Abstract
Objective
This paper describes the development of a theory-guided and evidence-based multimedia training module to facilitate breast cancer survivors’ preparedness for effective communication with their health care providers after active treatment.
Methods
The iterative developmental process used included: (1) theory and evidence-based content development and vetting; (2) user testing; (3) usability testing; and (4) participant module utilization.
Results
Formative evaluation of the training module prototype occurred through user testing (n = 12), resulting in modification of the content and layout. Usability testing (n = 10) was employed to improve module functionality. Preliminary web usage data (n = 256, mean age = 53, 94.5% White, 75% college graduate and above) showed that 59% of the participants accessed the communication module, for an average of 7 min per login.
Conclusion
The iterative developmental process was informative in enhancing the relevance of the communication module. Preliminary web usage results demonstrate the potential feasibility of such a program.
Practice implications
Our study demonstrates survivors’ openness to the use of a web-based communication skills training module and outlines a systematic iterative user and interface program development and testing process, which can serve as a prototype for others considering such an approach.
Keywords: Patient–provider communication, Web-based patient education, Formative evaluation, Usability testing, Breast cancer survivorship
1. Introduction
1.1. Background
Breast cancer is the most common cancer in women, with 86% surviving for at least five years, yielding more than two million US women living with a breast cancer history [1]. An increase in the population of breast cancer survivors has resulted in more women having to manage survivorship issues [2,3]. The Institute of Medicine (IOM) report, From Cancer Patient to Cancer Survivor: Lost in Transition [4], identifies a gap in scientific understanding about the survivor–physician communication process after active treatment, when women tend to feel most isolated from their health care providers and uncertain about the nature of their follow-up care [5–10]. Cancer survivors can have significant difficulty expressing their concerns during the medical visit and thus may refrain from engaging in information-seeking behavior [11]. Providers may therefore underestimate patients’ desires for information and overestimate the adequacy of their own communications [12–15].
1.2. The multimedia communication training module for breast cancer survivors
We developed a stand-alone patient–provider communication training module for breast cancer survivors in conjunction with the development of three innovative multimedia interventions for prostate cancer (Project 1), breast cancer (Project 2) patients, and breast cancer survivors (Project 3) under the Cancer Information Service Research Consortium (CISRC). The CISRC, which has been funded since 1993 by the National Cancer Institute (NCI), has conducted an integrated program of health communications research in partnership with the Cancer Information Service (CIS) of the NCI [16–18].
Using the same metaphor infrastructure as the other projects, the patient–provider communication training module, the focus of this paper, was designed specifically for breast cancer survivors. The objective of the training module is to facilitate the individual’s expression of concerns and goals during follow-up consultations with the medical team. To facilitate participants’ access to the program, we produced both website and CD-ROM versions [19,20]. This paper highlights the iterative developmental process used to design the module and presents initial module usage data obtained from the parent randomized trial currently underway.
2. Methods
2.1. Survivorship communication module components and description
Building on health communication principles and evidence-based tools to manage breast cancer survivorship issues, the module contains the following.
2.1.1. Text-based educational training
This component provides survivors with text-based instructional training content aimed at increasing knowledge and clarifying expectancies [21–24].
2.1.2. Role modeling video
The peer-modeling video illustrates a hypothetical “effective” interaction between a doctor and a mock breast cancer survivor, discussing the survivor’s fatigue concern [8,25].
2.1.3. Interactive question prompt list
A 80-question prompt list allows users to interactively view, select, and print questions pertinent to their post-treatment needs [7].
2.1.4. Survivorship care plan and adjuvant treatment summary
To emphasize the importance of personal medical records in facilitating the coordination between primary doctors and specialists during the post-treatment phase, we adapted the survivorship care plan and adjuvant treatment summary forms developed by the American Society of Clinical Oncology (ASCO) (with permission).
2.1.5. Health care team roles
To help survivors maximize their use of resources, we included an NCI fact sheet that describes various health care professional roles.
2.2. Developmental process and formative evaluation
2.2.1. Content development and initial prototype
We conducted a comprehensive theory-guided literature review and evidence-based content review to identify material for the module. The communication module was conceptualized by an integrated framework, the Cognitive-Social Health Information Processing (C-SHIP) Model [26] [27] and also modeled in part on the PACE system, designed to train adult patients to communicate more effectively during the medical visit by: Presenting detailed information, Asking questions, Checking their understanding of information, and Expressing any concerns [21–24]. Working with a team of literacy and patient education experts, we revised existing content and developed new breast cancer survivorship specific materials designed for a 7th grade reading level, as evaluated through plain language testing. In accordance with health communication best practices, we employed key messages, active verbs, short sentences, and chunking information, as well as visual cues and photographs, to maximize the appeal of, and engagement in, the module. Once the content was approved by the NCI CIS Office, an intensive planning process was implemented.
