Structured Abstract
Objective
This study sought to measure the incidence of perioperative beta-blocker non-compliance by patients who were prescribed chronic beta blocker therapy and presented for surgery from home. The effect of patient non-compliance on day of surgery presenting heart rate was also examined.
Design
Prospective observational study with outcome data obtained from review of the medical record.
Setting
The preoperative clinic and operating rooms of a Veterans Administration hospital.
Participants
Patients on chronic beta blocker therapy who presented from home for surgery.
Interventions
None.
Measurements and Main Results
Demographic and comorbidity data as well as data on self-reported compliance to beta-blocker therapy, initial day of surgery vital signs, and recent ambulatory vital signs were collected. Ten out of fifty subjects (20%; 95% CI = 9-31%) reported not taking their day of surgery beta-blocker. These self-reported non-adherers demonstrated a higher presenting heart rate on the day of surgery vs. adherent subjects (median of 78 beats per minute vs. 65 beats per minute, p=0.02 by Wilcoxon Rank-Sum Test). The difference-in-difference between baseline primary care and day of surgery heart rate was also statistically significant between compliant and non-compliant subjects (-7 beats per minute vs. +12.5 beats per minute, p<0.00001).
Conclusions
Patient self-report and physiologic data documented failure to take beta-blockers and possible beta-blocker withdrawal in 20% of patients who presented for surgery from home. If these findings are confirmed in larger studies, improved patient understanding of and compliance with medication instructions during preoperative visits should be a focus of future quality improvement initiatives.
Keywords: Beta Blockade, Preoperative Assessment, Medication Compliance
Introduction
In accordance with the 2009 American College of Cardiology/American Heart Association (ACC/AHA) Focused Update on Perioperative Beta-Blockade,1 physicians at preadmission testing appointments routinely instruct patients who are prescribed beta-blockers to continue them as directed on the morning of surgery. Indeed, according to the ACC/AHA guidelines, continuation of preexisting beta-blockade is the only class I indication for routine preoperative use of these drugs.1
There is reason to suspect however, that instructions to continue beta-blockers may be confusing for many patients. Along with directions regarding continuation of beta-blockers, patients also receive instructions to remain NPO and to stop or reduce the dose of other medications such as diuretics, anticoagulants, and hypoglycemic medications. In the context of the preoperative appointment when patients receive a relatively complex set of instructions, it is not known how often patients who are prescribed beta-blockers are able to execute this specific instruction and actually take their preoperative beta-blocker dose as directed.
Non-adherence to cardioprotective medications is well-recognized outside of the anesthesia literature as an important contributor to patient morbidity, and there is extensive published research regarding medication compliance across many medical specialties.2-6 Despite the importance of this issue, research within the field of anesthesiology regarding patients' perioperative medication compliance is almost non-existent. No study has yet examined adherence on the part of patients to beta-blocker therapy in the perioperative period - a period that is known to be associated with high stress,7,8 confusing medication changes, and deleterious effects of beta blocker withdrawal.9
The present study sought to address this gap in the medical literature by identifying the prevalence of self-reported day of surgery beta-blocker adherence in a cohort of patients presenting for surgery from home and correlating this information with presurgical heart rate.
Methods
Data for the present analysis were compiled by reviewing the medical records of 200 Veterans who were enrolled as part of an ongoing study of perioperative hypertension. Subjects were enrolled from January 2010 through August 20, 2010. Surgical encounters were tracked and analyzed for an additional one month following the end of enrollment, through September 20, 2010. All participants completed written informed consent, and the present analysis was conducted with approval of the local institutional review board. Inclusion for the present analysis required the following: 1) subjects must have been prescribed an outpatient beta-blocker (excepting ophthalmic preparations) prior to their day of surgery, 2) subjects must have presented for anesthesia and surgery from home on the day of surgery.
For all included subjects, anesthetic records were reviewed individually by study personnel to ascertain the subject report concerning the taking of his/her beta-blocker on the day of surgery. This method of anesthetic record review was made possible because of a quality improvement initiative at the study institution. For this initiative, treating anesthesiologists are asked to document on their anesthetic record whether or not a patient is prescribed a beta-blocker and if so, whether the patient reports taking their most recently scheduled dose on the day of surgery. Patients who lacked specific documentation of beta blocker status were excluded from the analysis.
