sundaram RVK, Niu JJ, Bhattacharyya S, Vitol EA, Schrlau MG, Papazoglou ES, Friedman G, Gogotsi Y. Multifunctional carbon-nanotube cellular endoscopes. Nat Nanotechnol. 2011;6:57–64. doi: 10.1038/nnano.2010.241. [DOI] [PubMed] [Google Scholar]
- 301.Hashmi S, Ling P, Hashmi G, Reed M, Gaugler R, Trimmer W. Genetic transformation of nematodes using arrays of micromechanical piercing structures. Biotechniques. 1995;19:766. [PubMed] [Google Scholar]
- 302.Chun K, Hashiguchi G, Toshiyoshi H, Fujita H. Fabrication of array of hollow microcapillaries used for injection of genetic materials into animal/plant cells. Jpn J Appl Phys Part 2Lett. 1999;38:279–281. [Google Scholar]
- 303.Kolhar P, Doshi N, Mitragotri S. Polymer nanoneedle-mediated intracellular drug delivery. Small. 2011;7:2094–2100. doi: 10.1002/smll.201100497. [DOI] [PubMed] [Google Scholar]
- 304.Reed ML, Wu C, Kneller J, Watkins S, Vorp DA, Nadeem A, Weiss LE, Rebello K, Mescher M, Smith AJC, Rosenblum W, Feldman MD. Micromechanical devices for intravascular drug delivery. J Pharm Sci. 1998;87:1387–1394. doi: 10.1021/js980085q. [DOI] [PubMed] [Google Scholar]
- 305.Choi Y, McClain MA, LaPlaca MC, Frazier AB, Allen MG. Three dimensional MEMS microfluidic perfusion system for thick brain slice cultures. Biomed Microdevices. 2007;9:7–13. doi: 10.1007/s10544-006-9004-8. [DOI] [PubMed] [Google Scholar]
- 306.Harper JC, Brozik SM, Flemming JH, McClain JL, Polsky R, Raj D, Ten Eyck GA, Wheeler DR, Achyuthan KE. Fabrication and testing of a microneedles sensor array for p-cresol detection with potential biofuel applications. ACS Appl Mater Interfaces. 2009;1:1591–1598. doi: 10.1021/am900259u. [DOI] [PubMed] [Google Scholar]
- 307.Martanto W, Moore JS, Couse T, Prausnitz MR. Mechanism of fluid infusion during microneedle insertion and retraction. J Controlled Release. 2006;112:357–361. doi: 10.1016/j.jconrel.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 308.Kendall MAF, Chong YF, Cock A. The mechanical properties of the skin epidermis in relation to targeted gene and drug delivery. Biomaterials. 2007;28:4968–4977. doi: 10.1016/j.biomaterials.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 309.Khanna P, Luongo K, Strom JA, Bhansali S. Sharpening of hollow silicon microneedles to reduce skin penetration force. J Micromech Microeng. 2010;20:045011. [Google Scholar]
- 310.Crichton ML, Donose BC, Chen XF, Raphael AP, Huang H, Kendall MAF. The viscoelastic, hyperelastic and scale dependent behaviour of freshly excised individual skin layers. Biomaterials. 2011;32:4670–4681. doi: 10.1016/j.biomaterials.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 311.Groves RB, Coulman SA, Birchall JC, Evans SL. Quantifying the mechanical properties of human skin to optimise future microneedle device design. Comput Methods Biomech Biomed Eng. 2012;15:73–82. doi: 10.1080/10255842.2011.596481. [DOI] [PubMed] [Google Scholar]
- 312.You SK, Noh YW, Park HH, Han M, Lee SS, Shin SC, Cho CW. Effect of applying modes of the polymer microneedle-roller on the permeation of L-ascorbic acid in rats. J Drug Target. 2010;18:15–20. doi: 10.3109/10611860903115274. [DOI] [PubMed] [Google Scholar]
- 313.Wang Q, Jaimes-Lizcano YA, Lawson LB, John VT, Papadopoulos KD. Improved dermal delivery of FITC–BSA using a combination of passive and active methods. J Pharm Sci. 2011;100:4804–4814. doi: 10.1002/jps.22687. [DOI] [PubMed] [Google Scholar]
- 314.Kalluri H, Kolli CS, Banga AK. Characterization of microchannels created by metal microneedles: Formation and closure. AAPS J. 2011;13:473–481. doi: 10.1208/s12248-011-9288-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Yang M, Zahn JD. Microneedle insertion force reduction using vibratory actuation. Biomed Microdevices. 2004;6:177–182. doi: 10.1023/B:BMMD.0000042046.07678.2e. [DOI] [PubMed] [Google Scholar]
