Abstract
Drug users are marginalized from typical primary care, often resulting in emergency department (ED) usage and hospitalization due to late-stage disease. Though data suggest methadone decreases such fragmented healthcare utilization (HCU), the impact of buprenorphine maintenance treatment (BMT) on HCU is unknown. Chart review was conducted on opioid dependent patients seeking BMT, comparing individuals (N=59) who left BMT ≤ 3 days with those retained on BMT (N=150), for ED use and hospitalization. Using negative binomial regressions, including comparison of time before BMT induction, ED utilization and hospitalization was assessed. Overall, ED utilization was 0.93 events per person year and was significantly reduced by BMT, with increasing time (retention) on BMT. BMT had no significant effect on hospitalizations or average length of stay.
Keywords: buprenorphine, methadone, substance abuse, opioid dependence, healthcare utilization, emergency department utilization, hospitalization, longitudinal cohort
1.0 Introduction
Drug users often have little or no access to mainstream healthcare resources, and as many drug treatment facilities are separate from primary care services, (Chuang et al., 2010; Mowbray et al., 2010; Roy and Miller, 2010) drug users remain marginalized from mainstream healthcare delivery systems (Pollack et al., 2002). As a result, they often rely on fragmented care provided in emergency department (ED) settings. Depending on the condition for which they seek healthcare in ED settings, and the severity of disease, such visits may result in hospitalization. Additionally, social and medical marginalization from traditional healthcare settings may result in delays in accessing healthcare services. Such delays may greatly aggravate medical problems, including preventable diseases and conditions associated with substance abuse. These conditions include a number of acute and chronic medical complications of substance use disorders, including pulmonary and cardiovascular disease, infectious diseases (e.g., HIV, viral hepatitis, etc), hepatic disease, seizures and neurological disorders, and endocrine abnormalities (Altice et al., 2010; McGeary and French, 2000). When left untreated, many of these conditions can result in advanced stage complications, thereby increasing morbidity and mortality. Numerous studies document the increased utilization of ED services among drug users compared to their non-drug using counterparts (French et al., 2000; McGeary and French, 2000; Stein et al., 1993). A significant amount of the excess morbidity and mortality is attributable to preventable illnesses, and unnecessary and inappropriate healthcare utilization (HCU) due to poor access to care (French et al., 2000; McGeary and French, 2000; Stein et al., 1993).
There is a substantial body of evidence supporting the use of medication-assisted treatment (MAT) – specifically methadone maintenance treatment (MMT) – in improving health outcomes and decreasing fragmented HCU among drug users (Friedmann et al., 2006; Laine et al., 2001; Laine et al., 2005; Stein and Anderson, 2003; Stenbacka et al., 1998). Entering effective drug treatment may potentially reduce HCU in a number of ways, including decreasing risks that result in the direct and indirect consequences of drug use, including direct injury, increasing access to primary care services, and stabilizing the lives of individuals whose lifestyle is chaotic. On the other hand, effective drug treatment may increase the identification of medical co-morbidities through increased access to primary care services, resulting in increased awareness of health care needs when the substance use disorder is effectively treated. Furthermore, the chronic and relapsing nature of opioid dependence often results in recidivism to and from evidence-based treatment, including from MAT. As such, treatment is seldom continuous and results in multiple treatment episodes over the life of a drug dependent person.
Buprenorphine (BPN) – a partial opioid agonist – became available for the treatment of opioid dependence in 2002 (Basu et al., 2006). Buprenorphine, unlike methadone maintenance, allows for the first time primary care providers to treat opioid dependence in primary and specialty care settings (Altice et al., 2011; Altice et al., 2006). Since its approval, however, there has been little investigation into the ancillary benefits of buprenorphine maintenance treatment (BMT), such as potential impacts it may have upon HCU. As buprenorphine has shown significant promise as effective MAT, (Barnett et al., 2001; Carrieri et al., 2006; Kakko et al., 2003) further investigation is warranted to better understand the added benefits BMT may offer both patients and health care systems. We therefore sought to examine the impact of buprenorphine treatment on ED utilization and hospitalization among a cohort of opioid dependent persons seeking BMT.
2.0 Methods
Chart review was conducted on a prospective cohort of opioid dependent persons who were seeking BMT to assess the longitudinal HCU of eligible subjects at the only two hospitals in the New Haven, Connecticut area. Using negative binomial regression of data from 209 enrolled subjects, we examined the association between buprenorphine treatment and HCU, measured by the incidence and duration of hospital admissions, and incidence of visits to the ED.