Initial heart rate and blood pressure on the day of surgery and the heart rate and blood pressure from the most recent non-urgent primary care appointment were obtained from the electronic medical record (EMR). For subjects with no record in the prior twelve months of a primary care visit at the study institution, the most recent non-urgent outpatient clinic visit at which vital signs were recorded was used.
If there were multiple vital sign recordings from either the reference ambulatory visit or the day of surgery, the initial reading at each visit was used in the current analysis. In addition to vital sign data, the following information was extracted from the EMR: demographic data (age, gender, surgery type, days between the preadmission testing visit and the surgery, and days between the baseline ambulatory vital signs and surgery); lifestyle factors (current smoking status and body-mass index calculated as weight in kilograms divided by the square of the height in meters); medical comorbidities (diagnosis of hypertension, hyperlipidemia, coronary artery disease, diabetes, depression, anxiety, and post-traumatic stress disorder); and outpatient anti-hypertensive medications as listed on the subjects' pharmacy record (prescriptions for beta-blockers, ace-inhibitors, angiotensin receptor blockers, diuretics, calcium channel blockers, nitrates, hydralazine, and alpha-2 agonists). Population characteristics for all demographic variables, medical co-morbidities, prescribed medications, and vital sign variables are reported for the cohort and stratified by self-reported beta-blocker status. Descriptive data are reported as either the proportion or the median and interquartile range (IQR) and are compared between groups using a two-tailed Fisher's Exact Test or Wilcoxon Rank-Sum Test as appropriate.
The primary endpoints for the current analysis were, 1) the percent (+/- 95% confidence interval) of patients prescribed preoperative beta-blockers who self-reported not taking them on the day of surgery, 2) a comparison of the distribution of presenting day of surgery heart rate among self-reported non-adherent subjects versus adherent subjects, and 3) a difference-in-difference analysis of heart rates between the initial day of surgery measurement and the reference outpatient clinic measurement. This third outcome was designed to investigate whether any observed heart rate differences on the day of surgery were merely reflective of longstanding differences in heart rates unrelated to acute perioperative beta blocker withdrawal. For significance testing, two-tailed, non-parametric tests are reported with a p-value <0.05 chosen as the level of statistical significance.
Results
Baseline Descriptive Analysis
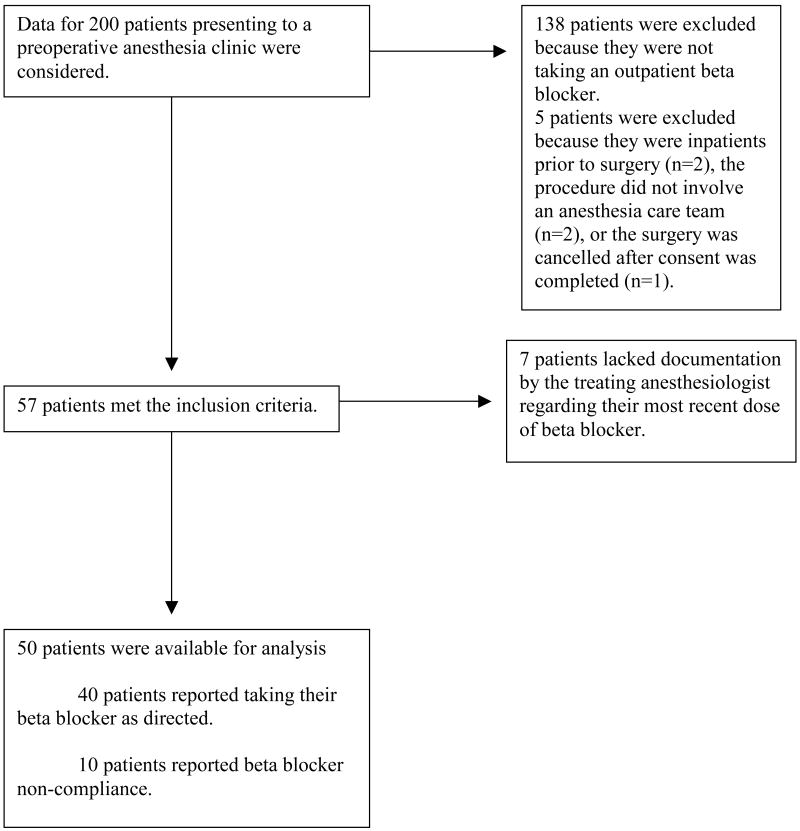
Of 200 subjects considered, a total of 57 subjects fulfilled the inclusion criteria. For seven of these subjects, the day of surgery anesthetic record did not specifically document beta blocker usage on the day of surgery, leaving 50 subjects for inclusion in the primary analysis (see figure 1), 10 of whom reported perioperative beta blocker non-compliance. Of the 50 subjects, 49 were male. The median age was 71.5 years (IQR = 64-78 years). The median time between the reference outpatient visit and the day of surgery was 48.5 days (IQR = 22.8–76.5 days), and the median time between the preadmission testing visit at which beta-blocker instructions are given and the day of surgery was 15.5 days (IQR = 10-22.5 days).