2.2.2. User testing of the survivorship communication training module
In the early phase of development, we conducted user testing with breast cancer survivors to assess the extent to which the module prototype and the materials were personally relevant and easily interpreted. Survivors were asked if they found the content topics helpful and if they thought other survivors would use the materials. Evaluative feedback was collected iteratively and used to refine the module prototype.
2.2.3. Usability testing of the survivorship communication training module
Based on NCI usability guidelines, participants were instructed to review the final prototype using the “task analysis” method to look for specific information and to use specific tools in the module [28]. Participants worked through task scenarios and explained what they were doing by “thinking aloud” [29]. Usability interviews were conducted with the Morae recorder system [30,31], in which participants’ real-time expressions (both facial and verbal) were recorded during their interaction with the prototype. Two research team members reviewed each of the usability testing video clips to identify navigational difficulties. Final module modifications were implemented to correct programming problems detected.
2.2.4. Preliminary usage of the survivorship communication training module from the randomized trial
The Project 3 breast cancer survivorship parent program is currently being evaluated in a clinical trial. Eligible participants were recruited from callers to the NCI’s CIS and the ACS’s National Cancer Information Center, as well as from the Love/Avon Army of Women website and email database, where potential study participants were prompted to call either the CIS or the CISRC project office for study enrollment. The eligibility criteria include callers who: (1) are diagnosed with invasive breast cancer and no confirmed metastasis; (2) anticipate treatment completion within 1 month or completed medical treatment fewer than 6 months previously; (3) can receive intervention in English; (4) can provide informed consent to receive intervention and complete follow-up assessments; and (5) have computer access. Demographic data are assessed at baseline interview. To track participants’ use of the program, we include web usage data of participants who accessed the program via the internet (as opposed to the CD-ROM) from January 2009 to February 2010, including total session time during their first session access, calculated from time of first hit on the communication module to time of the last hit.
3. Results
3.1. User testing of the survivorship communication training module
Twelve early stage breast cancer survivors were recruited to evaluate evolving versions of the content topics, mock storyboards, and components of the module prototype. Survivors were recruited from the Fox Chase Cancer Center Breast Cancer Support Group, with ages ranging from 47 to 68. All women had completed their active breast cancer treatment; 11 were Caucasian and one was African American. Examples of participant feedback and resulting modifications to the module selected from 25 identified issues are shown in Table 1. Overall, 11 participants reported that they found the module content helpful and would suggest that other breast cancer survivors use it.
Table 1.
Findings and recommendations from user testing.
| User feedback from user testing | Revision in the communication module |
|---|---|
| Individual components do not “stand out” on the module front page. | Module interface was redesigned to use graphical cues and key definitions to highlight the content of each component. |
| Patient in the video looked too young for a breast cancer survivor. | Role modeling video was re-filmed with a more appropriate actress. |
| The overall module layout feels kind of “cold”. | Pictures of clinicians and survivors were added to “warm up” the module look. |
| The prompt question list was helpful but I still have to write it down. | A “check and print” function was added so users could print selected questions. |
3.2. Usability testing of the survivorship communication training module
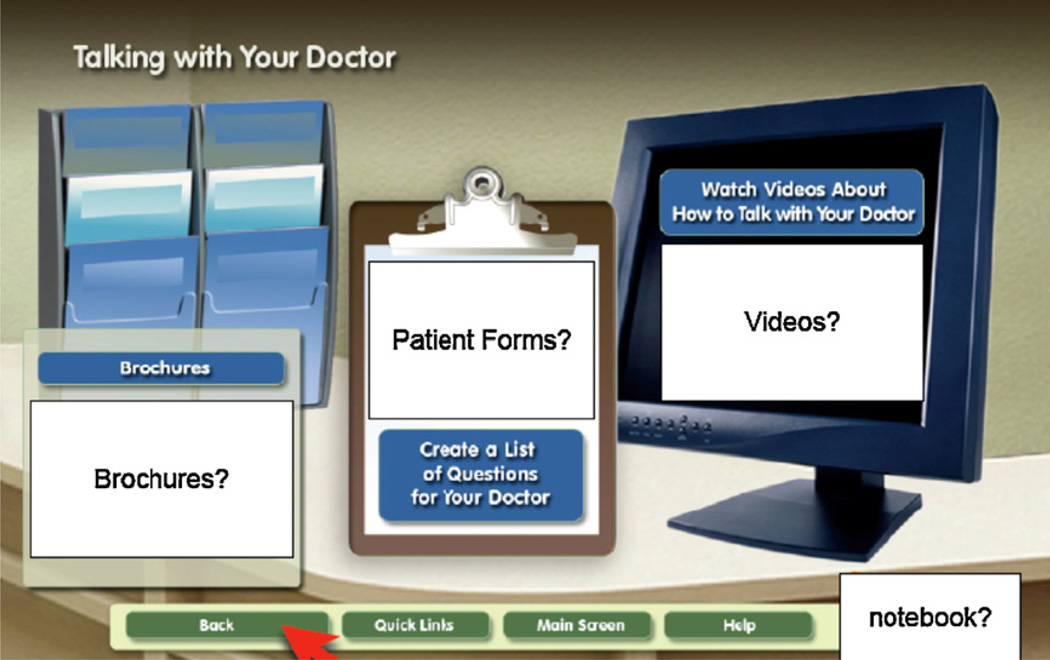