2.1 Study Setting
Project BEST (Buprenorphine Entry into Substance Abuse Treatment) began in January 2005, as the first mobile buprenorphine induction and maintenance program in the United States, linked to the syringe exchange program, and was provided through the Community Healthcare Van (CHCV) in New Haven, Connecticut. The research setting and sample has previously been described to compare tuberculin skin testing results of those in BMT with contemporaneously matched methadone-maintained subjects (Schwarz et al., 2009) and assessment of buprenorphine on hepatic safety (Bruce and Altice, 2007). Subjects were recruited from and BMT was provided through the CHCV, a mobile 40-foot health care clinic that operates in four neighborhoods in New Haven that are disproportionately affected by poverty, substance abuse, HIV/AIDS, viral hepatitis, and mental illness (Altice et al., 2003; Pollack et al., 2002).
2.2 Description of Project BEST
Project BEST was developed as part of a SAMHSA-funded demonstration project to expand BMT into community settings. In addition to the provision of BMT, subjects were also provided street-level case management, routine HIV testing, immediate access to buprenophine induction and stabilization in accordance with Treatment Improvement Protocol 40 (Center for Substance Abuse Treatment, 2004), and screening and treatment of underlying mental illness. In accordance with TIP 40, Project BEST subjects were required to: 1) meet DSM-IV criteria for opioid dependence; 2) have no evidence of benzodiazepine abuse, 3) have hepatic transaminase levels less than five times the upper limit of normal; and 4) have a negative pregnancy test for women of child-bearing age.
Prior to induction, a licensed buprenorphine-prescribing physician evaluated the patient for opioid dependence using standard DSM IV criteria. At induction, subjects are administered the Addiction Severity Index (ASI), (McLellan et al., 1992) and a standardized CHCV-intake interview that includes demographic and social characteristics. After induction, subjects were counseled weekly by a licensed drug treatment counselor and under went immunoassay rapid urine toxicology and standardized counseling as described previously (Copenhaver et al., 2007). Over the first 12 weeks, counseling included a combination of 4 weeks of motivational enhancement techniques and 8 weeks of cognitive behavioral therapy. As in most clinical settings, the counseling intervention was provided by licensed behavioral counselors and the medication prescription and oversight by a physician who evaluated subjects at least monthly. After 12 weeks, contingent upon individual patient stability, clinical staff could recommend changes to the frequency of counseling visits, urine toxicology screening and prescription refills.
Buprenorphine was dispensed from a single pharmacy. Buprenorphine is dispensed weekly throughout the first 12 weeks; substance abuse treatment counselors provided vouchers after counseling sessions that allowed weekly refills. Counselors had discretionary options for renewing vouchers in settings of documented medical or personal emergencies.
2.3 Study Design and Sample
All subjects who received even a single dose of buprenorphine were included in the longitudinal treatment cohort if they underwent buprenorphine induction over the 30-month enrollment period from January 1, 2005 through June 30, 2007. Subjects who were retained on treatment for less than one week were considered comparison subjects, and by definition, not retained on BMT. All subjects were observed for at least 12-months after induction, resulting in a maximum of 42 months of potential observation. Prior to induction, all subjects underwent routine consent procedures to access the relevant intake data as described, baseline laboratory testing including hepatic transaminase levels, serology for HIV and viral hepatitis (HBV and HCV) and urine toxicology screening. A medical release of information was also obtained to retrieve pharmacy data and to review all medical at both emergency departments and hospitals in New Haven (Yale-New Haven Hospital and Hospital of Saint Raphael).
2.4 Study Data
Standardized chart reviews were conducted for all subjects at the only two emergency departments and hospitals in New Haven; no subjects identified as using the Veteran Administration services. All psychiatric visits and hospitalizations are triaged through these EDs and are included in the study. Standardized chart review forms were created for both ED and hospital use. ED chart review forms included the demographic characteristics, date and time of entry to the ED, chief complaint, all discharge diagnoses coded using ICD-9 criteria, and disposition (e.g. home, against medical advice, hospitalization, etc). Hospitalization review included date of admission and discharge, primary and secondary diagnoses, and disposition. Chart review was conducted for all ED visits and hospitalizations for the 12-month period before and after BPN induction.
Buprenorphine utilization was collected using electronic dispensed pharmacy records. Prescriptions were linked to copies of vouchers provided to subjects during the routine provision of clinical care.
2.5 Study Measures and Definitions
ED use and hospitalization data was calculated over both the pre- and post-enrollment periods. ED use was recorded as rate ratios, calculated using the number of ED visits over an observed period of time. Similarly, hospitalization data was recorded as rate ratio count data, number of days hospitalized over an observed time period, and hospitalization average length of stay (ALOS) over an observed time period. Given the relapsing nature of opioid dependence, and because some subjects were inducted onto BMT more than once, retention on buprenorphine was recorded as the cumulative time on BPN and may have included more than one BMT observation period after the initial induction time point. All subjects were allowed to undergo repeat BPN inductions and/or restart BPN at any time. A comparison group, that was meant to describe those who were “treatment seeking” yet who were not retained on BPN, was defined as those who underwent BPN induction but who were retained for less than one week. The BMT group was further divided into those on continuous BMT and intermittent BMT. Individuals who were non persistent with their BMT for any period of 30 days or more, using prescription refill data and who restarted BPN, were defined as intermittent users.
