Abstract
The current study reports results from a pilot randomized controlled trial evaluating the feasibility and efficacy of Risk Reduction through Family Therapy (RRFT) for reducing substance use risk and trauma-related mental health problems among sexually assaulted adolescents. Thirty adolescents (aged 13–17 years; M=14.80; SD=1.51) who had experienced at least one sexual assault and their caregivers were randomized to RRFT or treatment as usual (TAU) conditions. Participants completed measures of substance use, substance use risk factors (e.g., family functioning), mental health problems (i.e., posttraumatic stress disorder, depression, and general internalizing/externalizing symptoms) and risky sexual behavior at four time points (baseline, post-treatment, and 3- and 6-month follow-up). Mixed-effects regression models yielded significantly greater reductions in substance use, specific substance use risk factors, and (parent-reported) PTSD, depression, and general internalizing symptoms among youth in the RRFT condition relative to youth in the TAU condition. However, significant baseline differences in functioning between the two conditions warrant caution in interpreting between-group findings. Instead, emphasis is placed on replication of feasibility findings and within-group improvements over time among the RRFT youth.
Keywords: Child Sexual Abuse, Treatment, Substance Use Problems, PTSD, Adolescents
Approximately 2.8 million youth are victims of childhood sexual assault (CSA) in the United States (Finkelhor, Turner, Ormrod, & Hamby, 2009). CSA is associated with early substance use initiation (Rothman et al., 2008), which in turn is strongly linked with later development of alcohol and drug abuse disorders (Kilpatrick et al., 2003). Other sequelae empirically related to CSA among adolescents include Posttraumatic Stress Disorder (PTSD) (Finkelhor et al., 2005), depression (Danielson et al., 2005), and risky sexual behavior (Rotheram-Borus et al., 1996). Epidemiological studies demonstrate that teens who have experienced CSA are over six times more likely to report comorbid PTSD and substance use (SU) disorders than those who do not report CSA (Kilpatrick et al., 2003). Risk for CSA-related mental health and SU problems continues into adulthood (e.g., Danielson et al., 2009).
Trauma-focused psychotherapies have been developed and rigorously evaluated for victims of CSA (e.g., Trauma Focused-Cognitive Behavioral Therapy; TF-CBT), yielding significant reductions in PTSD and other symptoms among youth (Cohen, Deblinger, Mannarino, & Steer, 2004). Nevertheless, existing models do not typically target some of the other clinical problems commonly experienced by this population, namely SU and risky sexual behavior. Failure to address these frequently comorbid issues among CSA victims could result in negative long-term outcomes for youth and their families (Kendler et al., 2000). Recently, experts have called for the development of integrated, family-involved interventions that aim to address CSA victims' mental health symptoms, SU, and other presenting problems concurrently (Cohen et al., 2003). Nevertheless, limited progress has been made in the validation of such integrated approaches.
In an effort to better address the multiple clinical problems commonly experienced by victims of CSA, the authors recently developed an integrated treatment protocol called Risk Reduction through Family Therapy (RRFT; Danielson et al., 2010a). RRFT builds upon the principles and interventions applied in empirically-supported treatments for adolescent SU (Multisystemic Therapy/MST; Henggeler et al., 2002), PTSD and depression (TF-CBT), and other negative sequelae (e.g., risky sexual behaviors; DiClemente et al., 2004). Importantly, the model utilizes exposure-based techniques (i.e., where one learns to gain control of the distress induced by trauma-related cues) from TF-CBT to address youths’ trauma symptoms, as well as involvement of the family, which has been demonstrated to be beneficial in the treatment of youth PTSD (Gilboa-Schechtman et al., 2010) and SU problems (Henggeler et al., 2002). Data from an open pilot suggest that RRFT is feasible and potentially efficacious in reducing risk for SU problems and decreasing PTSD and depression among youth (Danielson et al., 2010a).
The current pilot randomized controlled trial aimed to replicate the feasibility of RRFT and to evaluate the differential efficacy of RRFT and treatment as usual (TAU) in reducing SU problems (including early initiation), mental health symptoms, and risky sexual behavior among adolescent CSA victims. Given that the trial was conducted in a clinic where evidence-based interventions were commonly utilized, we hypothesized that the RRFT and TAU conditions would both yield reductions in symptoms over time. However, we expected RRFT to outperform TAU at reducing SU, SU risk factors (e.g., decreased conflict), and risky sexual behavior given that RRFT specifically targets these areas, whereas standard trauma-focused treatments do not.