Figure 1.
Flow diagram of patient selection and analysis.
Six subjects were not seen in primary care. Of these, 2 were seen at a cardiology clinic, 2 were seen at a neurosurgery clinic, 1 was seen at a hypertension management clinic, and 1 was seen at a hematology clinic. None of the fifty subjects were taking alpha-2 agonists or hydralazine, so these were removed from the analysis. Forty-seven of the 50 patients had been prescribed a beta-blocker for at least 30 days prior to surgery. Of the 3 patients with more recent beta blocker prescriptions, 1 was in the non-compliant group, and two were in the compliant group. Of the 50 included patients, 15 were prescribed atenolol once-daily, 12 were prescribed extended-release metoprolol formulations, 20 patients were prescribed metoprolol twice-daily, 1 was prescribed betaxolol once-daily, 1 was prescribed atenolol twice-daily, and 1 was prescribed labetalol thrice daily. The distribution of these drugs between compliant and non-compliant groups was unremarkable (of the 10 non-compliant patients, 3 were on atenolol, 3 were on extended release metoprolol, and 4 were on twice-daily metoprolol). There was no significant difference between self-reported beta-blocker adherent and non-adherent subjects on any of the demographic, medical co-morbidity, or prescribed medication data (see Table 1). For vital signs data, the reference ambulatory SBP was higher in the adherent versus non-adherent group (median of 132mmHg vs. 122mmHg, p=0.04). All vital signs data are summarized in Table 2.
Table 1. Descriptive Analysis of Cohort.
| Categorical Variables: | Overall Cohort Number (%) | Adherent Number (%) | Non-adherent Number (%) | P-Value for Difference |
|---|---|---|---|---|
| Male Gender | 49 (98) | 40 (100) | 9 (90) | 0.20 |
| Current Smoker | 8 (16) | 7 (18) | 1 (10) | 1.00 |
| Surgery type: | ||||
| Cardiothoracic or Vascular | 11 (22) | 8 (20) | 3 (30) | 0.67 |
| Diagnosis of: | ||||
| Hypertension | 47 (94) | 39 (98) | 8 (80) | 0.10 |
| Diabetes | 20 (40) | 16 (40) | 4 (40) | 1.00 |
| Coronary Artery Disease | 27 (54) | 21 (53) | 6 (60) | 0.74 |
| Hyperlipidemia | 11 (22) | 7 (18) | 4 (40) | 0.20 |
| Depression | 8 (16) | 7 (18) | 1 (10) | 1.00 |
| Anxiety | 5 (10) | 5 (13) | 0 (0) | 0.57 |
| PTSD | 2 (4) | 2 (5) | 0 (0) | 1.00 |
| Prescription for: | ||||
| Ace-inhibitor | 18 (36) | 16 (40) | 2 (20) | 0.30 |
| ARB | 8 (16) | 6 (15) | 2 (20) | 0.65 |
| Diuretic | 30 (60) | 24 (60) | 6 (60) | 1.00 |
| CCB | 17 (34) | 13 (33) | 4 (40) | 0.72 |
| Nitrate | 6 (12) | 5 (13) | 1 (10) | 1.00 |
| Continuous Variables: | Median (IQR) | Median (IQR) | Median (IQR) | P-Value for Difference |
| Age (years) | 71.5 (64-78) | 71 (64-78) | 74 (68-83) | 0.27 |
| BMI | 29.3 (27.3-33.5) | 30 (28-34) | 28 (24-35) | 0.20 |
| Days since Ambulatory Vitals | 48.5 (22.8-76.5) | 44 (18-70) | 61 (26-155) | 0.20 |
| Days since PAT Visit | 15.5 (10-22.5) | 17 (10-24) | 10 (5-25) | 0.11 |
PTSD=Post-Traumatic Stress Disorder, ARB=Angiotensin Receptor Blocker, CCB=Calcium Channel Blocker, BMI= Body-Mass Index, PAT=Preadmission Testing
Table 2. Vital Signs Stratified by Beta Blocker Status.