2.6 Statistical Analysis
To analyze the impact of BMT on HCU, we analyzed data from the pre- and post-induction time periods by estimating three separate models. Three dependent variables were used to assess HCU: ED use; hospitalization; and ALOS.
Our analysis aimed to examine the impact of BMT on each of the dependent variables. Since the dependent variables are expressed as number of events per unit time, a negative binomial regression was used to model the outcome in which the conditional mean of the outcome, λ, was modeled in the following manner:
Retention on BMT (Treatmenti) is defined as a continuous variable expressed in months. Timei is a dummy indicator for whether the outcome was observed during the pre- or post-induction period and attempts to address any temporal trends in ED availability or healthcare access over time for both the comparison and treatment groups. The interaction term between Treatment and Time is denoted as Treatmenti Timei and x, is a vector of additional covariates that include gender, race, cocaine use and age, to control for omitted variable bias. Exposure was included in the model to account for different entry and exit times of subjects over time. In this model, the parameter of interest is gamma, since it captures the difference in the outcomes that is neither due to time effects nor the average difference between treatment and comparison groups. The comparison group treatment variable was automatically set equal to zero.
Because ED use, hospitalization and ALOS was observed only for those that experienced an event, a zero-truncated negative binomial regression was estimated using the same covariates in order to compensate for the truncation of the dependent variable. The standard errors were clustered for the zero-truncated negative binomial regression, since there were individuals who had more than one visit to avoid double counting. The level of significance was set at p<0.05.
2.7 Ethical Oversight
All study protocols and investigators were approved under the Yale University Human Investigation Committee.
3.0 Results
3.1 Description of the Sample
Table 1 contains select demographic and health characteristics of the entire cohort stratified by whether they stopped BPN during the 3-day induction period (comparison, 28.2%) or were retained on BPN beyond induction. In general, the sample was comprised of white men in their late thirties who also used cocaine and qualified as meeting criteria for dual diagnosis. BPN-retained subjects differed statistically from comparison subjects in that the retained subjects are older and have lower prevalence of cocaine use co-morbidity. Relative to other characteristics such as race, gender, and hospitalizations, the two groups are statistically similar. Table 1 also contains a summary of HCU: subjects on average had 0.93 ED visits per year, and 0.19 hospital admissions per year across the pre- and post-induction periods. Among the subset of 92 individuals who were hospitalized, the ALOS was 3.92 days.
Table 1.
Comparison of Buprenorphine Maintenance Treatment and Comparison Groups in Project BEST
| Sample size | Total Sample (N=209) | BMT Retained Subjects (N=150, 71.8%) | Comparison Group (N=59, 28.2%) | P value, comparing BMT retained and comparison groups |
|---|---|---|---|---|
| Indicator | N (%) | N (%) | N (%) | |
|
| ||||
| Gender | ||||
| Male | 148 (71) | 105 (70) | 43 (73) | 0.34 |
| Female | 61 (29) | 45 (30) | 16 (27) | 0.34 |
| Race/ethnicity | ||||
| Black | 33 (16) | 21 (14) | 12 (20) | 0.13 |
| Hispanic | 50 (24) | 34 (22) | 16 (27) | 0.25 |
| White | 126 (60) | 95 (63) | 31 (53) | 0.08 |
| Mean Age, years | 36.5 | 36.9 | 35.4 | 0.17 |
| 19–30 | 69 (33) | 47 (31) | 22 (37) | 0.34 |
| 30–45 | 89 (43) | 62 (41) | 27 (46) | 0.28 |
| Over 45 | 51 (24) | 41 (27) | 10 (17) | 0.06 |