Method
Participants
Participants included 30 treatment seeking adolescent CSA victims (mean age=14.8; SD=1.5; range=13–17) and their caregivers (72.6% biological parents, 17.1% other family members, 10.3% non-familial guardians). Approximately 88% of the sample was female, 46% were African American (37.5% white, 4.2% Native American, 8.3% bi-racial, 4% Hispanic), and 70% received Medicaid. Participants were recruited through an urban clinic specializing in the treatment of trauma. Inclusion criteria were youth who: a) were aged 12–17; b) had experienced at least one lifetime CSA that could be recollected by the youth (defined as unwanted/forced vaginal or anal penetration by an object, finger, or penis; oral sex; or touching of one’s genitalia); and c) were not mentally retarded. Nine (30%) reported 2nd, 3rd, and 4th CSA revictimization experiences; age of first/only CSA experience ranged from 4–15; and 23 (67.7%) reported having experienced other traumatic events. Mean time since most recent assault was 3.7 years (SD=3.8).
Procedure
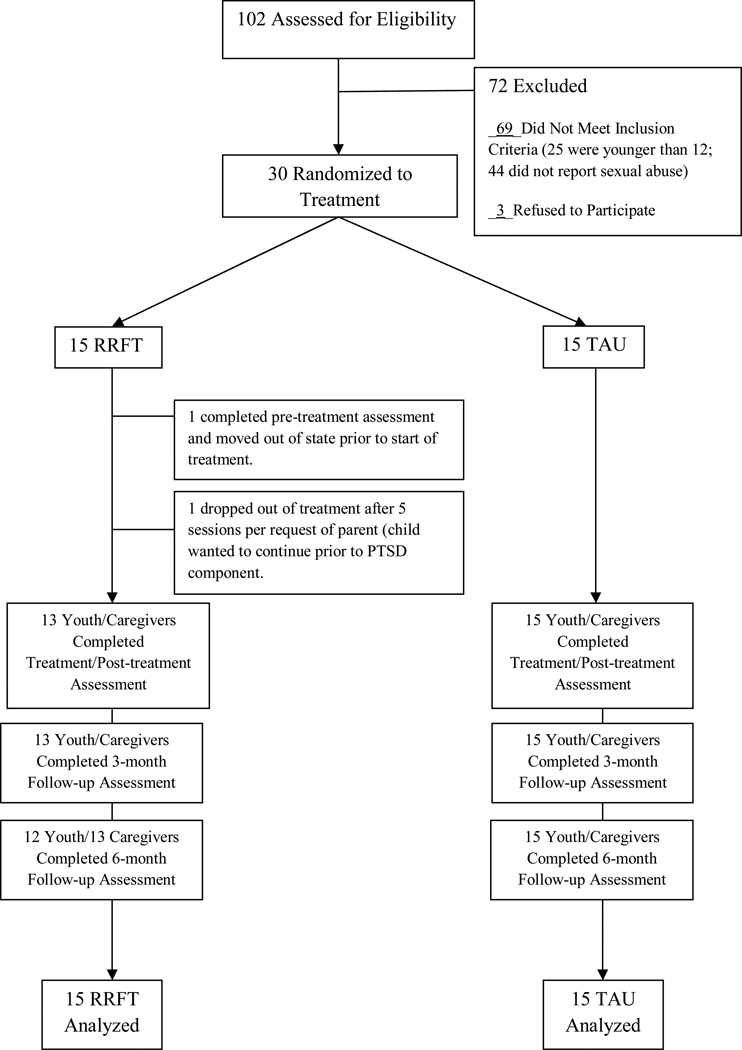
Youth were screened for eligibility through a weekly clinic staffing. Eligible adolescents and their (non-offending) caregivers were approached by a researcher to solicit participation. Of the eligible families, 91% agreed to participate (see Figure 1). Legal guardians provided consent and youth provided assent. Following consent, participants were randomly assigned to condition using a computerized blocked randomization method. Participants then completed a baseline assessment, which included the measures noted below and a urine drug screen. Assessment measures were re-administered at post-treatment, 3-, and 6-month follow-up using a match-timing design, where completion of treatment by a RRFT youth triggered the post-treatment assessment (and timing for the 3-month and 6-month post-treatment assessments) for that youth and his/her matched pair in the TAU condition. Participants were compensated for completing each assessment but were not paid to attend treatment. All procedures were approved by MUSC’s Institutional Review Board, and a certificate of confidentiality was obtained.
Figure 1.
Consort Flow Chart
Treatment Conditions
RRFT
RRFT was developed to reduce risk of SU and other high-risk behaviors and trauma-related psychopathology in adolescents who have experienced CSA. RRFT integrates the nine guiding principles of MST with other empirically-supported interventions with similar theoretical rationales targeting similar populations, including TF-CBT and psychoeducation strategies for prevention of high-risk sexual behavior (e.g., DiClemente et al., 2004) and sexual revictimization (Marx, Calhoun, Wilson, & Meyerson, 2001). The RRFT protocol is devised into 7 treatment components: Psychoeducation, Coping, Family Communication, Substance Abuse, PTSD, Healthy Dating and Sexual Decision Making, and Revictimization Risk Reduction and is administered through weekly, 60–90 minute sessions with adolescents and caregivers (meeting individually with the therapist and as a family). RRFT utilizes a clinical pathways approach that is driven by youth symptomatology (i.e., the order of and time spent on each component is determined by the needs of each youth and family).