| Variable: | Overall Cohort Median (IQR) | Adherers Median (IQR) | Non-adherers Median (IQR) | P-Value for Difference |
|---|---|---|---|---|
| Ambulatory SBP | 130 (118-140) | 132 (120-141) | 122 (107-131) | 0.04 |
| Ambulatory DBP | 68 (61-78) | 70 (63-78) | 62 (56-77) | 0.09 |
| Ambulatory HR | 69 (60-79) | 72 (64-79) | 60 (57-70) | 0.06 |
| Day of Surgery SBP | 133 (122-143) | 133 (122-142) | 140 (118-148) | 0.77 |
| Day of Surgery DBP | 75 (65-82) | 75 (64-83) | 74 (70-80) | 0.99 |
| Day of Surgery HR | 68 (60-77) | 65 (58-76) | 78 (65-90) | 0.02 |
| Change in SBP | +3 (-7.3 to +17.3) | -1 (-8.8 to +12) | +16.5 (+1.3 to +24.3) | 0.06 |
| Change in DBP | +3.5 (-4 to +11) | +2 (-4 to +8.5) | +10.5 (-1.8 to +16) | 0.07 |
| Change in HR | -2.5 (-11.5 to +6.3) | -7 (-14 to +3.8) | +12.5 (+7.5 to +23.8) | <0.001 |
SBP = Systolic blood pressure, DBP = Diastolic blood pressure, HR = Heart rate.
Analysis of Primary Outcomes
Of the fifty patients retained in the primary analysis, 20% (n=10) reported that they did not take their beta-blocker on the morning of surgery (95% confidence interval = 9-31%). These self-reported non-adherers demonstrated a higher presenting heart rate on the day of surgery vs. adherent subjects (median of 78 beats per minute vs. 65 beats per minute, p=0.02 by Wilcoxon Rank-Sum Test). In an alternative analysis, we first treated the 7 subjects with missing documentation as presumptively beta blocker adherent and demonstrated that the 10 self-reported non-adherers demonstrated a higher presenting heart rate on the day of surgery vs. this larger group of subjects (median of 78 beats per minute vs. 68 beats per minute, p=0.03). Second, we treated the 7 subjects with missing documentation as presumptively non-adherent, and again the group of 17 presumptively non-adherent subjects demonstrated a higher presenting heart rate on the day of surgery vs. the definitively adherent patients (median of 72 beats per minute vs. 65 beats per minute, p=0.03).
When the baseline primary care heart rate was included in the analysis, the non-adherent patients demonstrated a higher day of surgery heart rate vs. their primary care baseline by a median of 12.5 beats per minute (IQR = +7.5 to +23.8 beats per minute, p=0.005), while patients reporting beta-blocker adherence demonstrated a lower heart rate on the day of surgery vs. the reference ambulatory measurement by a median of 7 beats per minute (IQR = -14 beats per minute to +3.8 beats per minute, p=0.002). For the difference-in-difference analysis, heart rate differences between the adherent and non-adherent groups were significantly different from each other (p<0.00001). Box plots illustrating the difference-in-difference analysis of heart rate stratified between the two groups of subjects are shown in Figure 2.
Figure 2.