| Cocaine Use | 148 (71) | 95 (63) | 51 (86) | <0.001 |
| Health Care Utilization | Mean | Mean | Mean | P-value |
|---|---|---|---|---|
|
| ||||
| Mean Emergency Department visits per person year Mean number of Hospitalizations per person year | 0.93 | 0.95 | 0.86 | 0.35 |
| 0.19 N=209 |
0.20 N=150 |
0.17 N=59 |
0.29 | |
|
| ||||
| Average Length of Hospital Stay (days) | 3.92 N=92 |
4.11 N=79 |
2.77 N=13 |
0.15 |
Null hypothesis for a T test: the difference in the means between comparison and treatment is zero
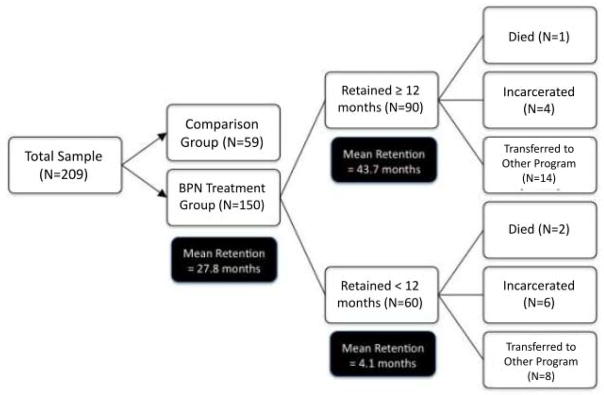
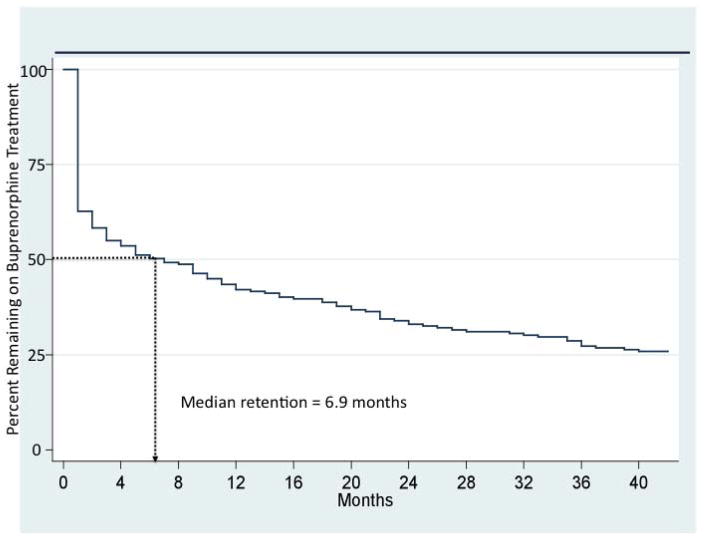
Figure 1 provides disposition and retention data for the cohort. For all subjects, including those in the comparison group, the median retention on BMT was 6.9 months. Among the BMT retained group, mean retention was 27.8 months (median 21.8 months; SD 24.0). Among the 150 subjects retained on BMT, 3 died, 10 had a prolonged incarceration resulting in discontinuation of BMT and 22 were transferred to other forms of treatment (counseling only, methadone maintenance, long-term inpatient treatment). Figure 2 displays Kaplan-Meier survival estimates for the duration of BMT including the comparison and treatment groups. Over one third (37.2%) of the sample discontinued BMT within the first month following induction, while 25% of the sample stayed for at least 43 months in treatment. The median time to BMT discontinuation was 6.9 months.
Figure 1.
Disposition of subjects who underwent buprenorphine induction
Figure 2.
Kaplan-Meier survival estimates of time to discontinuation of buprenorphine maintenance treatment (N=209)
3.2 Correlates of Emergency Department Use
The negative binomial regression results for our three dependent variables (ED use, hospitalization and ALOS) are provided in Table 2. Covariates associated with decreased ED use included younger age and an interaction between BMT (post-induction time period) and time on BPN. The over dispersion coefficient indicates that the data are over dispersed, meaning the variance of the dependent variable is larger than the expected value, confirming the choice of a negative binomial regression over a Poisson model. The other variables in the negative binomial regression were not statistically different from zero.
Table 2.
Results from Negative Binomial Regression
| Dependent Variables | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Emergency Department Visits (count) | Hospital Visits (count) | Average Length of Stay (count) | ||||
|
| ||||||
| Model | Negative Binomial | Negative Binomial | Zero Truncated Negative Binomial | |||
|
| ||||||
| Independent Variables | Coefficient | P-value | Coefficient | P-value | Coefficient | P-value |
|
| ||||||
| Time covariate | 0.24 | 0.301 | 0.51 | 0.172 | −0.21 | 0.39 |
| Treatment | 0.0096 | 0.054 | 0.003 | 0.844 | −0.0038 | 0.699 |
| Time*Treatment | −0.016 | 0.046 | −0.011 | 0.31 | −0.0056 | 0.492 |
| Age | 0.025 | <0.01 | 0.06 | <0.001 | 0.016 | 0.187 |
| Black Race Dummy | 0.02 | 0.95 | 0.1 | 0.37 | −0.3 | 0.318 |
| Hispanic Race Dummy | −0.14 | 0.56 | −0.24 | 0.38 | −0.29 | 0.421 |
| Gender | −0.23 | 0.26 | −0.46 | 0.122 | 0.218 | 0.434 |
| Cocaine Use | 0.54 | 0.02 | −0.4 | 0.212 | −0.69 | 0.093 |
| Constant | −7.07 | <0.001 | −9.47 | <0.001 | 1.1 | 0.05 |
| Overdisperson parameter | 2.31 | <0.001 | 2.31 | <0.001 | 0.51 | <0.001 |
| N | 418 | 418 | 92 | |||
| Log Likelihood | −572.15 | −226.05 | −194.92 | |||
Retention on BMT had a strong and significant effect on reducing ED use. For each additional month of receiving BMT, the log of expected ED usage declines 1.6% of the expected ED visits per person for the first month of BMT. For subjects receiving BMT for 12 months, this translates to a 17.5% decline in expected ED use per subject.