Several theories are incorporated into RRFT via multiple intervention strategies. First, RRFT is guided by ecological theory, which proposes that an adolescent’s behavior is influenced by multiple social and environmental contexts, including the family, peer network, school, and community (Bronfenbrenner, 1979). RRFT, like other ecological models (e.g., MST), adopts a family-based approach to intervention and encourages therapists to intervene in multiple social systems. As part of this ecological model, Strategic Family Therapy (e.g., Haley, 1976) is utilized to help the family define problems (in behaviorally specific terms—and from the perspective of both of the adolescent and the caregiver) and work together to solve those problems. The family is involved across all 7 treatment components. Mowrer’s Two-Factor Theory (Mowrer, 1960) and negative reinforcement theory (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004) also are applied in targeting PTSD, SU, and their overlap in RRFT. Additional information about the RRFT model can be found in Danielson et al. (2010a).
Treatment as Usual (TAU)
TAU was selected as the control condition because no empirically-supported integrated interventions for this population currently exist; thus, the research question at hand focused on whether RRFT outperformed the standard care that a CSA victim and family would typically receive when presenting for treatment in the clinic. To better understand the content of therapy received by participants assigned to the TAU condition, clinic chart reviews were performed, and post-treatment responses by youth and caregivers on a standardized services assessment (Services Assessment for Children and Adolescents; SACA; Horwitz et al., 2001) were reviewed; however, no one treatment emerged as being consistently delivered across youth and families assigned to this condition.
Therapist Training/Quality Assurance
Participants were treated by clinical psychology graduate students completing a predoctoral internship. Therapy was delivered through both an outpatient clinic and an outreach program offered at the same clinic (for families without transportation; 4 families in RRFT condition and 3 in TAU condition). The first author, a licensed clinical psychologist and RRFT developer, supervised all RRFT cases. TAU therapists were supervised by other licensed psychologists in the clinic. RRFT therapists received didactic training on the intervention prior to implementation.
Adherence to RRFT was assessed via review of randomly selected audiotaped sessions (two per client per month) by the first author. Given that the control condition was ‘treatment as usual’ (i.e., not one specific protocol), adherence was not monitored systematically in this condition. RRFT treatment adherence also was monitored through weekly individual supervision with the treatment developer. Further, participants were asked to complete an RRFT adherence checklist immediately following each session, which was then reviewed.
Dependent Measures
Mental Health Symptoms
PTSD symptoms were assessed with the UCLA PTSD Index for DSM-IV-Adolescent & Caregiver versions (Steinberg, Brymer, Decker, & Pynoos, 2004). The Child Depression Inventory (CDI; Kovacs, 1983) was used to assess depression symptoms and the Behavioral Assessment System for Children (BASC-2; Reynolds & Kamphaus, 1992) (parent and youth self-report) measured participants’ internalizing and externalizing symptoms. Internal consistency for all measures was high in the current sample (Cronbach’s alphas > .84).
Substance Use and Substance Use Risk Factors
The Time Line Follow Back Interview (TLFB), a well-established method of assessing SU (Sobell & Sobell, 1996), was conducted with each participant to identify specific amounts of alcohol and drugs consumed over the past 90 days. Urine drug screens were collected to validate self-reported SU (i.e., verify that denial of illicit drug use was accurate). The Cohesion and Conflict subscales of the Family Environment Scale (FES; Moos & Moos, 1986) were completed by adolescents and caregivers, as these aspects of family environment have been linked with SU risk. The reliabilities of these subscales have been established (Boyd et al., 1997; Cole & McPherson, 1993).
Risky Sexual Behavior
Two items were used to assess: 1) number of consensual sexual intercourse partners over the past 3 months (including new sexual partners), and 2) whether or not the youth had been diagnosed with a sexually transmitted disease in the past 3 months.
Data Analysis
Data were comprised of four repeated measurements (level-1) nested within 30 families (level-2), yielding a two-level Mixed-Effects Regression Model (MRM). The TLFB score represented the number of days with self-reported SU over the previous 90 days and was modeled as a count-distributed (i.e., Poisson) outcome. A Sexual Partners variable was modeled as a dichotomous (i.e., Bernoulli) outcome indicating whether the adolescent had any new consensual sexual partners over the previous 90 days. The remaining outcomes were modeled as continuous variables. Slopes were modeled using linear polynomials computed from assessment dates (Singer & Willett, 2003). Treatment condition was coded such that RRFT = 0 and TAU = 1. MRMs were performed using HLM software (v. 6.08; Raudenbush, Bryk, Cheong, Congdon, & du Toit, 2004), with restricted maximum likelihood estimation for the continuous outcomes and Laplace estimation for the Poisson and Bernoulli outcomes. Specification of random effects was based on the likelihood ratio test for the continuous outcomes and the Wald test for variance components for the Poisson and Bernoulli outcomes (Singer & Willett, 2003). The Wald test statistic for significance testing was computed using asymptotic standard errors.
