Abstract
Objectives
To document the stability, concurrent validity and clinical correlates of two fatigability severity measures as recommended by the American Geriatrics Society.
Design
Descriptive, cross-sectional.
Setting
Two independent-living and one community senior centers.
Participants
43 volunteers, average age 85 ± 6 years.
Measurements
Perceived fatigability severity was quantified by directly asking subjects to report change in energy following a standardized 10-minute walk at self-selected pace. Performance fatigability severity was defined as a ratio of change in walking speed and total distance walked. The walk test was repeated within two weeks to assess stability. Total daily physical activity (PA) was measured over seven consecutive days using waist-worn accelerometer. Frailty was measured with the VES13 interview scale and gait speed was measured using standardized 25-feet walk test.
Results
The perceived and performance fatigability severity measures were significantly correlated (r=.94, p<01) and stable over two assessments (r= .82 and .85, respectively p<.01). Both fatigability severity measures were significantly correlated with PA level (r=−.42 and −.44, respectively p<.05), frailty (r=.47 and .53, respectively p<.01) and gait speed (r= −.45 and −.54 respectively, p<.01.).
Conclusion
The methodology described in this study permits the calculation of two highly correlated fatigability severity scores, which summarize the relationship of a person’s change in self-reported tiredness or change in physical performance to concurrently measured PA. The fatigability severity scores are reproducible and correlated with clinical measures predictive of decline. The methods used to quantify fatigability severity can be implemented during a brief assessment (< 15 minutes) and should be useful in the design and evaluation of interventions to increase PA in older adults at risk for functional decline.
Keywords: fatigability, physical activity, elderly
INTRODUCTION
Fatigue is a common problem among people with chronic disease and a key component to definitions of frailty. However, the reported prevalence of fatigue among adults varies widely across studies (5–50%) which suggests inconsistencies in how this subjective, but clinically important, symptom is measured 1. Traditional methods of measuring fatigue generally ask subjects to self-report from memory their global feelings of tiredness or their fatigue levels during physical activities, such as stair climbing.
Mixed results also have been reported about the effects of aging on fatigue, with some studies reporting no more fatigue in older populations 2. The lack of a consistent trend for older adults to report more fatigue is surprising given the clear trend for older adults to show lower levels of physical activity (PA) with increased age 3. Increased fatigue should be at least one factor that intuitively is related to the lower PA that occurs with aging.
It has been hypothesized that these discrepancies between PA trends and self-reported fatigue measures may exist because older adults reduce their PA levels to maintain perceived fatigue levels within an acceptable range. This would explain why older adults reduce their PA and why they do not report higher levels of fatigue than more active younger or healthier adults4.
The relationships between PA level and changes in fatigue during an activity define the concept of fatigability. People who become more fatigued at lower levels of PA have more severe fatigability and, as a consequence, may be more sedentary. A recent American Geriatrics Society (AGS) conference called for the development of fatigability severity measures that will place fatigue in the context of PA and which will discriminate among different levels of fatigability severity4. We define the term fatigability severity in this paper as differences between people in the activity level that leads to increased fatigability and we demonstrate a practical method to quantify fatigability severity. It is thought that measuring changes in perceived fatigue and performance that occur concurrently with PA could be an objective and useful approach to understanding why people limit their PA.
A standardized performance assessment, such as a 10-minute walk, allows for the simultaneous measurement of two independent measures of fatigability severity: (1) self-reported change in tiredness (perceived fatigability) and (2) change in physical performance (e.g. decreased walking speed, or performance fatigability). These two fatigability severity measures are based on different data sources (subjective self-report and objective performance, respectively) and a correlation between these measures would offer evidence of concurrent validity for the construct of fatigability. Specifically, one would expect that changes in perceived fatigue should be associated with simultaneous changes in physical performance if both measures reflect lower capacity for PA. However, it was also acknowledged in the AGS conference that there was little known about the issues involved with measuring either type of fatigability and that these issues would have to be addressed prior to clinically relevant research 4.
The current study had two methodological objectives consistent with those recommended in the AGS conference:
Describe the association, or concurrent validity, of perceived and performance fatigability severity measures collected during a standardized walking assessment and the stability of these measures.