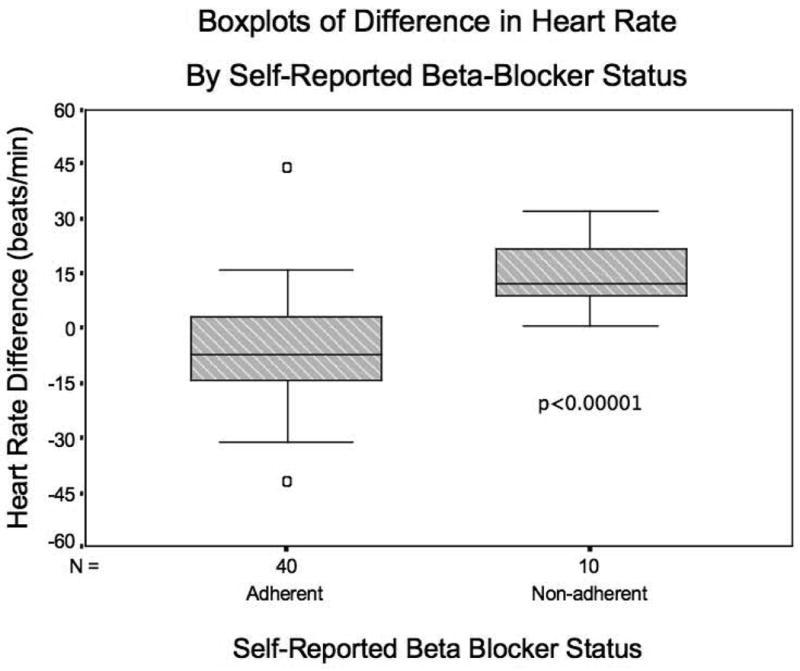
Difference-in-difference analysis. Heart rate difference was calculated as the initial day of surgery heart rate minus the reference ambulatory heart rate. A negative difference therefore corresponds to a lower heart rate on the morning of surgery. Shaded boxes represent the interquartile range (IQR) with solid line at the median. Whiskers represent the spread of data up to 1.5 times the IQR with outliers marked individually. P-value calculated by Wilcoxon Rank-Sum Test.
Discussion
Although small and based on data collected from the EMR, this study represents the first analysis of perioperative medication non-compliance on the part of patients within the field of anesthesiology. While a great amount of effort is being invested in defining the precise populations, timing, and type of beta-blockade that will most benefit surgical patients, very little work has gone into studying how the current guidelines are being followed by patients themselves in the “real world” presurgical environment. This gap in the literature has persisted despite work from fields outside of anesthesiology demonstrating that non-adherence to cardioprotective medications is substantial and associated with significant morbidity.5
Among the fifty patients included in our study, one in five were by self-report, non-compliant to day of surgery beta-blocker instructions despite receiving directions both verbally and in writing to continue taking beta-blockers on the morning of surgery. Although patient self-report is subject to problems of reliability, the accompanying heart rate analysis of these same subjects offers independent, physiologic support for a significant proportion of non-compliance to day of surgery beta-blockade in our cohort. Our results are consistent with data from outside the perioperative period, in which long-term patient adherence to beta blocker therapy at 6-months ranged from 61-88%.2-4,6
Although our study was not designed to follow intraoperative or post-anesthetic outcomes, it is reasonable to suggest that if our finding is confirmed in larger populations, the observed increases in heart rate may carry clinical relevance for patient outcomes. The beta-blocker withdrawal state, as an entity associated with increased cardiovascular risk, has been recognized since the 1970s,10,11 and recent literature has further highlighted the deleterious effects of beta-blocker withdrawal particularly in the perioperative period.9 Nevertheless, the evidence supporting continuation of perioperative beta blockade is not beyond question,12 and it may be that the level C evidence supporting the ACC/AHA class 1 recommendation may yet evolve. Accordingly, it is not known whether improved patient compliance to perioperative beta blockade would improve outcomes. Non-compliant patients in our study demonstrated a median presurgical rise in heart rate of 12.5 beats per minute, and sixty percent of them had presurgical heart rates greater than seventy beats per minute (versus thirty-eight percent in the adherent group). If tight heart rate control is desired, the current findings demonstrate the relevance of patient non-compliance and the associated need for interventions to address patient beta-blocker compliance on the day of surgery.
It is interesting to note that beta-blocker adherent subjects in our study demonstrated a significantly lower heart rate on day of surgery as compared to the reference ambulatory measurement (lower by a median of 7 beats per minute, p=0.002). This finding has led us to speculate that some of this group of so-called beta-blocker adherent subjects may actually have been newly adherent – i.e., some may not have been taking their beta-blockers on a regular basis, but when confronted with surgery and explicit instructions to take these medications, they became medication compliant. To investigate this possibility, we conducted a post hoc analysis of the self-reported adherent group comparing heart rates at three time points – primary care, the preadmission anesthesia clinic, and the day of surgery. Indeed, for the patients with self-reported day of surgery beta-blocker compliance, the primary care clinic and preoperative anesthesia clinic visit heart rates were not significantly different from each other (median of 72 beats per minute versus 75 beats per minute, p=0.32 by Wilcoxon Signed Rank Test). The reduction in heart rate was significant between both of these time points and the day of surgery (median day of surgery heart rate = 65 beats per minute, p<0.001 versus preoperative anesthesia clinic and p=0.002 versus the primary care clinic). If this suggestion of new-onset beta blocker compliance is confirmed in larger studies, our results would mean that not only are patients on chronic beta-blockers frequently presenting in acute withdrawal on the day of surgery, but that among those who are not withdrawing, a significant percentage may in fact be presenting for surgery with acute onset of beta-blockade. Such a finding would be of significant clinical import since both discontinuation of chronic beta-blockade and initiation of high-dose day of surgery beta-blockade13 may both increase perioperative morbidity. Future studies of beta-blocker adherence patterns may help to clarify any phenomenon of better perioperative medication adherence among a subset of patients presenting from home.