According to this model specification, the intercept and slope terms represent the average baseline score and monthly rate of change for youth in the RRFT condition. The condition and condition × linear terms represent the difference between TAU and RRFT at baseline and in the monthly rate of change. Variables representing number of sessions and treatment length were initially included in the MRMs to control for treatment intensity. Conclusions did not differ when intensity was controlled; therefore, results are presented for models without the covariates.
Results
Treatment Descriptives
Mean treatment length for RRFT was 23 sessions (SD=13); mean number of weeks in treatment was 34 (SD=17). Treatment completers were defined as having completed 5 of 7 RRFT components. All but two RRFT participants met this criterion. Based on review of audiotapes, supervision, and fidelity checklists, therapists adhered to the RRFT model 94% of the time. As determined by chart review and the SACA, a variety of interventions (psychoeducation, coping, safety planning, and CBT) were delivered to youth and families assigned to TAU, with no one treatment emerging as being consistently delivered; M number of sessions=13, SD=6; M weeks in treatment=20, SD=9.
Treatment Outcomes
Table 1 includes descriptive data for each outcome. The MRMs yielded significant condition effects on the UCLA PTSD-P, CDI, BASC-Internalizing, TLFB, FES Cohesion (adolescent- and parent-report), and FES Conflict (adolescent-report) scales (see Table 2), reflecting greater impairment among RRFT youth relative to TAU youth at baseline. These baseline differences need to be considered when interpreting the results pertaining to between-group differences on change over time. On the basis of the model building steps, random effects were not modeled for the slope terms reported in Table 2 and summarized below.
Table 1.
Descriptive Data (Mean and Standard Deviation) for each Outcome by Condition and Time
| RRFT |
TAU |
|||||||
|---|---|---|---|---|---|---|---|---|
| Outcome | Baseline | Post | 3-Month | 6-Month | Baseline | Post | 3-Month | 6-Month |
| UCLA PTSD-A | 40.0 (11.1) | 17.9 (12.8) | 23.1 (16.1) | 20.4 (12.7) | 35.6 (19.9) | 22.9 (13.5) | 20.5 (14.6) | 23.8 (17.9) |
| UCLA PTSD-P | 42.8 (14.5) | 15.9 (10.8) | 18.3 (15.5) | 20.5 (15.4) | 26.5 (13.9) | 20.7 (14.2) | 15.9 (8.9) | 19.8 (15.7) |
| CDI | 61.7 (12.7) | 48.1 (8.1) | 49.3 (10.6) | 47.0 (10.3) | 52.9 (10.9) | 47.6 (10.4) | 45.9 (8.8) | 48.4 (13.5) |
| BASC Internalizing | 68.1 (10.9) | 53.7 (10.4) | 51.9 (8.2) | 52.3 (6.6) | 56.6 (7.3) | 50.4 (9.9) | 51.9 (13.3) | 49.0 (7.9) |
| BASC Externalizing | 67.4 (17.9) | 57.4 (11.4) | 53.2 (10.9) | 53.5 (10.9) | 60.9 (13.6) | 54.8 (10.8) | 53.3 (12.9) | 55.7 (14.9) |
| TLFB Days w. Use | 15.9 (31.2) | 2.6 (6.1) | 2.4 (5.8) | 2.5 (5.8) | 0.4 (1.1) | 0.4 (1.3) | 1.6 (4.7) | 4.7 (6.9) |
| Any Sexual Partners | 0.5 (0.5) | 0.2 (0.4) | 0.2 (0.4) | 0.1 (0.3) | 0.5 (0.5) | 0.4 (0.5) | 0.3 (0.5) | 0.1 (0.3) |
| FES Cohesion-A | 38.8 (15.3) | 50.2 (13.0) | 54.4 (9.3) | 51.1 (9.5) | 55.0 (12.2) | 47.9 (16.6) | 49.2 (19.6) | 50.1 (17.7) |
| FES Cohesion-P | 43.3 (19.6) | 57.7 (5.3) | 57.2 (6.2) | 56.6 (7.5) | 58.2 (6.3) | 59.8 (12.2) | 56.8 (9.8) | 57.3 (13.3) |
| FES Conflict-A | 60.7 (9.7) | 43.8 (7.9) | 42.6 (6.5) | 42.9 (7.1) | 49.3 (10.4) | 46.7 (12.2) | 46.2 (14.9) | 48.3 (13.5) |
| FES Conflict-P | 55.7 (14.3) | 43.8 (7.1) | 43.0 (9.1) | 44.2 (9.3) | 48.2 (11.4) | 44.3 (10.9) | 46.3 (12.2) | 42.7 (12.4) |
Note. N = 30. UCLA PTSD-A=UCLA PTSD Index-Adolescent Report; UCLA PTSD-P=UCLA PTSD Index-Parent Report; CDI=Child Depression Inventory; BASC=Behavior Assessment System for Children; TLFB=Timeline Follow-Back; FES=Family Environment Scale.