Provide preliminary information about the clinical correlates, of the fatigability severity measures.
METHODS
Subjects and Setting
Study participants were recruited from two independent living facilities that housed approximately 200 residents at the time of the study and one local community senior center. Forty-three older adults volunteered to participate after hearing a discussion of the project at a group meeting. Recruitment procedures were approved by the university-affiliated institutional review board. Inclusion criteria required subjects to be: English-speaking, older than 65, able to provide informed self-consent, and walk without human assistance (i.e., walking aides, such as canes or walkers, were permitted). Participants who volunteered for the study were screened by research staff for eligibility
Fatigability Measures
Two fatigability severity measures were calculated during a standardized 10-minute walking assessment conducted in each research site. Perceived fatigability severity was measured based on the change a subject perceived in their self-reported energy level over time at the point they stopped walking. Performance fatigability severity was measured based on the change in each subject’s walking speed and, thus, did not require a self-report. Both change measures were then divided by the distance each subject walked to calculate perceived and performance fatigability severity. This method of calculating a ratio of change in perceived fatigue or change in physical performance and an estimate of the performed activity level (i.e., distance walked) is consistent with the recommendations made in the AGS conference 4 to measure fatigability severity.
Subjects were asked to walk at their self-selected pace for up to 10 minutes. In one setting the subjects walked on a 170 foot long hall and in two sites in a large room which allowed for the walk to be circular. In all sites the goal was to minimize the number of turns required. We chose a walking assessment based on the person’s self-selected, or normal, gait speed for two reasons. First, walking is a primary component of PA that defines non-sedentary behavior and it is the single most important PA recommended for elderly people due to its relationship with better health. It is thus important to study how fatigability may limit walking at the levels recommended for preventive health benefits (e.g. 30 minutes per day) 5. Secondly, self-selected walking speed is predictive of health outcomes (e.g., mortality); thus, it is clinically meaningful to understand the factors that may affect normal gait speed, such as fatigability 6.
Prior to the walking assessment, each participant was asked to rate their current level of tiredness (e.g., “How tired are you right now?”) on a seven-point scale from 7 (extremely tired) to 1 (extremely energetic). This subjective rating was considered a measure of fatigue because it did not involve a rating of change in tiredness nor was it evaluated in the context of PA. Each participant was then asked to rate their change in tiredness on a similar seven-point scale following 10 minutes of walking, or when they stopped walking if before 10 minutes ( 10 individuals stopped before 10 minutes )
Table 1 illustrates the fatigue and fatigability self-report questions. Briefly, subjects were asked at 10 minutes or when they stopped walking, “Are you more or less or at the same energy level as when started walking?” A score of 4 was assigned if there was no change in their perceived energy level. If the subject reported they had less energy, they were asked if they were extremely, somewhat or a little more tired. If they reported having more energy, they were asked if they were extremely, somewhat or a little more energetic. This branching question format was tested in preliminary work and found to be less confusing to elders than asking for a rating across the full seven-point scale of energy change.
Table 1.
Fatigue and Fatigability Scales
| (Before Walking Test) | (After Walking Test) | |
|---|---|---|
| Fatigue ScaleItems | Score | Fatigability Scale Items |
| Extremely tired | 7 | Extremely more tired |
| Somewhat tired | 6 | Somewhat more tired |
| Alittle tired | 5 | A little more tired |
| Neither tired nor energetic | 4 | Neither more tired or energetic |
| Alittle energetic | 3 | A little more energetic |
| Somewhat energetic | 2 | Somewhat more energetic |
| Extremely energetic | 1 | Extremely more energetic |
Perceived Fatigability Severity
Perceived fatigability severity was measured by dividing each subject’s perceived rating of change in tiredness by the number of meters walked. Thus, a subject who reported being “a little more tired” and who walked 100 meters would have a fatigability severity score of 5 (see Table 1) divided by 100, or .05. A subject who reported a similar level of change in tiredness but who walked 200 meters would generate a fatigability severity score of .025 such that a higher score indicated greater fatigability severity. The difference in scores places the fatigue ratings in the context of walking PA and differentiates between someone who is able to walk twice as far before reporting the same change in fatigue as another person.