There are no standardized definitions of intermittent BMT, despite opioid dependence being a chronic relapsing disease. Among the 150 subjects who remained on BPN more than one week, 120 (80%) had at least one BPN discontinuation lasting more than 30 days. Our findings of reduced ED use for those who received BPN beyond the first week was robust per month of being on BPN despite analysis controlling for one or more discontinuations (intermittent therapy). Therefore despite the high level of variation in the intermittent BMT group, the findings that retention on BMT is protective of ED use, irrespective of the number of gaps in treatment, remained robust (data not shown).
3.3 Correlates of Hospitalization
For hospitalization, only increasing age was associated with increased hospitalization visits. This result indicates that the association between BMT, or retention on BMT, and hospital admissions is not statistically significant. A similar conclusion was reached through a different analysis using semi-parametric duration models, which estimated the incidence of hospital admissions with a pre- and post-induction comparison for hazard rates between those who were treated and those who dropped out from BMT (data not shown).
3.4 Correlates of Hospital Average Length of Stay
When the dependent variable was defined as duration of hospitalization (days), a zero truncation negative binomial was estimated for the subset of subjects who were admitted at least once. Results from the regression indicated that individuals who received BMT did not have a statistically significant difference in length of hospital admission when compared to those who did not receive BMT.
4.0 Discussion
In this study, we examined the impact of retention on BPN on HCU among a cohort of treatment-seeking subjects who were prescribed BMT. Our data, for the first time, show that for each month of receiving BMT, there is a significant reduction in ED utilization; these findings when amortized over a one-year period of BMT, suggest that there is, on average, a 17.5% decrease in ED usage per subject. There was no significant effect, however, of BMT retention on hospital admissions or duration of hospitalization.
Previous research has identified correlates of HCU among people who use drugs, mostly in the early antiretroviral treatment era, including positive HIV sero status, (Palepu et al., 1999; Palepu et al., 2001) AIDS diagnosis, (Knowlton et al., 2001) cocaine (Palepu et al., 1999; Palepu et al., 2001) or methamphetamine use, (Kerr et al., 2005) and unstable housing status (Palepu et al., 1999; Palepu et al., 2001). Additional research assessing interventions that successfully decreased HCU among drug users include having health insurance (AOR = 0.58) or access to a case manager (Mizuno et al., 2006). Other studies have demonstrated that integration of drug treatment, specifically MMT, and primary care can significantly decrease fragmented HCU (Friedmann et al., 2006; Laine et al., 2001; Laine et al., 2005). In addition to the medical and social benefits of such programs for patients, linkage of primary care and drug treatment can be beneficial for the public sector, offsetting excessive costs incurred through the inappropriate usage of public healthcare facilities (Barnett and Hui, 2000; Barnett et al., 2001; Ettner et al., 2006). Other successful interventions include case management, which has offered a range medical benefits and effects across studies, (Magnus et al., 2001; Thompson et al., 1998) and mobile primary care and needle-exchange programs that provide readily available treatment for acute medical conditions (Pollack et al., 2002).
While existing data suggest that MMT is an effective strategy in reducing ED use, to our knowledge, no such effect upon ED has been investigated for patients on BMT, especially examining the impact of duration of being retained on BMT. To our knowledge, these are the first data affirming BMT retention on ED use. Moreover, the benefits persist with increasing time. These data therefore inform the public debate on buprenorphine’s role as a public health intervention impacting HCU, and specifically ED utilization. At a minimum, we must explore mechanisms to expand BMT and to refine our treatment to improve retention. In 2008, the average ED visit cost in the USA was $1265 (Agency for Healthcare Research and Quality, 2008) and thus an intervention that could decrease ED usage to the extent shown in our study would offer significant increases in efficiency and effectiveness of our healthcare system. As our data do not show an effect upon hospital admissions or ALOS, further research should be directed towards investigating reasons for hospitalizations within this population and whether BMT retention may offer an impact in particular diagnostic-related groups.