Table 2.
Mixed-Effect Regression Models for Treatment Outcome Measures
| Outcome | β | SE | df | p | 95% CI | |
|---|---|---|---|---|---|---|
| UCLA PTSD-A | ||||||
| Intercept: | RRFT | 37.24 | 4.02 | 28 | <.001 | (29.36, 45.12) |
| TAU v. RRFT | −4.60 | 5.65 | 28 | 0.422 | (−15.65, 6.45) | |
| Slope: | RRFT | −1.19 | 0.24 | 81 | <.001 | (−1.66, −0.72) |
| TAU v. RRFT | 0.42 | 0.34 | 81 | 0.215 | (−0.25, 1.09) | |
| UCLA PTSD-P | ||||||
| Intercept: | RRFT | 39.09 | 3.66 | 28 | <.001 | (31.92, 46.26) |
| TAU v. RRFT | −12.97 | 5.14 | 28 | 0.018 | (−23.04, −2.90) | |
| Slope: | RRFT | −1.46 | 0.21 | 82 | <.001 | (−1.87, −1.05) |
| TAU v. RRFT | 0.87 | 0.29 | 82 | 0.004 | (0.30, 1.44) | |
| CDI | ||||||
| Intercept: | RRFT | 60.42 | 2.73 | 28 | <.001 | (55.07, 65.77) |
| TAU v. RRFT | −8.54 | 3.83 | 28 | 0.034 | (−16.05, −1.03) | |
| Slope: | RRFT | −0.87 | 0.17 | 81 | <.001 | (−1.20, −0.54) |
| TAU v. RRFT | 0.52 | 0.24 | 81 | 0.036 | (0.05, 0.99) | |
| BASC Internalizing | ||||||
| Intercept: | RRFT | 67.45 | 2.47 | 28 | <.001 | (62.61, 72.29) |
| TAU v. RRFT | −10.71 | 3.44 | 28 | 0.004 | (−17.45, −3.97) | |
| Slope: | RRFT | −1.06 | 0.14 | 81 | <.001 | (−1.33, −0.79) |
| TAU v. RRFT | 0.53 | 0.20 | 81 | 0.008 | (0.14, 0.92) | |
| BASC Externalizing | ||||||
| Intercept: | RRFT | 66.94 | 3.27 | 28 | <.001 | (60.53, 73.35) |
| TAU v. RRFT | −6.43 | 4.52 | 28 | 0.166 | (−15.29, 2.43) | |
| Slope: | RRFT | −0.90 | 0.22 | 81 | <.001 | (−1.32, −0.46) |
| TAU v. RRFT | 0.42 | 0.31 | 81 | 0.181 | (−0.19, 1.03) | |
| TLFB Days w. Use | ||||||
| Intercept: | RRFT | 0.21 | 0.70 | 28 | 0.764 | (−1.16, 1.58) |
| TAU v. RRFT | −2.17 | 1.01 | 28 | 0.040 | (−4.13, −0.21) | |
| Slope: | RRFT | −0.17 | 0.01 | 81 | <.001 | (−0.19, −0.15) |
| TAU v. RRFT | 0.30 | 0.03 | 81 | <.001 | (0.24, 0.36) | |
| Any Sexual Partners | ||||||
| Intercept: | RRFT | −0.04 | 0.56 | 27 | 0.948 | (−1.14, 1.06) |
| TAU v. RRFT | 0.37 | 0.76 | 27 | 0.633 | (−1.12, 1.86) | |
| Slope: | RRFT | −0.12 | 0.05 | 82 | 0.026 | (−0.22, −0.02) |
| TAU v. RRFT | −0.01 | 0.07 | 82 | 0.912 | (−0.15, 0.13) | |
| FES Cohesion-A | ||||||
| Intercept: | RRFT | 40.16 | 3.78 | 28 | <.001 | (32.75, 47.57) |
| TAU v. RRFT | 12.80 | 5.31 | 28 | 0.023 | (2.39, 23.21) | |
| Slope: | RRFT | 0.76 | 0.21 | 81 | 0.001 | (0.35, 1.17) |
| TAU v. RRFT | −1.03 | 0.30 | 81 | 0.001 | (−1.62, −0.44) | |
| FES Cohesion-P | ||||||
| Intercept: | RRFT | 45.25 | 2.74 | 28 | <.001 | (39.88, 50.62) |
| TAU v. RRFT | 12.27 | 3.81 | 28 | 0.003 | (4.80, 19.74) | |
| Slope: | RRFT | 0.85 | 0.21 | 82 | <.001 | (0.44, 1.26) |
| TAU v. RRFT | −0.79 | 0.30 | 82 | 0.010 | (−1.38, −0.20) | |
| FES Conflict-A | ||||||
| Intercept: | RRFT | 58.69 | 2.72 | 28 | <.001 | (53.36, 64.02) |
| TAU v. RRFT | −9.15 | 3.80 | 28 | 0.023 | (−16.60, −1.70) | |
| Slope: | RRFT | −1.13 | 0.19 | 81 | <.001 | (−1.50, −0.76) |
| TAU v. RRFT | 0.92 | 0.27 | 81 | 0.001 | (0.39, 1.45) | |
| FES Conflict-P | ||||||
| Intercept: | RRFT | 54.70 | 2.72 | 28 | <.001 | (49.36, 60.02) |
| TAU v. RRFT | −6.44 | 3.81 | 28 | 0.102 | (−13.91, 1.03) | |
| Slope: | RRFT | −0.79 | 0.17 | 82 | <.001 | (−1.12, −0.46) |
| TAU v. RRFT | 0.47 | 0.25 | 82 | 0.058 | (−0.02, 0.96) | |
Note. N = 30. UCLA PTSD-A=UCLA PTSD Index-Adolescent Report; UCLA PTSD-P=UCLA PTSD Index-Parent Report; CDI=Child Depression Inventory; BASC=Behavior Assessment System for Children; TLFB=Timeline Follow-Back; FES=Family Environment Scale.
Mental Health