We did not use a treadmill for the walking assessment, which would have simplified the fatigability severity calculations by assuring that all people walked the same speed and distance. In this latter case, a ratio of change in tiredness to distance walked would not be necessary because the work performed would be standardized for all participants. We did not use the treadmill for three reasons. First, this population was highly variable in gait speed, and many had balance problems which would make the treadmill set at a standard speed unsafe. Second, we were interested in a measure of fatigability as it occurs during normal daily living conditions and a treadmill does not mimic normal walking. Third, a treadmill would not allow for a change in speed calculation and, hence, performance fatigability score.
Performance Fatigability Severity
Performance fatigability measures the change in an individual’s performance in the context of PA. To calculate performance fatigability severity, the distance that a person walked was calculated at 2.5 minute intervals during the 10-minute walk or until the subject stopped walking. Thus, walking speed could be calculated in meters-per-second at different segments of the walk by dividing distance walked by time. Percent changes in walking speed from the first 2.5 minute interval to the walking speed over the entire distance a subject walked during the 10-minute assessment defined the numerator of the statistic to calculate performance fatigability severity.
The formula used was speed over the full time walked divided by speed in first 2.5 minutes. Thus, if a subject showed no change in speed over the distance walked then they would be at 100% of their speed in the first 2.5 minutes. If the speed over the distance walked was .80 meters per second and their speed in the first 2.5 minutes was .82 meters per second then the change in speed would be .8 divided by .82 or .98. This number was then divided by total distance walked to place the change in performance in the context of PA as done with perceived fatigability severity. Thus, if two people showed a similar change in speed (.50) but walked different distances (100 versus 200 meters) they would have different fatigability severity scores (.50 / 100 = .005 versus .50 / 200 = .0025).
Perceived and performance fatigability severity scores were both calculated during each walking assessment and repeated during a second assessments separated by approximately two weeks per participant. Perceived and performance fatigability severity scores were multiplied by 1000 for reporting purposes. We hypothesized that perceived and performance fatigability severity measures would be significantly inter-correlated within each assessment, which reflects concurrent validity. We also hypothesized that each measure would be significantly intra-correlated across the two assessments indicating stability of the measures.
Clinical Measures
Three measures known to be predictive of health outcomes also were collected to determine their association with the fatigability measures to estimate the potential clinical importance, , of the fatigability measures.
Frailty
The VES13 is an interview instrument that generates a frailty score from 0–10 with higher scores indicating increased frailty. The score is generated by a combination of age, self-reported health and functional disabilities and does not include a fatigue item. The VES13 is highly predictive of both functional decline and mortality 7. It was hypothesized in this study that subjects with higher fatigability severity would score higher on the VES13 indicating that they were at increased risk for health decline.
Gait speed
Self-selected gait speed, as expressed in meters walked-per-second, has been shown to be highly predictive of both functional decline and mortality when measured over 4–8 meters6. Lower gait speeds and, in particular, a gait speed below.80 meters-per-second is associated with poor health outcomes. Self-selected gait speed has been recommended as a simple performance screening measure for older adults. Gait speed in meters-per-second was measured over 25 feet (7.62 meters) during both walking assessments in this study.
Physical Activity
Lower levels of PA are associated with adverse health outcomes. PA was measured over seven consecutive days (average 6.2 days) with Actigraph GT3X triaxial accelerometer worn on the waist dominant side. The walking assessments were completed on days when the accelerometers were not being worn. The total number of activity counts, divided by the total time a subject wore the device was used as the measure of PA. The counts are monitor-specific raw values reflecting movement of a person wearing it and comparable across the same study protocols. The counts can be used to predict physiological variables such as energy expenditure with population specific algorithms or calculate time spent in sedentary, light, moderate, or vigorous intensity physical activity. Participants were offered the option of not wearing the accelerometers and 28 people of the 41 who completed all other study assessments wore the accelerometer for 7 complete days during waking hours.. We hypothesized that participants who became fatigued at lower levels of activity during the walking assessment also would have lower levels of overall PA, as measured by the accelerometer.