Because the goal of usability testing focuses on navigation and functionality rather than on module concept or content, we included both breast cancer survivors (n = 5) and other women (n = 5) of the same age range as participants. Age of participants ranged from 45 to 58 years, on average they had completed high school, and nine of ten women were Caucasian. The usability video clips revealed a total of 20 system errors and navigational confusions that needed improvement (Table 2 lists five examples). Fig. 1 shows an early prototype mockup of the module’s front page; Fig. 2 is the final version which includes improvements in the module’s front page presentation, graphical cues, component layout, and color and text style.
Table 2.
Findings and recommendations from usability testing.
| Observation feedback from usability testing | Revision in the communication module |
|---|---|
| Participants were not clear that they could move between four tab pages by clicking on the “tab” interface. | Directions were added at the beginning of the tutorial to explain how to move between tabs. The titles on each tab (i.e., Presenting Information) were also highlighted and underlined to indicate that they are clickable. |
| Participants had problems using the interactive question prompt list. | Additional text and step-by-step graphic of the functionality of the interactive question prompt list were added at the beginning of the component to demonstrate how to review, select, and print sample questions. |
| Participants were not clear that they can click on the role-modeling video clips. | We added a “Watch Video” button under each video clip so it is clear that clicking on the button would start the video clip. |
| Participants were unsure how to move to the next page on the PACE content. | We added “To read more, click “Next” below” over the Next button, along with a directional arrow. |
| Participants were unsure how to go back to the previous page after opening up a new subcomponent. | We added a “Close” button at the upper right corner of the each popped up subcomponent. Once they clicked on the Close button, participants would be brought back to the previous higher-level page automatically. |
Fig. 1.
An early prototype mockup of the survivorship communication training module front page.
Fig. 2.
A final screenshot of the survivorship communication training module front page.
3.3. Preliminary usage of the survivorship communication training module from the randomized trial
We used the web tracking data of the first 256 participants in the randomized clinical trial who accessed the parent program via the Internet from January 2009 to February 2010. Table 3 shows that the majority of participants were Caucasian breast cancer survivors with a median age of 53, a college education or higher, household income of $80,000 or greater, and access to health care providers and insurance.
Table 3.
Study participant demographic characteristics.
| Total N = 256 | Mean | Min–max |
|---|---|---|
| Age | 53 | 29–81 |
| N | % | |
| Race | ||
| Non Hispanic White | 242 | 94.5% |
| African American | 6 | 2.3% |
| Hispanic or Latino | 3 | 1.2% |
| Asian | 3 | 1.2% |
| Native Hawaiian or other Pacific Islander | 1 | 0.4% |
| Other | 1 | 0.4% |
| Highest level of education | ||
| High school graduate | 12 | 4.7% |
| Some college | 52 | 20.3% |
| College graduate | 101 | 39.5% |
| Post-graduate | 91 | 35.5% |
| Household income | ||
| Less than $40,000 | 24 | 9.4% |
| $40,000–79,000 | 68 | 26.5% |
| $80,000 or more | 149 | 58.2% |
| Do not know/refused | 15 | 5.9% |
| Regular health care access | ||
| Yes | 249 | 97.3% |
| No | 7 | 2.7% |
| Health care insurance | ||
| Yes | 256 | 100% |
Fifty-nine percent (n = 152) accessed the survivorship communication training module during the 13-month period. Of these, the majority (53.6%) used the module for up to 5 min during their first module access. The median time spent during the first module session access was 4 min and the average time spent was 7 min. Approximately 26% of users spent 10 min or longer accessing information from the module during their first session. The most frequently accessed component across users was the survivorship care plan (71.7%), followed by the adjuvant treatment summary (67.8%), interactive question prompt list (64.5%), health care team roles (61.2%), text-based educational materials (48.7%), and role modeling video (25.7%).