In addition to its importance for patient safety, compliance with beta-blocker instructions has significant implications for interpreting epidemiologic data on the potential benefits of perioperative beta-blockade. If studies of surgical risk use populations that are assumed to be on chronic beta-blocker therapy9 but among whom are a significant subset of patients who are actually withdrawing from or acutely initiating these agents on their day of surgery, then the findings will tend to underestimate the true effects of chronic beta-blockade, acute initiation of beta-blockade, and acute beta-blocker withdrawal on outcomes. The recent article by Wallace, et al.9 demonstrating improved outcomes in a large cohort of veterans with chronic beta-blockade, for example, fails to address this issue of medication non-adherence. Assuming that the population of veterans described in that article was comparable to our population of veterans, the beneficial effects of beta-blockade may have been underestimated in that study.
The present study while suggestive had several limitations. Due to the small sample size and reliance on data from the medical records of consenting patients for ascertaining beta-blocker status, a more standardized measure of medication compliance across a larger population would be helpful. A larger cohort would also provide for a more powerful test of potential covariates, and of the variables that only approached significance. Complementary analyses of blood pressure changes that may accompany medication non-compliance would also be of interest to pursue in a larger study. Also, our study population was limited to United States veterans who may exhibit different medication-compliance behaviors as compared to the non-veteran population.14 In addition, while our physiologic heart rate data were consistent with patient self-report, it is likely that objective measurements of serum beta-blocker levels would have offered more precise determinations of beta-blocker status.
Our overall findings however, serve to highlight to the medical community the difficulty of translating beta-blockade guidelines into clinical practice, especially among populations that may be particularly prone to non-adherence. Indeed, these results suggest that attention to beta-blocker adherence prior to surgery should be a focus of directed efforts. Studies of adherence to perioperative beta-blocker guidelines have so far focused primarily on institutional behavior by studying hospital or care-giver adherence to perioperative beta-blocker recommendations.15-17 Our study highlights that even institutions or individual physicians who strictly follow beta-blocker recommendations likely still have a great deal of work to do to maximize cardiac protection among patients.
In conclusion, given the importance of perioperative cardiac protection and the potential morbidity of beta-blocker withdrawal, it is important for the anesthesiology community to dedicate further research toward defining typical non-compliance rates and the risk-factors for such non-compliance. If confirmed in larger studies, our results suggest that patients may benefit from focused efforts toward improving patient understanding of and motivation for following medication instructions during preoperative visits.
Acknowledgments
This material is based upon work supported in part by the Department of Veterans Affairs. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Funding support: This research was funded by National Institutes of Health grant number NIH T32 GM086287-01 (Niklason).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof EL, Fleischmann KE, Freeman WK, Froehlich JB, Kasper EK, Kersten JR, Riegel B, Robb JF. 2009 ACCF/AHA focused update on perioperative beta blockade incorporated into the ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation. 2009;120:e169–276. doi: 10.1161/CIRCULATIONAHA.109.192690. [DOI] [PubMed] [Google Scholar]
- 2.Akincigil A, Bowblis JR, Levin C, Jan S, Patel M, Crystal S. Long-term adherence to evidence based secondary prevention therapies after acute myocardial infarction. Journal of General Internal Medicine. 2008;23:115–21. doi: 10.1007/s11606-007-0351-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Butler J, Arbogast PG, BeLue R, Daugherty J, Jain MK, Ray WA, Griffin MR. Outpatient adherence to beta-blocker therapy after acute myocardial infarction. Journal of the American College of Cardiology. 2002;40:1589–95. doi: 10.1016/s0735-1097(02)02379-3. [DOI] [PubMed] [Google Scholar]