Relationship of Fatigue to Fatigability
One of the primary justifications given for the development of fatigability measures in the AGS conference is that these measures may be more sensitive to interventions to increase PA than traditional fatigue measures. We do not provide data directly relevant to this hypothesis, but we did measure the relationship of traditional fatigue measures to fatigability because they intuitively measure similar constructs and one previous study reported they were not correlated 8. In addition to the self-reported tiredness measure collected prior to the 10-minute walking assessment and which measured current fatigue (Table 1, 7-point fatigue rating scale) the Fatigue Severity Scale (FSS) interview scale also was used 9. This is a widely used interview scale which measures the effect of fatigue on daily living. Subjects rate nine items (e.g. exercise brings on my fatigue) from 1 (completely disagree) to 7 (completely agree). The average rating across all 9 items is used to summarize fatigue severity with average scores above 4 considered to reflect significant fatigue.
Statistics
We were primarily interested in establishing the stability as well as the potential concurrent and predictive validity of the two fatigability severity measures. We thus used simple correlational measures (Pearson) as recommended in the literature 10.
RESULTS
Table 2 shows the characteristics of the study participants whose average age was 85 (± 6). They were predominately female (72%) and Caucasian (100%). There was a wide range on most measures, but 81% met criteria for frailty (≥ 3 on the VES13) and showed generally slow gait speeds. Thirty-seven percent also met the Fatigue Severity Scale criteria for significant fatigue (FSS score > 4) and 28% also indicated they were “somewhat” or “a little tired” immediately before the walking test.
Table 2.
Characteristicsof Participants (N=43)
| Measures | N | Mean (±SD) or Percent (n) | Range |
|---|---|---|---|
| Age (years) | 42 | 85.33 (±5.90) | 72–96 |
| Percent Female | 43 | 72.1 (31) | |
| Percent White | 43 | 100 (43) | |
| Gait Speed (Meters/Second) | 43 | 0.65 (±0.20) | 0.25–1.27 |
| Vulnerable Elders Survey Total Score (VES) | 36 | 5.10 (± 3.00) | 0–10 |
| VES >= 3 | 36 | 80.6% (29) | |
| Total Counts/Minute Per Day( accelerometer) | 29 | 100.51 (±75.17) | 20.37–335.85 |
| Performance Fatigability* | 43 | 3.50 (±2.60) | 1.19–13.34 |
| Perceived Fatigability* | 43 | 21.04 (±24.00) | 2.36–137.52 |
| Tired Today scale | 43 | 3.09 (± 1.70) | 1–7 |
| Tired Today>= 5 | 43 | 27.9% (12) | |
| Fatigue Severity Scale Interview Score (FSS) | 35 | 3.60 (± 1.55) | 1.00–6.30 |
| FSS>4 | 35 | 37.2% (16) |
Multiplied by 1000; SD = Standard Deviation; VES = Vulnerable Elder Survey with scores above 3 indicating frailty; FSS = Fatigue Severity Scale with scores above 4 indicating significant fatigue. Differences in N’s primarily reflect subject refusal to participate in a particular assessment.
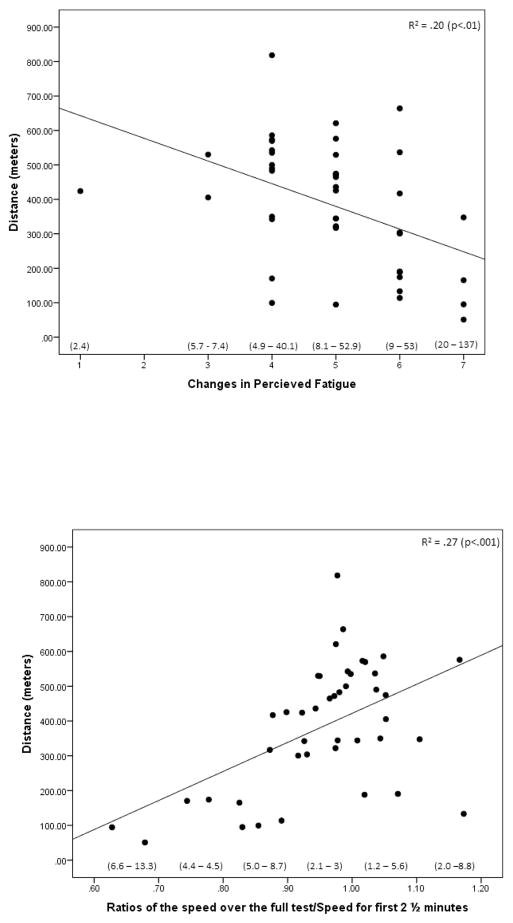
Figure 1 illustrates the relationship between reported changes in energy (upper panel) or change in speed (lower panel) and distance walked. The range in fatigability severity scores generated from these data for different data points along the abscissa in both graphs is also illustrated. There was considerable between-subject variability in distance walked for subjects who reported the same change in energy or who demonstrated similar changes in speed which translates into variability in fatigability severity scores. However, as demonstrated by the statistically significant regression lines, people who slowed the most and who reported higher changes in fatigue also tended to walk the shortest distances which generated higher perceived and performance fatigability severity scores. The correlations between the change in speed or change in perceived energy and distance walked was .52 and −.44 respectively ( p<.003)
Figure 1.