The MRMs yielded significant negative linear effects on the UCLA PTSD-P, CDI, and BASC Internalizing scales, indicating that RRFT youth demonstrated decreased parent-reported PTSD and adolescent-reported depression and internalizing symptoms from baseline to 6-month follow-up. In addition, the condition × linear effects on these outcomes were positive and significant, indicating that RRFT youth evidenced greater reductions in these symptoms relative to their TAU counterparts. For the UCLA PTSD-A and BASC Externalizing scales, there were significant negative linear effects but no condition × linear effects. Thus, the RRFT and TAU groups evidenced similar reductions on these scales over time.
Substance Use
The Poisson MRM yielded a significant negative linear effect on the TLFB outcome, indicating reduced days of SU from baseline to 6-month follow-up for youth in the RRFT condition. The condition × linear effect was positive. Thus, in contrast to TAU youth, RRFT youth reported greater reductions in SU over time.
Substance Use Risk: Family Functioning
MRM analyses yielded significant positive linear effects on the adolescent- and parent-report versions of the FES Cohesion scale, reflecting increased cohesion for RRFT families from baseline to 6-month follow-up. The significant negative condition × linear effects on these scales indicate that RRFT participants reported greater increases in cohesion relative to TAU participants. In addition, results revealed significant negative linear effects on the adolescent- and parent-report versions of the FES Conflict scale, reflecting decreased conflict for RRFT families. The condition × linear effect was significant on the adolescent-report version of this scale, providing some evidence that in contrast to TAU participants, RRFT participants evidenced greater reductions in family conflict.
Sexual Behavior
For the Sexual Partners outcome, the Bernoulli MRM revealed a significant negative linear effect but no condition × linear effect, indicating that the two groups evidenced similar reductions in the likelihood of new sexual partners over time. In absolute terms, RRFT youth reported fewer new sexual partners (42% RRFT vs. 60% TAU) and fewer STDs (8% RRFT vs. 27% TAU) at any given post-treatment assessment. Although these differences were not significant (per logistic regression analyses, p’s > .05), the data suggest this is an area for further development of the RRFT manual and an area for future research.
Discussion
Building upon promising results from an open pilot feasibility trial (Danielson et al., 2010a), the current study compared RRFT to TAU to determine whether the approach can be efficacious in reducing risk for SU problems, PTSD, and other related outcomes. Consistent with hypotheses, adolescents who received RRFT reported reduced SU and improvements in SU risk factors (e.g., increased family cohesion). Also as expected, participants in both conditions experienced reductions in PTSD and depression symptoms, although greater reductions were found for adolescents in the RRFT condition with regard to parent-reported PTSD, as well as adolescent-reported depression and internalizing symptoms. However, randomization failed to prevent inequality at baseline across the two conditions. Thus, caution should be utilized when interpreting the between-group differences. Of emphasis, within-group findings, which support the feasibility of RRFT and provide evidence that youth and families who received the intervention improved on key outcomes, are encouraging and support next research steps.