4. Discussion and conclusion
4.1. Discussion
Using an iterative developmental process and a multidisciplinary team approach, the survivorship communication training module was progressively developed and refined based on formative participant user and usability evaluation data. Compared to previous studies [2,3,32], preliminary web usage results from the ongoing randomized trial indicated that 59% of study participants used the communication module via the Internet, highlighting the module’s potential applicability to survivors. Over a quarter of the Internet users (26%) spent more than 10 min; another one half devoted 5 min or slightly less.
The finding that ASCO’s survivorship care plan and adjuvant treatment summary were the most frequently accessed components suggests that women are interested in obtaining materials that will facilitate continuity of care after completion of their medical treatment. Consistent with the IOM’s recommendation [4], there is a need to summarize cancer patients’ course of treatment into formal documents that also include recommendations for subsequent survivorship care management [33]. Our data show that even highly educated breast cancer survivors, as in our sample, are interested in these materials. Future studies should explore minority, underserved, and underinsured survivors’ reactions to the uptake of these materials in a web-based delivery format.
The finding that the interactive question prompt list was frequently accessed among this highly educated cohort of survivors highlights survivors’ need to frame questions for discussion with their health care providers. The low usage of the role modeling video also warrants research attention. A possible explanation is that the video and narrative story-telling approach may be more acceptable among minority populations [34,35] and our sample was predominately Caucasian. In subsequent usage analyses, we will explore what factors influence the use of content areas and formats, which will inform the design of future intervention studies to tailor more customized messages [36]. We will also examine amount of use as related to expected use over time in the context of participant’s outcomes across different user profiles.
4.2. Limitations
First, the samples for the user and usability testing were not ethnically diverse. The samples were predominantly Caucasians with high levels of education and income. Second, due to the fact this is an ongoing study, we are not yet able to report process and outcome variables. Third, we do not have data on use of the communication module via CD-ROM; thus, findings apply only to participants who accessed the program via the Internet.
4.3. Conclusion
The survivorship communication training module was developed and enhanced using feedback from the target audience during a systematic iterative developmental process. Participants’ preliminary usage provides support for the potential of the multimedia communication training intervention for breast cancer patients who are completing their active medical treatments and transitioning into survivorship.
4.4. Practice implications
Our study demonstrates that the breast cancer population is open to using a communication module designed to help address unresolved or confusing consultation and survivorship issues. We also outlined an iterative systematic multimedia program development and user interface testing process that can serve as a prototype for others considering this approach.
Acknowledgments
The project described is supported by NIH Grants 5-PO1-CA057596 and P30 CA006927 from the National Cancer Institute. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute, National Institutes of Health. In collaboration with the NCI’s Cancer Information Service (CIS) the research project and core resources support the work reported in this article are:
The Intervention Development and Measurement Core (PI: Suzanne M. Miller, PhD), responsible for developing and producing study interventions, including the multimedia education programs, and for ensuring standardization and quality control of the intervention and assessment protocols across projects, as well as taking the lead on designing and producing the communication module reported here.
Project 3 (PI: Annette L. Stanton, PhD), Pathways to Recovery after Breast Cancer Treatment, is aimed at CIS callers who will soon complete or have recently completed their primary treatments for breast cancer. Stanton and Jorge took the lead on selecting and developing content for the communication module reported here, in collaboration with the Intervention Development and Measurement Core.
The Administrative Core (PI: Alfred C. Marcus, PhD), responsible for coordinating and facilitating all administrative aspects of the Cancer Information Service Research Consortium (CISRC).