Relationship of distance walked to changes in perceived fatigue orchange of speed.
Upper panel shows relationship of distance walked to reported changes in energy level (7 Point scale). Lower panel shows relationship of distance walked to change in speed. Range of Fatigability severity scores shown in ( ) for subjects reporting each level of energy change (perceived fatigability -upper panel) or change in speed (performance fatigability -lower panel).
Seven subjects were lost from the first to the second walking assessment due to a change in health condition (5) or consent withdrawal (2). The performance fatigability and perceived fatigability severity measures were highly correlated between assessment one and two for the remaining 36 subjects (r = .85 and .82 respectively, p<.001) indicating stability of the measures. There was also a significant intra-correlation between the performance and perceived fatigability severity measures within each assessment indicating concurrent validity. (r = .94 and .93 respectively, p<.001).
Table 3 illustrates the correlations between the all measures. The two fatigue measures (FSS and “tired today” question) were correlated with both the performance and perceived fatigability severity measures. The Fatigue Severity Scale (FSS) score also was significantly correlated with the VES (r=.54), PA total counts (r=−.50) and gait speed (r= −.50). Both fatigability severity scores were significantly correlated with all clinically relevant measures, as shown in Table 3.
Table 3.
Correlations
| Performance | Perceived | Tired Today | Gait Speed | Activity Counts | FSS | VES | Age | Sex | |
|---|---|---|---|---|---|---|---|---|---|
| Performance | 1.00 | .94** | .59** | −.54** | −.44* | .53** | .49** | −.14 | −.29 |
| Perceived | 1.00 | .49** | −.45** | −.42* | .47** | .41** | −.14 | −.30* | |
| Tired Today | 1.00 | −.32 | −.37* | .48** | .26 | −.01 | −.03 | ||
| Gait Speed | 1.00 | .54** | −.50** | −.46** | −.01 | .05 | |||
| Avg. Counts | 1.00 | −.50* | −.45* | −.41* | .30 | ||||
| FSS | 1.00 | .54** | −.13 | −.14 | |||||
| VES | 1.00 | .23 | −.01 | ||||||
| Age | 1.00 | −.17 | |||||||
| Sex | 1.00 |
P< .01;
P< .05
PA = Physical Activity counts (based on accelerometer)
FSS = Fatigue Severity Score
VES = Vulnerable Elders Survey
DISCUSSION
This study demonstrated a feasible method to generate two independent measures of fatigability severity that summarize the relationship of change in performance and perceived energy level to the amount of walking activity. The two fatigability severity measures were highly correlated and stable over two assessments, which suggest that these measures offer a concurrently valid and reproducible method of assessing the same, or highly related, constructs. In addition to reproducibility, the potential usefulness of the fatigability measures for clinical research is supported by their significant correlation with all three clinical measures, each of which is predictive of health decline. Taken together, these findings support the AGS conference statement that underscores the need to develop measures of fatigability for use in future clinical research.