Adolescence is a developmental period marked with increased risk for experimentation with alcohol and illicit drugs. Adolescents with a CSA history are even more vulnerable to early onset SU and abuse. Thus, the improvements over time in SU and SU risk for the RRFT youth are noteworthy. Specifically, RRFT youth reported significantly more SU than TAU youth at baseline, but reported less use at each follow-up assessment. Although the baseline differences represent a salient limitation of the study, the increase in SU among TAU youth over time may be informative. Early SU initiation is linked with a host of costly SU problems among adolescents and adults. Thus, the identification of treatment strategies that can effectively delay initiation of SU would be useful. Indeed, the risk reduction approach taken in RRFT is consistent with recent arguments for future directions in psychotherapy research and practice, which include avoiding onset or reducing the severity of onset of mental illness (including substance abuse)—thereby reducing incidence and need for treatment (Kazdin & Blase, 2011).
Limitations of the current study should be noted. The primary limitation is that, despite rigorous randomization procedures, baseline differences existed between RRFT and TAU across most variables. This was likely due to the small sample size and the unrestrictive inclusion criteria, which permitted both substance using and non-substance using youth to participate (i.e., to capture a ‘real world’ adolescent CSA sample). Although this heterogeneity in symptom presentation among study participants is representative of the multiple trajectories of adolescents with a CSA history (Danielson et al., 2010b), which drove study design decisions to focus on this high risk population rather than a particular diagnosis, future studies will need to ensure equality on key variables across the two conditions. Similarly, dosage differences existed between the two conditions, where RRFT youth received more sessions on average than TAU youth. Analyses indicated that dosage was not significantly associated with any of the outcome variables. Nonetheless, an important future direction will involve use of an attention-matched control condition, as well as a much larger sample size to allow for an examination of mediators and/or moderators that may speak to RRFT’s ‘active ingredients.’ Finally, while the flexibility of offering treatment outside of the office can be viewed as a strength and representative of the real world barriers faced by many clients, this introduces another layer of heterogeneity within the sample and thus ‘noise’ when drawing conclusions about treatment efficacy.
Although several studies have demonstrated the efficacy of exposure-based approaches in the treatment of youth with PTSD, this is one of the first studies to examine its utility among a small number of youth who also were using substances at the onset of treatment. Thus, an important clinical implication is that exposure to trauma-related cues can be useful with youth who are also receiving treatment for SU-related problems. Given the small sample size and heterogeneity in pre-treatment SU behavior among the participants, additional research is needed to pursue this empirical question. If further support is found for its efficacy, RRFT could improve clinical practice by offering families a more efficient alternative to the current compartmentalized approach to treatment of this population, as well as a risk-reduction option for youth at elevated risk for developing substance abuse and related mental health problems in the future, but who are not currently meeting diagnostic thresholds.
Acknowledgments
The study was supported by grant award K23DA018686 from the National Institute on Drug Abuse (NIDA; PI: Danielson) and a Young Investigator Award from NARSAD (PI: Danielson). The views, policies, and opinions expressed in this article are those of the authors and do not necessarily reflect those of NIDA or NARSAD. Special thanks to the families who participated in this study and to Lauren Silcott Doherty and Stephanie Miller for their diligence in working on this project.
References
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Boyd CP, Gullone E, Needleman GL, Burt T. The Family Environment Scale: Reliability and normative data for an adolescent sample. Family Process. 1997;36:369–373. doi: 10.1111/j.1545-5300.1997.00369.x. doi: 10.1111/j.1545-5300.1997.00369.x. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:393–402. doi: 10.1097/00004583-200404000-00005. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino A, Zhitova AC, Capone ME. Treating child abuse-related posttraumatic stress and comorbid substance abuse in adolescents. Child Abuse & Neglect. 2003;27:1345–1365. doi: 10.1016/j.chiabu.2003.08.001. doi: 10.1016/j.chiabu.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Cole DA, McPherson AE. Relation of family subsystems to adolescent depression: Implementing a new family assessment strategy. Journal of Family Psychology. 1993;7:119–133. doi: 10.1037/0893-3200.7.1.119. [Google Scholar]