- 316.Sun L, Wang H, Chen L, Liu Y. A novel ultrasonic micro-dissection, technique for biomedicine. Ultrasonics. 2006;44:e255–e260. doi: 10.1016/j.ultras.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 317.Verbaan FJ, Bal SM, van den Berg DJ, Dijksman JA, van Hecke M, Verpoorten H, van den Berg A, Luttge R, Bouwstra JA. Improved piercing of microneedle arrays in dermatomed human skin by an impact insertion method. J Controlled Release. 2008;128:80–88. doi: 10.1016/j.jconrel.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 318.Crichton ML, Ansaldo A, Chen XF, Prow TW, Fernando GJP, Kendall MAF. The effect of strain rate on the precision of penetration of short densely-packed microprojection array patches coated with vaccine. Biomaterials. 2010;31:4562–4572. doi: 10.1016/j.biomaterials.2010.02.022. [DOI] [PubMed] [Google Scholar]
- 319.Enfield J, O’Connell ML, Lawlor K, Jonathan E, O’Mahony C, Leahy M. In-vivo dynamic characterization of microneedle skin penetration using optical coherence tomography. J Biomed Opt. 2010;15 doi: 10.1117/1.3463002. [DOI] [PubMed] [Google Scholar]
- 320.Coulman SA, Birchall JC, Alex A, Pearton M, Hofer B, O’Mahony C, Drexler W, Povazay B. In Vivo, In Situ Imaging of Microneedle Insertion into the Skin of Human Volunteers Using Optical Coherence Tomography. Pharm Res. 2011;28:66–81. doi: 10.1007/s11095-010-0167-x. [DOI] [PubMed] [Google Scholar]
- 321.Donnelly RF, Garland MJ, Morrow DIJ, Migalska K, Singh TRR, Majithiya R, Woolfson AD. Optical coherence tomography is a valuable tool in the study of the effects of microneedle geometry on skin penetration characteristics and in-skin dissolution. J Controlled Release. 2010;147:333–341. doi: 10.1016/j.jconrel.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 322.Davis SP, Landis BJ, Adams ZH, Allen MG, Prausnitz MR. Insertion of microneedles into skin: measurement and prediction of insertion force and needle fracture force. J Biomech. 2004;37:1155–1163. doi: 10.1016/j.jbiomech.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 323.Park JH, Prausnitz MR. Analysis of mechanical failure of polymer microneedles by axial force. J Korean Phys Soc. 2010;56:1223–1227. doi: 10.3938/jkps.56.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Takano N, Tachikawa H, Miyano T, Nishiyabu K. Insertion testing of polyethylene glycol microneedle array into cultured human skin with biaxial tension. J Solid Mech Mat Eng. 2009;3:604–612. [Google Scholar]
- 325.Tachikawa H, Takano N, Nishiyabu K, Miki N, Ami Y. Effect of tension and curvature of skin on insertion characteristics of microneedle array. J Solid Mech Mat Eng. 2010;4:470–480. [Google Scholar]
- 326.Aggarwal P, Johnston CR. Geometrical effects in mechanical characterizing of microneedle for biomedical applications. Sens Actuat B Chem. 2004;102:226–234. [Google Scholar]
- 327.Kong XQ, Zhou P, Wu CW. Numerical simulation of microneedles’ insertion into skin. Comput Methods Biomech Biomed Eng. 2011;14:827–835. doi: 10.1080/10255842.2010.497144. [DOI] [PubMed] [Google Scholar]
- 328.Martanto W, Baisch SM, Costner EA, Prausnitz MR, Smith MK. Fluid dynamics in conically tapered microneedles. AICHE J. 2005;51:1599–1607. [Google Scholar]
- 329.Gupta J, Park SS, Bondy B, Felner EI, Prausnitz MR. Infusion pressure and pain during microneedle injection into skin of human subjects. Biomaterials. 2011;32:6823–6831. doi: 10.1016/j.biomaterials.2011.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Gupta J, Gill HS, Andrews SN, Prausnitz MR. Kinetics of skin resealing after insertion of microneedles in human subjects. J Control Release. 2011;154:148–155. doi: 10.1016/j.jconrel.2011.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Kim YC, Quan FS, Compans RW, Kang SM, Prausnitz MR. Stability kinetics of influenza vaccine coated onto microneedles during drying and storage. Pharm Res. 2011;28:135–144. doi: 10.1007/s11095-010-0134-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Chen X, Fernando GJP, Crichton ML, Flaim C, Yukiko SR, Fairmaid EJ, Corbett HJ, Primiero CA, Ansaldo AB, Frazer IH, Brown LE, Kendall MAF. Improving the reach of vaccines to low-resource regions, with a needle-free vaccine delivery device and long-term thermostabilization. J Controlled Release. 2011;152:349–355. doi: 10.1016/j.jconrel.2011.02.026. [DOI] [PubMed] [Google Scholar]