Despite these findings, there are several study limitations. The lack of randomization among subjects does not make it possible to completely control for selection bias and unobserved heterogeneity among those who remained and who dropped out of BMT; motivation for treatment or even an unmeasured covariate may have contributed differentially to our outcomes. Data confirm that active cocaine use is associated with worse BMT retention (Alford et al., 2011; Leonardi et al., 2008; Marsch et al., 2005; Sullivan et al., 2006), a finding confirmed in our study. To address this finding, we controlled for cocaine use in our final model, yet we cannot provide the additional contribution of cocaine use alone to ED use or other types of HCU. In our estimates of the model, the time variable has a coefficient equal to zero suggesting that the ED visit rate does not change significantly over time on average for both comparison and treatment groups in our sample when we make a comparison between pre and post induction periods. An implicit assumption in the model is that the average change in ED use would have been the same for treatment and comparison groups, also known as the parallel trend assumption, which may have been violated due to possible selection bias. Further, our methodology of chart review is necessarily limited in its scope and does not account for ED use outside our catchment area, however we feel the likelihood that those who were retained on BMT, versus those who were not, used EDs differently in terms of geography is unlikely. Additionally, given the study accounted only for care received at the two hospitals in New Haven, Connecticut, care accessed at facilities in other areas may have been missed. Data from ED users in New Haven, however, suggest that these hospitals cover the overwhelming majority of ED use by drug users (Academic ED SBIRT Research Collaborative, 2010; Pollack et al., 2002). Further, while Project BEST included additional components such as counseling and case management, our methodology does not allow us to separate out the specific effect of BMT alone. Though stable benzodiazepine use was allowed, abuse was an exclusion criteria. This exclusion, however, is compatible with current TIP 40 recommendations, but may not be generalizable to similar patients where benzodiazepine abuse is not uncommon in this population. Moreover, our study was conducted in a unique mobile setting which differs from other venues where BMT may be offered, which potentially limits the generalizability of these results. The retention on BMT overall was similar to other primary care setting (Stein et al., 2005), thus reducing this concern. Finally, as our population was restricted by size and geographic scope, the generalizability of our conclusions may be limited to regions where the presence of cocaine use is different.
Generally, our cohort appears to be representative of studies that have examined HCU in opioid dependent patients, aside from the high prevalence of cocaine use. In general, the ED utilization ranges from 0.28 to 1.49 visits per person per year in such populations and hospitalization ranges from 0.22 to 0.65 total visits per person per year (Kerr et al., 2005; Laine et al., 2001; Laine et al., 2005; Masson et al., 2002; McGeary and French, 2000; Palepu et al., 1999; Palepu et al., 2001). Results from our study demonstrated 0.88 total visits per person per year for ED utilization, which is well within the range documented in previous studies and 0.18 visits per person for hospitalization, which is on the lower end of the range seen in other cohorts.
There are approximately 2 million opioid dependent persons in the United States, yet only a minority have access to MAT. Although MMT programs effectively decreases HCU in this population, arguing for an increase in medication-assisted therapy availability in general, enrollment into MMT remains limited due to its highly regulated structure as well as stigma associated with methadone treatment, thereby limiting the degree to which it will be an effective strategy overall to address opioid dependence in the US (Bruce, 2010). Thus, the demonstration that retention on BMT also impacts decreased fragmented HCU offers an additional strategy to treat opioid dependent persons while also more efficiently providing healthcare in an increasingly challenging health care environment.
Acknowledgments
The authors would like to acknowledge funding by the Substance Abuse and Mental Health Services Agency (Altice, H97 TI015767) for the provision of funding to provide the clinical care for subjects and to the National Institutes on Drug Abuse for career development awards for FLA (K24 DA017072) and RDB (K23 DA022143).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Academic ED SBIRT Research Collaborative. The impact of screening, brief intervention and referral for treatment in emergency department patients' alcohol use: a 3-, 6- and 12-month follow-up. Alcohol Alcohol. 2010;45:514–519. doi: 10.1093/alcalc/agq058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. 2008 Accessed at http://www.meps.ahrq.gov/mepsweb/ on May 25, 2011. accessed on. [PubMed]