This method of measuring perceived fatigability was developed for this study due to the absence of published studies validating an alternative method. The one published study in this area asked people to self-report fatigue on a four-point scale at different intervals during their normal daily living activities and then calculated the difference in the fatigue ratings between two time points as the measure of fatigability 8. This approach might have been applicable to the current study but, instead, participants were asked directly about their change in tiredness or energy level because “change” represents the key element that differentiates fatigue and fatigability and, as such, this approach has face or content validity.
We did not use a treadmill to standardize speed and distance walked for reasons discussed in the method section. However, the absence of standardization on these variables created problems in calculating the change in speed variable necessary to estimate performance fatigability. The method we used, which measured the ratio of overall speed compared to speed in first 2.5 minutes, is primarily limited by the fact that the same absolute change in speed would produce a different percentage change result for a person who started out walking slower as compared to one who walked faster. Using the speed in the last 2.5 minutes that someone walked instead of overall speed across the entire time a person walked produced similar results to those reported in this paper and has the same limitation. In addition, calculating speed for people who stopped before 10 minutes added another step to the calculation of speed in the last partial interval they walked.
Alternatively, using the absolute change in speed to estimate performance fatigability was primarily limited by the fact that two people who walked very different distances both showed “0” change in speed. In these cases a fatigability severity statistic which would capture the different work performed by these two individuals could not be calculated since any division into “0” would produce a “0” severity ratio.
There are limitations to any method to calculate change in walking speed when people are allowed to self-pace as they were in this study but it does not appear feasible to use an alternative approach with an elderly population who varies widely on normal gait speeds and safety issues.
The fatigability severity measures described in this study despite their limitations appear to be relevant to research to evaluate interventions to improve PA. There are at least two advantages of the fatigability measures for intervention research. First, the methodology described in this study is easy to implement and generates both a subjective (perceived) and objective (performance) measure of fatigability severity. The high correlation between the two measures provides some support for the validity of both measures and corrects for the limitations of any one approach, such as the potential for bias in self-report or limiting performance for reasons unrelated to fatigue (e.g., boredom). Second, the measures are proximal to important changes that occur concurrently with PA and, thus, should serve as sensitive outcome measures to evaluate interventions to enhance PA. For example, during a supervised walking intervention, both fatigability severity measures could be monitored during each exercise session with minimal expense. Measures of fatigability during each exercise session could provide timely feedback about intervention effects, which is optimal for individualizing intervention intensity (e.g. changing duration of walking exercise sessions based on changes in fatigability).
Despite the above methodological advantages, we cannot make the case that fatigability severity measures are causally related to PA or even that a person would report different changes in fatigue if they walked shorter or longer distances than those demonstrated within the 10 minute time frame used in this study. This argument would require an intervention that gradually expanded walking times, and which included fatigability severity, and PA measures as outcomes. It is also notable that FSS and fatigability severity measures had comparable correlation with PA in our study. This suggests that future interventional studies examining comparative utility of these measures as surrogate outcomes are warranted. In this regard, it is also not clear if it is useful to calculate fatigability severity by dividing changes in speed or perceived energy level by distance walked. The conceptual advantages to this approach have been discussed but this step does add a complexity to the calculations. Future work should compare the clinical utility of this methodology to simply measuring change in speed or perceptions of fatigue over a standardized walk without considering the distance walked.
The study is limited by the small number of participants, a 100% Caucasian sample, and the absence of an intervention to demonstrate the causal link between fatigability severity and PA but it does provide sufficient evidence to support more research utilizing the described methodology to measure fatigability. The next step would be to evaluate fatigability severity and its relationship to fatigue and clinical outcomes in a wider range of subjects, including those who suffer from conditions such as chronic kidney disease or congestive heart failure in which fatigue and low PA are common problems. One goal would be to identify the physiological mechanisms underlying the disease that may affect fatigability severity and PA. Participants who show low PA and high fatigability severity could be targeted for pilot interventions designed to decrease fatigability severity and increase PA level. The extent to which fatigability severity measures inform how interventions should be individualized based on the level of physical activity a person is capable of before experiencing intolerable fatigability and are also sensitive outcomes related to increased free living PA could then be evaluated.