- 4.Eagle KA, Kline-Rogers E, Goodman SG, Gurfinkel EP, Avezum A, Flather MD, Granger CB, Erickson S, White K, Steg PG. Adherence to evidence-based therapies after discharge for acute coronary syndromes: an ongoing prospective, observational study. American Journal of Medicine. 2004;117:73–81. doi: 10.1016/j.amjmed.2003.12.041. [DOI] [PubMed] [Google Scholar]
- 5.Ho PM, Magid DJ, Masoudi FA, McClure DL, Rumsfeld JS. Adherence to cardioprotective medications and mortality among patients with diabetes and ischemic heart disease. BMC Cardiovascular Disorders. 2006;6:48. doi: 10.1186/1471-2261-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong MCS, Jiang JY, Griffiths SM. Short-term adherence to beta-blocker therapy among ethnic Chinese patients with hypertension: a cohort study. Clinical Therapeutics. 2009;31:2170–7. doi: 10.1016/j.clinthera.2009.10.004. discussion 2150-1. [DOI] [PubMed] [Google Scholar]
- 7.Kain ZN, Sevarino F, Pincus S, Alexander GM, Wang SM, Ayoub C, Kosarussavadi B. Attenuation of the preoperative stress response with midazolam: effects on postoperative outcomes. Anesthesiology. 2000;93:141–7. doi: 10.1097/00000542-200007000-00024. [DOI] [PubMed] [Google Scholar]
- 8.Starkweather AR, Witek-Janusek L, Nockels RP, Peterson J, Mathews HL. Immune function, pain, and psychological stress in patients undergoing spinal surgery. Spine. 2006;31:E641–7. doi: 10.1097/01.brs.0000231795.85409.87. [DOI] [PubMed] [Google Scholar]
- 9.Wallace AW, Au S, Cason BA. Association of the Pattern of Use of Perioperative B-Blockade and Postoperative Mortality. Anesthesiology. 2010;113:794–805. doi: 10.1097/ALN.0b013e3181f1c061. [DOI] [PubMed] [Google Scholar]
- 10.Lederballe Pedersen O, Mikkelsen E, Lanng Nielsen J, Christensen NJ. Abrupt withdrawal of beta-blocking agents in patients with arterial hypertension. Effect on blood pressure, heart rate and plasma catecholamines and prolactin. European Journal of Clinical Pharmacology. 1979;15:215–7. doi: 10.1007/BF00563108. [DOI] [PubMed] [Google Scholar]
- 11.Miller RR, Olson HG, Amsterdam EA, Mason DT. Propranolol-withdrawal rebound phenomenon. Exacerbation of coronary events after abrupt cessation of antianginal therapy. New England Journal of Medicine. 1975;293:416–8. doi: 10.1056/NEJM197508282930902. [DOI] [PubMed] [Google Scholar]
- 12.London MJ. Perioperative beta-blockade, discontinuation, and complications: do you really know it when you see it? Anesthesiology. 2009;111:690–4. doi: 10.1097/ALN.0b013e3181b6a79f. [DOI] [PubMed] [Google Scholar]
- 13.Group PS, Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC, Xavier D, Chrolavicius S, Greenspan L, Pogue J, Pais P, Liu L, Xu S, Malaga G, Avezum A, Chan M, Montori VM, Jacka M, Choi P. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371:1839–47. doi: 10.1016/S0140-6736(08)60601-7. see comment. [DOI] [PubMed] [Google Scholar]
- 14.Morgan RO, Teal CR, Reddy SG, Ford ME, Ashton CM. Measurement in Veterans Affairs Health Services Research: veterans as a special population. Health Services Research. 2005;40:1573–83. doi: 10.1111/j.1475-6773.2005.00448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akhtar S, Assaad S, Amin M, Holt NF, Barash PG, Silverman DG. Preoperative beta-blocker use: impact of national guidelines on clinical practice. Journal of Clinical Anesthesia. 2008;20:122–8. doi: 10.1016/j.jclinane.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 16.Hepner DL, Correll DJ, Beckman JA, Klickovich RJ, Park KH, Govindarajulu U, Bader AM. Needs analysis for the development of a preoperative clinic protocol for perioperative beta-blocker therapy. Journal of Clinical Anesthesia. 2008;20:580–8. doi: 10.1016/j.jclinane.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Kolodner DQ, Do H, Cooper M, Lazar E, Callahan M. Lack of adherence with preoperative B-blocker recommendations in a multicenter study. Journal of General Internal Medicine. 2006;21:596–601. doi: 10.1111/j.1525-1497.2006.00408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]