- Alford DP, LaBelle CT, Kretsch N, Bergeron A, Winter M, Botticelli M, Samet JH. Collaborative care of opioid-addicted patients in primary care using buprenorphine: five-year experience. Arch Intern Med. 2011;171:425–431. doi: 10.1001/archinternmed.2010.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Bruce RD, Lucas GM, Lum PJ, Korthuis PT, Flanigan TP, Cunningham CO, Sullivan LE, Vergara-Rodriguez P, Fiellin DA, Cajina A, Botsko M, Nandi V, Gourevitch MN, Finkelstein R, Collaborative B. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: results from a multisite study. J Acquir Immune Defic Syndr. 2011;56(Suppl 1):S22–32. doi: 10.1097/QAI.0b013e318209751e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376:59–79. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Springer S, Buitrago M, Hunt DP, Friedland GH. Pilot study to enhance HIV care using needle exchange-based health services for out-of-treatment injecting drug users. J Urban Health. 2003;80:416–427. doi: 10.1093/jurban/jtg053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Sullivan LE, Smith-Rohrberg D, Basu S, Stancliff S, Eldred L. The potential role of buprenorphine in the treatment of opioid dependence in HIV-infected individuals and in HIV infection prevention. Clin Infect Dis. 2006;43(Suppl 4):S178–183. doi: 10.1086/508181. [DOI] [PubMed] [Google Scholar]
- Barnett PG, Hui SS. The cost-effectiveness of methadone maintenance. Mt Sinai J Med. 2000;67:365–374. [PubMed] [Google Scholar]
- Barnett PG, Zaric GS, Brandeau ML. The cost-effectiveness of buprenorphine maintenance therapy for opiate addiction in the United States. Addiction. 2001;96:1267–1278. doi: 10.1046/j.1360-0443.2001.96912676.x. [DOI] [PubMed] [Google Scholar]
- Basu S, Smith-Rohrberg D, Bruce RD, Altice FL. Models for integrating buprenorphine therapy into the primary HIV care setting. Clin Infect Dis. 2006;42:716–721. doi: 10.1086/500200. [DOI] [PubMed] [Google Scholar]
- Bruce RD. Methadone as HIV prevention: high volume methadone sites to decrease HIV incidence rates in resource limited settings. Int J Drug Policy. 2010;21:122–124. doi: 10.1016/j.drugpo.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce RD, Altice FL. Case series on the safe use of buprenorphine/naloxone in individuals with acute hepatitis C infection and abnormal hepatic liver transaminases. Am J Drug Alcohol Abuse. 2007;33:869–874. doi: 10.1080/00952990701653875. [DOI] [PubMed] [Google Scholar]
- Carrieri MP, Amass L, Lucas GM, Vlahov D, Wodak A, Woody GE. Buprenorphine use: The international experience. Clinical Infectious Diseases. 2006;43:S197–215. doi: 10.1086/508184. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Clinical Guidelines for the Use of Buprenorphine in the Treatment of Opioid Addiction. Treatment Improvement Protocol (TIP) Series 40. Substance Abuse and Mental Health Services Administration (SAMHSA) (Ed.). Department of Health and Human Services; Rockville, MD: 2004. [PubMed] [Google Scholar]
- Chuang E, Wells R, Alexander JA. Public Managed Care and Service Access in Outpatient Substance Abuse Treatment Units. J Behav Health Serv Res. 2010 doi: 10.1007/s11414-010-9230-y. [DOI] [PubMed] [Google Scholar]
- Copenhaver MM, Bruce RD, Altice FL. Behavioral counseling content for optimizing the use of buprenorphine for treatment of opioid dependence in community-based settings: a review of the empirical evidence. Am J Drug Alcohol Abuse. 2007;33:643–654. doi: 10.1080/00952990701522674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettner SL, Huang D, Evans E, Ash DR, Hardy M, Jourabchi M, Hser YI. Benefit-cost in the California treatment outcome project: does substance abuse treatment “pay for itself”? Health Serv Res. 2006;41:192–213. doi: 10.1111/j.1475-6773.2005.00466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French MT, McGeary KA, Chitwood DD, McCoy CB. Chronic illicit drug use, health services utilization and the cost of medical care. Soc Sci Med. 2000;50:1703–1713. doi: 10.1016/s0277-9536(99)00411-6. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, Hendrickson JC, Gerstein DR, Zhang Z, Stein MD. Do mechanisms that link addiction treatment patients to primary care influence subsequent utilization of emergency and hospital care? Med Care. 2006;44:8–15. doi: 10.1097/01.mlr.0000188913.50489.77. [DOI] [PubMed] [Google Scholar]
- Kakko J, Svanborg KD, Kreek MJ, Heilig M. 1-year retention and social function after buprenorphine-assisted relapse prevention treatment for heroin dependence in Sweden: a randomised, placebo-controlled trial. Lancet. 2003;361:662–668. doi: 10.1016/S0140-6736(03)12600-1. [DOI] [PubMed] [Google Scholar]
- Kerr T, Wood E, Grafstein E, Ishida T, Shannon K, Lai C, Montaner J, Tyndall MW. High rates of primary care and emergency department use among injection drug users in Vancouver. J Public Health (Oxf) 2005;27:62–66. doi: 10.1093/pubmed/fdh189. [DOI] [PubMed] [Google Scholar]
- Knowlton AR, Hoover DR, Chung SE, Celentano DD, Vlahov D, Latkin CA. Access to medical care and service utilization among injection drug users with HIV/AIDS. Drug Alcohol Depend. 2001;64:55–62. doi: 10.1016/s0376-8716(00)00228-3. [DOI] [PubMed] [Google Scholar]