- Danielson CK, Amstadter AB, Dangelmaier RE, Resnick HS, Saunders BE, Kilpatrick DG. Trauma-related risk factors for substance abuse among male versus female young adults. Addictive Behaviors. 2009;34:395–399. doi: 10.1016/j.addbeh.2008.11.009. doi: 10.1016/j.addbeh.2008.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson CK, de Arellano MA, Kilpatrick DG, Saunders BE, Resnick HS. Child maltreatment in depressed adolescents: Differences in symptomatology based on history of abuse. Child Maltreatment. 2005;10:37–48. doi: 10.1177/1077559504271630. doi: 10.1177/1077559504271630. [DOI] [PubMed] [Google Scholar]
- Danielson CK, McCart MR, de Arellano MA, Macdonald A, Silcott L, Resnick H. Risk reducation for substance use and trama-related psychopathology in adolescent sexual assault victims: Findings from an open trial. Child Maltreatment. 2010a;15:261–268. doi: 10.1177/1077559510367939. doi: 10.1177/1077559510367939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson CK, Macdonald A, Amstadter AB, Hanson R, de Arellano MA, Saunders BE, Kilpatrick DG. Risky behaviors and depression in conjunction with--or in the absence of--lifetime history of PTSD among sexually abused adolescents. Child Maltreatment. 2010b;15:101–107. doi: 10.1177/1077559509350075. doi: 10.1177/1077559509350075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davis SL, Hook EW, Robillard A. Efficacy of an HIV prevention intervention for African American adolescent girls: A randomized controlled trial. Journal of the American Medical Association. 2004;292:171–179. doi: 10.1001/jama.292.2.171. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: A comprehensive, national survey. Child Maltreatment. 2005;10:5–25. doi: 10.1177/1077559504271287. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner H, Ormrod R, Hamby SL. Violence, abuse, and crime exposure in a national sample of children and youth. Pediatrics. 2009;124:1411–1423. doi: 10.1542/peds.2009-0467. doi: 10.1542/peds.2009-0467. [DOI] [PubMed] [Google Scholar]
- Gilboa-Schechtman E, Foa EB, Shafran N, Aderka IM, Powers MB, Rachamim L, Yadin E, Apter A. Prolonged exposure versus dynamic therapy for adolescent PTSD: A pilot randomized controlled trial. JAACAP. 2010;49:1034–1042. doi: 10.1016/j.jaac.2010.07.014. doi: 10.1016/j.jaac.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley J. Problem-solving therapy: New strategies for effective family therapy. San Francisco: Jossey-Bass; 1976. [Google Scholar]
- Henggeler SW, Clingempeel W, Brondino M, Pickrel S. Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:868–874. doi: 10.1097/00004583-200207000-00021. doi: 10.1097/00004583-200207000-00021. [DOI] [PubMed] [Google Scholar]
- Horwitz SM, Hoagwood K, Stiffman AR, Summerfeld T, Weisz JR, Costello EJ, Norquist G. Reliability of the services assessment for children and adolescents. Psychiatric Services. 2001;52:1088–1094. doi: 10.1176/appi.ps.52.8.1088. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on Psychological Science. 2011;6:21–37. doi: 10.1177/1745691610393527. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: An epidemiological and cotwin control analysis. Archives of General Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Kilpatrick D, Ruggiero K, Acierno R, Saunders B, Resnick H, Best C. Violence & risk of PTSD, major depression, substance abuse/dependence, & comorbidity: Results from the NSA. Journal of Consulting & Clinical Psychology. 2003;71:692–700. doi: 10.1037/0022-006x.71.4.692. doi: 10.1037/0022-006X.71.4.692. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The interview schedule for children (ISC): Interrater and parent-child agreement. 1983 Unpublished manuscript. [Google Scholar]
- Marx BP, Calhoun KS, Wilson AE, Meyerson LA. Sexual revictimization prevention: An outcome evaluation. Journal of Consulting and Clinical Psychology. 2001;69:25–32. doi: 10.1037//0022-006x.69.1.25. doi: 10.1037/0022-006X.69.1.25. [DOI] [PubMed] [Google Scholar]
- Moos R, Moos B. FES Manual. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- Mowrer HO. Learning theory and behavior. Hoboken, NJ: John Wiley & Sons Inc.; 1960. [Google Scholar]
- Raundenbush SW, Bryk AS, Cheong YF, Congdon R, du Toit M. HLM 6: Hierarchical linear & nonlinear modeling. Scientific Software International. 2004 [Google Scholar]
- Reynolds CR, Kamphaus RW. BASC: Behavior Assessment System for Children : manual. Circle Pines, MN: American Guidance Service, Inc.; 1992. [Google Scholar]
- Rotheram-Borus MJ, Mahler KA, Koopman C, Langabeer K. Sexual abuse history and associated multiple risk behavior in adolescent runaways. American Journal of Orthopsychiatry. 1996;66:390–400. doi: 10.1037/h0080189. doi: 10.1037/h0080189. [DOI] [PubMed] [Google Scholar]
- Rothman EF, Edwards EM, Heeren T, Hingson RW. Adverse childhood experiences predict earlier age of drinking onset: Results from a representative US sample of current or former drinkers. Pediatrics. 2008;122:298–304. doi: 10.1542/peds.2007-3412. doi: 10.1542/peds.2007-3412. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto: Addiction Research Foundation; 1996. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The UCLA Post-traumatic Stress Disorder Reaction Index. Current Psychiatry Report. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]