We thank the CIS Project Office and Regional Staff for survivorship content review and approval, and Fox Chase Cancer Center’s Psychosocial and Biobehavioral Medicine Department, Behavioral Research Core Facility, and Office of Health Communications and Health Disparities’ Resource Education Center for recruitment and assistance in usability testing.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Verheijden MW, Jans MP, Hildebrandt VH, Hopman-Rock M. Rates and determinants of repeated participation in a web-based behavior change program for healthy body weight and healthy lifestyle. J Med Internet Res. 2007;9(1):pe1. doi: 10.2196/jmir.9.1.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van’t Riet J, Crutzen R, De Vries H. Investigating predictors of visiting, using, and revisiting an online health-communication program: a longitudinal study. J Med Internet Res. 2010;12(3):e37. doi: 10.2196/jmir.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hewitt M, Greenfield S, Stovall E. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: Institute of Medicine, National Academies Press; 2006. [Google Scholar]
- 5.Ganz PA. Monitoring the physical health of cancer survivors: a survivorship-focused medical history. J Clin Oncol. 2006;24(32):5105–5111. doi: 10.1200/JCO.2006.06.0541. [DOI] [PubMed] [Google Scholar]
- 6.Ganz PA, Rowland JH, Desmond K, Meyerowitz BE, Wyatt GE. Life after breast cancer: understanding women’s health-related quality of life and sexual functioning. J Clin Oncol. 1998;16(2):501–514. doi: 10.1200/JCO.1998.16.2.501. [DOI] [PubMed] [Google Scholar]
- 7.Stanton AL. Psychosocial concerns and interventions for cancer survivors. J Clin Oncol. 2006;24(32):5132–5137. doi: 10.1200/JCO.2006.06.8775. [DOI] [PubMed] [Google Scholar]
- 8.Stanton AL, Ganz PA, Kwan L, Meyerowitz BE, Bower JE, Krupnick JL, et al. Outcomes from the moving beyond cancer psychoeducational, randomized, controlled trial with breast cancer patients. J Clin Oncol. 2005;23(25):6009–6018. doi: 10.1200/JCO.2005.09.101. [DOI] [PubMed] [Google Scholar]
- 9.Hudson SV, Chubak J, Coups EJ, Blake-Gumbs L, Jacobsen PB, Neugut AI, et al. Identifying key questions to advance research and practice in cancer survivorship follow-up care: a report from the ASPO Survivorship Interest Group. Cancer Epidemiol Biomar Prev. 2009;18(7):2152–2154. doi: 10.1158/1055-9965.EPI-18-7-ASPO01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hudson S, Hahn K, Ohman-Strickland P, Cunningham R, Miller S, Crabtree B. Breast, colorectal and prostate cancer screening for cancer survivors and non-cancer patients in community practices. J Gen Intern Med. 2009;24(0):487–490. doi: 10.1007/s11606-009-1036-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luker KA, Beaver K, Leinster SJ, Owens RG. Information needs and sources of information for women with breast cancer: a follow-up study. J Adv Nurs. 1996;23(3):487–495. doi: 10.1111/j.1365-2648.1996.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 12.Arora NK. Interacting with cancer patients: the significance of physicians’ communication behavior. Soc Sci Med. 2003;57(5):791–806. doi: 10.1016/s0277-9536(02)00449-5. [DOI] [PubMed] [Google Scholar]
- 13.Beisecker AEP, Beisecker TDP. Patient information-seeking behaviors when communicating with doctors. Med Care. 1990;28(1):19–28. doi: 10.1097/00005650-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Quirt CF, Mackillop WJ, Ginsburg AD, Sheldon L, Brundage M, Dixon P, et al. Do doctors know when their patients don’t? A survey of doctor–patient communication in lung cancer. Lung Cancer. 1997;18(1):1–20. doi: 10.1016/s0169-5002(97)00048-2. [DOI] [PubMed] [Google Scholar]
- 15.Hack TF, Degner LF, Parker PA, Team TSC. The communication goals and needs of cancer patients: a review. Psycho-Oncology. 2005;14(10):831–845. doi: 10.1002/pon.949. [DOI] [PubMed] [Google Scholar]
- 16.Marcus A, Morra ME, Bright MA, Fleisher L, Kreps G, Perocchia R. The CIS model for collaborative research in health communications: a brief retrospective from the current generation of research. J Health Commun. 2005;10:235–245. doi: 10.1080/10810730500263612. [DOI] [PubMed] [Google Scholar]
- 17.Marcus AC, Morra ME, Bettinghaus E, Crane LA, Cutter G, Davis S, et al. The cancer information service research consortium: an emerging laboratory for cancer control research. Prevent Med. 1998;27:S3–S15. doi: 10.1006/pmed.1998.0245. [DOI] [PubMed] [Google Scholar]