- Laine C, Hauck WW, Gourevitch MN, Rothman J, Cohen A, Turner BJ. Regular outpatient medical and drug abuse care and subsequent hospitalization of persons who use illicit drugs. Jama. 2001;285:2355–2362. doi: 10.1001/jama.285.18.2355. [DOI] [PubMed] [Google Scholar]
- Laine C, Lin YT, Hauck WW, Turner BJ. Availability of medical care services in drug treatment clinics associated with lower repeated emergency department use. Med Care. 2005;43:985–995. doi: 10.1097/01.mlr.0000178198.79329.89. [DOI] [PubMed] [Google Scholar]
- Leonardi C, Hanna N, Laurenzi P, Fagetti R, Group IDAC. Multi-centre observational study of buprenorphine use in 32 Italian drug addiction centres. Drug Alcohol Depend. 2008;94:125–132. doi: 10.1016/j.drugalcdep.2007.10.017. [DOI] [PubMed] [Google Scholar]
- Magnus M, Schmidt N, Kirkhart K, Schieffelin C, Fuchs N, Brown B, Kissinger PJ. Association between ancillary services and clinical and behavioral outcomes among HIV-infected women. AIDS Patient Care STDS. 2001;15:137–145. doi: 10.1089/108729101750123607. [DOI] [PubMed] [Google Scholar]
- Marsch LA, Stephens MA, Mudric T, Strain EC, Bigelow GE, Johnson RE. Predictors of outcome in LAAM, buprenorphine, and methadone treatment for opioid dependence. Exp Clin Psychopharmacol. 2005;13:293–302. doi: 10.1037/1064-1297.13.4.293. [DOI] [PubMed] [Google Scholar]
- Masson CL, Sorensen JL, Batki SL, Okin R, Delucchi KL, Perlman DC. Medical service use and financial charges among opioid users at a public hospital. Drug Alcohol Depend. 2002;66:45–50. doi: 10.1016/s0376-8716(01)00182-x. [DOI] [PubMed] [Google Scholar]
- McGeary KA, French MT. Illicit drug use and emergency room utilization. Health Serv Res. 2000;35:153–169. [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The fifth edition of the addiction severity index. Journal of substance abuse treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Mizuno Y, Wilkinson JD, Santibanez S, Dawson Rose C, Knowlton A, Handley K, Gourevitch MN. Correlates of health care utilization among HIV-seropositive injection drug users. AIDS Care. 2006;18:417–425. doi: 10.1080/09540120500162247. [DOI] [PubMed] [Google Scholar]
- Mowbray O, Perron BE, Bohnert AS, Krentzman AR, Vaughn MG. Service use and barriers to care among heroin users: results from a national survey. Am J Drug Alcohol Abuse. 2010;36:305–310. doi: 10.3109/00952990.2010.503824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palepu A, Strathdee SA, Hogg RS, Anis AH, Rae S, Cornelisse PG, Patrick DM, O'Shaughnessy MV, Schechter MT. The social determinants of emergency department and hospital use by injection drug users in Canada. J Urban Health. 1999;76:409–418. doi: 10.1007/BF02351499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palepu A, Tyndall MW, Leon H, Muller J, O'Shaughnessy MV, Schechter MT, Anis AH. Hospital utilization and costs in a cohort of injection drug users. CMAJ. 2001;165:415–420. [PMC free article] [PubMed] [Google Scholar]
- Pollack HA, Khoshnood K, Blankenship KM, Altice FL. The impact of needle exchange-based health services on emergency department use. J Gen Intern Med. 2002;17:341–348. doi: 10.1046/j.1525-1497.2002.10663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy K, Miller M. Parity and the medicalization of addiction treatment. J Psychoactive Drugs. 2010;42:115–120. doi: 10.1080/02791072.2010.10400683. [DOI] [PubMed] [Google Scholar]
- Schwarz RK, Bruce RD, Ball SA, Herme M, Altice FL. Comparison of tuberculin skin testing reactivity in opioid-dependent patients seeking treatment with methadone versus buprenorphine: policy implications for tuberculosis screening. Am J Drug Alcohol Abuse. 2009;35:439–444. doi: 10.3109/00952990903447741. [DOI] [PubMed] [Google Scholar]
- Stein MD, Anderson B. Injection frequency mediates health service use among persons with a history of drug injection. Drug Alcohol Depend. 2003;70:159–168. doi: 10.1016/s0376-8716(02)00344-7. [DOI] [PubMed] [Google Scholar]
- Stein MD, Cioe P, Friedmann PD. Buprenorphine retention in primary care. J Gen Intern Med. 2005;20:1038–1041. doi: 10.1111/j.1525-1497.2005.0228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, O'Sullivan PS, Ellis P, Perrin H, Wartenberg A. Utilization of medical services by drug abusers in detoxification. J Subst Abuse. 1993;5:187–193. doi: 10.1016/0899-3289(93)90062-g. [DOI] [PubMed] [Google Scholar]
- Stenbacka M, Leifman A, Romelsjo A. The impact of methadone on consumption of inpatient care and mortality, with special reference to HIV status. Subst Use Misuse. 1998;33:2819–2834. doi: 10.3109/10826089809059353. [DOI] [PubMed] [Google Scholar]
- Sullivan LE, Moore BA, O'Connor PG, Barry DT, Chawarski MC, Schottenfeld RS, Fiellin DA. The association between cocaine use and treatment outcomes in patients receiving office-based buprenorphine/naloxone for the treatment of opioid dependence. Am J Addict. 2006;19:53–58. doi: 10.1111/j.1521-0391.2009.00003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson AS, Blankenship KM, Selwyn PA, Khoshnood K, Lopez M, Balacos K, Altice FL. Evaluation of an innovative program to address the health and social service needs of drug-using women with or at risk for HIV infection. J Community Health. 1998;23:419–440. doi: 10.1023/a:1018706107776. [DOI] [PubMed] [Google Scholar]