- 333.Choi H-J, Yoo D-G, Bondy BJ, Quan F-S, Compans RW, Kang S-M, Prausnitz MR. Stability of influenza vaccine coated onto microneedles. Biomaterials. 2012;33:3756–3769. doi: 10.1016/j.biomaterials.2012.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Birchall JC, Clemo R, Anstey A, John DN. Microneedles in clinical practice - An exploratory study into the opinions of healthcare professionals and the public. Pharm Res. 2011;28:95–106. doi: 10.1007/s11095-010-0101-2. [DOI] [PubMed] [Google Scholar]
- 335.Arnou R, Frank M, Hagel T, Prébet A. Willingness to vaccinate/get vaccinated with an intradermal seasonal influenza vaccine: a survey of general practitioners and the general public in France and Germany. Adv Ther. 2011;28:555–565. doi: 10.1007/s12325-011-0035-z. [DOI] [PubMed] [Google Scholar]
- 336.Kaushik S, Hord AH, Denson DD, McAllister DV, Smitra S, Allen MG, Prausnitz MR. Lack of pain associated with microfabricated microneedles. Anesth Analg. 2001;92:502–504. doi: 10.1097/00000539-200102000-00041. [DOI] [PubMed] [Google Scholar]
- 337.Gill HS, Denson DD, Burris BA, Prausnitz MR. Effect of microneedle design on pain in human volunteers. Clin J Pain. 2008;24:585–594. doi: 10.1097/AJP.0b013e31816778f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Bal SM, Caussin J, Pavel S, Bouwstra JA. In vivo assessment of safety of microneedle arrays in human skin. Eur J Pharm Sci. 2008;35:193–202. doi: 10.1016/j.ejps.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 339.Haq MI, Smith E, John DN, Kalavala M, Edwards C, Anstey A, Morrissey A, Birchall JC. Clinical administration of microneedles: skin puncture, pain and sensation. Biomed Microdevices. 2009;11:35–47. doi: 10.1007/s10544-008-9208-1. [DOI] [PubMed] [Google Scholar]
- 340.Noh Y-W, Kim T-H, Baek J-S, Park H-H, Lee SS, Han M, Shin S-C, Cho C-W. In vitro characterization of the invasiveness of polymer microneedle against skin. Int J Pharm. 2010;397:201–205. doi: 10.1016/j.ijpharm.2010.06.050. [DOI] [PubMed] [Google Scholar]
- 341.Hutin Y, Hauri A, Chiarello L, Catlin M, Stilwell B, Ghebrehiwet T, Garner J B. Members Injection Safety. Best infection control practices for intradermal, subcutaneous, and intramuscular needle injections. Bull WHO. 2003;81:491–500. [PMC free article] [PubMed] [Google Scholar]
- 342.Kupper TS, Fuhlbrigge RC. Immune surveillance in the skin: mechanisms and clinical consequences. Nat Rev Immunol. 2004;4:211–222. doi: 10.1038/nri1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Donnelly RF, Singh TRR, Tunney MM, Morrow DIJ, McCarron PA, O’Mahony C, Woolfson AD. Microneedle arrays allow lower microbial penetration than hypodermic needles in vitro. Pharm Res. 2009;26:2513–2522. doi: 10.1007/s11095-009-9967-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Zahn JD, Talbot NH, Liepmann D, Pisano AP. Microfabricated polysilicon microneedles for minimally invasive biomedical devices. Biomed Microdevices. 2000;2:295–303. [Google Scholar]
- 345.Lin LW, Pisano AP. Silicon-processed microneedles. J Microelectromech S. 1999;8:78–84. [Google Scholar]
- 346.Brazzle J, Papautsky I, Frazier AB. Micromachined needle arrays for drug delivery or fluid extraction - Design and fabrication aspects of fluid coupled arrays of hollow metallic microneedles. IEEE Eng Med Biol Mag. 1999;18:53–58. doi: 10.1109/51.805145. [DOI] [PubMed] [Google Scholar]
- 347.Belshe RB, Newman FK, Cannon J, Duane C, Treanor J, Van Hoecke C, Howe BJ, Dubin G. Serum antibody responses after intradermal vaccination against influenza. N Engl J Med. 2004;351:2286–2294. doi: 10.1056/NEJMoa043555. [DOI] [PubMed] [Google Scholar]
- 348.Ansaldi F, Durando P, Icardi G. Intradermal influenza vaccine and new devices: a promising chance for vaccine improvement. Expert Opin Biol Ther. 2011;11:415–427. doi: 10.1517/14712598.2011.557658. [DOI] [PubMed] [Google Scholar]
- 349.Gupta SK, Bernstein KJ, Noorduin H, Van Peer A, Sathyan G, Haak R. Fentanyl delivery from an electrotransport system: Delivery is a function of total current, not duration of current. J Clin Pharmacol. 1998;38:951–958. doi: 10.1002/j.1552-4604.1998.tb04392.x. [DOI] [PubMed] [Google Scholar]