- 18.Perocchia R, Hodorowski J, Williams L, Kornfeld J, Davis N, Monroe M, et al. Patient-centered communication in cancer care: the role of the NCI’s cancer information service. J Cancer Educ. 2010:1–8. doi: 10.1007/s13187-010-0121-y. [DOI] [PubMed] [Google Scholar]
- 19.Bright MA, Fleisher L, Thomsen C, Morra ME, Marcus A, Gehring W. Exploring e-health usage and interest among cancer information service users: the need for personalized interactions and multiple channels remains. J Health Commun Int Perspec. 2005;10(7 Suppl. 1):35–52. doi: 10.1080/10810730500265609. [DOI] [PubMed] [Google Scholar]
- 20.Marcus AC, Diefenbach MA, Stanton AL, Miller SM, Fleisher L, Raich PC, Morra ME, Perocchia RS, Tran ZV, Bright MA. On behalf of the CISRC research team, Cancer patient and survivor research from the Cancer Information Service Research Consortium: A preview of three large randomized trials and initial lessons learned. J Health Commun. doi: 10.1080/10810730.2012.743629. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cegala DJ, Marinelli T, Post D. The effects of patient communication skills training on compliance. Arch Fam Med. 2000;9(1):57–64. doi: 10.1001/archfami.9.1.57. [DOI] [PubMed] [Google Scholar]
- 22.Cegala DJ, McClure L, Marinelli TM, Post DM. The effects of communication skills training on patients’ participation during medical interviews. Patient Educ Couns. 2000;41(2):209–222. doi: 10.1016/s0738-3991(00)00093-8. [DOI] [PubMed] [Google Scholar]
- 23.Cegala DJ, Post DM, McClure L. The effects of patient communication skills training on the discourse of older patients during a primary care interview. J Am Geriatr Soc. 2001;49(11):1505–1511. doi: 10.1046/j.1532-5415.2001.4911244.x. [DOI] [PubMed] [Google Scholar]
- 24.Cegala DJ, Post DM. The impact of patients’ participation on physicians’ patient-centered communication. Patient Educ Couns. 2009;77(2):202–208. doi: 10.1016/j.pec.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 25.Kreuter MK, Green MC, Cappella JN, Slater MD, Wise M, Storey D, et al. Narrative communication in cancer prevention and control: a framework to guide research and application. Ann Behav Med. 2007;33:221–235. doi: 10.1007/BF02879904. [DOI] [PubMed] [Google Scholar]
- 26.Miller SM, Diefenbach MA. C-SHIP: a cognitive-social health information processing approach to cancer. In: Medicine D, Krantz, editors. Perspectives in Behavioral. NJ: Lawrence Erlbaum; 1998. pp. 219–244. [Google Scholar]
- 27.Miller SM, Shoda Y, Hurley K. Applying cognitive-social theory to health-protective behavior: breast self-examination in cancer screening. Psychol Bull. 1996;119:70–94. doi: 10.1037/0033-2909.119.1.70. [DOI] [PubMed] [Google Scholar]
- 28.Nielsen J. Usability Engineering. Cambridge, MA: Academic Press; 1993. [Google Scholar]
- 29.Monique WMJ, Thiemo S, Cor van den B, Maud G. The think aloud method: a guide to user interface design. Int J Med Inform. 2004;73(11):781–795. doi: 10.1016/j.ijmedinf.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 30.Morae Techsmith: Usability Testing for Software and Websites. http://www.techsmith.com/morae.asp.
- 31.Capra M, Andre T, Brandt J, Collingwood I, Kempic J. Practical tips for designing a usability evaluation environment: what equipment and software do you really need? Human Factors and Ergonomics Society Annual Meeting Proceedings. 2009;vol 53:1517–1521. [Google Scholar]
- 32.Eysenbach G. The law of attrition. J Med Internet Res. 2005;7(1):e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ganz PA, Hahn EE. Implementing a survivorship care plan for patients with breast cancer. J Clin Oncol. 2008;26(5):759–767. doi: 10.1200/JCO.2007.14.2851. [DOI] [PubMed] [Google Scholar]
- 34.Kreuter MW, Holmes K, Alcaraz K, Kalesan B, Rath S, Richert M, et al. Comparing narrative and informational videos to increase mammography in low-income African American women. Patient Educ Couns. 2010;81:S6–S14. doi: 10.1016/j.pec.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chiu L. Culturally competent health promotion: the potential of participatory video for empowering migrant and minority ethnic communities. Int J Migr Health Social Care. 2009;5(1):5–14. [Google Scholar]
- 36.Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res. 2008;23(3):454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]