In addition, the physiological mechanisms that underlie fatigability or improvements in PA that result from improving fatigability could be identified with bioenergetics measures. A comparison of a fatigability severity measure using distance walked as the estimate of energy expenditure could be compared to a fatigability severity measure using a direct measure of energy expenditure to determine if the more precise energy expenditure measures add important information. Knaggs et al in their recent report suggest that people with more disabilities may expend more energy for the same task 11. This finding would provide one plausible explanation for why people reported similar levels of fatigability while walking different distances in this study.
The current paper also focused on fatigability during a walking activity based on the rationale provided earlier that walking frequency and duration is associated with a sedentary lifestyle. Fatigability during other types of activity such as resistance training or cognitive exercise may be controlled by different mechanisms. We have recently reported that, unlike for the walking activity described in this paper, perceived and performance fatigability severity measures are not correlated for tasks that require low EE 12. In short, fatigability is a multidimensional construct and the performance measures described in this paper may not be able to measure aspects of fatigue related to psychological or behavioral issues.
In conclusion, we report the stability and concurrent validity of two newly developed perceived and performance fatigability measures in older adults. Our data indicate that these measures are correlated with validated clinical measures predictive of decline in PA. Thus, the long-term goal is to evaluate these fatigability severity measures during interventions aimed at improving PA in older adults.
Acknowledgments
Sponsor’s Role: MSB was supported in part by CTSA grant UL1 RR024975 and Vanderbilt Diabetes Research and Training Center NIH grant DK2059.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions:
All authors contributed to: Study concept, design, data analysis and manuscript preparation
References
- 1.Lerdal A, Wahl A, Rustoen T, et al. Fatigue in the general population: A translation and test of the psychometric properties of the Norwegian version of the fatigue severity scale. Scand J Public Health. 2005;33:123–130. doi: 10.1080/14034940410028406. [DOI] [PubMed] [Google Scholar]
- 2.Hickie IB, Hooker AW, Hadzi-Pavlovic D, et al. Fatigue in selected primary care settings: sociodemographic and psychiatric correlates. Med J Aust. 1996;164:585–588. doi: 10.5694/j.1326-5377.1996.tb122199.x. [DOI] [PubMed] [Google Scholar]
- 3.Frisard MI, Fabre JM, Russell RD, et al. Physical activity level and physical functionality in nonagenarians compared to individuals aged 60–74 years. J Gerontol A Biol Sci Med Sci. 2007;62:783–788. doi: 10.1093/gerona/62.7.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alexander NB, Taffet GE, Horne FM, et al. Bedside-to-Bench conference: Research agenda for idiopathic fatigue and aging. J Am Geriatr Soc. 2010;58:967–975. doi: 10.1111/j.1532-5415.2010.02811.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Min L, Yoon W, Mariano J, et al. The vulnerable elders-13 survey predicts 5-year functional decline and mortality outcomes in older ambulatory care patients. J Am Geriatr Soc. 2009;57:2070–2076. doi: 10.1111/j.1532-5415.2009.02497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy SL, Smith DM. Ecological measurement of fatigue and fatigability in older adults with osteoarthritis. J Gerontol A Biol Sci Med Sci. 2010;65:184–189. doi: 10.1093/gerona/glp137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herlofson K, Larsen JP. Measuring fatigue in patients with Parkinson's disease - the Fatigue Severity Scale. Eur J Neurol. 2002;9:595–600. doi: 10.1046/j.1468-1331.2002.00444.x. [DOI] [PubMed] [Google Scholar]
- 10.Higgins PA, Straub AJ. Understanding the error of our ways: mapping the concepts of validity and reliability. Nurs Outlook. 2006;54:23–29. doi: 10.1016/j.outlook.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Knaggs JD, Larkin KA, Manini TM. Metabolic cost of daily activities and effect of mobility impairment in older adults. J Am Geriatr Soc. 2011;59:2118–2123. doi: 10.1111/j.1532-5415.2011.03655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buchowski MS, Simmons SF, Whitaker LE, et al. Fatigability as a function of physical activity energy expenditure in older adults. Age (Dordr ) 2011 doi: 10.1007/s11357-011-9338-x. [DOI] [PMC free article] [PubMed] [Google Scholar]